Académique Documents
Professionnel Documents
Culture Documents
Primary Care Issues Paper Correct
Transféré par
AlexanderWarrenTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Primary Care Issues Paper Correct
Transféré par
AlexanderWarrenDroits d'auteur :
Formats disponibles
Running head: NEED FOR AUTHORITY AND AUTONOMY FOR NURSES
The Need for an Increased Level of Authority and Autonomy
for Advanced Practice Nurses
Alexander Warren, R.N.
Scholarly Report
Dr. Zelda Peters D.N.P
Albany State University
10/08/2014
NEED FOR AUTHORITY AND AUTONOMY FOR NURSES
The Need for an Increased Level of Authority and Autonomy for Advanced Practice Nurses
Nurse practitioners are an integral part of health care here in the United States and have
been for decades. It is hard to understand not only the discrepancies in their ability to practice
across state lines but also their limitations as health care providers. What could be the benefits of
the barriers to practice? The role of Advanced Practice Nurses (APNs) is confused by these
restrictions and can cause communication difficulties between APNs and other providers and
APNs. Ultimately this can be detrimental to the patient and hinder his or her ability to receive
quality health care. If APNs cannot gain full autonomy a set standard regarding their ability to
provide care nationwide is needed.
When discussing the autonomy of APNs, patients become concerned about the level of
care they are provided when they are treated by non-physicians. This is a valid concern, and
several studies have attempted to determine if non-physicians provide comparable quality of care
relative to doctors. One such study attempted to determine not only how the overall care of nonphysicians compared to that of physicians but how their care concerning a particular disease
process compared. In blood pressure control, length of hospital stay, mortality, duration of
ventilation, hospitalization/rehospitalization rates, and care provided in the emergency
department, non-physicians provided comparable care and comparable outcomes (Newhouse et
al., 2011). In the same study, lipid control was better achieved under the care of non-physicians
than physicians (Newhouse et al., 2011). The need for lawmakers to understand the capability of
APNs to provide care is paramount. With the growing population, the need for expanded
provider roles for APNs is crucial.
The elderly population is growing and is in need health care providers. With the baby
boomers achieving retirement age, the need for healthcare, especially providers, will be at a
NEED FOR AUTHORITY AND AUTONOMY FOR NURSES
premium. By 2030, 20% of the population in the United States will be aged 65 years or older.
That is a staggering 72.1 million people who will be in need of health care (McGill, 2013). How
can we possibly provide care to another 72.1 million patients using our current health care
system? Mid-level providers must be granted increased autonomy and authority to help control
the flood of new patients.
Mid-level providers were instituted to fill the gap in health care. We already know that
there are more senior citizens than can be adequately provided for by the current ranks of family
practice physicians. This does not include the specialties that also need covering by medical
doctors. Nurse practitioners and physicians assistants, the mid-levels, are the family practice
providers of the future. This is especially true in more rural areas where hospitals and large
practices already have a difficult time recruiting and retaining physicians. The Federal Office of
Rural Health Policy states that 77% of rural counties are facing a physician shortage and 8% do
not have any primary care providers at all (Kutscher, 2013). The number of primary care
providers in rural areas will only continue to decline. APNs will have to be the providers to fill
that gap. We cannot have a larger deficit than we currently have, with current patients having to
drive long distances to see a provider.
The cost of health care is climbing, and patients are having a difficult time affording their
copays, not to mention subsequent bills and medications. The majority of Medicare patients
struggle to pay their bills since most live on a fixed income. Working in home health, I have
come across several patients that had to choose between buying groceries and buying their
medications. Even on Medicare, these patients have a responsibility to pay for a portion of their
health care, and the combination of a few comorbidities raises the amount they will have to pay.
We, as a country, have to make changes to help decrease the cost of providing health care, not
NEED FOR AUTHORITY AND AUTONOMY FOR NURSES
only to Medicare patients but to everyone. APNs can help regulate the high costs of health care.
Currently, APNs are being reimbursed at a rate of 85% of what a physician would be paid
(American Association of Nurse Practitioners, 2013). This 15% reduction in cost may seem
small, but if half of the primary care visits in the nation were performed by APNs, this would
represent a substantial cost savings. There is one reported instance where a single nurse
practitioner ran a worksite clinic. This resulted in direct medical savings of $2.18 million dollars
over the course of two years (Iowa Nurses Association, 2012). The total of $2.18 million dollars
did not include the savings the company made by not having to pay for lost productivity or
absences. This shows the flexibility provided when nurse practitioners practice under their own
license. APNs have the potential to work independently for corporations, run on-site clinics, do
yearly physicals, and potentially save companies millions of dollars. It is also shown that nurse
practitioners are more thoughtful when it comes to the price of medications they are prescribing.
Nurse practitioners prescribe more generic medications in lieu of the more costly brand name
medications, resulting in saved medical costs for the patient (Iowa Nurses Association, 2012).
The burden of health care costs is far-reaching. Granting full autonomy in practice to nurse
practitioners is one possible method of decreasing those costs.
Across the country, the level of practice that APNs can provide varies dramatically.
Every state has different laws concerning the practice of APNs and what is required of them to
practice under physicians. This creates confusion between the APN and his or her physician.
Not only do laws that affect ones ability to practice vary from state to state but ones title also
changes. Some states do not designate a difference between titles such as Psychiatric Nurse
Practitioner and Psychiatric Clinical Nurse Specialist. In some states, both of these titles get
lumped into the all-encompassing and confusing title of Advanced Practice Nurse. This can
NEED FOR AUTHORITY AND AUTONOMY FOR NURSES
happen with any nurse specialist and obscures the nurses abilities and scope of practice. How
can we expect physicians to understand the subtleties of our abilities to practice if the states
cannot decide on a standard form of title? The need for national standards in scope of practice
and title designation is important for the advancement of all APNs.
Advanced Practice Nurses are trying to change this situation. Currently, they are
proposing the Consensus Model for Advanced Practice Registered Nurse (APRN) Regulation.
This model attempts to set standards for titles and defines a set of guidelines that must be met
prior to the nurse functioning as an Advanced Practice Nurse. The model also sets standards on
accreditation, education, and certification. In doing so, it attempts to create a uniform model for
APRNs throughout the United States. It is essential that nurses themselves endorse a uniform set
of standards for practice. If we cannot agree on what our abilities and titles should be, how can
we expect the government to make laws regulating set standards?
Job satisfaction is something everyone strives for, and APRNs are no different. With
restrictions placed on their scopes of practice and feelings of constantly being monitored by
physicians, their job effectiveness diminishes. All practitioners feel they have the education and
ability to diagnose and prescribe; APRNs are specifically trained to do so. Yet with all the
education, APNs are still limited in their abilities. This limitation causes a decrease in job
satisfaction. An APN at a nurse managed health center (NMHC) has an increased level of
autonomy in comparison to an APN who works at a physician's office. One study revealed that
98% of APNs who work in a NMHC would recommend this type of work to new APNs (Pron,
2013). Their perceived autonomy was also high. Even in states that disallowed full prescriptive
authority, the APNs who worked in NMHCs felt as if their autonomy was greater. The feeling of
NEED FOR AUTHORITY AND AUTONOMY FOR NURSES
being able to practice at your full potential is an important goal of many APNs and leads to much
higher job satisfaction.
With more than 47 million people in the United States without health insurance, we are
seeing more convenient care clinics (CCC) providing care for non-chronic health issues (Evans,
2010). Patients need care for their acute illnesses like sore throats, upper respiratory tract
infections, rashes, and fevers. These patients do not have medical insurance, so these CCCs fill a
gap of care. There are now over 1000 CCCs nationwide, and they are expanding quickly (Evans,
2010). Advanced Practice Nurses are the primary care providers in these clinics, and they are
providing an invaluable resource. These patients without health insurance need no less health
care than patients who are covered. APN led care clinics are the primary care provider system of
the future, and the need for increased autonomy/authority is integral for appropriate delivery of
this care.
With the increasing need for primary care providers, the advanced practice nurse is
becoming ever more important in our health care system. Current laws vary significantly across
states regarding the APNs ability to practice and prescribe medications autonomously. This
discrepancy from state to state causes confusion with physicians and patients which inhibits the
APNs ability to provide care. The cost of healthcare is ballooning, and the number of people
without insurance in the United States continues to grow. Mid-levels, like APNs, are the future
of providing family practice medicine, and nurse led CCCs are helping to provide care to
underprivileged and uninsured patients. We need increased autonomy for APNs and a standard
level of practice nationwide to help provide quality care to the masses.
NEED FOR AUTHORITY AND AUTONOMY FOR NURSES
References
American Association of Nurse Practitioners. (2013). Fact sheet: Medicare reimbursement.
Retrieved from http://www.aanp.org/practice/reimbursement/68-articles/325-medicarereimbursement
Evans, S. W. (2010). Convenient care clinics: Making a positive change in health care. Journal
of the American Academy Of Nurse Practitioners, 22, 23-26. doi:10.1111/j.17457599.2009.00466.x
Iowa Nurses Association. (2012, December). The cost effectiveness of nurse practitioner care.
Iowa Nurse Reporter, 25(3), 10-12.
Kutscher, B. (2013). The rural route. Hospitals in underserved areas taking different roads to
recruit, retain physicians. Modern Healthcare, 43(18), 30-31.
McGill, N. (2013). As senior population grows, aging in place gains popularity: Communities
conducting outreach. The Nation's Health, 43(8), 1-16. Retrieved from
http://thenationshealth.aphapublications.org/content/43/8/1.2.full
Newhouse, R. P., Stanik-Hutt, J., White, K. M., Johantgen, M., Bass, E. B., Zangaro, G., & ...
Weiner, J. P. (2011). Advanced practice nurse outcomes 1990-2008: A systematic
review. Nursing Economic$, 29(5), 1-22.
Pron, A. L. (2013). Job satisfaction and perceived autonomy for nurse practitioners working in
nurse-managed health centers. Journal of The American Association Of Nurse
Practitioners, 25(4), 213-221. doi:10.1111/j.1745-7599.2012.00776.x
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Urgent Care Calendar and ObjectivesDocument3 pagesUrgent Care Calendar and ObjectivesAlexanderWarrenPas encore d'évaluation
- Soap Note Mary HailshamDocument1 pageSoap Note Mary HailshamAlexanderWarren0% (1)
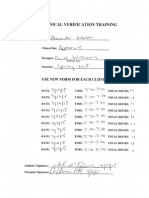
- Applecare Clinical VerificationDocument1 pageApplecare Clinical VerificationAlexanderWarrenPas encore d'évaluation
- Conference CertificateDocument1 pageConference CertificateAlexanderWarrenPas encore d'évaluation
- Primary Care Clinical Verification LogDocument2 pagesPrimary Care Clinical Verification LogAlexanderWarrenPas encore d'évaluation
- Practicum Episodic 3Document2 pagesPracticum Episodic 3AlexanderWarren100% (1)
- Primary Care Clinical Verification LogDocument2 pagesPrimary Care Clinical Verification LogAlexanderWarrenPas encore d'évaluation
- Clinical LogsDocument601 pagesClinical LogsAlexanderWarrenPas encore d'évaluation
- Urgent Care Calendar and ObjectivesDocument2 pagesUrgent Care Calendar and ObjectivesAlexanderWarrenPas encore d'évaluation
- Urgent Care Calendar and ObjectivesDocument2 pagesUrgent Care Calendar and ObjectivesAlexanderWarrenPas encore d'évaluation
- Urgent Care Calendar and ObjectivesDocument3 pagesUrgent Care Calendar and ObjectivesAlexanderWarrenPas encore d'évaluation
- Primary Care Calendar and ObjectivesDocument3 pagesPrimary Care Calendar and ObjectivesAlexanderWarrenPas encore d'évaluation
- Episodic 1Document6 pagesEpisodic 1AlexanderWarrenPas encore d'évaluation
- Episodic 2Document5 pagesEpisodic 2AlexanderWarrenPas encore d'évaluation
- Applecare Objectives ChecklistDocument1 pageApplecare Objectives ChecklistAlexanderWarrenPas encore d'évaluation
- Applecare Student EvalDocument2 pagesApplecare Student EvalAlexanderWarrenPas encore d'évaluation
- Conference SummaryDocument6 pagesConference SummaryAlexanderWarrenPas encore d'évaluation
- Applecare Clinical Site EvalDocument2 pagesApplecare Clinical Site EvalAlexanderWarrenPas encore d'évaluation
- NPI SignatureDocument3 pagesNPI SignatureAlexanderWarrenPas encore d'évaluation
- Georgia SignatureDocument13 pagesGeorgia SignatureAlexanderWarrenPas encore d'évaluation
- Business PlanDocument5 pagesBusiness PlanAlexanderWarrenPas encore d'évaluation
- DEA SignatureDocument4 pagesDEA SignatureAlexanderWarrenPas encore d'évaluation
- Initial DiscussionDocument1 pageInitial DiscussionAlexanderWarrenPas encore d'évaluation
- Employee ContractDocument5 pagesEmployee ContractAlexanderWarrenPas encore d'évaluation
- ResponseDocument1 pageResponseAlexanderWarrenPas encore d'évaluation
- Midterm Clinical Site EvalDocument2 pagesMidterm Clinical Site EvalAlexanderWarrenPas encore d'évaluation
- Collaborative AgreementDocument3 pagesCollaborative AgreementAlexanderWarrenPas encore d'évaluation
- Final Summary of Clinical Experience PDFDocument2 pagesFinal Summary of Clinical Experience PDFAlexanderWarrenPas encore d'évaluation
- Final Summary of Clinical Experience PDFDocument2 pagesFinal Summary of Clinical Experience PDFAlexanderWarrenPas encore d'évaluation
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- ACFrOgAUTMl8Xt31z9R Bha0n5a c1S2g31eEYqYd9r9EG1r7I6PoFo9orDZoay8eaEN1BNbXyne01QqUo19M2cM60XJO4QgQ2RtpPLz 4 Uo9 KQ6EE7HLrMsLpIEsDocument14 pagesACFrOgAUTMl8Xt31z9R Bha0n5a c1S2g31eEYqYd9r9EG1r7I6PoFo9orDZoay8eaEN1BNbXyne01QqUo19M2cM60XJO4QgQ2RtpPLz 4 Uo9 KQ6EE7HLrMsLpIEsPaul Bedard98% (62)
- Ateneo de Manila University Philippine StudiesDocument17 pagesAteneo de Manila University Philippine StudiesJearim FamosoPas encore d'évaluation
- Policy Write Up GMC200 Great EasternDocument15 pagesPolicy Write Up GMC200 Great EasternPrakash VellayanPas encore d'évaluation
- MediCard Outpatient FormDocument1 pageMediCard Outpatient FormMichael Vincent DosadoPas encore d'évaluation
- Health 1Document527 pagesHealth 1venika SharmaPas encore d'évaluation
- January 20, 2016 Tribune Record GleanerDocument16 pagesJanuary 20, 2016 Tribune Record GleanercwmediaPas encore d'évaluation
- Wage and Tax Statement: Copy B - To Be Filed With Employee's FEDERAL Tax ReturnDocument7 pagesWage and Tax Statement: Copy B - To Be Filed With Employee's FEDERAL Tax ReturnLovely HeartPas encore d'évaluation
- Annual Report 2010Document56 pagesAnnual Report 2010amatamesPas encore d'évaluation
- 2021.02.24 Gette Final TrialDocument19 pages2021.02.24 Gette Final TrialBrigette DomingoPas encore d'évaluation
- Ncci EditsDocument18 pagesNcci EditsJeswin JosePas encore d'évaluation
- 2024 Medicard IF Application FormDocument2 pages2024 Medicard IF Application FormAlyzza EscalantePas encore d'évaluation
- Contact List 10.05.2023Document37 pagesContact List 10.05.2023John Benedict Sta AnaPas encore d'évaluation
- History of Health SpendingDocument37 pagesHistory of Health SpendingDouglas EstradaPas encore d'évaluation
- Dental Service Trends For Older U.S. Adults, 1998-2006: ArticleDocument7 pagesDental Service Trends For Older U.S. Adults, 1998-2006: ArticleKhalid AhmedPas encore d'évaluation
- HMKP 115 IF00 Transcript 20170308Document1 271 pagesHMKP 115 IF00 Transcript 20170308mokilpoPas encore d'évaluation
- Pro Health Billing Setup GuideDocument22 pagesPro Health Billing Setup Guideapi-248512169100% (1)
- Banzai Life ScenariosDocument12 pagesBanzai Life Scenariosapi-380813240Pas encore d'évaluation
- A Primer On Hospital Accounting & FinanceDocument40 pagesA Primer On Hospital Accounting & FinanceYantoPas encore d'évaluation
- Medicare Claims Processing Manual: Chapter 12 - Physicians/Nonphysician PractitionersDocument185 pagesMedicare Claims Processing Manual: Chapter 12 - Physicians/Nonphysician PractitionersPimo HypkaPas encore d'évaluation
- RICU Telehealth LawsuitDocument32 pagesRICU Telehealth LawsuitAlex KacikPas encore d'évaluation
- Financial Environment of Health Care OrganizationsDocument40 pagesFinancial Environment of Health Care OrganizationsNeicy Wilson100% (1)
- NMC SVMH Presentation 7Mar2012Final-2Document37 pagesNMC SVMH Presentation 7Mar2012Final-2dram408Pas encore d'évaluation
- CMS Organizational ChartDocument1 pageCMS Organizational ChartSarahPas encore d'évaluation
- 01 Hartman's Nursing Asst Care - Long Term Care 4eDocument34 pages01 Hartman's Nursing Asst Care - Long Term Care 4ehPas encore d'évaluation
- Budget 2024Document184 pagesBudget 2024Liberty NationPas encore d'évaluation
- Medicard Philippines V Cir (Vat - Hmo)Document1 pageMedicard Philippines V Cir (Vat - Hmo)Jerome MagpantayPas encore d'évaluation
- Equity, Tax Reform and RedistributionDocument101 pagesEquity, Tax Reform and RedistributionPeter WhitefordPas encore d'évaluation
- Lancaster County Court of Common Pleas Preliminary Injunction For Emergency Relief Re FOR PAIN MEDICATIONS of Wednesday June 14, 2017Document838 pagesLancaster County Court of Common Pleas Preliminary Injunction For Emergency Relief Re FOR PAIN MEDICATIONS of Wednesday June 14, 2017Stan J. CaterbonePas encore d'évaluation
- Susan Manheimer Eyes Candidacy For Sheriff: An Open HouseDocument32 pagesSusan Manheimer Eyes Candidacy For Sheriff: An Open HouseSan Mateo Daily JournalPas encore d'évaluation
- Comp 01 Instructor ManualDocument54 pagesComp 01 Instructor ManualP D SpencerPas encore d'évaluation