Académique Documents
Professionnel Documents
Culture Documents
Selective Patient With Metastatic Melanoma May Benefit From LR 2005
Transféré par
grigmihDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Selective Patient With Metastatic Melanoma May Benefit From LR 2005
Transféré par
grigmihDroits d'auteur :
Formats disponibles
2006 by the Societe Internationale de Chirurgie
Published Online: 4 December 2006
World J Surg (2007) 31: 171174
DOI: 10.1007/s00268-006-0375-z
Selected Patients with Metastatic Melanoma May
Benefit from Liver Resection
Paulo Herman,1,2 Marcel Autran C. Machado,1 Andre Luis Montagnini,1
Luiz A. C. DAlbuquerque,2 William A. Saad,2 Marcel C. C. Machado1
1
2
Department of Abdominal Surgery, A.C. Camargo Cancer Hospital, Sao Paulo, Brazil
Department of Gastroenterology, University of Sao Paulo Medical School, Sao Paulo, Brazil
Abstract
Background: In the last few years there has been expanding use of hepatic resection for noncolorectal metastases. The purpose of this study is to evaluate the experience of liver resection for
patients with metastatic melanoma.
Methods: Eighteen patients with metastatic melanoma were explored for possible surgical
resection. All patients fitted the following criteria: absence of extra-hepatic disease after evaluation
with CT/MRI and FDG-PET scans; disease-free interval longer than 24 months after the resection
of the primary melanoma; presumed completely resectable lesions; absence of clinical co-morbidities.
Results: Liver resection was performed in 10 patients; 8 out of 18 presented with irresectable
tumors and/or peritoneal metastases and were not operated. One patient presented with postoperative biliary fistula and was conservatively managed. No other complications or postoperative
mortality were observed. After a mean follow-up of 25.4 months, 5 patients are alive and without
evidence of recurrence. Overall median survival was 22 months; overall survival and disease-free
survival were 70% and 50% respectively.
Conclusions: Resection of liver metastases from melanoma in a selected group of patients may
increase survival. Exploratory laparoscopy should be included in the preoperative armamentarium
of diagnostic tools.
iver resection is considered the only potential curative treatment for colorectal and neuroendocrine
secondaries; however, its role in other metastatic tumors
is not completely defined. In the last few years, mortality
rates for liver resection have dramatically declined to less
than 2% in specialized centers,1 due to advances in
surgical expertise and perioperative care. This has led to
increasing enthusiasm for surgical treatment for metastatic disease, with special attention directed at cases for
which no other modality of treatment is effective.24
Correspondence to: Paulo Herman, Praca Santos Coimbra, 10, Sao
Paulo, SP, CEP 05614-050, Brazil, e-mail: pherman@uol.com.br
Liver metastases are diagnosed in 10%20% of patients with melanoma, being associated with a bad
prognosis and short survival time rates (mean = 4.4
months).5 Patients with melanoma liver metastases used
to be considered unsuitable for resection because this
approach did not increase survival significantly. However,
in the last few years, some groups have reported liver
resections with long-term survival rates.58
We have faced the same problem and decided to
operate on a highly selected group of patients with melanoma liver metastasis, since we believe that some patients can benefit from surgery. According to criteria
based on our experience and on data from the literature,
patients who were clinically well, presented no other sites
172
Herman et al.: Melanoma Metastases Liver Resection
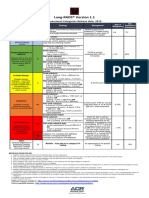
Table 1.
Patients characteristics, surgical findings, procedure, and follow-up
Origin/gender/age
Ocular/female/38 years
Ocular/female/39 years
Ocular/male/42 years
Ocular/male/42 years
Ocular/male/46 years
Cutaneous (lower limb)/
female/35 years
Cutaneous (foot finger)/
female/69 years
Cutaneous (lower limb)/
female/42 years
Cutaneous (lower limb)/
female/57 years
Cutaneous
(upper limb)/male/58 years
Status (follow-up)
Alive; disease free
(28 months)
Alive; disease free
(12 months)
Alive; disease free
(40 months)
Alive; disease free
(20 months)
Alive; recurrent
disease (12 months)
Alive; disease free
(48 months)
Alive; recurrent disease
(46 months)
Dead (15 months
after liver resection)
Dead (24 months
after liver resection)
Dead (9 months after
liver resection)
of metastasis and had had at least 24 months free of
disease since treatment of the primary tumor were subjected to hepatic resection. The aim of the present study
was to describe our selection criteria and to evaluate
surgical results and survival.
Surgery performed
Metastases number
(size in cm)
Segmentectomy I
1 (6)
Bisegmentectomies II, III and
VI,VII + wedge resection
Left hepatectomy + right lobe
nodule wedge resection
Bisegmentectomy VII, VIII
6 (2; 1; 1; 1; 1; 1)
Bisegmentectomy II, III +
wedge resection
Left hepatectomy
4 (5; 3; 1.5; 0.7)
1 (2.5)
2 (2.5; 1)
2 (4; 1)
Right hepatectomy +
wedge resection
Segmentectomy VI
2 (10; 1)
1 (2.5)
Left hepatectomy
2 (7; 3)
Right hepatectomy
1 (2.5)
tases were detected, resection was not performed. Liver
resection was performed only if the complete removal of
metastatic disease was possible.
RESULTS
PATIENTS AND METHODS
Eighteen out of 367 patients with liver metastatic
melanoma from 2 different institutions specialized in
cancer and liver surgery, between December 1999 and
January 2005, fit the proposed selection criteria (4.9%)
as follows:
1. Presumed resectable lesion(s) with normal liver function
2. A 24-month disease-free interval since the resection of
the primary melanoma
3. Absence of extra-hepatic disease after computed
tomography or magnetic resonance evaluation
4. A negative whole body 18-fluorodeoxyglucose positron emission tomography (FDG-PET scan)
5. No significant clinical co-morbidities (e.g. cardiac or
pulmonary disease).
During surgery, all patients were subjected to evaluation
of the abdominal cavity and liver ultrasound. If diffuse
hepatic disease or peritoneal and/or lymph node metas-
Ten out of the 18 patients (6 women, with ages ranging
between 35 and 69 years, mean 46) fulfilled the selection
criteria, including the intraoperative evaluation, and were
subjected to liver resection. Five patients had ocular primary melanomas and 5 had cutaneous tumors. A surgical
margin of at least 1 cm was obtained in all patients. In the
8 unoperated patients, resection was not performed due
to diffuse hepatic disease (n = 6) and peritoneal metastases (n = 2).
Clinical data, surgical findings, and procedures are
shown in Table 1. Four patients had single liver metastases, the other presented two nodules (n = 4), 4 nodules
(n = 1), and 6 nodules (n = 1).
One patient developed a postoperative biliary fistula,
which was conservatively managed with a good outcome.
No other postoperative complications were observed and
there was no operative mortality. None of the patients
received adjuvant local or systemic therapy.
Histological examination of the resected specimens
confirmed the diagnosis of malignant melanoma and free
surgical margins in all cases.
Herman et al.: Melanoma Metastases Liver Resection
All patients with ocular melanoma metastasis are alive,
4 (80%) without recurrent disease. One patient is alive
(after 12 months follow-up) with lung recurrence
9 months after liver resection. Two of the patients (2 out
of 5) with cutaneous melanoma are alive, 1 is disease
free (after 48 months follow-up) and the other developed
lung and liver recurrences 16 months after surgery
(46 months of follow-up). Three patients died, 1 with brain
and lung recurrence, 1 with liver, peritoneal, and lung
tumors and 1 with liver and peritoneal recurrence, 9, 15,
and 24 months after liver resection respectively. After a
mean follow-up of 25.4 months, overall survival rate was
70% and disease-free survival 50%.
Overall median survival time was 22 months. Five patients (50%) are alive and have been disease free for at
least 12 months after resection (range between 12 and
48 months). Two patients are alive 12 and 46 months
after liver resection and presented recurrences 9 and
16 months after surgery. Three patients died due to
recurrent disease 9, 15, and 24 months after liver
resection.
DISCUSSION
Melanoma recurs in approximately one-third of the
patients after treatment of the primary lesion9,10 and, with
the routine use of ultrasound and the improvement of
imaging diagnostic tools, metastatic disease has become
more frequently identified, with liver metastases diagnosed in up to 20% of the patients.
Patients with stage IV melanoma have a 5-year survival
rate of 6% and a mean survival time between 4 and 6
months.5 The benefit of the surgical treatment for melanoma metastases remains controversial; however, there
is some evidence that resection, in a selected group of
patients, can increase survival time and rates ranging
between 24 and 49 months have already been reported
after the resection of adrenal, gastrointestinal, pulmonary, and splenic metastasis.1115
Foster16 collected a series of 13 patients from several
institutions who were subjected to liver resection for
metastatic melanoma. In his survey, the 5-year survival
rate was 8% and mean survival time was 10 months.
Other authors, with series ranging from 1 to 10 patients,
report mean survival of between 10 and 20 months.14
In a cooperative study of the John Wayne Cancer
Institute and the Sydney Melanoma Unit, more than
26,000 melanoma patients were evaluated and 1,750
(7%) had liver metastasis. Twenty-four of them (1.4%)
underwent liver resection and the 5-year disease-free and
173
overall survival were 12% and 29% respectively. Median
overall survival time in the resected group was
28 months; on the other hand, overall median survival
time in patients with non-resected liver metastasis was 6
months and the 5-year survival rate was 4%.5
The criteria for patient selection seem to be critical for
better results. Rose et al. pointed out that patients subjected to complete resection of metastasis with histologically negative margins and the absence of extrahepatic
disease had better survival rates compared with those
undergoing exploration alone.5 The available data on
prognostic factors following resection of metastatic melanoma at other sites indicate that a longer disease-free
interval and complete resection are associated with improved outcome.1214 Indeed, we agree with these authors and, in our series, there was a rigorous selection of
patients who were suitable for liver resection. We treated
patients with good liver function, metachronic disease,
without any signs of extra-hepatic metastases and performed a complete resection independent of the number
and size of the nodules, with adequate margins in all
cases. With this refinement of selection, around 5% of the
patients with hepatic metastases can benefit from resection. With regard to our experience, 5 patients (50%) are
disease free after a median follow-up of 22.7 months and
2 are still alive, although presenting with recurrences.
Patients with recurrence were treated by systemic chemotherapy with dacarbazine associated with interferon
alpha according to the clinical and oncological protocol.
The shortest survival time in this series was 9 months and
the other deaths occurred 15 and 24 months after surgery.
Given that life expectancy for patients with stage IV melanoma ranges between 4 and 6 months, the survival time
of all treated patients seemed to be increased.
Studies have shown a poor prognosis for patients with
metastases of primary ocular melanoma compared with
those with a cutaneous primary site; however, reports of
resection for stage IV melanoma include very few patients with primary intraocular tumors.8 Therefore, the role
of surgical resection for ocular metastatic melanoma is
very difficult to assess from the current literature. In our
series, the 5 patients with ocular melanoma metastasis
treated according to our selection criteria are alive, 4 of
them disease-free. On the other hand, 2 out of 5 patients
with cutaneous melanoma metastasis are alive, with only
one disease free.
In the last few years, the use of FDG-PET scanning has
become routine for the detection of occult metastatic disease because it has been shown to be more sensitive than
CT in staging patients with metastatic melanoma.9,17 In our
study, all patients were subjected to FDG-PET, and those
174
Herman et al.: Melanoma Metastases Liver Resection
presenting with extra-hepatic disease were not operated
on. Unfortunately, in our experience, CT, MRI and FDGPET scanning were not able to identify metastases smaller
than 10 mm on the liver, peritoneum or lymph nodes.
Recently, Clark et al. showed no utility for PET in the
detection of occult metastases of melanoma.18 Indeed, in
8 out of 18 patients initially selected for liver resection
(44%), small metastases were identified during surgery.
Similar results were observed by Rose et al. in which 29%
of the patients were operated on but not resected.5 Thus,
we are now performing staging laparoscopy as a routine
preoperative procedure in all patients selected for resection in order to avoid unnecessary laparotomy.
Minimally invasive techniques as ablative procedures
were developed as alternative treatments for patients
with irresectable liver lesions and led to more patients
treated with non-resective therapy. Radiofrequency, the
most recent ablative modality, is safe and effective,
especially for tumors smaller than 4 cm in diameter, but
time is needed to evaluate the results properly. Perhaps,
in the near future, studies may show the benefit of this
less aggressive treatment modality.
Despite of the lack of long-term results there is no doubt
that, in this small series, patients presented longer survival
times compared with non-resected patients. We, therefore
encourage the surgical treatment of liver metastasis in a
highly selected group of patients, according to the described criteria. With an increase in experience and the
employment of new methods of treatment, the selection
criteria or even the results may be improved, perhaps in
the near future. Large-scale multi-center studies should be
encouraged to allow the enrolment of larger series and
better assessment of the patients. However, the poor
overall prognosis of the disease still indicates the need for
more effective therapies.
REFERENCES
1. Elias D, Albuquerque AC, Eggenspieler P, et al. Resection
of liver metastases from a noncolorectal primary: indications
and results based on 147 monocentric patients. J Am Coll
Surg 1998;187:487493.
2. Hemming AW, Sielaff TD, Gallinger S, et al. Hepatic
resection of noncolorectal nonneuroendocrine metastases.
Liver Transpl 2000;6:97101.
3. Weitz J, Blumgart LH, Fong Y, et al. Partial hepatectomy for
metastases from noncolorectal, nonneuroendocrine carcinoma. Ann Surg 2005;241:269276.
4. Laurent C, Rullier E, Feyler A, et al. Resection of noncolorectal and nonneuroendocrine liver metastases: late
metastases are the only chance of cure. World J Surg
2001;25:15321536.
5. Rose DM, Essner R, Hughes TMD, et al. Surgical resection
for metastatic melanoma to the liver: the John Wayne
Cancer Institute and Sydney Melanoma Unit experience.
Arch Surg 2001;136:950955.
6. Salmon RJ, Levy C, Plancher C, et al. Treatment of liver
metastases from uveal melanoma by combined surgery
chemotherapy. Eur J Surg Oncol 1998;24:127130.
7. Mondragon-Sanchez R, Barrera-Franco JL, Cordoba-Gutierrez H, et al. Repeat hepatic resection for recurrent metastatic melanoma. Hepatogastroenterology 1999;46:459
461.
8. Hsueh EC, Essner R, Foshag LJ, et al. Prolonged survival
after complete resection of metastases from intraocular
melanoma. Cancer 2004;100:122129.
9. Wong SL, Coit DG. Role of surgery in patients with stage IV
melanoma. Curr Opin Oncol 2004;16:155160.
10. Allen PJ, Coit DG. The surgical management of metastatic
melanoma. Ann Surg Oncol 2002;9:762770.
11. Branum GD, Epstein RE, Leight GS, et al. The role of
resection in the management of melanoma metastatic to
the adrenal gland. Surgery 1991;109:127131.
12. Mosimann F, Fontolliet C, Genton A, et al. Resection of
metastases to the alimentary tract from malignant melanoma. Int Surg 1982;67:257260.
13. Lejeune FJ, Lienard D, Sales F, et al. Surgical management
of distant melanoma metastases. Semin Surg Oncol
1992;8:381391.
14. Wong JH, Euhus DM, Morton DL. Surgical resection for
metastatic melanoma to the lung. Arch Surg
1988;123:10911095.
15. De Wilt JHW, McCarthy WH, Thompson JF. Surgical
treatment of splenic metastases in patients with melanoma.
J Am Coll Surg 2003;197:3843.
16. Foster JH. Survival after liver resection for secondary tumors. Am J Surg 1978;135:389394.
17. Stas M, Stroobants S, Dupont P. 18-FDG PET scan in the
staging of recurrent melanoma: additional value and therapeutic impact. Melanoma Res 2002;12:479490.
18. Clark PB, Victoria Soo BS, Kraas J, et al. Futility of fluorodeoxyglucose F-18 positron emission tomography in
initial evaluation of patients with T2 to T4 melanoma. Arch
Surg 2006;141:284288.
Vous aimerez peut-être aussi
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Foot reflexology chart shows how hand acupressure points relate to body partsDocument3 pagesFoot reflexology chart shows how hand acupressure points relate to body partsgautamlipika100% (2)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Acute Kidney Injury W/ Hyperkalemia NCPDocument5 pagesAcute Kidney Injury W/ Hyperkalemia NCPMyrvic Ortiz La OrdenPas encore d'évaluation
- Advanced Burn Life SupportDocument118 pagesAdvanced Burn Life SupportIntan Noa100% (1)
- Blood Bank ChecklistDocument4 pagesBlood Bank ChecklistFIAZ MAQBOOL FAZILIPas encore d'évaluation
- Guidelines For The Management of Severe Pre-Eclampsia (Anaes and Analgesia) 31.07.06Document5 pagesGuidelines For The Management of Severe Pre-Eclampsia (Anaes and Analgesia) 31.07.06grigmihPas encore d'évaluation
- How To Write A Clinical PaperDocument5 pagesHow To Write A Clinical PapergrigmihPas encore d'évaluation
- 1957213973Document173 pages1957213973grigmihPas encore d'évaluation
- HE2012 - Immunise Against HPVDocument6 pagesHE2012 - Immunise Against HPVgrigmihPas encore d'évaluation
- Dhillon 2022 How To Write A Good Scientific ReviDocument11 pagesDhillon 2022 How To Write A Good Scientific Revi邢振凯Pas encore d'évaluation
- General Best PracticeDocument193 pagesGeneral Best PracticegrigmihPas encore d'évaluation
- Global Routine Immunization Strategies and Practices: (Grisp)Document80 pagesGlobal Routine Immunization Strategies and Practices: (Grisp)Novita Dian PertiwiPas encore d'évaluation
- PIIS0748798322004966Document10 pagesPIIS0748798322004966grigmihPas encore d'évaluation
- Development and Novel Therapeutics in Hepatocellular Carcinoma A ReviewDocument11 pagesDevelopment and Novel Therapeutics in Hepatocellular Carcinoma A ReviewgrigmihPas encore d'évaluation
- 361 Full PDFDocument5 pages361 Full PDFgrigmihPas encore d'évaluation
- Guidelines For Obstetric Epidural Blood Patch NPS 5.4.06Document2 pagesGuidelines For Obstetric Epidural Blood Patch NPS 5.4.06grigmihPas encore d'évaluation
- Aasld 2018 HCCDocument28 pagesAasld 2018 HCCAzuzephre ClaraPas encore d'évaluation
- Multimodal Treatment of HCCDocument8 pagesMultimodal Treatment of HCCgrigmihPas encore d'évaluation
- Dual GraftDocument25 pagesDual GraftgrigmihPas encore d'évaluation
- BiomedJ382173-2563889 070718 PDFDocument4 pagesBiomedJ382173-2563889 070718 PDFgrigmihPas encore d'évaluation
- Thromboprophylaxis in Preg Following Vaginal CS Section 16-11-07Document9 pagesThromboprophylaxis in Preg Following Vaginal CS Section 16-11-07grigmihPas encore d'évaluation
- Nexavar GuideDocument8 pagesNexavar GuidegrigmihPas encore d'évaluation
- How To Practise Evidence-Based SurgeryDocument5 pagesHow To Practise Evidence-Based SurgerygrigmihPas encore d'évaluation
- Guide To Registration - 10 June 2009Document40 pagesGuide To Registration - 10 June 2009grigmihPas encore d'évaluation
- Influence of Hepatitis Viruses On Clinico-Pathological Profiles and Long-Term Outcome in Patients Undergoing Surgery For Hepatocellular CarcinomaDocument11 pagesInfluence of Hepatitis Viruses On Clinico-Pathological Profiles and Long-Term Outcome in Patients Undergoing Surgery For Hepatocellular CarcinomagrigmihPas encore d'évaluation
- Ha Tace For MMLM 2008Document6 pagesHa Tace For MMLM 2008grigmihPas encore d'évaluation
- Staging HCCDocument5 pagesStaging HCCgrigmihPas encore d'évaluation
- Gpc3 Generate de Celule Dendritice 2010Document11 pagesGpc3 Generate de Celule Dendritice 2010grigmihPas encore d'évaluation
- Nursing Practice (5th Ed.) - Pitman, Nursing: Assessment and Management of Clinical Problems (9th Ed.) - St. Louis: ElsevierDocument5 pagesNursing Practice (5th Ed.) - Pitman, Nursing: Assessment and Management of Clinical Problems (9th Ed.) - St. Louis: ElsevierDr-Marudhar MarudharPas encore d'évaluation
- Ir Medical 2017 A3 PDFDocument25 pagesIr Medical 2017 A3 PDFHeidi BluePas encore d'évaluation
- Elevated BilirubinDocument5 pagesElevated BilirubinNovita ApramadhaPas encore d'évaluation
- Hypertension in PregnancyDocument18 pagesHypertension in Pregnancyshubham kumarPas encore d'évaluation
- Periapical Radiolucencies As Evaluated by Bisecting-Angle and Paralleling Radio Graphic TechniquesDocument9 pagesPeriapical Radiolucencies As Evaluated by Bisecting-Angle and Paralleling Radio Graphic TechniquesFlorin Ionescu100% (1)
- rút gọnDocument3 pagesrút gọnUyen VuPas encore d'évaluation
- Kasus Farter 2 10 Mei 2019Document3 pagesKasus Farter 2 10 Mei 2019YonicaryanPas encore d'évaluation
- Bronchopulmonary Dysplasia (BPD)Document13 pagesBronchopulmonary Dysplasia (BPD)Joan BuiPas encore d'évaluation
- Abnormal PuerperiumDocument65 pagesAbnormal PuerperiumNigus AfessaPas encore d'évaluation
- Artikel IlmiahDocument12 pagesArtikel IlmiahAsti NurchasanahPas encore d'évaluation
- Lung RADS® Version 1.1: Assessment Categories Release Date: 2019Document1 pageLung RADS® Version 1.1: Assessment Categories Release Date: 2019S Francisco MotPas encore d'évaluation
- Definition:: Between 16Document3 pagesDefinition:: Between 16NIDA MUSTAFAPas encore d'évaluation
- Adult Hippocampal NeurogenesisDocument14 pagesAdult Hippocampal NeurogenesisElaine HermansPas encore d'évaluation
- Femoral Acetabular Impingement: RadiographyDocument9 pagesFemoral Acetabular Impingement: Radiography杨钦杰Pas encore d'évaluation
- CNA Chapter 1 & 2 TermsDocument1 pageCNA Chapter 1 & 2 TermsMarina ChakarPas encore d'évaluation
- Basic pharmacology of anaesthesia drugs in 40 charactersDocument56 pagesBasic pharmacology of anaesthesia drugs in 40 charactersrajvikram87Pas encore d'évaluation
- Aula 1Document14 pagesAula 1Brigida Cirqueira GuimaraesPas encore d'évaluation
- HematologyDocument100 pagesHematologyerzaraptorPas encore d'évaluation
- Ann JeinaDocument7 pagesAnn JeinaMizumoriFumairaPas encore d'évaluation
- It 18 - Neonatal Seizure - HerDocument35 pagesIt 18 - Neonatal Seizure - HerRurie Awalia SuhardiPas encore d'évaluation
- Acute Respiratory Distress Syndrome Nursing Management and Interventions - NurseslabsDocument2 pagesAcute Respiratory Distress Syndrome Nursing Management and Interventions - NurseslabsSachin SinghPas encore d'évaluation
- Type2 Diabetes HandoutDocument1 pageType2 Diabetes Handouthendra_darmawan_4Pas encore d'évaluation
- Choose 2 From The Disease Below That Are Emerging in The PhilippinesDocument4 pagesChoose 2 From The Disease Below That Are Emerging in The PhilippinesMICHELLE BIANCA PATRICE CRUZPas encore d'évaluation
- Case Report模板Document18 pagesCase Report模板ChenPas encore d'évaluation
- Kali Bichromicum 30C For COPD 2005Document8 pagesKali Bichromicum 30C For COPD 2005Dr. Nancy MalikPas encore d'évaluation
- Corneal Dystrophies: Causes, Symptoms, and TreatmentDocument2 pagesCorneal Dystrophies: Causes, Symptoms, and TreatmentBadgal BazingaPas encore d'évaluation