Académique Documents
Professionnel Documents
Culture Documents
Zcase Recaida en Cavidad Oral de LLA T V23n06a15 PDF
Transféré par
erickmattosDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Zcase Recaida en Cavidad Oral de LLA T V23n06a15 PDF
Transféré par
erickmattosDroits d'auteur :
Formats disponibles
Braz Dent J (2012) 23(6): 711-715
Relapse of acute leukemia in the oral cavity
ISSN 0103-6440
711
Isolated Relapse in the Oral Cavity of a Child with
T-lineage Acute Lymphoblastic Leukemia
Andra Conceio BRITO
Hermnia Marques CAPISTRANO
Mayara Louise TORRES2
Gilberto RAMOS1
Marcos Borato VIANA3
Benigna Maria de OLIVEIRA3
1Hematology
Division, Clinics Hospital, UFMG - Federal University of Minas Gerais, Belo Horizonte, MG, Brazil
of Dentistry, PUC/MG - Pontifical Catholic University of Minas Gerais, Belo Horizonte, MG, Brazil
3Department of Pediatrics, UFMG - Federal University of Minas Gerais, Belo Horizonte, MG, Brazil
2Department
Despite high cure rates, approximately 20% of patients with acute lymphoblastic leukemia (ALL) have disease relapse. Isolated
recurrence in oral cavity is extremely unusual. The aim of this paper is to report a case of an isolated relapse occurred in a child
with T-lineage ALL. Clinical picture included swelling and pain in the right upper gingiva of the oral cavity, with no other clinical
or hematological alterations. Diagnosis was confirmed by biopsy and immunohistochemical staining. Bone marrow aspiration was
normal. Five months later leukemic infiltration of the bone marrow was detected and systemic chemotherapy was reintroduced. This
case report highlights the relevance of dental care during and after chemotherapy, not only to treat lesions in the oral cavity resulting
from the disease itself or from treatment side effects, but also to detect unusual sites of ALL relapse.
Key Words: lymphoid leukemia, relapse, gingival tissues.
INTRODUCTION
Acute leukemias are the most common
malignancy in childhood. They represent approximately
30% of malignant diseases in patients under the age of
15 years. Acute lymphoblastic leukemia (ALL) is the
most frequent type of leukemia in children (1-3).
Leukemia etiology remains unknown and seems
to involve both genetic mechanisms and environmental
factors. Its clonal origin is well established. Disorganized
proliferation of a single progenitor cell disturbs
hematopoiesis (2,3). Clinical manifestations are due
to the inhibition of hematopoiesis by leukemic cells
and to leukemic infiltration in several organs and
systems. Anemia, secondary to decreased red blood
cell production, bleeding due to thrombocytopenia
and infections due to neutropenia are the cardinal
manifestations. Infiltration of organs results in
hepatomegaly, splenomegaly and lymphadenopathy.
Leukemic infiltration in the central nervous system
(CNS) and testes are also common events.
ALL diagnosis is confirmed when more than 25%
of leukemic cells are detected in bone marrow aspiration.
Immunophenotyping, molecular and cytogenetic tests
are useful to characterize the leukemic cells and also have
prognostic value (1). ALL treatment involves long-term
chemotherapy, which has in the last decades undergone
striking advances, leading to the current mark of around
80% of children and adolescents with ALL achieving
cure (3). Despite these high cure rates, approximately
20% still have disease relapse (3), with bone marrow
as the most frequent site, followed by the CNS (3-5).
Nevertheless, relapse can occur in any tissue or organ.
Isolated recurrence in the oral cavity is extremely
uncommon in ALL. Few case reports were found in a
literature review, mostly in adolescents or adult patients
who had histologically proven lesions in the oral cavity
months or years after the end of the leukemia treatment.
Correspondence: Benigna Maria de Oliveira, Departamento de Pediatria, Faculdade de Medicina, UFMG, Avenida Alfredo Balena, 190, sala 267,
30130-100 Belo Horizonte, MG, Brasil. Tel: +55-31-3409-9772. Fax: +55-31-3409-9397. e-mail: benigna@uol.com.br
Braz Dent J 23(6) 2012
712
A.C. Brito et al.
Most patients had concomitant bone marrow relapse or
had marrow infiltration detected shortly after the oral
cavity relapse (6-9).
The purposes of this paper are to report a case
of isolated recurrence in the oral cavity of a child with
T-lineage ALL and highlight the relevance of dental care
during and after chemotherapy for ALL.
CASE REPORT
other organ infiltration. Gingival lesion spontaneously
remitted soon after biopsy. Watchful waiting (no
treatment) was adopted in view of the spontaneous
regression and no signs of infiltration in other organs
and systems.
Five months after the initial manifestation in
the oral cavity, mild leukopenia and neutropenia were
detected, without any other clinical or laboratory
manifestations. Bone marrow aspiration showed
infiltration by lymphoblasts with T-immunophenotype.
Karyotype of bone marrow cells was 46, XY, t (10;
11) (p11; q13) [14]/46, XY [16]. No CNS infiltration
was detected. Relapse treatment was started according
to the GBTLI-LLA 2009 chemotherapy protocol for
T-immunophenotype ALL. The child has been in
remission now for 25 months, with no changes in
the oral cavity. He is scheduled to receive additional
maintenance therapy in up to 34 months. An HLAmatched donor has not been identified yet for eventual
bone marrow transplantation. Regular dental follow-up
has been maintained.
A 4-year-old male child was first diagnosed with
T-lineage ALL and treated according to the protocol
of the Brazilian Group for Leukemia Treatment in
Childhood ALL-99 (GBTLI-LLA99) for patients with
high-risk for recurrence (10), relapsing at the age of 8.
At diagnosis karyotyping of bone marrow (BM) cells
showed no metaphases for analysis. Dental monitoring
was done during the whole treatment.
One year and four months after the end of the
treatment, the child had swelling and pain in the oral
cavity, in the right maxilla, with no other clinical
or hematological signs or symptoms. The extraoral
DISCUSSION
evaluation revealed swelling on the middle third of the
right side of the face, with no signs of inflammation,
Dental monitoring of patients with leukemia
causing facial asymmetry. Oroscopy showed swelling in
during and after treatment is extremely relevant for
the vestibular region of the primary maxillary right first
early detection and appropriate treatment of diseaseand second molars and the permanent maxillary right
related lesions and side effects of chemotherapy (6,11).
first molar. The swelling extended further anteriorly into
The oral cavity in leukemia is prone to complications
the palatal mucosa. The involved teeth had abnormal
mobility and no caries. The swelling was firm and
painful upon palpation and was covered
by intact mucosa. Panoramic radiograph
image showed radiolucent area involving
an unerupted tooth and the presence of
radiodensity on the right maxillary sinus
(Fig. 1).
An incisional biopsy of the lesion
was performed. The histological diagnosis
confirmed oral mucosa infiltration by
lymphoid precursor neoplastic T-cells.
Histochemically they were positive for
BCL-2, cytoplasmatic CD3 (polyclonal),
CD45/LCA, CD99, and irregularly
positive for TDT (polyclonal). Bone
marrow aspiration and cerebrospinal
fluid examination did not show evidence
of leukemia infiltration. Computed
Figure 1. Radiographic features of child with acute lymphoblastic leukemia:
tomographs of chest, sinuses, neck,
panoramic radiograph showing radiolucent lesion near the unerupted permanent
abdomen, and pelvis were all negative for
mandibular left canine and presence of radiodensity of the right maxillary sinus.
Braz Dent J 23(6) 2012
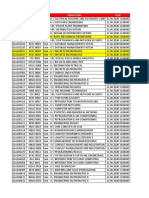
5 months after BMT
After 3 years in remission
6 years after second BMT
10 months after BMT
Female, 12, ALL
Male, 33, AML
Female, 17, AML
Female, 10, B-ALL
Ph1+ at recurrence
Female, 22, pre-B
ALL
Female, 15, B-ALL
Male, 34,
Lymphoma/T-ALL
Male, 4, ALL
Williams, 1983
Peterson, 1983
Lee, 2000
Benson, 2007
Au, 2008
Bakathir, 2009
Bgon , 2010
Present report
Remission
Chemotherapy, imatinib,
BMT
No report
Chemotherapy
Chemotherapy
Facial swelling, sensory disturbances
of the face, and abnormal teeth
mobility
Painful erosions of the oral cavity
involving the tongue, hard palate
and lips
Facial swelling, pain and swelling
in the upper right gingiva and
abnormal tooth mobility
8 months after
chemotherapy
16 months after
chemotherapy, in remission
ALL: acute lymphoblastic leukemia; AML: acute myeloid leukemia; BMT: bone marrow transplantation; Ph1: Philadelphia chromosome.
Radiotherapy
Gingival swelling
Pain and paresthesia
Remission
Clinical support
Death, 6 months after
recurrence
Death due to infection
after radiotherapy
Remission
Chemotherapy
Local radiotherapy Lymphocyte infusion
No report
Death due to infection
Chemotherapy
Pain in the mandibular
right molar region
During maintenance phase
of chemotherapy
Remission
Chemotherapy and local
radiotherapy
Paresthesia on the face, pain and
swelling in the vestibular sulcus
Bone marrow relapse,
2 years later
Outcome
Chemotherapy
Relapse treatment
After 2 years, in remission
Pain and swelling in the bucal sulcus
After chemotherapy and
radiotherapy
Female, 6, ALL
Williams, 1983
Clinical manifestation
Author
Time of relapse
Patients
characteristics:
gender, age at
initial diagnosis
(years), and type
of leukemia
Table 1. Case reports of leukemia relapse in the oral cavity reported in English-language data literature from 1983 to date.
Relapse of acute leukemia in the oral cavity
713
Braz Dent J 23(6) 2012
714
A.C. Brito et al.
ranging from exacerbation of pre-existing pathological
conditions to new mucosal lesions and infections (11-13).
Lesions resulting from infiltration of oral tissues
by leukemia cells may occur in the gingival tissues or less
frequently in the alveolar bones. These are less common
in ALL than in the myeloid subtypes (14).
Isolated relapses of ALL are rare in the oral
cavity (Table 1). Clinical and radiological characteristics
are manifold (6-9,15). Differential diagnosis includes
infections and other malignancies (7,16). While biopsy
and immunohistochemical study are mandatory,
microbiological tests can be useful in many cases (7).
Very few relapses of ALL in the oral cavity of
children have been reported (16,17). Most cases refer
to adolescents and adult patients (Table 1). Nonspecific
clinical manifestations - swelling and pain in the gingiva
- were detected in the present report. Evaluation by
an oral and maxillofacial surgeon, lesion biopsy, and
immunohistochemical study were essential for the
correct diagnosis, as also reported by many authors.
Relapse treatment can be done with combined
chemotherapy, radiotherapy or bone marrow
transplantation (BMT), whether autologous or
allogeneic. Treatment results are usually unsatisfactory,
since most institutions do not have standard treatment
protocols for this type of relapse and the best therapy
has not yet been defined. The option should take into
consideration the prognostic factors for survival of
children with relapse (4,5,18). The patient referred to
in this report had unfavorable prognostic factors such
as bone marrow infiltration and T-immunophenotype.
Children with isolated extramedullar relapse usually have
a better prognosis than those with medullar involvement
and patients with T-ALL had unfavorable outcome in
several studies (5). Many papers demonstrated that the
duration of the first remission is the most significant
variable to influence an event-free survival. Children
with late relapses have better prognosis than those with
early recurrences. The reported case can be classified
as of late recurrence, since it occurred three years after
the initial diagnosis (4,5,18).
Spontaneous local remission and absence of
infiltration in other organs led to the initial approach
of watchful waiting. As in most of the reported cases
(6-9), bone marrow infiltration occurred shortly after
relapse in the oral cavity. Systemic chemotherapy was
chosen, so far with favorable results.
In summary, even considering that ALL is curable
in about 80% of the children, the challenge remains in
Braz Dent J 23(6) 2012
trying to avoid relapses and in treating the relapsed child.
As shown in the literature, new recurrences are the main
obstacle for curing a significant number of patients.
Isolated relapses in the oral cavity are rare and may
precede bone marrow infiltration. Dental monitoring
and investigation of lesions in this region are extremely
relevant for an integral approach to the child with ALL
and for early detection of disease relapse.
RESUMO
Apesar dos altos ndices de cura, cerca de 20% dos pacientes com
leucemia linfide aguda (LLA) apresentam recidiva da doena.
Recidiva isolada na cavidade oral extremamente incomum.
O objetivo deste trabalho relatar um caso de recidiva isolada
em criana com LLA de linhagem T. A apresentao clnica foi
quadro de edema e dor na cavidade oral, na regio superior da
gengiva direita, sem outras alteraes clnicas ou hematolgicas.
O diagnstico foi confirmado por meio de bipsia e imunohistoqumica. O mielograma era normal. Cinco meses aps a
manifestao inicial na cavidade oral, foi detectada infiltrao
leucmica na medula ssea. O tratamento com quimioterapia
sistmica foi reintroduzido. Este relato de caso ressalta a
importncia do acompanhamento clnico e odontolgico durante
e aps o tratamento quimioterpico, no somente com o objetivo
de tratar as alteraes na cavidade oral decorrentes da prpria
doena ou dos efeitos adversos do tratamento, mas para que
sejam detectadas apresentaes incomuns de recidiva na LLA.
REFERENCES
1. Ziegler DS, Dalla Pozza L, Waters KD, Marshall GM. Advances
in childhood leukemia: successful clinical-trials research leads to
individualized therapy. Med J Aust 2005;182:78-81.
2. Pui CH, Schrappe M, Ribeiro RC, Niemeyer CM. Childhood and
adolescent lymphoid and myeloid leukemia. Hematology Am Soc
Hematol Educ Program 2004:118-145.
3. Pui CH, Robison LL, A Look T. Acute lymphoblastic leukemia.
Lancet 2008;371:1030-1043.
4. Gaynon PS. Childhood acute lymphoblastic leukaemia and
relapse. Br J Haematol 2005;131:579-587.
5. Uderzo C, Conter V, Dini G, Locatelli F, Miniero R, Tamaro P.
Treatment of childhood acute lymphoblastic leukemia after the
first relapse: curative strategies Haematologica 2001;86:1-7.
6. Bakathir AA, Al-Hamdani AS. Relapse of acute lymphoblastic
leukemia in the jaw. Oral Surg Oral Med Oral Pathol Oral Radiol
Endod 2009;107:e14-e16.
7. Au WY, Wong KY, Leung RYY, Tong ACK. Isolated gingival
relapse of acute lymphoblastic leukemia after transplantation. J
Oral Pathol Med 2008;37:249-251.
8. Bgon E, Blum L, Benramdane R, Leroux C, Pascal F, Lvy A,
et al.. Oral manifestation of T-cell leukemia/lymphoma. Arch
Dermatol 2010;146:804-805.
9. Peterson DE, Gerad H, Williams LT. An unusual instance of
leukemic infiltrate diagnosis and management of periapical tooth
involvement. Cancer 1983;51:1716-1719.
10. Scrideli CA, Assumpo JG, Ganazza MA, Araujo M, Toledo
SR, Lee MLM, et al.. A simplified minimal residual disease
polymerase chain reaction method at early treatment points can
Relapse of acute leukemia in the oral cavity
11.
12.
13.
14.
stratify children with acute lymphoblastic leukemia into good and
poor outcome groups. Haematologica 2009;94:781-789.
Carrillo C, Fava M, Vizeu H, Soares-Junior LA, Odone Filho V.
Dental approach in the pediatric oncology patient: characteristics
of the population treated at the dentistry unit in a Pediatric
Oncology Brazilian Teaching Hospital. Clinics 2010;65:569-573.
Declerck D, Vinckier F. Oral complications of leukemia.
Quintessence Int 1988;19:575-583.
Soares AF, Aquino ARL, Carvalho CHP, Nonaka CFW, Almeida D,
Pereira Pinto L. Frequency of oral mucositis and microbiological
analysis in children with acute lymphoblastic leukemia treated
with 0.12% chlorhexidine gluconate. Braz Dent J 2011;22:312316.
Abdullah BH, Yahya HI, Kummoona RK, Hilmi FA, Mirza KB.
Gingival fine needle aspiration cytology in acute leukemia. J Oral
Path Med 2002;31:55-58.
715
15. Lee KH, Lee JH, Kim S, Lee JS, Kim SH, Kim WK. High
frequency of extramedullary relapse of acute leukemia after
allogenic bone marrow transplantation. Bone Marrow Transplant
2000;6:147-152.
16. Benson RE, Rood HD, North S, Loescher AR, Farthing PM, Payne
M. Leukemic infiltration of the mandible in a young girl. Int J
Paediatr Dent 2007;17:145-150.
17. Williams SA, Duggan MB, Bailey CC. Jaw involvement in acute
lymphoblastic leukemia. Br Dent J 1983;155:164-166.
18. Raetz EA, Bhatla T. Where do we stand in the treatment of relapsed
acute lymphoblastic leukemia? Hematology Am Soc Hematol
Educ Program 2012; 2012:129-136.
Received May 22, 2012
Accepted August 15, 2012
Braz Dent J 23(6) 2012
Vous aimerez peut-être aussi
- Adolescentes BFM HyperCVAD Alacacioglu2015Document5 pagesAdolescentes BFM HyperCVAD Alacacioglu2015erickmattosPas encore d'évaluation
- BFM 2009 Colombia 0120-0011-Rfmun-64-03-00417Document9 pagesBFM 2009 Colombia 0120-0011-Rfmun-64-03-00417erickmattosPas encore d'évaluation
- LMA BFM 2004 1-S2.0-S0006497119422519-MainDocument3 pagesLMA BFM 2004 1-S2.0-S0006497119422519-MainerickmattosPas encore d'évaluation
- NIH Public Access: Author ManuscriptDocument15 pagesNIH Public Access: Author ManuscripterickmattosPas encore d'évaluation
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Staff Code Subject Code Subject Data FromDocument36 pagesStaff Code Subject Code Subject Data FromPooja PathakPas encore d'évaluation
- History of Costa RicaDocument2 pagesHistory of Costa Ricakrishnan MishraPas encore d'évaluation
- X Glo LED Strip Lighting For Tunnelling BrochureDocument6 pagesX Glo LED Strip Lighting For Tunnelling BrochureJOSE HUAMANIPas encore d'évaluation
- TRL Explanations - 1Document4 pagesTRL Explanations - 1Ana DulcePas encore d'évaluation
- Traffic Cases in GSMDocument18 pagesTraffic Cases in GSMkamal100% (1)
- Quiz - Ionic EquilibriumDocument2 pagesQuiz - Ionic EquilibriumSiddPas encore d'évaluation
- Tas 5731Document60 pagesTas 5731charly36Pas encore d'évaluation
- Homoeopathy and MigraineDocument4 pagesHomoeopathy and MigraineEditor IJTSRDPas encore d'évaluation
- 08 A330 Ata 35Document32 pages08 A330 Ata 35Owen100% (1)
- N Methylpyrrolidone: Chemical Synonym General InformationDocument5 pagesN Methylpyrrolidone: Chemical Synonym General InformationMohamed AdelPas encore d'évaluation
- Free-Field Equivalent Localization of Virtual AudioDocument9 pagesFree-Field Equivalent Localization of Virtual AudiojulianpalacinoPas encore d'évaluation
- DysphagiaDocument4 pagesDysphagiaMicaPas encore d'évaluation
- 34 Plaza Newsletter 101317 FINALDocument4 pages34 Plaza Newsletter 101317 FINALJosef SzendePas encore d'évaluation
- EE 411-Digital Signal Processing-Muhammad TahirDocument3 pagesEE 411-Digital Signal Processing-Muhammad TahirQasim FarooqPas encore d'évaluation
- Using A Wet Film ThicknessDocument2 pagesUsing A Wet Film ThicknesssanoopvkPas encore d'évaluation
- One - Touch Fittings: Series: WP2Document12 pagesOne - Touch Fittings: Series: WP2PrashantPas encore d'évaluation
- HPLC Columns by SciencixDocument49 pagesHPLC Columns by SciencixBrett HarrisPas encore d'évaluation
- The Church of Kapnikarea in Athens - N. GkiolesDocument13 pagesThe Church of Kapnikarea in Athens - N. GkiolesMaronasPas encore d'évaluation
- Curriculum Jaime Alvarado (Jaime Alvarado)Document3 pagesCurriculum Jaime Alvarado (Jaime Alvarado)yuly aldanaPas encore d'évaluation
- T60n02rg PDFDocument8 pagesT60n02rg PDFsandor9116100% (2)
- Augustine's Confessions - Philosophy in AutobiographyDocument241 pagesAugustine's Confessions - Philosophy in AutobiographyAlfonso Flórez100% (2)
- Content For Essay and Paragraph Writing On Maritime HistoryDocument15 pagesContent For Essay and Paragraph Writing On Maritime HistoryRaju KumarPas encore d'évaluation
- An Overview of The IEEE Color BooksDocument6 pagesAn Overview of The IEEE Color BooksOhm666Pas encore d'évaluation
- MPI Report 009 Sub Structure B668Document1 pageMPI Report 009 Sub Structure B668John DolanPas encore d'évaluation
- Jerms B 2109 - 0BDocument10 pagesJerms B 2109 - 0BNothing is ImpossiblePas encore d'évaluation
- WEG CTM Dwb400 10004024165 Installation Guide EnglishDocument1 pageWEG CTM Dwb400 10004024165 Installation Guide Englishjeffv65Pas encore d'évaluation
- M.E Construction Engineering ManagementDocument43 pagesM.E Construction Engineering ManagementLeilani JohnsonPas encore d'évaluation
- Mold Maintenance StepDocument0 pageMold Maintenance StepMonica JoynerPas encore d'évaluation
- Tools, Equipment, and ParaphernaliaDocument35 pagesTools, Equipment, and Paraphernaliajahnis lopez100% (1)
- Power - Distribution Transformers @2020V2Document34 pagesPower - Distribution Transformers @2020V2Musfiqul AzadPas encore d'évaluation