Académique Documents
Professionnel Documents
Culture Documents
งาน 3.3.3 - 3.3.5
Transféré par
Man Lor0 évaluation0% ont trouvé ce document utile (0 vote)
7 vues6 pagesMED
Copyright
© © All Rights Reserved
Formats disponibles
DOC, PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentMED
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme DOC, PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
7 vues6 pagesงาน 3.3.3 - 3.3.5
Transféré par
Man LorMED
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme DOC, PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 6
Effects of changing in inspired gases graphs provided V T, RR, VE
3.3.3 Hypoxia alone
. 5206535
ventilatory acclimatization to hypoxia produces a timedependent increase in ventilation, a decrease in arterial Pco
2(PaCO2), and an increase in the hypoxic ventilatory response
(HVR). This process has been well characterized in humans which
exhibits the most humanlike ventilatory acclimatization to hypoxia.
3.3.4 Hyperoxia
The idea of pre-oxygenation is to replace air in the
Functional Residual Capacity (that is the residual volume of air in
the lungs after the end of a normal breath) with 100% oxygen.
The volume of the FRC in a 70kg adult is about 2.5 liters. The
total oxygen demand of the same person at rest is about
250ml/min. With no pre-oxygenation the total amount of oxygen
in the FRC will be 500ml (2.5L * 21%) - exhausted in approx. 2
min. With pre-oxygenation you can increase the time until your
lung stores of oxygen are depleted by about 5 times to 10
minutes.
In that 10 minutes, arterial CO2 levels will climb by about
0.5 kPa/min, from about 5 kPa to 10, the blood pH will probably
drop to about 7.2. This is not ideal, but it really isn't life
threatening. Lack of oxygen will kill you way before the build up
of CO2 does.
The caveat to that is that the urge to breath is predominately
driven by CO2 build up, and inhaling one breath of O2 wouldn't
do anything much to your CO2 levels so it would be difficult to
. 5206535
resist your urge to breath, although probably not impossible with
enough will power.
Our blood has evolved to capture the oxygen we breathe in
and bind it safely to the transport molecule called haemoglobin. If
you breathe air with a much higher than normal O2 concentration,
the oxygen in the lungs overwhelms the blood's ability to carry it
away. The result is that free oxygen binds to the surface proteins
of the lungs, interferes with the operation of the central nervous
system and also attacks the retina. Contrary to popular myth,
hyperventilating air at ordinary pressures never causes oxygen
toxicity (the dizziness is due to CO2 levels dropping too low
3.3.5 Hypercapnia alone
Optimal V/Q matching occurs when the ratio of the volume
of gas to the volume of blood into the lungs approximates 1.
Pulmonary venoarterial shunts and alveolar hypoventilation result
in V/Q mismatch, which is probably the most important
mechanism of gas exchange impairment in infants with respiratory
failure due to various causes, including respiratory distress
syndrome (RDS). Hypoventilation is frequently seen in infants with
apnea of prematurity.
The effect of assisted ventilation on hypercapnia strongly
depends on the mechanism of gas exchange impairment.
. 5206535
Hypercapnia secondary to severe V/Q mismatch may be treatable
with CMV or could require high-frequency ventilation (HFV).
Hypercapnia secondary to hypoventilation is usually easily
managed with CMV. CO2 normally diffuses readily from the blood
into the alveoli. Elimination of CO2 from the alveoli is directly
proportional to alveolar minute ventilation, which is determined by
the product of tidal volume (minus dead-space ventilation) and
frequency.
Relationships among ventilator-controlled variables (shaded circles)
and pulmonary mechanics (unshaded circles) that determine minute
ventilation during pressure-limited time-cycled ventilation. The
relationships between the circles joined by solid lines are described
by simple mathematical equations. The dashed lines represent
relationships that cannot be calculated precisely without
considering other variable such as pulmonary mechanics. Thus,
. 5206535
simple mathematical equations determine the time constant of the
lungs, the pressure gradient, and the inspiratory time. In turn, these
determine the delivered tidal volume, which, when multiplied by
the respiratory frequency, provides the minute ventilation. Alveolar
ventilation can be calculated from the product of tidal volume and
frequency when dead space is subtracted from the former
. 5206535
Effects of incomplete inspiration (A) or incomplete expiration (B)
on gas exchange. An incomplete inspiration leads to decreases in
tidal volume and mean airway pressure. Hypercapnia and
hypoxemia may result. An incomplete expiration may lead to
decreases in compliance and tidal volume and an increase in mean
airway pressure. Hypercapnia with a decrease in PaO2 may result.
However, gas trapping and its resulting increase in mean airway
pressure may decrease venous return, decreasing cardiac output and
impairing oxygen delivery
. 5206535
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Clinicalapproachtogynecologicalpatientpart1 130803014047 Phpapp01Document32 pagesClinicalapproachtogynecologicalpatientpart1 130803014047 Phpapp01Man LorPas encore d'évaluation
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Combined GyneDocument32 pagesCombined GyneMan LorPas encore d'évaluation
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Benign Skin TumoursDocument7 pagesBenign Skin TumoursMan LorPas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (894)
- ReadmeDocument1 pageReadmejacksonrandyjjPas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- 114Document9 pages114Man LorPas encore d'évaluation
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Calendar July 2016 LandscapeDocument1 pageCalendar July 2016 LandscapeMan LorPas encore d'évaluation
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Acute AbdomenDocument29 pagesAcute AbdomenMan LorPas encore d'évaluation
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- 100 Cases in Ear, Nose & ThroatDocument45 pages100 Cases in Ear, Nose & Throatapi-3730930100% (17)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- 114Document9 pages114Man LorPas encore d'évaluation
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- How Does Smoking Affect The Heart and Blood Vessels - NHLBI, NIHDocument2 pagesHow Does Smoking Affect The Heart and Blood Vessels - NHLBI, NIHMan LorPas encore d'évaluation
- Radical Cystectomy With Ileal Conduit Urinary Diversion - Department of UrolDocument8 pagesRadical Cystectomy With Ileal Conduit Urinary Diversion - Department of UrolMan LorPas encore d'évaluation
- Bowen's Disease: Understanding The SkinDocument6 pagesBowen's Disease: Understanding The SkinMan LorPas encore d'évaluation
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Frizzell - Handbook of PathophysiologyDocument973 pagesFrizzell - Handbook of PathophysiologyididgamaPas encore d'évaluation
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Calendar September 2016 LandscapeDocument1 pageCalendar September 2016 LandscapeMan LorPas encore d'évaluation
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- HIV Handbook VOL2Document528 pagesHIV Handbook VOL2Man LorPas encore d'évaluation
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Viral Entry in The HIV Life Cycle.Document1 pageViral Entry in The HIV Life Cycle.Man LorPas encore d'évaluation
- Viral EntryDocument27 pagesViral EntryMan LorPas encore d'évaluation
- Update of Antiretroviral Agents inDocument100 pagesUpdate of Antiretroviral Agents inMan LorPas encore d'évaluation
- Figure 1 - Enfuvirtide - Nature Reviews Drug DiscoveryDocument2 pagesFigure 1 - Enfuvirtide - Nature Reviews Drug DiscoveryMan LorPas encore d'évaluation
- Anti-HIV Therapeutic Research - Institute of Human VirologyDocument3 pagesAnti-HIV Therapeutic Research - Institute of Human VirologyMan LorPas encore d'évaluation
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- All ANS DrugsDocument52 pagesAll ANS DrugsMan Lor100% (1)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- CVS PresentDocument78 pagesCVS PresentMan LorPas encore d'évaluation
- LCE-24C100F (K) LCE-24C100F (N) LCE-24C100F (R) LCE-24C100F (S) : Instruction ManualDocument20 pagesLCE-24C100F (K) LCE-24C100F (N) LCE-24C100F (R) LCE-24C100F (S) : Instruction ManualMan LorPas encore d'évaluation
- CVS CaseDocument28 pagesCVS CaseMan LorPas encore d'évaluation
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- History: A 65-Year-Old Man Presented To TheDocument3 pagesHistory: A 65-Year-Old Man Presented To TheMan LorPas encore d'évaluation
- Skin Diseases and DisordersDocument45 pagesSkin Diseases and DisordersMan LorPas encore d'évaluation
- History: A 65-Year-Old Man Presented To TheDocument3 pagesHistory: A 65-Year-Old Man Presented To TheMan LorPas encore d'évaluation
- Pharmacokinetics and Efficacy of A Vaginally Administered Maraviroc Gel in RDocument10 pagesPharmacokinetics and Efficacy of A Vaginally Administered Maraviroc Gel in RMan LorPas encore d'évaluation
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Case Hematology + Genetics I: Β Thalassemia/Hbe DiseaseDocument1 pageCase Hematology + Genetics I: Β Thalassemia/Hbe DiseaseMan LorPas encore d'évaluation
- L.D..Occlusion in FPDDocument138 pagesL.D..Occlusion in FPDApurva Deshmukh67% (3)
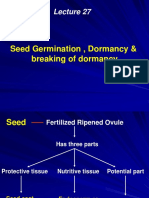
- Seed Germination, Dormancy & Breaking of DormancyDocument35 pagesSeed Germination, Dormancy & Breaking of DormancySaravananPas encore d'évaluation
- Artificial Lung Design & Gas ExchangeDocument25 pagesArtificial Lung Design & Gas Exchangealoove66Pas encore d'évaluation
- Importance of Functional Groups in Drug SelectionDocument6 pagesImportance of Functional Groups in Drug SelectionNuruel HassanPas encore d'évaluation
- MSC 060913 PDFDocument44 pagesMSC 060913 PDFViroopaksha V JaddipalPas encore d'évaluation
- Amino Acid Sequences Reveal Evolutionary RelationshipsDocument6 pagesAmino Acid Sequences Reveal Evolutionary RelationshipsAbby Gail DigalPas encore d'évaluation
- Pe Lecture NotesDocument7 pagesPe Lecture NotesAnonymous LJrX4dzPas encore d'évaluation
- Cell Cycle Lesson PlanDocument4 pagesCell Cycle Lesson PlanJustine Pama94% (17)
- Radiation Biology: Presented By: Aarya.H.NairDocument83 pagesRadiation Biology: Presented By: Aarya.H.NairAARYAPas encore d'évaluation
- January 2016 (IAL) QP - Unit 1 Edexcel Biology A-LevelDocument24 pagesJanuary 2016 (IAL) QP - Unit 1 Edexcel Biology A-LevelkirthikaPas encore d'évaluation
- Chapter 6 Cell DivisionDocument20 pagesChapter 6 Cell DivisionVinash Shka RaoPas encore d'évaluation
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Neurodegenerative Cerebellar AtaxiaDocument26 pagesNeurodegenerative Cerebellar AtaxiaМилица МилошевићPas encore d'évaluation
- The Integumentary SystemDocument11 pagesThe Integumentary SystemHamdy Pagilit DimaporoPas encore d'évaluation
- Mechanisms of Cardiac Arrhythmias From Automatici+Document24 pagesMechanisms of Cardiac Arrhythmias From Automatici+Malar MannanPas encore d'évaluation
- How Can We Use Neurotransmitters in Emotion and Reward System To Study DepressionDocument22 pagesHow Can We Use Neurotransmitters in Emotion and Reward System To Study DepressionGlobal Research and Development ServicesPas encore d'évaluation
- Altitude PhysiologyDocument41 pagesAltitude Physiologyshepherd jeremiahPas encore d'évaluation
- Biology PDFDocument1 447 pagesBiology PDFPrincess Ethel Atillo100% (2)
- CorneaDocument41 pagesCorneaNikhil KorripatiPas encore d'évaluation
- MRCP 2 Nephrology NOTESDocument74 pagesMRCP 2 Nephrology NOTESMuhammad HaneefPas encore d'évaluation
- Electrolyte Imbalance 1Document3 pagesElectrolyte Imbalance 1Marius Clifford BilledoPas encore d'évaluation
- Circulatory System: Heart, Blood Vessels & Their FunctionsDocument17 pagesCirculatory System: Heart, Blood Vessels & Their FunctionskangaanushkaPas encore d'évaluation
- Anatomy and Diseases of The UveaDocument102 pagesAnatomy and Diseases of The UveaVishakh IsloorPas encore d'évaluation
- Science (Digestion) Notes/ActivityDocument4 pagesScience (Digestion) Notes/ActivityHi HelloPas encore d'évaluation
- A Kinesiological Analysis of Shot BY WILLISDocument16 pagesA Kinesiological Analysis of Shot BY WILLISNoraina AbdullahPas encore d'évaluation
- HeparinDocument2 pagesHeparinNinoska Garcia-Ortiz100% (4)
- Foliar FertilizerDocument7 pagesFoliar FertilizerDjugian GebhardPas encore d'évaluation
- Mitosis and MeiosisDocument4 pagesMitosis and MeiosisMicah Porcal ArelladoPas encore d'évaluation
- Exam 3 NotesDocument3 pagesExam 3 NotesStanley ChuPas encore d'évaluation
- BTLDocument60 pagesBTLCamiPas encore d'évaluation
- Answer Key For Comprehensive Exam XVDocument18 pagesAnswer Key For Comprehensive Exam XVQharts SajiranPas encore d'évaluation
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionD'EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionÉvaluation : 4 sur 5 étoiles4/5 (402)
- Why We Die: The New Science of Aging and the Quest for ImmortalityD'EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityÉvaluation : 3.5 sur 5 étoiles3.5/5 (2)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisD'EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisÉvaluation : 4 sur 5 étoiles4/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedD'EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedÉvaluation : 5 sur 5 étoiles5/5 (78)
- The Age of Magical Overthinking: Notes on Modern IrrationalityD'EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityÉvaluation : 4 sur 5 étoiles4/5 (13)