Académique Documents
Professionnel Documents
Culture Documents
Icft05i1p3 PDF
Transféré par
Anjum ShakeelaDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Icft05i1p3 PDF
Transféré par
Anjum ShakeelaDroits d'auteur :
Formats disponibles
Indian Journal of Neurotrauma (IJNT)3
2005, Vol. 2, No. 1, pp. 3-6
Review Article
Current Management of Odontoid Fractures
Awadhesh Kumar Jaiswal M Ch, Manish S Sharma M Ch, Sanjay Behari M Ch
Bernard T. Lyngdoh M Ch, Subodh Jain M Ch, Vijendra K. Jain M Ch
Department of Neurosurgery
Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow 226014
Abstract: Odontoid fracture frequently occurs following cervical trauma. As C1-2 vertebral level
allows
the maximum motion in the cervical spine, these fractures may often be unstable, causing catastrophic
spinal cord trauma and respiratory compromise. In this article, the current management of odontoid
fractures is reviewed.
Keywords: cervical spine injury, odontoid fracture, odontoid process
INTRODUCTION AND CLASSIFICATION
Off all the cases of cervical trauma, about one out of five
involves the axis1. The commonest type of the axis injury is
an odontoid fracture at the junction of the dens and the
body (type II odontoid fracture)2.
The C1-2 complex allows far more motion than any other
single level in the cervical spine. This motion is
predominantly rotational, since translational motion at C1C2 is limited by the strong transverse ligament. This
restriction is lost after fracture of the odontoid and may be
associated with antero- or retrolisthesis of the C1-C2
complex in relation to the C2 body. This may result in spinal
cord compression producing severe neurological deficits3.
associated with posterior displacement of the C1 archfragment relative to the body of axis5.
FIGURE 1: Diagrams showing a) the transverse ligament supporting
the dens to the C1 arch; and, b) the cruciate ligament supporting
the occipito-atlanto-axial complex
Anderson and D Alonzo2 classified dens fracture into
three types:
Type I- involves the tip of the odontoid process. This is the
least common type of odontoid fracture.
Type II- is the commonest type of dens fracture. The fracture
line involves the junction of the body of dens with the
body of axis. Sometimes type II fracture is associated with
a comminuted fragment at the base of dens called the type
II A variety of fracture. This fracture is markedly unstable4.
Type III- The fracture line involves the body of C2 in
addition to passing through dens.
The commonest cause of dens fracture is hyperflexion
at the neck. This may lead to an anterior displacement of
C1 on C2 (atlanto-axial subluxation). Extension only
occasionally produces odontoid fracture and this is usually
Address for correspondence: Dr. Sanjay Behari, MCh, DNB
Associate Professor, Department of Neurosurgery, Sanjay Gandhi
Postgraduate Institute of Medical Sciences, Lucknow 226014,
E mail: sbehari27@yahoo.com; sbehari@sgpgi.ac.in, Fax: 91-5222668017, 2668078
FIGURE 2: Diagrams showing a) the type I; b) type II; and, c) type
III odontoid fractures
Indian Journal of Neurotrauma (IJNT), Vol. 2, No. 1, 2005
Awadhesh Kumar Jaiswal, Manish S Sharma, Sanjay Behari
Bernard T. Lyngdoh, Subodh Jain, Vijendra K. Jain
FIGURE 3. Coronal CT scan showing a) type II; and, b) type III
odontoid fractures
CLINICAL FEATURES
Patients with acute dens fractures usually present with
upper cervical pain and restriction of neck movements.
They may have a tendency to support their head with their
hands while moving from an upright to a supine position.
In case of cord compression by the displaced fracture
segments, cervical myelopathy may occur. In a study, 82%
patients of type II fractures presented with intact
neurological status; 8% had minimal sensory disturbances
over the scalp or limb; and 10% had significant neurological
deficits. Type I and type III odontoid fractures are rarely
associated with neurological deficits6. About 25-40% of
dens fractures are fatal at the time of accident.
MANAGEMENT
fracture odontoid treated with external immobilization alone.
Hadley4 described that type II A dens fractures have a very
high tendency of non-union. The current role of external
immobilization in case of type II dens fractures is where
patients are unfit for general anesthesia or they have
sustained severe concurrent injury that precludes primary
surgical intervention for the fractured odontoid. Apfelbaum
et al17 have found a lower rate of bony fusion in patients
with anterior oblique fractures when compared to patients
in whom posterior oblique or horizontal fractures were
demonstrated.
FIGURE 4. Sagittal MR scan showing an atlantoaxial dislocation
due to type II odontoid fracture
Surgical treatment
Type I odontoid fractures
Anterior approach
Most neurosurgeons agree that these fractures are
generally stable and can be managed with external
immobilization using a hard cervical collar. There is very
low incidence of non-union, and surgery is seldom
indicated for these fractures2,7.
Anterior odontoid screw fixation was first reported by
Nakanishi 18 and Bohler 19 . This procedure provides
immediate spinal stability, preserves the normal rotation
between C1-2, allows the best anatomical and functional
outcome for type II odontoid fracture, and is associated
with rapid patient mobilization, minimal postoperative pain
and a short hospital stay. Acute odontoid fractures treated
by anterior screw fixation have a fusion rate of approximately
90 percent20.
Type II odontoid fractures
Conservative treatment
In the management of type II odontoid fractures, longenduring controversies exist: Should conservative
management with halo immobilization be adopted; or, should
surgical reduction and fusion be undertaken? In case of
the latter, should the approach be anterior or posterior?
Studies utilizing external immobilization have reported a
wide-ranging result8-15 varying from ineffectualness14 to
93 percent15 success. Various factors affecting the rate of
union of fractured odontoid include elderly age, degree of
dens displacement, presence of concomitant C1-2 fracture,
pre-existing pathological condition and age of the fracture16.
Apuzzo et al8 reported that dens displacement exceeding
4mm and an age above 40 years are associated with 88%
chance of non-union of fracture odontoid treated with
external immobilization alone. Dunn et al12 reported that
age greater than 65 years along with retrolisthesis
correlated with about 70-78% chance of non-union of
Indian Journal of Neurotrauma (IJNT), Vol. 2, No. 1, 2005
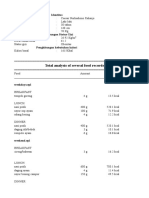
Table 1: Surgical approaches for odontoid fracture
Anterior approach
Anterior odontoid screw fixation
Single screw
Multiple screw
Posterior approach
C1-2 sublaminer wire fixation and bone grafting
Gallies method
Brooks method
Sonntags method
Posterior C1-2 transarticular screw fixation
Magerls procedure
Magerls procedure supplemented with
C1-2 sublaminar wire fixation
Jains method of creating artificial arch on the
occipital bone with sublaminar wiring
Ransfords contoured rod fixation
Current Management of Odontoid Fractures
In the anterior screw fixation procedure, one or more
screws may be used. Earlier studies emphasized on the
concept of multiple screw usage for type II odontoid
fractures mentioning that multiple screws augment the
structural strength of the fusion and prevent the rotation
of odontoid on the body of C221,22. Recent studies found
no significant difference in the fusion rate in the patients
treated with single or two odontoid screws23.
Various types of screws are available, including cortical
or cancellous bone screws, self-tapping or non self-tapping
screws, lag screws or cannulated screws, and, fully or
partially threaded screws. Partially threaded lag screws are
commonly used for fixating the odontoid. Lag compression
helps to unite the fracture line by producing a compressive
force. This helps in coupling the fractured fragments in
addition to providing rigid fixation. Non self- tapping screws
provide stronger screw purchase in the bone than self
tapping screws16.
The anterior odontoid screw fixation has certain
limitations. Surgery requires adequate high cervical
exposure and soft tissue retraction, which create anatomical
limitations, as does the inability to add graft material to
enhance fusion stability. Patients with short neck and barrelshaped chest may not be suitable surgical candidates for
the anterior approach because their anatomy interferes with
an appropriate screw trajectory. A prerequisite for anterior
screw fixation is an intact transverse ligament and a
horizontal fracture line, which may not always be the case.
In cases of chronic odontoid fracture, anterior screw fixation
is associated with a high chance of non-union. The anterior
screw fixation for odontoid fracture should be only
performed when the fractured odontoid and the remaining
C2 body are adequately aligned prior to screw insertion16.
Posterior approach
Posterior approach for stabilization of odontoid fracture is
indicated in the cases of odontoid fracture that are not
amenable to anterior screw fixation. Commonly used
procedures involve wedging a bone graft between posterior
arch of C1 and the C2 lamina with sublaminar wiring. The
well-described different methods for this C1- 2 posterior
fusion procedure are the Gallie24, Brooks25, Sonntag26
techniques. These procedures have a satisfactory fusion
rate of about 74 percent20. The demerit of this procedure is
that it causes elimination of the normal C1-2 rotatory motion
( which accounts for more than 50% of all cervical spine
rotatory movements) and reduced cervical spine flexion
extension by 10 percent21.
Another excellent alternative technique for odontoid
fracture is the posterior C1-2 transarticular screw fixation
(Magerls procedure) using unilateral or bilateral screws27,28.
This provides an excellent spinal rotational spinal stability.
This is an indirect method of stabilizing the fracture (in
which the normal anatomical configuration is disrupted).
Preoperative CT evaluation is mandatory to avoid vertebral
artery injury in this procedure. This technique can be
supplemented with metal plate for occipito-cervical
stabilization. Alternatively, Jains technique of
occipitocervical fusion29, Goels plate and screw lateral mass
fixation30, or a Ransfords contoured rod technique31 may
be utilized.
Type III odontoid fracture
Conservative treatment
For type III odontoid fractures, external immobilization is a
successful treatment option. Various studies have reported
about 85% fusion rate for type III dens fractures treated by
external immobilization2,7. Age was not clearly a predictor
of successful fusion. The degree of fracture displacement
had a negative correlation in few studies. About 97% fusion
rate has been demonstrated in cases of type III dens fracture
treated with posterior cervical fixation methods and almost
100% fusion rate has been shown by anterior screw
fixation20.
CONCLUSIONS
For type I and type III dens fractures, external
immobilization provides a satisfactory fusion rate of almost
100% and 84% respectively. However, anterior screw fixation
for type III dens fractures improves the fusion rate to nearly
100%. For type II odontoid fractures, the role of external
immobilization is limited to only select cases who are not fit
for a surgical procedure as it provides a fusion rate of
approximately 65%. Anterior screw or posterior cervical
stabilization procedures provide a 74 to 90% fusion rate.
The former is preferred in acute Type II fractures due to its
ability to preserve C1-C2 axial rotation but cannot be applied
in cases of transverse ligament disruption, significantly
displaced fractured segment or with communited fractures.
REFERENCES
1.
Huelke DF, ODay J, Mendelson RA. Cervical injuries suffered
in automobile crashes.
J Neurosurg 1989; 54: 316-22
2.
Anderson LD, DAlonzo RT. Fractures of the odontoid process
of the axis.
J Bone Joint Surg (Am). 1974; 56: 1663-74.
3.
White AA III, Panjabi MM. Clinical Biomechanics of the Spine,
ed 2. Philadelphia: JB Lippincott, 1990, pp 92-7.
4.
Hadley MN, Browner CM, Liu SS et al New subtype of acute
odontoid fracture (type II A).
Neurosurgery 1988; 22: 67-71.
Indian Journal of Neurotrauma (IJNT), Vol. 2, No. 1, 2005
Awadhesh Kumar Jaiswal, Manish S Sharma, Sanjay Behari
Bernard T. Lyngdoh, Subodh Jain, Vijendra K. Jain
5.
Stillerman CB, Roy RS, Weis MH. Cervical spine injuries:
Diagnosis and treatment. In Wilkins RH, Rengachary SS (eds)
Neurosurgery Vol II, ed 2. 2875-2904.
6.
Przybylski GJ. Management of odontoid fractures.
Contemp Neurosurg 1998; 20: 1-6.
7.
Hadley MN, Bishop RC. Injuries of the craniocervical junction
and upper cervical spine, in Tindall GT, Cooper PR, Barrow
DL (eds): The Practice of Neurosurgery. Baltimore: Williams
and Wilkins, 1996; 2: 1687-701.
8.
Apuzzo MLJ, Heiden JS, Weiss MH et al, et al. Acute fracture
of the odontoid process. An analysis of 45 cases.
J Neurosurg 1978;48: 85-91.
9.
Fujii E, Kobayashi K, Hirabayashi K. Treatment in the fractures
of the odontoid process.
Spine 1988; 13: 604-609.
10. Schatzker J, Rorabeck CH, Waddell JP. Fracture of the dens
(odontoid process). Analysis of thirty-seven cases.
J Bone Joint Surg (Br) 1971; 53: 392-405.
11. Hadley MN, Browner C, Sonntag VKH. Axis fractures: a
comprehensive review of management and treatment in 107 cases.
Neurosurgery 1985; 17: 281-90.
12. Dunn ME, Seljeskog EL. Experience in the management of
odontoid process injuries: an analysis of 128 cases.
Neurosurgery 1986; 18: 306-10
13. Wang GJ, Mabie KN, Whitehill R et al. The nonsurgical
management of odontoid fracture in adults.
Spine 1984; 9: 229-30.
14. Maiman DJ, Larson SJ. Management of odontoid fractures.
Neurosurgery 1982; 11: 471-6.
unions of the dens.
J Bone Joint Surg (Am) 1982; 64: 18-27.
20. Julien TD, Frankel B, Traynelis VC, Ryken TC. Evidencebased analysis of odontoid fracture management.
Neurosurg Focus 2000; 8: 1-6.
21. Apfelbaum RI: Anterior screw fixation of odontoid fractures,
in Camins MB, OLeary PF (eds): Diseases of the cervical
spine. Baltimore: Williams and Wilkins, 1992, pp 603-8.
22. Geisler FH, Cheng C, Poka A et al. Anterior screw fixation of
posteriorly displaced Type II odontoid odontoid fractures.
Neurosurgery 1989; 25: 34-8.
23. Jenkins JD, Coric D, Branch CL Jr. a clinical comparison of
one and two screw odontoid fixation.
J Neurosurg 1998; 89: 366-70.
24. Gallie WE. Fractures and dislocations of the cervical spine.
Am J Surg 1939; 46: 495-9.
25. Brooks Al, Jenkins EB. Atlanto-axial arthrodesis by the wedge
compression method.
J Bone Joint Surg (Am) 1978; 60:279-284
26. Dickman CA, Sonntag VKH, Papadopoulos SM et al. The
interspinous method of posterior atlantoaxial arthrodesis.
J Neurosurg 1991; 74: 190-8.
27. Jeanneret B, Magerl F. Primary posterior fusion of C1/2 in
odontoid fractures: indication, technique, and result of transarticular screw fixation.
J Spinal Disord 1992; 5: 464-75.
28. Magrel F, Seemann PS. Stable posterior fusion of the atlas and
axis by transarticular screw fixation, in Weidner PA (ed):
Cervical Spine. New York: Springer-Verlag, 1987, Vol 1, 322-7.
15. Lind B, Nordwall A, Sihlbom H. Odontoid fracture treated with
halo-vest.
Spine 1987; 12: 173-7.
29. Jain VK, Behari S. Posterior occipitoaxial fusion for
atlantoaxial dislocation associated with occipitalized atlas.
In: Wilkins R, Rengachary S (eds):Neurosurgical Operative
atlas, Volume 7. American Association of Neurological
Surgeons, Illinois,1997, pp 249-56
16. SK Shilpakar S, McLaughlin MR, Haid RW, Rodts GE et al.
Management of acute odontoid fractures: operative techniques
and complication avoidance.
Neurosurg Focus 2000; 8: 17-23.
30. Goel A, Laheri V: Plate and screw fixation for atlantoaxial
subluxation.
Acta Neurochir (Wien) 1994; 129:47-53.
17. Apfelbaum RI, Lonser RR, Veres R, Casey A. Direct anterior
screw fixation for recent and remote odontoid fractures.
Neurosurg Focus 2000; 8: 7-16.
18. Nakanishi T. Internal fixation of odontoid fractures.
Cent J Orthop Trauma Surg 1980; 23: 399-406.
19. Bohler J. Anterior stabilization for acute fractures and non-
Indian Journal of Neurotrauma (IJNT), Vol. 2, No. 1, 2005
31. Ransford AO, Crockard HA, Pozo JL, et al. Craniocervical
instability treated by contoured loop fixation.
J Bone Joint Surg (Br) 1986; 68:173-7.
Acknowledgment
All sketches in this paper have been prepared by Dr.
Bernard T. Lyngdoh
Vous aimerez peut-être aussi
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- Quant Job Application ChecklistDocument4 pagesQuant Job Application Checklistmetametax22100% (1)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- GEC PE 3 ModuleDocument72 pagesGEC PE 3 ModuleMercy Anne EcatPas encore d'évaluation
- Writing Workshop G7 PDFDocument12 pagesWriting Workshop G7 PDFJobell AguvidaPas encore d'évaluation
- The List InditexDocument126 pagesThe List InditexRezoanul Haque100% (2)
- Final Paper17Document722 pagesFinal Paper17Anjum Shakeela100% (1)
- ZX 470Document13 pagesZX 470Mohammed Shaheeruddin100% (1)
- Strategic CompensationDocument45 pagesStrategic CompensationAnjum ShakeelaPas encore d'évaluation
- 07 Post Task Theory Matrix Table RevisedDocument8 pages07 Post Task Theory Matrix Table RevisedHemalyn Bereber100% (1)
- UGC-Social Case Work-Multiple Choice Questions and AnswersDocument11 pagesUGC-Social Case Work-Multiple Choice Questions and AnswersAnjum Shakeela100% (2)
- CHT Wfa Boys P 0 2 Who Growth Chart Boys AdoptionDocument1 pageCHT Wfa Boys P 0 2 Who Growth Chart Boys Adoptiondrjohnckim100% (1)
- Investment PerspectiveDocument4 pagesInvestment PerspectiveAnjum ShakeelaPas encore d'évaluation
- Sampling and MeasurementDocument16 pagesSampling and MeasurementAkshay RajPas encore d'évaluation
- Bone Banking in A Community Hospital: Original StudyDocument6 pagesBone Banking in A Community Hospital: Original StudyAnjum ShakeelaPas encore d'évaluation
- Imm Material FinalDocument216 pagesImm Material FinalAnjum Shakeela100% (1)
- Pathology Compilation (Solved) - SinghDocument59 pagesPathology Compilation (Solved) - SinghAnjum ShakeelaPas encore d'évaluation
- (22)Document19 pages(22)Anjum ShakeelaPas encore d'évaluation
- 01organisationalchange 130127233413 Phpapp02Document22 pages01organisationalchange 130127233413 Phpapp02SamBensonPas encore d'évaluation
- 670 Challan From PDFDocument1 page670 Challan From PDFSharif JamaliPas encore d'évaluation
- Common Mistakes: Dr. Muhammad Javaid Asad Associate Professor Department of BiochemistryDocument4 pagesCommon Mistakes: Dr. Muhammad Javaid Asad Associate Professor Department of BiochemistryAnjum ShakeelaPas encore d'évaluation
- Strategichrm 131009132007 Phpapp01Document109 pagesStrategichrm 131009132007 Phpapp01Anjum ShakeelaPas encore d'évaluation
- VisionDocument1 pageVisionAnjum ShakeelaPas encore d'évaluation
- Format of The PresentationDocument1 pageFormat of The PresentationAnjum ShakeelaPas encore d'évaluation
- Application Form For Testing: BarcodeDocument5 pagesApplication Form For Testing: BarcodeAasir NaQviPas encore d'évaluation
- QM ch6Document31 pagesQM ch6Shrestha HemPas encore d'évaluation
- Lecture 1Document75 pagesLecture 1Anjum ShakeelaPas encore d'évaluation
- Nlcaf2016 PDFDocument5 pagesNlcaf2016 PDFHamid MasoodPas encore d'évaluation
- KFUEIT Employment Application FormDocument2 pagesKFUEIT Employment Application FormAnjum ShakeelaPas encore d'évaluation
- Punjab Food Authority: S T NS T NDocument4 pagesPunjab Food Authority: S T NS T NAnjum ShakeelaPas encore d'évaluation
- PSSP CWDocument1 pagePSSP CWAnjum ShakeelaPas encore d'évaluation
- KFUEIT Employment Application FormDocument2 pagesKFUEIT Employment Application FormAnjum ShakeelaPas encore d'évaluation
- Political ScienceDocument33 pagesPolitical ScienceAnjum ShakeelaPas encore d'évaluation
- Political ScienceDocument33 pagesPolitical ScienceAnjum ShakeelaPas encore d'évaluation
- Helping Employees Cope With ChangeDocument9 pagesHelping Employees Cope With ChangeAnjum ShakeelaPas encore d'évaluation
- History of International HRMDocument5 pagesHistory of International HRMAnjum ShakeelaPas encore d'évaluation
- Change Managemen1Document11 pagesChange Managemen1Anjum ShakeelaPas encore d'évaluation
- Business EthicsDocument42 pagesBusiness EthicsAsesh MandalPas encore d'évaluation
- EarthmattersDocument7 pagesEarthmattersfeafvaevsPas encore d'évaluation
- CV Ilham AP 2022 CniDocument1 pageCV Ilham AP 2022 CniAzuan SyahrilPas encore d'évaluation
- 2 Avaliação Edros 2023 - 7º Ano - ProvaDocument32 pages2 Avaliação Edros 2023 - 7º Ano - Provaleandro costaPas encore d'évaluation
- Ciac - HW Brochure Seer 16Document2 pagesCiac - HW Brochure Seer 16Tatiana DiazPas encore d'évaluation
- Retrenchment in Malaysia Employers Right PDFDocument8 pagesRetrenchment in Malaysia Employers Right PDFJeifan-Ira DizonPas encore d'évaluation
- Tugas Gizi Caesar Nurhadiono RDocument2 pagesTugas Gizi Caesar Nurhadiono RCaesar 'nche' NurhadionoPas encore d'évaluation
- The Stony Brook Press - Volume 11, Issue 4Document28 pagesThe Stony Brook Press - Volume 11, Issue 4The Stony Brook PressPas encore d'évaluation
- CA02 ParchamentoJVMDocument6 pagesCA02 ParchamentoJVMJohnrey ParchamentoPas encore d'évaluation
- Cardiovascular Pharmacology: DR Muhamad Ali Sheikh Abdul Kader MD (Usm) MRCP (Uk) Cardiologist, Penang HospitalDocument63 pagesCardiovascular Pharmacology: DR Muhamad Ali Sheikh Abdul Kader MD (Usm) MRCP (Uk) Cardiologist, Penang HospitalCvt RasulPas encore d'évaluation
- Plumber (General) - II R1 07jan2016 PDFDocument18 pagesPlumber (General) - II R1 07jan2016 PDFykchandanPas encore d'évaluation
- Dyestone Blue MX SDS SA-0186-01Document5 pagesDyestone Blue MX SDS SA-0186-01gede aris prayoga mahardikaPas encore d'évaluation
- Good Laboratory Practice GLP Compliance Monitoring ProgrammeDocument17 pagesGood Laboratory Practice GLP Compliance Monitoring ProgrammeamgranadosvPas encore d'évaluation
- Soduim Prescription in The Prevention of Intradialytic HypotensionDocument10 pagesSoduim Prescription in The Prevention of Intradialytic HypotensionTalala tililiPas encore d'évaluation
- Thornburg Letter of RecDocument1 pageThornburg Letter of Recapi-511764033Pas encore d'évaluation
- Nepal Health Research CouncilDocument15 pagesNepal Health Research Councilnabin hamalPas encore d'évaluation
- RA 9344 (Juvenile Justice and Welfare Act)Document10 pagesRA 9344 (Juvenile Justice and Welfare Act)Dan RamosPas encore d'évaluation
- Gpat Reference NotesDocument9 pagesGpat Reference NotesPreethi KiranPas encore d'évaluation
- Pioneer Deh-P4850mp p4850mphDocument76 pagesPioneer Deh-P4850mp p4850mphVxr GsiPas encore d'évaluation
- Kerala Medico Legal Code - Annexure2Document19 pagesKerala Medico Legal Code - Annexure2doctor82Pas encore d'évaluation
- DoDough FriedDocument7 pagesDoDough FriedDana Geli100% (1)
- Evolution of Fluidized Bed TechnologyDocument17 pagesEvolution of Fluidized Bed Technologyika yuliyani murtiharjonoPas encore d'évaluation
- Zemoso - PM AssignmentDocument3 pagesZemoso - PM AssignmentTushar Basakhtre (HBK)Pas encore d'évaluation
- Day Case Open Appendectomy: A Safe and Cost-Effective ProcedureDocument9 pagesDay Case Open Appendectomy: A Safe and Cost-Effective ProcedureAcademecian groupPas encore d'évaluation
- Catalogo StafsjoDocument12 pagesCatalogo StafsjoBruno Bassotti SilveiraPas encore d'évaluation