Académique Documents
Professionnel Documents
Culture Documents
CT-scan On Pedia
Transféré par
GeeTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
CT-scan On Pedia
Transféré par
GeeDroits d'auteur :
Formats disponibles
Pediatric Head Injury 1
A Validation Study of the OMMC Department of Surgery
Protocol on Head Injuries on Pediatric Patients
Nolan Ortega Aludino, MD
Alfonso Nunez, MD, FPCS
Department of Surgery
Ospital ng Maynila Medical Center
Reprint requests:
Nolan O. Aludino, MD, Department of Surgery, Ospital ng Maynila Medical
Center, Quirino Avenue, Malate, Manila, Philippines
email:ommcsurgery@yahoo.com
Protocol on Head Injuries on Pediatric Patients
Pediatric Head Injury 2
Abstract:
Objective To validate the protocol formulated by the OMMC Department of
Surgery in diagnosing pediatric patients with head injuries.
Methods A validation study of the department protocol on head injuries. It is a
prospective study. Pediatric patients aged 0-13 years old are included in the
study.
Results From January 1, 2005 up to August 31, 2005, data collection done on
pediatric patients with head injuries. Persistent vomiting was identified as a
possible indicator for head injury on a pediatric patient and subsequent CT scan.
Conclusion Persistent vomiting has been shown to an ineffective indicator for
head injury in pediatric patients. The routine use of CT scan is therefore not
advocated as part of the management of head injury in pediatric patients.
The department policy of the Department of Surgery, Ospital ng Maynila
Medical Center, regarding the non-use of routine CT scan in pediatric head
trauma patient is validated.
Key words: pediatric head injuries, CT scan
Pediatric Head Injury 3
Introduction:
The diagnosis of head injury has always caused controversies. While
there is no problem in diagnosing patients with obvious head injuries, patients
with mild head injuries present more difficulties. Physicians have always been
wary of discharging patients with apparent mild head injuries for fear that these
patients may be harboring an occult injury.
The advent of different imaging modalities have provided the clinician
some sense of security in the diagnosis and management such patients.
Computer aided tomography scans (CT-scans) and magnetic resonance imaging
(MRI) have become part of the armamentarium of the clinician in diagnosing
head injury.
Pediatric patients with head injuries are more difficult to diagnose that your
usual adult patient. These may be due to inability to communicate freely with the
physician, especially those in the very young age group. Should we now consider
using the routine use of the CT scan?
Current literature has defined the following as the indications for CT scan
in a pediatric patient: posttraumatic seizures, amnesia, progressive headache,
unreliable history or examination because of possible alcohol or drug ingestion,
loss of consciousness for longer than 5 minutes, physical signs of basilar skull
fracture, repeated vomiting or vomiting for more than 8 hours after injury, and
instability following multiple traumas.
Pediatric Head Injury 4
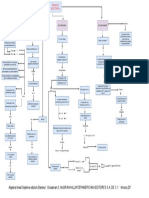
The Department of Surgery in Ospital ng Maynila Medical Center believes
that routine CT scan in all pediatric patients is an unnecessary financial burden to
the patient and it result in unnecessary exposure to radiation. As such, the
Department formulated a Health Process Evidence Based Clinical Practice
Guideline with regards to patients with head injury. Validation of this protocol
would mean less health costs for the patient and elimination of unnecessary
exposure to radiation thus improving the quality of care given to them.
Pediatric Head Injury 5
Objective:
This study aims to validate the protocol formulated by the OMMC
Department of Surgery regarding the diagnosis of patients with head injuries in
the pediatric age group. The author wishes to prove whether or not the use of
persistent vomiting can be used as an indicator for traumatic brain injury.
Pediatric Head Injury 6
Methods
This will be a validation study of the department protocol on head injuries.
It is designed as a prospective study. All pediatric patients aged 0-13 years old
who seek consult at the ER due to head injuries will be examined. Patients
fulfilling the inclusion criteria will be included in the study and records will be kept.
All pediatric patients with persistent vomiting and have no evident
fractures on the skull x-ray will be included in this study
All pediatric patients with persistent vomiting without changes in GCS for
twenty four hours do not have to undergo a CT scan. All patients with persistent
vomiting with changes in GCS greater than or equal to two (2) should undergo a
CT scan.
Persistent vomiting is defined as vomiting of at least 4 times 8 hours from
time of consult. The following will be taken note of: those with persistent vomiting,
changes in GCS status, CT scan results, morbidities and mortalities.
All patients will have to come in for follow up at the Surgery OPD 10 days
from date of discharge.
A checklist/form would be formulated to facilitate standardization of
examination at the ER, ward and upon follow up at the Surgery OPD.
Pediatric Head Injury 7
The following GCS scoring will be used (1):
Eye Opening
Score
>1 Year
0-1 Year
Opens eyes
Opens eyes
spontaneously
spontaneously
4
Opens eyes to a verbal
3
Opens eyes to a shout
command
Opens eyes in response Opens eyes in
2
1
to pain
response to pain
No response
No response
Best Motor Response
Score
>1 Year
0-1 Year
Obeys command
N/A
Localizes pain
Localizes pain
Flexion withdrawal
Flexion withdrawal
Flexion abnormal
Flexion abnormal
(decorticate)
(decorticate)
3
2
Extension (decerebrate) Extension (decerebrate)
No response
No response
Pediatric Head Injury 8
Best Verbal Response
Score
>5 Years
2-5 Years
0-2 Years
Uses
Oriented and able to
5
appropriate
Cries appropriately
converse
words
Uses
Disoriented and able
4
inappropriate
Cries
to converse
words
Cries and/or
Uses inappropriate
Cries and/or
words
screams
screams
inappropriately
Makes
incomprehensible
Grunts
Grunts
No response
No response
sounds
1
No response
Pediatric Head Injury 9
Results:
Table 1 shows the age distribution of pediatric patient patients with
vomiting secondary to head trauma from Jan 1, 2005 to August 31, 2005. During
this time period. there were forty-eight patients aged thirteen and below who
sought consult at the OMMC Surgery Emergency Room due to vomiting as a
result of head trauma. Of these patients, only thirty-three had persistent vomiting.
Majority of the patients with persistent vomiting are aged two to three.
Table 2 shows the age distribution of pediatric patients who sought consult
due to head trauma with positive findings on x-ray of the skull. Two out of the
thirty-three patients were excluded because of positive initial skull x-ray readings.
Table 3 shows the number of pediatric patients seeking consult due to
head trauma with changes in their GCS (2). There were 4 patients who showed
a change in GCS of more than two. One was excluded from the study because of
positive initial findings on skull x-ray.
Table 4 shows the number of pediatric patients who sought consult due to
head trauma and eventually underwent CT scan. CT scan was eventually
performed on four patients. Three out of these four had normal CT scan results.
One patient showed a subdural hematoma on CT scan. One patient who had a
normal CT was excluded from the study because of positive initial findings on
skull x-ray.
Pediatric Head Injury 10
Discussion
Diagnosing traumatic head injury continues to be one of the challenges
confronting clinicians, both within and outside our local setting. Pediatric patients
with head injuries confound the problem because of the difficulty of establishing
an effective communication between the physician and the patient.
Patients with obvious head injuries and those whose skull x-rays showed
positive findings are easier for the physician to diagnose and therefore institute
the appropriate treatment. It is those patients who present with a history of head
trauma, with some signs of head injuries like a history loss of consciousness, and
vomiting and yet upon closer examination show no signs of neurologic deficit that
are somewhat more difficult to diagnose with a high degree of certainty.
From January 1, 2005 up to August 31, 2005, the author has been
collecting data on pediatric patients with head injuries. Persistent vomiting was
identified as a possible indicator for head injury on a pediatric patient.
There were thirty-three patients who fulfilled the inclusion criteria. Four of
them underwent CT scan. Three of those who underwent CT scan showed
normal results while one patient showed evidence of intracranial bleeding. It must
be pointed out however, that only one patient who presented with vomiting had
an actual traumatic head injury. All other patients were discharged without any
neurologic deficit. Follow up of these patients showed no recurrence of
symptoms or downgrade in their neurologic status.
Pediatric Head Injury 11
Other studies have shown that clinical signs of brain injury are insensitive
indicators of intracranial injury in infants and that only significant scalp
hematomas would indicate an intracranial injury necessitating radiographic
imaging. Asymptomatic infants older than 3 months of age who have no
significant scalp hematoma may be safely managed without radiographic
imaging. (1)
Another study has shown that Glasgow Coma Scale (GCS) score of 12 or
lower and the presence of focal neurological deficits were significant predictors of
an abnormal CT scan. Ninety-five per cent of those with abnormal CT scans and
100% of those with intracranial injury could be identified by the presence of one
or more of the nine clinical findings, particularly by a GCS score of 12 or lower,
and the presence of focal neurological deficits. Identification was also possible to
a lesser degree by loss of consciousness, ataxia, amnesia, drowsiness,
headache, seizure or vomiting. (2) Headache and nausea did not increase the
risk of skull fracture and intracranial lesions on the CT. (3)
For some head injuries, there is little debate about which patients need an
imaging test. The accepted high-risk indicators include: (a) loss of consciousness
for more than 5 minutes, (b) depressed or decreasing level of consciousness (c)
focal neurological findings (d) seizure (e) failure of the mental status to improve
over time in an alcohol-intoxicated patient (f) penetrating skull injuries (g) signs of
a basal or depressed skull fracture (4,5,6,7) (h) confusion or aggression on
Pediatric Head Injury 12
examination. Headache, dizziness, scalp hematomas, lacerations, contusions,
and abrasions are not considered high-risk factors. (8,9,10,11)
Clearly it can be seen that even international studies support the idea that
routine CT scan should not be included in the management of head injuries in
pediatric patients. Furthermore, vomiting is clearly not an indicator for requesting
a CT scan.
Pediatric Head Injury 13
Conclusion:
Persistent vomiting has been shown to an ineffective indicator for head
injury in pediatric patients. Thus, requesting for a CT scan, just because the
patient presents with persistent vomiting may not be cost effective. The clinician
must look at other clinical findings to determine the need for further imaging
studies. The routine use of CT scan is therefore not advocated as part of the
management of head injury in pediatric patients.
It is also concluded that the department policy of the Department of
Surgery, Ospital ng Maynila Medical Center, regarding the non-use of routine CT
scan in pediatric head trauma patient is validated.
Pediatric Head Injury 14
References:
1. Greene SG, Schutzman SA. Clinical indicators of intracranial injury in
head-injured infants. Pediatrics 1999.
2. Ng SM, Toh EM, Sherrington CA. Clinical predictors of abnormal
computed tomography scans in paediatric head injury. J Paediatr Child
Health. 2002; 38(4):388-92.
3. Shiomi N, Echigo T. A guide to initial management of minor head injuryNo
Shinkei Geka. 2004 ;32(5):465-70.
4. Jeret JS, Mandell M, Anziska B, et al. Clinical predictors of abnormality
disclosed by computed tomography after mild head trauma. Neurosurgery
1993; 32:915.
5. Moran SG, McCarthy MC, Uddin DE, Poelstra RJ. Predictors of positive
CT scans in the trauma patient with minor head injury. Am Surg 1994;
60:533536.
6. Duus BR, Lind B, Christensen H, Nielsen OA. The role of neuroimaging in
the initial management of patients with minor head injury. Ann Emerg Med
1994; 23:12791283.
7. Cummins RO, LoGerfo JP, Inui TS, Weiss NS. High-yield referral criteria
for posttraumatic skull roentgenography. Response of physicians and
accuracy of criteria. JAMA 1980; 244:673676.
8. Thornbury JR, Campbell JA, Masters SJ, Fryback DG. Skull fracture and
the low risk of intracranial sequelae in minor head trauma. AJR Am J
Roentgenol 1984; 143:161164.
Pediatric Head Injury 15
9. Vydareny KH, Harle TS, Potchen EJ. An algorithmic approach to the
roentgenographic evaluation of head trauma: medical and financial
implications. Invest Radiol 1983; 18:390395.
10. Ingebrigtsen T, Romner B. Management of minor head injuries in
hospitals in Norway. Acta Neurol Scand 1997; 95:5155.
11. Schunk JE, Rodgerson JD, Woodward GA. The utility of head computed
tomographic scanning in pediatric patients with normal neurologic
examination in the emergency department. Pediatr Emerg Care 1996;
12:160165.
12. Stock A, Singer L, Head Trauma, Emedicine, 2004
13. Maier B, Maier-Hemming A, Lehnert M, Mutschler WE, et al. Relevance of
CT-scans for pediatric head injuries, Unfallchirurg. 2003;106(3):220-5.
14. Kaplan M. , Faik Ozveren M., Topsakal C., et al. Asymptomatic interval in
delayed traumatic intracerebral hemorrhage: report of two cases, Clinical
Neurology and Neurosurgery Volume 105, Issue 3 , 2003, 153-155.
15. Miller L., Kent R. and Tennant A., Audit of head injury management in
Accident and Emergency at two hospitals: implications for NICE CT
guidelines, BMC Health Services Research 2004, 4:7.
16. Ibanez J, Arikan F, Pedraza S, et al., Reliability of clinical guidelines in the
detection of patients at risk following mild head injury: results of a
prospective study. J Neurosurg. 2004;100(5):825-34.
Pediatric Head Injury 16
17. Ng SM, Toh EM, Sherrington CA. Clinical predictors of abnormal
computed tomography scans in paediatric head injury. J Paediatr Child
Health. 2002;38(4):388-92.
18. Abdul Latip, L.S., Ahmad Alias, N.A., Ariff A.R., et al. CT scan in minor
head injury: a guide for rural doctors. Journal of Clinical Neuroscience
Volume 11, Issue 8 ,2004, 835-839.
19. Palchak MJ, Holmes J, Vance C, et al., A Decision Rule for Identifying
Children at Low Risk for Brain Injuries After Blunt Head Trauma, Annals of
Emergency Medicine 42:4 2003.
20. J Dunning, J Batchelor, P Stratford-Smith, et al., A meta-analysis of
variables that predict significant intracranial injury in minor head trauma,
Arch Dis Child 2004;89:653659.
Pediatric Head Injury 17
Table 1. Age distribution of pediatric patient patients with vomiting
secondary to head trauma from Jan 1, 2005 to August 31, 2005.
AGE
0-1
2-3
4-5
6-7
8-9
10-11
12-13
Total
VOMITING
8
17
10
6
1
4
2
47
PERSISTENT VOMITING
3
10
7
6
1
5
1
33
Pediatric Head Injury 18
Table 2: Age distribution of pediatric patients who sought consult due to
head trauma with positive findings on x-ray of the skull.
AGE
0-1
2-3
4-5
6-7
8-9
10-11
12-13
Total
SKULL AP/L
0
2
0
0
0
0
0
2
Pediatric Head Injury 19
Table 3: Number of pediatric patients seeking consult due to head trauma
with changes in their GCS (>2).
AGE
0-1
2-3
4-5
6-7
8-9
10-11
12-13
Total
GCS CHANGES
0
1
0
1
1
1
0
4
Pediatric Head Injury 20
Table 4: Number of pediatric patients who sought counsult due to head
trauma and eventually underwent CT scan.
AGE
0-1
2-3
4-5
6-7
8-9
10-11
12-13
Total
CT SCAN
0
1
0
1
1
1
0
4
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (120)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- DIN EN 12516-2: January 2015Document103 pagesDIN EN 12516-2: January 2015ReytingPas encore d'évaluation
- United States Court of Appeals Fifth CircuitDocument4 pagesUnited States Court of Appeals Fifth CircuitScribd Government DocsPas encore d'évaluation
- Article On Financial PlanningDocument16 pagesArticle On Financial PlanningShyam KumarPas encore d'évaluation
- DeathoftheegoDocument123 pagesDeathoftheegoVictor LadefogedPas encore d'évaluation
- The Confederation or Fraternity of Initiates (1941)Document82 pagesThe Confederation or Fraternity of Initiates (1941)Clymer777100% (1)
- Right To Freedom From Torture in NepalDocument323 pagesRight To Freedom From Torture in NepalAnanta ChalisePas encore d'évaluation
- Roger Dean Kiser Butterflies)Document4 pagesRoger Dean Kiser Butterflies)joitangPas encore d'évaluation
- Civil Procedure Pros. Zehan Loren E. Tocao-Talipasan, RebDocument4 pagesCivil Procedure Pros. Zehan Loren E. Tocao-Talipasan, Rebxeileen08100% (2)
- Bahaa CVDocument3 pagesBahaa CVbahaa ahmedPas encore d'évaluation
- MigrationDocument6 pagesMigrationMaria Isabel PerezHernandezPas encore d'évaluation
- State Public Defender's Office InvestigationDocument349 pagesState Public Defender's Office InvestigationwhohdPas encore d'évaluation
- Algebra Lineal Septima Edicion Stanley I. Grossman S. Mcgraw-Hilliinteramericana Editores S.A. de C.V Mexico, DFDocument1 pageAlgebra Lineal Septima Edicion Stanley I. Grossman S. Mcgraw-Hilliinteramericana Editores S.A. de C.V Mexico, DFJOSE JULIAN RAMIREZ ROJASPas encore d'évaluation
- Independence of Costa RicaDocument2 pagesIndependence of Costa Ricaangelica ruizPas encore d'évaluation
- SyerynDocument2 pagesSyerynHzlannPas encore d'évaluation
- Due Books List ECEDocument3 pagesDue Books List ECEMadhumithaPas encore d'évaluation
- Campus Design: School of Architecture & Planning at PondicherryDocument9 pagesCampus Design: School of Architecture & Planning at Pondicherrynadhir sulaimanPas encore d'évaluation
- Right To Information: National Law University AND Judicial Academy, AssamDocument20 pagesRight To Information: National Law University AND Judicial Academy, Assamsonu peterPas encore d'évaluation
- Bba 2ND Year Business Communication NotesDocument11 pagesBba 2ND Year Business Communication NotesDivya MishraPas encore d'évaluation
- How A Type 4 Multiverse WorksDocument4 pagesHow A Type 4 Multiverse WorksIdkPas encore d'évaluation
- High-Performance Cutting and Grinding Technology For CFRP (Carbon Fiber Reinforced Plastic)Document7 pagesHigh-Performance Cutting and Grinding Technology For CFRP (Carbon Fiber Reinforced Plastic)Dongxi LvPas encore d'évaluation
- Disciplinary Literacy Strategies To Support Transactions in Elementary Social StudiesDocument11 pagesDisciplinary Literacy Strategies To Support Transactions in Elementary Social Studiesmissjoseph0803Pas encore d'évaluation
- Basic OmDocument242 pagesBasic OmRAMESH KUMARPas encore d'évaluation
- Bed BathDocument6 pagesBed BathKristil ChavezPas encore d'évaluation
- Team 12 Moot CourtDocument19 pagesTeam 12 Moot CourtShailesh PandeyPas encore d'évaluation
- Minimalist Aesthetics Business Plan by SlidesgoDocument63 pagesMinimalist Aesthetics Business Plan by Slidesgorandom potatoPas encore d'évaluation
- Exeter: Durance-Class Tramp Freighter Medium Transport Average, Turn 2 Signal Basic Pulse BlueDocument3 pagesExeter: Durance-Class Tramp Freighter Medium Transport Average, Turn 2 Signal Basic Pulse BlueMike MitchellPas encore d'évaluation
- Class 11 Class Biology Syllabus 2011-12Document5 pagesClass 11 Class Biology Syllabus 2011-12Sunaina RawatPas encore d'évaluation
- Arthropods: Surviving The Frost: Charmayne Roanna L. GalangDocument2 pagesArthropods: Surviving The Frost: Charmayne Roanna L. GalangBabes-Rose GalangPas encore d'évaluation
- 130004-1991-Maceda v. Energy Regulatory BoardDocument14 pages130004-1991-Maceda v. Energy Regulatory BoardChristian VillarPas encore d'évaluation
- Draft DAO SAPA Provisional AgreementDocument6 pagesDraft DAO SAPA Provisional AgreementStaff of Gov Victor J YuPas encore d'évaluation