Académique Documents
Professionnel Documents
Culture Documents
Clinical, Biochemical, Immunological and Virological Profiles Of, and Differential Diagnosis Between, Patients With Acute Hepatitis B and Chronic Hepatitis B With Acute Flare
Transféré par
Raison D'etreTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Clinical, Biochemical, Immunological and Virological Profiles Of, and Differential Diagnosis Between, Patients With Acute Hepatitis B and Chronic Hepatitis B With Acute Flare
Transféré par
Raison D'etreDroits d'auteur :
Formats disponibles
doi:10.1111/j.1440-1746.2008.05600.
H E PAT O L O G Y
Clinical, biochemical, immunological and virological profiles
of, and differential diagnosis between, patients with acute
hepatitis B and chronic hepatitis B with acute flare
Yongnian Han, Qun Tang, Wei Zhu, Xiaoqing Zhang and Longying You
Research Unit of Liver Disease, Shanghai No. 8 Peoples Hospital, Shanghai, China
Key words
acute hepatitis B, alpha-fetoprotein, chronic
hepatitis B, differential diagnosis, hepatitis B
virus.
Accepted for publication 24 February 2008.
Correspondence
Dr Yongnian Han, Research Unit of Liver
Disease, Shanghai No. 8 Peoples Hospital,
8 Caobao Road, Shanghai 200235, China.
Email: hanyn88@163.com
Abstract
Background and Aim: In areas with high or intermediate endemicity for chronic hepatitis
B virus (HBV) infection, it is difficult to distinguish acute hepatitis B (AHB) from chronic
hepatitis B with an acute flare (CHB-AF) in patients whose prior history of HBV infection
has been unknown. The present study aimed to screen laboratory parameters other than
immunoglobulin M antibody to hepatitis B core antigen (IgM anti-HBc) to discriminate
between the two conditions.
Methods: A retrospective and prospective study was conducted in patients first presenting
clinically as HBV-related acute hepatitis to sort out acute self-limited hepatitis B (ASLHB). Then, clinical and laboratory profiles were compared between patients with ASL-HB
and CHB-AF. Parameters closely associated with ASL-HB were chosen to evaluate sensitivity, specificity, accuracy, positive predictive values and negative predictive values for
diagnosing AHB.
Results: There were significant differences between patients with ASL-HB and CHB-AF
in relation to clinical and laboratory aspects, with many outstanding differences in levels of
serum HBV-DNA, hepatitis B e antigen (HBeAg) and alpha-fetoprotein (AFP) as well as
IgM anti-HBc. In particular, there was a greater difference between the two groups in low
levels of HBeAg (ratio of the optical density of the sample to the cut-off value [S/CO] <20)
than in negativity for HBeAg (42.7% and 13.5% vs 49.3% and 45.9%). 1:10 000 IgM
anti-HBc had a sensitivity and specificity of 96.2% and 93.1%, respectively, for predicting
ASL-HB. Combining it with AFP, HBeAg or HBV-DNA could improve diagnostic power.
A combination of IgM anti-HBc, HBV-DNA and HBeAg had a predictive value of 98.9%
and a negative predictive value of 100.0%, similar to that of a combination of IgM anti-HBc
and HBV-DNA. Adding AFP to the combinations of IgM anti-HBc and HBV-DNA or
HBeAg could further heighten the positive predictive value. The positive predictive value
and negative predictive value of the combination of IgM anti-HBc, HBV-DNA and AFP
were both 100.0%.
Conclusions: (i) There are significant differences with respect to clinical, biochemical,
immunological and virological aspects between ASL-HB and CHB-AF. (ii) Of several
diagnostic combinations, IgM anti-HBc jointing HBV-DNA is most effective and most
practicable in distinguishing ASL-HB from CHB-AF. (iii) A low HBeAg level is more
useful than negative HBeAg in differential diagnosis between ASL-HB and CHB-AF. (iv)
In those patients with a high level of IgM anti-HBc, serum AFP level >10 upper reference
limit could rule out a probability of ASL-HB.
Introduction
Hepatitis B virus (HBV) is a peculiar virus, leading to both an
acute infection and a chronic one. HBV-related acute hepatitis may
be a true episode of acute hepatitis B (AHB) or an acute flare of
chronic hepatitis B (CHB) hitherto unknown. It is important to
distinguish AHB patients, a great number of whom will have a
1728
self-limited, benign course and not require intervention, from
patients with CHB with an acute flare (CHB-AF) who will
not have such a benign course and benefit from treatment with
antiviral agents.1
The presence of serum hepatitis B surface antigen (HBsAg)
with clinical and biochemical features of acute hepatitis usually
suggests AHB in patients from low HBV infection endemic areas
Journal of Gastroenterology and Hepatology 23 (2008) 17281733 2008 The Authors
Journal compilation 2008 Journal of Gastroenterology and Hepatology Foundation and Blackwell Publishing Asia Pty Ltd
Y Han et al.
but not in patients from high or intermediate HBV endemic
regions, where AHB and CHB-AF may be misdiagnosed mutually,
especially if patients antecedent HBV carrier status is unknown.
Immunoglobulin M antibody to hepatitis B core antigen (IgM
anti-HBc) has been well recognized as a gold standard for
diagnosis of acute HBV infection.2,3 The commercially available
enzyme immunoassays (EIA) for IgM anti-HBc have been
designed to detect only higher titers of the antibody, but IgM
anti-HBc is present in approximately 1015% of patients with
CHB, especially in those with CHB-AF.2,3 IgM anti-HBc in high
titers had a high sensitivity (90100%) and specificity (90100%)
for the diagnosis of acute HBV infection.46 The results, however,
were obtained by comparison of acutely HBV-infected patients
with those with common CHB without an acute flare, even with
healthy individuals who were only positive for anti-HBc. When
CHB-AF was compared, IgM anti-HBc in a titer of 1:1000 had a
sensitivity of only 77.6% and a specificity of 70.0% for diagnosing
AHB.7 Although a fully automated microparticle chemiluminescent immunoassay in which significant specimen dilution and
multiple steps are avoided, has recently been developed, an ideal
cut-off value to differentiate AHB from CHB-AF seems not to be
established, because a great range (1.5, 2.42.5 and 10) of cut-off
index values have been reported in patients from Greece, Taiwan
and Italy; 9085% and 100%, respectively, regarding sensitivity
and 8690% and 99%, respectively, regarding specificity for diagnosing acute hepatitis B were shown in the two latter studies.810
However, the nearly perfect diagnostic power from Italys study
also resulted from comparison of AHB with common CHB
without acute exacerbation.10
Therefore, it is necessary to seek other parameters to assist IgM
anti-HBc to distinguish AHB from CHB-AF in patients with no
prior HBV infection history information whose diagnosis could
not be made by IgM anti-HBc alone during hospitalization. It has
been reported that HBV-DNA <0.5 pg/mL at initial presentation
had a sensitivity of 95.9% and a specificity of 86.6% for predicting
AHB in a recent study.7 Unfortunately, there were only 49 patients
with AHB in the study and the diagnostic performance of a
combination of IgM anti-HBc and HBV-DNA was not displayed.
The present large study is intended to find better methods to
discriminate the two diseases by comparison of the characteristics
of patients with ASL-HB and CHB-AF with regard to clinical,
biochemical, immunological and virological aspects.
Methods
Patients and study design
A retrospective investigation (from January 2003 to March 2005)
and a prospective study (from April 2005 to June 2006) were put
into practice in patients with their first attack of HBV-related acute
hepatitis whose status of prior HBV infection had been unknown.
HBV-related acute hepatitis was defined according to: (i) biochemical parameters: levels of serum alanine aminotransferase
(ALT) >10-fold the upper reference limit (URL), or total serum
bilirubin (TBil) >5 URL, and serum alkaline phosphatase (ALP)
<3 URL;11 and (ii) HBV markers: positive for serum hepatitis B
surface antigen (HBsAg), or serum antibodies to HBsAg, hepatitis
B e antigen (HBeAg), and hepatitis B core antigen (HBcAg).
Hepatitis A, C, D and E, and non-viral causes, such as drugs,
Profiles and differential diagnosis of AHB
alcohol, pregnancy, ischemia, etc. that can lead to the same biochemical profiles, were all excluded. Patients who showed ultrasonographic evidence of cirrhosis were also excluded. They would
be examined retrospectively or followed up prospectively. Acute
self-limiting hepatitis B (ASL-HB) was defined as HBsAg clearing from serum after the disease remitted, or positivity for IgM
anti-HBc and for antibodies to HBsAg, HBeAg and HBcAg, with
infections with other non-hepatotropic viruses, such as human
cytomegalovirus (CMV), EpsteinBarr virus (EBV) and enteric
viruses being excluded. Alternatively, if serum HBsAg had
persisted for at least 12 months after the onset of clinically acute
hepatitis (HBsAg occasionally became undetectable until 1 year
after acute HBV infection,12 and one of our patients with ASL-HB
cleared HBsAg from serum at the 12th month after the onset of the
illness), the condition was classified as CHB.
Meanwhile, known chronically HBV-infected patients with the
same biochemical profiles as described above hospitalized during
the same period were named as CHB-AF, recruited as a control
group when other types of viral hepatitis and the above non-viral
causes were excluded, and compared with ASL-HB patients with
regard to clinical, biochemical, immunological and virological
profiles. Then, parameters with great differences and little overlap
in values were selected to assess their sensitivity, specificity,
accuracy, positive predictive value and negative predictive value
for diagnosing AHB or ASL-HB.
Data collection
Data were collected including clinical symptoms, physical signs
and laboratory examinations. The latter included: (i) biochemical
tests reflecting hepatocytic damage, such as serum TBil, ALT,
g-glutamyl transferase (GGT), prealbumin, all assayed by a colorimetric method (CSL Behring, King of Prussia, PA, USA), and
prothrombin time (PT), done as described by the manufacturers
instruction (Trinity Biotech, Wicklow, Ireland); (ii) HBV markers,
such as HBV antigens and antibodies, detected by commercially available enzyme immunoassays (Shanghai Kehua Bioengineering Co., Shanghai, China) and HBV-DNA, determined
by a fluorescent quantifying polymerase chain reaction (PCR)
method with a low limit of detection of 103 copies/mL (PG Biotech,
Shenzhen, China); (iii) alpha-fetoprotein (AFP), measured by
the electrochemiluminescence immunoassay (Roche Diagnostics,
Mannheim, Germany).
For the patients in the retrospective subgroup, HBV immunological markers were recorded on the basis of inpatient and outpatient information stored in our hepatic clinic, and outpatient
information in other hospitals acquired by questionnaire or telephone visits with copies of test reports being sent to us. Those who
had no results of HBV markers were called to our clinic to undergo
the examination. For patients in the prospective subgroup, HBV
markers were determined monthly during the first 6 months or
bimonthly during the next 6 months.
Statistical analysis and diagnostic performance
of laboratory tests
Independent Students t-test was used for measurement of data,
the MannWhitneys U-test for ranked enumeration data, and the
c2-test for other enumeration data. If the expected value in any cell
Journal of Gastroenterology and Hepatology 23 (2008) 17281733 2008 The Authors
Journal compilation 2008 Journal of Gastroenterology and Hepatology Foundation and Blackwell Publishing Asia Pty Ltd
1729
Profiles and differential diagnosis of AHB
Y Han et al.
was less than 5, Fishers exact test was used for the data suitable
for a fourfold table and MannWhitneys U-test was used for those
unsuitable for a fourfold table. All tests were two-sided and all
analyses were carried out with the SPSS version 11.5 software
package (SPSS Inc., Chicago, IL, USA).
Sensitivity, specificity, accuracy, positive predictive values, and
negative predictive values of each or combinations of parameters
screened out were calculated, respectively.
Results
Outcomes of HBV-related acute hepatitis
Of the 219 patients with HBV-related acute hepatitis, 27 of 141
in the retrospective subgroup were not located, but none of 78 in
the follow-up subgroup was lost. Of 192 patients studied, 138 were
confirmed to have ASL-HB, diagnosed by the disappearance of
serum HBsAg, whereas the remaining 54 were shown to remain
HBsAg positive after remission of the disease, diagnosed as
having CHB, including CHB to which AHB evolved, and real
CHB with acute exacerbation that had not been found before,
which is a common phenomenon in China.
Symptomatic cases were more common (95.7% vs 79.7%,
P < 0.001) in the ASL-HB group than in the CHB-AF group.
Influenza-like symptoms including pyrexia, poor appetite and
vomiting were all observed in more patients with ASL-HB than in
those with CHB-AF. As for physical signs, jaundice was found
more frequently and splenomegaly more infrequently in ASL-HB
patients than in CHB-AF patients.
Compared to those with CHB-AF, ASL-HB patients had more
severe necroinflammation of the liver, being characterized by
higher levels of serum TBil, ALT, and GGT, but less impaired
instantaneous liver functions, being characterized by higher levels
of serum prealbumin, and a shorter PT (Table 2). One of the most
remarkable findings was a difference in serum AFP levels between
the two groups. Elevated levels of serum AFP were found in fewer
patients with ASL-HB than in those with CHB-AF (26.1% vs
63.2%, P < 0.001) and, among individuals with elevation of serum
AFP, ASL-HB patients had a far lower average concentration than
did patients with CHB-AF (13.9 ng/mL vs 171.7 ng/mL,
P < 0.001), with only one of 36 (2.8%) versus 42 of 85 (49.4%) in
the two groups, respectively, having an AFP level >5 URL
(35.1 ng/mL) (P < 0.001).
Immunological and virological characteristics
Clinical and biochemical characteristics
A comparison of clinical manifestations between 138 patients with
ASL-HB and 133 patients with an acute flare of known chronic
hepatitis B (CHB-AF group) is displayed in Table 1. No differences were found in sex, age and family history of CHB between
the two patient groups.
Table 1 Patient demographics and clinical characteristics of ASL-HB
and CHB-AF
CHB-AF
(n = 133)
General profile
Age (years; mean SD)
35.9 10.9
Male/female
105/28
Family history of chronic HBV infection
None, or not known (%)
106 (79.7)
Yes (%)
27 (20.3)
Symptoms
Flu-like symptoms including pyrexia (%)
7 (5.3)
Poor appetite (%)
82 (61.7)
Abdomen distention after meals (%)
92 (69.2)
Nausea (%)
55 (41.4)
Vomiting (%)
15 (11.3)
Anorexia for greasy food (%)
12 (9.0)
Vague ache in hepatic region (%)
38 (28.6)
Lassitude and fatigue (%)
90 (67.7)
Physical findings
Jaundice (%)
75 (56.4)
Hepatomegaly (%)
22 (16.5)
Splenomegaly (%)
42 (31.6)
ASL-HB
(n = 138)
36.6 10.2
113/25
120 (87.0)
18 (13.0)
23
109
102
69
34
16
29
95
(16.7)*
(79.0)*
(73.9)
(50.0)
(24.6)*
(11.6)
(21.0)
(68.8)
129 (93.5)**
18 (13.1)
24 (17.5)*
*P < 0.01; **P < 0.001.
ASL-HB, acute self-limited hepatitis B; CHB-AF, chronic hepatitis B with
acute flare.
1730
The prevalence of serum HBsAg and HBeAg was found to be
similar between the two groups, but the titers, as reflected by the
ratio of the optical density of the sample to the cut-off value
(S/CO) in the EIA method, were both lower, and the rate of HBeAg
seroconversion during hospitalization was higher in ASL-HB
patients than in those with CHB-AF (Table 3). An outstanding
finding was that HBeAg with S/CO <20 had been found in many
Table 2
Comparison of biochemical tests in ASL-HB and CHB-AF
Variable
TBil
Normal (%)
Elevated (mmol/L):
n/mean SD
ALT (URL)
GGT
Normal (%)
Elevated (URL):
n/mean SD
PT
Normal (%)
Elevated (INR):
n/mean SD
AFP
Normal (%)
Elevated (ng/mL):
n/mean SD
Prealbumin (mg/mL)
CHB-AF (n = 133)
ASL-HB (n = 138)
15 (11.3)
118/68.1 71.2
3 (2.2)*
135/109.1 82.1**
18.2 9.4
32.4 19.9**
9 (6.8)
124/3.1 2.1
5 (3.6)
133/4.1 3.7*
105 (78.9)
28/2.0 1.0
127 (92.0)*
11/2.3 1.4
49 (36.8)
84/171.7 328.2
102 (73.9)**
36/13.9 8.3**
153.6 88.7
199.4 106**
*P < 0.01; **P < 0.001.
AFP, alpha-fetoprotein; ALT, alanine aminotransferase; ASL-HB, acute
self-limited hepatitis B; CHB-AF, chronic hepatitis B with acute flare;
GGT, gamma-glutamyl transferase; INR, international normalized ratio;
PT, prothrombin time; TBil, total bilirubin; URL, upper reference limit.
Journal of Gastroenterology and Hepatology 23 (2008) 17281733 2008 The Authors
Journal compilation 2008 Journal of Gastroenterology and Hepatology Foundation and Blackwell Publishing Asia Pty Ltd
Y Han et al.
Table 3
Profiles and differential diagnosis of AHB
Serological findings of ASL-HB and CHB-AF
CHB-AF
ASL-HB
HBV immunological markers**
HBsAg+, HBeAg+/anti-HBe- (%) 71 (53.4)
69 (50.0)
43 (31.2)
HBsAg+, HBeAg-/anti-HBe+ (%) 54 (40.6)
8 (6.0)
12 (8.7)
HBsAg+, HBeAg-/anti-HBe- (%)
HBsAg- (%)
0
14 (10.1)
HBsAg***, S/CO <50 (%)
31 (23.3)
64 (46.4)
HBeAg***
Negativity
61 (45.9)
68 (49.3)
S/CO <20 (%)
18 (13.5)
59 (42.7)
S/CO 20 (%)
54 (40.6)
11 (8.0)
HBeAg seroconversion* (%)
8 (11.3)
18 (26.1)
IgM anti-HBc*** (%)
Negativity
100 (76.9)
0
Positivity at 1:1000
21 (16.2)
5 (3.8)
Positivity at 1:10 000
9 (6.9)
126 (96.2)
HBV-DNA PCR quantifying
detection
Under the low limit of the
8 (6.2)
29 (22.1)
test*** (%)
122, 6.59 1.42 102, 4.53 1.23
Positivity, log10 copies/mL***
Compared with CHB-AF group: *P < 0.05; **P < 0.01; ***P < 0.001.
Including patients with a negative test result.
Test was not done in seven patients with ASL-HB and in three patients
with CHB-AF in the retrospective group.
anti-HBe, antibody to hepatitis B e antigen; IgM anti-HBc, immunoglobulin M antibody to hepatitis B core antigen; ASL-HB, acute self-limited
hepatitis B; CHB-AF, chronic hepatitis B with acute flare; HBeAg, hepatitis B e antigen; HBsAg, hepatitis B surface antigen; HBV, hepatitis B
virus; PCR, polymerase chain reaction; S/CO, ratio of optical density of
samples read at 450 nm to cut-off value.
more patients with ASL-HB than in those with CHB-AF (92.0% vs
59.4%, P < 0.001), with a much greater difference between the
two groups existing in patients with a low level of HBeAg (S/CO
<20) than in patients negative for HBeAg (42.7% and 13.5% vs
49.3% and 45.9%). In 131 ASL-HB patients, 126 (96.2%), five
(3.8%) and 0 were found positive for serum IgM anti-HBc in the
titer of 1:10 000, positive and negative in the titer of 1:1000,
respectively, whereas of 130 patients with CHB-AF, the numbers
were only nine (6.9%), 21 (16.2%) and 100 (76.9%), respectively.
In addition, no serum HBsAg was detected on admission in 14
(10.1%) patients with ASL-HB, which was not seen in any patients
in the CHB-AF group.
A significant difference was observed in serum HBV-DNA
levels between the two patient groups. Not only was an undetectable level of serum HBV-DNA found in more patients with
ASL-HB than in CHB-AF patients (22.1% vs 6.2%, P < 0.001),
but also the average concentration was lower in ASL-HB than in
CHB-AF patients among those with positive serum HBV-DNA
(4.53 vs 6.59 log10 copies/mL, P < 0.001).
overlapping values, were chosen. Table 4 shows differentially
diagnostic performances of each or different combinations of these
parameters calculated on the basis of 138 patients with ASL-HB
and on 133 with CHB-AF.
HBeAg with S/CO <20 (including negativity) and HBV-DNA
<105 copies/mL held a poorer sensitivity and a poorer specificity
than did 1:10 000 IgM anti-HBc (86.6%, 75.4% and 96.2%, vs
57.1%, 79.2% and 93.1%, respectively). A sensitivity of 1:10 000
IgM anti-HBc combining with AFP <5 URL, or HBeAg with
S/CO <20, or HBV-DNA <105 copies/mL, was 100.0%, 100.0%
and 98.9%, respectively; specificity was 89.4%, 90.7% and 98.9%,
respectively; a positive predictive value was 96.2%, 95.8% and
98.9%, respectively; a negative predictive value was 100.0%,
100.0% and 99.0%, respectively. A combination of IgM anti-HBc,
HBV-DNA, and HBeAg had a positive predictive value of 98.9%
and a negative predictive value of 100.0%, similar to those (98.9%
and 99.0%, respectively) of a combination of IgM anti-HBc and
HBV-DNA. Adding AFP to the combinations of IgM anti-HBc and
HBV-DNA or HBeAg could further heighten positive predictive
values. The positive predictive value and negative predictive value
of the combination of IgM anti-HBc, HBV-DNA and AFP were
both 100.0%.
Analysis of the causes of CHB
Of 192 patients studied, there were 54 patients who were classified
as having CHB because they remained HBsAg positive after the
onset of disease, except for 138 patients who were confirmed as
being ASL-HB. Does CHB evolve from acute hepatitis B or is it
actually an acute onset of unknown chronic HBV infection?
Forty-one patients were found negative and six positive for IgM
anti-HBc in a titer of 1:1000. According to the recognition that
negativity for, or a low level of, serum IgM anti-HBc can exclude
the possibility of AHB,3,5,13 these 47 patients were recognized as
having acute exacerbation of previously unrecognized HBV carriage. The remaining seven patients possessed positive IgM antiHBc in a titer of 1:10 000. Three patients were positive for HBeAg
with S/CO >20 and for HBV-DNA >107 copies/mL, and one with
the lowest level of HBV-DNA had a serum AFP level of
105.1 ng/mL (15 URL). The other two were negative for
HBeAg, one having serum AFP of 286 ng/mL and HBV-DNA of
2.46 106 copies/mL, with a typical image of chronic hepatitis by
ultrasonic examination and a few vascular spiders, congestive
palms, and the other having HBV-DNA of 5.37 106 copies/mL,
and serum AFP of 31.03 ng/mL, near 5 URL. According to our
diagnostic criteria, the probability of AHB in the preceding four
patients was ruled out and the diagnosis of CHB with a first
episode of acute hepatitis was made, and it was difficult to confirm
the diagnosis of the last patient, but a tendency for unrecognized
CHB existed. The remaining two patients had low levels of serum
HBeAg, simultaneously bearing low levels of serum HBV-DNA
and AFP, and were classified as having AHB developing into CHB.
Therefore, the chronicity rate of clinical acute hepatitis B in our
patients was 1.4% (2/140).
Discussion
Diagnostic power of laboratory parameters
According to the above analyses, four parameters, IgM anti-HBc,
HBeAg, HBV-DNA and AFP, all with great differences and little
Chronic HBV infection occurs in 8090% of infants who are
infected with HBV through vertical transmission from their
mothers or fathers, which is the most common mode of transmis-
Journal of Gastroenterology and Hepatology 23 (2008) 17281733 2008 The Authors
Journal compilation 2008 Journal of Gastroenterology and Hepatology Foundation and Blackwell Publishing Asia Pty Ltd
1731
Profiles and differential diagnosis of AHB
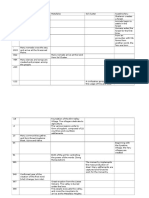
Table 4
Y Han et al.
Diagnostic performance of laboratory tests for ASL-HB
Laboratory tests
Sensitivity
Specificity
Accuracy
Positive
predictive
value
Negative
predictive
value
Positive IgM anti-HBc at 1:10 000
HBV-DNA <105 copies/mL
HBeAg S/CO <20
IgM anti-HBc at 1:10 000 plus AFP <5 URL
IgM anti-HBc at 1:10 000 plus HBeAg S/CO <20
IgM anti-HBc at 1:10 000 plus HBV-DNA <105 copies/mL
IgM anti-HBc at 1:10 000 plus HBV-DNA <105 copies/mL plus HBeAg S/CO <20
IgM anti-HBc at 1:10 000 plus HBeAg S/CO <20 plus AFP <5 URL
IgM anti-HBc at 1:10 000 plus HBV-DNA <105 copies/mL plus AFP <5 URL
96.2
75.4
86.6
100.0
100.0
98.9
100.0
100.0
100.0
93.1
79.2
57.1
89.4
90.7
99.0
97.9
89.5
100.0
94.6
77.0
66.8
97.1
97.0
99.0
99.3
98.2
100.0
93.3
78.4
63.8
96.2
95.8
98.9
98.9
98.3
100.0
96.0
75.7
75.0
100.0
100.0
99.0
100.0
100.0
100.0
Including HBeAg-negative patients.
AFP, alpha-fetoprotein; ASL-HB, acute self-limited hepatitis B; HBeAg, hepatitis B e antigen; HBV, hepatitis B virus; IgM anti-HBc, immunoglobulin
M antibody to hepatitis B core antigen; S/CO, ratio of optical density of samples read at 450 nm to cut-off value; URL, upper reference limit.
sion for HBV in China.14,15 Thus, we have been taught that AHB is
rare in China after HBV infection has prevailed for centuries. The
lifetime risk of HBV infection, as judged by the peak prevalence of
HBV markers in elderly people, is approximately 80% in China,
but the rate of chronic HBV carriage is only 8.511.1%,14 suggesting that a great majority of HBV-infected individuals have spontaneously cleared the HBV, particularly in adults. Taking this into
consideration, we paid special attention to the follow-up care of
adult patients with a first episode of HBV-related acute hepatitis
whose previous history of HBV infection had not been known.
During the follow-up period, most of them cleared HBV from their
serum and were confirmed as ASL-HB. Sequentially, we located
and retrospectively investigated the patients who were admitted
with signs, symptoms and biochemical tests suggestive of acute
hepatitis, and were diagnosed as CHB due to evidence of HBV
infection when they were discharged from our hospital from
January 2003 to March 2005. A prospective arm on similar patients was conducted simultaneously. As we suspected, sporadic
ASL-HB is not rare but common now in China, opposite to what
has generally been accepted. So ensues a practical problem of
distinguishing AHB from CHB-AF. Here, we first compared
ASL-HB patients with CHB-AF patients in relation to clinical,
biochemical, immunological and virological aspects, and then
sought the methods to discriminate between the two diseases.
Comparison of patients with ASL-HB and CHB-AF had shown
that ASL-HB patients were more symptomatic, had a more severe
necroinflammatory liver but a more functionally compensated
liver. This finding could be explained by the fact that clinically
acute hepatitis occurred in a healthy and injured liver, respectively,
in the two conditions. Unfortunately, none of these biochemical
parameters at initial presentation could differentiate between
patients with ASL-HB and CHB-AF, which is in keeping with
Kumar et al.s observation.7
The cause of elevated AFP in patients with non-tumor liver
disease is unclear. Our findings that the peak production of a great
majority of the two groups of patients with elevated AFP levels
was observed at early phase of the disease, when liver damage was
the severest, but not at the convalescent phase (data not shown),
when hepatocytic regeneration occurred, suggest that elevations of
serum AFP in acute and chronic liver diseases may not be due to
1732
subsequent hepatocyte regeneration induced by hepatic inflammation. The literature on the mechanism of serum AFP elevation in
AHB patients is not available at the present. Longitudinal studies
showed that elevations of serum AFP levels at baseline in CHB
patients confirmed by liver biopsy had been proven to be associated with a higher risk of decompensated cirrhosis, hepatocellular
carcinoma (HCC),16,17 implying that patients with elevated serum
AFP had more advanced liver disease than did those with normal
levels. Very high levels of serum AFP suggestive of the possibility
of HCC were occasionally found in patients with chronic HBV
infection, especially those with cirrhosis, but no occurrence of
HCC.18,19 In the setting of chronic hepatitis C, the mean serum
AFP value was significantly greater in patients with more marked
fibrosis.20 All these observations put forward the hypothesis that
marked fibrosis or cirrhosis, a state of significant altered hepatocyte architecture, may be the underlying cause of increased serum
AFP and, just at the presence of fibrosis or cirrhosis, hepatocyte
necroinflammation can trigger elevations of AFP. This can explain
why AFP elevations have frequently been found in CHB patients,
with remarkable AFP elevations being associated with exacerbations of the underlying liver disease,16,21 whereas normal AFP
levels are found in a great majority of patients with ASL-HB and
only low levels of AFP in a minority of them, although they had
more severe liver necroinflammation.
As shown by other researchers,7,10 ASL-HB patients had a
higher level of serum IgM anti-HBc, lower levels of serum HBVDNA, HBeAg and HBsAg than those with CHB-AF. These phenomena can be explained by a rapid clearance of serum HBVDNA as a result of a coordinated response of innate and adaptive,
humoral and cellular immune systems in AHB.15,22 The reason why
the proportion of patients with negative HBeAg in the two groups
is similar (49.3% vs 45.9%) is that some CHB patients are infected
with HBeAg-negative variants of HBV. The finding that a low level
of serum HBeAg was observed in more patients with ASL-HB
than in patients with CHB-AF suggests that a low HBeAg level is
more useful than negative HBeAg in the differential diagnosis
between ASL-HB and CHB-AF.
Very important differences in HBV-DNA, HBeAg and AFP, as
well as IgM anti-HBc, between the two groups have been observed
in our study. When used singly, the diagnostic power for ASL-HB
Journal of Gastroenterology and Hepatology 23 (2008) 17281733 2008 The Authors
Journal compilation 2008 Journal of Gastroenterology and Hepatology Foundation and Blackwell Publishing Asia Pty Ltd
Y Han et al.
of 1:10 000 IgM anti-HBc was comparable to what has been
reported,46 whereas that of HBV-DNA <105 copies/mL was poorer
than that of HBV-DNA <0.5 pg/mL (95.9% sensitivity and 86.6%
specificity) in Kumar et al.s study.7 The discrepancy between the
two studies may stem from incomparable quantitative HBV-DNA
measurement methods and cut-off values selected.
Diagnostic performance of combinations of laboratory tests for
ASL-HB has not been seen so far and we make an attempt. Among
combinations of two parameters, 1:10 000 IgM anti-HBc uniting
HBV-DNA <105 copies/mL had the best diagnostic performance,
with a positive predictive value of 98.9% and a negative predictive
value of 99.0% and, after adding AFP <5 URL to it, both values
amounted to 100.0%. Even so, AFP is not necessarily used in
diagnosing AHB because it has only a marginal improvement
in diagnostic power in test combinations, and is not a routine test
in acute hepatitis. Alternatively, when a differential diagnosis
cannot be made, a high level (>10 URL) of serum AFP may
be helpful in ruling out the probability of AHB, according to the
observation that only one of 47 patients ASL-HB had serum AFP
level >5 URL and no patient >10 URL.
Moreover, it has been a surprise finding that a family history of
chronic HBV infection was helpful in distinguishing between
ASL-HB and CHB-AF, because, in China, a family history of
chronic HBV infection usually brings CHB to mind. Our finding is
in accordance with Thakur et al.s study in which the chronic
HBV infection rate in first-degree relatives of CHB patients was
only 29%.23
In conclusion: (i) there are significant differences with respect
to clinical, biochemical, immunological and virological aspects
between ASL-HB and CHB-AF; (ii) a low HBeAg level is more
useful than negative HBeAg in differential diagnosis between
ASL-HB and CHB-AF; (iii) a combination serum IgM anti-HBc in
a titer of 1:10 000 with serum HBV-DNA <105 copies/mL and/or
HBeAg S/CO <20 could effectively distinguish ASL-HB from
CHB-AF in patients with a first episode of HBV-related acute
hepatitis; and (iv) in those with a high level of IgM anti-HBc,
serum AFP level >10 URL could rule out the probability of
ASL-HB.
References
1 Lok ASF, McMahon BJ. Chronic hepatitis B. Hepatology 2007; 45:
50739.
2 Dufour DR, Lott JA, Nolte FS, Gretch DR, Koff RS, Seeff LB.
Diagnosis and monitoring of hepatic injury. II. Recommendations for
use of laboratory tests in screening, diagnosis, and monitoring. Clin.
Chem. 2000; 46: 205068.
3 Decker RH. Diagnosis of acute and chronic hepatitis B. In:
Zuckerman AJ, Thomas HC, eds. Viral Hepatitis. Singapore:
Harcourt Asia, 2000; 20116.
4 Lemon SM, Gates NL, Simms TE, Bancroft WH. IgM antibody to
hepatitis B core antigen as a diagnostic parameter of acute infection
with hepatitis B virus. J. Infect. Dis. 1981; 143: 8039.
5 Paraevangelou G, Poumeliotou-Karayannis A, Tassopoulos N,
Stathopoulou P. Diagnostic value of anti-HBc IgM in high HBV
prevalence area. J. Med. Virol. 1984; 13: 3939.
Profiles and differential diagnosis of AHB
6 Govindarayan S, Ashcavai M, Chau KH, Nevalainen DE, Perters RL.
Evaluation of enzyme immunoassay for anti-HBc IgM in the
diagnosis of acute hepatitis B virus infection. Am. J. Clin. Pathol.
1984; 82: 3235.
7 Kumar M, Jain S, Sharma BC, Sarin SK. Differentiating acute
hepatitis B from the first episode of symptomatic exacerbation of
chronic hepatitis B. Dig. Dis. Sci. 2006; 51: 5949.
8 Tassopoulos NC, Papatheodoridis GV, Kalantzakis Y et al.
Differential diagnosis of acute HBsAg positive hepatitis using IgM
anti-HBc by a rapid, fully automated microparticle enzyme
immunoassay. J. Hepatol. 1997; 26: 1419.
9 Huang YW, Lin CL, Chen PJ, Lai MY, Kao JH, Chen DS. Higher
cut-off index value of immunoglobulin M antibody to hepatitis B
core antigen in Taiwanese patients with hepatitis B. J. Gastroenterol.
Hepatol. 2006; 21: 85962.
10 Rodella A, Galli C, Terlenghi L, Perandin F, Bonfanti C, Manca N.
Quantitative analysis of HBsAg, IgM anti-HBc and anti-HBc avidity
in acute and chronic hepatitis B. J. Clin. Virol. 2006; 37: 20612.
11 Dufour DR, Lott JA, Nolte FS, Gretch DR, Koff RS, Seeff LB.
Diagnosis and monitoring of hepatic injury. I. Performance
characteristics of laboratory tests. Clin. Chem. 2000; 46: 202749.
12 McMahon BJ, Alward WLM, Hall DB et al. Acute hepatitis B virus
infection: relation of age to the clinical expression of disease and
subsequent development of the carrier state. J. Infect. Dis. 1985;
151: 599603.
13 Kaganov BS, Nisevich NI, Uchaikin VF et al. Acute viral hepatitis B
in children: lack of chronicity. Lancet 1990; 336: 3745.
14 Liu X, Schinazi RF. Molecular and serum epidemiology of HBV and
HCV infection and the impact of antiviral agents in China. In:
Schinazi RF, Sommadossi JP, Rice CM, eds. Frontiers in Viral
Hepatitis. Amsterdam: Elsevier BV, 2003; 1533.
15 Hyams KC. Risks of chronicity following acute hepatitis B virus
infection: a review. Clin. Infect. Dis. 1995; 20: 9921000.
16 Di Bisceglie AM, Hoofnagle JH. Elevations in serum
alpha-fetoprotein levels in patients with chronic hepatitis B. Cancer
1989; 64: 211720.
17 Xu B, Hu D-C, Rosenberg DM et al. Chronic hepatitis B: a
long-term retrospective cohort study of disease progression in
Shanghai, China. J. Gastroenterol. Hepatol. 2003; 18: 134552.
18 Bae JS, Park SJ, Park KB et al. Acute exacerbation of hepatitis in
liver cirrhosis with very high levels of alpha-fetoprotein but no
occurrence of hepatocellular carcinoma. Korean J. Intern. Med.
2005; 20: 805.
19 Yao FY. Dramatic reduction of the alpha-fetoprotein level after
lamivudine treatment of patients with chronic hepatitis B virus
infection and cirrhosis. J. Clin. Gastroenterol. 2003; 36: 4402.
20 Goldstein NS, Blue DE, Hankin R et al. Serum alpha-fetoprotein
levels in patients with chronic hepatitis C. Relationships with
serum alanine aminotransferase values, histologic activity index,
and hepatocyte MIB-1 scores. Am. J. Clin. Pathol. 1999; 111:
81116.
21 Lok AS, Lai CL. alpha-Fetoprotein monitoring in Chinese patients
with chronic hepatitis B virus infection: role in the early detection of
hepatocellular carcinoma. Hepatology 1989; 9: 11015.
22 Chemello L, Mondelli M, Bortolotti F et al. Natural killer activity in
patients with acute viral hepatitis. Clin. Exp. Immunol. 1986; 64:
5964.
23 Thakur V, Guptan RC, Malhotra V, Basir SF, Sarin SK. Prevalence
of hepatitis B infection within family contacts of chronic liver
disease patientsdoes HBeAg positivity really matter? J. Assoc.
Physicians India 2002; 50: 138694.
Journal of Gastroenterology and Hepatology 23 (2008) 17281733 2008 The Authors
Journal compilation 2008 Journal of Gastroenterology and Hepatology Foundation and Blackwell Publishing Asia Pty Ltd
1733
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (894)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Coral of The MoonDocument33 pagesCoral of The MoonViolettaFlowerPas encore d'évaluation
- Timeline Ar TonelicoDocument43 pagesTimeline Ar TonelicoRaison D'etrePas encore d'évaluation
- 07 Eosinophilic MeningitisDocument37 pages07 Eosinophilic MeningitisMai ChanisaraPas encore d'évaluation
- survival the finalist (เน็ทน้อย) PDFDocument377 pagessurvival the finalist (เน็ทน้อย) PDFPiich Kwang100% (1)
- Clinical, Biochemical, Immunological and Virological Profiles Of, and Differential Diagnosis Between, Patients With Acute Hepatitis B and Chronic Hepatitis B With Acute FlareDocument6 pagesClinical, Biochemical, Immunological and Virological Profiles Of, and Differential Diagnosis Between, Patients With Acute Hepatitis B and Chronic Hepatitis B With Acute FlareRaison D'etrePas encore d'évaluation
- Cyanotic Heart LesionsDocument40 pagesCyanotic Heart LesionsRaison D'etrePas encore d'évaluation