Académique Documents
Professionnel Documents
Culture Documents
Treatment Modalities For Angle Fractures
Transféré par
ashajangamTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Treatment Modalities For Angle Fractures
Transféré par
ashajangamDroits d'auteur :
Formats disponibles
Int. J. Oral MaxilloJhc. Surg.
1999; 28:243~52
Printed flz Denmark. All rights reserved
Copyright 9 Munksgaard 1999
Intemadona]Joumal of
Oral8r
Maxill@cial Surgery
ISSN 090t-5027
Leading article
Treatment methods for
fractures of the mandibular
angle
E d w a r d Ellis III
Oral and Maxillofacial Surgery, The University
of Texas Southwestern Medical Center,
Dallas, Texas, USA
E. Ellis III. Treatment methods for fractures of the mandibular angle. Int. J. Oral
Maxillofac. Surg. 1999, 28." 243~52. 9 Munksgaard, 1999
Abstract. Fractures of the mandibular angle are plagued with the highest rate of
complication of all mandibular fractures. Over the past 10 years, various forms
of treatment for these fractures were performed on an indigent inner city
population. Treatment included: 1) closed reduction or intraoral open reduction
and non-rigid fixation; 2) extraoral open reduction and internal fixation with an
AO/ASIF reconstruction bone plate; 3) intraoral open reduction and internal
fixation using a solitary lag screw; 4) intraoral open reduction and internal
fixation using two 2.0 mm mini-dynamic compression plates; 5) intraoral open
reduction and internal fixation using two 2.4 mm mandibular dynamic
compression plates; 6) intraoral open reduction and internal fixation using two
non-compression miniplates; 7) intraoral open reduction and internal fixation
using a single non-compression miniplate; and 8) intraoral open reduction and
internal fixation using a single malleable non-compression miniplate. This paper
reviews the results of those modes of treatment when used for the same patient
population at one hospital. Results of treatment show that, in this patient
population, the use of either an extraoral open reduction and internal fixation
with the AO/ASIF reconstruction plate or intraoral open reduction and internal
fixation, using a single miniplate, are associated with the fewest complications.
Fractures of the mandibular angle represent the largest percentage of mandibular fractures in many studies. The
etiology of the injury has something to
do with the location of the mandible
that fractures. Fractures sustained in
altercations show a high incidence of
fractures of the angle of the mandible 33'4~176
The prevailing
thought is that a blow to the lateral
portion of the mandible causes a fracture at that point, and commonly a
fracture on the opposite body/symphysis region.
Why is the angle of the mandible
commonly associated with fractures?
There are several proposed reasons that
include: 1) the presence of third molars;
2) a thinner cross-sectional area than
the tooth-bearing region; and 3) bio-
mechanically the angle can be considered a "lever" area. Several authors
have implicated the presence of third
molars, especially impacted third molars, as a reason for mandibular fractures occurring in the region of the
angle. In fact, some have recommended
prophylactic removal of third molars to
eliminate their weakening effect in the
angle region, in hopes of preventing
fractures from occurring 1,2,39'61'64'68.
While this seems an extreme stance on
the issue, there is scientific evidence indicating that third molars do weaken
the angle of the jaw and are associated
with fractures more commonly than
when no tooth is present. For instance,
a study by REITZlK et al. s3 found monkey mandibles with unerupted third
molars fractured at 60% of the force re-
Key words: mandibular fracture; bone plates;
fracture fixation.
Accepted for publication 24 January 1999
quired when no tooth was present, Clinical investigations have shown that patients with third molars present are
more likely to sustain fractures of the
angle than when no tooth is present s6,7~ Further, the amount of space
occupied by the third molar was found
to directly relate to weakness in that region of the mandible 56,
One would logically expect fractures
to occur at points of greatest weakness
in a structure. One would also logically
expect that thinner cross-sectional areas
of a structure would be weaker than
those areas with greater cross-sectional
areas. A study by SHVBERT et al. 63 has
shown that the region of the mandibular angle is thinner than both the bone
of the body region located more anteriorly, and the bone of the ramus located
244
Ellis
more posteriorly. Thus, a given force
applied to the lateral aspect of the mandible might be expected to fracture at
the region with the smallest cross-sectional area the angle of the mandible.
Combine this with the fact that the
angle of the mandible is where there is
an abrupt change in shape from horizontal to vertical rami, which would imply that this region might be subjected
to more complex forces than a more linear geometric shape, and one can begin
to understand why fractures occur in
this location.
Fractures of the mandibular angle
represent an important clinical challenge because their treatment is plagued
with the highest postsurgical complication rate of all mandibular fractures 16,34,36,s9,72. Even traditional treatment methods have a high complication
rate in some patient populations49.
With the introduction and popularity
of plate and screw fixation over the past
30 years, a number of fixation methods
have been advocated for the treatment
of fractures occurring through the angle
of the mandible. Many of these techniques are seemingly disparate. For instance, the AO/ASIF originally felt that
plate and screw fixation should provide
sufficient rigidity to the fragments to
prevent interfragmentary mobility during active use of the mandible66,67.
LUItR42 similarly recommended large
bone plates, usually with compression,
fastened with bicortical bone screws to
provide such rigidity. Primary bone
union, which necessitates absolute immobility of fragments, is the goal of
treatment of mandibular fractures by
these surgeons.
In 1973, MICHELET et al. 45 reported
on the treatment of mandibular fractures using small, easily bendable noncompression bone plates, placed transorally, attached with monocortical
screws. The application of this technique was a seeming dichotomy to the
more widely accepted dictum of rigid
fixation, and sparked a revolution in the
treatment of facial fractures. CHAMPYet
al.8 12 performed several investigations
with a "miniplate" system to validate
the technique, in their experiments,
they determined the "ideal lines of osteosynthesis" in the mandible, or the
locations where bone plate fixation
should provide the most stable means
of fixation. For fractures of the mandibular angle, the most effective plate
location was found to be along the superior border of the mandible. Because
the bone plates were small and the
screws inserted monocortically, fixation
could be applied in this most mechanically advantageous area without damaging teeth. Unlike the AO/ASIF surgeons and LUHR, absolute immobilization of bone fragments and
primary bone union was deemed unnecessary. Clinical studies since have
proven the usefulness of this technique7,24,26,27,29,31,47,51,73
Questions about the degree of stability provided by these "mini-plates"
have become a point of contention
among surgeons. RAVEH et al. 52,
LUHR44 and AO/ASIF advocates 4 do
not feel that the plates offer adequate
stabilization of the fracture to eliminate
the need for intermaxillary fixation.
Other surgeons who routinely used the
more rigid AO/ASIF plates began to relent and use miniplates26'27.
Unfortunately, whether or not one
method is "superior" to another is difficult to determine. Studies in the literature vary widely in the rates of complication reported when treating fractures
of the angle. For instance, LUHR &
HAUSMANN43 report a 0.9% rate of complications in 352 patients treated by
compression plates for fractures of the
angle, whereas ELLIS & SINN22 report a
32% rate of complication in 65 patients
treated with compression plates for
angle fractures. IIZUKA & L1NDQVIST35
reported a 6.6% rate of infection and a
14% rate of malocclusion for 121 fractures of the angle. Analysis in that study
showed that complications were most related to the use of compression and two
points of fixation.
How can rates of complication be so
varied? There are several problems when
one attempts to compare treatment
methods for fractures of the mandibular
angle. The first difficulty is that there are
few studies that restrict their focus to
fractures of the mandibular angle. Most
studies evaluating results for mandibular
fractures include fractures in all regions
of the mandible, making it difficult to determine the actual rate of complication
for angle fractures. Another problem is
that treatment in one country may be
very different from treatment in another.
For instance, patients treated for mandibular fractures in some of the European countries may spend 7 21 days in
hospital after surgery. In the United
States, they are usually discharged the
same or the next day. It is therefore
doubtful that the quality and quantity of
postsurgical care is similar. Studies also
vary in the etiology of the injury. Studies
from the United States generally have
samples drawn from large inner-city hospitals where most of the injuries result
from interpersonal violence, i n many
European, Middle Eastern and Asian
studies, motor vehicle-related injuries
are more common. Hand in hand with
the cause of the injury is the socioeconOmic status of the patients. Those injured by interpersonal violence and
treated in major inner-city hospitals in
the United States tend to be poor, with
poor oral hygiene and a poor state of
dentition. Those patients whose fractures are sustained in motor vehicle accidents, sports or in bicycle accidents tend
to be a higher socioeconomic group and
are more concerned with oral and general health. There are also great differences in the literature in what constitutes
a complication. In countries where routing removal of fixation devices is common, soft tissue dehiscence with plate exposure may not be counted as a complication because the plate will be removed
anyway. In the United States, where
plate removal is not routine, any unplanned intervention should be considered a complication. Another major
variable is in the number of surgeons involved in the operative intervention. Because of these factors and a host of
others, it becomes difficult to accurately
assess treatment results with different
fixation techniques.
The following presents the experience
of one faculty surgeon treating fractures
of the mandibular angle at one institution, with a consistent patient population, using eight different techniques.
While a number of residents were involved in the surgeries, the same faculty
member (E.E.) was present for over
95% of the actual open part of the operations.
Methods
Over the past 10 years, various methods of
treatment for fractures of the angle of the
mandible have been studied at Parkland
Memorial Hospital in Dallas, Texas. The continuing quest for a simple but effective technique drove us to use different modes of treatment and to examine their efficacy. The following study relates our experience with
several accepted methods for treating fractures of the mandibular angle19 25,49,51. The
first two methods, closed reduction with or
without non-rigid fixation, and the use of the
AO/ASIF reconstruction plate, were retrospective studies. All others were prospectivein
their data collection.With the exception of the
extraoral approach used in those patients
Treatment o f mandibular angle.fractures
treated with the AO/ASIF reconstruction
plate, all techniques were intraoral, with the
exception of transfacial trocar instrumentation.
The population in these studies was largely
inner-city indigent patients with poor dentitions and poor oral hygiene. The majority
of the cases occurred in males (approximately 85%). The racial/ethnic breakdown was
approximately 50% African-Americans, 30%
Non-Hispanic Caucasians, and 20% Hispanic. The average age of the patients was approximately 27 years, with the vast majority
in the third and fourth decades of life. Approximately half of the angle fractures were
isolated mandibular fractures; the other half
having a contralateral fracture of the mandibular condyle, angle, body or symphysis.
All patients had arch-bars attached to the
dentition during surgery but none of the patients reported below were placed into postsurgical intermaxillary fixation (IMF) unless
otherwise noted. However, the arch-bars were
left in place until the patient was fnnctionally
rehabilitated with an interincisal opening of
greater than 40 ram. This usually was from 4
to 8 weeks post-surgery. All other fractures
of the mandible (with the possible exception
of subcondylar) were treated with plate and/
or screw fixation, allowing immediate mandibular function. Even those patients who
had closed treatment of condylar fractures
were allowed immediate mobilization of the
mandible, but may have had elastics applied
to the dentition to "guide" them into proper
occlusion. The vast majority of fractures in
this patient population were sustained in
altercations/assaults (approximately
85
95%). The time between injury and presentation for treatment ranged from a few hours
to several weeks, with an average of approximately 2.5 days. The average time between
injury and surgery was just over 3 days.
The data that were collected in each study
included: 1) age, 2) sex, 3) race, 4) number of
fractures per patient, 5) etiology, 6) associated
maxillofacial or other system trauma, 7) type
of fracture, i.e. comminuted versus linear, oblique versus straight, 8) concomitant mandibular fractures, 9) presence of a tooth in the
line of fracture, 10) extraction of tooth in line
of fracture, 11) complications during surgery,
12) posts urgical occlusal relationship, and 13)
complications, which were defined as a need
for further surgical intervention. Only patients with a m i n i m u m follow-up of six weeks
were included. Approximately 80% of cases
had a tooth associated with the fracture in the
angle, and these were removed during surgery
in 60 80% of cases.
Closed reduction or intraoral open
reduction and non-rigid internal fixation
With the implementation of rigid forms of
internal fixation, closed reduction or non-rigid internal fixation methods have become
less fashionable. However, when assessing
treatment results of new techniques, it is important to have a group for comparison. The
245
Fig. 1. Immediate postoperative radiograph showing angle fracture treated with transosseous
wire fixation and intermaxillary fixation. Wire was inserted through the buccal cortex of the
extraction socket.
"gold standard"
closed reduction or open
reduction using non-rigid fixation has been
used for centuries and constitutes such a
group. A retrospective study was performed
to gain an appreciation for the complication
rate of traditional treatment of angle fractures in our patient population 49.
The records of patients treated by non-rigid means of fixation for mandibular angle
fractures in a 3-year period were evaluated
retrospectively. Treatment of the fractures
was by closed reduction and/or open reduction with non-rigid means of interosseous
fixation such as transosseous wires, circummandibular wires or small positional bone
plates (Fig. 1). Postsurgical I M F was prescribed for six weeks in all patients.
During the 3-year period, 96 patients with
99 fractures through the mandibular angle
(three were bilateral) had charts available
with sufficient information for inclusion in
this studY. Of the 99 fractures, 59 were
treated with closed reduction (59%), 34 with
open reduction and placement of a transosseous wire (34"/0), five with open reduction
and a positional bone plate, and one fracture
was treated by closed reduction with the addition of a circummandibular wire (1%). All
patients were placed into postsurgical I M F
for an average of 40 days (range 20 -80 days).
Follow-up ranged from 21 252 days with an
average of 75 days.
Complications developed in 17 fractures
(17%), of which there were 13 with infections
and four cases where infection was combined
with malunion and malocclusion. There were
no cases of non-union. The time between initial presentation and surgery in these patients
was similar to the overall group of patients.
All patients underwent incision and drainage
procedures for their infections. Nine patients
were hospitalized at least once for their infection and/or malocclusion/malunion. During
the incision and drainage procedures, four
patients underwent removal of osteosynthesis; two had teeth in the line of fracture extracted; three patients whose initial treatment
was closed reduction had transosseous wires
placed to control the proximal segment; one
patient required osteotomy to correct malocclusion. Two patients required a second admission; one for incision and drainage, the
other for an osteotomy.
The results of this study showed that mandibular angle fractures in this patient population were associated with a high incidence of
postsurgical complications, even when traditional methods of treatment were employed.
Extraoral open reduction and internal
fixation using the AO/ASIF reconstruction
plate
The AO reconstruction bone plate is a reinforced plate that is thicker and stronger
than the standard AO/ASIF compression
bone plate. It comes in various lengths and
the plate is three-dimensionally bendable,
allowing accurate contouring to the surface
of the mandible. The use of three screws on
each side of the fracture with this bone pIate
is claimed to provide adequate neutralization
of functional forces in the absence of coinpression 6~ it is useful in areas of comminution, bone loss or obliquity where one cannot use standard compression bone plates.
The records of all patients with unilateral
fractures of the mandibular angle treated
with a reconstruction bone plate over a 3year period were collected. The technique for
application of the plate has been published
elsewhere and consisted of an extraoral approach in most instances (Fig. 2) 21.
The records of fifty-two patients with unilateral angle fractures treated in the 3-year
period, who had adequate follow-up information in their chart, were available for review. The fractures were categorized as being
comminuted in 31 cases, oblique in 12 and
simple linear fractures in 9. Following application of the bone plate,' all fractures appeared to be well reduced and stable. All
dentulous patients had a reproducible occlusion in the operating room. Four patients
had pre-existent infections of the fracture
246
El/is
and irrigation drains were placed during
surgery in these patients. No other patient
had drainage of the wound. Postoperative
radiographs taken within the first two days
showed excellent reduction in aII cases. There
was no radiographic evidence of damage to
the inferior alveolar neurovascuIar structures
from placement of the fixation hardware. The
occlusal relationships were judged as normal
in all but four of the dentulous patients at
one week following surgery. These four patients had slight occlusal irregularities that
required two to three weeks of elastic traction
therapy. All four of these patients had concomitant fractures of the mandible in the
tooth-bearing area making it difficult to determine which fracture(s) were not perfectly
reduced.
Follow-up ranged from 9 to 104 weeks
with a mean of 18 weeks. All dentulous patients had what was thought to be the normal occlusal relationship for that individual
at longest follow-up. Four fractures (7.5%)
required further surgical intervention for
postsurgical infections. These patients developed acute infections within the first three
postsurgical weeks that were refractory to
antimicrobial treatment. These patients required hospitalization for extraoral incision
and drainage, irrigation through drains, and
intravenous "antibiotics". One patient re-
quired plate removal to completely clear the
infection.
Lag screws for mandibular angle fractures
In 1981, NIEDERDELLMANNet al. 46 described
a method of internal fixation of mandibular
angle fractures using a single lag screw. We
began to use the lag screw technique in 1988
and found it to be an extremely rapid and
simple method for treating fractures of the
mandibular angle. The technique for placing
the lag screw has been described in previous
publications (Fig. 3) 19,25.
Eighty-eight patients that were treated by
open reduction and internal fixation of angle
fractures by the lag screw technique were included in this study. Intraoperatively, reductions were judged as excellent in all patients.
However, 17 were noted to be unstable to aggressive bimanual manipulation of the mandible. Supplemental methods of fixation were
applied in these cases. In three patients, a 2.0
mm compression bone plate was applied at
the inferior border. In the remaining 14 patients, postoperative I M F was used for varying periods (3-8 weeks). Follow-up ranged
from 6 to 167 weeks, with a mean of 22
weeks.
Immediate postoperative radiographic
evaluation showed excellent reduction in
every patient except one whose mandibular
ramus was slightly flared laterally on the submentovertex view. No treatment was necessary, as the facial form was minimally altered.
Seven patients were found to have very minor
occlusaI discrepancies in the first two postoperative weeks. These were treated satisfactory with 3M weeks of intermaxillary elastics. No other postsurgical malocclusion resulted in any patient. One patient had
radiographic evidence of probable impalement of the mandibular canal by the screw.
Eleven patients developed minor postsurgical
soft tissue infections/bone exposures within
the first several weeks (no cases of osteomyelitis occurred). Six resolved on oral antimicrobial treatment without any further intervention. Five patients (13%) required
further intervention, including removal of the
screws and small sequestra. One patient also
had extraction of a terminal molar that was
thought to be nonvital. Another patient developed non-union and was subsequently
bone-grafted.
Intraoral open reduction and internal
fixation using two 2.0 mm mini-dynamic
compression plates
One AO/ASIF method to neutralize the functional forces of an angle fracture is by restor-
Fig. 2. Immediate postoperative radiograph showing infected angle
fracture treated with AO reconstruction bone plate. Plate was placed
through an extraoral approach. Penrose drain that was inserted during surgery to help resolve infection can be seen. Drains were only
placed if fractures were infected.
Fig. 4. Immediate postoperative radiograph showing angle fracture
treated with two 2.0 mm dynamic compression plates.
Fig. 3. Immediate postoperative radiograph showing angle fracture
treated with solitary lag screw.
Fig. 5. Immediate postoperative radiograph showing angle fracture
treated with two AO/ASIF 2.4 mm compression plates designed for
use in mandible.
Treatment o f mandibular angle fractures
Fig. 6. Immediate postoperative radiograph showing angle fracture
treated with two non-compression miniplates.
ing the tension and compression trajectories
in the mandible 67. The recommended method
to restore these trajectories in fractures of the
mandibular angle is by the application of two
bone plates; one at the superior and one at
the inferior border of the buccal cortex. Traditionally, the plate at the superior border
was a small compression plate secured with
monocortical screws, whereas the one at the
inferior border was a large compression
plate, using bicortical screws. The application of these two bone plates is not difficult
through an extraoral approach. However,
placement of these plates via an intraoral approach is more demanding due to decreased
visibility, making adaptation of the bone
plates difficult. Because of the difficulties encountered in adapting and securing the larger
bone plates, the implementation of two 2.0
mm mini-dynamic compression plates was
undertaken in a sample of patients (Fig. 4) 2~
Thirty consecutive patients with 31 fractures of the mandibular angle that were
amenable to compression plate osteosynthesis were treated by open reduction and internal fixation using two mini-dynamic compression plates placed through a transoral incision with transbuccal trocar instrumentation. Nine fractures (29%) experienced
complications requiring secondary surgical
intervention. Three were early infections requiring incision and drainage, removal of the
plates and postoperative IME One was a
non-union with malocclusion requiring application of a more rigid bone plate. Five
fractures developed late chronic swelling and
low-grade infection requiring plate removal.
Osseous union had occurred in these cases
and no postoperative IMF was necessary.
Intraoral open reduction and internal
fixation using two 2.4 mm mandibular
dynamic compression plates
Because of the high rate of postsurgical complications in patients treated with two 2.0
mm mini-dynamic compression plates, it was
decided to study the standard AO/ASIF technique for treating fractures of the mandibular angle by the application of two com-
247
Fig. 7. Immediate postoperative radiograph showing angle fracture
treated with single non-compression miniplate according to the principles of CHAMPY et al) 2.
pression bone plates specifically designed for
the mandible. The tension band dynamic
compression plate employed 2.4 mm screws
that were applied monocortically in locations
where bicortical engagement would damage
normal anatomic structures, such as over
tooth roots. The stabilization plate was a
larger compression bone plate using 2.4 mm
bone screws. Additionally, postsurgical suction drainage was used in all cases.
Sixty-five consecutive patients with 65
fractures of the mandibular angle were
treated by open reduction and internal fixation using two dynamic compression plates
placed through a transoral incision with
transbuccal trocar instrumentation and 2.4
mm screws (Fig. 5) 22. Overall, 21 fractures
(32%) experienced infections requiring secondary surgical intervention. Of the 21 fractures which required plate removal, nine fractures were healed and required no further
treatment; 12 had no firm bony union and
required postsurgical IME Only one case resulted in a malunion with resulting malocclusion.
Intraoral open reduction and internal
fixation using two noncompression
miniplates
The AO/ASIF recommendation for application of two compression bone plates for
angle fractures was found to result in very
high rates of complication in our patient
population 2~
Because large bony sequestra were frequently encountered in these
patients, we thought that a reason for the
high rate of postoperative infection was devi-
talization of bone resulting from the use of
compression plates. The hypothesis was put
forward that eliminating the use of compression might improve treatment results.
The next series of patients with fractures of
the mandibular angle were, therefore, treated
with two 2.0 mm non-compression miniplates (Fig. 6). The superior bone plate was
applied monocortically, the inferior bone
plate bicortically. The technique for application of the two bone plates has been published elsewhere23.
Sixty-seven consecutive patients with 69
fractures of the mandibular angle were
treated by open reduction and internal fixation using two non-compression miniplates
placed through a transoral incision with
transbuccal trocar instrumentation and 2.0
mm self-threading screws. Overall, 19 fractures (28%) experienced complications requiring secondary surgical intervention.
Most of the complications were postoperative infections requiring surgical drainage
(n=lT) and subsequent plate removal (rl=
16). Of the 17 infected fractures, 11 were
healed at the time of plate removal and required no further treatment. Five were still
mobile and required a period of I M F for
healing. One of the fractures did not heal and
required bone grafting.
Intraoral open reduction and internal
fixation using one non-compression
miniplate
Because of the high rates of complication resulting when two bone plates were placed, it
was decided to attempt the use of a single
Table 1. Comparison of 2.0 mm and 1.3 mm miniplates*
Thickness (mm)
In-plane stiffness (N-m 2)
Out-of-plane stiffness (N-m 2)
In-plane bending strength (N-m 2)
Out-of-plane bending strength (N-m 2)
* Provided by Synthes USA, Paoli, PA,USA
2.0 mm plate
1.3 mm plate
0.9
0.007
0.158
0.14
0.93
0.5
0.001
0.029
0.04
0.40
248
Ellis
Fig. 8. Photograph of standard 2.0 m m miniplate and 1.3 m m miniplate used in this investigation (A). 1.3 m m plate is extremely thin
and malleable as shown in this photograph (B).
miniplate according to the principles of
CHAMPu et al. 12 (Fig. 7). Eighty-one consecutive dentate patients with non-comminuted
fractures of the mandibular angle were
treated by intraoral open reduction and
internal fixation using a single four-hole
miniplate and monocortical screws in a twoyear period23i Following application of the
bone plate, all fractures appeared to be well
reduced and stable. Postoperative radiographs taken within the first two days showed
excellent reduction in all cases except four,
where a 2~4 m m gap was noted at the inferior border. In spite of this finding on
radiographs, immediate occlusal relationships were judged as normal in all but one of
these patients, who had an slight posterior
open bite on the side of the fracture, and responded to light elastic traction for 10 days.
Besides this case, two other patients had
slight malocclusions that responded to the
wearing of elastics for one or two weeks. At
the time of arch-bar removal, occlusal relationships were judged as n o r m a l in all
cases.
Overall, 13 angle fractures (16%) experienced complications requiring secondary surgical intervention. Most of the complications
( n = l l ) , however, were minor and could be
treated in the outpatient setting. Most commonly, intraoral incision and drainage and
later removal of the bone plate were required.
All patients with minor complications had
bony union. Only two complications required hospitalization for intravenous antimicrobial treatment and further surgery. One
of these patients had a fibrous union, requiring a bone graft.
Intraoral open reduction and internal
fixation using one malleable noncompression miniplate
The use of a single miniplate for fractures of
the angle of the mandible was a simple, reliable technique with a relatively small number of major complications. However, the
question "how m u c h fixation is adequate?"
was still not known. LoDD~ 13 has reduced the
volume of the original CHAMPY miniplate by
half, making them much more malleable, and
has not noted any increase in complications
when used for mandibular fractures. How
much reduction in material is tolerable? The
purpose of this last investigation was to prospectively evaluate the use of a thin, malleable miniplate (Synthes Maxillofacial, Paoli,
PA, USA) that employs 1.3 m m screws for
stabilization of fractures of the mandibular
angle. This plate was not designed for use in
the mandible, but was designed for use in the
non-load bearing regions of the midface
(Table 1)(Fig. 8). Patients had a seven-hole
strip of the plate secured across the fracture
Fig. 9. Immediate postoperative radiograph showing angle fracture treated with single 1.3 m m
non-compression plate.
using three monocortical strews on each side
of the fracture. Because of the thinness and
malleability of the plates, it was unnecessary
to bend the bone plates, allowing the screws
to simply coapt the plates to the bone upon
tightening. No transbuccal trocar was necessary for instrumentation. All screws were 5
m m in length.
Forty-six consecutive patients with 51
fractures of the angle of the mandible were
treated by the above method (five were bilateral) in a 1.5-year period (Fig. 9) St. Following
application of the bone plate, all fractures
appeared to be well reduced and stable. Postoperative radiographs taken within the first
two days showed excellent reduction in all
cases. Immediate occlusal relationships were
judged as normal in all but one patient,
whose mandible was shifted to the contralateral side in association with moderate
swelling of the right submandibular and lateral pharyngeal spaces due to infection of
these spaces present prior to surgery. This resolved with the resolution of infection and
the use of light elastics for 14 days. At the
time of arch-bar removal, one patient was
judged to have a malocclusion that was attributed to malunion at a fracture site other
than the angle. All other occlusal relationships were judged normal.
Seven patients (13.7%) developed complications from their angle fracture postoperatively, only four (8.7%) required further surgical intervention. All complications were
considered minor and consisted of plate fracture, local infection, or both. Three of the
seven patients (42.9%) had asymptomatic
fracture of the plate diagnosed on radiographs, however there was bony union of the
fracture and no intervention was required.
Two patients (28.6%) had fracture of the
plate with clinical mobility of the fracture
and were placed into I M F for a period of
6 weeks. One of these patients subsequently
developed a localized infection of a devitalized tooth in the line of fracture and was
treated with oral antimicrobial drugs and extraction of the offending tooth. One patient
(14.3%) developed an isolated infection associated with a nonvital tooth that was
Treatment of mandibular angle.fi'actures
249
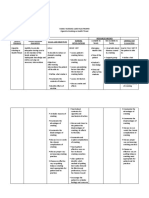
Table 2. Treatment for angle fractures (Parkland Memorial Hospital)
Treatment
Study Reference
Non-rigid fixation
AO reconstruction plate (2.7 mm)
Solitary lag screw
Two mini-dynamic compression plates (2.0 mm)
Two mandibular dynamic compression plates (2.4 ram)
Two non-compression miniplates (2.0 mm)
One non-compression miniplate (2.0 ram)
One malleable non-compr miniplate (1.3 mm)
PASSEI et al., 199349
ELLIS, 199321
ELLIS & GHALI,199119
ELLIS & KARAS,19922o
ELLIS& SINN, 199322
E>LIS & WALrCER,199423
ELLIS& WALKER,199624
POTTER& ELLIS, 199951
Sample (no. of angles)
Major Complication~
99
52
88
30
65
67
81
51
17%
7.5%
13%
13%
32%
23%
2.5%
0%
~ Major complication refers to the necessity of hospitalization to treat complication
treated by intraoral incision and drainage,
extraction of the tooth, and oral "antibiotics" without plate removal. One patient
(14.3%) developed an isolated infection associated with loosening of the. plates several
weeks after completing rehabilitation, and
was treated with oral "antibiotics" and removal of the plate under local anesthesia. No
patient developed major complications that
required hospitalization or intravenous antimicrobial therapy.
Discussion
In our patient population, treatment of
angle fractures with even traditional
methods closed reduction and/or nonrigid fixation produced a high rate of
complication (17%) 49. This might surprise those surgeons from countries
where fractures occur in a higher socioeconomic group of patients. However,
the association of poor oral hygiene,
poor dentition, substance abuse and a
variety of other factors may predispose
this particular sample of patients to
postsurgical complications48.
The most useful techniques in this
patient population were the use of
either an extraoral open reduction and
internal fixation with the AO/ASIF reconstruction plate, or intraoral open reduction and internal fixation using a
single miniplate (Table 2). The use of
the reconstruction bone plate was
found to result in few complications in
a study of angle fractures by IIZUKA&
LINDQVIST35. However, the application
of this plate is much easier through an
extraoral approach that can create its
own set of complications. Obviously, we
currently employ the latter approach
with a 2.0 mm plating system for the
vast majority of cases. Every attempt
we made at using a two-plate technique
via a transoral approach was fraught
with high rates of sequestra formation,
infection and need for subsequent
surgery. We no longer recommend an
intraoral two-plate technique.
At the beginning of these investigations, we never would have considered using a single miniplate to adequately stabilize a fracture of the angle
of the mandible without supplemental
IME Ten years ago, indoctrinated by
the AO/ASIF teaching that absolute rigid fixation was necessary, stable
methods were deemed necessary and
were used in this patient population.
Reconstruction plates, lag screws, and
two-plate systems were implemented
with the thought that they were absolutely stable methods. However, other
than the reconstruction plate, the intraoral techniques of stable fixation proved
either unstable in a certain percentage
of cases (solitary lag screw) or fraught
with high rates of major postsurgical
complications (two plates).
The results of these consecutive
series of clinical investigations performed in our hospital on a similar patient population indicate that, contrary
to popular beliefs, up to a point, the incidence of major complications after
fractures of the mandibular angle are
inversely proportional to the rigidity of
the fixation applied. Whenever two
points of fixation were used for fractures of the angle, the complication rate
was much higher than when one point
of fixation was applied. That is not to
say that using a single miniplate does
not result in complications. However,
the vast majority of problems that arose
in patients treated by a single miniplate,
such as wound dehiscence, wound infections, plate exposure etc., were easily
treated in the outpatient clinic under local anesthesia. Even removal of the
bone plate after healing of the fracture,
when necessary, is a simple procedure in
the outpatient setting. However, when a
second plate was applied at the inferior
border, the complications tended to be
more severe, with large areas of nonvital
bone, sequestra formation and need for
plate removal, which were difficult to
treat in the outpatient setting. If one defines a complication as an unplanned
intervention, the two-plate techniques
have a higher complication rate than
single plate techniques. However, when
one defines a major complication as one
that requires hospitalization to treat the
problem, the difference between treatment techniques becomes much more
clear and dramatic in incidence (see
Table 2).
The finding that a single minipiate
outperforms two plates and other more
stable forms of fixation defies logic, because conventional wisdom would indicate that more stable fixation should
provide fewer complications. However,
our experience has been the opposite.
The use of a single miniplate was associated with much fewer complications
than if two plates were used, irrespective
of whether the two plates were compression or non-compression plates.
This seeming dichotomy highlights the
limitations of relying on the results of
biomechanical bench testing for clinical
treatment recommendations. All biomechanical tests performed to date indicate that two plates are more stable
than one 14,15,18,2a'38,57,58,62. Based upon
these biomechanical studies and clinical
results, some investigators have advocated the use of two miniplates for fractures of the mandibular angle 14,15,41,71
LEvY et al. 41 compared a small sample
of patients who had fractures of the
angle treated with either one or two
miniplates without postsurgical IME
There were no complications in the 18
patients who had double miniplates,
but two complications in the ten patients (20%) who had a single miniplate.
Interestingly, another sample of 14 patients with two miniplates plus postsurgical I M F had a greater rate of complication (7.1%) than when no IMF was
used.
Our clinical experience is exactly the
opposite - a single miniplate worked
250
Ellis
much better than double plating systems. SHIERLE et al. 58 compared a single
miniplate to the use of two and found
no significant difference in results. The
results of our studies and the one by
SCHIRLE et al. 58 indicate that biomechanics are only one factor to be
considered when treating fractures.
There are many others that may be
more important. Perhaps improved
maintenance of the blood supply to the
bone because of limited dissection is
one such factor s 7,17,32. We, therefore,
agree with EWERS & HARLE 26'27 who
questioned the need for absolute rigidity for treatment of fractures. F r o m the
foregoing, it is obvious that fractures of
the mandibular angle do not require the
amount of stability as determined in
biomechanical tests. This should not be
surprising in light of bite force studies
by GERLACH et al. 3~ and TATE et al. 69
which showed that bite forces are subnormal for many weeks after fracture of
the mandible.
W h a t has yet to be determined is
exactly what are the requirements for
fixation of angle fractures. Based upon
the results of using a malleable 1.3 m m
plating system, this plate should not be
routinely used for such fractures because some fractured during function.
However, the fact that most did not
fracture indicates that the 2.0 m m miniplates are probably over-engineered for
this task. Perhaps a thinned down version of the 2.0 mm miniplate system
will prove even simpler to apply and adequately stable without plate fracture.
Another alternative might be to thicken
the 1.3 m m plate. These results also indicate that biodegradable fixation systems, which do not have the same
strength as metallic plates of the same
dimension, may provide adequate fixation in this region.
There have been studies on the treatment of fractures of the mandible that
have shown that operator experience is
an important factor in treatment results 3'34'37. There is no question that experienced surgeons can treat injuries
faster and perhaps with less surgical
trauma that those who are less experienced. Because the techniques that
proved most beneficial were those completed latest in this 10-year experience,
one might argue that the improved results are not due to treatment methods
but instead due to operator experience,
which one would presume to increase
over time. There is one factor that refutes this supposition, however. A var-
iety of residents were involved with the
operative procedures over the 10-year
pcriod. The experience level of the residents was similar because they rotated
to the treating hospital for the same
duration during their training programs. The only individual present over
the entire 10 years was the faculty surgeon, who merely directed and assisted
during the surgery. At least one other
study has also demonstrated that single
plates perform as well as when two are
used 58.
A more important consideration
about operator experience, however, is
that it takes much less experience to become adept at using a single miniplate
than the other techniques. Application
of a single miniplate takes only a few
minutes and can be taught very quickly
to a trainee. Placement of the second
plate at the inferior border is a more
difficult task and requires more experience to become facile. Placement of a
solitary lag screw is also technique sensitive. Fortunately, the technique that
offers the best results is also that which
is the simplest to learn.
The use of a single miniplate was not
in keeping with the original A O / A S I F
principles. Historically, the four AO/
A S I F principles for treating skeletal
fractures were: 1) anatomic reduction;
2) rigid fixation; 3) atraumatic surgical
technique; and 4) immediate active
function, in 1994, the A O / A S I E for the
first time in its history, changed the second principle to "functionally stable
fixation", rather than rigid fixation.
This change arose out of orthopedic
surgery, where intramedullary nails and
other less "rigid" forms of fixation were
proven to be "functionally" stable. The
ability of a single miniplate applied at
the superior border of the mandible to
"neutralize" functional forces and allow
immediate active mobility is finally recognized by the A O / A S I F as a reliable
means of providing functional stability
of the fracture.
The above relates the experience of
one hospital, with one patient population, treated by a large group of residents with one faculty member.
Whether or not the results are repeatable at other institutions is unknown.
Scientifically, the question about which
technique offers the best result will
require a randomized
prospective
study. This type of a study will allow
factors such as operator experience,
patient population and the multitude
of other uncontrolled factors to be less
likely to affect the outcome. Such a
study has not yet been performed but
is currently underway in the United
States.
References
1. ALLING CC. Mandibular fractures. In:
ALLINa CC, OSBORNDB, eds.: Maxillofacial trauma. Philadelphia: Lea & Febiger, 1988:238 86.
2. ALL1NGCC, ALLINGRD. Indications for
management of impacted teeth. In: ALLING CC, HELFRICKJE ALLING RE), eds.:
Impacted teeth. Philadelphia: Saunders,
1993:46 64.
3. ASSAEL L. Evaluation of rigid internal
fixation of mandible fractures performed
in the teaching laboratory. J Oral MaxilIofac Surg 1993: 51:1315 9.
4. B~crd~R R. Stable compression plate fixation of mandibular fractures. Br J Oral
Surg 1974: 12: 13--23.
5. BRADLEYJC. A radiological investigation
into the age changes of the inferior dental
artery. Br J Oral Surg 1975: 14:82 90.
6. BRADLEYJC. The clinical significance of
age changes in the vascular supply to the
mandible. Int J Oral Surg 1981:10 (Suppl
1): 71-6.
7. CAWOODJI. Small plate osteosynthesis of
mandibular fractures. Br J Oral Maxillofac Snrg 1985: 23:77 91.
8. CHAMPY M, WILK A, SCHNEBELEN JM.
Die Behandlung der Mandibularfrakturen mittels Ost6osynth6se ohne intermaxillfire Ruhigstellung nach der Technik von
Michelet. Dtsch Zahn Mund Kieferheilk
1975: 63: 33942.
9. CHAMPY M, LODDIdJR JAEGER JH, et al.
Ost6osynth6ses mandibulaires selon la
technique de Michelet. I. Bases biom6chaniques. Rev Stomat 1976: 77:569
76.
10. CHAMPYM, LODDEJR JAEGERJH, et al.
Ost6osynth6ses mandibulaires selon la
technique de Michelet. II. Presentation
d'un nouveau mat6riel rcsultats. Rev
Stomat 1976: 77: 577-82.
11. CtIAMPY M, CODDle.JR Etude des contraintes dans la mandibule fracturee chez
l'homme. Measures theoriques et verification par jauges extensometriques in
situ. Rev Stomat 1977: 78:545 51.
12. CHAMPYM, LODDEJR SCHMITTR, et al.
Mandibular osteosynthesis by miniature
screwed plates via a buccal approach. J
Max-Fac Surg 1978: 6: 14--21.
13. CHAMPY M, KAHN JL. Discussion of
SHETTY V, McBREARTY 12), FOURNEY M,
et al. Fracture line stability as a function
of the internal fixation system: an in vitro
comparison using a mandibular angle
fracture model. J Oral Maxillofac Surg
1995: 53:801 2.
14. CHOI BH, KIM KN, KANG HS. Clinical
and in vitro evaluation of mandibular
angle fracture fixation with two-miniplate system. Oral Surg 1995: 79: 692-5.
Treatment o f rnandibular angle fractures
15. CHOI BH, Yoo JH, KIM KN, et al. Stability testing of a two-miniplate fixation
technique for mandibular angle fractures.
An in vitro study. J Craniomaxillo~hc
Surg 1995: 23: I22-5.
16. CHUONG R, DONOFF RB, GURALNICK
WC. A retrospective analysis of 327 mandibular fractures. J Oral Maxillofac Surg
1983: 41:305 9.
17. COHENL. Further studies into the vascular architecture of the mandible. J Dent
Res 1960: 39: 936-44.
18. D1CHARD A, KLOTCH DW. Testing biomechanical strength of repairs for the
mandibular angle fracture. Laryngoscope
1994: 104: 201-8.
19. ELLIS E, GHALI GE. Lag screw fixation
of mandibular angle fractures. J Oral
Maxillofac Surg 1991: 49: 234M3.
20. ELLIS E, KARAS N. Treatment of mandibular angle fractures using two minidynamic compression plates. J Oral Maxillofac Surg 1992: 50: 958-63.
21. ELLIS E. Treatment of mandibular angle
fractures using the AO reconstruction
plate. J Oral Maxillofac Surg 1993: 51:
2504.
22. ELLIS E, SINN DR Treatment of mandibular angle fractures using two 2.4 mm
dynamic compression plates. J Oral Maxillofac Surg 1993: 51: 969-73.
23. ELLIS E, WALrO~RL. Treatment of mandibular angle fractures using two noncompression miniplates. J Oral Maxiilofac Surg 1994: 52: i032-6.
24. ELLIS E, WAL~R LR. Treatment of mandibular angle fractures using one noncompression miniplate. J Oral Maxillofac
Surg 1996: 54: 864-71.
25. ELLIS E. Lag screw fixation of mandibular fractures. J Craniomaxillofac Trauma
1997: 3: 16~6.
26. EWERSR, HXRLE E Biomechanics of the
midface and mandibular fractures: is a
stable fixation necessary? In: HJORTINGHANSEN E, ed.: Proceedings from the 8th
International Conference on Oral and
Maxillofacial Surgery. Chicago: Quintessence, 1985: 207-11.
27. EWERS R, HXRLE E Experimental and
clinical results of new advances in the
treatment of facial trauma. Hast Reconstr Surg 1985: 75: 25-31.
28. FEDOK FG, VAN KOOTEN DW, DEJoSEPH
L, et al. Plating techniques and plate
orientation in repair of mandibular angle
fractures: an in vitro study. Laryngoscope
1998: 108: 1218-24.
29. GERLACHKL, PAPEHD. Prinzip und Indikation der Miniplattenost6osynth6se.
Dtsch Zahnaerztl Z 1980: 35: 346-8.
30. GERLACH KL, PAPE HI), NUSSBAUM P.
Untersuchungen zur Belastbarkeit nach
der Miniplattenosteosynthese von Unterkieferfrakturen. Dtsch Z Kiefer Gesichtschit 1984: 8: 363-6.
31. GERLACHKL, KHOURIM, PAPEHD, et al.
The Strasbourg miniplate osteosynthesis.
In: HJORTING-HANSENE, ed.: Proceedings
from the 8th International Conference on
Oral and Maxillofacial Surgery. Chicago:
Quintessence, 1985: 138.
32. HAYTER JP, CAWOOD Ji. The functional
case for miniplates in maxillofacial
surgery, lnt J Oral Maxillofac Surg 1993:
22:91 6.
33. HOFFMANWY, BARTONRM, PRICE M, et
al. Rigid internal fixation vs traditional
techniques for the treatment of mandibular fractures. J Trauma 1990: 30:1032
6.
34. IIZUKAT, LINDQVISTC, HALLIKAINEND,
PAUKKU P Infection after rigid internal
fixation of mandibular fractures. A clinical and radiologic study. J Oral Maxillofac Surg 1991: 49: 585-93.
35. IIZUKA T, LINDQVIST C. Rigid internal
fixation of fractures in the angular region
of the mandible: an analysis of factors
contributing to different complications.
Plast Reconstr Surg 1993: 91:265 71.
36. JAMES RB, FREDRICKSON C, KENT JN.
Prospective study of mandibular fractures. J Oral Surg 1981: 39:275 81.
37. KEARNS GJ, PERROTT DH, KABAN LB.
Rigid fixation of mandibular fractures:
does operator experience reduce complications? J Oral Maxillofac Surg 1994: 52:
226 31.
38. KROON FHM, MATHISSON M, CORDEY
JR, et al. The use of miniplates in mandibular fractures. J Craniomaxillofac
Surg i991: 19: 199-204.
39. KRvOEg E. Mandibular fractues. In:
KRUGER E, SCHII~LI W, eds.: Oral and
maxillofacial traumatology.
Chicago:
Quintessence, 1982:211 36.
40. KURIAKOSEMA, FARDY M, SIRIKUMARA
M, et al. A comparative review of 266
mandibular fractures with internal fixation using rigid (AO/ASIF) plates or
miniplates. Br J Oral Maxillofac Surg
1996: 34:315 21.
41. LEVYFE, SMITHRW, ODLANDRM, et al.
Monocortical miniplate fixation of mandibular fractures. Arch Otolaryngol
Head Neck Surg 1991: 117:149 54.
42. LUHR HG. Compression plate osteosynthesis through the Luhr System. In:
KROGER E, SCHILLI W, eds.: Oral and
maxillofacial traumatology. Vol. 1. Chicago: Quintessence, 1982.
43. LUHR HG, HAUSMANN DF. Ergebnisse
der Kompressionsosteosynthese mit intraoralem Zugang bei 922 Unterkieferfrakturen. Fortschr Kiefer Gesichtschir
1996: 41:77 80.
44. LVHa HG. Personal communication,
1986.
45. MICHELET FX, DEYMESJ, DESSUSB. Osteosynthesis with miniaturized screwed
plates in maxillofacial surgery. 3 MaxFac Surg 1973: 1: 79-84.
46. NIEDERDELLMANN H, AKUAMOA-BOATENG E, UtILIG G. Lag-screw osteosynthesis: a new procedure for treating fractures of the mandibular angle. J Oral
Surg 1981: 39: 93840.
47. PAPE HD, GERLACH KL. Le traitement
des fractures des maxillaires chez l'enfant
251
et l'adolescent. Rev Stolnatol Chir Maxillofac 1980: 81: 2804.
48. PASSER1LA, EI,LIS E, SrNN DR Relationship of substance abuse to complications
with mandibular fractures. J Oral Maxillofac Surg 1993: 51:22 5.
49. PASSERILA, ELLIS E, SINN DR Complications of non-rigid fixation of mandibular angle fractures. J Oralmaxillofac Surg
1993: 51: 382-4.
50. PELED M, ARDEKIANL, ABU-EL-NAAJ 1,
et al. Complications of miniplate osteosynthesis in the treatment of mandibular
fractures. J Cranio-Maxillofac Trauma
1997: 3: 14-7.
51. POTTER J, ELLIS E. Treatment of mandibular angle fractures with a malleable
non-compression miniplate. J Oral Maxillofac Surg 1999: 57:288 92.
52. RAVEHJ, VUILLEMINT, L~2DRACHK, et al.
Plate osteosynthesis of 367 mandibular
fractures. J Craniomaxillofac Surg 1987:
15: 244-53.
53. REITZ1K M, LOWNIE JE JONES C, et al.
Experimental fractures of monkey mandibles. Int J Oral Surg 1978: 7: 1004.
54. RENTON TF, V~ISENFELDD. Mandibular
fracture osteosynthesis: a comparison of
three techniques. Br J Oral Maxillofac
Surg 1996: 34:166 73.
55. RIx L, STEVENSONARL, PUNNIA-MOORTHY A. An analysis of 80 cases of mandibuIar fractures treated with miuiplate
osteosynthesis. Int J Oral Maxillofac
Surg 1991: 20: 33741.
56. SAFDAR N, MEECHAN JG. Relationship
between fractures of the mandibular
angle and the presence and state of eruption of the lower third molar. Oral Surg
1995: 79: 6804.
57. SCI-IIERLEHE SCHMELZEISENR, RAHN B.
Experimentelle Untersuchungen zur biomechanischen Stabilitiit unterschiedlicher
Miniplattenkonfigurationen am Kieferwinkel. Fortschr Kiefer Gesichtschir
1996: 41: 166-70.
58. SCmEr~LEHE SCHMELZEISENR, RAHN B,
et al. One- or two-plate fixation of mandibular angle fractures? J Craniomaxillofac Surg 1997: 25:162 8.
59. SCh'~ELZEISEN R, MClFF T, RAHN B.
Further development of titanium miniplate fixation for mandibular fractures.
Experience gained and questions raised
from a prospective clinical pilot study
with 2.0 mm fixation plates. J Craniomaxillofac Surg 1992: 20: 251-6.
60. SCHMOKER R, SPIESSL B, MATtlYS R. A
total mandibular plate to bridge large defects of the mandible. In: SPIESSLB, ed.:
New concepts in maxillofacial bone
surgery. Berlin: Springer-Verlag, 1976:
156.
61. SCI-rVVIMMERA, STERN R, KRITCHMAND.
Impacted third molars: a contributing
factor in fractures in contact sports. Am
J Sports Med 1983: 11:262 6.
62. SHETTY V, MCBREARTY D, FOURNEY M,
et al. Fracture line stability as a function
of the internal fixation system: an in vitro
252
63.
64.
65.
66.
67.
68.
Ellis"
comparison using a mandibular angle
fracture model. J Oral Maxillofac Surg
1995: 53:791 801.
SmJBERT W, KOBIENIA B J, POLLOCK RA.
Cross-sectional area of the mandible. J
Oral Maxillofac Surg 1997: 55:689 92.
SINN DR HmL SC, WATSON SW Mandibular fractures. In: FOSTER CA, SHERMAN JE, eds.: Surgery of facial bone fractures. New York: Churchill Livingstone,
1987:171 93.
SMITH WR Delayed miniplate osteosynthesis for mandibular fractures. Br J
Oral Maxillofac Surg 1991: 29: 73-6.
SPrESSL B. New concepts in maxillofacial
bone surgery. Berlin: Springer-Verlag,
1976:169 74.
SPIESSL B. Internal fixation of the mandible. New York: Springer-Verlag, 1989:
191 5.
STANELY RB. Pathogeneses and evaluation of mandibular fractures. In: MA-
69.
70.
71.
72.
73.
THOG RH, ed.: Maxillofacial trauma.
Baltimore: Williams & Wilkins, 1984:
13647.
TArE GS, ELLIS E, THROCKNORTON GS.
Bite forces in patients treated for mandibular angle fractures - implications for
fixation recommendations. J Oral Maxillofac Surg 1994: 52: 734-6.
TEVEVA~JGrIDB, DODSON TB. Are mandibular third molars a risk factor for
angle fractures? A retrospective cohort
study. J Oral Maxillofac Surg 1995: 53:
646 9.
VALENTINOJ, LEVY FE, MARENTETTE LJ.
Intraoral monocortical miniplating of
mandible fractures. Arch Otolaryngol
Head Neck Surg 1994: 120: 605-12.
WAGNERWF, NEAL DC, ALPERT B. Morbidity associated with extraoral open reduction of mandibular fractures. J Oral
Surg 1979: 37:97 100.
WALD RM, ABEMAYORE, ZEMPLENYIJ, et
al. The transoral treatment of mandibular fractures using noncompression miniplates: a prospective study. Ann Plast
Surg 1988: 20: 409~ 13.
74. YAMADAT, SAWAKIY, TOHNAI I, et al. A
study of sports-related mandibular angle
fracture: relation to the position of the
third molars. Scand J Med Sci Sports
1998: 8:116 9.
Address:
Edward Ellis 11I, D.D.S., M.S.
Professor, Oral and Maxillofacial Surgery
The University of Texas Southwestern
Medical Center
5323 Harry Hines Blvd. CS3.104
Dallas, Texas 75235 9109
USA
Tel." +1 214 648 8963
Fax: +1 214 648 7620
e-mail: eellis@mednet.swmed.edu
Vous aimerez peut-être aussi
- Desai 2015Document3 pagesDesai 2015ashajangamPas encore d'évaluation
- Hohmann 2006Document6 pagesHohmann 2006ashajangamPas encore d'évaluation
- Evolution and Controversies in Palatoplasty TechniquesDocument11 pagesEvolution and Controversies in Palatoplasty TechniquesNavatha MorthaPas encore d'évaluation
- 24Document7 pages24ashajangamPas encore d'évaluation
- Pi Is 0278239109005710Document12 pagesPi Is 0278239109005710ashajangamPas encore d'évaluation
- AOMSI Fellowship Centres - Trauma-1Document1 pageAOMSI Fellowship Centres - Trauma-1ashajangamPas encore d'évaluation
- Multidimensional Diagnosis and Treatment Planning in Maxillofacial SurgeryDocument1 pageMultidimensional Diagnosis and Treatment Planning in Maxillofacial SurgeryashajangamPas encore d'évaluation
- Hbot 3Document11 pagesHbot 3Nantini GopalPas encore d'évaluation
- Advances in Pain TreatmentDocument10 pagesAdvances in Pain TreatmentrizjkuramaPas encore d'évaluation
- Internationally Indexed Journal Internationally Indexed Journal Internationally Indexed Journal Internationally Indexed JournalDocument5 pagesInternationally Indexed Journal Internationally Indexed Journal Internationally Indexed Journal Internationally Indexed JournalashajangamPas encore d'évaluation
- 1Document7 pages1Delia StaricaPas encore d'évaluation
- Distraction Osteogenesis of The Maxillofacial Skeleton Biomechanics andDocument10 pagesDistraction Osteogenesis of The Maxillofacial Skeleton Biomechanics andMauricio Alejandro Maureira CifuentesPas encore d'évaluation
- Ooo JRNLDocument7 pagesOoo JRNLashajangamPas encore d'évaluation
- ContentsdDocument1 pageContentsdashajangamPas encore d'évaluation
- Maxillomandibular Advancement For Obstructive Sleep Apnea: Kasey K. Li, DDS, MDDocument8 pagesMaxillomandibular Advancement For Obstructive Sleep Apnea: Kasey K. Li, DDS, MDashajangamPas encore d'évaluation
- Dedication: Oral Maxillofacial Surg Clin N Am 20 (2008) XiDocument1 pageDedication: Oral Maxillofacial Surg Clin N Am 20 (2008) XiashajangamPas encore d'évaluation
- 1750-1172-9-9 13Document5 pages1750-1172-9-9 13ashajangamPas encore d'évaluation
- Advances in Extraction TechniquesDocument13 pagesAdvances in Extraction TechniquesashajangamPas encore d'évaluation
- 03 MFDS Regulations & Syllabus 2011Document15 pages03 MFDS Regulations & Syllabus 2011FarahMohammed1Pas encore d'évaluation
- 2011Document2 pages2011ashajangamPas encore d'évaluation
- BjomsDocument11 pagesBjomsSagar JangamPas encore d'évaluation
- Palmer 2011 Dental Clinics of North AmericaDocument12 pagesPalmer 2011 Dental Clinics of North AmericaashajangamPas encore d'évaluation
- Patients DiaryDocument7 pagesPatients Diarysagarjangam123Pas encore d'évaluation
- Transitioning From Residency To Private Practice: M. Todd Brandt, DDS, MDDocument9 pagesTransitioning From Residency To Private Practice: M. Todd Brandt, DDS, MDГулпе АлексейPas encore d'évaluation
- Aggressive Pediatric Tumor of The Jaw-Ameloblastoma: AbstractDocument1 pageAggressive Pediatric Tumor of The Jaw-Ameloblastoma: AbstractashajangamPas encore d'évaluation
- Oral Maxillofacial Surg Clin N Am 20 (2008Document2 pagesOral Maxillofacial Surg Clin N Am 20 (2008Гулпе АлексейPas encore d'évaluation
- IjomsauthDocument1 pageIjomsauthashajangamPas encore d'évaluation
- Hemostab, Blknktic AgentsDocument7 pagesHemostab, Blknktic AgentsashajangamPas encore d'évaluation
- AOMSI 2014 National Conference Registration FormDocument2 pagesAOMSI 2014 National Conference Registration FormashajangamPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- PONTIC DESIGN FACTORS FOR SUCCESSDocument53 pagesPONTIC DESIGN FACTORS FOR SUCCESSmanjulikaPas encore d'évaluation
- Team 2 Presents Vital SignsDocument44 pagesTeam 2 Presents Vital Signswiwin100% (1)
- Functional Crown Lengthening Surgery Periodontic and Prosthodontic ConsiderationsDocument5 pagesFunctional Crown Lengthening Surgery Periodontic and Prosthodontic ConsiderationsNajeeb UllahPas encore d'évaluation
- CNPASDocument3 pagesCNPASaneeshPas encore d'évaluation
- Day 1 BacteriaDocument251 pagesDay 1 BacteriaLisa NetherlandPas encore d'évaluation
- Know Your Magnetic FieldDocument75 pagesKnow Your Magnetic FieldAtma Jnani100% (5)
- Pre - and Post Test Cardiac ArrhythmiasDocument6 pagesPre - and Post Test Cardiac ArrhythmiasEköw Santiago JavierPas encore d'évaluation
- Surgical Pathology of The Gastrointestinal System Bacterial, Fungal, Viral, and Parasitic Infections PDFDocument234 pagesSurgical Pathology of The Gastrointestinal System Bacterial, Fungal, Viral, and Parasitic Infections PDFBogdan CarabasPas encore d'évaluation
- Strategic ManagementDocument24 pagesStrategic ManagementSonetAsrafulPas encore d'évaluation
- Siemens Healthcare Diagnostics Reagent Strips For UrinalysisDocument16 pagesSiemens Healthcare Diagnostics Reagent Strips For Urinalysisrex2005Pas encore d'évaluation
- 1001 Arab Inventions WorksheetDocument4 pages1001 Arab Inventions WorksheetVictorPas encore d'évaluation
- A Deprogrammer For Occlusal Analysis and Simplified Accurate Case MountingDocument7 pagesA Deprogrammer For Occlusal Analysis and Simplified Accurate Case MountingMichael XuPas encore d'évaluation
- Data Persediaan Medis XL OceDocument38 pagesData Persediaan Medis XL OceRonyChanyaPas encore d'évaluation
- ECG Interpretation Cheat Sheet PDFDocument1 pageECG Interpretation Cheat Sheet PDFChristine MerrittPas encore d'évaluation
- Key Points: Schwartz's Principles of Surgery Chapter 23. Arterial DiseaseDocument142 pagesKey Points: Schwartz's Principles of Surgery Chapter 23. Arterial DiseaseMohammad FareedPas encore d'évaluation
- Risks of Elective Cesarean SectionDocument11 pagesRisks of Elective Cesarean SectionLutfiAnny Rahman HakimPas encore d'évaluation
- Principles of Practice For Pharmaceutical CareDocument29 pagesPrinciples of Practice For Pharmaceutical CareNgetwa TzDe TheWirymanPas encore d'évaluation
- Esthetic Analysis of The SmileDocument7 pagesEsthetic Analysis of The SmileNitin H.c.Pas encore d'évaluation
- The World Health Organization's WHOQOL-BREF Quality of LifeDocument12 pagesThe World Health Organization's WHOQOL-BREF Quality of LifeLIDIYA MOL P V100% (1)
- Learning Related Vision ProblemsDocument38 pagesLearning Related Vision Problemseva.benson100% (1)
- Intravenous Nutrient TherapyDocument15 pagesIntravenous Nutrient TherapySuresh IndiaPas encore d'évaluation
- International Journal of Psychophysiology: Helen Beuzeron-Mangina, Constantine A. ManginaDocument6 pagesInternational Journal of Psychophysiology: Helen Beuzeron-Mangina, Constantine A. ManginaIcaroPas encore d'évaluation
- Inspection Workbook Obstetrics and GynecologyDocument40 pagesInspection Workbook Obstetrics and Gynecologydelap05Pas encore d'évaluation
- Nursing Assignments GuideDocument54 pagesNursing Assignments GuideEya CamillerPas encore d'évaluation
- Cerumen ImpactionDocument6 pagesCerumen ImpactionNin DuskPas encore d'évaluation
- Psychiatric Medication Guidelines Pregnancy LactationDocument27 pagesPsychiatric Medication Guidelines Pregnancy LactationSunija SelvamPas encore d'évaluation
- Trigger Points Massage Therapy GuideDocument24 pagesTrigger Points Massage Therapy GuideTaina Avramescu100% (2)
- Family Nursing Care Plan Proper Cigarette Smoking As Health ThreatDocument2 pagesFamily Nursing Care Plan Proper Cigarette Smoking As Health ThreatWishley Ann PiñedaPas encore d'évaluation
- Ex Harvard Medical School Personal Statement ExampleDocument3 pagesEx Harvard Medical School Personal Statement ExamplekikyPas encore d'évaluation
- Procedure For DefibrillationDocument6 pagesProcedure For DefibrillationTasia DeastutiPas encore d'évaluation