Académique Documents
Professionnel Documents
Culture Documents
Ultrasound-Guided Intervention Around The Hip Joint: Emma L. Rowbotham Andrew J. Grainger
Transféré par
andrew herringTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Ultrasound-Guided Intervention Around The Hip Joint: Emma L. Rowbotham Andrew J. Grainger
Transféré par
andrew herringDroits d'auteur :
Formats disponibles
M u s c u l o s k e l e t a l I m a g i n g R ev i ew
Rowbotham and Grainger
Ultrasound-Guided Intervention in Hip Joint
Downloaded from www.ajronline.org by 132.174.255.215 on 02/10/15 from IP address 132.174.255.215. Copyright ARRS. For personal use only; all rights reserved
Musculoskeletal Imaging
Review
Ultrasound-Guided Intervention
Around the Hip Joint
Emma L. Rowbotham1
Andrew J. Grainger
Rowbotham EL, Grainger AJ
OBJECTIVE. The purpose of this article is to review some of the most common reasons
for ultrasound intervention around the hip joint, and describe the techniques involved.
CONCLUSION. Ultrasound alleviates the need for exposure to radiation and is already
the modality of choice for aspiration of the hip joint, an intervention that may be helpful in
guiding antimicrobial therapy and help avoid the need for surgical intervention. Ultrasound
can also be used to access the hip for diagnostic or therapeutic injection.
Keywords: greater trochanteric bursa, hip, iliopsoas
tendon bursa, ultrasound
DOI:10.2214/AJR.10.6344
Received December 14, 2010; accepted without revision
December 28, 2010.
1
Both authors: Department of Musculoskeletal
Radiology, Leeds Teaching Hospitals, Chapel Allerton
Hospital, Chapeltown Rd, Leeds, West Yorkshire LS7
4SA, United Kingdom. Address correspondence to
A. J. Grainger (andrew.grainger@leedsth.nhs.uk).
WEB
This is a Web exclusive article.
AJR 2011; 197:W122W127
0361803X/11/1971W122
American Roentgen Ray Society
W122
ltrasound of the adult hip is a
commonly performed investigation that may be used to assess
for both intra- and extraarticular
pathology. Common findings include joint
fluid, bursitis, hematoma, and paralabral cyst
formation. Increasingly, ultrasound is being
used to guide intervention around the hip
joint for both diagnostic and therapeutic purposes. Ultrasound alleviates the need for exposure to radiation and is already the modality of choice for aspiration of the hip joint [1],
an intervention that may be helpful in guiding antimicrobial therapy and help avoid the
need for surgical intervention. Ultrasound
can also be used to access the hip for diagnostic or therapeutic injection [2]. Guided injection of the greater trochanteric bursa or
the iliopsoas tendon bursa may have enormous therapeutic benefits to the patient without the need for surgery or exposure to ionizing radiation. We review some of the most
common reasons for ultrasound intervention
around the hip joint: intraarticular injection,
aspiration of joint fluid for both therapeutic
and diagnostic purposes, injection of trochanteric or iliopsoas bursitis, and treatment
of the symptomatic snapping hip. We describe the techniques used at our institution
for these ultrasound-guided interventions,
along with tips to aid a successful procedure.
Intervention Technique
In many cases, diagnostic ultrasound will
be performed at the same appointment as
any appropriate intervention. With modern
equipment, a high-frequency linear probe
can be used to image the hip joint, typically
with frequencies around 915 MHz depending on patient body habitus. Occasionally, a
lower-frequency probe may be required if
the patient is obese.
Providing an aseptic environment is of
paramount importance in minimizing the introduction of infection, particularly when injecting into the joint itself. This essentially
involves using sterile gloves and probe covers; cleaning of the skin with an antiseptic
skin preparation, such as chlorhexidine solution; and ensuring the needle tip passes
through the cleaned area of skin, avoiding
any areas of broken skin or overlying infected areas. With the probe positioned over the
hip joint in the sagittal plane, the femoral
head is visualized and just superior to it, the
acetabular roof and acetabular labrum. The
labrum is a hyperechoic triangular structure
attached to the brightly hyperechoic bone of
the acetabulum (Fig. 1).
There are several important factors to
consider that will aid a successful ultrasound
guided procedure. Namely, always know
where the needle is, have a good knowledge
of the surrounding anatomy, and only inject
when the tip of the needle is visible. The crucial factor in keeping the needle visible on
the screen is to keep the probe and the needle in the same place throughout the procedure. However, it is important to realize that
the needle is best visualized when the needle
and probe face are parallel. With increasing
angle of insonation, the visualization of the
needle becomes less clear and may even become invisible due to the reflection of sound
AJR:197, July 2011
Downloaded from www.ajronline.org by 132.174.255.215 on 02/10/15 from IP address 132.174.255.215. Copyright ARRS. For personal use only; all rights reserved
Ultrasound-Guided Intervention in Hip Joint
sity at 6 months when performed in vivo [3].
Consequently, we prefer the use of lidocaine
for anesthetizing the skin and bupivacaine
for intraarticular injection. The equipment
needed for injection of the hip is shown in
Figure 4.
Fig. 1Hip anatomy.
A, Radiograph shows normal anatomy of hip in healthy subject. Plane of transducer (blue) is parallel to
femoral neck.
B, Sonogram in 28-year-old man shows hip joint with transducer placed in oblique axial plane along femoral
neck (F) and corresponding normal anatomy of hip joint. Hyperechoic labrum is seen covering superior aspect
of femoral head (blue arrow). There is small joint effusion seen at this hip joint (white arrow).
Fig. 2Greater trochanteric bursa in 68-year-old woman.
A, Normal radiograph from healthy subject (provided for comparison) shows probe position (blue) is placed
along lateral aspect of hip in plane parallel to lateral surface of greater trochanter.
B, Needle parallel to probe. Image shows needle (arrow) being introduced into soft tissues toward greater
trochanter (GT) in plane parallel to transducer. This is optimal angle and entire needle is easily seen.
away from the probe (Fig. 2). Careful planning of the needle path will allow exquisite
visualization of the needle during the procedure. Marking of the skin at the chosen entry point before injection is a valuable step in
the procedure (Fig. 3). This allows the needle to be positioned into the subcutaneous
tissues first without the need for also holding the transducer. The transducer can then
be brought over the needle tip and the position confirmed before advancing the needle
into the desired location. A 22-gauge needle
is usually used for injections around the hip.
A larger bore needle, such as a 16 or 18 gauge
may be needed for aspiration, particularly if
the fluid is infected.
With all the described injections, a combination of local anesthetic and steroids is
used to maximize symptom relief. The steroid used in our institution is 40 mg triamcinolone and the local anesthetic is 1% lidocaine, usually in a volume of 5 mL. A recent
study comparing the chondrocyte-damaging
properties of local anesthetics used in joint
injections has shown that 0.5% bupivacaine
resulted in a reduction in chondrocyte den-
Ultrasound-Guided Aspiration
of the Hip
One of the most common indications for
ultrasound of the adult hip is the detection
and aspiration of a joint effusion. Pain in the
groin or medial thigh, pain aggravated by lying on the side, decreased extension or internal rotation or abduction or flexion, painful
external rotation, and pain on palpation in
the groin showed a significant relation (adjusted for age and radiologic osteoarthritis of
the hip) with ultrasonic hip joint effusion [4].
The most common reason for aspiration in
the hip is for the diagnosis of infection. However, reliance on the ultrasound appearance
of the effusion is not sufficient to distinguish
between infection and a simple effusion. Pus
can appear anechoic, and a complex appearance to the effusion does not reliably indicate
sepsis (Fig. 5). The presence of a joint effusion is confirmed by an increased volume
of fluid in the anterior recess. This is usually measured in the oblique sagittal plane
along the line of the femoral neck and should
be compared with a measurement from the
contralateral side (Fig. 6). The normal distance from femoral neck to the capsule has
been described as between 4 and 10 mm. It
can sometimes be difficult to differentiate
thickened synovium from joint effusion because both have similar appearances on ultrasound. If this is the case, asking the patient to move the hip is helpful because this
will disperse an effusion around the joint,
whereas synovial thickening would remain
constant in appearance. Aspiration of joint
effusion is not always necessary and should
be confined to patients in whom there is a
high clinical suspicion of sepsis.
Ultrasound-Guided Injection
Injection of the hip joint is undertaken for
a variety of reasons. Inflammatory arthritides
may be treated with direct injection of cortisone into the hip. Similarly, symptomatic relief of osteoarthritis may also be achieved.
Frequently, it is unclear whether a patients
symptoms are due to hip pathology, for instance if the patient has both hip osteoarthritis and degenerative change in the spine. In this
situation, a diagnostic injection of long-acting
AJR:197, July 2011 W123
Downloaded from www.ajronline.org by 132.174.255.215 on 02/10/15 from IP address 132.174.255.215. Copyright ARRS. For personal use only; all rights reserved
Rowbotham and Grainger
Fig. 3Photograph shows hip injection skin marking in 32-year-old woman. Marking of skin before injection
allows accurate placement of needle into tissues and then placing probe back onto skin to guide final
positioning. This image shows marking of skin before hip joint injection with probe in axial plane.
A and B, Axial ultrasound image (B) shows corresponding normal anatomy with probe in axial plane as in A.
Labrum is indicated with blue arrow and psoas muscle overlying femoral head (F) is indicated with white arrow.
Fig. 5Complex hip effusion in 74-year-old woman.
There is large amount of complex fluid (arrow) seen
within hip joint in patient who has had dynamic
hip screw inserted into femoral headneck after
fractured neck of femur (F). Hip aspirate revealed
frank pus within joint and patient was taken to theater
for washout of septic joint.
Fig. 4Photograph shows injection equipment.
Chlorhexidine cleaning sticks are now used for
all procedures at our institution, and 1% lidocaine
is usually adequate for subcutaneous analgesia.
Duraprene manufactured by Allegiance Healthcare.
the needle to be introduced almost parallel
to the probe face. This technique also means
the skin puncture is made laterally, well away
from the medially located neurovascular bundle. This enables the operator to place the needle and then confirm position with the sterile probe. For aspiration, the needle should be
placed into the deepest pool of fluid within the
joint and aspirated into a sterile syringe. Samples should be sent for culture and sensitivity.
Aspiration should be as complete as possible
to maximize relief of symptoms.
As with aspiration of the hip, we prefer an
axial approach to the hip joint for injection.
The femoral head is identified and the probe is
then positioned to obtain an axial view through
the head. Sweeping the probe distally identifies the junction of the femoral neck and head
in the axial plane, which is the point targeted
for the injection. The needle is introduced from
the lateral side along the long axis of the probe
and as parallel to the probe face as is feasible.
When the needle is seen (and felt) to contact the
bone, it will lie within the joint on the anterolateral aspect of the headneck junction (Fig.
7). A sterile technique is again of paramount
importance, and marking the skin at the appropriate needle entry point before preparing
the sterile equipment is helpful. A combination
of local anesthetic and steroids should be prepared in the same syringe. The injectate should
be placed into the anterior recess at the femoral
headneck junction (Fig. 8). Unless the examination is being undertaken for arthrography,
anesthetic into the hip can help make the distinction. We also make use of ultrasound guidance for the injection of contrast material for
MRI arthrography. In this instance, the technique is essentially the same as for therapeutic
injection, with contrast medium instilled into
the joint as opposed to local anesthetic and steroids. The introduction of contrast material for
arthrography can be combined with diagnostic
anesthetic injection if required.
Aspiration and Injection Technique
For both injection into the hip joint and aspiration of the hip joint the patient should be
positioned supine and the transducer placed in
the longitudinal oblique plane along the axis
of the femoral neck to examine the anterior
recess and confirm the presence of effusion
(Fig. 6). Intervention can be performed either
in the axial or sagittal plane. In our institution,
the axial plane is preferred because it allows
W124
Fig. 6Axial oblique approach to hip joint in 82-year-old woman.
A, Photograph shows transducer placed in axial oblique plane along femoral neck and needle placed into soft
tissues along line of transducer.
B, Sonogram shows hip effusion (arrow). In this case, effusion has been measured (calipers) in anteroposterior
direction and measurement was compared with contralateral side to confirm presence of effusion.
AJR:197, July 2011
Downloaded from www.ajronline.org by 132.174.255.215 on 02/10/15 from IP address 132.174.255.215. Copyright ARRS. For personal use only; all rights reserved
Ultrasound-Guided Intervention in Hip Joint
gluteus medius and gluteus minimus muscles have been described in the literature as
the rotator cuff of the hip, and tendinopathy
or tears of these two muscles have also been
shown to be present in most patients presenting with trochanteric bursitis [5].
Fig. 7Hip injection video in 71-year-old man. This
animation shows needle entering tissues distal to
hip joint and then being guided to hip joint before
injecting mixture of local anesthetic and steroid into
joint space under ultrasound guidance. For this
video, see Figure S7 in supplemental data at www.
ajronline.org.
Fig. 8Sagittal sonogram of hip joint in 68-year-old
woman shows femoral head (F) and needle within
hip joint (arrow) immediately before injection. (See
also Fig. S8, cine loop, in supplemental data at www.
ajronline.org.)
it is helpful to inject a little air at the start of
the injection. This is easily seen on ultrasound
and confirms the intraarticular location of the
injection. If the patient is to undergo MRI arthrography, the presence of air is to be avoided
because it may be confused for pathology, such
as intraarticular loose bodies.
The patient should be warned that there
might be an aching sensation in the hip in
the 24 hours after injection and, when cortisone has been injected, that the maximal
therapeutic benefit may not be experienced
for several days after the procedure.
Ultrasound-Guided Injection of
the Greater Trochanteric Bursa
Trochanteric bursitis is a relatively common condition affecting physically active pa-
tients and usually presenting with pain to the
lateral aspect of the hip, particularly on walking. This condition either occurs secondary to
an injuryusually overuse injuryor more
rarely as a manifestation of rheumatoid arthritis. Traumatic injury includes bursal irritation as a result of the iliotibial band moving over the bursa repetitively and is usually
seen in athletes. The trochanteric bursa is best
thought of as a bursal complex with bursae
present between the gluteal tendons. The trochanteric bursa itself is often described as being situated between the iliotibial tract and the
gluteal tendons (Fig. 9). In addition there is
a subgluteus medius bursa beneath the gluteus medius tendon, and similarly, a subgluteus
minimus bursa. Inflammation of any of these
bursae will present with lateral hip pain. The
Greater Trochanteric
Bursa Technique
The trochanteric bursae are best approached
with the patient lying on the side in the lateral
decubitus position with the symptomatic side
uppermost (Fig. 9A). The bursae are relatively
superficial structures and therefore readily accessible. The superficial position also makes
keeping the probe face and needle track parallel relatively easy. Both axial and sagittal imaging will show fluid within the bursa, provided
not too much pressure is applied with the transducer, which may compress the inflamed bursa. As in assessment of joint effusion, comparison with the contralateral side is useful when
findings are equivocal. Again, sterile conditions are essential. A combination of local anesthetic and steroids (typically 40 mg triamcinolone) should be prepared and injected into the
fluid collection (Fig. 10).
Ultrasound-Guided Treatment
of Iliopsoas Pathology
When the patient moves the hip through certain positions, snapping of the iliopsoas tendon
over the iliopectineal eminence may cause an
audible snap or click that can be painful and
felt anteriorly. This condition may occur secondary to previous trauma or injury, particularly overuse injury [6]. The iliopsoas muscle
functions as a hip flexor and arises from the
Fig. 9Trochanteric bursitis injection position in 57-year-old woman.
A, Photograph shows position of transducer in longitudinal plane with relation to greater trochanter. Position of proximal end of transducer has been marked before
injection.
B, Trochanteric bursa (blue arrow) is thickened in this axial image and shows echo-poor line immediately adjacent to bone cortex, in keeping with trochanteric bursitis.
Gluteus medius bursa is also thickened in this example (white arrow). GT = greater trochanter.
C, Further more florid example of trochanteric bursitis (arrow) is shown in this longitudinal image. GT = greater trochanter.
AJR:197, July 2011 W125
Downloaded from www.ajronline.org by 132.174.255.215 on 02/10/15 from IP address 132.174.255.215. Copyright ARRS. For personal use only; all rights reserved
Rowbotham and Grainger
bundle. The patient is best positioned in the
supine position. A combination of local anesthetic and steroids is again required. The
approach is similar to that used to inject the
hip in the axial plane. By positioning the
probe over the bursa or tendon, the needle
can be advanced in the lateral side of the
thigh, parallel to the probe face, maintaining exquisite visualization. Injection typically comprises 40 mg of triamcinolone mixed
with a small amount of lidocaine.
A
Fig. 10Needle position in greater trochanteric bursa in 68-year-old woman.
A and B, Sonograms show start (A) and end (B) positions of needle as it is positioned into greater trochanteric
bursa as shown in video Figure S10A (available in supplemental data at www.ajronline.org).A shows needle
(blue arrow) entering tissues proximal to greater trochanter (GT) and greater trochanteric bursa (white arrow),
and B shows final position of needle in trochanteric bursa immediately before injection. Needle (blue arrow) is
seen clearly with tip in bursa (white arrow).
Fig. 11Snapping iliopsoas tendon in 27-year-old man.
A and B, Sonograms show start (A) and end (B) of snapping iliopsoas tendon (IP) (blue arrow) as it flips across
iliopectineal eminence of pelvis. (See also Fig. S11A in supplemental data at www.ajronline.org).
anterior inferior iliac spine and inserts into the
lesser trochanter of the femur. A similar sensation is produced by the iliotibial band snapping over the greater trochanter but is felt in
a lateral position and usually felt as the hip
moves from extension to flexion. Iliopsoas tendinopathy is a recognized complication in patients who have had hip replacement surgery
[7]. It may be possible to show impingement of
the iliopsoas tendon on a prominent aspect of
the hip arthroplasty. It is important to exclude
other pathology that may present with similar
symptoms, such as labral tears, cartilage defects, and intraarticular loose bodies.
Ultrasound can be used to show the iliopsoas muscle flipping over the iliacus muscle
to confirm the diagnosis of snapping iliopsoas
(Fig. 11), and in many cases an associated ilio-
W126
psoas bursitis will also be visualized. Iliopsoas
bursitis may also be seen be seen in isolation
and is treated the same way.
In some cases, surgical intervention is necessary to alleviate symptoms, but a combination of
local anesthetic and corticosteroid injection can
often provide symptomatic relief and avoid the
need for surgery. The injection is performed into
the iliopsoas bursa or, in the absence of a bursa,
deep to the iliopsoas tendon. Failure of the injection to provide symptomatic relief suggests that
an alternative pathology may be responsible for
the patients hip or groin pain.
Iliopsoas Technique
With the probe oriented along the femoral head and neck, the iliopsoas tendon can
be seen to lie lateral to the neurovascular
Complications of Ultrasound-Guided
Intervention Around the Hip Joint
Complications after ultrasound-guided intervention at the hip are not common. However, as with every interventional procedure,
complications do occasionally occur. The most
common include infection both at the puncture site and of the hip joint itself, bleeding into
the joint, and injury to the femoral nerve. Allergy to the local anesthetic may present with
systemic symptoms of headache, dizziness,
circumoral numbness and tachycardia, or local symptoms related to nerve damage, such as
paraesthesia or prolonged anesthesia.
Introducing infection into the joint is rare,
but if it occurs it may have long-term consequences in terms of damage to the joint.
Patients should be informed of this potential
complication when giving consent for the
procedure to be performed. Aseptic conditions minimize this risk, but patients should
be aware that ongoing or worsening symptoms accompanied by redness and swelling
around the joint may be a sign of infection.
Bleeding into the joint is minimized by
ensuring the international normalized ratio is below 1.5. Patients on anticoagulation
therapy should be advised to stop the therapy
before the procedure is performed.
Injury to the femoral nerve is rare but is
documented in the literature [8]. This is usually temporary and results in diminished sensation over the anterior thigh and inability to
flex the hip or put weight on the extremity.
One of the major advantages of ultrasound
guidance over fluoroscopy for intervention
around the hip is that the femoral nerve and
other neurovascular structures are well visualized and therefore injury is minimized.
References
1. Sofka CM, Collins AJ, Adler RS. Use of ultrasonographic guidance in interventional musculoskeletal procedures: a review from a single institution. J Ultrasound Med 2001; 20:2126
2. Micu MC, Bogdan GD, Fodor D. Steroid injection
AJR:197, July 2011
Downloaded from www.ajronline.org by 132.174.255.215 on 02/10/15 from IP address 132.174.255.215. Copyright ARRS. For personal use only; all rights reserved
Ultrasound-Guided Intervention in Hip Joint
for hip osteoarthritis: efficacy under ultrasound
guidance. Rheumatology 2010; 49:14901494
3. Chu CR, Coyle CH, Chu CT, et al. In vivo effects
of single intra-articular injection of 0.5% bupivacaine on articular cartilage. J Bone Joint Surg Am
2010; 92:599608
4. Bierma-Zeinstra SM, Bohnen AM, Verhaar JA,
Prins A, Ginai-Karamat AZ, Lamris JS. Sonog-
raphy for hip joint effusion in adults with hip pain.
Ann Rheum Dis 2000; 59:178182
5. Kumar G, Warren O, Somashekar N, Marston RA.
Use of ultrasound in trochanteric bursitis. (abstr) J
Bone Joint Surg Br 2005; 88B[suppl 1]: 76
6. Deslandes M, Gullin R, Cardinal E, Hobden R, Bureau NJ. The snapping iliopsoas tendon: new mechanisms using dynamic sonography. AJR 2008;
190:576581
7. Brew CJ, Stockley I, Grainger AJ, Stone MH. Iliopsoas tendonitis caused by overhang of a collared
femoral prosthesis. J Arthroplasty 2011; 26:504
8. Leopold SS, Battista V, Olivero JA. Safety and efficacy of intra-articular hip injection using anatomic landmarks. Clin Orthop Relat Res 2001;
391:192197
F O R YO U R I N F O R M AT I O N
The data supplement accompanying this Web exclusive article can be viewed from
the information box in the upper right corner of the article at: www.ajronline.org.
AJR:197, July 2011 W127
Vous aimerez peut-être aussi
- Current Challenges with their Evolving Solutions in Surgical Practice in West Africa: A ReaderD'EverandCurrent Challenges with their Evolving Solutions in Surgical Practice in West Africa: A ReaderPas encore d'évaluation
- Percutaneous Imaging-Guided Spinal Facet Joint InjectionsDocument6 pagesPercutaneous Imaging-Guided Spinal Facet Joint InjectionsAlvaro Perez HenriquezPas encore d'évaluation
- Eular Us Course Modulo 5 Tornozelo e PeDocument44 pagesEular Us Course Modulo 5 Tornozelo e PeGustavo Bernardo DamascenoPas encore d'évaluation
- Minimally Invasive Surgery for Chronic Pain Management: An Evidence-Based ApproachD'EverandMinimally Invasive Surgery for Chronic Pain Management: An Evidence-Based ApproachGiorgio PietramaggioriPas encore d'évaluation
- Ultrasound Guided Lower Limb Blocks Tony AllenDocument39 pagesUltrasound Guided Lower Limb Blocks Tony Allenrepre64Pas encore d'évaluation
- Peripheral Nerve Blocks Lower ExtremityDocument53 pagesPeripheral Nerve Blocks Lower ExtremityArief Hariyadi SantosoPas encore d'évaluation
- MSK Us ProtocolsDocument40 pagesMSK Us Protocolsjamir59Pas encore d'évaluation
- Cervical Spine Trauma: Shreya Kangovi Radiology Core, BIDMC July 25th, 2004Document25 pagesCervical Spine Trauma: Shreya Kangovi Radiology Core, BIDMC July 25th, 2004ComagaPas encore d'évaluation
- Ultrasound Guided Interventional Procedures In.13Document14 pagesUltrasound Guided Interventional Procedures In.13andrew herring100% (1)
- Hill - Workshop - Intro To MSK US Shoulder WS 2014-1Document32 pagesHill - Workshop - Intro To MSK US Shoulder WS 2014-1Raihan LuthfiPas encore d'évaluation
- Platelet-Rich Plasma in Osteoarthritis Treatment: Review of Current EvidenceDocument18 pagesPlatelet-Rich Plasma in Osteoarthritis Treatment: Review of Current EvidenceIrham KhairiPas encore d'évaluation
- Limb Length DiscrepancyDocument2 pagesLimb Length DiscrepancyMuhammed BarznjiPas encore d'évaluation
- Fundamentals of Diagnostic RadiologyDocument52 pagesFundamentals of Diagnostic RadiologyYabets100% (1)
- Knee Differential DiagnosisDocument2 pagesKnee Differential DiagnosisJade Kenneth Gonzales LomansocPas encore d'évaluation
- USG - Hip & Knee-Dr - NarayanDocument92 pagesUSG - Hip & Knee-Dr - NarayancmonmanPas encore d'évaluation
- Regional Anesthesia For Scapular Fracture Surgery: An Educational Review of Anatomy and TechniquesDocument6 pagesRegional Anesthesia For Scapular Fracture Surgery: An Educational Review of Anatomy and TechniquesSean SmythPas encore d'évaluation
- Acetabular FractureDocument136 pagesAcetabular FracturePicha PichiPas encore d'évaluation
- Peroneal Nerve Palsy PDFDocument10 pagesPeroneal Nerve Palsy PDFChristian Reza WibowoPas encore d'évaluation
- Crozer-Keystone Ex Tern Ship ManualDocument187 pagesCrozer-Keystone Ex Tern Ship ManualRihamary CruzPas encore d'évaluation
- Lumbar Radiculopathy Medback Castillo Mendez EDITEDDocument12 pagesLumbar Radiculopathy Medback Castillo Mendez EDITEDSteve ColbertPas encore d'évaluation
- SJAMS 43B 750 754 Thesis Tibial PlateauDocument5 pagesSJAMS 43B 750 754 Thesis Tibial PlateauNisheshJainPas encore d'évaluation
- Collateral Ligament Injury MRIDocument29 pagesCollateral Ligament Injury MRILeksmana AcPas encore d'évaluation
- Suspecting and Diagnosing The Patient With Spondyloarthritis 2021. CLINICSDocument15 pagesSuspecting and Diagnosing The Patient With Spondyloarthritis 2021. CLINICSluisa100% (1)
- Bone AgeDocument65 pagesBone AgeueumanaPas encore d'évaluation
- Diagnosis in OrthopaedicsDocument48 pagesDiagnosis in OrthopaedicsBakta Giri100% (1)
- Quadrilatral and Ischial SocketDocument133 pagesQuadrilatral and Ischial Socketjay prakashPas encore d'évaluation
- Review - Presby Residency ManualDocument400 pagesReview - Presby Residency ManualSneha SutharPas encore d'évaluation
- Treatment of SLAC-CartagenaDocument40 pagesTreatment of SLAC-CartagenaProfesseur Christian DumontierPas encore d'évaluation
- Transition To Anterior Approach in Primary Total Hip Arthroplasty Learning Curve ComplicationsDocument7 pagesTransition To Anterior Approach in Primary Total Hip Arthroplasty Learning Curve ComplicationsAthenaeum Scientific PublishersPas encore d'évaluation
- PDFDocument328 pagesPDFBreak DerulsPas encore d'évaluation
- Outpatientassessmentand Managementofthediabeticfoot: John A. DipretaDocument21 pagesOutpatientassessmentand Managementofthediabeticfoot: John A. DipretaAnonymous kdBDppigEPas encore d'évaluation
- LEAN Boards Review CL 2011Document9 pagesLEAN Boards Review CL 2011pudding35Pas encore d'évaluation
- Rheumatology - For BPTsDocument72 pagesRheumatology - For BPTsfire_n_icePas encore d'évaluation
- Journal ReadingDocument7 pagesJournal ReadingTommy HardiantoPas encore d'évaluation
- Braun Neurology Endoscope SystemDocument132 pagesBraun Neurology Endoscope SystemMārcis RancānsPas encore d'évaluation
- Sample ResumeDocument5 pagesSample ResumeAstro BlackPas encore d'évaluation
- EMR Documentation TemplatesDocument25 pagesEMR Documentation TemplatesFlint Ray100% (1)
- Checklist For Physical Examination of Knee PDFDocument13 pagesChecklist For Physical Examination of Knee PDFpadmja4purohitPas encore d'évaluation
- Rheumatology Examination: Physical Examination-N ManoliosDocument7 pagesRheumatology Examination: Physical Examination-N ManoliosRohit SharmaPas encore d'évaluation
- 4.the Pathogenesis of Psoriatic ArthritisDocument12 pages4.the Pathogenesis of Psoriatic ArthritisstuckinbedPas encore d'évaluation
- Long Case OrthopaedicDocument24 pagesLong Case OrthopaedicSyimah UmarPas encore d'évaluation
- Wiki TractographyDocument4 pagesWiki TractographynsurgphotoPas encore d'évaluation
- Pelvic Fractures. Part 2. Contemporary Indications and Techniques For Definitive Surgical Management PDFDocument11 pagesPelvic Fractures. Part 2. Contemporary Indications and Techniques For Definitive Surgical Management PDFJulio Cesar Guillen MoralesPas encore d'évaluation
- Ankle Arthrodesis - Screw FixationDocument26 pagesAnkle Arthrodesis - Screw FixationChristopher HoodPas encore d'évaluation
- Aaos PDFDocument4 pagesAaos PDFWisnu CahyoPas encore d'évaluation
- Entrapmentneuropathiesof Theupperextremity: Christopher T. Doughty,, Michael P. BowleyDocument14 pagesEntrapmentneuropathiesof Theupperextremity: Christopher T. Doughty,, Michael P. BowleydwiPas encore d'évaluation
- Tannoury C Failed BackDocument24 pagesTannoury C Failed BackneareastspinePas encore d'évaluation
- Chapter 4 and 4a Introduction To Medicine and DermatologyDocument16 pagesChapter 4 and 4a Introduction To Medicine and DermatologypodmmgfPas encore d'évaluation
- Orthopedics: Notes, 1/eDocument26 pagesOrthopedics: Notes, 1/evkPas encore d'évaluation
- Aaos Pediatric 2020Document57 pagesAaos Pediatric 2020ABUBAKER ZANBOUZIPas encore d'évaluation
- Neurologic AssessmentDocument28 pagesNeurologic AssessmentJoshua KellyPas encore d'évaluation
- Advances in Spinal Stabilization PDFDocument333 pagesAdvances in Spinal Stabilization PDFMateo CortesPas encore d'évaluation
- Ficat and Arlet Staging of Avascular Necrosis of Femoral HeadDocument6 pagesFicat and Arlet Staging of Avascular Necrosis of Femoral HeadFernando Sugiarto0% (1)
- Mri Clinics - Imaging of Sports InjuriesDocument182 pagesMri Clinics - Imaging of Sports Injuriespinky003100% (2)
- Spondylolisthesis: To Reduce or Not Case Discussion: Early Onset ScoliosisDocument36 pagesSpondylolisthesis: To Reduce or Not Case Discussion: Early Onset ScoliosisneareastspinePas encore d'évaluation
- Orthopediatric LWWDocument398 pagesOrthopediatric LWWかちえ ちょうPas encore d'évaluation
- Gpe - 017.1 - Orthopaedic ExaminationDocument3 pagesGpe - 017.1 - Orthopaedic ExaminationImiey Eleena HanumPas encore d'évaluation
- Charnley Ankle ArthrodesisDocument12 pagesCharnley Ankle Arthrodesisdr_s_ganeshPas encore d'évaluation
- Roux 2013Document7 pagesRoux 2013andrew herringPas encore d'évaluation
- Buprenorphine 2016-7-18Document1 pageBuprenorphine 2016-7-18andrew herringPas encore d'évaluation
- Highland Guidelines - LDK 2013-2-15Document3 pagesHighland Guidelines - LDK 2013-2-15andrew herringPas encore d'évaluation
- K Opiods For Pain BupDocument2 pagesK Opiods For Pain Bupandrew herringPas encore d'évaluation
- Original Article: Serratus Plane Block: A Novel Ultrasound-Guided Thoracic Wall Nerve BlockDocument7 pagesOriginal Article: Serratus Plane Block: A Novel Ultrasound-Guided Thoracic Wall Nerve Blockandrew herringPas encore d'évaluation
- Rib Fracture W: PecsDocument8 pagesRib Fracture W: Pecsandrew herring100% (1)
- Rib Fracture SerratusDocument3 pagesRib Fracture Serratusandrew herring100% (1)
- Ultrasound-Guided Block of TheDocument6 pagesUltrasound-Guided Block of Theandrew herringPas encore d'évaluation
- Intravenous Lidocaine To Treat Postoperative Pain : Lidocaína Intravenosa No Tratamento Da Dor Pós-OperatóriaDocument6 pagesIntravenous Lidocaine To Treat Postoperative Pain : Lidocaína Intravenosa No Tratamento Da Dor Pós-Operatóriaandrew herringPas encore d'évaluation
- Herring ED Intractable Abdominal pain-N+VDocument1 pageHerring ED Intractable Abdominal pain-N+Vandrew herringPas encore d'évaluation
- 3.2.16.highland Emergency Medicine Journal Club Methods.2Document2 pages3.2.16.highland Emergency Medicine Journal Club Methods.2andrew herringPas encore d'évaluation
- Ketamine As Rescue Treatment FDocument8 pagesKetamine As Rescue Treatment Fandrew herringPas encore d'évaluation
- Dex For Dental Pain & SwellingDocument7 pagesDex For Dental Pain & Swellingandrew herring100% (1)
- Nej MR A 1511480Document9 pagesNej MR A 1511480Tohari Masidi AminPas encore d'évaluation
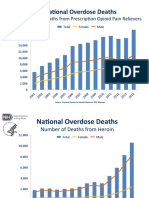
- OPR - Heroin DeathsDocument2 pagesOPR - Heroin Deathsandrew herringPas encore d'évaluation
- CVS Action Plan v2Document1 pageCVS Action Plan v2andrew herringPas encore d'évaluation
- Ultrasound Guided Interventional Procedures In.13Document14 pagesUltrasound Guided Interventional Procedures In.13andrew herring100% (1)
- Ultrasound Guided Interventional Procedures In.4Document13 pagesUltrasound Guided Interventional Procedures In.4andrew herringPas encore d'évaluation
- Cedar Crest College Clinical and Concept Map Worksheet For Nursing 330 PediatricsDocument13 pagesCedar Crest College Clinical and Concept Map Worksheet For Nursing 330 Pediatricsapi-405374041Pas encore d'évaluation
- 10 Dapat Tandaan Sa Pagsulat NG Artikulo Sa WikiFilipinoDocument2 pages10 Dapat Tandaan Sa Pagsulat NG Artikulo Sa WikiFilipinoFrancisJudeRafilPas encore d'évaluation
- Ethical Judgments Limit The Methods Available in The Production of Knowledge in Both The Arts and The Natural SciencesDocument5 pagesEthical Judgments Limit The Methods Available in The Production of Knowledge in Both The Arts and The Natural SciencesMilena ŁachPas encore d'évaluation
- Orthorexia Nervosa: HistoryDocument3 pagesOrthorexia Nervosa: HistorySimona LeafuPas encore d'évaluation
- Phylum PlatyhelminthesDocument19 pagesPhylum PlatyhelminthesBudi AfriyansyahPas encore d'évaluation
- 1 66th WHA Provisional AgendaDocument6 pages1 66th WHA Provisional AgendaRenzo R. GuintoPas encore d'évaluation
- Manila Standard Today - July 21, 2012 IssueDocument16 pagesManila Standard Today - July 21, 2012 IssueManila Standard TodayPas encore d'évaluation
- Occlusion - DevelopmentDocument33 pagesOcclusion - Developmentsameerortho100% (1)
- FRE - L3 Core Terminology - 2018Document28 pagesFRE - L3 Core Terminology - 2018RahulPas encore d'évaluation
- The Radiology AssistantDocument30 pagesThe Radiology AssistantIcha IchaPas encore d'évaluation
- Lesson Plan NutritionDocument7 pagesLesson Plan NutritionPraveenPas encore d'évaluation
- Use of Autism Diagnostic Interview1 Adi R in Clinical PracticeDocument1 pageUse of Autism Diagnostic Interview1 Adi R in Clinical Practiceaspire centerPas encore d'évaluation
- 5 Nursing Services Scheduling PolicyDocument7 pages5 Nursing Services Scheduling PolicyVin BitzPas encore d'évaluation
- Clinical Study: Overjet and Overbite Influence On Cyclic Masticatory Movements: A CT StudyDocument7 pagesClinical Study: Overjet and Overbite Influence On Cyclic Masticatory Movements: A CT Studyarya091193Pas encore d'évaluation
- Occupational Health Hazards Among Textile WorkersDocument9 pagesOccupational Health Hazards Among Textile WorkersINSTITUTE OF LEGAL EDUCATIONPas encore d'évaluation
- Toxoplasma GondiiDocument7 pagesToxoplasma GondiiDedy SavradinataPas encore d'évaluation
- Case Presentation OB - GYNDocument14 pagesCase Presentation OB - GYNRaidah Ayesha RazackPas encore d'évaluation
- Module 2 HistopathologyDocument34 pagesModule 2 HistopathologyKim RuizPas encore d'évaluation
- Dental ImplantsDocument1 pageDental ImplantsPaWan VelagaPas encore d'évaluation
- Laboratory Tests InterpretationDocument12 pagesLaboratory Tests InterpretationKaloy Kamao100% (1)
- 09 Marijuana Facts For TeensDocument24 pages09 Marijuana Facts For Teensapi-309082881Pas encore d'évaluation
- DafpusDocument1 pageDafpusJeliny Bintan MaisuriPas encore d'évaluation
- Health and WellnessDocument59 pagesHealth and Wellnessvenkata karthikPas encore d'évaluation
- Aberdeenvaricoseveinsquestionnaire PDFDocument4 pagesAberdeenvaricoseveinsquestionnaire PDFdesyislamiatiPas encore d'évaluation
- Okir A DatuDocument6 pagesOkir A DatuRonel FillomenaPas encore d'évaluation
- Hain GenoType Line Probe Assay TestDocument20 pagesHain GenoType Line Probe Assay Testpacome abdulPas encore d'évaluation
- Goat ManualDocument64 pagesGoat ManualIrfan YaqoobPas encore d'évaluation
- Ventilation: Kinematics and Kinetics.: Thorax Structure and FunctionDocument52 pagesVentilation: Kinematics and Kinetics.: Thorax Structure and FunctionAlejandra RomeroPas encore d'évaluation
- Ulibas V Republic - DigestDocument2 pagesUlibas V Republic - DigesttheamorerosaPas encore d'évaluation
- IM-Module B Summarized Notes (IBD)Document69 pagesIM-Module B Summarized Notes (IBD)DeepbluexPas encore d'évaluation