Académique Documents
Professionnel Documents
Culture Documents
2014 Passive DPPO Benefits Summary Final
Transféré par
samypalCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
2014 Passive DPPO Benefits Summary Final
Transféré par
samypalDroits d'auteur :
Formats disponibles
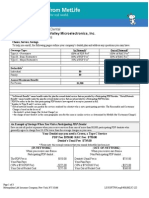
Stantec Consulting Services Inc.
Effective Date: 01-01-2014
Dental Benefits Summary
Passive PPO
With PPOII Network
Annual Deductible*
Individual
Family
Preventive Services
Basic Services
Major Services
Annual Benefit Maximum
Orthodontic Services (Adult and Child)
Orthodontic Deductible
Orthodontic Lifetime Maximum
*The deductible applies to: Basic & Major services only
Partial List of Services
$50
$150
100%
80%
50%
$2,000
50%
None
$2,500
Passive PPO
With PPOII Network
Preventive
Oral examinations (a)
Cleanings (a) Adult/Child
Fluoride (a)
Sealants (permanent molars only) (a)
Bitewing Images (a)
Full mouth series Images (a)
Space Maintainers
Basic
Root canal therapy
Anterior teeth / Bicuspid teeth
Root canal therapy, molar teeth
Scaling and root planing (a)
Gingivectomy*
Amalgam (silver) fillings
Composite fillings (anterior teeth only)
Stainless steel crowns
Incision and drainage of abscess*
Uncomplicated extractions
Surgical removal of erupted tooth*
Surgical removal of impacted tooth (soft tissue)*
Osseous surgery (a)*
Surgical removal of impacted tooth (partial bony/ full bony)*
General anesthesia/intravenous sedation*
Crown Lengthening
Major
Inlays
Onlays
Crowns
Full & partial dentures
Pontics
Denture repairs
Crown Build-Ups
Implants
Occlusal/Mouth Guards
100%
100%
100%
100%
100%
100%
100%
80%
80%
80%
80%
80%
80%
80%
80%
80%
80%
80%
80%
80%
80%
80%
50%
50%
50%
50%
50%
50%
50%
50%
50%
*Certain services may be covered under the Medical Plan. Contact Member Services for more details.
(a) Frequency and/or age limitations may apply to these services. These limits are described in the booklet/certificate.
Page: 1
Prepared: 05/15/2013 11:47 AM
Stantec Consulting Services Inc.
Effective Date: 01-01-2014
Dental Benefits Summary
Passive PPO
Other Important Information
This Aetna Dental Preferred Provider Organization (PPO) benefits summary is provided by Aetna Life Insurance Company for
some of the more frequently performed dental procedures. Under the Dental Preferred Provider Organization (PPO) plan, you
may choose at the time of service either a PPO participating dentist or any nonparticipating dentist. With the PPO plan,
savings are possible because the participating dentists have agreed to provide care for covered services at negotiated rates.
Non-participating benefits are subject to usual and prevailing charge limits, as determined by Aetna.
Emergency Dental Care
If you need emergency dental care for the palliative treatment (pain relieving, stabilizing) of a dental emergency, you are
covered 24 hours a day, 7 days a week.
When emergency services are provided by a participating PPO dentist, your co-payment/coinsurance amount will be based on
a negotiated fee schedule. When emergency services are provided by a non-participating dentist, you will be responsible for
the difference between the plan payment and the dentist's usual charge. Refer to your plan documents for details. Subject to
state requirements. Out-of-area emergency dental care may be reviewed by our dental consultants to verify appropriateness of
treatment.
Partial List of Exclusions and Limitations* - Coverage is not provided for the following:
1. Services or supplies that are covered in whole or in part:
(a) under any other part of this Dental Care Plan; or
(b) under any other plan of group benefits provided by or through your employer.
2. Services and supplies to diagnose or treat a disease or injury that is not:
(a) a non-occupational disease; or
(b) a non-occupational injury.
3. Services not listed in the Dental Care Schedule that applies, unless otherwise specified in the Booklet-Certificate.
4. Those for replacement of a lost, missing or stolen appliance, and those for replacement of appliances that have been
damaged due to abuse, misuse or neglect.
5. Those for plastic, reconstructive or cosmetic surgery, or other dental services or supplies, that are primarily intended to
improve, alter or enhance appearance. This applies whether or not the services and supplies are for psychological or
emotional reasons. Facings on molar crowns and pontics will always be considered cosmetic.
6. Those for or in connection with services, procedures, drugs or other supplies that are determined by Aetna to be
experimental or still under clinical investigation by health professionals.
7. Those for dentures, crowns, inlays, onlays, bridgework, or other appliances or services used for the purpose of splinting, to
alter vertical dimension, to restore occlusion, or to correct attrition, abrasion or erosion.
8. Those for any of the following services (Does not apply to the DMO plan in TX):
(a) an appliance or modification of one if an impression for it was made before the person became a covered person;
(b) a crown, bridge, or cast or processed restoration if a tooth was prepared for it before the person became a covered
person; or
(c) root canal therapy if the pulp chamber for it was opened before the person became a covered person.
9. Services that Aetna defines as not necessary for the diagnosis, care or treatment of the condition involved. This applies
even if they are prescribed, recommended or approved by the attending physician or dentist.
10. Those for services intended for treatment of any jaw joint disorder, unless otherwise specified in the Booklet-Certificate.
11. Those for space maintainers, except when needed to preserve space resulting from the premature loss of deciduous teeth.
12. Those for orthodontic treatment, unless otherwise specified in the Booklet-Certificate.
13. Those for general anesthesia and intravenous sedation, unless specifically covered. For plans that cover these services,
they will not be eligible for benefits unless done in conjunction with another necessary covered service.
14. Those for treatment by other than a dentist, except that scaling or cleaning of teeth and topical application of fluoride may
be done by a licensed dental hygienist. In this case, the treatment must be given under the supervision and guidance of a
dentist.
15. Those in connection with a service given to a person age 5 or older if that person becomes a covered person other than:
(a) during the first 31 days the person is eligible for this coverage, or
(b) as prescribed for any period of open enrollment agreed to by the employer and Aetna. This does not apply to charges
incurred:
(i) after the end of the 12-month period starting on the date the person became a covered person; or
(ii) as a result of accidental injuries sustained while the person was a covered person; or
(iii) for a primary care service in the Dental Care Schedule that applies as shown under the headings Visits and
Exams, and X-rays and Pathology.
Page: 2
Prepared: 05/15/2013 11:47 AM
Stantec Consulting Services Inc.
Effective Date: 01-01-2014
Dental Benefits Summary
PPO
16. Services given by a nonparticipating dental provider to the extent that the charges exceed Passive
the amount
payable for the
services shown in the Dental Care Schedule that applies.
17. Those for a crown, cast or processed restoration unless:
(a) it is treatment for decay or traumatic injury, and teeth cannot be restored with a filling material; or
(b) the tooth is an abutment to a covered partial denture or fixed bridge.
18. Those for pontics, crowns, cast or processed restorations made with high-noble metals, unless otherwise specified in the
Booklet-Certificate.
19. Those for surgical removal of impacted wisdom teeth only for orthodontic reasons, unless otherwise specified in the
Booklet-Certificate.
20. Services needed solely in connection with non-covered services.
21. Services done where there is no evidence of pathology, dysfunction or disease other than covered preventive services.
Any exclusion above will not apply to the extent that coverage of the charges is required under any law that applies to the
coverage.
*This is a partial list of exclusions and limitations, others may apply. Please check your plan booklet for details.
Your Dental Care Plan Coverage Is Subject to the Following Rules:
Replacement Rule
The replacement of; addition to; or modification of: existing dentures; crowns; casts or processed restorations; removable
denture; fixed bridgework; or other prosthetic services is covered only if one of the following terms is met:
The replacement or addition of teeth is required to replace one or more teeth extracted after the existing denture or
bridgework was installed. This coverage must have been in force for the covered person when the extraction took place.
The existing denture, crown; cast or processed restoration, removable denture, bridgework, or other prosthetic service cannot
be made serviceable, and was installed at least 8 years before its replacement.
The existing denture is an immediate temporary one to replace one or more natural teeth extracted while the person is covered,
and cannot be made permanent, and replacement by a permanent denture is required. The replacement must take place within
12 months from the date of initial installation of the immediate temporary denture.
The extraction of a third molar does not qualify. Any such appliance or fixed bridge must include the replacement of an
extracted tooth or teeth.
Tooth Missing But Not Replaced Rule
Coverage for the first installation of removable dentures; fixed bridgework and other prosthetic services is subject to the
requirements that such removable dentures; fixed bridgework and other prosthetic services are (i) needed to replace one or
more natural teeth that were removed while this policy was in force for the covered person; and (ii) are not abutments to a
partial denture; removable bridge; or fixed bridge installed during the prior 8 years.
Alternate Treatment Rule: If more than one service can be used to treat a covered persons dental condition, Aetna may decide
to authorize coverage only for a less costly covered service provided that all of the following terms are met:
(a) the service must be listed on the Dental Care Schedule;
(b) the service selected must be deemed by the dental profession to be an appropriate method of treatment; and
(c) the service selected must meet broadly accepted national standards of dental practice.
If treatment is being given by a participating dental provider and the covered person asks for a more costly covered service
than that for which coverage is approved, the specific copayment for such service will consist of:
(a) the copayment for the approved less costly service; plus
(b) the difference in cost between the approved less costly service and the more costly covered service.
Finding Participating Providers
Consult Aetna Dentals online provider directory, DocFind, for the most current provider listings. Participating providers are
independent contractors in private practice and are neither employees nor agents of Aetna Dental or its affiliates. The
availability of any particular provider cannot be guaranteed, and provider network composition is subject to change without
notice. For the most current information, please contact the selected provider or Aetna Member Services at the toll-free number
on your ID card, or use our Internet-based provider directory (DocFind) available at www.aetna.com.
Specific products may not be available on both a self-funded and insured basis. The information in this document is subject to
change without notice. In case of a conflict between your plan documents and this information, the plan documents will govern.
In the event of a problem with coverage, members should contact Member Services at the toll-free number on their ID cards for
information on how to utilize the grievance procedure when appropriate.
All member care and related decisions are the sole responsibility of participating providers. Aetna Dental does not provide
health care services and, therefore, cannot guarantee any results or outcomes.
Page: 3
Prepared: 05/15/2013 11:47 AM
Stantec Consulting Services Inc.
Effective Date: 01-01-2014
Dental Benefits Summary
Passive
PPO of California Inc.
Dental plans are provided or administered by Aetna Life Insurance Company, Aetna Dental Inc.,
Aetna Dental
and/or Aetna Health Inc.
This material is for informational purposes only and is neither an offer of coverage nor dental advice. It contains only a partial,
general description of plan or program benefits and does not constitute a contract. The availability of a plan or program may
vary by geographic service area. Certain dental plans are available only for groups of a certain size in accordance with
underwriting guidelines. Some benefits are subject to limitations or exclusions. Consult the plan documents (Schedule of
Benefits, Certificate/Evidence of Coverage, Booklet, Booklet-Certificate, Group Agreement, Group Policy) to determine
governing contractual provisions, including procedures, exclusions and limitations relating to your plan.
Page: 4
Prepared: 05/15/2013 11:47 AM
Vous aimerez peut-être aussi
- The Dental Assistant's Guide: Mastering Dental Care ExcellenceD'EverandThe Dental Assistant's Guide: Mastering Dental Care ExcellencePas encore d'évaluation
- BlueDental Copayment QF Plan BrochureDocument4 pagesBlueDental Copayment QF Plan BrochureJoshua JohnsonPas encore d'évaluation
- Dental Implant Treatment Planning for New Dentists Starting Implant TherapyD'EverandDental Implant Treatment Planning for New Dentists Starting Implant TherapyÉvaluation : 4 sur 5 étoiles4/5 (1)
- Member Care: Your Plan Includes Access To 3 National Networks: Dentemax, Careington & Connection DentalDocument2 pagesMember Care: Your Plan Includes Access To 3 National Networks: Dentemax, Careington & Connection DentalClari HerreraPas encore d'évaluation
- The Complete Guide to Dental Implants: All About DentistryD'EverandThe Complete Guide to Dental Implants: All About DentistryPas encore d'évaluation
- Removable Prosthodontics: Instructions For UseDocument6 pagesRemovable Prosthodontics: Instructions For UseYuaninda FajarinPas encore d'évaluation
- Orthodontic CDTDocument2 pagesOrthodontic CDTnaharmampillyPas encore d'évaluation
- Dental InsuranceDocument4 pagesDental InsuranceJason100% (1)
- AAA Consent FormDocument3 pagesAAA Consent FormAlex LamPas encore d'évaluation
- 2015-16 Delta PPO Plan HighlightsDocument2 pages2015-16 Delta PPO Plan HighlightsamberarunPas encore d'évaluation
- Orthodontic Contract and Consent Form PDFDocument6 pagesOrthodontic Contract and Consent Form PDFjack100% (1)
- Humana Dental BrochureDocument4 pagesHumana Dental BrochureJeffrey PowellPas encore d'évaluation
- Go Smile Dental Clinic - Pcpi ProposalDocument4 pagesGo Smile Dental Clinic - Pcpi ProposalRosette GoPas encore d'évaluation
- English Free Whitening For Life Contract v2Document2 pagesEnglish Free Whitening For Life Contract v2api-295067164Pas encore d'évaluation
- Our Dental Plan For Individuals and FamiliesDocument4 pagesOur Dental Plan For Individuals and Familiesapi-41207808Pas encore d'évaluation
- Peace Corps Office of Medical Services Dental Technical Guideline 180 - Dental PolicyDocument8 pagesPeace Corps Office of Medical Services Dental Technical Guideline 180 - Dental PolicyAccessible Journal Media: Peace Corps DocumentsPas encore d'évaluation
- Guidelines 1Document2 pagesGuidelines 1Rajah KanoPas encore d'évaluation
- Dental Insurance Policy-WordingDocument10 pagesDental Insurance Policy-WordingAnthony GuoPas encore d'évaluation
- Metlife - Dental Ppo 12 15Document3 pagesMetlife - Dental Ppo 12 15api-252555369Pas encore d'évaluation
- Budget Hospital and General Extras Plus Product SummaryDocument4 pagesBudget Hospital and General Extras Plus Product SummaryJames SandersPas encore d'évaluation
- From Medicare Benefits ManualDocument3 pagesFrom Medicare Benefits ManualSam AntoniosPas encore d'évaluation
- Dental Prosthesis Package ContractDocument3 pagesDental Prosthesis Package ContractRostum AgapitoPas encore d'évaluation
- 2003 Delta SumDocument1 page2003 Delta SumbpracticalPas encore d'évaluation
- The Canadian Forces Dental Care PlanDocument12 pagesThe Canadian Forces Dental Care PlanAshley MarkPas encore d'évaluation
- Dental Option 1Document2 pagesDental Option 10pt618Pas encore d'évaluation
- Consent FormDocument3 pagesConsent Form82cristi82Pas encore d'évaluation
- Unitedhealthcare Dental Dental Glossary of TermsDocument1 pageUnitedhealthcare Dental Dental Glossary of TermsDarshilPas encore d'évaluation
- Dentistry-Informed Consent For Orthodontic Treatment-MedPro GroupDocument3 pagesDentistry-Informed Consent For Orthodontic Treatment-MedPro Groupednrg123Pas encore d'évaluation
- LEC 12 Dental AuxiliaryDocument9 pagesLEC 12 Dental Auxiliaryطيبة نعمانPas encore d'évaluation
- Dental Blue Program 2: (With Orthodontics)Document5 pagesDental Blue Program 2: (With Orthodontics)Cande ArPas encore d'évaluation
- Informed Consent For Crown and Bridge ProstheticsDocument3 pagesInformed Consent For Crown and Bridge ProstheticsVikkii VeerakumarPas encore d'évaluation
- (20120228110933 Am) Samwumed Benefitsbrochure2012 WebDocument16 pages(20120228110933 Am) Samwumed Benefitsbrochure2012 WebsafinditPas encore d'évaluation
- Dental 06102011Document2 pagesDental 06102011Lisa HendersonPas encore d'évaluation
- Young Singles and Couples Product Summary: You Get With HCFDocument4 pagesYoung Singles and Couples Product Summary: You Get With HCFJames SandersPas encore d'évaluation
- Hpdai Standard SvcsDocument14 pagesHpdai Standard SvcsSHNN CLMLMPas encore d'évaluation
- Six Month Smiles Consent FormDocument3 pagesSix Month Smiles Consent Formabarbel1Pas encore d'évaluation
- Medical Coding For Dental PracticesDocument15 pagesMedical Coding For Dental Practicesghassan ahmedPas encore d'évaluation
- Dental Implants PDFDocument2 pagesDental Implants PDFJudy CarterPas encore d'évaluation
- Periodontal Profit Center ProjectDocument9 pagesPeriodontal Profit Center Projectapi-643485887Pas encore d'évaluation
- Integrating Orthodontics Into General Dental Practice A Starter Guide LDiDocument16 pagesIntegrating Orthodontics Into General Dental Practice A Starter Guide LDiNurmaira JayantiPas encore d'évaluation
- Cover For Dental TreatmentDocument14 pagesCover For Dental TreatmentLil JLazzyPas encore d'évaluation
- Dental Act 2018Document110 pagesDental Act 2018copyourpairPas encore d'évaluation
- Med 2Document2 pagesMed 2api-259279833Pas encore d'évaluation
- Dental Form DD 2813Document1 pageDental Form DD 2813Harvey A TolleyPas encore d'évaluation
- Kaiser Permanente California Dental Insurance Plan Brochure KPIF 2011Document2 pagesKaiser Permanente California Dental Insurance Plan Brochure KPIF 2011Dennis100% (1)
- GDC Training Standards in Implant DentistryDocument9 pagesGDC Training Standards in Implant Dentistrylg_1234Pas encore d'évaluation
- C550 Humana Dentral PlanDocument22 pagesC550 Humana Dentral Plananguyen22153319Pas encore d'évaluation
- Dental ImplantDocument2 pagesDental ImplantUmair RizwanPas encore d'évaluation
- Immediate DenturesDocument35 pagesImmediate DenturesPrince AhmedPas encore d'évaluation
- Keep Smiling: Delta Dental PPO™Document2 pagesKeep Smiling: Delta Dental PPO™olimaziPas encore d'évaluation
- HCF - Top PlusDocument14 pagesHCF - Top PluscraivaimPas encore d'évaluation
- Consent For Complete DenturesDocument2 pagesConsent For Complete DenturesPulkit Kinra100% (1)
- Slater Inc Dental EnglishDocument4 pagesSlater Inc Dental Englishapi-531507901Pas encore d'évaluation
- CD Dental Implant Consent Form PDFDocument3 pagesCD Dental Implant Consent Form PDFMuaiyed Buzayan AkremyPas encore d'évaluation
- GDC Scope of PracticeDocument4 pagesGDC Scope of Practicesam paulPas encore d'évaluation
- Orthodontic Consent FormDocument12 pagesOrthodontic Consent FormMahardika Dyah KumalasariPas encore d'évaluation
- Locum Tenens Guide - 080123Document6 pagesLocum Tenens Guide - 080123Tom ThumbPas encore d'évaluation
- Informed Consent For The Orthodontic Patient: Consent of Orthodontic Treatment Provided by DR Mohammed AlmuzianDocument8 pagesInformed Consent For The Orthodontic Patient: Consent of Orthodontic Treatment Provided by DR Mohammed AlmuzianVidal Almanza AvilaPas encore d'évaluation
- Perio Profit CenterDocument21 pagesPerio Profit Centerapi-643485887Pas encore d'évaluation
- Guide DentalBenefits2017 2.7Document10 pagesGuide DentalBenefits2017 2.7naharmampillyPas encore d'évaluation
- Electrochimica Acta: Ramasamy Palaniappan, Gerardine G. BotteDocument10 pagesElectrochimica Acta: Ramasamy Palaniappan, Gerardine G. BottesamypalPas encore d'évaluation
- OrthoAminoPhenol EIS StudiesDocument5 pagesOrthoAminoPhenol EIS StudiessamypalPas encore d'évaluation
- Propiedades ColigativasDocument12 pagesPropiedades Coligativaschigui1Pas encore d'évaluation
- Make A Payment Confirmation - CitibankDocument1 pageMake A Payment Confirmation - CitibanksamypalPas encore d'évaluation
- Propiedades ColigativasDocument12 pagesPropiedades Coligativaschigui1Pas encore d'évaluation
- Effect of Ammonia On PT, Ru, RH, and Ni Cathodes During The Alkaline Hydrogen Evolution ReactionDocument13 pagesEffect of Ammonia On PT, Ru, RH, and Ni Cathodes During The Alkaline Hydrogen Evolution ReactionsamypalPas encore d'évaluation
- Partial Differential Equations in MATLABDocument23 pagesPartial Differential Equations in MATLABAsterix100% (20)
- Newton's Law Proportionality Constant (G Sub C GC) - University Institute of Pharmaceutical Sciences, PUCHDDocument3 pagesNewton's Law Proportionality Constant (G Sub C GC) - University Institute of Pharmaceutical Sciences, PUCHDsamypalPas encore d'évaluation
- Resume SamyPal 2015Document2 pagesResume SamyPal 2015samypal100% (1)
- A Simple Model For Estimation of Methanol Loss To Vapor PhaseDocument10 pagesA Simple Model For Estimation of Methanol Loss To Vapor PhasesamypalPas encore d'évaluation
- CASACWEABisolidsWorkshopFINAL4 1 15Document3 pagesCASACWEABisolidsWorkshopFINAL4 1 15samypalPas encore d'évaluation
- Corrosion Scientist - Refining 12716BR: Position DescriptionDocument9 pagesCorrosion Scientist - Refining 12716BR: Position DescriptionsamypalPas encore d'évaluation
- CV SamyPal 2015 ForReviewer May2015Document4 pagesCV SamyPal 2015 ForReviewer May2015samypalPas encore d'évaluation
- Cleaning and Decon For Ebola ResponseDocument4 pagesCleaning and Decon For Ebola ResponsesamypalPas encore d'évaluation
- Separation EfficiencyDocument4 pagesSeparation EfficiencysamypalPas encore d'évaluation
- Project Assessment Form Rev. 1Document2 pagesProject Assessment Form Rev. 1samypalPas encore d'évaluation
- Right Weight Week 1Document8 pagesRight Weight Week 1samypalPas encore d'évaluation
- 2013 RW Book - Intro and Week 0Document11 pages2013 RW Book - Intro and Week 0samypalPas encore d'évaluation
- Soda Ash Storage HandlingDocument26 pagesSoda Ash Storage Handlingsamypal100% (2)
- NIOSH Medical Emergency Response KitDocument100 pagesNIOSH Medical Emergency Response KitsamypalPas encore d'évaluation
- 2013 RW Book - Intro and Week 0Document11 pages2013 RW Book - Intro and Week 0samypalPas encore d'évaluation
- Curriculum VitaeDocument4 pagesCurriculum VitaesamypalPas encore d'évaluation
- CNG MsdsDocument2 pagesCNG MsdssamypalPas encore d'évaluation
- Pump Curve ExampleDocument7 pagesPump Curve ExamplesamypalPas encore d'évaluation
- Electrolyte (21 New)Document21 pagesElectrolyte (21 New)samypalPas encore d'évaluation
- Instrument AbbreviationsDocument3 pagesInstrument AbbreviationssamypalPas encore d'évaluation
- CSTR Energy Balance PDFDocument182 pagesCSTR Energy Balance PDFfasdasd123Pas encore d'évaluation
- Park MapDocument1 pagePark MapsamypalPas encore d'évaluation
- WEEK13 PicksDocument1 pageWEEK13 PickssamypalPas encore d'évaluation
- - الملف الذهبي رقم 1+2 CorrectedDocument49 pages- الملف الذهبي رقم 1+2 Correctedmohammed alsaad100% (1)
- Significance of The Cant of The Posterior Occlusal Plane in Class II Division 1 MalocclusionsDocument14 pagesSignificance of The Cant of The Posterior Occlusal Plane in Class II Division 1 MalocclusionsHoàng Đức TháiPas encore d'évaluation
- Ijed 2022 03 s0340CracksGerdolleBrowetDocument17 pagesIjed 2022 03 s0340CracksGerdolleBrowetkhaled emadPas encore d'évaluation
- OptraSculpt Pad PDFDocument2 pagesOptraSculpt Pad PDFSharmaine JucoPas encore d'évaluation
- Systematic Review of Lithium Disilicate MaterialsDocument9 pagesSystematic Review of Lithium Disilicate Materialscarolina_indian100% (1)
- 3 Practical Procedures in The Management of Tooth WearDocument238 pages3 Practical Procedures in The Management of Tooth WearMarius GrigorasPas encore d'évaluation
- Flouride Relessing Material-FinalDocument95 pagesFlouride Relessing Material-FinalDr. Nikhil saranPas encore d'évaluation
- Clear Aligners Generations and Orthodontic Tooth Movement: Journal of OrthodonticsDocument10 pagesClear Aligners Generations and Orthodontic Tooth Movement: Journal of OrthodonticsTanushree JainPas encore d'évaluation
- Rely X Luting 2Document32 pagesRely X Luting 2Muhammad Boggi RiswantoPas encore d'évaluation
- Apr 4Document2 pagesApr 4Rambabu SatipedakalaPas encore d'évaluation
- Diagnosis and Treatment Planning in FPDDocument46 pagesDiagnosis and Treatment Planning in FPDSujanaPas encore d'évaluation
- Management of Root FractureDocument61 pagesManagement of Root FractureVăn Trọng MinhPas encore d'évaluation
- IMPLANTS Diagnosis & Treatment PlanningDocument40 pagesIMPLANTS Diagnosis & Treatment Planningneethu67% (3)
- The Frequency of Dental Caries in Adult Patients With Gastroesophageal Reflux DiseaseDocument4 pagesThe Frequency of Dental Caries in Adult Patients With Gastroesophageal Reflux DiseasefdhfuwhuPas encore d'évaluation
- Stress BreakersDocument7 pagesStress BreakerssavyasachinPas encore d'évaluation
- A Technique For Digital Impression and Bite Registration For A Single Edentulous ArchDocument5 pagesA Technique For Digital Impression and Bite Registration For A Single Edentulous ArchsaniaPas encore d'évaluation
- Diseases of The PulpDocument1 pageDiseases of The PulpFidz LiankoPas encore d'évaluation
- Maxicare Benefits and Coverage PDFDocument16 pagesMaxicare Benefits and Coverage PDFRZ Zamora43% (7)
- Brochure GC Fuji IX FamilyDocument4 pagesBrochure GC Fuji IX FamilyIka Kusumawati100% (1)
- Forensic OdontologyDocument28 pagesForensic Odontologydinesh11rPas encore d'évaluation
- Theme 2 - Partial Acrylic Removable Denture: Maxilla LimitsDocument3 pagesTheme 2 - Partial Acrylic Removable Denture: Maxilla LimitsShany SchwarzwaldPas encore d'évaluation
- Distribution Channel For ColgateDocument2 pagesDistribution Channel For ColgateAbcdePas encore d'évaluation
- Normal Occlusion: Presented By: DR Ghulam RasoolDocument41 pagesNormal Occlusion: Presented By: DR Ghulam RasoolAbdul MohaiminPas encore d'évaluation
- ADA Guidelines Dental RecordsDocument10 pagesADA Guidelines Dental RecordsNikitha KanithiPas encore d'évaluation
- Catalogue Laboratory Products - Heraeus KulzerDocument288 pagesCatalogue Laboratory Products - Heraeus KulzerDentaDentPas encore d'évaluation
- Classification and Impression Techniques of ImplantsDocument72 pagesClassification and Impression Techniques of ImplantsvanillalavenderPas encore d'évaluation
- Section 032 RPD ImpressionsDocument3 pagesSection 032 RPD Impressionsapi-3710948Pas encore d'évaluation
- 1 4988197119476105255 PDFDocument171 pages1 4988197119476105255 PDFParneetPas encore d'évaluation
- Determination of Fluoride Release and Strength of A Fluoride Treated Heat Cured Acrylic ResinDocument5 pagesDetermination of Fluoride Release and Strength of A Fluoride Treated Heat Cured Acrylic ResinSaatvik AtriPas encore d'évaluation
- Qualifying Examination PolicyDocument5 pagesQualifying Examination PolicyLaila LailaPas encore d'évaluation
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsD'EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsPas encore d'évaluation
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisD'EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisÉvaluation : 4.5 sur 5 étoiles4.5/5 (42)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeD'EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeÉvaluation : 2 sur 5 étoiles2/5 (1)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsD'EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsÉvaluation : 5 sur 5 étoiles5/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityD'EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityÉvaluation : 4 sur 5 étoiles4/5 (24)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedD'EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedÉvaluation : 5 sur 5 étoiles5/5 (80)
- The Comfort of Crows: A Backyard YearD'EverandThe Comfort of Crows: A Backyard YearÉvaluation : 4.5 sur 5 étoiles4.5/5 (23)
- The Obesity Code: Unlocking the Secrets of Weight LossD'EverandThe Obesity Code: Unlocking the Secrets of Weight LossÉvaluation : 4 sur 5 étoiles4/5 (6)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaD'EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsD'EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsÉvaluation : 4.5 sur 5 étoiles4.5/5 (169)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDD'EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDÉvaluation : 5 sur 5 étoiles5/5 (1)
- Why We Die: The New Science of Aging and the Quest for ImmortalityD'EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityÉvaluation : 4 sur 5 étoiles4/5 (3)
- Gut: the new and revised Sunday Times bestsellerD'EverandGut: the new and revised Sunday Times bestsellerÉvaluation : 4 sur 5 étoiles4/5 (392)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeD'EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeÉvaluation : 4.5 sur 5 étoiles4.5/5 (253)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsD'EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsÉvaluation : 3.5 sur 5 étoiles3.5/5 (3)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisD'EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisÉvaluation : 3.5 sur 5 étoiles3.5/5 (2)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningD'EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningÉvaluation : 4 sur 5 étoiles4/5 (3)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.D'EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Évaluation : 4.5 sur 5 étoiles4.5/5 (110)
- To Explain the World: The Discovery of Modern ScienceD'EverandTo Explain the World: The Discovery of Modern ScienceÉvaluation : 3.5 sur 5 étoiles3.5/5 (51)
- An Autobiography of Trauma: A Healing JourneyD'EverandAn Autobiography of Trauma: A Healing JourneyÉvaluation : 5 sur 5 étoiles5/5 (2)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessD'EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessÉvaluation : 4.5 sur 5 étoiles4.5/5 (328)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisD'EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisÉvaluation : 4 sur 5 étoiles4/5 (1)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryD'EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryÉvaluation : 4 sur 5 étoiles4/5 (44)
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisD'EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisÉvaluation : 4 sur 5 étoiles4/5 (9)