Académique Documents
Professionnel Documents
Culture Documents
Velopharyngeal Incompetence: A Guide For Clinical Evaluation
Transféré par
ahmedatefTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Velopharyngeal Incompetence: A Guide For Clinical Evaluation
Transféré par
ahmedatefDroits d'auteur :
Formats disponibles
CME
Velopharyngeal Incompetence: A Guide for
Clinical Evaluation
Donnell F. Johns, Ph.D., Rod J. Rohrich, M.D., and Mariam Awada, M.D.
Dallas, Texas
Learning Objectives: After studying this article, the participant should be able to: 1. Understand the mechanism of speech
production. 2. Recognize the specific cause of a speech abnormality (structural deficit, neurogenic deficit, misarticulation,
or mechanical interference). 3. Perform a thorough clinical assessment using an intraoral examination and speech
production analysis. 4. Understand the advantages and disadvantages of various types of instrumental modalities and their
specific indications in diagnosing speech abnormalities.
Various causes of velopharyngeal disorders and the
myriad of diagnostic methods used by speech-language
pathologists and plastic surgeons for assessment are described in this article. Velopharyngeal incompetence occurs when the velum and lateral and posterior pharyngeal
walls fail to separate the oral cavity from the nasal cavity
during speech and deglutination. The functional goals of
cleft palate operations are to facilitate normal speech and
hearing without interfering with the facial growth of a
child. Basic and helpful techniques are presented to help
the cleft palate team identify preoperative or postoperative velopharyngeal incompetence. This information will
enable any member of the multidisciplinary cleft palate
team to better assist in the differential diagnosis and management of patients with speech disorders. (Plast. Reconstr. Surg. 112: 1890, 2003.)
pose of this article is to describe the various
causes of velopharyngeal disorders and the
myriad of diagnostic methods used by speechlanguage pathologists and plastic surgeons for
assessment. This will enable any member of the
multidisciplinary cleft palate team to better assist in the differential diagnosis and management of patients with speech disorders.
Velopharyngeal closure refers to the normal
apposition of the soft palate, or velum, with the
posterior and lateral pharyngeal walls.1218 It is
primarily a sphincteric mechanism consisting
of a velar component and a pharyngeal component. Movement of the velar component is
produced principally by the action of the levator veli palatini muscle. Movement of the pharyngeal component is more dependent on the
contraction of the superior constrictor muscle
and the palatopharyngeal muscles. The upward and backward movement of the velum,
coupled with the mesial movement of the lateral pharyngeal walls and the slight anterior
movement of the posterior pharyngeal walls (at
the level of the first cervical vertebra), separates the oral cavity from the nasal cavity during deglutination and speech. Velopharyngeal
incompetence occurs when the velum and lateral and posterior pharyngeal walls fail to separate the oral cavity from the nasal cavity during speech and deglutination.
The functional goals of cleft palate surgery
are to facilitate normal speech and hearing
without interfering with the facial growth of a
child. Unfortunately, after primary palatoplasty, up to 20 percent of patients have unsatisfactory speech results and require secondary
management because of insufficient velopharyngeal closure.111 The speech-language pathologist plays a vital role in identifying this
group of patients. With early recognition and
intervention, the chances for development of
normal speech and hearing are increased. Further, the specific treatment plan and surgical
procedure will be based on the causes of the
inadequate velopharyngeal closure. The pur-
From the Department of Plastic Surgery, University of Texas Southwestern Medical Center. Received for publication April 24, 2003; revised
May 30, 2003.
DOI: 10.1097/01.PRS.0000091245.32905.D5
1890
Vol. 112, No. 7 /
1891
EVALUATING VELOPHARYNGEAL INCOMPETENCE
ETIOLOGY
Different nomenclature exists that attempts
to describe subgroups of velopharyngeal disorders based on etiology. We prefer the use of a
single generic term, velopharyngeal incompetence, to denote any type of abnormal velopharyngeal function in which the velum and lateral and posterior pharyngeal walls fail to
separate the oral cavity from the nasal cavity.
The etiology of velopharyngeal incompetence
includes structural deficits, neurogenic impairment, and mechanical interference to velopharyngeal closure.19 30
Of particular concern to the craniofacial surgeon is velopharyngeal incompetence occurring in patients with cleft palate secondary to a
structural deficit of the velum or pharyngeal
walls at the level of the nasopharynx with insufficient tissue to accomplish closure. Structural congenital defects include gross tissue
deficiency, submucous or overt unoperated
clefts, a short or immobile soft palate, a large
and deep nasopharynx, or a palatal fistula.
Velopharyngeal incompetence may also be acquired due to anatomic pathology as a result of
cancer treatment or maxillofacial trauma.
Similarly, neurogenic impairment can result
in partial or total immobility of the soft palate
and/or pharyngeal walls and lead to velopharyngeal incompetence. This neurogenic, impaired velopharyngeal valve closure will produce dysarthric speech. Protective and
reflexive acts such as gagging and swallowing
may be impaired depending on the nature and
the level of the lesion. Velopharyngeal incompetence secondary to a neurogenic deficit may
be congenital, although it is most often acquired after trauma. The disturbance in
speech production is caused by a weakness,
paralysis, or a lack of coordination of speech
musculature. The injury may be localized to
cranial nerves IX, X, or XI, lower motor nerves,
upper motor nerves, and/or the cerebellum.
The localization and severity of the impairment will dictate whether speech intelligibility
will improve with velopharyngeal valve
remediation.
Velopharyngeal incompetence may also be
present secondary to mechanical interference
with the velopharyngeal valve closure. For example, severely hypertrophied tonsils can
cause a mechanical interference resulting in
incomplete valve closure. Similarly, an exces-
sively wide pharyngeal flap may inhibit apposition of the velum with the pharyngeal walls.
Misarticulations may present in a manner
similar to that seen in velopharyngeal incompetence.3133 Phoneme-specific misarticulations
refer to the occurrence of nasal emission on
certain (but not all) pressure consonants in the
absence of any hypernasal resonance. Fricatives (s, z) and affricates (ts, dz) are most vulnerable to this type of misarticulation. Recognizing this selective phoneme emission is
crucial in identifying the cause of articular impairment in patients with inconsistent nasal
emission, since a resonance disorder does not
exist.
VELOPHARYNGEAL FUNCTION
The ability to achieve properly articulated
speech pivots on the dynamic interaction of
the palatal and pharyngeal wall musculature,
which is driven by neural pathways to constrict
the velopharyngeal portal. Because the entire
vocal tract is a resonating cavity, coupling and
uncoupling of the nasal and oral cavity are
necessary to produce various sounds and intelligible speech. The velum and pharynx act as a
valve that selectively channels airflow and
acoustic energy under different pressures into
the oral and nasal cavities. To produce nasal
sounds (m, n, ng), the velopharyngeal valve
channels airflow to the nasal cavity. Similarly,
for the oral sounds (all vowels and remaining
consonants), the valve closes off the nasal cavity and selectively transmits airflow and energy
through the oral cavity. Thus, for normal
speech, one must have rapid and competent
velopharyngeal function in addition to being
able to produce appropriate airflow and adequate pressure. With competent velopharyngeal valving, a pressure column of exhaled air
is shared with the oral cavity, where interrelating tongue, palatine shelves, dentition, and lips
fashion the various sound waves. Combined
intermittently with nasal resonance, these
sound waves characterize human speech.
Abnormal resonance can result from previously described structural, neurogenic, physiologic, or mechanical impairment. When the
normal space relationship or coupling between
the velum and nasopharynx is disturbed, velopharyngeal incompetence results. This produces three common speech characteristics
secondary to increased transmission through
the nasal cavity: hypernasality, nasal emission,
and reduced aspiration and frication. Hyper-
1892
PLASTIC AND RECONSTRUCTIVE SURGERY,
nasality is secondary to excess nasal resonance
(particularly with vowel production) just as turbulent airflow through the nasal cavity is responsible for nasal emission. On the other
hand, stop plosives and fricatives are secondary
to a leak, which prohibits the accumulation of
sufficient oral pressures.
EVALUATION
OF
VELOPHARYNGEAL ACTIVITY
Two types of evaluation are used to obtain a
thorough assessment of velopharyngeal function: a clinical evaluation and an instrumental
evaluation. An understanding of the various
subjective and objective techniques of each
type of evaluation that are available to assess
velopharyngeal function will enable the practitioner to identify the exact cause and determine the specific management of any velopharyngeal disorder. As no single modality is
adequate for complete appraisal of velopharyngeal function, a variety of techniques should be
used for evaluation. Utilizing different modalities will reveal the presence, size, location, and
contour of an opening between the oral and
nasal cavities during speech and delineate the
nature of the velar and pharyngeal wall movements and interactions. The following is a description of the methods available, with particular focus on the approaches used most often
at our institution in the diagnosis and treatment of velopharyngeal incompetence.
Clinical Assessment of Velopharyngeal Activity
The clinicians eyes and ears are used as the
first and primary diagnostic tools. As the most
valid measure of adequate velopharyngeal
function is sound produced during normal
speech, by simply listening, one can judge
whether further investigation is warranted.
When a patients speech deviates from normal,
a complete clinical evaluation is performed.
After a thorough history is obtained, the clinical examination proceeds with an intraoral examination to assess structural integrity, reflexive behavior, and voluntary phonetic behavior.
The speech production characteristics are then
assessed. Particular focus is paid to resonance
quality, airflow, air pressure, and whether compensatory articulatory productions exist.
Intraoral Examination
The first step in the intraoral examination is
the direct visual assessment of structural integrity. The lips, teeth, tongue, tonsils, hard and
soft palate, uvula, and pharyngeal walls should
December 2003
be carefully inspected. The symmetry of the
velum, tonsils, and nasopharynx is noted. Submucous clefts are revealed through palpation
of a notch in the hard palate, identification of
a zona pellucida in the soft palate, or a bifid
uvula. The presence of an oral nasal fistula
should be sought. A rhinoscopic examination
should be included to check for hypertrophied
turbinates, septal deviation, and nasal
obstruction.
The second step in the intraoral examination is to assess reflexive and voluntary behavior. Reflexive behavior assists in determining
the overall dysarthric status. This assessment is
performed by repetitive stimulation of a gag
reflex at different loci. Delay, fatigue, asymmetry, or lack of response is noted. The presence
or absence of nasal regurgitation during swallowing of liquids should also be determined.
Unlike reflexive behavior, a voluntary behavioral assessment is limited to competent, cooperative patients. Visual intraoral assessment
during sustained phonation of a assists in
determining velar motion (elevation, length,
asymmetry, amplitude, fatigue, and speed).
Speech Production Characteristics
Upon completion of a thorough intraoral
examination, the clinical examination proceeds with an assessment of speech production
characteristics. Four specific characteristics are
assessed: resonance quality, airflow, air pressure, and compensatory articulation. Deviations in the normal movement of a pressurized
airstream through the resonating vocal tract
will cause specific alterations in these four
characteristics. The recognition of these alterations will assist in obtaining the correct
diagnosis.
The first characteristic, resonance quality, is
assessed by checking for the presence of nasal
vibration during vowel production (i, u, and e).
With an incomplete velopharyngeal seal, the
nasal cavity becomes coupled with the oral cavity and the airstream escapes through the open
velopharyngeal port, causing hypernasal resonance. This resonance can be detected clinically by comparing occluded and unoccluded
nares for the presence of a nasal vibration during vowel production.
The presence or absence of nasal emission of
the airstream is the second speech production
characteristic to assess. Nasal emission may be
audible or inaudible. In addition to the noise
that may be produced, the occurrence of nasal
Vol. 112, No. 7 /
1893
EVALUATING VELOPHARYNGEAL INCOMPETENCE
flaring assists in identification. Other methods
helpful in diagnosing inaudible nasal emission
include a mirror that fogs when placed under
the nares during vowel production and the
deflection of tissue paper.
The third characteristic is the adequacy of
intraoral air pressure build-up. The average
adult requires 5 to 7 cm of water pressure
build-up in the oral cavity behind the site of
constriction to produce most oral consonants,
particularly plosives (p) and fricatives (f).
When velopharyngeal insufficiency is present,
an inadequate amount of pressure is accrued
in the oral cavity secondary to incomplete closure of the velopharyngeal valve. The phrase
used frequently at our institution to test air
pressure is I pet puppies.
To complete the speech production assessment, the presence or absence of compensatory articulation productions should be sought.
Patients with cleft palate will derive compensatory articulation in a different anatomic area
that will compensate for a poor or absent velopharyngeal valve. Specific types of compensatory articulations used by these patients include glottal stops, pharyngeal fricatives,
pharyngeal stops, velar fricatives, posterior nasal fricatives, and middorsal palatal stops (Table I). In other words, the patient substitutes a
functioning glottis or pharynx or uses the mid
dorsum and the back of the tongue to valve the
airflow. The neurogenic patient, however, will
have compensatory productions occurring at
the same anatomic level but deviating in the
manner of speech production. Thus, glottal
and pharyngeal productions are absent.
Rather, labial substitution is performed for
tongue inadequacy. Regardless of the derivation of compensatory productions, they are all
learned behaviors, which frequently persist
even after adequate surgical or prosthetic
management.
Instrumental Assessment of Velopharyngeal Activity
The subjective yet invaluable information
gathered from the clinical examination should
be used to complement objective structural
data obtained from an instrumental assessment. The goal of the instrumental assessment
is to obtain anatomic data regarding the adequacy of velar length, palatal elevation, velopharyngeal gap, excursion of the lateral and
posterior pharyngeal walls, nasopharyngeal
depth, pattern, and level of attempted closure.
Two subgroups of techniques are used in the
diagnostic process: direct and indirect. Direct
instrumental techniques are those that enable
the investigator to observe activity at the velopharyngeal port. Examples of direct techniques include lateral cephalogram, cineradiography, multiview videofluoroscopy, oralnasal panendoscopy, and magnetic resonance
imaging. Indirect instrumental techniques provide information about vocal tract behavior,
and gathered data are used to make relative
inferences. Phototransduction, electromyography, and movement transduction are a few
examples of indirect instrumental techniques.
Direct Instrumental Techniques
Lateral cephalometric radiography. The lateral
cephalometric radiograph continues to be a
mainstay of the evaluation process at our institution as well as many others. It is the primary
direct method of assessing structures of the
velopharynx and the surrounding tissues. Obtained at a constant magnification factor both at
rest and during a sustained -ee production,
lateral cephalogram views permit visualization
of soft palate elevation and its contact with the
posterior pharyngeal wall. The addition of barium allows for enhanced visualization of the
margins of the velum and pharyngeal wall. Using this technique, we have had a greater than
90 percent rate of accurate prediction of the
need for a pharyngeal flap based solely on this
radiographic study.
Obvious advantages include the ability to assess structural features and velopharyngeal relationships in a simple, reliable, and quantifiable method. The length of a pharyngeal flap is
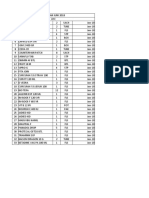
TABLE I
The Phonetic Alphabet: Consonants
Bilabial
Nasals
Plosives
Fricatives
Sibilants
Affricates
Labiodental
m
p-b (pat-bat)
f-v (fat-vat)
Dentoalveolar
n
t-d (tot-dot)
th-th (thank-than)
s-z (sue-zoo)
ts-dz (cheap-jeep)
Palatoalveolar
Velar
ng (sing)
k-g (coat-goat)
sh-zh (ash-azure)
sh-z (ash-azure)
ts-dz (cheap-jeep)
1894
determined by assessing the relationships provided.34,35 Because the velopharyngeal mechanism is three-dimensional and dynamic, the
disadvantages of a lateral still radiograph are
obvious: it is a two-dimensional study representative of structural features only in the sagittal
plane. Hence, the width of a pharyngeal flap
cannot be determined by this method. Further,
because it is a static study, the events occurring
between the two extremes of movement (between the resting state and the -ee production) are not visualized. Despite its limitations,
it continues to be a vital part of the diagnostic
battery at multidisciplinary cleft palate centers.
Multiview videofluoroscopy. In response to the
limitations of the lateral still radiograph, lateral
view motion picture radiography was introduced to study velopharyngeal function in motion. With advances in technology, this evolved
from cine (motion picture films) to multiview
videofluoroscopy. Multiview videofluoroscopy
has distinct advantages, such as less radiation
exposure (10 times less than cinefluoroscopy),
the ability to record and replay immediately,
assessment of velopharyngeal function in three
planes (sagittal, coronal, and transverse), and a
dynamic view during connected speech from
beginning to end.36 42 The lateral views depict
movements of the velum and posterior pharyngeal walls. The frontal view of the oropharynx
demonstrates gradations of mesial motion of
the lateral pharyngeal walls, which ultimately
determines the width of a proposed pharyngeal
flap. Although its primary limitation is the inability to provide an absolute measurement of
structural relationships, the width of a proposed
pharyngeal flap is easily determined by a relative scale. The degree of lateral pharyngeal wall
motion ranges from zero (no motion during
quiet respiration) to five (maximal motion to
the midline; Fig. 1). This ability to obtain an
accurate preoperative assessment of lateral pharyngeal wall motion appears to be a prime determinant of postoperative success after a pharyngeal flap operation. In addition to being
excellent in depicting necessary information on
velopharyngeal function and dictating surgical
management, compared with other techniques,
it has the least variability and is most reflective
of actual speech pattern.
Nasopharyngoscopy. The limitations of nasopharyngoscopy are similar to those of videofluoroscopy. The information obtained to assess gap size is in the form of a ratio than an
absolute number. Although nasopharyngos-
PLASTIC AND RECONSTRUCTIVE SURGERY,
December 2003
FIG. 1. Diagrammatic frontal view of the oropharynx
demonstrates gradations of mesial motion of the lateral pharyngeal walls. Zero represents no motion during quiet respiration, and 5 depicts maximal motion of each lateral pharyngeal wall to the midline. Reprinted from Johns, D. F.,
Cannito, M. P., Rohrich, R. J., and Tebbetts, J. B. The selflined superiorly based pull-through velopharyngoplasty: Plastic surgery-speech pathology interaction in the management
of velopharyngeal insufficiency. Plast. Reconstr. Surg. 94: 436,
1994.
copy provides a substantial amount of information through visualization of the velum and
pharyngeal walls, it is difficult to obtain standardized views or infer relative dimensions.
Other limitations include the inability to identify small velopharyngeal gaps or pinpoint the
exact anatomical location of the gap. Patient
cooperation becomes a critical factor that further limits the use of nasopharyngoscopy in the
pediatric population unless the patient is anesthetized. DAntonio et al.43,44 have described the
criteria, indications, and impact of nasal endoscopy on tailoring pharyngeal flaps, flap revisions, and the fitting of palatal prostheses. Similarly, Pigott finds the 70-degree endoscope to
be indispensable and complementary to multiview videofluoroscopy in the evaluation of the
velopharyngeal sphincter.45,46
Magnetic resonance imaging. Magnetic resonance imaging uses the resonant absorption and
remission of radio waves by hydrogen nuclei to
Vol. 112, No. 7 /
1895
EVALUATING VELOPHARYNGEAL INCOMPETENCE
obtain images. It has a number of advantages over
the methodologies currently used to study the
vocal tract and velopharyngeal mechanism.47,48
Magnetic resonance imaging technology allows
noninvasive visualization of the vocal tract without
exposure to radiation or any known biohazards
and provides better soft-tissue resolution. Functional images at any chosen level can be obtained
in the sagittal, frontal, and transaxial views without changing the position of the patient. The
current limitations of this method for imaging
include the potential distortion of the velopharyngeal mechanism by gravitational forces in the
supine position, the need for patient cooperation,
and cost. It is hoped that further technological
developments will result in nearreal-time functional imaging that will soon reach its full potential and provide unique full-range vocal tract configuration data.
Indirect Instrumental Techniques
Indirect techniques used to study the velopharyngeal mechanism are those that provide
inferences through data about the structure
and kinematics of the velopharyngeal mechanism. Examples include phototransduction,
electromyography, and movement transduction. Other types of indirect measures study
the effects of velopharyngeal function on other
physiologic parameters. Aerodynamics, acoustics, sound pressure, and spectrography fall under this category. Although indirect measures
provide objective information, they do not necessarily dictate the decision-making process.
Phototransduction. Photoelectric technology
uses light transmission to obtain relative information on the velopharyngeal port. A fiberoptic
device couples a light source to an electronic
detector. The two fibers are introduced
through the nasal cavity until the light source is
below the velopharyngeal port and the detector
fiber is above the velopharyngeal port. Quantifiable data are produced that provide information regarding the opening and closing
movements of the velopharyngeal port.
Electromyography. Electromyography studies
the electrical activity produced by muscle contraction using hooked wire electrodes. The limitations of electromyography are intuitive, such
as discomfort from placement of needle electrodes, small and malpositioned muscles in cleft
patients, and multiple passive and active forces
acting on the velopharynx.
Movement transduction. Movement transduction combines the use of mechanical and elec-
trical devices to transduce velopharyngeal
movement. The second maxillary molar acts as
an anchor, with placement of a bar/spring attachment along the oral midline. With velar
motion, the spring sensor converts motion into
an electrical output along the strain gauge resistor. Although this technique is not currently
used as an evaluation tool, it has been helpful
as a biofeedback device.
Aerodynamics. The study of pressure and
flow provides significant information that allows a distinction to be made between velopharyngeal insufficiency and dysfunction secondary to other anatomic valve abnormalities. In
addition, it helps determine the presence and
magnitude of velopharyngeal incompetence
and obstruction (nasal or pharyngeal). Specific
information details the relative contributions of
velopharyngeal components and nasal components to total airway resistance. In a complex
case, this technique may be useful before surgical intervention to isolate and determine various contributions to insufficiency. Similarly, it
is helpful after surgical intervention to determine whether a pharyngeal flap is the cause of
a patients difficulty with nasal respiration.
Acoustics. Quantitative changes in nasal resonance that occur with different degrees of coupling (the nasal and oral cavities) provide information about the presence and degree of
velopharyngeal incompetence. In these patients, excessive acoustic energy in the nasal
cavity is observed during reading from passages
with oral sounds. In children with velopharyngeal obstruction, lack of acoustic energy in the
nasal cavity is observed during reading from
passages containing many nasal sounds. In addition to deciphering the location and degree
of abnormal resonance, the information is provided instantaneously. Therefore, the acoustic
assessment is a helpful method used for
biofeedback during treatment sessions. Further, acoustic analyses with a sound spectrograph will identify subtle changes in the acoustic signal and can be used to monitor speech
characteristics objectively. These acoustic findings should validate the more subjective perceptual ratings.
DISCUSSION
The multidisciplinary cleft palate team is indispensable in coordinating evaluation, diagnosis, and management of velopharyngeal insufficiency, as is the speech pathologist. The
focus of this article is to present basic and
1896
PLASTIC AND RECONSTRUCTIVE SURGERY,
helpful techniques to improve the capabilities
of any member of the cleft palate team in
identifying preoperative or postoperative velopharyngeal incompetence. Through improvements in preoperative diagnostic techniques,
improvements in outcomes are sure to follow.
Similarly, the ability to critique a speech outcome after surgical intervention and to identify
factors in patients with poor outcomes that
may be avoided or modified in the future will
lead to an improvement in outcomes. A thorough understanding of the mechanism of velopharyngeal function and the instrumental
techniques used for evaluation may inspire
new treatment modalities or improve those
that currently exist. It is hoped that the multidisciplinary team will use the thorough clinical
assessment and data obtained from instrumental techniques discussed in this article to determine the most appropriate intervention for a
given patient. Clearly, without an armamentarium of several surgical techniques, the surgeon
will be limited to applying a single treatment
modality to a problem with varied physiological
and structural causes.
Rod J. Rohrich, M.D.
Department of Plastic Surgery
University of Texas Southwestern Medical Center
5323 Harry Hines Boulevard, E7.212
Dallas, Texas 75390-9132
rod.rohrich@utsouthwestern.edu
ACKNOWLEDGMENT
This is the last paper written by Dr. Donnell F. Johns before
his untimely death. He left it on his desk, almost completed.
The last time I spoke with him, he reminded me that he
needed to finish it. His dedication to the correction of neurogenic velopharyngeal insufficiency, particularly in underprivileged children, demonstrated his humanity. His dedication exemplified who he was as an individual. He was a
tremendous asset to us and to our profession. We miss him.
REFERENCES
1. Dorf, D., and Curtain, J. W. Early cleft palate repair and
speech outcome. Plast. Reconstr. Surg. 70: 74, 1982.
2. Rohrich, R. J., Johns, D., and Shewmake, K. Optimal
management of the cleft palate patient with plastic
surgery/speech pathology interaction. Tex. J. Audiol.
Speech Pathol. 17: 44, 1991.
3. Rohrich, R. J., Love, E. J., Byrd, H. S., and Johns, D. F.
Optimal timing of cleft palate closure. Plast. Reconstr.
Surg. 106: 413, 2000.
4. Witt, P., and DAntonio, L. Velopharyngeal insufficiency and secondary palatal management. Clin. Plast.
Surg. 4: 707, 1993.
5. Ysunza, A., Pamplona, C., and Mendoza, M. Speech
outcome and maxillary growth in patients with unilateral complete cleft lip. Plast. Reconstr. Surg. 102: 675,
1998.
December 2003
6. Rohrich, R. J., Rowsell, A. R., Johns, D. F., et al. Timing
of hard palatal closure: A critical long-term analysis.
Plast. Reconstr. Surg. 98: 236, 1996.
7. Owsley, J. Poor speech following the pharyngeal flap
operation. Cleft Palate J. 9: 32, 1972.
8. Hollier, L. Cleft palate and velopharyngeal incompetence. Selected Readings Plast. Surg. 8: 1, 1997.
9. Spriestersbach, D. C. Clinical research in cleft lip and
cleft palate. Cleft Palate J. 10: 113, 1973.
10. Johns, D., Tebbetts, J. B., and Cannito, M. Cleft Lip and
Palate: Long-Term Results and Future Prospects. Manchester, United Kingdom: Manchester University Press,
1990.
11. DAntonio, L., and Marsh, J. L. Evaluation and management of velopharyngeal dysfunction. Probl. Plast.
Reconstr. Surg. 2: 86, 1992.
12. Trost, J. E. Articulatory additions to the classical descriptions of speech in patients with cleft palate. Cleft
Palate J. 18: 193, 1981.
13. Johns, D. Anatomy and Physiology of the Velopharyngeal
Valving Mechanism. Dallas, Texas: Department of Plastic Surgery, University of Texas Southwestern Medical
Center Grand Rounds, 2001.
14. Warren, D. Aerodynamics of speech production. In
N. J. Lass, L. V. McReynolds, J. L. Northern, and D. E.
Yoder (Eds.), Speech, Language, and Hearing. Philadelphia: Saunders, 1982.
15. Brooks, A., and Shelton, R. Compensatory tongue-palate-posterior pharyngeal wall relationships in cleft palate. J. Speech Hear. Disord. 30: 166, 1965.
16. Locke, J. The explanation and treatment of sound disorders. J. Speech Hear. Disord. 48: 339, 1983.
17. Oller, D. K. The emergence of sounds of speech in
infancy. In G. H. Yeni-Komshian, J. F. Kavanagh, and
C. A. Ferguson (Eds.), Child Phonology, Vol. 1. New
York: Academic Press, 1980.
18. Iglesisas, A., and Morris, H. Simultaneous assessment of
pharyngeal wall and velar displacement for selected
speech sounds. J. Speech Hear. Res. 23: 429, 1980.
19. Morris, H. L. Communicative Disorders Related to Cleft Palate, 2nd Ed. Boston: Little, Brown, 1979.
20. Bernthal, J. Articulation and Phonological Disorders. Englewood Cliffs, N. J.: Prentice Hall, 1988.
21. Bzoch, K. Articulatory proficiency and error patterns of
preschool cleft and normal children. Cleft Palate J. 2:
340, 1965.
22. Johns, D. Clinical Management of Neurogenic Communicative Disorders. Boston: Little, Brown, 1985.
23. Lewin, M. L., Croft, C. B., and Shprintzen, R. J. Velopharyngeal insufficiency due to hypoplasia of the muscular uvula and occult submucous cleft palate. Plast.
Reconstr. Surg. 65: 585, 1980.
24. Darley, F. L., and Aronson, A. E. Motor Speech Disorders.
Philadelphia: Saunders, 1975.
25. Noordhoff, M. S. Development of articulation before
delayed hard palate closure in children with cleft palate. Plast. Reconstr. Surg. 80: 518, 1987.
26. Penslar, K. M., and Bauer, B. Levator repositioning and
palatal lengthening for submucous clefts. Plast. Reconstr. Surg. 82: 765, 1988.
27. Powers, G., and Starr, C. The effects of muscle exercises
on velopharyngeal gap and nasality. Cleft Palate J. 11:
28, 1984.
28. Trier, W. The pharyngeal flap operation. Clin. Plast.
Surg. 12: 4, 1985.
29. Smith, J. Teflon injection in the nasopharynx to im-
Vol. 112, No. 7 /
30.
31.
32.
33.
34.
35.
36.
37.
38.
39.
EVALUATING VELOPHARYNGEAL INCOMPETENCE
prove velopharyngeal closure. Ann. Otolaryngol. 86:
559, 1977.
Croft, C. B., and Shprintzen, R. J. Velopharyngeal Insufficiency Relieved by Tonsillectomy. Atlanta, Ga.: American
Cleft Palate Association, April 1978.
Peterson, S. J. Nasal emission as a component of the
misarticulations of sibilants and affricates. J. Speech
Hear. Disord. 40: 106, 1975.
Trost, J. E. Articulatory additions to the classic descriptions of speech of persons with cleft palate. Cleft Palate
J. 18: 193, 1981.
Johns, D., Tebbetts, J. B., and Cannito, M. Perceptual
acoustic analysis. Cleft Lip Palate 69: 1990.
Johns, D., Rohrich, R. J., and Tebbetts, J. B. The selflined superiorly based pull-through velopharyngoplasty. Plast. Reconstr. Surg. 94: 436, 1994.
Shprintzen, R. A comprehensive study of pharyngeal
flap surgery: Tailor made flaps. Cleft Palate J. 16: 1,
1979.
Stringer, D. A., and Witzel, M. A. Velopharyngeal insufficiency on videofluoroscopy: Comparison of projections. Am. J. Radiol. 146: 15, 1986.
Cohn, E. R., Rood, S. R., McWilliams, B. J., Skolnick,
M. L., and Abdelmalek, L. R. Barium sulphate coating on the nasopharynx in lateral view videofluoroscopy. Cleft Palate J. 21: 7, 1984.
Skolnick, M. L. Videofluoroscopy with nasal speech,
emphasis on lateral pharyngeal motion in velopharyngeal closure. Radiology 93: 747, 1984.
McWilliams, B. J., Glaser, E. R., Philips, B. J., et al. A
comparative study of four methods of evaluating velopharyngeal adequacy. Plast. Reconstr. Surg. 68: 1, 1981.
1897
40. Harington, J. A cinefluorographic study of the pharyngeal flap. Cleft Palate J. 9: 127, 1975.
41. Hoopes, J. E., Dellon, A. L., Fabrikant, J. I., and Soliman,
A. H. Idiopathic hypernasality: Cineradiographic
and etiologic considerations. J. Speech Hear. Disord. 35:
44, 1970.
42. Hoopes, J. E., Dellon, A. L., Fabrikant, J. I., Edgerton,
M. T., Jr., and Soliman, A. H. Cineradiographic definition of the functional anatomy and pathophysiology of the velopharynx. Cleft Palate J. 7: 443, 1970.
43. DAntonio, L., Muntz, H. R., Marsh, J. L., Marty-Grames,
L., and Backensto-Marsh, R. Practical application of
flexible fiberoptic nasopharyngoscopy for evaluating
velopharyngeal function. Plast. Reconstr. Surg. 82: 611,
1988.
44. DAntonio, L. L., Achauer, B. M., and Vander Kam, V. M.
Results of a survey of a cleft palate teams concerning
the use of nasendoscopy. Cleft Palate Craniofac. J. 30: 35,
1993.
45. Pigott, R. The results of nasopharyngoscopic assessment of pharyngoplasty. Scand. J. Plast. Reconstr. Surg.
8: 148, 1980.
46. Pigott, R. W., and Makepeace, A. P. Some characteristics of endoscopic and radiological systems used in
elaboration of the diagnosis of velopharyngeal incompetence. Br. J. Plast. Surg. 35: 19, 1982.
47. Johns, D., and Rohrich, R. J. Use of MRI in vocal tract
imaging for assessing velopharyngeal incompetency:
Technique and future applications. Plast. Reconstr.
Surg. 8: 1, 1994.
48. Baer, T. Application of MRI to the analysis of speech
production. Magn. Reson. Imag. 5: 1, 1987.
Self-Assessment Examination follows on
the next page.
Self Assessment Examination
Velopharyngeal Incompetence: A Guide for Clinical Evaluation
by Donnell F. Johns, Ph.D., Rod J. Rohrich, M.D., and Mariam Awada, M.D.
1. WHICH OF THE FOLLOWING IS THE MOST COMMON CAUSE OF VELOPHARYNGEAL INCOMPETENCE?
A) Undiagnosed submucous cleft palate
B) Short or immobile palate following primary cleft repair
C) Mechanical obstruction
D) Neurologic deficit
E) Palatal fistula
2. DURING VELOPHARYNGEAL CLOSURE, MOVEMENT OF SOFT PALATE IS PRINCIPALLY DUE TO ACTION
OF WHICH MUSCLE?
A) Tensor veli palatini
B) Levator veli palatini
C) Pharyngopalatinus
D) Palatoglossus
E) Superior constrictor
3. SINCE THE ENTIRE VOCAL TRACT IS A RESONATING CAVITY, NORMAL SPEECH PRODUCTION REQUIRES
THE VELOPHARYNGEAL PORT COUPLING AND UNCOUPLING OF THE NASAL AND ORAL CAVITIES.
A) True
B) False
4. SURGICAL CORRECTION OF VELOPHARYNGEAL INCOMPETENCE WILL IMPROVE EACH OF THE
FOLLOWING EXCEPT:
A) Resonance quality
B) Nasal airflow
C) Intraoral air pressure
D) Articulation errors
E) Nasal regurgitation
5. ACCORDING TO THE AUTHORS, THE BEST METHOD TO ASSESS SOFT-PALATE ELEVATION AND
CONTACT WITH THE POSTERIOR PHARYNGEAL WALL IS:
A) Lateral cephalometric radiography
B) Magnetic resonance imaging
C) Multiview videofluoroscopy
D) Nasopharyngoscopy
E) Aerodynamics
6. ACCORDING TO THE AUTHORS, THE DEGREE OF LATERAL WALL MOTION USED TO DETERMINE THE
WIDTH OF A PLANNED PHARYNGEAL FLAP IS BEST DETERMINED USING:
A) Lateral cephalometric radiography
B) Magnetic resonance imaging
C) Multiview videofluoroscopy
D) Nasopharyngoscopy
E) Movement transduction
To complete the examination for CME credit, turn to page 1982 for instructions and the response form.
Vous aimerez peut-être aussi
- Odell Problem Solving Cases MCQs-combined PDFDocument114 pagesOdell Problem Solving Cases MCQs-combined PDFVishakha Saboo100% (9)
- Botox in Facial AestheticsDocument27 pagesBotox in Facial AestheticsTip Piraya100% (5)
- Position Paper About Legalization of Marijuana in The PhilippinesDocument2 pagesPosition Paper About Legalization of Marijuana in The PhilippinesHabibi Waishu93% (14)
- Tor Proyek Stunting-BangdaDocument26 pagesTor Proyek Stunting-BangdaKiky Nurfayanti Denra'Pas encore d'évaluation
- How To Use Akpi Seed For Hips, Butts and Breasts EnlargementDocument5 pagesHow To Use Akpi Seed For Hips, Butts and Breasts EnlargementLinda PridePas encore d'évaluation
- Prosthetic Management of Soft Palate Defects: Presented byDocument57 pagesProsthetic Management of Soft Palate Defects: Presented byPiyush DongrePas encore d'évaluation
- 2017 Whats New in Cleft Palate and VelopharyngealDocument13 pages2017 Whats New in Cleft Palate and VelopharyngealDimitris RodriguezPas encore d'évaluation
- Velopharyngeal Insufficiency and Its Management: DR T BalasubramanianDocument15 pagesVelopharyngeal Insufficiency and Its Management: DR T BalasubramanianDr. T. Balasubramanian100% (2)
- SeminarsTypesofVPD KummerDocument10 pagesSeminarsTypesofVPD KummerAmiteshwar SinghPas encore d'évaluation
- Kliegman: Nelson Textbook of Pediatrics, 18th Ed.: 2007 Saunders, An Imprint of ElsevierDocument14 pagesKliegman: Nelson Textbook of Pediatrics, 18th Ed.: 2007 Saunders, An Imprint of ElseviermelindamentariPas encore d'évaluation
- Classification of SSDDocument19 pagesClassification of SSDprathamesh patilPas encore d'évaluation
- Caracterização Do Padrão de Fechamento Velofaríngeo em Pacientes Com Fissura PalatinaDocument6 pagesCaracterização Do Padrão de Fechamento Velofaríngeo em Pacientes Com Fissura PalatinaValentina SalasPas encore d'évaluation
- Speech Evalwith CLPDocument12 pagesSpeech Evalwith CLPnelly alconzPas encore d'évaluation
- Dlobasic Apr11Document27 pagesDlobasic Apr11Dr. T. BalasubramanianPas encore d'évaluation
- Correction of Ant Openbite Very Important PaperDocument18 pagesCorrection of Ant Openbite Very Important PaperMahdi ZakeriPas encore d'évaluation
- Congenital MalformationsDocument20 pagesCongenital Malformationsapi-19500641Pas encore d'évaluation
- Kummer 2014Document18 pagesKummer 2014Ana Claudia MarquesPas encore d'évaluation
- Cleft Lip and PalateDocument83 pagesCleft Lip and Palategracy davidPas encore d'évaluation
- Review Article: Ramesh Kumar Sharma, Vipul NandaDocument5 pagesReview Article: Ramesh Kumar Sharma, Vipul Nandaintanmaryani9_943390Pas encore d'évaluation
- Oropharyngeal Dysphagia HNCDocument15 pagesOropharyngeal Dysphagia HNCKhumaira SantaPas encore d'évaluation
- Airway Management in The Adult - Miller's Anesthesia 2009Document38 pagesAirway Management in The Adult - Miller's Anesthesia 2009UrgenciasCol FoamPas encore d'évaluation
- "Camouflage Treatment in Adenoid Facies: Long Face Syndrome"-A Case Report. - Orthodontic Cyber JouDocument11 pages"Camouflage Treatment in Adenoid Facies: Long Face Syndrome"-A Case Report. - Orthodontic Cyber Joudrrajesh27100% (1)
- 2011 @dentallib John Beumer III, Mark T Marunick, Salvatore J Esposito-171-229Document139 pages2011 @dentallib John Beumer III, Mark T Marunick, Salvatore J Esposito-171-229TariqPas encore d'évaluation
- Cleft Lip and PalateDocument5 pagesCleft Lip and PalateChristopher Ivan Herrera MontielPas encore d'évaluation
- Vocal Fold Polyp: Case ReportDocument9 pagesVocal Fold Polyp: Case ReportIndah Afriani NasutionPas encore d'évaluation
- Swallowing DisorderDocument10 pagesSwallowing DisorderDhiel Muhammad FarreyraPas encore d'évaluation
- Anterior Open Bite Correction by Le Fort I or Bilateral Sagittal Split OsteotomyDocument18 pagesAnterior Open Bite Correction by Le Fort I or Bilateral Sagittal Split Osteotomyloren camila Daza GomezPas encore d'évaluation
- Speech / Communication Disorders: Down SyndromeDocument31 pagesSpeech / Communication Disorders: Down SyndromeRavi ShahPas encore d'évaluation
- Speech Therapy For Compensatory Articulations and Velopharyngeal Function: A Case ReportDocument6 pagesSpeech Therapy For Compensatory Articulations and Velopharyngeal Function: A Case ReportjhfgPas encore d'évaluation
- Rai Frenillo2Document8 pagesRai Frenillo2Karen DanielaPas encore d'évaluation
- 2.3 Voice - Disorders2Document20 pages2.3 Voice - Disorders2Fernanda MerichesPas encore d'évaluation
- Duaa DuaaDocument27 pagesDuaa DuaaDoaa TahseenPas encore d'évaluation
- Mandulak Baylis Thurmes PDFDocument179 pagesMandulak Baylis Thurmes PDFAli JdeedPas encore d'évaluation
- Cleft Lip and PalateDocument2 pagesCleft Lip and PalateTracy100% (1)
- 20 .Malocclusion and Upper Airway ObstructionDocument7 pages20 .Malocclusion and Upper Airway ObstructionSoe San Kyaw0% (1)
- 1 s2.0 S2212426823000155 MainDocument9 pages1 s2.0 S2212426823000155 MainMuhammadFauzun TFPas encore d'évaluation
- Assessing Palatal Mobility in Post-Tonsillectomy Patients: Egyptian Journal of Ear, Nose, Throat and Allied SciencesDocument3 pagesAssessing Palatal Mobility in Post-Tonsillectomy Patients: Egyptian Journal of Ear, Nose, Throat and Allied SciencesYessyParamitaPas encore d'évaluation
- Palatoplasty Case StudyDocument26 pagesPalatoplasty Case StudySometwo C. Hangal100% (1)
- Speech Intelligibility of Patients With Cleft Lip and Palate After Placement of Speech Prosthesis.Document7 pagesSpeech Intelligibility of Patients With Cleft Lip and Palate After Placement of Speech Prosthesis.Luiz Guilherme LoivosPas encore d'évaluation
- Policy On Management of The Frenulum inDocument6 pagesPolicy On Management of The Frenulum inمعتزباللهPas encore d'évaluation
- 36 Cleft Lip and PalateDocument45 pages36 Cleft Lip and PalateCristian VieyraPas encore d'évaluation
- Diagnosis and Management of Velopharyngeal DysfunctionDocument8 pagesDiagnosis and Management of Velopharyngeal Dysfunctiondrgurpal74Pas encore d'évaluation
- Effect of Cleft Palate Closure Technique On SpeechDocument15 pagesEffect of Cleft Palate Closure Technique On SpeechLEONARDO ALBERTO CRESPIN ZEPEDAPas encore d'évaluation
- Velopharyngeal Insufficiency: Current Concepts in Diagnosis and ManagementDocument6 pagesVelopharyngeal Insufficiency: Current Concepts in Diagnosis and Managementsnehal jaiswalPas encore d'évaluation
- Submucous CleftDocument2 pagesSubmucous CleftNovia SetyowatiPas encore d'évaluation
- Anquiloglosia 2Document9 pagesAnquiloglosia 2trilcePas encore d'évaluation
- Eating and Swallowing Disorders in Children With Cleft Lip Andor Palate - 2022Document9 pagesEating and Swallowing Disorders in Children With Cleft Lip Andor Palate - 2022Tânia DiasPas encore d'évaluation
- Baba Jaswant Singh Dental College and Research Institute, LudhianaDocument40 pagesBaba Jaswant Singh Dental College and Research Institute, LudhianaPalak VashistPas encore d'évaluation
- Pediatric Laryngotracheal Stenosis and Airway Reconstruction: A Review of Voice Outcomes, Assessment, and Treatment IssuesDocument11 pagesPediatric Laryngotracheal Stenosis and Airway Reconstruction: A Review of Voice Outcomes, Assessment, and Treatment Issuescanndy202Pas encore d'évaluation
- Effects of Voice Therapy Using The Lip Trill Technique in P - 2019 - Journal ofDocument9 pagesEffects of Voice Therapy Using The Lip Trill Technique in P - 2019 - Journal ofJulia GavrashenkoPas encore d'évaluation
- Ruda 2012Document17 pagesRuda 2012Camila MillarPas encore d'évaluation
- Assessment of VP FunctionDocument27 pagesAssessment of VP FunctionDaniel BramantyoPas encore d'évaluation
- Policy On Management of The Frenulum inDocument6 pagesPolicy On Management of The Frenulum inLaura Sánchez LoperaPas encore d'évaluation
- Todentj 11 436Document11 pagesTodentj 11 436Anurag NahataPas encore d'évaluation
- Laryngeal SeparationDocument27 pagesLaryngeal Separationhossamh3Pas encore d'évaluation
- Signs and Symptoms of Abnormal Swallow: Aspiration (Coughing, Choking)Document2 pagesSigns and Symptoms of Abnormal Swallow: Aspiration (Coughing, Choking)Anda DorofteiPas encore d'évaluation
- HN9 Pharynx 03Document12 pagesHN9 Pharynx 03Farhan HasbiPas encore d'évaluation
- Provisional Prosthesis For Class 1 Radical Mandibular Alveolectomy Patient - A Case ReportDocument5 pagesProvisional Prosthesis For Class 1 Radical Mandibular Alveolectomy Patient - A Case ReportRastia UtamiPas encore d'évaluation
- Oral Development PathologyDocument6 pagesOral Development PathologyKathyWPas encore d'évaluation
- Aberrant Frenum and Its TreatmentDocument90 pagesAberrant Frenum and Its TreatmentheycoolalexPas encore d'évaluation
- The Case For Environmental Etiology of Malocclusion in Modern Civilizations-Airway Morphology and Facial GrowthDocument26 pagesThe Case For Environmental Etiology of Malocclusion in Modern Civilizations-Airway Morphology and Facial GrowthMoises Adriano Pulido GuimarãesPas encore d'évaluation
- Cleft Lip and Palate PresentationDocument69 pagesCleft Lip and Palate PresentationAli Murtuza100% (1)
- Surgical Treatment of Snoring & Obstructive Sleep Apnoea: Review ArticleDocument10 pagesSurgical Treatment of Snoring & Obstructive Sleep Apnoea: Review ArticleSiddharth DhanarajPas encore d'évaluation
- Cleft PalateDocument16 pagesCleft PalateAnu Priya GopuPas encore d'évaluation
- Differential Diagnosis and Treatment of Children with Speech DisorderD'EverandDifferential Diagnosis and Treatment of Children with Speech DisorderÉvaluation : 5 sur 5 étoiles5/5 (1)
- Water Soluble VitaminsDocument89 pagesWater Soluble Vitaminsahmedatef100% (1)
- Lip and Cheek Reconstruction: BY DR Mohammad Akheel Omfs PGDocument90 pagesLip and Cheek Reconstruction: BY DR Mohammad Akheel Omfs PGahmedatefPas encore d'évaluation
- Orthognathic Surgery For Patients With Maxillofacial DeformitiesDocument25 pagesOrthognathic Surgery For Patients With Maxillofacial DeformitiesahmedatefPas encore d'évaluation
- Secondary Deofrmities of Cleft Lip NoseDocument8 pagesSecondary Deofrmities of Cleft Lip NoseahmedatefPas encore d'évaluation
- LESSON 1 Basic Home Care NursingDocument28 pagesLESSON 1 Basic Home Care Nursing1-PASCUAL, Patricia Nicole P.Pas encore d'évaluation
- Cream Powder Standard: Product DefinitionDocument2 pagesCream Powder Standard: Product DefinitionMurat SariyarPas encore d'évaluation
- Food Industry Research and Development L.: Mary D. Earle and Richard EarleDocument2 pagesFood Industry Research and Development L.: Mary D. Earle and Richard EarleAbi PajenadoPas encore d'évaluation
- Lifting and Basic Life SupportDocument37 pagesLifting and Basic Life SupportmijaPas encore d'évaluation
- Axis III GMCDocument4 pagesAxis III GMCFasya GhaffarPas encore d'évaluation
- Barang Ed DekatDocument12 pagesBarang Ed DekatAkhmad “Billy Rafi” HambaliPas encore d'évaluation
- Minutes of Meeting On Perioperative NursingDocument5 pagesMinutes of Meeting On Perioperative NursingJeezreelPas encore d'évaluation
- Essential General InstrumentsDocument17 pagesEssential General InstrumentsSimone FrazãoPas encore d'évaluation
- Learn Fron MCQ Mba Net - Copy 1Document64 pagesLearn Fron MCQ Mba Net - Copy 1santosh kumarPas encore d'évaluation
- Intervention Plan Sy 2022 2023 TemplateDocument2 pagesIntervention Plan Sy 2022 2023 TemplateJared Ram JuezanPas encore d'évaluation
- Agen Anti-Infective 2 Jul 2009Document34 pagesAgen Anti-Infective 2 Jul 2009Anonymous SDqQcmgPas encore d'évaluation
- 2019 HSPD Report - WebDocument40 pages2019 HSPD Report - WebNevin SmithPas encore d'évaluation
- Working at Height PolicyDocument7 pagesWorking at Height PolicyAniekan AkpaidiokPas encore d'évaluation
- Yr 9 CORMS IntroductionDocument17 pagesYr 9 CORMS Introduction13obasuyioPas encore d'évaluation
- Excessive Weight Lifting PDFDocument6 pagesExcessive Weight Lifting PDFDownTheTheRabbitHole108Pas encore d'évaluation
- Malamed Local Anesthesia - 1Document100 pagesMalamed Local Anesthesia - 1Ines delacroix33% (3)
- Technical Article Onf Extrusion Process For Preparation of Instant CerealDocument10 pagesTechnical Article Onf Extrusion Process For Preparation of Instant Cerealgurusamy kandasamyPas encore d'évaluation
- Effect of Xylitol With Various Concentration and Duration On The Growth of Candida Albicans (In Vitro Study)Document5 pagesEffect of Xylitol With Various Concentration and Duration On The Growth of Candida Albicans (In Vitro Study)gien fortunasiaPas encore d'évaluation
- DR M Javed Aftab - 2020Document9 pagesDR M Javed Aftab - 2020Dr. Muhammad Javed AftabPas encore d'évaluation
- MS Civil Engineering Construction and Safety Management Assignment No. 1 MCE191010 Abdur RehmanDocument5 pagesMS Civil Engineering Construction and Safety Management Assignment No. 1 MCE191010 Abdur RehmanAbdur RehmanPas encore d'évaluation
- Soal Speaking 11Document9 pagesSoal Speaking 11Naila SaidahPas encore d'évaluation
- Ezra MOV WORK WEEK PLAN 1 NEWDocument6 pagesEzra MOV WORK WEEK PLAN 1 NEWezra britanicoPas encore d'évaluation
- Education in Finland: A Success Story and ModelDocument20 pagesEducation in Finland: A Success Story and ModelZaw Ye HtikePas encore d'évaluation
- STGP Solwel PDFDocument94 pagesSTGP Solwel PDFKoustubh MohantyPas encore d'évaluation
- G10 Las Health Q4Document2 pagesG10 Las Health Q4ALBERT IAN CASUGAPas encore d'évaluation
- Les 3 IELTS WRITING Task 2 - Food WasteDocument4 pagesLes 3 IELTS WRITING Task 2 - Food WasteĐỗ Huy HùngPas encore d'évaluation