Académique Documents
Professionnel Documents
Culture Documents
Paper Malaysian
Transféré par
Julio HuapayaCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Paper Malaysian
Transféré par
Julio HuapayaDroits d'auteur :
Formats disponibles
Malaysian J Pathol 2009; 31(2) : 93 97
ORIGINAL ARTICLE
The manual MGIT system for the detection of M tuberculosis in
respiratory specimens: an experience in the University Malaya
Medical Centre
FADZILAH Mohd Nor
MBBS,
Kee Peng NG
MBBS, PhD,
Yun Fong NGEOW
FRCPath, MD
Department of Medical Microbiology, Faculty of Medicine, University of Malaya, Kuala Lumpur,
Malaysia
Abstract
A prospective study was conducted on 510 respiratory specimens for the presence of M. tuberculosis
detected by direct acid-fast bacilli (AFB) smear examination, culture in the Manual Mycobacteria
Growth Indicator Tube (BBL MGIT, Becton-Dickinson) and culture on Lowenstein-Jensen (LJ)
medium. From positive BBL MGIT tubes, Ziehl-Neelsen and Gram stains were performed and
subcultures were put up on LJ medium. A total of 101 (19.8%) specimens were positive by the BBL
MGIT, 60 (11.8%) by primary LJ medium culture, 31 (6.1%) by direct smear examination and 29
(5.7%) by all three methods. Using primary LJ culture as the gold standard, the sensitivity and
specificity of the BBL MGIT were 90% and 89.6% respectively but the sensitivity of AFB smear
microscopy was only 48.3%. About half (51.1%) of the BBL MGIT false positives were due to
contamination by non-AFB bacteria. The remaining false positives comprised specimens that were
AFB microscopy positive but LJ culture negative. Of the AFB isolates obtained on LJ primary
and sub-cultures, almost all (93.3%) were identified as Mycobacterium tuberculosis complex. The
mean time-to-detection was significantly shorter (p<0.0001) for the BBL MGIT than for LJ culture.
For the former, positive results were available within 14 days for both AFB smear-positive and
AFB smear-negative specimens. On the average, positive results were obtained 1.8 days earlier
for direct AFB smear-positive samples than for AFB smear-negative samples. On the other hand,
positive growth on LJ medium appeared after at least 33 days of incubation. These findings suggest
that the BBL MGIT system will be a suitable alternative to LJ culture for the routine diagnosis
of pulmonary tuberculosis, but a combination of liquid and solid cultures is still required for the
highest diagnostic accuracy.
Keywords: Mycobacterium tuberculosis diagnosis, manual MGIT system
INTRODUCTION
Mycobacterium tuberculosis, the aetiological
agent of tuberculosis (TB), is one of the most
successful bacterial pathogens in the history
of mankind. Despite the availability of antituberculosis chemotherapy for the past 5 decades,
this organism continues to cause extensive
morbidity and mortality, infecting one third of the
worlds population and causing an estimated 8.8
million new cases and approximately 2 million
deaths each year.1 TB is also the primary cause
of death among individuals infected by the human
immunodeficiency virus. The World Health
Organization (WHO) in 1993 declared TB to be a
global public health emergency and reported that
more than 95% of the estimated annual new cases
and deaths occur in the developing world.2
The M. tuberculosis complex comprises
human and bovine strains of M. tuberculosis as
well as M. microti, M. africanum, M. canettii, M.
caprae and M. pinnipedii which are very closely
related genetically but can be differentiated
by biochemical and molecular characteristics.
Currently, all commercially available tests for TB
detect the M. tuberculosis complex as a single
entity. The Mycobacterium Growth Indicator
Tube (MGIT) system from Becton-Dickinson was
introduced about a decade ago as a means to speed
Address for correspondence and reprint requests: Professor Ng Kee Peng, Department of Medical Microbiology, Faculty of Medicine, University of
Malaya, 59603 Kuala Lumpur, Malaysia.Tel: 603 79492418. Email: kpng@ummc.edu.my
93
Malaysian J Pathol
up the isolation of slow-growing mycobacteria.
This is done by liquid culture in a modified
Middlebrook 7H9 broth and detection of growth
by a ruthenium pentahydrate fluorescent oxygen
sensor embedded in silicon at the bottom of
the culture tube. Oxygen reduction induced
by metabolising bacteria reduces fluorescence
quenching. Hence, the level of fluorescence
that the tube emits corresponds to the amount
of oxygen consumed by organisms in the tube,
and is proportional to the number of bacteria
present.
This test is now automated for continuous
monitoring in the BACTEC MGIT 960 (Becton
Dickinson) but the older manual system requires
tubes to be examined for fluorescence under a
Woods lamp or with some other long wave UV
light source. Though requiring more technical
time, the manual system is a lot more affordable
for laboratories with a smaller budget. In this
study, the manual MGIT system (BBL MGIT)
from Becton Dickinson was evaluated against
conventional culture on Lowenstein-Jensen (LJ)
agar slopes and microscopical examination for
acid-fast bacilli (AFB) in Ziehl-Neelsen (ZN)
stained smears.
MATERIALS AND METHODS
Clinical samples
The clinical samples studied comprised sputa,
bronchoalveolar lavages, pleural fluids and
tracheal aspirates collected from patients
suspected to be having pulmonary or pleural
TB. These were all consecutive samples received
in the TB and Fungus Laboratory, University
Malaya Medical Centre, from March 28, 2007
until September 26, 2007. All specimens were
processed for AFB smear microscopy and culture
on the day of collection.
Microscopy
Smears were screened by Auramine-O
fluorescence microscopy under 40x magnification.
Positive smears were re-examined with ZN
staining for AFB under oil immersion.
Culture on Lowenstein-Jensen medium
Regardless of microscopy results, all specimens
were decontaminated and digested using the
BBL MycoPrep Reagent (Becton Dickinson)
containing N-acetyl L-cysteine- 2% sodium
hydroxide (NALC-NaOH). For each specimen,
equal volumes (about 1 ml each) of reagent and
specimen were pipetted into a centrifuge tube,
vortexed briefly and allowed to stand at room
94
December 2009
temperature for 15 minutes. The BBL MycoPrep
Phosphate Buffer (pH6.8) was added to the 10
ml mark on the centrifuge tube and the resulting
mixture was centrifuged at 3,000 rpm for 15
minutes. The supernatant fluid was discarded.
A small amount of phosphate buffer was added
to resuspend the sediment which was used to
inoculate a slant of LJ medium (Oxoid). All
cultures were incubated at 370C and examined
daily until the appearance of colonies resembling
mycobacteria. ZN staining was carried out on
the colonies to identify AFB. Confirmed AFB
were sent to the TB Reference Laboratory at the
National Public Health Laboratory, Sg. Buloh,
Selangor, for speciation.
The time-to-detection for LJ culture was
defined as the time between inoculation and
the earliest reading when colonies resembling
mycobacteria were noted on the agar surface.
Specimens were considered culture negative if
there were still no colonies formed after 8 weeks
of incubation.
Culture by the manual MGIT system (BBL
MGIT)
Specimens were decontaminated and digested as
described above for LJ culture. A portion (0.5ml)
of the processed specimen was inoculated into
each BBL MGIT tube together with BACTEC
MGIT Growth supplement (oleic acid-albumindextrose-catalase) and BBL MGIT PANTA
antibiotic mixture (polymyxin B, amphotericin
B, nalidixic acid, trimethoprim, and azlocillin).
The BBL MGIT tubes were incubated at 370C
and examined daily in a 365nm wavelength UV
light source fluorescence detector (Bactec TM
MicroMGIT device, Sparks, MD, Maryland,
USA) up to 8 weeks of incubation. A positive
and a negative control tube were included with
every batch of test tubes examined. In addition,
bacterial growth was detected by the presence
of a non-homogenous turbidity or small grains
or flakes in the culture medium. When a tube
was found to be positive for bacterial growth, a
portion of the tube content was removed and used
to prepare two smears, one for ZN staining and
one for Gram staining. If AFB were present in
the ZN smear, the tube content was subcultured
onto a slant of LJ medium. If organisms grew on
subculture and were identified as M. tuberculosis
complex, the BBL MGIT culture was considered
a true positive. However, if AFB were not seen
but the Gram stained smear showed other bacteria
or fungi, the BBL MGIT culture was considered
contaminated. Time-to-detection was defined
MGIT SYSTEM FOR M TUBERCULOSIS
as the interval between the incubation of an
inoculated tube and a positive reading in a tube
whose content was also AFB smear positive.
RESULTS
During the 6-month study period, a total of 510
respiratory specimens collected from 332 patients
were processed. The specimen types consisted
of 457sputum samples (90.0%). 37 pleural fluids
(7.0%), 10 bronchoalveolar lavages (2.0%), and
6 tracheal secretions (1.0%)
The results showed 101 (19.8%) positives by
the BBL MGIT, 60 (11.7%) by LJ medium culture,
31 (6.1%) by direct AFB smear examination and
29 (5.7%) by all three methods (Tables 1 & 2).
From the speciation tests carried out in the
National Reference TB Laboratory, Sg. Buluh,
54 (93.3%) of the 60 isolates on LJ agar were
identified as M. tuberculosis complex. Members
of the M. fortuitum complex made up the
remaining 6 isolates.
Sensitivity and specificity
The BBL MGIT was positive for all the LJ culture
positive specimens except for 6 specimens that
grew M. tuberculosis complex, thus giving a
sensitivity of 90% (54/60) against LJ culture. In
contrast, the sensitivity of the AFB microscopy
was only 48.3% (29/60). Of the 54 BBL MGIT
positives, 29 (53.7%) were ZN smear positive
and 25 (46.3%) were ZN smear negative. The
specificity of the BBL MGIT was calculated to be
89.6%, as this test was negative in 403 of the 450
LJ culture negative specimens. Of the 47 false
positives defined by the absence of mycobacterial
growth on LJ agar, 24 were due to obvious
contamination by other aerobic bacteria, thus
giving an overall breakthrough contamination
rate of 4.7% (24/510) for the BBL MGIT
system. In the other 23 BBL MGIT positive
tubes, AFB were seen in the ZN stains done on
the tube contents but the LJ subcultures were
negative for mycobacteria. The corresponding
primary LJ cultures of these specimens were
also negative. Two specimens were positive by
direct AFB smear examination but negative by
both culture systems. Clinical information was
not available to determine whether or not these
specimens were taken after the start of anti-TB
treatment.
Repeat samples
Of 107 patients who gave repeat samples (2 to 3
samples each), the BBL MGIT test was negative
in 80 and positive in 27 patients. Discrepant
results from consecutive cultures were seen in
only 6 (5.6%) patients.
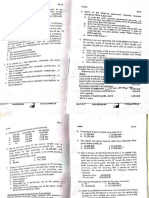
TABLE 1. BBL MGIT and LJ culture results in direct AFB microscopy positive specimens
BBL MGIT +
BBL MGIT
Total
LJ culture +
29
29
LJ culture
Total
29
31
+ Positive result
Negative result
TABLE 2. BBL MGIT and LJ culture results in direct AFB microscopy negative specimens
excluding specimens with negative results in all 3 tests
BBL MGIT +
BBL MGIT
Total
LJ culture +
25
31
LJ culture
47*
47
Total
72
78
+ Positive result
Negative result
* Made up of 23 tubes that were positive in the AFB stain but negative in the LJ subculture and 24
tubes with Gram-stain showing contamination by other bacteria.
95
Malaysian J Pathol
Time to detection
The mean time to detection by culture was
determined for AFB smear-positive versus
AFB smear-negative specimens. With the AFB
smear-positive specimens, the mean times to
detection were 11.5 days (SD 3.4 days; median,
12.0 days) with the BBL MGIT system, and 31.2
days (SD 5.8 days; median 32.0 days) with LJ
culture. For AFB smear- negative specimens,
the corresponding times were 13.2 days (SD 5.0
days; median 13.0 days) with the BBL MGIT
system, and 35.3 days (SD 5.3 days; median 34.0
days) with LJ culture. The difference between
BBL MGIT and LJ culture was statistically
significant (p<0.0001).
DISCUSSION
TB in its typical clinical presentation is often
diagnosed and treated on suspicion. Laboratory
confirmation is however, very important not only
for the optimal management of patients and their
close contacts, but also for the generation of
accurate epidemiological data to be used as the
foundation for appropriate and effective control
strategies. The strength of the laboratory network
in a country is often a direct reflection of the
success of its TB control programme.
Improvements in the laboratory diagnosis of
TB have focused on the reduction of turn-around
time for detection and drug susceptibility testing,
to allow for earlier detection of drug resistance
and treatment failure. Light microscopy is rapid,
inexpensive, technically simple, and specific
for AFB, but will only detect open infectious
cases of TB. The overall sensitivity of AFB
microscopy has been reported to be 22 to 78%
for respiratory specimens. While 106 AFB/ml of
sputum usually results in a positive smear, the
detection rate drops to 60% if 104 AFB/ml are
present and to only 10% if less than 103 AFB/ml
are in the smear.3,4 Microscopy is frequently
negative for non-respiratory specimens because
of the lower bacterial load, and for NTM, because
some species have cell walls that do not stain
well in AFB stains.5 Furthermore, microscopy
will not discriminate between M. tuberculosis
and other mycobacteria, nor viable from dead
bacilli. Hence, microscopy is not very useful
for the diagnosis of early TB, post-treatment
TB and some NTM infections. However, it
is of epidemiologic and clinical interest to be
able to diagnose TB in patients who are AFB
smear-negative, because at this stage they are
less contagious and have lower morbidity and
mortality.6,7
96
December 2009
M. tuberculosis culture is still the cornerstone
on which definitive diagnosis of TB relies. It
can be performed on a variety of respiratory and
non-respiratory samples, is much more sensitive
than microscopy and allows the recovery
of the bacteria for other studies, such as the
identification of mycobacterial species, drug
susceptibility testing and genotyping. Liquid
cultures generally require a shorter incubation
time than culture on solid media for the detection
of M. tuberculosis.8 Automated systems such as
the BACTEC MGIT 960, ESP Culture System II,
and MB/BacT ALERT 3D system enable large
numbers of specimens to be processed rapidly
with positive results appearing usually within 1012 days of incubation. However, these systems
have similar problems of contamination, crosscontamination and the need for subculture onto
solid media for the confirmation of identity and
purity. Cruciani et al.,9 in a meta-analysis of 10
studies, reported that the BACTEC 960/MGIT
and BACTEC 460 systems showed a sensitivity
and specificity in detecting mycobacteria of 81.5
and 99.6% and 85.8 and 99.9%, respectively, but
when combined with solid media, the sensitivity
of the two systems increased to 87.7 and
89.7%, respectively. Both systems had a higher
sensitivity for smear-positive specimens. Rates
of breakthrough contamination were 12.8% with
solid media, 8.6% with the BACTEC 960/MGIT
and 4.4% with the BACTEC 460.
In this study, the sensitivity (90%) and
breakthrough contamination rate (4.7%) of the
manual BBL MGIT were better than those of
the automated BACTEC systems described
in Crucianis meta-analysis but the specificity
(89.6%) was significantly lower. This inferior
specificity could be due to the large number of
specimens that were considered false positives
in the BBL MGIT because they were negative in
the ZN smear and LJ primary and subcultures.
Although technical error could not be ruled
out, some of these apparent false positives
could be due to the growth of non-tuberculous
mycobacterial species that require special
growth factors not provided in LJ medium, or
grew better in liquid than solid media.10 With
the exclusion of these contentious results, the
BBL MGIT specificity would be 92.8%. As
reported by other workers 9,10 the BBL MGIT
was positive more often for AFB smear-positive
than smear-negative specimens and the mean
time-to-detection was significantly shorter for
the BBL MGIT than for LJ culture, for both
AFB smear-positive and AFB smear-negative
MGIT SYSTEM FOR M TUBERCULOSIS
specimens. The highest recovery rate is also
obtained with a combination of liquid and solid
media.
Overall, the findings in this study indicate a
useful role for the manual BBL MGIT system
in the routine diagnosis of pulmonary TB,
especially in laboratories with a small number
of specimens for TB detection. Although it
is more costly and laborious, it has distinct
advantages over the conventional LJ culture with
respect to faster growth and better growth of
fastidious mycobacterial species. Nevertheless,
as shown by the 6 LJ culture positive but BBL
MGIT negative specimens, a combination of
solid and liquid culture systems is still required
for the highest recovery of mycobacteria from
clinical specimens. Furthermore, as shown by the
inconsistent detection in some repeat samples,
the sensitivity of culture will increase with more
number of specimens cultured.
9. Cruciani M., Scarparo C, Malena M, Bosco O,
Serpelloni G, Mengoli C. Meta-analysis of BACTEC
MGIT 960 and BACTEC 460 TB, with or without
Solid Media, for Detection of Mycobacteria. J Clin
Microbiol. 2004 May; 42(5): 23215.
10. Vibeke stergaard Thomsen V, Dragsted UB, Bauer
J, Fuursted K, Lundgren J. Disseminated Infection
with Mycobacterium genavense: a Challenge
to Physicians and Mycobacteriologists. J Clin
Microbiol 1999;37:3901-5
ACKNOWLEDGEMENT
The authors thank Becton Dickinson Malaysia
for the supply of BBL MGIT kits and technical
support.
REFERENCES
1. Dye C, Scheele S, Dolin P, et al. Consensus
statement. Global burden of tuberculosis: Estimated
incidence, prevalence, and mortality by country.
WHO Global Surveillance and Monitoring Project.
JAMA 1999;282:677-86
2. Sudre P, Dam GT, Kochi A. Tuberculosis: a global
overview of situation today. Bull.WHO 1992;149-59.
3. Palomino JC. Nonconventional and new methods
in the diagnosis of tuberculosis: Feasibility and
applicability in the field. Eur Respir J 2005;26;33950
4. Pfyffer GE, Brown-Elliot BA, Wallace Jr RJ.
Mycobacterium: General characteristics,
isolation and staining procedures. Manual Clin
Microbiol 2003;532-59
5. Lipsky BA, Gates J, Tenover FC, Plorde JJ. Factors
affecting the clinical value of
microscopy for acid-fast bacilli. Rev Infect Dis
1984;6:214-22
6. Menzies D. Issues in the management of contacts
in patients with active pulmonary tuberculosis. Can
J Public Health 1997;88:197-201
7. Behr MA, Warren SA, Salamon H, et al.
Transmission of Mycobacterium tuberculosis from
patients smear-negative for acid-fast bacilli. Lancet
1999;353:444-9
8. Morgan MA, Horstmeier CD, De Young DR, Robers
GD. Comparison of radiometric method (BACTEC)
and conventional culture media for recovery of
mycobacteria from smear-negative specimens. J
Clin Microbiol 1983;18:384-8
97
Vous aimerez peut-être aussi
- Hypercalcemia MalignancyDocument1 pageHypercalcemia MalignancyJulio HuapayaPas encore d'évaluation
- Clinical Experience 6 Cases 2003Document6 pagesClinical Experience 6 Cases 2003Julio HuapayaPas encore d'évaluation
- Quality of Life of Idiopathic Pulmonary Fibrosis Patients 2001Document8 pagesQuality of Life of Idiopathic Pulmonary Fibrosis Patients 2001Julio HuapayaPas encore d'évaluation
- MecanografiaDocument4 pagesMecanografiaJulio HuapayaPas encore d'évaluation
- Development of The ATAQ-IPf 2010Document9 pagesDevelopment of The ATAQ-IPf 2010Julio HuapayaPas encore d'évaluation
- Nocardia and Lung 66 Cases ReviewDocument7 pagesNocardia and Lung 66 Cases ReviewJulio HuapayaPas encore d'évaluation
- Review Quality of Life IPFDocument7 pagesReview Quality of Life IPFJulio HuapayaPas encore d'évaluation
- Descriptive Patterns Severe Pulmonary Hypertension Compared To EchoDocument8 pagesDescriptive Patterns Severe Pulmonary Hypertension Compared To EchoJulio HuapayaPas encore d'évaluation
- Imaging in Pulmonary HypertensionDocument17 pagesImaging in Pulmonary HypertensionJulio HuapayaPas encore d'évaluation
- Analysis Regression TreesDocument10 pagesAnalysis Regression TreesJulio HuapayaPas encore d'évaluation
- Right Ventricular Dysfuction PDFDocument6 pagesRight Ventricular Dysfuction PDFJulio HuapayaPas encore d'évaluation
- Analysis Lancet Study GabapentinDocument2 pagesAnalysis Lancet Study GabapentinJulio HuapayaPas encore d'évaluation
- Bonus 2010 FA Step 1 Micro HIVDocument1 pageBonus 2010 FA Step 1 Micro HIVGabriel F. SotoPas encore d'évaluation
- Heffner Chest 1997Document13 pagesHeffner Chest 1997Julio HuapayaPas encore d'évaluation
- Machu PicchuDocument16 pagesMachu PicchuJulio HuapayaPas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Lesson On Inferring Tone and MoodDocument32 pagesLesson On Inferring Tone and MoodAngel PabilloPas encore d'évaluation
- PRTC Tax Final Preboard May 2018Document13 pagesPRTC Tax Final Preboard May 2018BonDocEldRicPas encore d'évaluation
- The Prediction of Travel Behaviour Using The Theory of Planned BehaviourDocument16 pagesThe Prediction of Travel Behaviour Using The Theory of Planned Behaviourhaneena kadeejaPas encore d'évaluation
- Fogarty HardwickDocument35 pagesFogarty HardwickBen KellerPas encore d'évaluation
- Do 18-A and 18 SGV V de RaedtDocument15 pagesDo 18-A and 18 SGV V de RaedtThomas EdisonPas encore d'évaluation
- Sand Cone Method: Measurement in The FieldDocument2 pagesSand Cone Method: Measurement in The FieldAbbas tahmasebi poorPas encore d'évaluation
- Bebras2021 BrochureDocument5 pagesBebras2021 BrochureJeal Amyrrh CaratiquitPas encore d'évaluation
- Soal Passive VoiceDocument1 pageSoal Passive VoiceRonny RalinPas encore d'évaluation
- Mall Road HistoryDocument3 pagesMall Road HistoryKaleem Ahmed100% (1)
- ATM BrochuresDocument5 pagesATM Brochuresगुंजन सिन्हाPas encore d'évaluation
- Corporation True or FalseDocument2 pagesCorporation True or FalseAllyza Magtibay50% (2)
- Max3080 Max3089Document21 pagesMax3080 Max3089Peter BirdPas encore d'évaluation
- Math Grade 7 Q2 PDFDocument158 pagesMath Grade 7 Q2 PDFIloise Lou Valdez Barbado100% (2)
- SPM Bahasa Inggeris PAPER 1 - NOTES 2020Document11 pagesSPM Bahasa Inggeris PAPER 1 - NOTES 2020MaryPas encore d'évaluation
- NE5000E V800R003C00 Configuration Guide - QoS 01 PDFDocument145 pagesNE5000E V800R003C00 Configuration Guide - QoS 01 PDFHoàng Tùng HưngPas encore d'évaluation
- Drimaren - Dark - Blue HF-CDDocument17 pagesDrimaren - Dark - Blue HF-CDrajasajjad0% (1)
- The Role of The Board of Directors in Corporate GovernanceDocument12 pagesThe Role of The Board of Directors in Corporate GovernancedushyantPas encore d'évaluation
- Span of ControlDocument8 pagesSpan of Controlnaveen_gwl100% (4)
- Education-and-Life-in-Europe - Life and Works of RizalDocument3 pagesEducation-and-Life-in-Europe - Life and Works of Rizal202202345Pas encore d'évaluation
- Aristotle Metaphysics Book V-Delta SachsDocument10 pagesAristotle Metaphysics Book V-Delta Sachsvmishka100% (1)
- How To Get Into Top IIMs - Ahmedabad, Bangalore, Calcutta and Lucknow - CareerAnnaDocument97 pagesHow To Get Into Top IIMs - Ahmedabad, Bangalore, Calcutta and Lucknow - CareerAnnaMoinak94Pas encore d'évaluation
- Part 1: Hôm nay bạn mặc gì?Document5 pagesPart 1: Hôm nay bạn mặc gì?NamPas encore d'évaluation
- Bible QuizDocument4 pagesBible QuizjesukarunakaranPas encore d'évaluation
- Thesis - Behaviour of Prefabricated Modular Buildings Subjected To Lateral Loads PDFDocument247 pagesThesis - Behaviour of Prefabricated Modular Buildings Subjected To Lateral Loads PDFFumaça FilosóficaPas encore d'évaluation
- Farm Gate TasmaniaDocument20 pagesFarm Gate TasmaniaplouffrPas encore d'évaluation
- System of Units: Si Units and English UnitsDocument7 pagesSystem of Units: Si Units and English UnitsJp ValdezPas encore d'évaluation
- Offsites Engineering Works For The Erbil Refinery 40,000 B/D Expansion ProjectDocument12 pagesOffsites Engineering Works For The Erbil Refinery 40,000 B/D Expansion ProjectSardar PerdawoodPas encore d'évaluation
- EPM Key Design Decisions - Design PhaseDocument7 pagesEPM Key Design Decisions - Design PhaseVishwanath GPas encore d'évaluation
- KULT Divinity Lost - Scenario - An Echo From The Past (28-29)Document2 pagesKULT Divinity Lost - Scenario - An Echo From The Past (28-29)Charly SpartanPas encore d'évaluation
- B Blunt Hair Color Shine With Blunt: Sunny Sanjeev Masih PGDM 1 Roll No.50 Final PresentationDocument12 pagesB Blunt Hair Color Shine With Blunt: Sunny Sanjeev Masih PGDM 1 Roll No.50 Final PresentationAnkit Kumar SinghPas encore d'évaluation