Académique Documents
Professionnel Documents
Culture Documents
Choice of Vasopressor in Septic Shock: Does It Matter?: Commentary
Transféré par
joseluisjams0 évaluation0% ont trouvé ce document utile (0 vote)
19 vues2 pagesChoice of vasopressor in septic shock: does it matter?
Titre original
Do Pamina
Copyright
© © All Rights Reserved
Formats disponibles
PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentChoice of vasopressor in septic shock: does it matter?
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
19 vues2 pagesChoice of Vasopressor in Septic Shock: Does It Matter?: Commentary
Transféré par
joseluisjamsChoice of vasopressor in septic shock: does it matter?
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 2
Available online http://ccforum.
com/content/11/6/174
Commentary
Choice of vasopressor in septic shock: does it matter?
Gourang P Patel and Robert A Balk
Rush Medical College, Rush University Medical Center, 1753 West Congress Parkway, Chicago, Illinois 60612, USA
Corresponding author: Robert A Balk, rbalk@rush.edu
Published: 6 November 2007
This article is online at http://ccforum.com/content/11/6/174
2007 BioMed Central Ltd
Critical Care 2007, 11:174 (doi:10.1186/cc6159)
Abstract
In an attempt to determine the optimum vasopressor to use in
the management of patients with septic shock, Annane and
coworkers conducted a multicenter, prospective, randomized,
double-blind, controlled clinical trial evaluating epinephrine
versus norepinephrine (with dobutamine, if indicated) in the
management of a well-defined adult population with septic
shock [1]. The trial involved patients from 19 intensive care
units throughout France and was funded by the French
Ministry of Health. The study enrolled adults with well-defined
septic shock and evidence of organ dysfunction and/or
hypoperfusion. The primary outcome parameter was 28 day
all-cause mortality. Despite finding a significantly higher
arterial lactate level and lower pH during the first four days of
therapy in the epinephrine treated patients, there was not a
significant difference in 28 day all-cause mortality or other
important outcome parameters. Specifically, there was no
significant difference in discharge from the intensive care unit
(ICU) or hospital, hemodynamic parameters, vasopressor
withdrawal or organ dysfunction between the two treatment
strategies. Importantly, there was also no difference in
adverse events, such as arrhythmias or cardiac, neurologic, or
ischemic events [1].
Septic shock is a medical emergency that is associated with
mortality rates of 40-70%. Prompt recognition and institution of
effective therapy is required for optimal outcome. When the shock
state persists after adequate fluid resuscitation, vasopressor
therapy is required to improve and maintain adequate tissue/organ
perfusion in an attempt to improve survival and prevent the
development of multiple organ dysfunction and failure. Controversy
surrounding the optimum choice of vasopressor strategy to utilize
in the management of patients with septic shock continues. A
recent randomized study of epinephrine compared to norepinephrine (plus dobutamine when indicated) leads to more
questions than answers.
The significant economic and mortality impact of severe
sepsis and septic shock has often resulted in some
controversy concerning optimum management strategies,
particularly in regard to choice of vasopressor support [1,2].
Annane and colleagues have recently reported on the
evaluation of two vasopressor strategies in a multicenter trial
of adult French septic shock patients [1]. The results of such
controlled clinical trials are valuable to clinicians since septic
shock has a reported mortality rate of 40-70% and currently
there are no convincing data supporting the use of one
vasopressor strategy over another [2]. Current consensus
recommendations from 11 different societies in the Surviving
Sepsis Campaign guidelines recommend either dopamine or
norepinephrine as the initial vasopressor for patients with
septic shock [3]. The 2004 practice parameter for
hemodynamic support of sepsis in adult patients from the
Society of Critical Care Medicine (SCCM) also recommends
the use of dopamine or norepinephrine as the initial
vasopressor(s) to use in adults with septic shock [4].
Dopamine was the traditional vasopressor choice for shock
management, until recent reports of dopamine resistance
and/or its potential for tachyarrhythmias resulted in norepinephrines emergence as the preferred initial vasopressor
in North America and Europe [4-6].
As we consider these intriguing results from the study by
Annane and coworkers we are impressed by the intricacies of
study design and acknowledge their use of an expanded
definition for early septic shock in the inclusion and exclusion
criteria for study enrollment. The study was multi-centered,
randomized, with a double-blind treatment algorithm. The
study participants were reasonably well randomized at the
start. The majority of infections were community acquired with
the lung as the predominant site of infection. Given the
predominance of dopamine use in North America and
Europe, we were surprised investigators chose to compare
epinephrine and norepinephrine [4-6]. A trial design
comparing norepinephrine to dopamine, epinephrine, and
possibly vasopressin or phenylephrine would have had more
ICU = intensive care unit; SCCM = Society of Critical Care Medicine.
Page 1 of 2
(page number not for citation purposes)
Critical Care
Vol 11 No 6
Patel and Balk
clinical relevance for physicians in North America and Europe
[4-6]. The use of epinephrine as an initial vasopressor for the
management of septic shock would represent a significant
paradigm shift for North America and a majority of Europe
[5,6].
In regard to the study results, it is remarkable that the 28 day
all-cause mortality rate was 40% in the epinephrine and 34%
in the norepinephrine patients [1]. This impressive mortality
rate is lower than typical reports of 40-70% for septic shock
patients and raises questions regarding the reason for the
improvement in 28 day all-cause mortality rate [2]. This
observation is even more curious in light of the increased
arterial lactate and lower pH in the epinephrine group over
the first few days of management. Even though there was
recovery of this metabolic derangement by the fourth study
day, there did not appear to be any adverse sequelae. The
finding that epinephrine can produce exaggerated aerobic
glycolysis within muscles, decrease splanchnic and hepatic
blood flow, and may increase oxygen consumption, despite
an increase in oxygen delivery to the tissues likely explains the
increased arterial lactate and reduced pH [4,7,8]. Lactate has
been an important surrogate marker for assessing tissue
hypoperfusion [9]. Its measurement and prognostic implications have resulted in its incorporation into sepsis bundles
which have been widely adopted to guide initial sepsis
management [10,11]. Rivers and colleagues also reported a
distinct correlation between lactate clearance and outcome in
septic shock [9,12]. Increased lactate formation and delayed
clearance of lactate have been associated with increased
mortality rates in septic shock patients [9]. However, these
results demonstrate a survival benefit irregardless of the early
increases in lactate formation and presumed decrease in
clearance. The explanation for the positive survival benefits
could be related to the potential impact of the high
prevalence of steroid use (approximately 80% of all patients)
in this study. This percent of patients managed with
corticosteroid replacement therapy is higher that the typical
sepsis trial and represents yet another controversial area of
sepsis management [5]. Finally, it is noteworthy that adverse
events reported during this trial were similar. The authors also
evaluated the patients for significant ischemic events
involving the cardiac, neurologic, or peripheral circulation and
again there were no significant differences between the two
groups, supporting the safety of epinephrine in this study
population.
We applaud the efforts of the French investigators to
determine if there is a preferred vasopressor to use in septic
shock. The current study was particularly well-done, but
unfortunately, did not answer the question and raised
additional questions for the practicing intensivists. The
excellent survival results of this current trial (approximately
60%) for both epinephrine and norepinephrine treated
patients raises the question of whether the excellent outcome
was reflective of the vasopressor strategy, increased
Page 2 of 2
(page number not for citation purposes)
corticosteroid use, or another variable. The epinephrine
outcomes were even more impressive in light of the initial
increase in arterial lactate and decrease in pH observed in
these patients compared to the norepinephrine treatment. To
help answer these questions and determine if there is a best
vasopressor we need another large, multicenter, prospective, randomized, controlled trial to compare norepinephrine,
dopamine, and epinephrine. Until this data becomes
available, it appears that there is no clear best vasopressor
to use in the management of adults with septic shock.
Competing interests
The authors declare that they have no competing interests.
References
1.
Annane D, Vignon P, Renault A, Bollaert EP, Charpentier C,
Martin C, Troche G, Ricard JD, Nitenberg GN, Papazian L,
Azoulay E, Bellissant E, for the CATS Study Group: Norepinephrine plus dobutamine versus epinephrine alone for the management of septic shock: A randomized trial. Lancet 2007,
370:676-684.
2. Russel JA: Management of sepsis. N Engl J Med 2006, 355:
1699-1713.
3. Dellinger RP, Carlet JM, Masur H, Gerlach H, Calandra T, Cohen
J, Gea-Banacloche J, Keh D, Marshall JC, Parker MM, et al.: Surviving Sepsis Campaign Guidelines for the management of
patients with sepsis and septic shock. Crit Care Med 2004,
32:858-873.
4. Hollenberg SM, Ahrens TS, Annane D, et al.: Practice parameters for hemodynamic support of sepsis in adult patients:
2004 update. Crit Care Med 2004, 32:1928-1948
5. Levy B, Dusang B, Annane D, Annane D, Gibot S, Bollaert PE,
and the College Interregional Des Reanimateurs du Nord-Est:
Cardiovascular response to dopamine and early prediction of
outcome in septic shock: A prospective multiple-center study.
Crit Care Med 2005, 33:2172-2177.
6. Sakr Y, Reinhart K, Vincent JL, Spring CL, Moreno R, Ranieri M,
De Backer D, Payen D: Does dopamine administration in
shock influence outcome? Results of the Sepsis Occurrence
in Acutely Ill Patients (SOAP) Study. Crit Care Med 2006,
34:589-597.
7. Levy B, Bollaert PE, Charpentier C, Nace L, Audibert G, Bauer P,
Nabet P, Larcan A: Comparison of norepinephrine and dobutamine to epinephrine for hemodynamics, lactate metabolism,
and gastric tonometric variables in septic shock: a prospective, randomized study. Intes Care Med 1997, 23:282-287.
8. Seguin P, Bellissant E, Le Tulzo Y, Laviolle B, Lessard Y, Thomas
R, Malledant Y: Effects of epinephrine compared with the
combination of dobutamine and norepinephrine on gastric
perfusion in septic shock. Clin Pharm Ther 2002, 71:381-388.
9. Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B,
Peterson E, Tomlanovich M, for the Early Goal-Directed Therapy
Collaborative Group: Early-goal directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 2001,
345:1368-1377.
10. Levy MM, Pronovost PJ, Dellinger RP, Townsend S, Resar RK,
Clemmer TP, Ramsay G: Sepsis change bundles: Converting
guidelines into meaningful change in behavior and clinical
outcome. Crit Care Med 2004, 32:S595-S597.
11. Kortgen A, Niederprum P, Bauer M: Implementation of an evidenced-based standard operating procedure and outcome
in septic shock Crit Care Med 2006 34:943-949.
12. Nguyen HB, Rivers EP, Knobloch BP, Jacobsen G, Muzzin A,
Ressler JA, Tomlanovich MC: Early lactate clearance is associated with improved outcome in severe sepsis and septic
shock. Crit Care Med 2004, 32:1637-1642.
Vous aimerez peut-être aussi
- DSM 5 Vs DSM 4 Case StudiesDocument18 pagesDSM 5 Vs DSM 4 Case Studiesapi-261267976100% (1)
- Pulmonary HipertensionDocument481 pagesPulmonary HipertensionFransiskus A Danu KrisbiantoroPas encore d'évaluation
- Pals Studyguide Jan2021Document3 pagesPals Studyguide Jan2021prippon100% (2)
- Metabolic Acidosis - Alkalosis Study GuideDocument1 pageMetabolic Acidosis - Alkalosis Study GuideJe KirstenePas encore d'évaluation
- Emergency Care Emt 13th Edition Ebook PDFDocument61 pagesEmergency Care Emt 13th Edition Ebook PDFadolfo.milliken17896% (49)
- Cardio Vol23no1Document44 pagesCardio Vol23no1Taman TirtoPas encore d'évaluation
- Management of Pulmonary Arterial Hypertension (PAH)Document119 pagesManagement of Pulmonary Arterial Hypertension (PAH)caishamPas encore d'évaluation
- DemetiaDocument288 pagesDemetialiramishelPas encore d'évaluation
- Short Diagnosis Report: PatientDocument6 pagesShort Diagnosis Report: PatientCarmen JurcoanePas encore d'évaluation
- Complementary and Alternative Medical Lab Testing Part 8: UrologyD'EverandComplementary and Alternative Medical Lab Testing Part 8: UrologyÉvaluation : 3 sur 5 étoiles3/5 (1)
- Pulmonary Hipertension PDFDocument481 pagesPulmonary Hipertension PDFRadhiatul AdillahPas encore d'évaluation
- Burke-Fahn-Marsden Dystonia Rating ScaleDocument2 pagesBurke-Fahn-Marsden Dystonia Rating ScaleCNS WARDPas encore d'évaluation
- 10 1016@j Chest 2020 09 269Document29 pages10 1016@j Chest 2020 09 269Wanderson100% (1)
- Top Trials in Gastroenterology & Hepatology, 2nd EditionD'EverandTop Trials in Gastroenterology & Hepatology, 2nd EditionPas encore d'évaluation
- ECTDocument11 pagesECTmanu sethi75% (4)
- Psychological Complication in PuerperiumDocument17 pagesPsychological Complication in PuerperiumAnitha ThankappanPas encore d'évaluation
- Clinical ResearchDocument13 pagesClinical ResearchkarmilaPas encore d'évaluation
- 5 Recent Trials in Stress Ulcer ProphylaxisDocument6 pages5 Recent Trials in Stress Ulcer ProphylaxisCharan Teja Reddy AvulaPas encore d'évaluation
- Ardsnetwork (Nhlbi) Studies: Successesand Challengesinards ClinicalresearchDocument10 pagesArdsnetwork (Nhlbi) Studies: Successesand Challengesinards ClinicalresearchEduardo SoaresPas encore d'évaluation
- Real World Experiences Pirfenidone and Nintedanib Are Effective and Well Tolerated Treatments For Idiopathic Pulmonary FibrosisDocument12 pagesReal World Experiences Pirfenidone and Nintedanib Are Effective and Well Tolerated Treatments For Idiopathic Pulmonary FibrosismaleticjPas encore d'évaluation
- Low-Versus High-Chloride Content Intravenous Solutions For Critically Ill and Perioperative Adult Patients: A Systematic Review and Meta-AnalysisDocument9 pagesLow-Versus High-Chloride Content Intravenous Solutions For Critically Ill and Perioperative Adult Patients: A Systematic Review and Meta-AnalysisAlexandre CavalcantiPas encore d'évaluation
- Goz 043Document8 pagesGoz 043nPas encore d'évaluation
- Vignon Echo Fluid ResponsivenessDocument46 pagesVignon Echo Fluid ResponsivenesscsquizzardPas encore d'évaluation
- Criterio Nuevo para Transfusion 2014Document2 pagesCriterio Nuevo para Transfusion 2014Humberto Liu BejaranoPas encore d'évaluation
- High-Flow Nasal Oxygen-The Pendulum Continues To Swing in The Assessment of Critical Care TechnologyDocument2 pagesHigh-Flow Nasal Oxygen-The Pendulum Continues To Swing in The Assessment of Critical Care TechnologyRodrigoSachiFreitasPas encore d'évaluation
- 12 - 2015 - LT Safety and Efficacy of Imatinib in PAH - IMPRES (10) 70Document10 pages12 - 2015 - LT Safety and Efficacy of Imatinib in PAH - IMPRES (10) 70edward the iiiPas encore d'évaluation
- Peep, Prona e Proteina C ReativaDocument0 pagePeep, Prona e Proteina C ReativaEduardo SoaresPas encore d'évaluation
- ARA II y Cancer EditorialDocument2 pagesARA II y Cancer EditorialFabiana MuriasPas encore d'évaluation
- Zampieri 2019Document8 pagesZampieri 2019Peter AgabaPas encore d'évaluation
- Current Therapy of Eisenmenger Syndrome: PMC DisclaimerDocument7 pagesCurrent Therapy of Eisenmenger Syndrome: PMC DisclaimerANISA RIFKA RIDHOPas encore d'évaluation
- Argenta 2011Document4 pagesArgenta 2011NYONGKERPas encore d'évaluation
- Heart & Lung: Ying Guo, MD, Wei Gao, MD, Hongxia Yang, MD, Cheng 'En Ma, MD, Shujian Sui, MDDocument6 pagesHeart & Lung: Ying Guo, MD, Wei Gao, MD, Hongxia Yang, MD, Cheng 'En Ma, MD, Shujian Sui, MDnoviPas encore d'évaluation
- The Use of Sildenafil in Persistent Pulmonary Hypertension of The Newborn PDFDocument6 pagesThe Use of Sildenafil in Persistent Pulmonary Hypertension of The Newborn PDFmaciasdrPas encore d'évaluation
- Cherukuri Et Al. 2018 - Home Haemodialysis Treatment and Outcomes, Retrospective Analysis of KIHDNEyDocument10 pagesCherukuri Et Al. 2018 - Home Haemodialysis Treatment and Outcomes, Retrospective Analysis of KIHDNEyShareDialysisPas encore d'évaluation
- 2014 Prednisolone vs. Pentoxifylline For Severe Alcoholic HepatitisDocument2 pages2014 Prednisolone vs. Pentoxifylline For Severe Alcoholic HepatitisJairo Torres SoteloPas encore d'évaluation
- 8 - The Effectiveness of A Routine Versus An Extensive Laboratory Analysis in The Diagnosis of Anaemia in General PracticeDocument8 pages8 - The Effectiveness of A Routine Versus An Extensive Laboratory Analysis in The Diagnosis of Anaemia in General PracticenivmastPas encore d'évaluation
- Silversides2017 Article ConservativeFluidManagementOrDDocument18 pagesSilversides2017 Article ConservativeFluidManagementOrDDillaPas encore d'évaluation
- 1 - A Randomized Trial of Epinephrine in Out-Of-Hospital Cardiac Arrest - NEJMDocument19 pages1 - A Randomized Trial of Epinephrine in Out-Of-Hospital Cardiac Arrest - NEJMFernando YaksicPas encore d'évaluation
- PROCESSDocument11 pagesPROCESSandrea vargasPas encore d'évaluation
- Document Journal Review 4.09Document11 pagesDocument Journal Review 4.09Anonymous diwFs3MsWRPas encore d'évaluation
- Simvastatin For The Prevention of Exacerbations in Moderate-to-Severe COPDDocument10 pagesSimvastatin For The Prevention of Exacerbations in Moderate-to-Severe COPDdhamaraPas encore d'évaluation
- Trial of Early, Goal-Directed Resuscitation For Septic ShockDocument11 pagesTrial of Early, Goal-Directed Resuscitation For Septic Shockapi-308365861Pas encore d'évaluation
- Dialyzer Membrane Permeability and Survi PDFDocument7 pagesDialyzer Membrane Permeability and Survi PDFNurul SaufikaPas encore d'évaluation
- Propofol 1998Document23 pagesPropofol 1998peace makerPas encore d'évaluation
- 2Document8 pages2Maria RenjaanPas encore d'évaluation
- Management and Treatment Guidelines For Sepsis in Pediatric PatientsDocument9 pagesManagement and Treatment Guidelines For Sepsis in Pediatric PatientsIhsan PutraPas encore d'évaluation
- Bab IiDocument17 pagesBab IiTakaPas encore d'évaluation
- Jazul Lang MalakasDocument5 pagesJazul Lang MalakasDarl VelardePas encore d'évaluation
- PIIS0007091221004359Document7 pagesPIIS0007091221004359luisfernandoamaya89Pas encore d'évaluation
- Antiemetics: American Society of Clinical Oncology Focused Guideline UpdateDocument8 pagesAntiemetics: American Society of Clinical Oncology Focused Guideline UpdateHataitap ChonchepPas encore d'évaluation
- Zhu 2019Document9 pagesZhu 2019Blank Aguilar MPas encore d'évaluation
- Adequacy of Blood Pressure Control and Level of Adherence With Antihypertensive TherapyDocument8 pagesAdequacy of Blood Pressure Control and Level of Adherence With Antihypertensive TherapyDr YusufPas encore d'évaluation
- Early Management of Acute Pancreatitis-A Review of The Best Evidence. Dig Liver Dis 2017Document32 pagesEarly Management of Acute Pancreatitis-A Review of The Best Evidence. Dig Liver Dis 2017América FloresPas encore d'évaluation
- Nej Mo A 1012740Document9 pagesNej Mo A 1012740Mifta 'hera' Khaerati IIPas encore d'évaluation
- Acumulacion de Liquidos PulmonDocument4 pagesAcumulacion de Liquidos PulmonWando LunPas encore d'évaluation
- Jurnal 2Document9 pagesJurnal 2PulseWangminPas encore d'évaluation
- The Relationshep of Tidal Volume and Driving Presure Whit Mortality in Hypoxic Patients Receiving Mechanical VentilationDocument15 pagesThe Relationshep of Tidal Volume and Driving Presure Whit Mortality in Hypoxic Patients Receiving Mechanical VentilationDante Leonardo Garcia MenaPas encore d'évaluation
- Osborn 2017Document22 pagesOsborn 2017uci 2Pas encore d'évaluation
- Sepsis YaDocument22 pagesSepsis YaGita ListawatiPas encore d'évaluation
- Nejme 2209132Document2 pagesNejme 2209132Carlos RamírezPas encore d'évaluation
- Haspel 2014Document7 pagesHaspel 2014FOURAT OUERGHEMMIPas encore d'évaluation
- ExtubationDocument7 pagesExtubationbalab2311Pas encore d'évaluation
- Amlodipine AtenololDocument7 pagesAmlodipine AtenololBidhur Chakma 1935371673Pas encore d'évaluation
- Intermittent Vs Continuous Proton Pump Inhibitor Therapy For High-Risk Bleeding Ulcers - PMCDocument1 pageIntermittent Vs Continuous Proton Pump Inhibitor Therapy For High-Risk Bleeding Ulcers - PMCmuhammed barznjiPas encore d'évaluation
- Piis0149291815001484 PDFDocument10 pagesPiis0149291815001484 PDFWarunee MingpunPas encore d'évaluation
- 11 - 2015 - Efficacy and Safety of Long-Term Imatinib Therapy For PAH, Speich (10) 20Document10 pages11 - 2015 - Efficacy and Safety of Long-Term Imatinib Therapy For PAH, Speich (10) 20edward the iiiPas encore d'évaluation
- RECOVER Evidence and Knowledge Gap Analysis On Veterinary CPR. Part 6: Post-Cardiac Arrest CareDocument18 pagesRECOVER Evidence and Knowledge Gap Analysis On Veterinary CPR. Part 6: Post-Cardiac Arrest CareCitra Dwi LestariPas encore d'évaluation
- Running Head: Normal Saline vs. Heparin 1Document9 pagesRunning Head: Normal Saline vs. Heparin 1MaureenAmilcaPas encore d'évaluation
- Eria 2Document11 pagesEria 2ruth angelinaPas encore d'évaluation
- Klinefelter SyndromeDocument3 pagesKlinefelter SyndromeMuhammad FikriePas encore d'évaluation
- PM 3.10 SMI Eligibility Determination 02082023Document9 pagesPM 3.10 SMI Eligibility Determination 02082023hawenjamesPas encore d'évaluation
- Prevalence Statistics For Types of Anxiety DisordersDocument23 pagesPrevalence Statistics For Types of Anxiety DisordersAgung Nur SamiajiPas encore d'évaluation
- Pronóstico en TCEDocument15 pagesPronóstico en TCEobedalejandro28Pas encore d'évaluation
- Heart Disease: Prevention Is Better Than CureDocument3 pagesHeart Disease: Prevention Is Better Than CureTan Soong WeiPas encore d'évaluation
- Halgin6e PPT Ch02 (Classification&Treatment Plans)Document11 pagesHalgin6e PPT Ch02 (Classification&Treatment Plans)PooWenFooPas encore d'évaluation
- Causes: Respiratory Acidosis Respiratory AlkalosisDocument4 pagesCauses: Respiratory Acidosis Respiratory AlkalosisKristie Stiles100% (1)
- Impact of Ageing On Depression and Activities of Daily Livings in Normal Elderly Subjects Living in Old Age Homes and Communities of Kanpur, U.PDocument8 pagesImpact of Ageing On Depression and Activities of Daily Livings in Normal Elderly Subjects Living in Old Age Homes and Communities of Kanpur, U.PDr. Krishna N. SharmaPas encore d'évaluation
- Approach To An Unconscious PatientDocument16 pagesApproach To An Unconscious PatientKIBET ERNEST MUTAIPas encore d'évaluation
- (2020) - Bipolar Disorders SeminarDocument16 pages(2020) - Bipolar Disorders SeminarAarón ParedesPas encore d'évaluation
- STS ReportDocument4 pagesSTS ReportEjhay EnriquezPas encore d'évaluation
- Eating DisordersDocument4 pagesEating DisordersCarina ChicaizaPas encore d'évaluation
- MRCP PearlsDocument682 pagesMRCP Pearlssherbiny alnaghyPas encore d'évaluation
- Prevention Identification and Management of PE EclampsiaDocument15 pagesPrevention Identification and Management of PE EclampsiaRuva Oscass JimmyPas encore d'évaluation
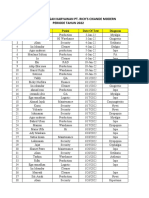
- Laporan Kunjungan Karyawn Rich's Jan-Des 2022Document19 pagesLaporan Kunjungan Karyawn Rich's Jan-Des 2022Andri AngbawiPas encore d'évaluation
- Pica - Movie Character Conceptualization Paper - July 27 2022Document10 pagesPica - Movie Character Conceptualization Paper - July 27 2022Adriana Medeiros 'student'Pas encore d'évaluation
- Evaluation of Sleep Disturbances in Children With Epilepsy A Questionnaire BasedDocument4 pagesEvaluation of Sleep Disturbances in Children With Epilepsy A Questionnaire BasednoiPas encore d'évaluation
- Endocrine FinalDocument7 pagesEndocrine FinalBell GatesPas encore d'évaluation
- Edu Adhd PaperDocument8 pagesEdu Adhd Paperapi-534406008Pas encore d'évaluation
- Essential Tremor: Clinical Features and DiagnosisDocument13 pagesEssential Tremor: Clinical Features and DiagnosisMegSepulvedaPas encore d'évaluation
- M.K.Jayarajan Paper CuttingDocument5 pagesM.K.Jayarajan Paper CuttingMas ThulanPas encore d'évaluation