Académique Documents
Professionnel Documents
Culture Documents
Osteosarcoma - A Randomized, Prospective Trial of The Addition of Ifosfamide And:or Muramyl Tripeptide To Cisplatin, Doxorubicin, and High-Dose Methotrexate
Transféré par
Rasheid MekkiTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Osteosarcoma - A Randomized, Prospective Trial of The Addition of Ifosfamide And:or Muramyl Tripeptide To Cisplatin, Doxorubicin, and High-Dose Methotrexate
Transféré par
Rasheid MekkiDroits d'auteur :
Formats disponibles
VOLUME
23
NUMBER
MARCH
20
2005
JOURNAL OF CLINICAL ONCOLOGY
O R I G I N A L
R E P O R T
Osteosarcoma: A Randomized, Prospective Trial of the
Addition of Ifosfamide and/or Muramyl Tripeptide to
Cisplatin, Doxorubicin, and High-Dose Methotrexate
Paul A. Meyers, Cindy L. Schwartz, Mark Krailo, Eugenie S. Kleinerman, Donna Betcher,
Mark L. Bernstein, Ernest Conrad, William Ferguson, Mark Gebhardt, Allen M. Goorin,
Michael B. Harris, John Healey, Andrew Huvos, Michael Link, Joseph Montebello, Helen Nadel,
Michael Nieder, Judith Sato, Gene Siegal, Michael Weiner, Robert Wells, Lester Wold, Richard Womer,
and Holcombe Grier
From the Childrens Oncology Group,
Arcadia, CA.
Submitted June 3, 2004; accepted
December 1, 2004.
A complete listing of grant support for
research conducted by the Childrens
Cancer Group and the Pediatric
Oncology Group before initiation of the
Childrens Oncology Group grant in
2003 is available online at http://www
.childrensoncologygroup.org/admin/
grantinfo.htm.
Authors disclosures of potential conflicts of interest are found at the end of
this article.
Address reprint requests to Paul A.
Meyers, MD, Department of Pediatrics,
Memorial Sloan-Kettering Cancer
Center, 1275 York Ave, New York, NY
10021; e-mail: meyersp@mskcc.org.
2005 by American Society of Clinical
Oncology
0732-183X/05/2309-2004/$20.00
DOI: 10.1200/JCO.2005.06.031
Purpose
To determine whether the addition of ifosfamide and/or muramyl tripeptide (MTP) encapsulated in liposomes to cisplatin, doxorubicin, and high-dose methotrexate (HDMTX) could
improve the probability for event-free survival (EFS) in newly diagnosed patients with
osteosarcoma (OS).
Patients and Methods
Six hundred seventy-seven patients with OS without clinically detectable metastatic disease
were treated with one of four prospectively randomized treatments. All patients received
identical cumulative doses of cisplatin, doxorubicin, and HDMTX and underwent definitive
surgical resection of the primary tumor. Patients were randomly assigned to receive or not
to receive ifosfamide and/or MTP in a 2 2 factorial design. The primary end point for
analysis was EFS.
Results
Patients treated with the standard arm of therapy had a 3-year EFS of 71%. We could not
analyze the results by factorial design because we observed an interaction between the
addition of ifosfamide and the addition of MTP. The addition of MTP to standard chemotherapy achieved a 3-year EFS rate of 68%. The addition of ifosfamide to standard chemotherapy
achieved a 3-year EFS rate of 61%. The addition of both ifosfamide and MTP resulted in a
3-year EFS rate of 78%.
Conclusion
The addition of ifosfamide in this dose schedule to standard chemotherapy did not
enhance EFS. The addition of MTP to chemotherapy might improve EFS, but additional
clinical and laboratory investigation will be necessary to explain the interaction between
ifosfamide and MTP.
J Clin Oncol 23:2004-2011. 2005 by American Society of Clinical Oncology
INTRODUCTION
Osteosarcoma (OS) is a pleomorphic malignant tumor of bone in which the proliferating spindle cells produce osteoid or
immature bone.1 It can arise in any bone
but is most common in the metaphyses
of long bones. Roughly 20% of patients
present with clinically detectable metastatic disease.
The value of adjuvant chemotherapy
for treatment of OS is well established.2,3
Agents that have shown activity against OS
include doxorubicin, cisplatin, and highdose methotrexate with leucovorin rescue
(HDMTX).4 Some investigators reported
2004
Downloaded from jco.ascopubs.org on February 11, 2015. For personal use only. No other uses without permission.
Copyright 2005 American Society of Clinical Oncology. All rights reserved.
Addition of MTP and Ifosfamide in OS
objective responses with ifosfamide in patients with OS
whose disease relapsed after treatment with these agents.5-7
Muramyl tripeptide (MTP) phosphatidylethanolamine (MTP-PE) is a synthetic lipophilic analog of muramyl dipeptide, which is a component of the cell wall of
Bacille Calmette-Guerin. MTP-PE has been encapsulated
in liposomes to deliver the agent selectively to monocytes
and macrophages to activate them to become tumoricidal and was active in rodent xenograft models and in
spontaneous canine OS.8-9 In preclinical studies, chemotherapy did not interfere with liposomal MTP-PE stimulation of macrophage cytotoxicity.10 We have shown
that simultaneous administration of ifosfamide and liposomal MTP-PE did not increase toxicity of either agent
and did not interfere with liposomal MTP-PE stimulation of cytokines.11
From November 1993 through November 1997, the
Childrens Cancer Group (CCG) and the Pediatric Oncology Group (POG) carried out Intergroup Study 0133
(CCG-7921 and POG-9351). This was a prospective, randomized phase III trial of treatment of newly diagnosed
OS in patients who were 30 years old or younger. The
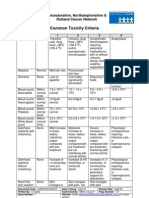
study posed two questions in a 2 2 factorial design (Fig
1). The first question was whether addition of ifosfamide
to doxorubicin, cisplatin, and HDMTX would improve
event-free survival (EFS). The second question was
whether addition of liposomal MTP to chemotherapy
would improve EFS. We report the results of this trial for
patients who presented without clinically detectable
metastatic disease.
PATIENTS AND METHODS
Patient Selection
Study patients had to have histologically confirmed, highgrade, intramedullary OS. Initial surgery was specified as biopsy
only, but patients who had primary ablative surgery, typically
amputation, were eligible. Patients who received any prior chemotherapy or radiation were ineligible. Patients with clinically detectable metastatic disease were eligible at CCG institutions but
ineligible at POG institutions. Patients had to have adequate renal
function, as defined by serum creatinine 1.5 normal or
creatinine clearance more than 40 mL/min/m2 or more than 70
mL/min/1.73 m2; adequate hepatic function, as defined by bilirubin 1.5 normal and AST or ALT 2.5 normal; and
adequate cardiac function, as defined by fractional shortening on
echocardiogram 29% or ejection fraction by radionuclide
angiography 50%. Approval from the institutional review
board (IRB) was required at every institution before enrollment. Informed consent was obtained from all patients or their
guardians, and the appropriate IRB-approved written informed consent was signed.
Treatment
Treatment began when the patients orthopedic surgeon determined that wound healing was adequate for initiation of chemotherapy. Patients were ineligible if more than 30 days elapsed
between diagnostic biopsy and enrollment. Patients were assigned
randomly to one of four regimens. There were two chemotherapy
arms, regimens A (cisplatin, doxorubicin, and HDMTX) and B
(ifosfamide, doxorubicin, HDMTX, and cisplatin), and within
those regimens, patients were assigned randomly to receive liposomal MTP or not. Even though MTP treatment did not begin
until week 12 of protocol therapy, randomization of treatment
assignment was done at entry. This resulted in four treatment
Fig 1. Protocol road map. DOXO, doxorubicin; CDDP, cisplatin; HDMTX, high-dose
methotrexate; L-MTP-PE, liposomal muramyl tripeptide phosphatidylethanolamine;
IFOS, ifosfamide.
2005
www.jco.org
Downloaded from jco.ascopubs.org on February 11, 2015. For personal use only. No other uses without permission.
Copyright 2005 American Society of Clinical Oncology. All rights reserved.
Meyers et al
arms, A or B for chemotherapy and or for whether or not
patients received liposomal MTP.
Both regimens called for an initial period of chemotherapy,
which was designated as induction, that lasted 10 weeks, followed
by definitive resection of primary tumor. Maintenance was scheduled to begin at week 12 but did not begin until the surgeon
determined that wound healing was adequate. Maintenance continued until week 31 in regimen A and week 38 in regimen B.
Regimen A consisted of four courses of cisplatin 120 mg/m2
over 4 hours combined with doxorubicin 75 mg/m2 administered
as a 72-hour continuous infusion administered twice during induction at weeks 0 and 5 and twice during maintenance at weeks
12 and 17. An additional two courses of doxorubicin without
cisplatin were administered at weeks 22 and 27. HDMTX 12 g/m2
with a maximum dose of 20 g was administered as a 4-hour
infusion followed by leucovorin administration at 10 mg (not
adjusted to body-surface area) beginning 24 hours from initiation
of methotrexate infusion and continuing until the serum methotrexate level was less than 1 107 mol/L (100 nmol/L). Serum
methotrexate levels and renal function were monitored daily, and
hydration, alkalinization, and leucovorin doses were specified in
the event of delayed methotrexate excretion. HDMTX was administered 12 times, four times during induction at weeks 3, 4, 8, and
9 and eight times during maintenance at weeks 15, 16, 20, 21, 25,
26, 30, and 31. To maintain dose-intensity of doxorubicin, the
protocol specified that, if there was a delay greater than 1 week
between the first and second of each pair of HDMTX administrations, the second was omitted.
Regimen B included ifosfamide 1.8 g/m2/d with mesna uroprotection for 5 days; a total dose of 9 g/m2 was administered five
times, twice during induction at weeks 0 and 5 and three times
during maintenance at weeks 17, 27, and 35. The first four courses
of ifosfamide were to be administered with doxorubicin. Cisplatin
120 mg/m2 was administered four times, all during maintenance,
at weeks 12, 22, 32, and 38. The first two courses of cisplatin were
scheduled to be administered with doxorubicin. Doxorubicin and
methotrexate were administered at the same doses and in the same
weeks as regimen A.
Total doses of cisplatin, doxorubicin, and HDMTX were the
same in the two arms (cisplatin 480 mg/m2, doxorubicin 450
mg/m2, and HDMTX 144 g/m2). Timing of doxorubicin and
HDMTX was the same in both arms. Patients assigned to regimen
B received ifosfamide during induction to maximize its effect on
tumor response. Thus, from the perspective of evaluating tumor
necrosis, regimen B could be considered a substitution of ifosfamide for cisplatin. The overall strategy was that regimen B
differed from regimen A by the addition of ifosfamide to the
combination of cisplatin, doxorubicin, and HDMTX.
Half the patients were assigned randomly at entry to receive
liposomal MTP beginning at week 12. It was administered at a
dose of 2 mg/m2. Patients initially were not permitted to have
premedications and were monitored for signs of biologic activity,
which was defined as fever, chills, or increase in the C-reactive
protein. If a patient had no sign of biologic activity, the next dose
of MTP was 2 mg/m2, with an additional 1 mg. If a patient had no
sign of biologic activity after the first dose escalation, a second dose
escalation of 2 mg/m2, with an additional 2 mg, was used for the
third dose of MTP. No further escalation was allowed. Each subsequent dose of MTP was either the dose that provoked signs of
biologic activity or the maximum dose. Premedication limited to
acetaminophen and diphenhydramine was permitted with the
2006
fourth and subsequent doses to prevent fevers or chills. Corticosteroids were not permitted during MTP administration because
the presumptive mechanism of MTP activity was recruitment of
effector cells, which could be inhibited by corticosteroids. MTP
was administered twice weekly for 12 weeks beginning at week 12
and then weekly for an additional 24 weeks beginning at week 24.
MTP was not interrupted for delays in chemotherapy.
MTP was administered through a 3-m filter to decrease risk
of infusion of large aggregates of liposomes into patients. Filters
were supplied by the sponsor and distributed by the National
Cancer Institute. In June 1995, the filter manufacturer was unable
to provide filters. The study committee instructed investigators to
continue to administer MTP to patients who had already begun
this agent. Patients who were due to begin receiving this agent had
initiation delayed until filters were available in January 1996. Patients who entered during that period and were assigned to receive
MTP-PE were at risk of not receiving the assigned treatment. We
designated all patients during this period as a noncompliance
cohort and increased planned accrual to compensate for them.
Accrual continued until the number of patients accrued reached
the number designed in the a priori power calculations, even
allowing for exclusion of the noncompliance cohort.
Definitive surgery was performed at week 10. Procedure
choice was left to the institutional orthopedic surgeon. Limb preservation was encouraged strongly whenever possible. After primary tumor removal, global assessment of necrosis was made by
the institutional pathologist. Necrosis was classified using the
scoring system designed by Huvos, as modified by CCG to subdivide grade 2.3,12
Statistical Methods
The study was conducted as a factorial design. At enrollment,
a patient was assigned one of the following treatment plans:
(1) chemotherapy A without MTP-PE; (2) chemotherapy A with
MTP-PE; (3) chemotherapy B without MTP-PE; and (4) chemotherapy B with MTP-PE. Assignment randomization was blocked
in groups of eight within each of 12 possible strata, which were
defined by presence versus absence of metastatic disease, lactate
dehydrogenase above versus below the institutional upper limit of
normal, and initial tumor resection versus biopsy; patients without evidence of metastases also were stratified by tumor location
(proximal v distal to knee or elbow).
The primary goals of the study were to be addressed in
patients without detectable metastases at diagnosis. We planned to
assess relative risks associated with two different chemotherapies
and biologic intervention with a factorial approach. Patients assigned to regimen A would be compared with patients assigned to
regimen B after stratification for MTP-PE assignment to assess
effects of the regimens. A similar approach was to be used for
assessing the effects of MTP-PE.
Using the factorial analysis approach, we determined that we
needed a sample of 585 patients enrolled over 4 years and observed
for another 2 years to detect reduction in risk for therapy-related
events of 0.64 with 80% power, using a two-sided test of 0.05. The
analytic procedure included a test of assumption of equal relative
risks for one intervention compared across strata defined for
the second intervention. Assumption of absence of interaction
between regimens was crucial to the validity of the factorial
analysis approach.
EFS was the primary outcome measure used to compare
efficacy of regimens. It was defined as the time from entry until an
adverse event or last patient contact, whichever came first. EFS
JOURNAL OF CLINICAL ONCOLOGY
Downloaded from jco.ascopubs.org on February 11, 2015. For personal use only. No other uses without permission.
Copyright 2005 American Society of Clinical Oncology. All rights reserved.
Addition of MTP and Ifosfamide in OS
after definitive surgery was defined as the time from start of first
course of maintenance therapy until an adverse event or last patient contact, whichever came first. Adverse events included disease progression, diagnosis of second malignant neoplasm, or
death before disease progression or second malignant neoplasm.
Patients without adverse events were censored at date of last contact. Data current to April 2003 were used for this analysis.
One hundred eighteen patients comprised the noncompliance cohort. Of these patients, 101 did not have metastases at
diagnosis. Outcomes and relative risks of comparisons examined
in this report were virtually the same in the compliance and
noncompliance cohorts, so data from all eligible patients were
used in the analysis.
EFS was estimated with the Kaplan-Meier method.13 Risk of
adverse events was compared across groups defined by treatment
or prognostic factors using the log-rank statistic.13 Patient assignments were used in all comparisons that involved regimens. Prognostic significance and associated relative risk of various
patient characteristics measured at entry were assessed with a
proportional hazards regression model with the characteristic
of interest as the only component.13 CIs for relative risks were
derived from the proportional hazards regression model. Interim monitoring was conducted three times during the period
of accrual. The method of Lan and DeMets13 was used with the
spending function t2.
RESULTS
Patient Characteristics
Among 793 patients enrolled onto Intergroup Study
0133, 16 were considered ineligible. Ten patients were not
treated within 30 days of diagnostic biopsy, as required by
the protocol. Three patients were determined subsequently
to not have OS; one patient had low-grade OS and two had
chondrosarcoma. One patient did not have normal cardiac
function at enrollment. Two patients were declared ineligible because the IRBs at their institutions had not completed
protocol review before entry.
Of the remaining 777 patients, 100 had clinically
detectable metastases. The 677 patients without metastases are the subjects of this report. Among them, 373
(55%) were male, and 304 (45%) were female (Table 1).
Patient ages ranged from 1 to 30 years, with a median age
at entry of 13 years.
Surgery
Twelve patients had amputations before entry, and 19
of the remaining 665 patients had axial tumors. Among the
other 646 patients, 14 had adverse events before definitive
surgery, and data were not available to classify operations of
91 patients. Four hundred fifteen patients had limb-sparing
surgery, and 126 had amputations.
Toxicity of Therapy
Toxicity was reported for all patients on study, including the noncompliance cohort. There were five treatmentrelated deaths; four deaths were from infections during
Table 1. Patient Characteristics
Sex
Male
Female
Age at enrollment (years)
0-11 years
12-14 years
15-30 years
Race
White
Hispanic
Black
Asian
Other
Primary tumor site
Femur
Below knee
Humerus
Below elbow
Leg NOS
Arm NOS
Pelvis
Other axial
Not reported
Alkaline phosphatase
ULN
ULN
Not reported
Lactate dehydrogenase
ULN
ULN
No. of
Patients
373
304
55
45
224
204
249
33
30
37
453
84
93
14
33
67
12
14
2
5
374
185
73
12
2
1
12
10
8
55
27
11
2
1
1
2
2
392
268
17
58
40
438
239
65
35
Abbreviations: NOS, not otherwise specified; ULN, upper limit of normal.
The ULN for this analysis was the ULN in the institution where the patient
was treated.
periods of pancytopenia, and one was an intraoperative
death. One patient died in an accident, and the cause of
death could not be determined for another patient,
although there was no evidence that it was disease related. There was no excess of treatment-related mortality in
any arm. Principal toxicities were elevations in ALT after
HDMTX, stomatitis, and infections. Renal dysfunction was
rare. Objective hearing loss, as defined by the protocol, was
reported in 11% of patients. There was no difference among
the treatment arms for most of the toxicities reported.
Administration of MTP was associated with fever and
chills. The protocol called for dose escalation of MTP until
these effects were observed to assure biologic activity. Most
patients did not need dose escalation. Reactions to MTP
decreased with time for most patients, but fever and chills
continued for some patients with each administration of
MTP, despite premedication. Administration was scheduled to continue beyond completion of chemotherapy in
both arms that called for MTP. Patients were more likely to
2007
www.jco.org
Downloaded from jco.ascopubs.org on February 11, 2015. For personal use only. No other uses without permission.
Copyright 2005 American Society of Clinical Oncology. All rights reserved.
Meyers et al
withdraw from therapy before completion of all protocolspecified therapy on these arms.
Outcome
As of April 2003, 230 of 677 patients had adverse
events. Seven patients (1%) died without evidence of disease progression, 11 patients (1.6%) developed second malignant neoplasms, and 212 patients (31%) experienced
disease recurrence. Of the seven patients who experienced
death as a first event, three were treated on regimen A
without MTP, two were treated on regimen B with MTP,
and two were treated on regimen B without MTP. Four
patients died of infectious complications, one patient died
of an operative complication after definitive surgery, one
patient died from an overdose of a self-administered illegal
Table 2. Relative Risk of Adverse Event for Patients Without
Detectable Metastases at Diagnosis
Characteristic
Sex
Male
Female
Age at diagnosis
11 years
12-14 years
15 years
Race
White
Hispanic
Black
Other
Tumor
Distal extremity
Proximal extremity
Axial skeleton
Not determined
Maximum tumor size
8 cm
9 cm
Not determined
Maximum tumor size
6 cm
7-8 cm
9-11 cm
11 cm
Not determined
Lactate dehydrogenase
Below ULN
At or above ULN
Alkaline phospatase
Below ULN
At or above ULN
Not reported
Prior amputation
Yes
No
No. of
Patients
Relative
Risk
95% CI
373
304
1.0
1.1
0.81 to 1.4
.68
224
204
249
1.0
0.84
1.0
0.60 to 1.2
0.75 to 1.4
.44
453
84
93
47
1.0
1.3
0.87
0.94
0.87 to 1.8
0.58 to 1.3
0.54 to 1.6
.53
197
447
22
11
1.0
1.5
2.4
1.1 to 2.0
1.2 to 4.5
.0095
260
338
79
1.0
1.5
1.1 to 2.0
.0044
128
132
158
180
79
1.0
1.0
1.4
1.6
0.63 to 1.6
0.90 to 2.1
1.1 to 2.4
.0041
438
239
1.0
1.7
1.3 to 2.2
.00016
Prognostic Factors
Age, sex, and race did not correlate with EFS (Table 2).
Patients with alkaline phosphatase levels above their institutions upper limit of normal had worse prognoses. Patients with lactate dehydrogenase levels above institutional
upper limit of normal also had worse prognoses. Patients
with primary tumors of the distal appendicular skeleton
had the best prognosis, followed by those with tumors of the
proximal appendicular skeleton. Patients with axial primary tumors had the worst prognosis. There was no difference in outcome between patients who had primary
ablation of their tumor and patients who had definitive
surgery after induction.
Necrosis After Induction Chemotherapy
Patients who underwent definitive resection after induction underwent evaluation of necrosis by an institutional
pathologist. Necrosis was graded according to the method of
Huvos, as modified by CCG.3,12 Because MTP was not introduced until after surgery, patients were classified only by regimen assignment (A or B; Table 3). Besides the 12 patients who
had amputations before chemotherapy, 22 had adverse events
before definitive resection after induction. Necrosis grading
was not available for an additional 59 patients. Overall, 265
(45%) of 584 patients exhibited grade 3 or 4 necrosis. There
was no difference in frequency of favorable necrosis between
chemotherapy arms.
Necrosis after induction correlated with prognosis
monotonically (Fig 2). Necrosis is not a true prognostic
factor because it cannot be evaluated before therapy and,
therefore, cannot be used for patient stratification at entry.
EFS
For patients without metastases, EFS was 70% at 3 years
and 63% at 5 years from entry (Fig 3). One hundred one
Table 3. Necrosis in the Primary Tumor After Induction Chemotherapy
392
268
17
1.0
1.8
1.4 to 2.4
.00001
12
665
1.0
1.2
0.46 to 3.4
.66
Abbreviation: ULN, upper limit of normal.
Log-rank trend test.
2008
drug, and the cause of one death could not be determined.
Of the 11 patients who developed second malignant neoplasms, three each were treated on regimen A without MTP,
regimen A with MTP, and regimen B with MTP, and two
were treated on regimen B without MTP. Neither death as a
first event nor secondary malignancy was associated with a
specific treatment arm. The median follow-up for patients
with no adverse events at analysis was 4.8 years.
Necrosis Grade
1
2A
2B
Chemotherapy
Regimen
No.
No.
No.
No.
No.
A
B
11
7
4
2
44
33
15
11
112
112
38
38
84
95
29
33
41
45
14
15
NOTE. P .51 for the equality of proportions across chemotherapy groups.
Huvos grading as modified by the Childrens Cancer Group.12,13
JOURNAL OF CLINICAL ONCOLOGY
Downloaded from jco.ascopubs.org on February 11, 2015. For personal use only. No other uses without permission.
Copyright 2005 American Society of Clinical Oncology. All rights reserved.
Addition of MTP and Ifosfamide in OS
Fig 2. Necrosis observed in the primary tumor at the time of definitive surgical
resection after induction chemotherapy correlates with event-free survival.
patients entered onto the study while filter availability compromised MTP administration. Our analysis that excluded the
noncompliance cohort did not alter study conclusions.
We used a 2 2 factorial design. To analyze the study
in accordance with the initial factorial design, there had to
be no interaction between the two study questions. We
observed an interaction between the study interventions
(Fig 4). The usual factorial analytic strategy estimates a
treatment effect by an analysis stratifying the population by
the other treatment factor. The presence of an interaction
invalidates this procedure because there is no single treatment effect of interest; the effect differs across groups
formed by stratifying according to the other intervention.
We considered regimen A (cisplatin, doxorubicin, and
Fig 4. Event-free survival for patients according to treatment arm. Regimen
A consisting of cisplatin, doxorubicin, and high-dose methotrexate was the
standard arm of this study. Regimen B included the same agents with the
addition of ifosfamide. Regimens A and B also included the investigational agent muramyl tripeptide (MTP). Overall trend for difference was
significant (P .04).
HDMTX without MTP) the standard arm of this trial. The
easiest way to recognize the interaction was to observe the
effect of MTP addition to the patients assigned to receive
ifosfamide compared with the standard arm. Patients
treated with regimen A had a 64% probability of EFS at
5 years. Patients who received cisplatin, doxorubicin,
HDMTX, and ifosfamide (regimen B) had a 53% probability of EFS at 5 years. Patients who received cisplatin,
doxorubicin, HDMTX, ifosfamide, and MTP (regimen
B) had a 72% probability of EFS at 5 years. Addition of
ifosfamide to standard treatment seemed to decrease
EFS, whereas the addition of ifosfamide and MTP
seemed to increase EFS (Table 4).
Because the study could not be analyzed according to
its original factorial design, we provided estimates of EFS
according to treatment assignments. The results of the four
arms are shown in Figure 4. Regimen A was associated
with a 71% and 64% probability of EFS at 3 and 5 years,
Table 4. Relative Risk of Adverse Event for Patients Without Detectable
Metastases at Diagnosis According to Randomized Regimen
Fig 3. Event-free survival (EFS) and overall survival for patients newly
diagnosed with osteosarcoma without clinically detectable metastatic disease.
Randomized
Regimen
No. of
Patients
Relative
Risk
95% CI
A
A
A
B
A
B
172
168
172
167
172
170
1.0
1.0
1.0
1.3
1.0
0.78
0.71 to 1.5
0.93 to 1.9
0.54 to 1.2
.88
.12
.22
2009
www.jco.org
Downloaded from jco.ascopubs.org on February 11, 2015. For personal use only. No other uses without permission.
Copyright 2005 American Society of Clinical Oncology. All rights reserved.
Meyers et al
respectively. The addition of MTP (regimen A) resulted
in a 68% and 63% probability of EFS at 3 and 5 years,
respectively. The addition of ifosfamide (regimen B) resulted in a 61% and 56% probability of EFS at 3 and 5 years,
respectively. The addition of ifosfamide and MTP resulted
in a 78% and 72% probability of EFS at 3 and 5 years,
respectively (Fig 4).
DISCUSSION
We sought to obtain prospective information about several
factors at diagnosis that were reported to correlate with EFS.
We confirmed that serum alkaline phosphatase and lactate
dehydrogenase elevations above institutional normal values
correlated with lower probability for EFS. We confirmed
that proximal tumors and tumors of the axial skeleton, especially pelvic primary tumors, have lower probability for EFS.
Tumor size correlated with outcome. Unlike some reports that
used retrospective analysis, we did not identify age, sex, or
ethnicity as predictive of outcome. Eligibility was limited to
patients 30 years of age or younger, so we cannot comment on
the effect on prognosis of age beyond 30 years.
EFS for all 677 patients was 70% and 63% at 3 and 5 years
from diagnosis, respectively. Most outcome reports of OS have
focused on EFS of patients 21years old or younger with tumors
limited to the appendicular skeleton. In the current series, we
treated 622 patients who met these criteria, and their 3- and
5-year EFS rates were 70% and 63%, respectively.
We used a factorial design, and a priori power calculations were based on the assumption that we would collapse
study arms to aggregate all patients for each question. Factorial analysis relies on no interaction between the interventions tested. Before this study, we performed a small pilot
study of simultaneous chemotherapy and MTP.11 We did
not observe any interaction. We chose to introduce MTP
after definitive surgery. We did not wish to introduce it
before surgery because we believed that the biologic agent
would have its best opportunity to influence survival after
tumor bulk was minimized. We considered delaying MTP
introduction until after completion of chemotherapy to
avoid the risk of interaction completely. We rejected this
option because clinical progression of OS is observed weeks
to months after tumor cells develop resistance to chemotherapy and begin to proliferate. The timing of relapse after
treatment for OS suggested that most patients whose treatments fail develop resistant tumor clones while still receiving chemotherapy. If we had delayed the introduction of
MTP until after chemotherapy, we might have lost the
opportunity to see an effect on tumor control.
Unfortunately, we did observe an interaction between
addition of ifosfamide and addition of MTP. Factorial analysis does not require that the magnitude of the effect of an
intervention be the same, but the direction of that effect
2010
must be the same. The easiest way to observe the interaction
between the two interventions is to compare treatment
regimen B and regimen B to the standard arm (regimen
A) of the protocol. When ifosfamide was added to cisplatin, doxorubicin, and HDMTX (regimen B), EFS decreased. When ifosfamide was added to the same three
agents with MTP (regimen B), EFS increased.
The interaction made it impossible to perform the
factorial analysis as planned, so we had to examine study
outcome as a four-arm trial. The study was not designed to
analyze four arms with adequate power. We consider regimen A to be the standard arm of this trial. None of the
other three arms of this study was significantly different
from regimen A (Table 4).
Rates of favorable necrosis for the two induction arms
were identical. We concluded that ifosfamide and cisplatin are
equivalent in their ability to contribute to favorable necrosis.
The addition of ifosfamide to cisplatin, doxorubicin,
and HDMTX did not enhance EFS. The four-drug B
regimen actually seemed to have the worst outcome. Addition of MTP to the standard chemotherapy treatment (regimen A) had no impact on EFS. Addition of MTP to the
four-drug chemotherapy regimen (regimen B) resulted in
the most favorable EFS of the four arms.
How can we understand these confusing results? One
possible explanation is that the apparent differences among the
arms were the result of chance. Because of failure of the factorial design, our study did not have the power to exclude that
possibility with complete confidence. The 2 analysis for homogeneity suggested that the probability of the outcome we
observed is only 4%, but a major contribution to the inhomogeneity is the unexpectedly inferior outcome of regimen B.
A possible biologic explanation for the observed outcome
involves the interaction between fas and fas ligand. Lafleur et
al14 showed that 4-hydroperoxy-cyclophosphamide, an active
metabolite of oxazaphosphorine chemotherapy, enhances fas
ligand expression in an OS cell line. This upregulation was not
observed with doxorubicin, cisplatin, or methotrexate. They
found that MTP stimulates multiple cytokines, including interleukin (IL) -12, and that IL-12 upregulates expression of fas
in an OS cell line selected for high probability to metastasize.15
Administration of ifosfamide and MTP could activate the fas/
fas-ligand pathway that initiates apoptosis. This hypothesis
suggests that we should investigate other agents with the potential to affect IL-12 and the fas/fas-ligand pathway.
We were unable to detect an improvement in the treatment of OS from the addition of ifosfamide in this dose
schedule to cisplatin, doxorubicin, and HDMTX. The EFS
we documented using that three-drug combination was
similar to that reported by other groups using multiagent
regimens and superior to the simpler combination of cisplatin and doxorubicin alone.15 We observed a potential
interaction between the alkylating agent ifosfamide and
JOURNAL OF CLINICAL ONCOLOGY
Downloaded from jco.ascopubs.org on February 11, 2015. For personal use only. No other uses without permission.
Copyright 2005 American Society of Clinical Oncology. All rights reserved.
Addition of MTP and Ifosfamide in OS
MTP. This interaction will need further laboratory and
clinical investigation to evaluate potential mechanisms and
confirm any clinical value.
Authors Disclosures of Potential
Conflicts of Interest
The following authors or their immediate family members have indicated a financial interest. No conflict exists for
REFERENCES
1. Meyers PA: Malignant bone tumors in
childhood: Osteosarcoma. Hematol Oncol Clin
North Am 1:655-665, 1987
2. Link MP, Goorin AM, Miser AW, et al: The
effect of adjuvant chemotherapy on relapse-free
survival in patients with osteosarcoma of the
extremity. N Engl J Med 314:1600-1606, 1986
3. Meyers PA, Heller G, Healey J, et al:
Chemotherapy for nonmetastatic osteogenic
sarcoma: The Memorial Sloan-Kettering experience. J Clin Oncol 10:5-15, 1992
4. Link MP, Meyers PA, Gebhardt M: Osteosarcoma, in Pizzo PA, Poplack DG (eds): Principles and Practice of Pediatric Oncology (ed 4).
Philadelphia: Lippincott Williams & Wilkins,
2001, pp 1051-1089
5. Harris MB, Cantor AB, Goorin AM, et al:
Treatment of osteosarcoma with ifosfamide:
Comparison of response in pediatric patients
with recurrent disease versus patients previously untreatedA Pediatric Oncology Group
study. Med Pediatr Oncol 24:87-92, 1995
drugs or devices used in a study if they are not being evaluated as part of the investigation. Consultant: Michael Link,
Onyx Pharmaceutical, Yamaguchi Pharmaceutical. Research Funding: Michael Link, Bristol-Meyers Squibb. For a
detailed description of these categories, or for more information about ASCOs conflict of interest policy, please refer
to the Author Disclosure Declaration and the Disclosures of
Potential Conflicts of Interest section of Information for
Contributors found in the front of every issue.
6. Miser JS, Kinsella TJ, Triche TJ, et al: Ifosfamide with mesna uroprotection and etoposide:
An effective regimen in the treatment of recurrent
sarcomas and other tumors of children and young
adults. J Clin Oncol 5:1191-1198, 1987
7. Kung FH, Pratt CB, Vega RA, et al: Ifosfamide/etoposide combination in the treatment
of recurrent malignant solid tumors of childhood:
A Pediatric Oncology Group phase II study. Cancer 71:1898-1903, 1993
8. Fidler IJ, Sone S, Fogler WE, et al: Eradication of spontaneous metastases and activation
of alveolar macrophages by intravenous injection
of liposomes containing muramyl dipeptide. Proc
Natl Acad Sci U S A 78:1680-1684, 1981
9. MacEwen EG, Kurzman ID, Rosenthal RC,
et al: Therapy of osteosarcoma in dogs with
intravenous injection of liposome encapsulated
muramyl tripeptide. J Natl Cancer Inst 81:935936, 1989
10. Kleinerman ES, Snyder JS, Jaffe N: Influence of chemotherapy administration on monocyte activation by liposomal muramyl tripeptide
phosphatidylethanolamine in children with osteosarcoma. J Clin Oncol 9:259-267, 1991
11. Kleinerman ES, Meyers PA, Raymond AK,
et al: Combination therapy with ifosfamide and
liposome-encapsulated muramyl tripeptide: Tolerability, toxicity, and immune stimulation. J Immunother Emphasis Tumor Immunol 17:181-193,
1995
12. Provisor AJ, Ettinger LJ, Nachman JB, et
al: Treatment of nonmetastatic osteosarcoma of
the extremity with preoperative and postoperative chemotherapy: A report from the Childrens
Cancer Group. J Clin Oncol 15:76-84, 1997
13. Kalbfleisch J, Prentice R: The Statistical
Analysis of Failure Time Data. New York, NY:
John Wiley and Sons, 1980
14. Lafleur EA, Jia S-F, Worth LL, et al: Interleukin (IL)-12 and IL-12 gene transfer up-regulate
fas expression in human osteosarcoma and
breast cancer cells. Cancer Res 61:4066-4071,
2001
15. Souhami RL, Craft AW, Van der Eijken JW,
et al: Randomised trial of two regimens of chemotherapy in operable osteosarcoma: A study of
the European Osteosarcoma Intergroup. Lancet
350:911-917, 1997
2011
www.jco.org
Downloaded from jco.ascopubs.org on February 11, 2015. For personal use only. No other uses without permission.
Copyright 2005 American Society of Clinical Oncology. All rights reserved.
Vous aimerez peut-être aussi
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Adult Medical Emergencies HandbookDocument317 pagesAdult Medical Emergencies HandbookRasheid Mekki100% (16)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Gut Health Guidebook 9 22Document313 pagesGut Health Guidebook 9 2219760227Pas encore d'évaluation
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- 10a General Pest Control Study GuideDocument128 pages10a General Pest Control Study GuideRomeo Baoson100% (1)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- VBA 21 526ez AREDocument12 pagesVBA 21 526ez AREBiniam GirmaPas encore d'évaluation
- Canadian Pharmacy Review Ver1Document6 pagesCanadian Pharmacy Review Ver1Dr-Usman Khan30% (10)
- LP MAPEH 9 (Health)Document4 pagesLP MAPEH 9 (Health)Delima Ninian100% (2)
- Preterm Prelabour Rupture of MembranesDocument12 pagesPreterm Prelabour Rupture of MembranesSeptiany Indahsari DjanPas encore d'évaluation
- Oet Test Material: Occupational English Test Reading Sub-Test NursingDocument13 pagesOet Test Material: Occupational English Test Reading Sub-Test NursingRyu Tse33% (3)
- Management of Stage III Non-Small Cell Lung Cancer - UpToDateDocument23 pagesManagement of Stage III Non-Small Cell Lung Cancer - UpToDateRasheid MekkiPas encore d'évaluation
- Five Elements Chart TableDocument7 pagesFive Elements Chart TablePawanPas encore d'évaluation
- Tamiflu and ADHDDocument10 pagesTamiflu and ADHDlaboewe100% (2)
- Roadmap For TelemedicineDocument48 pagesRoadmap For TelemedicinePradip Gupta100% (2)
- Cancer in Sub-Saharan Africa 2015Document49 pagesCancer in Sub-Saharan Africa 2015Rasheid MekkiPas encore d'évaluation
- 2015 Asco EdbookDocument924 pages2015 Asco EdbookRasheid MekkiPas encore d'évaluation
- Understanding Money Handbook PDFDocument46 pagesUnderstanding Money Handbook PDFRasheid MekkiPas encore d'évaluation
- Milestones in Cancer NATURE 0Document17 pagesMilestones in Cancer NATURE 0bioletimPas encore d'évaluation
- NICE Guidelines-Prostate CA 01:14Document48 pagesNICE Guidelines-Prostate CA 01:14Rasheid MekkiPas encore d'évaluation
- Milestones in Cancer NATURE 0Document17 pagesMilestones in Cancer NATURE 0bioletimPas encore d'évaluation
- Systemic Treatment of Metastatic Breast Cancer in Women: ChemotherapyDocument18 pagesSystemic Treatment of Metastatic Breast Cancer in Women: ChemotherapyRasheid MekkiPas encore d'évaluation
- Common Toxicity CriteriaDocument3 pagesCommon Toxicity CriteriaRasheid MekkiPas encore d'évaluation
- Metabolites 02 00303Document34 pagesMetabolites 02 00303Rasheid MekkiPas encore d'évaluation
- Program Implementation With The Health Team: Packages of Essential Services For Primary HealthcareDocument1 pageProgram Implementation With The Health Team: Packages of Essential Services For Primary Healthcare2A - Nicole Marrie HonradoPas encore d'évaluation
- Information On The Use of Domperidone To Increase Milk Production in Lactating WomenDocument3 pagesInformation On The Use of Domperidone To Increase Milk Production in Lactating WomenKhairul HananPas encore d'évaluation
- Fat Soluble VitaminsDocument20 pagesFat Soluble VitaminsWati WindayaniPas encore d'évaluation
- Delayed Homicides and The Proximate Cause.8Document5 pagesDelayed Homicides and The Proximate Cause.8rheanditahafsaPas encore d'évaluation
- Msds ChloroformDocument9 pagesMsds ChloroformAhmad ArisandiPas encore d'évaluation
- Class IX - Worksheet 4 (Comprehension & Writing Skill)Document6 pagesClass IX - Worksheet 4 (Comprehension & Writing Skill)Anis FathimaPas encore d'évaluation
- Classifying Giant Cell Lesions A Review.21Document5 pagesClassifying Giant Cell Lesions A Review.21shehla khanPas encore d'évaluation
- Operator MGC Ultima PFX - English - 142152-001rCDocument65 pagesOperator MGC Ultima PFX - English - 142152-001rCEvangelosPas encore d'évaluation
- BM Procedure and ProcessingDocument28 pagesBM Procedure and ProcessingNidhi JaisPas encore d'évaluation
- DSM OcdDocument2 pagesDSM Ocdnmyza89Pas encore d'évaluation
- Escala de Apatia de StarksteinDocument6 pagesEscala de Apatia de StarksteinVanessa HernandezPas encore d'évaluation
- Sri Lanka - Averting A National Nutrition Anomaly 2Document16 pagesSri Lanka - Averting A National Nutrition Anomaly 2Rushan LakdimuthuPas encore d'évaluation
- 2018 Surgical Rescue in Medical PatientsDocument11 pages2018 Surgical Rescue in Medical PatientsgiseladlrPas encore d'évaluation
- Paper Roleplay Group 3Document7 pagesPaper Roleplay Group 3Endah Ragil SaputriPas encore d'évaluation
- Test Bank For Pilbeams Mechanical Ventilation 5th Edition CairoDocument13 pagesTest Bank For Pilbeams Mechanical Ventilation 5th Edition Cairochowryurduq0krhPas encore d'évaluation
- Clinchers: RheumatologyDocument22 pagesClinchers: RheumatologyvarrakeshPas encore d'évaluation
- ESC - 2021 - The Growing Role of Genetics in The Understanding of Cardiovascular Diseases - Towards Personalized MedicineDocument5 pagesESC - 2021 - The Growing Role of Genetics in The Understanding of Cardiovascular Diseases - Towards Personalized MedicineDini SuhardiniPas encore d'évaluation
- Long-Term Survey of Tooth Loss in 600 PtsDocument15 pagesLong-Term Survey of Tooth Loss in 600 PtsAndy HePas encore d'évaluation
- GENERAL RISK ASSESSMENT Mechatronics LaboratoryDocument2 pagesGENERAL RISK ASSESSMENT Mechatronics LaboratoryJason TravisPas encore d'évaluation
- 24 Bio Fertilization of BananaDocument6 pages24 Bio Fertilization of Bananamiceli57Pas encore d'évaluation