Académique Documents
Professionnel Documents
Culture Documents
Clinical Study: Development of Dengue Infection Severity Score
Transféré par
Valencius SunandarTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Clinical Study: Development of Dengue Infection Severity Score
Transféré par
Valencius SunandarDroits d'auteur :
Formats disponibles
Hindawi Publishing Corporation
ISRN Pediatrics
Volume 2013, Article ID 845876, 6 pages
http://dx.doi.org/10.1155/2013/845876
Clinical Study
Development of Dengue Infection Severity Score
Surangrat Pongpan,1,2 Apichart Wisitwong,3 Chamaiporn Tawichasri,4
Jayanton Patumanond,5 and Sirianong Namwongprom6
1
Program in Clinical Epidemiology, Faculty of Medicine, Chiang Mai University, Chiang Mai 50200, Thailand
Department of Occupational Medicine, Phrae Hospital, Phrae 54000, Thailand
3
Department of Social Medicine, Sawanpracharak Hospital, Nakorn Sawan 60000, Thailand
4
Clinical Epidemiology Society at Chiang Mai, Chiang Mai 50200, Thailand
5
Clinical Epidemiology Unit, Faculty of Medicine, Chiang Mai University, Chiang Mai 50200, Thailand
6
Department of Radiology, Faculty of Medicine, Chiang Mai University, Chiang Mai 50200, Thailand
2
Correspondence should be addressed to Sirianong Namwongprom; sirianong@hotmail.com
Received 13 July 2013; Accepted 12 September 2013
Academic Editors: G. J. Casimir, K. Tokiwa, and B. Vasarhelyi
Copyright 2013 Surangrat Pongpan et al. This is an open access article distributed under the Creative Commons Attribution
License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly
cited.
Objectives. To develop a simple scoring system to predict dengue infection severity based on patient characteristics and routine
clinical profiles. Methods. Retrospective data of children with dengue infection from 3 general hospitals in Thailand were reviewed.
Dengue infection was categorized into 3 severity levels: dengue infection (DF), dengue hemorrhagic fever (DHF), and dengue
shock syndrome (DSS). Coefficients of significant predictors of disease severity under ordinal regression analysis were transformed
into item scores. Total scores were used to classify patients into 3 severity levels. Results. Significant clinical predictors of dengue
infection severity were age >6 years, hepatomegaly, hematocrit 40%, systolic pressure <90 mmHg, white cell count >5000 /L,
and platelet 50000 /L. The derived total scores, which ranged from 0 to 18, classified patients into 3 severity levels: DF (scores
<2.5, = 451, 58.1%), DHF (scores 2.511.5, = 276, 35.5%), and DSS (scores >11.5, = 50, 6.4%). The derived score correctly
classified patients into their original severity levels in 60.7%. An under-estimation of 25.7% and an over-estimation of 13.5% were
clinically acceptable. Conclusions. The derived dengue infection severity score classified patients into DF, DHF, or DSS, correctly
into their original severity levels. Validation of the score should be reconfirmed before application of routine practice.
1. Introduction
Dengue infection has become an international public health
burden. Half of the world population are presently at risk
of dengue infection. Approximately 50100 million infected
cases were reported annually. Among those infected, 500000
patients had severe infection and required hospital admission; most were children. Approximately 2.5% died from the
infection [1]. The cost of care was as high as $US 2.1 billion
per year in The United States of America [2]. No specific
treatments are available except for symptomatic [3], which
are effective in early detection [4]. In patients with severe
infection, shock and hemorrhage usually follow [4, 5]. If
not treated, death may be a consequence. Early detection or
correct prognostication may avoid such severe complications
[4, 6].
Clinical risks and various laboratory results were studied
to explore their roles in the prediction of dengue severity.
Among many of them were girls [7], children above 5 years of
age [8], persistent abdominal pain [9], lethargy, cold hand and
feet [10], hepatomegaly [11], abnormal bleeding [12], overweight [13], malnourished children [14], ascites [8], plural
effusion [15], leucopenia (white blood count < 4,000/L) [8],
thrombocytopenia [16], hemoconcentration [16], prolonged
prothrombin time (PT) [16], prolonged partial thromboplastin time (PTT) [17], elevated aspartate aminotransferase
(AST), and alanine aminotransferase (ALT) enzymes [18].
The scoring system, such as the Pediatric Logistic Organ
Dysfunction (PELOD) Score and the Disseminated Intravascular Coagulation (DIC) Score, was used to forecast mortality in DSS [19]. A decision tree algorithm was used to
differentiate dengue fever from other types of fever and also
ISRN Pediatrics
Table 1: Patient profiles by types of dengue infection: dengue fever (DF), dengue hemorrhagic fever (DHF), and dengue shock syndrome
(DSS).
Patient profiles
Demographic
Male (, %)
Age (year)
Mode of presentation
Hepatomegaly (, %)
Headache (, %)
Myalgia (, %)
Vomiting (, %)
Cough (, %)
Abdominal pain (, %)
Rash (, %)
Pleural effusion (, %)
Petechiae (, %)
Any bleeding episodes (, %)
Hemodynamic
SBP (mmHg)
DBP (mmHg)
Pulse pressure (mmHg)
Hematological
Hematocrit (%)
Hemoglobin (g/dL)
White cell count (/L)
Lymphocytes (%)
Neutrophils (%)
Platelet (/L)
Biochemical
AST (U/L)
ALT (U/L)
PT (sec)
PTT (sec)
Case management
Inbound referral (, %)
Discharged
Alive (, %)
Outbound referral (, %)
In hospital dead (, %)
DF ( = 391)
Mean SD
DHF ( = 296)
Mean SD
DSS ( = 90)
Mean SD
value
185 (47.3)
9.5 3.4
153 (51.7)
10.1 3.1
38 (42.2)
9.0 3.5
0.888
0.903
8 (2.1)
228 (58.3)
84 (21.5)
244 (62.4)
120 (30.7)
160 (40.9)
166 (42.5)
0 (0)
27 (6.9)
73 (18.7)
26 (8.8)
145 (49.0)
30 (10.1)
216 (73.0)
94 (31.8)
181 (61.2)
132 (44.6)
20 (6.8)
26 (8.8)
80 (27.0)
55 (61.1)
35 (38.9)
12 (13.3)
56 (62.2)
32 (35.6)
60 (66.7)
26 (28.9)
34 (37.8)
14 (15.6)
51 (56.7)
<0.001
<0.001
0.001
0.187
0.425
<0.001
0.124
<0.001
0.016
<0.001
97.0 9.2
58.4 7.7
33.1 6.7
96.9 10.1
58.2 8.6
32.1 7.6
91.3 10.3
58.6 8.4
24.0 7.7
<0.001
0.084
<0.001
38.8 4.5
12.7 1.5
3748.0 1706.5
44.9 17.3
44.7 18.8
122693.6 9763.9
40.5 4.8
13.4 1.5
4271.3 1821.8
40.8 15.7
49.5 18.1
81869.0 7975.7
42.4 5.4
14.1 1.8
5479.3 2063.4
40.0 16.3
48.9 17.6
50481.5 6262.9
<0.001
<0.001
<0.001
<0.001
<0.001
<0.001
126.7 313.7
60.1 216.1
12.0 1.5
30.4 5.4
269.0 457.1
95.0 271.7
12.1 1.8
42.0 10.0
558.9 659.0
219.8 413.2
15.5 9.5
44.7 12.3
<0.001
0.001
0.012
0.004
43 (11.0)
78 (26.4)
48 (53.3)
<0.001
391 (100.0)
0 (0)
0 (0)
296 (100.0)
0 (0)
0 (0)
88 (97.8)
2 (2.2)
0 (0)
1.000
value from nonparametric test for trend.
SD: standard deviation; SBP: systolic blood pressure; DBP: diastolic blood pressure; AST: aspartate aminotransferase; ALT: alanine aminotransferase; PT:
prothrombin time; PTT: partial thromboplastin time.
to forecast severity in dengue infection [20]. Some studies
applied DIC scoring system to diagnose DIC more precisely,
using clinical signs and symptoms and routine laboratory
investigations to differentiate DHF from DF [21]. Most of the
prediction systems in the past focused on clinical outcomes
of the disease. There are few studies that focused directly on
dengue infection severity.
The aim of the present study was to develop a simple
clinical risk scoring system to predict dengue infection
severity, based on patient clinical characteristics and routine
laboratory investigations, obtained from the previous investigation [22].
2. Materials and Methods
2.1. Patients. The medical records of children aged 115 years
with dengue infection between 2007 to 2010 in the three
university-affiliated general hospitals located in the northern
region of Thailand, Sawanpracharak Hospital in Nakorn
ISRN Pediatrics
3
Table 2: Significant predictors of dengue infection severity and assigned item scores.
Predictors
Age (year)
Hepatomegaly
Hematocrit (%)
SBP (mmHg)
White cell count (/L)
Platelet (/L)
Category
>6
6
Yes
No
40
<40
<90
90
>5000
5000
50000
>50000
OR
1.46
12.31
1.34
1.70
1.40
3.95
95% CI
1.121.91
Ref
8.8417.15
Ref
1.101.64
Ref
1.322.17
Ref
1.131.75
Ref
3.144.96
Ref
value
Coefficient
0.005
0.38
<0.001
2.51
0.003
0.30
<0.001
0.53
0.002
0.34
<0.001
1.37
Score
1
0
8.5
0
1
0
2
0
1
0
4.5
0
Coefficients from multivariable ordinal logistic regression. OR: odds ratio; CI: confidence interval; ref: reference category; SBP: systolic blood pressure.
Table 3: Severity score levels, severity levels, and risk estimation validity.
Severity score levels
Mean SD
IQR
DF ( = 451)
DHF ( = 276)
DSS ( = 50)
Score range
<2.5
2.511.5
>11.5
DF ( = 391)
3.6 2.1
2.04.8
297
94
0
Severity levels
DHF ( = 296)
5.1 3.2
3.85.8
149
136
11
DSS ( = 90)
11.0 4.1
6.813.3
5
46
39
Total
Risk estimation validity
Over (%)
Correct (%)
Under (%)
12.1
1.4
13.5
38.2
17.5
5.0
60.7
19.8
5.9
25.7
Percentage of total patients.
SD: standard deviation; IQR: interquartile range.
Sawan, Uttaradit Hospital in Uttaradit, and Kamphaeng Phet
Hospital in Kamphaeng Phet, were reviewed. The data were
retrieved from the hospital database, under the following
ICD-10: A90-dengue fever, A91-dengue hemorrhagic fever,
and A910-dengue hemorrhagic fever with shock.
(1) dengue infection (DF): acute or abrupt onset of fever,
accompanied by a positive tourniquet test, and white
blood count 5,000/L [23];
(2) dengue hemorrhagic fever (DHF): all of the following
items [24]:
2.2. Indicator Parameters. The patient characteristics with
potential prediction included
(5) biochemical profiles: aspartate aminotransferase
(AST), alanine aminotransferase (ALT), prothrombin
time (PT), and partial thromboplastin time (PTT).
(i) acute or abrupt fever for 27 days,
(ii) at least one of the following bleeding episodes:
(a) positive tourniquet test,
(b) petechiae, ecchymoses, or purpura,
(c) bleeding from mucosa, gastrointestinal
tract, injection sites, or other location,
(d) hematemesis or melena,
(iii) platelet 100,000/L,
(iv) at least one of the following plasma leakage
evidence items:
(a) hemoconcentration assessed by an increase
in hematocrit 20% from previous hematocrit,
(b) signs of plasma leakage, such as pleural
effusion or ascites, or evidence of hypoalbuminemia;
2.3. Definition of Dengue Severity. The severity of dengue
infection was operationally defined by the following criteria:
(3) dengue shock syndrome (DSS): all items for dengue
hemorrhagic fever above, accompanied with evidence
of circulatory failure [24]:
(1) demographic: gender and age;
(2) mode of presentation: hepatomegaly, headache, myalgia, vomiting, cough, abdominal pain, rash, pleural
effusion, petechiae, and any bleeding episodes;
(3) hemodynamic profiles: pulse pressure, systolic blood
pressure (SBP), and diastolic blood pressure (DBP);
(4) hematological profiles: hematocrit, hemoglobin,
white cell count, lymphocytes, neutrophils, and platelet;
ISRN Pediatrics
(i) rapid and weak pulse,
(ii) pulse pressure 20 mmHg,
or manifested by
(i) hypotension,
(ii) cold body temperature or irritable.
Dengue severity was classified into 4 grades, based on
bleeding episodes and shock, as follows:
grade 1: no evidence of bleeding, Positive Tourniquet
test,
grade 2: evidences of bleeding episodes,
grade 3: presence of week and rapid pulse rate, low
blood pressure, or narrow pulse pressure,
grade 4: nonmeasurable blood pressure or nonpalpable pulse.
grades 1-2 were classified as DHF and grades 3-4 were
classified as DSS [24].
2.4. Data Analysis. Potential predictors for dengue severity
from a previous report [22] were tested with nonparametric test for trend. The predictive ability was analyzed by
multivariable ordinal logistic regression and presented with
coefficients and odds ratios. Missing data were replaced by
the mean values of the parameters. Assigned item scores were
derived by transformation of coefficient of parameters. The
total (sum) scores were used to classify patients into 3 severity
levels. The distribution of scores across the three severity
groups were presented with box plots. The discriminative
and predictive abilities of the scores were presented with
probability curves.
2.5. Ethical Approval. The present investigation was approved
by the Research Ethical Committee of the Faculty of
Medicine, Chiang Mai University, and the research ethical
committees of the three hospitals.
3. Results
A total of 777 patients with dengue infection were classified
based on the above criteria into 3 severity levels: DF ( =
391), DHF ( = 296), and DSS ( = 90).
3.1. Significant Predictors. Under the univariable analysis, the
three severity groups were similar in gender ( = 0.888), age
( = 0.903), presence of vomiting ( = 0.187), cough ( =
0.425), rash ( = 0.124), and DBP ( = 0.084) but were difference according to the presence of hepatomegaly, headache,
myalgia, abdominal pain, pleural effusion, petechiae, bleeding episodes, SBP, pulse pressure, hematocrit, hemoglobin,
white cell count, lymphocytes, neutrophils, platelets, AST,
ALT, PT, and PTT (Table 1).
Under the multivariable analysis, the clinical characteristics with significant predictive ability for dengue severity
included age > 6 years (OR = 1.46, 95% CI = 1.121.91, =
0.005), hepatomegaly (OR = 12.31, 95% CI = 8.8417.15, <
0.001), hematocrit 40% (OR = 1.34, 95% CI = 1.101.64,
= 0.003), SBP < 90 mmHg (OR = 1.70, 95% CI = 1.322.17,
< 0.001), white cell count > 5000/L (OR = 1.40, 95% CI
= 1.131.75, = 0.002), and platelet 50000/L (OR = 3.95,
95% CI = 3.144.96, < 0.001). The strongest predictors were
hepatomegaly (OR = 12.31) and platelet 50000/L (OR =
3.95) (Table 2).
3.2. The Scoring System. Transformation of significant parameter coefficients into item scores was done by division
of each coefficient with the smallest coefficient of the model
(0.30) and rounded up or down to the nearest 0.5 integers. The
item scores ranged from 0 to 8.5, and the total score ranged
from 0 to 18 (Table 2).
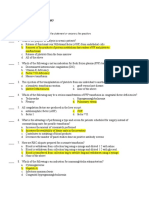
3.3. Discriminations. The mean total severity scores in
patients with DF, DHF, and DSS were 3.6 2.1, 5.1 3.2,
and 11.0 4.1 (Table 3). The distribution of the derived
severity scores was different among the three severity groups
(Figure 1). The derived scores also discriminated DHF from
DF and also discriminated DSS from DHF (Figure 2).
3.4. Clinical Predictions. Our scoring system discriminated
DSS and DHF from DF with an area under the receiver
operation curve (AuROC) of 0.7416 (95% CI = 0.72940.7537,
figure not shown) and discriminated DSS from DHF and DF
with a higher AuROC of 0.8877 (95% CI = 0.87880.8964,
figure not shown).
Cut-off points were assigned to classified patients as 3
severity groups: scores <2.5 (DF), scores 2.511.5 (DHF), and
scores >11.5 (DSS). The score <2.5 predicted DF correctly in
297 out of 391 patients with 1-level underestimation in 149
patients (19.2%) and 2-level underestimation in 5 patients
(0.6%) or a total of 19.8% underestimation.
The scores between 2.5 and 11.5 predicted DHF correctly
in 136 out of 296 patients, with an underestimation in 46
patients (5.9%) and an overestimation in 94 patients (12.1%).
The scores >11.5 predicted DSS correctly in 39 out of 90
patients, with 1-level overestimation in 1 out of 11 patients
(1.4%), with no 2-level overestimation (0%), or a total of 1.4%
overestimation (Table 3).
4. Discussions
Dengue infection is an urgent condition requiring prompt
diagnosis and treatment before patients enter into bleeding
or shock states. Previous scoring systems trying to evaluate or
forecast disease severity included the Dengue Fever Scoring
System based on epidemiological information and clinical
signs or symptoms, which might be useful in detecting
DF very early prior to laboratory results [25]. Other scoring systems were the Pediatric Logistic Organ Dysfunction
(PELOD) Score and the Pediatric Risk of Mortality III
(PRISM III), used to evaluate the mortality rates [26], and
the Disseminate Intravascular Coagulation (DIC) Score to
diagnose DIC and to discriminate DF and DHF from other
febrile illnesses [27].
ISRN Pediatrics
5
nonroutine predictors were not available in many primary
care centers. An investment on such facilities may not be
feasible and may not be cost effective.
Our study developed a scoring system based on clinical risk and routine laboratory parameters and categorized
patients with dengue infection into DF, DHF, or DSS.
DSS
DHF
DF
10
12
14
16
18
20
Dengue severity score
Figure 1: Distribution of dengue severity scores by severity levels.
Vertical lines in box represent medians. Box boundaries represent
the twenty-fifth and seventy-fifth percentiles.
1
Probability
0.8
DF
0.6
DHF
0.4
DSS
0.2
0
0
10
12
14
16
18
20
Dengue severity score
DF versus DHF
DHF versus DSS
Figure 2: Discrimination of dengue severity scores. Solid line:
dengue fever (DF) versus dengue hemorrhagic fever (DHF). Dash
line: dengue hemorrhagic fever (DHF) versus dengue shock syndrome (DSS). Vertical dotted lines represent boundaries (cut-off
points) of the scores.
Decision tree algorithms were also applied to classify
dengue infections into DF, DHF grade I, DHF grade II, and
DHF grade III [28]. They may also predict patients with low
risk who may be discharged safely and select patients with
high risk who should be admitted for close monitoring [29].
These studies used clinical symptoms and/or laboratory
tests to evaluate or forecast the risks. Some studies included
only adult patients [25, 29] which may or may not be relevant
for children. In studies which included children, some studies
used information on the first few days of admission in
pediatric intensive care unit (PICU) [19]. In some studies,
included DHF patients did not experience shock and may not
be inferred to patients with DSS [21]. Risk prediction in many
studies was based on nonroutine laboratory investigations
[19, 20, 26, 28, 29]. Despite their high predictive powers, those
(1) Patients scoring <2.5 were classified as DF which
is the mildest form. These patients normally do
not require hospital admission even in the feverish
stage. Patients may safely be handled as outpatients
with symptomatic treatments and may be advised
to observe any abnormal signs or symptoms with a
follow-up appointment.
(2) Patients scoring between 2.5 and 11.5 were classified
as a risk group for DHF. These patients should be
admitted to be closely monitored for early signs of
plasma leakage, hemoconcentration, coagulopathy,
thrombocytopenia.
(3) Patients scoring >11.5 were classified as a risk group
for DSS. These patients should also be admitted to
monitor any early signs of shock.
Our scoring system predicted DSS correctly with a positive predictive value (PPV) of 88%, similar to other studies
which reported a PPV of 8295% [20, 26]. The score may be
used to discriminate DSS from DF and DHF.
However, the fact that the derived scores in DF and DHF
were more or less overlapping made it less likely to be used
to differentiate DHF for DF. Other nonroutine predictors
specifically for DHF may be required.
In case of continuous routine laboratory investigations,
our score may also be used to monitor the patients risk for
DSS as the disease progresses from day to day. In case of
outpatients, this will help clinicians make decision when to
admit the patients to hospital. Application of this scoring
system into routine patient care may help reduce unnecessary
admission and also reduce case facility in severe cases that are
admitted based on high risk scores.
5. Conclusions
The derived dengue infection severity score classified patients
into DF, DHF, or DSS, correctly into their original severity
levels. Validation of the score should be reconfirmed before
application into routine practice.
Conflict of Interests
This investigation was partially supported by the Research
Grant for Basic and Applied Sciences, the Faculty of
Medicine, Chiang Mai University.
Acknowledgments
The authors wish to thank the authorities of the three
hospitals for their support in data collection and wish to
thank the Faculty of Medicine, Chiang Mai University, for the
partial grant support.
References
[1] World Health Organization, Dengue and dengue haemorrhagic fever, Fact sheet no. 117, World Health Organization,
Geneva, Switzerland, 2008, http://www.who.int/mediacentre/
factsheets/fs117/en/.
[2] D. S. Shepard, L. Coudeville, Y. A. Halasa, B. Zambrano, and G.
H. Dayan, Economic impact of dengue illness in the Americas,
American Journal of Tropical Medicine and Hygiene, vol. 84, no.
2, pp. 200207, 2011.
[3] Y. K. Sarin, S. Singh, and T. Singh, Dengue viral infection,
Indian Pediatrics, vol. 35, no. 2, pp. 129137, 1998.
[4] M. G. Guzman and G. Kour, Dengue diagnosis, advances and
challenges, International Journal of Infectious Diseases, vol. 8,
no. 2, pp. 6980, 2004.
[5] C. X. T. Phuong, N. T. Nhan, R. Kneen et al., Clinical diagnosis
and assessment of severity of confirmed dengue infections
in Vietnamese children: is the World Health Organization
classification system helpful? American Journal of Tropical
Medicine and Hygiene, vol. 70, no. 2, pp. 172179, 2004.
[6] M. Neeraja, V. Lakshmi, V. D. Teja, P. Umabala, and M. V.
Subbalakshmi, Serodiagnosis of dengue virus infection in
patients presenting to a tertiary care hospital, Indian Journal
of Medical Microbiology, vol. 24, no. 4, pp. 280282, 2006.
[7] K. L. Anders, N. M. Nguyet, N. V. V. Chau et al., Epidemiological factors associated with dengue shock syndrome and
mortality in hospitalized dengue patients in Ho Chi Minh City,
Vietnam, American Journal of Tropical Medicine and Hygiene,
vol. 84, no. 1, pp. 127134, 2011.
[8] V. Gupta, T. P. Yadav, R. M. Pandey et al., Risk factors of dengue
shock syndrome in children, Journal of Tropical Pediatrics, vol.
57, no. 6, pp. 451456, 2011.
[9] J. Junia, H. Garna, and D. Setiabudi, Clinical risk factors for
dengue shock syndrome in children, Paediatrica Indonesiana,
vol. 47, no. 1, pp. 711, 2007.
[10] S. B. Halstead and L. C. Lum, Assessing the prognosis of
dengue-infected patients, F1000 Medicine Reports, vol. 1, article
73, 2009.
[11] A. K. I. Falconar and C. M. E. Romero-Vivas, Simple prognostic criteria can definitively identify patients who develop
severe versus non-severe dengue disease, or have other febrile
illnesses, Journal of Clinical Medicine Research, vol. 4, no. 1, pp.
3344, 2012.
[12] T. Tantracheewathorn and S. Tantracheewathorn, Risk factors
of dengue shock syndrome in children, Journal of the Medical
Association of Thailand, vol. 90, no. 2, pp. 272277, 2007.
[13] N. Pichainarong, N. Mongkalangoon, S. Kalayanarooj, and
W. Chaveepojnkamjorn, Relationship between body size and
severity of dengue hemorrhagic fever among children aged 014
years, Southeast Asian Journal of Tropical Medicine and Public
Health, vol. 37, no. 2, pp. 283288, 2006.
[14] S. Kalayanarooj and S. Nimmannitya, Is dengue severity
related to nutritional status? Southeast Asian Journal of Tropical
Medicine and Public Health, vol. 36, no. 2, pp. 378384, 2005.
[15] K. Alam, S. A. S. Sulaiman, A. A. Shafie, and E. Yusuf, Clinical
manifestations and laboratory profile of dengue fever among
the patients general Hospital, Penang, Archives of Pharmacy
Practice, vol. 1, no. 1, pp. 2529, 2010.
[16] A. Chuansumrit, C. Puripokai, P. Butthep et al., Laboratory
predictors of dengue shock syndrome during the febrile stage,
Southeast Asian Journal of Tropical Medicine and Public Health,
vol. 41, no. 2, pp. 326332, 2010.
ISRN Pediatrics
[17] I. Shah, G. C. Deshpande, and P. N. Tardeja, Outbreak of
dengue in Mumbai and predictive markers for dengue shock
syndrome, Journal of Tropical Pediatrics, vol. 50, no. 5, pp. 301
305, 2004.
[18] F. R. F. G. Azin, R. P. Goncalves, M. H. D. S. Pitombeira, D.
M. Lima, and I. C. Branco, Dengue: profile of hematological
and biochemical dynamics, Revista Brasileira de Hematologia e
Hemoterapia, vol. 34, no. 1, pp. 3641, 2012.
[19] L. P. Dewi and E. Nurfitri, Pediatric logistic organ dysfunction
score as a predictive tool of dengue shock syndrome outcomes,
Paediatrica Indonesiana, vol. 52, no. 2, pp. 7277, 2012.
[20] L. Tanner, M. Schreiber, J. G. H. Low et al., Decision tree
algorithms predict the diagnosis and outcome of dengue fever
in the early phase of illness, PLoS Neglected Tropical Diseases,
vol. 2, no. 3, article e196, 2008.
[21] C. C. Carlos, K. Oishi, M. T. D. D. Cinco et al., Comparison
of clinical features and hematologic abnormalities between
dengue fever and dengue hemorrhagic fever among children
in the Philippines, American Journal of Tropical Medicine and
Hygiene, vol. 73, no. 2, pp. 435440, 2005.
[22] S. Pongpan, A. Wisitwong, C. Tawichasri, and J. Patumanond,
Prognostic indicators for dengue infection severity, International Journal of Clinical Pediatrics, vol. 2, no. 1, pp. 1218, 2013.
[23] S. Sawasdivorn, S. Vibulvattanakit, M. Sasavatpakdee, and S.
Iamsirithavorn, Efficacy of clinical diagnosis of dengue fever
in paediatric age groups as determined by WHO case definition
1997 in Thailand, Dengue Bulletin, vol. 25, pp. 5664, 2001.
[24] World Health Organization, Dengue Hemorrhagic Fever: Diagnosis, Treatment, Prevention and Control, World Health Organization, Geneva, Switzerland, 1997.
[25] K. Chang, P.-L. Lu, W.-C. Ko et al., Dengue fever scoring
system: new strategy for the early detection of acute dengue
virus infection in Taiwan, Journal of the Formosan Medical
Association, vol. 108, no. 11, pp. 879885, 2009.
[26] H. R. Iskandar, D. Mulyo, P. Agnes, and Y. Suryatin, Comparison of pediatric logistic organ dysfunction (PELOD) score and
pediatric risk of mortality (PRISM) III as a mortality predictor
in patients with dengue shock syndrome, Pediatrics, vol. 121,
supplement 2, p. S129, 2008.
[27] K. Oishi, C. A. Mapua, C. C. Carlos et al., Dengue and other
febrile illnesses among children in the Philippines, Dengue
Bulletin, vol. 30, pp. 2634, 2006.
[28] D. Thitiprayoonwongse, P. Suriyapkol, and N. Soonthornphisaj,
Data mining of dengue infection using decision tree, in Latest
Advances in Information Science and Applications: The 12th
WSEAS International Conference on Applied Computer Science,
pp. 154159, 2012.
[29] V. J. Lee, D. C. Lye, Y. Sun, and Y. S. Leo, Decision tree
algorithm in deciding hospitalization for adult patients with
dengue haemorrhagic fever in Singapore, Tropical Medicine
and International Health, vol. 14, no. 9, pp. 11541159, 2009.
Vous aimerez peut-être aussi
- Infectious Diseases: Smart Study Guide for Medical Students, Residents, and Clinical ProvidersD'EverandInfectious Diseases: Smart Study Guide for Medical Students, Residents, and Clinical ProvidersPas encore d'évaluation
- Complementary and Alternative Medical Lab Testing Part 8: UrologyD'EverandComplementary and Alternative Medical Lab Testing Part 8: UrologyÉvaluation : 3 sur 5 étoiles3/5 (1)
- RMHP 7 045Document5 pagesRMHP 7 045melisaberlianPas encore d'évaluation
- Dengue Infection in Cancer Patients: Department of MedicineDocument18 pagesDengue Infection in Cancer Patients: Department of MedicinesummiyaPas encore d'évaluation
- SOFA ScoreDocument9 pagesSOFA ScoreIfone takahepisPas encore d'évaluation
- Chairuddin P. Lubis, Syahril Pasaribu, Ayodhia P. Pasaribu, Inke Nadia D. LubisDocument58 pagesChairuddin P. Lubis, Syahril Pasaribu, Ayodhia P. Pasaribu, Inke Nadia D. LubisAhmed MawardiPas encore d'évaluation
- 1 StrokeDocument10 pages1 StrokeRekyan ListyaningsihPas encore d'évaluation
- 1382-Article Text-5022-1-10-20180430 PDFDocument4 pages1382-Article Text-5022-1-10-20180430 PDFFadillPas encore d'évaluation
- Nternational Ournal of Esearch Cience & AnagementDocument6 pagesNternational Ournal of Esearch Cience & AnagementhafizmahruzzaPas encore d'évaluation
- Abses HeparDocument4 pagesAbses HeparIecHa RizkaMaulidaPas encore d'évaluation
- L4. T2.M2 y M6. Predictive Factors For Induction of Remission in Patients With Active ARDocument5 pagesL4. T2.M2 y M6. Predictive Factors For Induction of Remission in Patients With Active ARJhon Andy RamosPas encore d'évaluation
- Asia - Pan - Dysglycaemia and Cardiovascular Risk Û Asian ExperienceDocument18 pagesAsia - Pan - Dysglycaemia and Cardiovascular Risk Û Asian ExperienceputrakartonoPas encore d'évaluation
- E Cacy of Emergency Severity Index (ESI) in Early Identi Cation of Patients With Sepsis and Septic Shock at TriageDocument10 pagesE Cacy of Emergency Severity Index (ESI) in Early Identi Cation of Patients With Sepsis and Septic Shock at Triageputujunidtd13Pas encore d'évaluation
- Hellp 2Document7 pagesHellp 2Nur Rahmat WibowoPas encore d'évaluation
- Moulis2018 PDFDocument4 pagesMoulis2018 PDFDwita MargarethPas encore d'évaluation
- Mottling Score - ICM 2011Document7 pagesMottling Score - ICM 2011cyelzPas encore d'évaluation
- Carraro 2013 RSBMTV 46 N 2 P 161Document5 pagesCarraro 2013 RSBMTV 46 N 2 P 161Emerson CarraroPas encore d'évaluation
- Intravenous IbuprofenDocument13 pagesIntravenous Ibuprofenhumberto_freirePas encore d'évaluation
- Survival Advantage of Hemodialysis Relative To Peritoneal Dialysis in Patients With End-Stage Renal Disease and Congestive Heart FailureDocument8 pagesSurvival Advantage of Hemodialysis Relative To Peritoneal Dialysis in Patients With End-Stage Renal Disease and Congestive Heart FailureaduhbingungPas encore d'évaluation
- Role of Platelet Transfusions in Dengue Hemorrhagic Fever-6 Months ReportDocument5 pagesRole of Platelet Transfusions in Dengue Hemorrhagic Fever-6 Months ReportAnonymous 7jKR9XbPas encore d'évaluation
- Clinical Profile of Young Hypertensives.Document8 pagesClinical Profile of Young Hypertensives.IOSRjournalPas encore d'évaluation
- Maternal and Fetal Factors in Pregnancy With Oligohydramnios and Maternal and Perinatal OutcomeDocument4 pagesMaternal and Fetal Factors in Pregnancy With Oligohydramnios and Maternal and Perinatal Outcomepuji arisPas encore d'évaluation
- Zhes055740 ww1Document8 pagesZhes055740 ww1Vincent PratamaPas encore d'évaluation
- DR Suhendro - Sepsis SOLODocument25 pagesDR Suhendro - Sepsis SOLOOlivia DwimaswastiPas encore d'évaluation
- Bài Giảng Cô Siripen (SXH Ngày 9.5.2018)Document64 pagesBài Giảng Cô Siripen (SXH Ngày 9.5.2018)Minh HoàngPas encore d'évaluation
- Komplikasi Stroke PDFDocument7 pagesKomplikasi Stroke PDFJose Hady PuteraPas encore d'évaluation
- IJCRT23A5059Document9 pagesIJCRT23A5059Agus SunardiPas encore d'évaluation
- AppbjDocument6 pagesAppbjGilang IrwansyahPas encore d'évaluation
- Angina Pectoris and Atherosclerotic Risk Factors in The MultisiteDocument8 pagesAngina Pectoris and Atherosclerotic Risk Factors in The Multisiteger4ld1nPas encore d'évaluation
- Etiology of Peritonitis and Factors Predicting PDFDocument4 pagesEtiology of Peritonitis and Factors Predicting PDFadistayaPas encore d'évaluation
- Disseminated Intravascular Coagulation Initial Score As A Predictor ofDocument6 pagesDisseminated Intravascular Coagulation Initial Score As A Predictor ofPriska ForceveeanaPas encore d'évaluation
- Clinical Characteristics of 161 Cases of Corona Virus Disease 2019 (COVID-19) in ChangshaDocument7 pagesClinical Characteristics of 161 Cases of Corona Virus Disease 2019 (COVID-19) in ChangshaHesbon MomanyiPas encore d'évaluation
- Factors Which Affect Mortality in Neonatal Sepsis: Original ArticleDocument6 pagesFactors Which Affect Mortality in Neonatal Sepsis: Original ArticleNabila NatasyaPas encore d'évaluation
- Dengue Score A Proposed Diagnostic Predictor For PDocument8 pagesDengue Score A Proposed Diagnostic Predictor For PAmiImoetPas encore d'évaluation
- Journal SDocument6 pagesJournal SLyla SandyPas encore d'évaluation
- 2019 Glomerulonefritis Pos-Inf Pedi Clin NADocument14 pages2019 Glomerulonefritis Pos-Inf Pedi Clin NA0511821012 KATHERIN YULEIMA CAMACHO MARIN ESTUDIANTE ACTIVOPas encore d'évaluation
- Garuda 1352125Document6 pagesGaruda 1352125lisa anggrianiPas encore d'évaluation
- Sex Transm Infect. 2011 Aug 87 (5) 385-8Document6 pagesSex Transm Infect. 2011 Aug 87 (5) 385-8Cynthia Patricia Manotas AltamarPas encore d'évaluation
- Cazuri CliniceDocument32 pagesCazuri CliniceHeba VerebceanPas encore d'évaluation
- GMR 6939Document6 pagesGMR 6939Alfa FebriandaPas encore d'évaluation
- Syphilis in Pregnancy - Prevalence at Different Levels of Health Care in DurbanDocument2 pagesSyphilis in Pregnancy - Prevalence at Different Levels of Health Care in DurbanIqaPas encore d'évaluation
- Increased Serum Hyaluronic Acid and Heparan Sulfate in Dengue Fever: Association With Plasma Leakage and Disease SeverityDocument9 pagesIncreased Serum Hyaluronic Acid and Heparan Sulfate in Dengue Fever: Association With Plasma Leakage and Disease SeverityLaura Zuñiga TorresPas encore d'évaluation
- Age +estimated+glomerular+filtration+rate+and+ejection+fraction+score+predicts+contrast-Induced+acute+kidney+injury+in+patients+with+diabetes+and+chronic+kidney+disease +insight+from+the+TRACK-D+studyDocument5 pagesAge +estimated+glomerular+filtration+rate+and+ejection+fraction+score+predicts+contrast-Induced+acute+kidney+injury+in+patients+with+diabetes+and+chronic+kidney+disease +insight+from+the+TRACK-D+studyangga_darmawan26Pas encore d'évaluation
- Impact of Genotype On Endocrinal Complications in Thalassemia PatientsDocument9 pagesImpact of Genotype On Endocrinal Complications in Thalassemia PatientsZakirPas encore d'évaluation
- The Distribution of Intraocular Pressure and Its Association With Metabolic Syndrome in A CommunityDocument6 pagesThe Distribution of Intraocular Pressure and Its Association With Metabolic Syndrome in A CommunityAngkat Prasetya Abdi NegaraPas encore d'évaluation
- PVDI Scientific AbstractsDocument2 pagesPVDI Scientific AbstractsBombinTallerdeTeatroPas encore d'évaluation
- Comparative Analysis of Severe Pediatric and Adult Leptospirosis in Sa o Paulo, BrazilDocument3 pagesComparative Analysis of Severe Pediatric and Adult Leptospirosis in Sa o Paulo, BrazilShofura AzizahPas encore d'évaluation
- AOMS Art 27572-10Document5 pagesAOMS Art 27572-10nugroho agung cahyonoPas encore d'évaluation
- Prevalence and Risk Factors of Thyroid-Associated Ophthalmopathy Among IndiansDocument4 pagesPrevalence and Risk Factors of Thyroid-Associated Ophthalmopathy Among IndiansLastry WardaniPas encore d'évaluation
- Prevalence of Hypothyroidism in Patients With Chronic Kidney Disease: A Cross-Sectional Study From North IndiaDocument4 pagesPrevalence of Hypothyroidism in Patients With Chronic Kidney Disease: A Cross-Sectional Study From North IndiaReuben JosephPas encore d'évaluation
- Research Journal4Document5 pagesResearch Journal4Jayhan AmbrocioPas encore d'évaluation
- The Use of Procalcitonin As A Marker of Sepsis in Children: Abst TDocument3 pagesThe Use of Procalcitonin As A Marker of Sepsis in Children: Abst TAsri RachmawatiPas encore d'évaluation
- Original Article Knowledge, Attitudes and Practices of Health Care Workers Regarding Needle Stick Injuries at A Tertiary Care Hospital in PakistanDocument4 pagesOriginal Article Knowledge, Attitudes and Practices of Health Care Workers Regarding Needle Stick Injuries at A Tertiary Care Hospital in PakistanAntonio LaraPas encore d'évaluation
- Mottling Score Predicts Survival in Septic Shock: OriginalDocument7 pagesMottling Score Predicts Survival in Septic Shock: OriginalSolange Muñoz ArayaPas encore d'évaluation
- Jof 06 00318Document10 pagesJof 06 00318Robertus RonnyPas encore d'évaluation
- Umapathy 2017Document11 pagesUmapathy 2017Karinaayu SerinPas encore d'évaluation
- Predictors of Spontaneous Bleeding in DengueDocument4 pagesPredictors of Spontaneous Bleeding in DengueSawettachai JaitaPas encore d'évaluation
- Maternal Early WarningDocument10 pagesMaternal Early WarningJEFFERSON MUÑOZPas encore d'évaluation
- Sepsis-3: Jeffrey Ariesta PutraDocument35 pagesSepsis-3: Jeffrey Ariesta PutraMaria FernandezPas encore d'évaluation
- Top Trials in Gastroenterology & Hepatology, 2nd EditionD'EverandTop Trials in Gastroenterology & Hepatology, 2nd EditionPas encore d'évaluation
- Breastfeeding BasicsDocument38 pagesBreastfeeding BasicsValencius SunandarPas encore d'évaluation
- Clinical Profile and Outcome of Dengue Fever CasesDocument2 pagesClinical Profile and Outcome of Dengue Fever CasesValencius SunandarPas encore d'évaluation
- BFHI Revised Section2.4.a SlidesDocument92 pagesBFHI Revised Section2.4.a SlidesValencius SunandarPas encore d'évaluation
- Paediatric Imaging Guidelines - FinDocument7 pagesPaediatric Imaging Guidelines - FinValencius SunandarPas encore d'évaluation
- Tekgul S Et A Eur Urol 2012 62 (3) 534 EAU Guidelines On Veicoureteral Reflux in ChildrenDocument9 pagesTekgul S Et A Eur Urol 2012 62 (3) 534 EAU Guidelines On Veicoureteral Reflux in ChildrenValencius SunandarPas encore d'évaluation
- Bode Anyas 1999Document19 pagesBode Anyas 1999Valencius SunandarPas encore d'évaluation
- CP Boys CurveDocument4 pagesCP Boys CurveValencius SunandarPas encore d'évaluation
- Mesenteric Cyst, Cause or EffectDocument5 pagesMesenteric Cyst, Cause or EffectValencius SunandarPas encore d'évaluation
- RBC PathoDocument40 pagesRBC PathoMadhumitha ElangovanPas encore d'évaluation
- Disorders of Coagulation FactorsDocument35 pagesDisorders of Coagulation FactorsMelesPas encore d'évaluation
- IFU Dia TT EN 20170915Document2 pagesIFU Dia TT EN 20170915P managerPas encore d'évaluation
- Borromeo vs. Family Care HospitalDocument2 pagesBorromeo vs. Family Care HospitalRyo100% (1)
- Management of Severe Malaria CasesDocument100 pagesManagement of Severe Malaria CasesAshis karmakarPas encore d'évaluation
- UpToDate Massive Blood TransfusionDocument10 pagesUpToDate Massive Blood TransfusionAlice HuiiPas encore d'évaluation
- Hemodynamic Disorders, Thromboembolic Disease, and ShockDocument87 pagesHemodynamic Disorders, Thromboembolic Disease, and Shockgifty100% (1)
- Bleeding & Coagulopathies in Clinical CareDocument20 pagesBleeding & Coagulopathies in Clinical CareKarina Mega WPas encore d'évaluation
- V3 Eng PDFDocument848 pagesV3 Eng PDFaidhaPas encore d'évaluation
- Mehlmanmedical Hy Heme/OncDocument46 pagesMehlmanmedical Hy Heme/Oncnav_malhiPas encore d'évaluation
- Hematologic DisorderDocument16 pagesHematologic Disorderjulesubayubay5428Pas encore d'évaluation
- Torts and Damages IIDocument39 pagesTorts and Damages IIMichael JoffPas encore d'évaluation
- Transfusion TherapyDocument14 pagesTransfusion TherapyCMLPas encore d'évaluation
- Disseminated Intravascular CoagulationDocument29 pagesDisseminated Intravascular CoagulationAnju RadhikaPas encore d'évaluation
- Disseminated Intravascular Coagulopathy Dic 1 1Document25 pagesDisseminated Intravascular Coagulopathy Dic 1 1api-394684626Pas encore d'évaluation
- Midterm NotesDocument28 pagesMidterm NotesGen FranchesKyle Cortez ErigbuagasPas encore d'évaluation
- DIC in Pregnancy - Pathophysiology, Clinical CharDocument4 pagesDIC in Pregnancy - Pathophysiology, Clinical CharSaurabh SalunkhePas encore d'évaluation
- PNLE III For Medical Surgical Nursing - RNpediaDocument13 pagesPNLE III For Medical Surgical Nursing - RNpediaLot RositPas encore d'évaluation
- J Transci 2018 10 013Document7 pagesJ Transci 2018 10 013Clara Espinosa ArnandisPas encore d'évaluation
- Coagulation of BloodDocument16 pagesCoagulation of BloodMoner ManushPas encore d'évaluation
- Hema Finals LabDocument2 pagesHema Finals LabKimverlyn Balanay AgpaloPas encore d'évaluation
- Blood TransfusionDocument22 pagesBlood TransfusionDinda KusumaPas encore d'évaluation
- Transes Pre Final HematologyDocument20 pagesTranses Pre Final HematologyMrdy CaiPas encore d'évaluation
- DIC in PregnancyDocument24 pagesDIC in PregnancySergio Alberto Sulub NavarretePas encore d'évaluation
- Chilblain MicroangiopathyDocument6 pagesChilblain MicroangiopathytitoPas encore d'évaluation
- Final Hand Book of Covid 19 AFMCDocument174 pagesFinal Hand Book of Covid 19 AFMCPadmapriya SrinivasanPas encore d'évaluation
- CT BTDocument20 pagesCT BTZainMalikPas encore d'évaluation
- 47 - Cruz Vs Court of AppealsDocument2 pages47 - Cruz Vs Court of AppealsJoannah GamboaPas encore d'évaluation
- Pregnancy and Hemostasis: From Physiology To Pathological StatesDocument7 pagesPregnancy and Hemostasis: From Physiology To Pathological StatesasclepiuspdfsPas encore d'évaluation
- Path NotesDocument111 pagesPath NotesNirav Patel100% (1)