Académique Documents
Professionnel Documents
Culture Documents
Antepartum
Transféré par
Alisha Bhimani0 évaluation0% ont trouvé ce document utile (0 vote)
88 vues3 pagesnursing maternity
Copyright
© © All Rights Reserved
Formats disponibles
DOCX, PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentnursing maternity
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme DOCX, PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
88 vues3 pagesAntepartum
Transféré par
Alisha Bhimaninursing maternity
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme DOCX, PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 3
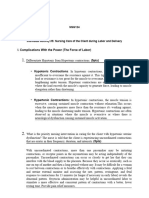
Antepartum Unit Clinical Questions
Define preterm labor. What are common signs?
Preterm labor is defined as uterine contractions and cervical changes that
occur between 20 and 37 weeks of gestation.
Increase, change or blood in vaginal discharge
Change in cervical dilation
Premature rupture of membranes
Regular uterine contractions with a frequency of every 10 minutes or
greater, lasting 1 hour or longer
3 medications used to treat preterm contractions are: magnesium sulfate,
terbutaline, and nifedipine.
What is a tocolytic?
Tocolytics are medications used to suppress premature labor. They are given
when delivery would result in premature birth.
Why might terbutaline cause an increased heart rate in mom and/or baby?
It is a beta-adrenergic agonist that relaxes uterine smooth muscle by
stimulating beta-2 receptors in the smooth muscle fibers to inhibit uterine
activity. Since it is a beta agonist, it works by stimulating the sympathetic
nervous system. Thus, increasing heart rate.
Why might a patient on nifedipine be at an increased risk for falls?
Nifedipine is a calcium channel blocker and it is used to decrease blood
pressure. It dilates arterioles/veins and a potential side effect is peripheral
edema (swelling in legs). Therefore, it may cause an increased risk of falls.
Magnesium Sulfate is often given to women in preterm labor. How does
this drug work to treat preterm labor?
It relaxes the smooth muscle of the uterus and thus inhibits uterine activity
by suppressing contractions.
When a patient is being given magnesium sulfate, the RN needs to
regularly assess these parameters: I&O, respiratory rate, lung sounds, and
DTRs (usually patellar reflexes). Explain why each should be regularly
assessed and what an abnormal finding might look like.
An order for magnesium sulfate typically begins with a loading dose of 4
grams IV to be given over 30 minutes. If magnesium sulfate is supplied in
a concentration of 1 gram in 25 ml IV fluids, what is the correct rate of
administration for the loading dose?
Why are antibiotics commonly given to women experiencing preterm
labor?
For glucocorticoids given IM to a woman likely to delivery preterm, what
are three benefits to the baby? What are 2 possible adverse effects for
mom?
Betamethasone is a glucocorticoid that is administered IM and requires a 24hr period to be effective. The therapeutic action is to enhance fetal lung
maturity and surfactant production.
Side effects for mom: pulmonary edema and hyperglycemia
For a patient with preterm premature rupture of membranes (pPROM), the
RN needs to assess for signs of chorioamnionitis. What is
chorioamnionitis?
Chorioamnionitis is the infection of the amniotic membranes.
What are 4 clinical (subjective or objective) indications that the patient
might have chorioamnionitis? What should the RN do if she suspects
chorio?
Maternal temperature
Increased maternal or FHR
Foul-smelling fluid or vaginal discharge
Abdominal tenderness
Know that chronic hypertension and preeclampsia are treated
differently and understand why.
What is the most common antihypertensive medication used to treat
chronic hypertension in pregnancy? Why would this medication be the
preferred antihypertensive in pregnancy?
A medication often used for patients who have preeclampsia is magnesium
sulfate. What complication is magnesium sulfate intended to prevent (for
someone with preeclampsia) and how does it do this?
What are some common symptoms (subjective) of preeclampsia?
Define preeclampsia, eclampsia and gestational hypertension and chronic
hypertension. How are they different?
Define hyperemesis gravidarum. How is it usually treated?
What are normal blood glucose values in an adultfasting and 2-hour
postprandial?
Vous aimerez peut-être aussi
- Lectures in FabellaDocument7 pagesLectures in FabellaLucille Dela Cruz EbuePas encore d'évaluation
- Group 1Document47 pagesGroup 1Karen AntoniettePas encore d'évaluation
- Module Obsterics DrugsDocument5 pagesModule Obsterics Drugsjanina mykaPas encore d'évaluation
- UNIT XIII Drugs Affecting The Reproductive SystemDocument90 pagesUNIT XIII Drugs Affecting The Reproductive Systemrichardmd2100% (1)
- DrugsDocument81 pagesDrugsrevathidadam55555100% (1)
- Drugs and It's Indication: Nursing ConsiderationsDocument4 pagesDrugs and It's Indication: Nursing ConsiderationsKenneth NovenoPas encore d'évaluation
- Maternity and Newborn MedicationsDocument38 pagesMaternity and Newborn MedicationsJaypee Fabros EdraPas encore d'évaluation
- Drugs I (Obgy)Document85 pagesDrugs I (Obgy)Aman Shaikh100% (2)
- Preterm Labor and Birth ACOGDocument3 pagesPreterm Labor and Birth ACOGPretty NoviannisaPas encore d'évaluation
- Hesi Hints MaternityDocument4 pagesHesi Hints MaternityThomas Stewart91% (11)
- What Is Ectopic Pregnancy?: Bautista, Shaina Mae A / BSN 2 - IDocument6 pagesWhat Is Ectopic Pregnancy?: Bautista, Shaina Mae A / BSN 2 - Ishenuh bPas encore d'évaluation
- What Is Ectopic Pregnancy?: Bautista, Shaina Mae A / BSN 2 - IDocument6 pagesWhat Is Ectopic Pregnancy?: Bautista, Shaina Mae A / BSN 2 - Ishenuh bPas encore d'évaluation
- What Is Ectopic Pregnancy?: Bautista, Shaina Mae A / BSN 2 - IDocument6 pagesWhat Is Ectopic Pregnancy?: Bautista, Shaina Mae A / BSN 2 - Ishenuh bPas encore d'évaluation
- Magnesium Sulfate Is Used To Treat PreDocument7 pagesMagnesium Sulfate Is Used To Treat Preporsche_41_poosh6244Pas encore d'évaluation
- Drug Use During Pregnancy and LactationDocument45 pagesDrug Use During Pregnancy and LactationSayli GorePas encore d'évaluation
- 15 DrugsDocument10 pages15 Drugscharles babasaPas encore d'évaluation
- Pharmacotherapeutics in ObstetricsDocument14 pagesPharmacotherapeutics in ObstetricsmercyPas encore d'évaluation
- Drug StudyDocument14 pagesDrug StudyAthena Irish LastimosaPas encore d'évaluation
- Acob, Jamil C. BSN2-ADocument5 pagesAcob, Jamil C. BSN2-AACOB, Jamil C.Pas encore d'évaluation
- Reproductive System PharmaDocument67 pagesReproductive System PharmaRoselyn VelascoPas encore d'évaluation
- Hyperemesis GravidarumDocument36 pagesHyperemesis GravidarumjanissPas encore d'évaluation
- Maternity Ati RemediationDocument2 pagesMaternity Ati Remediationcse100% (1)
- The Infant Should Always Be in A Rear-Facing Car Seat From Birth To 9.1 KGDocument7 pagesThe Infant Should Always Be in A Rear-Facing Car Seat From Birth To 9.1 KGSabhi Sandhu100% (1)
- Maternal CareDocument3 pagesMaternal CareMikko McDonie Veloria100% (1)
- Government College of Nursing Jodhpur (Raj.) : Procedure On-Cordiotocography Subject-Obstetrics & Gynecology Specialty-IDocument6 pagesGovernment College of Nursing Jodhpur (Raj.) : Procedure On-Cordiotocography Subject-Obstetrics & Gynecology Specialty-Ipriyanka100% (1)
- Health Education For Record BookDocument24 pagesHealth Education For Record BookRoselineTiggaPas encore d'évaluation
- Drugs Used in ObstetricsDocument21 pagesDrugs Used in Obstetricssuchismita panda100% (2)
- UntitledDocument14 pagesUntitledpunya anacaPas encore d'évaluation
- Midwifery AssingmentDocument10 pagesMidwifery AssingmentNena MinePas encore d'évaluation
- Thyroid Disease in PregnancyDocument36 pagesThyroid Disease in Pregnancypeni_dwiPas encore d'évaluation
- CTG Interpretation Made EasyDocument11 pagesCTG Interpretation Made EasySeneeth Peramuna100% (2)
- Anaesthetic of Choice During Pregnancy and LactationDocument5 pagesAnaesthetic of Choice During Pregnancy and LactationDegefu TadessePas encore d'évaluation
- Drugs in ObstetricsDocument36 pagesDrugs in ObstetricsPwani aquaponicsPas encore d'évaluation
- Chapter 40: Drugs Used in Obstetrics Test Bank: Multiple ChoiceDocument10 pagesChapter 40: Drugs Used in Obstetrics Test Bank: Multiple ChoiceNurse UtopiaPas encore d'évaluation
- Full Test BankDocument1 pageFull Test Bankjwjimmy20Pas encore d'évaluation
- NCM 102 Power and PsycheDocument13 pagesNCM 102 Power and Psychelarissedeleon100% (1)
- Preeclampsia Prep Questions-HaleyVestDocument5 pagesPreeclampsia Prep Questions-HaleyVestHaley Vest MustaficPas encore d'évaluation
- Common Drugs During PregnancyDocument16 pagesCommon Drugs During Pregnancymdsoukar2000Pas encore d'évaluation
- Questions in CasesDocument10 pagesQuestions in CasesRoselyn VelascoPas encore d'évaluation
- Drug Study On CARBOPROSTDocument4 pagesDrug Study On CARBOPROSTshadow gonzalez100% (1)
- Oxytocin Generic Name: Oxytocin Brand Name: Pitocin/ Syntocinon IndicationsDocument5 pagesOxytocin Generic Name: Oxytocin Brand Name: Pitocin/ Syntocinon IndicationsKish SuguitanPas encore d'évaluation
- OVARIAN STIMULANTS AND OXYTOCICS - PPTX - 22.04.2021 - Dr. SSDocument43 pagesOVARIAN STIMULANTS AND OXYTOCICS - PPTX - 22.04.2021 - Dr. SSRashitha NalarangaPas encore d'évaluation
- Simulation PaperworkDocument5 pagesSimulation Paperworkjustgraduate1408100% (1)
- Ob - ReportingDocument2 pagesOb - ReportingMAZON, DHANYCIA XYREENPas encore d'évaluation
- Clinical Obstetrics/Gynecology Review 2023: For USMLE Step 2 CK and COMLEX-USA Level 2D'EverandClinical Obstetrics/Gynecology Review 2023: For USMLE Step 2 CK and COMLEX-USA Level 2Évaluation : 4 sur 5 étoiles4/5 (1)
- Intrapartum AssesmentDocument71 pagesIntrapartum AssesmentHusain ChherawalaPas encore d'évaluation
- Seminar Drug.... Mohan.sDocument28 pagesSeminar Drug.... Mohan.smOHAN.S0% (1)
- LASMARIAS IndivAct5Document25 pagesLASMARIAS IndivAct5AngelicaJaneA.SuanPas encore d'évaluation
- Mother Baby Final Exam ReviewDocument14 pagesMother Baby Final Exam ReviewAngelina mendezPas encore d'évaluation
- 2022.TP (Ectopic Pregnancy) NOUNSDocument6 pages2022.TP (Ectopic Pregnancy) NOUNSWilson BenitezPas encore d'évaluation
- Parto y Nacimiento PreterminoDocument9 pagesParto y Nacimiento PreterminoIsabell PavónPas encore d'évaluation
- I Will Avoid Taking This Medication With Orange Juice.Document7 pagesI Will Avoid Taking This Medication With Orange Juice.jose godfreycPas encore d'évaluation
- AntepartumDocument128 pagesAntepartumIris Caberte100% (1)
- Oxytocin (Pitocin) : Slide 1Document16 pagesOxytocin (Pitocin) : Slide 1Kalesha JonesPas encore d'évaluation
- Childbirth: Student HandoutDocument13 pagesChildbirth: Student HandoutDiana AyónPas encore d'évaluation
- By: Marius Clifford R. Billedo BSN Ii AngelicaDocument4 pagesBy: Marius Clifford R. Billedo BSN Ii AngelicaMarius Clifford BilledoPas encore d'évaluation
- Case Study P.TDocument5 pagesCase Study P.TSharon WilliamsPas encore d'évaluation
- Methotrexate: Department of GynaecologyDocument8 pagesMethotrexate: Department of GynaecologyFakhrul IslamPas encore d'évaluation
- Therapeutic Strategies For The Prevention and Treatment ofDocument40 pagesTherapeutic Strategies For The Prevention and Treatment ofHILLARY DANDURUPas encore d'évaluation
- Winning against Prostatitis in the Elderly. Insider’s View of a Medical Worker.D'EverandWinning against Prostatitis in the Elderly. Insider’s View of a Medical Worker.Pas encore d'évaluation
- Nursing Mnemonics: Ob/Peds Labs PharmacologyDocument2 pagesNursing Mnemonics: Ob/Peds Labs PharmacologyAlisha BhimaniPas encore d'évaluation
- Total Body: Each Day, Choose 2-3 Items From The Schedule and Combine For A Complete Workout!Document1 pageTotal Body: Each Day, Choose 2-3 Items From The Schedule and Combine For A Complete Workout!Alisha BhimaniPas encore d'évaluation
- Nclex ChartsDocument39 pagesNclex ChartsDuvu99100% (6)
- Hemodynamics and Hypovolemic ShockDocument11 pagesHemodynamics and Hypovolemic ShockAlisha BhimaniPas encore d'évaluation
- LactationDocument2 pagesLactationAlisha BhimaniPas encore d'évaluation
- Maternity Care Plan 2 - Alisha BhimaniDocument9 pagesMaternity Care Plan 2 - Alisha BhimaniAlisha BhimaniPas encore d'évaluation
- Early Detection and Intervention of Autism Spectrum DisorderDocument7 pagesEarly Detection and Intervention of Autism Spectrum DisorderIgnacio WettlingPas encore d'évaluation
- DK Memory Activity BookDocument226 pagesDK Memory Activity Bookasif dxb100% (2)
- Drug and Alcohol Awareness ClassDocument71 pagesDrug and Alcohol Awareness ClassRinkish DalliahPas encore d'évaluation
- Apollo Case AnalysisDocument8 pagesApollo Case AnalysismuddanapPas encore d'évaluation
- Is Technology Isolating UsDocument2 pagesIs Technology Isolating UsJOANA LLANAPas encore d'évaluation
- HSE-OCP-017. Control of Hazardous SubstancesDocument6 pagesHSE-OCP-017. Control of Hazardous SubstancesibrahimPas encore d'évaluation
- Microbiome-Directed Therapies - Past, Present, and Future Prebiotics and Probiotics in Digestive HealthDocument12 pagesMicrobiome-Directed Therapies - Past, Present, and Future Prebiotics and Probiotics in Digestive HealthcrackintheshatPas encore d'évaluation
- SkiMaskDuets - Newsletter Email #6Document3 pagesSkiMaskDuets - Newsletter Email #6afonsovindo22Pas encore d'évaluation
- Whiteboard Communication SOPDocument24 pagesWhiteboard Communication SOPDewi Ratna SariPas encore d'évaluation
- Golf Exercise For BasicDocument3 pagesGolf Exercise For BasicDaniel AndreanPas encore d'évaluation
- Analysis of TheoryDocument4 pagesAnalysis of Theory19 - CELENDRO ADVINNPas encore d'évaluation
- The Real Secret - Psych-K: A New Approach To Changing Your LifeDocument5 pagesThe Real Secret - Psych-K: A New Approach To Changing Your Lifesjanko3325% (4)
- 2023 SS - Written Timetable 3 4 2023Document8 pages2023 SS - Written Timetable 3 4 2023asdsaPas encore d'évaluation
- Clinical Teams Mental Health ManualDocument18 pagesClinical Teams Mental Health Manualapi-609422028Pas encore d'évaluation
- Dream Job EssayDocument4 pagesDream Job Essaysirthana697547Pas encore d'évaluation
- Deep Venous Thrombosis Harrison'sDocument3 pagesDeep Venous Thrombosis Harrison'sMaria Agustina Sulistyo WulandariPas encore d'évaluation
- Pathology Integumentary SystemDocument4 pagesPathology Integumentary SystemMaui GamutanPas encore d'évaluation
- Growth of World PopulationDocument6 pagesGrowth of World Populationsally hakutangwiPas encore d'évaluation
- Contoh Analisis Jurnal Dengan PicoDocument2 pagesContoh Analisis Jurnal Dengan PicoRida OfficialPas encore d'évaluation
- The Top 100 Drugs Clinical Pharmacology and PracDocument4 pagesThe Top 100 Drugs Clinical Pharmacology and Pracyona0% (1)
- Assignment MeasurementDocument48 pagesAssignment MeasurementMuhammad TariqPas encore d'évaluation
- The British High Commission Is An Equal Opportunity EmployerDocument4 pagesThe British High Commission Is An Equal Opportunity EmployerFahim John BhattiPas encore d'évaluation
- University of Waterloo - 2016 CIW National Report - How Are Canadians Really Doing?Document96 pagesUniversity of Waterloo - 2016 CIW National Report - How Are Canadians Really Doing?RBeaudryCCLEPas encore d'évaluation
- Maria Leah J. Preglo, Sharina Caranzo Calvadores, Rose Ann B. Gayon, Mildred M. Mustausa, Aris Rex D. Espinas, and Irah Vone P. AlfecheDocument10 pagesMaria Leah J. Preglo, Sharina Caranzo Calvadores, Rose Ann B. Gayon, Mildred M. Mustausa, Aris Rex D. Espinas, and Irah Vone P. AlfechedawnPas encore d'évaluation
- Theory of Chronic SorrowDocument13 pagesTheory of Chronic Sorrowrusni rockabilly0% (1)
- Leg EdemaDocument13 pagesLeg Edemacamila perillaPas encore d'évaluation
- Health Safety Report 2015 PDFDocument51 pagesHealth Safety Report 2015 PDFPedro HenriquesPas encore d'évaluation
- Lecture 7 Dystocia in Farm AnimalsDocument39 pagesLecture 7 Dystocia in Farm AnimalsgnpobsPas encore d'évaluation
- Medical Admission Proforma: Hospital Name Patient DetailsDocument11 pagesMedical Admission Proforma: Hospital Name Patient DetailsAngelus129Pas encore d'évaluation
- Travelling of CraneDocument3 pagesTravelling of CraneDelta akathehuskyPas encore d'évaluation