Académique Documents
Professionnel Documents
Culture Documents
Acute Hepatic Necrosis and Ischemic Limb Necrosis 2012
Transféré par
Hania Asmarani RahmanitaCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Acute Hepatic Necrosis and Ischemic Limb Necrosis 2012
Transféré par
Hania Asmarani RahmanitaDroits d'auteur :
Formats disponibles
correspondence
Acute Hepatic Necrosis and Ischemic Limb Necrosis
To the Editor: Thrombosis can complicate the
coagulopathy of chronic liver disease, probably
because of decreased levels of the naturally occurring anticoagulants antithrombin and protein C, with resulting procoagulant imbalance.1
A disturbance of procoagulantanticoagulant balance is a fundamental concept in the pathogenesis of microvascular thrombosis that results in
ischemic limb necrosis despite palpable arterial
pulses. This latter condition has been reported in
patients with heparin-induced thrombocytopenia2 or adenocarcinoma3 two prothrombotic
disorders featuring greatly increased thrombin
generation in whom severe depletion of protein C (a vitamin Kdependent natural anticoagulant) develops during treatment with warfarin
(a vitamin K antagonist).2,3 In theory, acute liver
failure could similarly be prothrombotic,4 especially with rapid, profound depletion of protein C,
which has one of the shortest half-lives (9 hours)
of the hepatically synthesized factors.
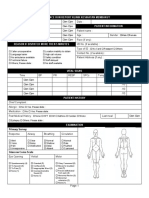
Acute ischemic hepatitis (peak alanine aminotransferase level, 2468 U per liter [reference range,
0 to 28]; peak total bilirubin level, 11.3 mg per
deciliter [193 mol per liter]) developed in a
61-year-old woman after cardiac arrest. Emergency coronary-artery bypass surgery restored
hemodynamic stability (with no ongoing requirements for vasopressors), but hepatic ischemia
persisted because of 99% atherosclerotic hepatic-artery stenosis that was detected on angiography. Ischemic limb necrosis (bilateral, acral, and
involving both the hands and feet) began on day
4, when the international normalized ratio increased to 5.1 (reference range, 0.9 to 1.3) and
the fibrinogen level decreased to 70 mg per deciliter (reference range, 160 to 420).
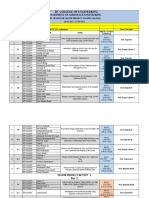
Figure 1 shows the patients clinical course
and platelet counts, the laboratory markers indicating a disturbance of the procoagulantanticoagulant balance, and the correlation between
factor activity levels and the respective factor
half-lives. We found an increase in levels of procoagulant markers (thrombinantithrombin complexes, fibrin monomers, and fibrin d-dimers) to
levels that were approximately 100 to 200 times
as high as normal values, with severe depletion
of protein C and antithrombin (nadir values of
1% and 20% of the normal values, respectively).
Thus, the ratio of procoagulant to anticoagulant
markers was more than 1000 to 10,000 times as
high as the normal ratio.
To examine the role of impaired hepatic synthesis of coagulation factors, we performed a
regression analysis of levels of coagulation factor activity (for factors II, V, VII, IX, X, XI, XII,
and XIII; prekallikrein; high-molecular-weight
kininogen; protein C; protein S; and antithrombin) versus their respective half-lives.5 We found
a highly significant positive association (r2=0.62,
P=0.001), indicating that differing factor halflives could help to explain the observed profile
of reduced levels of coagulation factors, particularly the very low levels of protein C activity.
Testing for heparin-dependent platelet-activating
antibodies was negative. We postulate that a disturbance of procoagulantanticoagulant balance
Figure 1 (following page). Findings in a Patient with
Acute Hepatic Necrosis and Ischemic Limb Necrosis.
Panel A shows the patients clinical course and platelet
counts. Limb necrosis began 4 days after cardiac arrest
and progressed despite heparin therapy. The expanded
figure of days 4.00 to 6.00 shows a disturbance of the
procoagulantanticoagulant balance. Levels of procoagulant markers (fibrin d-dimer, fibrin monomer, and
thrombinantithrombin complexes) were 100 to 200
times as high as the upper limit of the normal range
(dashed line), whereas the nadir levels of the natural
anticoagulants, protein C and antithrombin, were only
1% (0.01 U per milliliter [reference range, 0.70 to 1.80])
and 20% (0.20 U per milliliter [reference range, 0.77 to
1.25]) of the normal values (at day 4.75), respectively,
with subsequent increases in protein C after transfusion of frozen plasma and protein C concentrate. Panel
B shows levels of coagulation factor activity (based on
mean values of two plasma samples obtained approximately 4.75 days after admission and before plasma
administration) versus factor half-lives. The dashed
line indicates the least-squares regression line fitted
through the data points shown. Factor VIII coagulant
levels were approximately four times as high as normal
levels (not shown). These findings are consistent with
the role of factor VIII as an acute-phase reactant.
n engl j med 367;9 nejm.org august 30, 2012
The New England Journal of Medicine
Downloaded from nejm.org on March 4, 2014. For personal use only. No other uses without permission.
Copyright 2012 Massachusetts Medical Society. All rights reserved.
879
The
n e w e ng l a n d j o u r na l
of
m e dic i n e
A
Norepinephrine
and dopamine
300,000
Platelet Count/mm3
Heparin
Admission for acute myocardial infarction
Cardiac arrest after heart catheterization
Emergency cardiac surgery
Platelet transfusions
Death
200,000
Continuous renal-replacement therapy
Ischemic limb necrosis
100,000
Heparin
103
Value Relative to Upper Limit
of Normal Range (log10 scale)
102
Procoagulant
Thrombinantithrombin
complex
Fibrin monomer
Fibrin D-dimer
101
Protein C
concentrate
Frozen plasma (2 units each)
Normal
100
101
Anticoagulant
Antithrombin
Protein C
102
4.00
4.25
4.50
4.75
5.00
5.25
5.50
5.75
6.00
Days after Admission
Factor Activity Level
(U/ml)
1.0
0.8
Factor XII
Prekallikrein
Factor IX
Factor XIII
Factor XI
0.4
Factor VII
0.2
0.0
High-molecular-weight
kininogen
Protein S
0.6
Factor II
Protein C
Factor V
0
20
40
r2 =0.62
Antithrombin
Factor X
60
80
100
120
140
160
Factor Half-Life (hr)
arising from the combination of greatly in- tors (protein C and antithrombin) can explain
creased thrombin generation with impaired he- ischemic limb necrosis despite palpable pulses
patic synthesis of key natural anticoagulant fac- in patients with acute hepatic necrosis.
880
n engl j med 367;9 nejm.org august 30, 2012
The New England Journal of Medicine
Downloaded from nejm.org on March 4, 2014. For personal use only. No other uses without permission.
Copyright 2012 Massachusetts Medical Society. All rights reserved.
notices
Deborah M. Siegal, M.D.
corrections
McMaster University
Hamilton, ON, Canada
Richard J. Cook, Ph.D.
Nighttime Intensivist Staffing and Mortality among Critically
Ill Patients (May 31, 2012;366:2093-101). In Table 3 (page
2099), the P value in the last row of the table should have been
0.053, rather than <0.001. The article is correct at NEJM.org.
University of Waterloo
Waterloo, ON, Canada
Theodore E. Warkentin, M.D.
McMaster University
Hamilton, ON, Canada
twarken@mcmaster.ca
Supported by a grant (T6950) from the Heart and Stroke Foundation of Ontario.
Disclosure forms provided by the authors are available with
the full text of this letter at NEJM.org.
1. Tripodi A, Mannucci PM. The coagulopathy of chronic liver
disease. N Engl J Med 2011;365:147-56.
Transcatheter Aortic-Valve Replacement for Inoperable Severe
Aortic Stenosis (May 3, 2012;366:1696-704). In Figure 2 (page
1700), the y axis should have been labeled Mortality (%),
rather than Survival (%). The article is correct at NEJM.org.
Pregnancy in a Woman with a Leptin-Receptor Mutation
(March 15, 2012;366:1064-5). In the list of authors (page 1065),
the second authors surname should have been Dommergues,
rather than Dommergue. The article is correct at NEJM.org.
2. Warkentin TE, Elavathil LJ, Hayward CPM, Johnston MA,
Russell JI, Kelton JG. The pathogenesis of venous limb gangrene
associated with heparin-induced thrombocytopenia. Ann Intern
Med 1997;127:804-12.
3. Warkentin TE. Venous limb gangrene during warfarin treatment of cancer-associated deep venous thrombosis. Ann Intern
Med 2001;135:589-93.
4. Idem. Heparin-induced thrombocytopenia in critically ill patients. Crit Care Clin 2011;27:805-23.
5. Harmening DM, Escobar CE, McGlasson DL. Introduction to
hemostasis. In: Harmening DM, ed. Clinical hematology and
fundamentals of hemostasis. 5th ed. Philadelphia: F.A. Davis,
2009:543-76.
DOI: 10.1056/NEJMc1207074
Correspondence Copyright 2012 Massachusetts Medical Society.
instructions for letters to the editor
Letters to the Editor are considered for publication, subject
to editing and abridgment, provided they do not contain
material that has been submitted or published elsewhere.
Please note the following:
Letters in reference to a Journal article must not exceed 175
words (excluding references) and must be received within
3 weeks after publication of the article.
Letters not related to a Journal article must not exceed 400
words.
A letter can have no more than five references and one figure
or table.
A letter can be signed by no more than three authors.
Financial associations or other possible conflicts of interest
must be disclosed. Disclosures will be published with the
letters. (For authors of Journal articles who are responding
to letters, we will only publish new relevant relationships
that have developed since publication of the article.)
Include your full mailing address, telephone number, fax
number, and e-mail address with your letter.
All letters must be submitted at authors.NEJM.org.
Letters that do not adhere to these instructions will not be
considered. We will notify you when we have made a decision
about possible publication. Letters regarding a recent Journal
article may be shared with the authors of that article. We are
unable to provide prepublication proofs. Submission of a
letter constitutes permission for the Massachusetts Medical
Society, its licensees, and its assignees to use it in the Journals
various print and electronic publications and in collections,
revisions, and any other form or medium.
notices
Notices submitted for publication should contain a mailing
address and telephone number of a contact person or department. We regret that we are unable to publish all notices
received. Notices also appear on the Journals website
(NEJM.org/medical-conference). The listings can be viewed
in their entirety or filtered by specialty, location, or month.
Electronic Health and Medicine: Advances
and Challenges
The seminar will be held in Warsaw, Poland, on Sept. 27. It
is presented by the Polish Academy of Sciences.
Contact Ms. R. Kuskowska, Polish Academy of Sciences,
PKiN, 00901 Warsaw, Poland; or call 4822 6566371; or fax 4822
6203374; or e-mail renata.kuskowska@pan.pl; or see http://
www.english.pan.pl.
Mayo Medical Laboratories
The following meeting will be held in Rochester, MN:
Phlebotomy 2012: Why We Do What We Do Creating Excellence in Patient Care (Oct. 4 and 5).
Contact Mayo Medical Laboratories, 3050 Superior Dr. NW,
Rochester, MN 55901; or call (800) 533-1710 or (507) 538-4510;
or see http://www.mayomedicallaboratories.com/education.
Harvard School of Public Health
The following courses will be offered in Boston: Forces of
Change: New Strategies for the Evolving Health Care Marketplace (Sept. 1014) and Leadership Strategies for Evolving
Health Care Executives (Oct. 28Nov. 2).
Contact Peter J. Bretton, Center for Continuing Professional
Education, Harvard School of Public Health, 677 Huntington
Ave., Boston, MA 02115; or call (617) 384-8965; or fax (617)
384-8690; or e-mail pbretton@hsph.harvard.edu; or see https://
ccpe.sph.harvard.edu.
Laser & Aesthetic Skin Therapy: Whats the Truth?
The course will be offered in Boston, Oct. 26 and 27. It is
jointly sponsored by Harvard Medical School Department of
Continuing Education, Massachusetts General Hospital Department of Dermatology, and the Wellman Center for Photomedicine.
Contact Harvard Medical School Department of Continuing
Education, P.O. Box 417476, Boston, MA 02241-7476; or call
(617) 384-8600; or e-mail hms-cme@hms.harvard.edu; or see
http://www.cme.hms.harvard.edu/courses/LASER.
n engl j med 367;9 nejm.org august 30, 2012
The New England Journal of Medicine
Downloaded from nejm.org on March 4, 2014. For personal use only. No other uses without permission.
Copyright 2012 Massachusetts Medical Society. All rights reserved.
881
Vous aimerez peut-être aussi
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Hunger Scale: Healthyfutures - Nhs.uk/llbDocument3 pagesThe Hunger Scale: Healthyfutures - Nhs.uk/llbHania Asmarani RahmanitaPas encore d'évaluation
- Prontosan®: What Is Prontosan® Wound Irrigation Solution and Gel?Document6 pagesProntosan®: What Is Prontosan® Wound Irrigation Solution and Gel?Hania Asmarani RahmanitaPas encore d'évaluation
- Tocolytic AgentDocument13 pagesTocolytic AgentHania Asmarani RahmanitaPas encore d'évaluation
- World Breastfeeding Week 2007: An Early Start On Breast Milk Saves Infants' LivesDocument2 pagesWorld Breastfeeding Week 2007: An Early Start On Breast Milk Saves Infants' LivesHania Asmarani RahmanitaPas encore d'évaluation
- Panduan Acara - Jambore Nasional Sastra 2017.v2Document30 pagesPanduan Acara - Jambore Nasional Sastra 2017.v2Hania Asmarani RahmanitaPas encore d'évaluation
- Research ArticleDocument5 pagesResearch ArticleHania Asmarani RahmanitaPas encore d'évaluation
- Perspectives in Diabetes: Postprandial Hyperglycemia and Diabetes ComplicationsDocument7 pagesPerspectives in Diabetes: Postprandial Hyperglycemia and Diabetes ComplicationsHania Asmarani RahmanitaPas encore d'évaluation
- Ped AppBDocument47 pagesPed AppBHania Asmarani RahmanitaPas encore d'évaluation
- DMSOTT 4790 Inhibition of Dipeptidyl Peptidase 4 The Mechanisms of Acti 061109Document8 pagesDMSOTT 4790 Inhibition of Dipeptidyl Peptidase 4 The Mechanisms of Acti 061109Hania Asmarani RahmanitaPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Jesus Prayer-JoinerDocument13 pagesJesus Prayer-Joinersleepknot_maggotPas encore d'évaluation
- De Thi Hoc Ki 1 Mon Tieng Anh Lop 5 Co File NgheDocument10 pagesDe Thi Hoc Ki 1 Mon Tieng Anh Lop 5 Co File Nghetuyen truongPas encore d'évaluation
- Homework 1 W13 SolutionDocument5 pagesHomework 1 W13 SolutionSuzuhara EmiriPas encore d'évaluation
- Huawei R4815N1 DatasheetDocument2 pagesHuawei R4815N1 DatasheetBysPas encore d'évaluation
- Analizador de Combustion Kigaz 310 Manual EngDocument60 pagesAnalizador de Combustion Kigaz 310 Manual EngJully Milagros Rodriguez LaichePas encore d'évaluation
- User Manual For Speed Control of BLDC Motor Using DspicDocument12 pagesUser Manual For Speed Control of BLDC Motor Using DspicTrung TrựcPas encore d'évaluation
- V737 OverheadDocument50 pagesV737 OverheadnewahPas encore d'évaluation
- AlpaGasus: How To Train LLMs With Less Data and More AccuracyDocument6 pagesAlpaGasus: How To Train LLMs With Less Data and More AccuracyMy SocialPas encore d'évaluation
- Sba 2Document29 pagesSba 2api-377332228Pas encore d'évaluation
- Presentation 11Document14 pagesPresentation 11stellabrown535Pas encore d'évaluation
- Dtu Placement BrouchureDocument25 pagesDtu Placement BrouchureAbhishek KumarPas encore d'évaluation
- Chronic Kidney DiseaseDocument15 pagesChronic Kidney Diseaseapi-270623039Pas encore d'évaluation
- Iec TR 61010-3-020-1999Document76 pagesIec TR 61010-3-020-1999Vasko MandilPas encore d'évaluation
- Functions in C++Document23 pagesFunctions in C++Abhishek ModiPas encore d'évaluation
- Grade 7 ExamDocument3 pagesGrade 7 ExamMikko GomezPas encore d'évaluation
- Obesity - The Health Time Bomb: ©LTPHN 2008Document36 pagesObesity - The Health Time Bomb: ©LTPHN 2008EVA PUTRANTO100% (2)
- Parliament of India: Rajya SabhaDocument64 pagesParliament of India: Rajya SabhaSivapothuraju KonathalaPas encore d'évaluation
- Review1 ScheduleDocument3 pagesReview1 Schedulejayasuryam.ae18Pas encore d'évaluation
- Syllabus DresserDocument2 pagesSyllabus DresserVikash Aggarwal50% (2)
- Making Effective Powerpoint Presentations: October 2014Document18 pagesMaking Effective Powerpoint Presentations: October 2014Mariam TchkoidzePas encore d'évaluation
- Excon2019 ShowPreview02122019 PDFDocument492 pagesExcon2019 ShowPreview02122019 PDFSanjay KherPas encore d'évaluation
- Unit 7: Anthropology: Q2e Listening & Speaking 4: Audio ScriptDocument6 pagesUnit 7: Anthropology: Q2e Listening & Speaking 4: Audio ScriptĐại học Bạc Liêu Truyền thông100% (1)
- German Atv-Dvwk Rules and StandardsDocument25 pagesGerman Atv-Dvwk Rules and StandardsMehmet Emre Bastopcu100% (1)
- Borang Ambulans CallDocument2 pagesBorang Ambulans Callleo89azman100% (1)
- Working Capital in YamahaDocument64 pagesWorking Capital in YamahaRenu Jindal50% (2)
- CH 1 - Democracy and American PoliticsDocument9 pagesCH 1 - Democracy and American PoliticsAndrew Philip ClarkPas encore d'évaluation
- WEB DESIGN WITH AUSTINE-converted-1Document9 pagesWEB DESIGN WITH AUSTINE-converted-1JayjayPas encore d'évaluation
- Lithuania DalinaDocument16 pagesLithuania DalinaStunt BackPas encore d'évaluation
- Strucure Design and Multi - Objective Optimization of A Novel NPR Bumber SystemDocument19 pagesStrucure Design and Multi - Objective Optimization of A Novel NPR Bumber System施元Pas encore d'évaluation
- LM74680 Fasson® Fastrans NG Synthetic PE (ST) / S-2050/ CK40Document2 pagesLM74680 Fasson® Fastrans NG Synthetic PE (ST) / S-2050/ CK40Nishant JhaPas encore d'évaluation