Académique Documents
Professionnel Documents
Culture Documents
2nd Sem - Hema1 - An Overview of Clinical Laboratory Hematology
Transféré par
Aisle Malibiran PalerTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
2nd Sem - Hema1 - An Overview of Clinical Laboratory Hematology
Transféré par
Aisle Malibiran PalerDroits d'auteur :
Formats disponibles
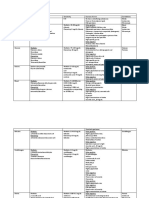
Chapter 1: An Overview of Clinical Laboratory Hematology
Blood- transports oxygen from lungs to tissue
clears tissues of carbon dioxide
transports glucose, proteins, and fats
Moves wastes to the liver and kidneys.
Plasma
The liquid portion of the blood among many other
components
coagulation enzymes that protect vessels from trauma and
maintain the circulation
Transports and nourishes blood cells.
Three families of blood cells
1. red blood cells (RBCs) or erythrocytes
2. white blood cells (WBCs) leukocytes
3. platelets or thrombocytes
Hematology 1
Buffy Coat
light-colored layer between the RBCs and plasma
Contains WBCs and platelets.
Three Numerical Results
1. RBC count
2. Hemoglobin
3. Hematocrit
To compute the RBC indices
1. mean cell volume (MCV)
2. mean cell hemoglobin (MCH)
3. mean cell hemoglobin concentration
Mean Cell Volume (MCV)
measure of volume
reflects RBC diameter on a Wright-stained blood film
Mean Cell Hemoglobin Concentration (MCHC)
reflects RBC staining intensity or degree of pallor
Mean Cell Hemoglobin (MCH)
expresses the mass of hemoglobin and closely reflects the
MCHC
RBC distribution width (RDW)
expresses the degree of variation in RBC volume
Extreme RBC volume variability is visible on the Wrightstained blood film as variation in diameter and is called
anisocytosis.
based on the standard deviation of RBC volume
Reported by automated cell counters but cannot be provided
using manual RBC measurements.
Hematology- the study of blood cells
Wrights Romanowsky- type stain (polychromatic, a mixture of acidic
and basic dyes) remains the heart of blood cell identification
Red Blood Cells
Red Blood Cells (RBC)
a nucleate biconcave cells filled with a reddish protein,
hemoglobin (Hb, HGB) which trans- ports oxygen and
carbon dioxide
pink to red ; 6 to 8 m
Anemia loss of oxygen-carrying capacity; reduced RBC count
Polycythemia increased RBC count reflecting increased body
RBC mass; leads to hyperviscosity
To count RBCs, laboratory scientists carefully pipetted a tiny
aliquot of whole blood and mixed it with 0.85% (normal)
saline.
A 1 : 200 dilution was typical for RBC counts, and a glass
pipette designed to provide this dilution
Thoma pipette used routinely until the advent of automation
The diluted blood was transferred to a counting
chamber or
Report the RBC count in cells per microliter (mcL),
milliliter (mL, also called cubic centimeter, or cc), or liter
(L).
Coulter Counters first electronic counter by Joseph and
Wallace Coulter of Chicago, Illinois, was used so widely that
today automated cell counters
Hemoglobin measurement relies on a weak solution of
potassium cyanide and potassium ferricyanide, called
Drabkin reagent.
Hemoglobin
is
converted
to
stable
cyanmethemoglobin(hemiglobincyanide), and the solution is
placed in a photometer at 540 nm wavelength.
Some automated hematology profiling instruments use a
formulation
of
the
ionic
surfactant
(detergent) sodium
dodecyl
sulfate to reduce
environmental cyanide.
Hematocrit
ratio of the volume of RBCs to the volume of whole blood
determined
by
transferring
blood
to
a
graduated plastic tube, centrifuging, measuring the column
of
RBCs, and dividing by the total length of RBCs plus
plasma
The normal ratio approaches 50%
Also called packed cell volume (PCV), the packed cells
referring to RBCs.
RBC count, hemoglobin, hematocrit, indices, and RBC
morphology are used to detect, diagnose, assess the severity
of, and monitor the treatment of anemia, polycythemia, and
numerous systemic conditions that affect RBCs
Reticulocytes
Polychromatophilic erythrocytes- in the Wright-stained film,
1% to 2% of RBCs exceed the 6- to 8-m ; slightly blue-gray
newly released from the RBC production site, the bone
marrow
closely observed because they indicate bone marrow
regeneration during blood loss and certain anemias
Methylene blue dyes- called nucleic acid stains or vital stain
used to differentiate and count these young RBCs
Vital stains -dyes absorbed by live cells. Young RBCs
contain ribonucleic acid (RNA) and are called reticulocytes
when the RNA is highlighted using vital stains.
White Blood Cells
White Blood Cells or Leukocytes (WBC)
are not really blood cells
they are a loosely related grouping of cell families
dedicated to protecting their host from infection and injury
WBCs hitch a ride in the blood from their source,
usually bone marrow or lymphoid tissue, to their tissue
destination.
They are so named because they are nearly colorless in
an unstained cell suspension
WBCs may be counted visually using a microscope, hemacytometer, and a Thoma pipette
The technique is the same as RBC counting, but the typical
dilution is 1: 20, and the diluent is composed of dilute acetic
acid in normal saline.
Chronic leukemia
an extreme increase in the WBC count imparts a milky
appearance to the blood
Chapter 1: An Overview of Clinical Laboratory Hematology
Hematology 1
**Acid causes RBCs to lyse or rupture
Leukopenia
decreased WBC count (fewer than 4500/mcL)
Leukocytosis
increased WBC count (more than 11,500/ mcL)
Types of White Blood Cells
1. Polymorphonuclear neutrophils (PMNs, or segmented
neutrophils or Segs
phagocytic cells whose sole purpose is to engulf and
destroy bacteria that have been earlier labeled as
harmful by the immune system.
Neutrophilia
increase in segs; signals bacterial infection.
Neutropenia
decrease in segs; caused by long-term drug administration
or a viral infection.
2.
3.
-
Band neutrophils (bands)
part of the seg family
less differentiated or less mature than segs
increase also signals bacterial infection and is customarily
called a left shift
The cytoplasm
of segmented neutrophils and bands
contains submicroscopic, pink-staining granules filled with
bactericidal secretions.
Eosinophils (Eos)
bright orange, regular cytoplasmic granules filled with
antihistamine.
Eosinophilia
elevated eosinophil count is called and
response to allergy or parasitic infection.
4.
-
signals
most common form of childhood leukemia
6.
-
Monocytes (monos)
immature macrophage passing through the blood from its
point of origin, usually the bone marrow, to a targeted
tissue location
Macrophages
Most abundant cell in the body, more abundant than RBCs
or skin cells, although they are a minor component of the
blood film differential count
Some are motile and some immobilized.
Their task is to identify and phagocytose (engulf) foreign
particles and assist the lymphocytes in mounting an
immune response through the assembly and presentation
of immunogenic epitopes
Monocytosis
An increase in the number of monocytes may signal a
hematologic disease, such as leukemia
Platelets
Basophils (basos)
dark purple, irregular cytoplasmic granules that obscure
the nucleus
Basophilia
elevated basophil count
signals a hematologic disease, such as leukemia.
Platelets or thrombocytes
Are true blood cells that maintain blood vessel integrity
by instigating vessel wall repairs
Rapidly adhere to the surfaces of damaged blood vessels,
form aggregates with neighboring platelets to plug the
vessels, and secrete proteins and small molecules that
trigger thrombosis, or clot formation. Platelets are the cells
that control hemostasis,
Hemostasis
Series of cellular and plasma-based mechanisms that seals
wounds, repairs vessel walls, and maintains vascular
patency.
Thrombocytosis
Elevated platelet counts; signal inflammation or trauma but
carry small intrinsic significance.
Essential thrombocythemia
rare malignant condition characterized by extremely high
platelet counts and uncontrolled platelet production.
Thrombocytopenia
low platelet count
a common consequence of drug treatment and may be
life-threatening
accounts
for
the
majority of hemorrhage-related
emergency department visits.
** Segs, bands, eosinophils, and
basophils- collectively called
granulocytes because of their prominent cytoplasmic granules
Leukemia
is uncontrolled proliferation of WBCs.
may be chronic,
for example chronic myelogenous
(granulocytic) leukemia, or acute,
such as
acute
myeloblastic leukemia
5.
-
Lymphocytes (lymphs)
Complex system of cells that provide for host immunity
recognize
foreign
antigens
and mount antibody
(humoral) and cell-mediated antagonistic responses
Lymphocytosis
Increase in the lymphocyte count; associated with viral
infections.
Lymphopenia or lymphocytopenia
abnormally low lymphocyte count is and is associated with
long-term drug therapy or immunodefi- ciency
Chronic lymphocytic leukemia
prevalent in people older than 70 years
Acute lymphoblastic leukemia
Complete Blood Count
Complete Blood Count
The scientist is responsible for the integrity of the specimen
and ensures that it is free of clots, hemolysis, and
inappropriate anticoagulant- to-specimen ratios known as
short draws.
When one of the results from the profiling instru- ment is
abnormal, the instrument provides an indication of this,
sometimes called a flag. In this case, the scientist performs
a reflex blood film examination
Blood Film Examination
Chapter 1: An Overview of Clinical Laboratory Hematology
Blood Film Examination
wedge-prep blood film on a glass microscope slide,
allows it to dry, and fixes and stains it using Wright or
Wright-Giemsa stain
Endothelial cells
Important in maintaining normal blood flow, in snaring
platelets during times of injury, and in enabling WBCs to
escape from the vessel to the surrounding tissue when
called upon.
Plasma coagulation
is one component of hemostasis; another is platelets
Coagulation system
complex sequence of plasma proteins, some enzymes,
and some enzyme cofactors to produce clot formation
after blood vessel injury.
Erythroid series
precursors to RBCs
Hematology 1
Myeloid series cells
mature to form bands and segmented neu- trophils,
eosinophils, and basophils
Megakaryocytes
produce platelets
Osmotic fragility test
Uses graduated concentrations of saline
solutions to
detect spherocytes, RBCs with proportionally reduced
surface membrane area, in hereditary spherocytic or warm
autoim- mune hemolytic anemia
Glucose-6-phosphate dehydrogenase assay tests
For an inherited RBC enzyme deficiency causing severe
episodic hemolytic anemia
Hb electrophoresis
used to detect and diagnose sickle cell anemia and
other inherited qualitative hemoglobin abnormalities and
thalassemias
Vous aimerez peut-être aussi
- Hematology 1Document5 pagesHematology 1jaish8904100% (1)
- (Hema) 1.1 Intro To Hema (Perez) - PANDADocument6 pages(Hema) 1.1 Intro To Hema (Perez) - PANDATony DawaPas encore d'évaluation
- Immunology and Serology TestsDocument2 pagesImmunology and Serology TestsPearlregine Cianne MirandaPas encore d'évaluation
- MTAP ISBB - Sir JJ (Merged)Document9 pagesMTAP ISBB - Sir JJ (Merged)Nathan DrakePas encore d'évaluation
- Histopath ReviewerDocument43 pagesHistopath ReviewerMika De VeraPas encore d'évaluation
- University of The Immaculate Conception: ProteinDocument13 pagesUniversity of The Immaculate Conception: ProteinDams ZainalPas encore d'évaluation
- Revalida Reviewer CC - Microbio.cmDocument12 pagesRevalida Reviewer CC - Microbio.cmAsherLamataoObeja0% (1)
- Clinical Chemistry RTP 1Document9 pagesClinical Chemistry RTP 1Reham Que100% (1)
- Clinical Chemistry Notes With BlanksDocument34 pagesClinical Chemistry Notes With Blanksepson printerPas encore d'évaluation
- Wintrobe Test PDFDocument9 pagesWintrobe Test PDFMaria Chacón CarbajalPas encore d'évaluation
- Hematology ReviewerDocument10 pagesHematology ReviewerAldren BeliberPas encore d'évaluation
- Recalls of Compilation of Clinical ChemistryDocument10 pagesRecalls of Compilation of Clinical ChemistryDeniel BusiPas encore d'évaluation
- HistopathDocument23 pagesHistopathElla SalesPas encore d'évaluation
- Clinical Chemistry (Lecture) - PrelimsDocument12 pagesClinical Chemistry (Lecture) - Prelimsisprikitik3100% (1)
- Hematology2 - Laboratory TestsDocument3 pagesHematology2 - Laboratory Testskthmnts100% (1)
- MTAP - HematologyDocument13 pagesMTAP - HematologyKassandra CordetaPas encore d'évaluation
- Clinical Chemistry KeyNotes For Board ExaminationDocument12 pagesClinical Chemistry KeyNotes For Board ExaminationPrincess Alen Aguilar100% (2)
- Histopath Guide QuestionsDocument2 pagesHistopath Guide QuestionsMartin ClydePas encore d'évaluation
- Clinical Microscopy ExamDocument3 pagesClinical Microscopy ExamKarla GiorlaPas encore d'évaluation
- Recalls Ascp (Exam) - 2021 - 240103 - 185452Document16 pagesRecalls Ascp (Exam) - 2021 - 240103 - 185452gaber 230100% (2)
- Hematology NotesDocument17 pagesHematology NotesEly Sibayan100% (2)
- Klubsybear Additional Recalls: Hematology A.karyolysisDocument2 pagesKlubsybear Additional Recalls: Hematology A.karyolysisMartin ClydePas encore d'évaluation
- Rodak Questions CompilationDocument40 pagesRodak Questions CompilationGertrudeshane IletoPas encore d'évaluation
- Clinical Chemistry Review NotesDocument54 pagesClinical Chemistry Review NotesALEONA AMON ARANTEPas encore d'évaluation
- CHEM 2 CH 29 Review QuestionsDocument2 pagesCHEM 2 CH 29 Review QuestionsthrowawyPas encore d'évaluation
- Disorders of Iron Kinetics and Heme MetabolismDocument12 pagesDisorders of Iron Kinetics and Heme MetabolismJoanne JardinPas encore d'évaluation
- Part3 Clinical ChemistryDocument4 pagesPart3 Clinical ChemistryGodofredo Hermosura100% (1)
- Clin ChemDocument7 pagesClin ChemkthmntsPas encore d'évaluation
- Histologic TechniquesDocument12 pagesHistologic TechniquesCatherine Merilleno100% (1)
- Hematology Review NotesDocument29 pagesHematology Review NotesCattrainuh100% (2)
- Recalls Sept 2018 PDFDocument12 pagesRecalls Sept 2018 PDFRomina LacsonPas encore d'évaluation
- Clinical ChemistryDocument26 pagesClinical Chemistryazoooz502Pas encore d'évaluation
- Summary of Reagent Strip TestsDocument8 pagesSummary of Reagent Strip TestsDarla YsavelPas encore d'évaluation
- Group 6 - Immunohematology - Blood BankingDocument8 pagesGroup 6 - Immunohematology - Blood Bankingjulo_05Pas encore d'évaluation
- Clinical Chemistry NotesDocument24 pagesClinical Chemistry Notesclower112100% (3)
- Immunology Serology ReviewDocument211 pagesImmunology Serology ReviewRachel Marie M. Gania100% (1)
- Isbb 2019 RecallsDocument159 pagesIsbb 2019 RecallsInah Mae Coleen CapuyanPas encore d'évaluation
- Clinical Chemistry Notes Without Blanks LegitDocument43 pagesClinical Chemistry Notes Without Blanks LegitPearl Isabelle SudarioPas encore d'évaluation
- Histopathologic Techniques PretestDocument38 pagesHistopathologic Techniques Pretestedwineiou93% (15)
- MTLBDocument3 pagesMTLBDanPas encore d'évaluation
- Immunohematology/ Blood BankingDocument2 pagesImmunohematology/ Blood BankingSophia AmpatuanPas encore d'évaluation
- Acts Reinforcement Mar2020 PDFDocument8 pagesActs Reinforcement Mar2020 PDFErika Kate MedadoPas encore d'évaluation
- Chapter 4 Physical Examination PDFDocument4 pagesChapter 4 Physical Examination PDFJulie Anne Soro ValdezPas encore d'évaluation
- Must To Know MTLDocument15 pagesMust To Know MTLMae MacalandaPas encore d'évaluation
- MUST To KNOW in Blood Banking 1Document19 pagesMUST To KNOW in Blood Banking 1Aya Virtucio100% (1)
- Clin Chem Lec Notes 1Document6 pagesClin Chem Lec Notes 1Jamie BartolomePas encore d'évaluation
- Chapter 13 Rodaks HematologyDocument10 pagesChapter 13 Rodaks HematologyRALPH JAN T. RIOPas encore d'évaluation
- Hematology Ii Lectures Introduction To HemostasisDocument28 pagesHematology Ii Lectures Introduction To HemostasisJoshua Trinidad100% (1)
- Ilovepdf MergedDocument56 pagesIlovepdf MergedAngela ReyesPas encore d'évaluation
- Chapter Blood: RBC Platelet HemostasisDocument89 pagesChapter Blood: RBC Platelet Hemostasisapi-19916399100% (1)
- Agglutination, Complement, Neutralization, and Inhibition: Methods in Immunology and Immunochemistry, Vol. 4D'EverandAgglutination, Complement, Neutralization, and Inhibition: Methods in Immunology and Immunochemistry, Vol. 4Pas encore d'évaluation
- MedtechDocument7 pagesMedtechLyudmyla GillegoPas encore d'évaluation
- Hema Notes (Lec)Document50 pagesHema Notes (Lec)Anonymous 0zrCNQPas encore d'évaluation
- ISBBhandoutDocument55 pagesISBBhandoutRed GillianPas encore d'évaluation
- Long Quiz Hema Lec 2021 MergedDocument49 pagesLong Quiz Hema Lec 2021 MergedAngela ReyesPas encore d'évaluation
- CM Review Notes 2Document22 pagesCM Review Notes 2USMAN JuhaminPas encore d'évaluation
- Tietz's Applied Laboratory MedicineD'EverandTietz's Applied Laboratory MedicineMitchell G. ScottÉvaluation : 3 sur 5 étoiles3/5 (1)
- Safe Blood: Purifying the Nations Blood Supply in the Age of AD'EverandSafe Blood: Purifying the Nations Blood Supply in the Age of APas encore d'évaluation
- 68th AACC Annual Scientific Meeting Abstract eBookD'Everand68th AACC Annual Scientific Meeting Abstract eBookPas encore d'évaluation
- Genpath Midterms1Document3 pagesGenpath Midterms1Aisle Malibiran PalerPas encore d'évaluation
- Bacte Chapt. 16Document4 pagesBacte Chapt. 16Aisle Malibiran PalerPas encore d'évaluation
- 2nd Sem - ImmunoSero - Introduction and Natural ImmunityDocument5 pages2nd Sem - ImmunoSero - Introduction and Natural ImmunityAisle Malibiran PalerPas encore d'évaluation
- (MT-RES) Peer Evaluation (New)Document1 page(MT-RES) Peer Evaluation (New)Aisle Malibiran PalerPas encore d'évaluation
- (MID) IMMUNOSERO - Chapter 10 - Labeled ImmunoassaysDocument4 pages(MID) IMMUNOSERO - Chapter 10 - Labeled ImmunoassaysAisle Malibiran PalerPas encore d'évaluation
- (MID) IMMUNOSERO - Chapter 13 - Hypersensitivity (Reviewer)Document6 pages(MID) IMMUNOSERO - Chapter 13 - Hypersensitivity (Reviewer)Aisle Malibiran PalerPas encore d'évaluation
- (MT-RES) Manuscript Evaluation ToolDocument5 pages(MT-RES) Manuscript Evaluation ToolAisle Malibiran PalerPas encore d'évaluation
- Pharma NotesDocument4 pagesPharma NotesAisle Malibiran PalerPas encore d'évaluation
- (F) Chapter 16 - Digestive System I, Oral Cavity and Associated StructuresDocument5 pages(F) Chapter 16 - Digestive System I, Oral Cavity and Associated StructuresAisle Malibiran PalerPas encore d'évaluation
- Bacteriology LectureDocument38 pagesBacteriology LectureAisle Malibiran Paler100% (1)
- Bacte Chapt. 16Document4 pagesBacte Chapt. 16Aisle Malibiran PalerPas encore d'évaluation
- Research ProtocolDocument1 pageResearch ProtocolAisle Malibiran PalerPas encore d'évaluation
- Chapter21 (Acinetobacter, Stenotrophomonas and Similar OrganismsDocument3 pagesChapter21 (Acinetobacter, Stenotrophomonas and Similar OrganismsAisle Malibiran PalerPas encore d'évaluation
- Urinary System - LabDocument1 pageUrinary System - LabAisle Malibiran PalerPas encore d'évaluation
- I Am Filipino by Carlos RomuloDocument1 pageI Am Filipino by Carlos RomuloAisle Malibiran PalerPas encore d'évaluation
- I Am Filipino by Carlos RomuloDocument1 pageI Am Filipino by Carlos RomuloAisle Malibiran PalerPas encore d'évaluation
- 1 - Overview of ComputersDocument99 pages1 - Overview of ComputersAisle Malibiran PalerPas encore d'évaluation
- Microbiology, Bailey - S and Scotts Chapter 28, Moraxella and Related Orgs. by MT1232Document3 pagesMicrobiology, Bailey - S and Scotts Chapter 28, Moraxella and Related Orgs. by MT1232Aisle Malibiran PalerPas encore d'évaluation
- Ra8504 - Aids LawDocument8 pagesRa8504 - Aids LawEnna TrivilegioPas encore d'évaluation
- 1987 Philippine ConstitutionDocument1 page1987 Philippine ConstitutionAisle Malibiran PalerPas encore d'évaluation
- Public Health Bylaws Under The Community CharterDocument9 pagesPublic Health Bylaws Under The Community CharterAisle Malibiran PalerPas encore d'évaluation
- Secrets of The New ManilaDocument1 pageSecrets of The New ManilaAisle Malibiran PalerPas encore d'évaluation
- HistoryDocument1 pageHistoryAisle Malibiran PalerPas encore d'évaluation
- Description of The BarangayDocument1 pageDescription of The BarangayAisle Malibiran PalerPas encore d'évaluation
- Why Cysteine Is SpecialDocument3 pagesWhy Cysteine Is SpecialAisle Malibiran PalerPas encore d'évaluation
- Paler, Aisle M. MT12221: Sonnet 144Document1 pagePaler, Aisle M. MT12221: Sonnet 144Aisle Malibiran PalerPas encore d'évaluation
- Igh 1Document4 pagesIgh 1Aisle Malibiran PalerPas encore d'évaluation
- InsulinDocument10 pagesInsulinAisle Malibiran PalerPas encore d'évaluation
- FootnotesDocument6 pagesFootnotesAisle Malibiran PalerPas encore d'évaluation
- Buffalo LeprosyDocument4 pagesBuffalo LeprosyALTAF HUSAINPas encore d'évaluation
- (2009) Study Guide To GeriatricPsychiatry - QsDocument41 pages(2009) Study Guide To GeriatricPsychiatry - QsPepe Garcia Estebez100% (1)
- Cardiovascular System QuizDocument4 pagesCardiovascular System QuizIrams KitchenPas encore d'évaluation
- Safety Data Sheet: Virbac New Zealand LimitedDocument5 pagesSafety Data Sheet: Virbac New Zealand LimitedХорен МакоянPas encore d'évaluation
- Information Technology in SurgeryDocument38 pagesInformation Technology in Surgerydooshy50% (4)
- Bishinik2002 10 OriginalDocument12 pagesBishinik2002 10 Originalalan woolardPas encore d'évaluation
- Human Anatomy QsDocument31 pagesHuman Anatomy QsAzhagar Ramesh SPas encore d'évaluation
- Anesthesia For TurpDocument5 pagesAnesthesia For Turptnim.dsPas encore d'évaluation
- Reliance Policy Extn Request FormDocument1 pageReliance Policy Extn Request Formanshu_204Pas encore d'évaluation
- Comparing Risk Factors of HIV Among Hijra SexDocument9 pagesComparing Risk Factors of HIV Among Hijra SexmariaelismecaPas encore d'évaluation
- Biopharmaceutics and Clinical Pharmacokinetics - 20210831 - 212949Document22 pagesBiopharmaceutics and Clinical Pharmacokinetics - 20210831 - 212949Md. Abu Bakar Siddique TayefPas encore d'évaluation
- 0 - Management of HyperuricemiaDocument44 pages0 - Management of HyperuricemiaYayuk Abay TambunanPas encore d'évaluation
- Procalcitonin Testing To Guide Antibiotic Therapy in Acute Upper and Lower Respiratory Tract InfectionsDocument2 pagesProcalcitonin Testing To Guide Antibiotic Therapy in Acute Upper and Lower Respiratory Tract InfectionsMr. LPas encore d'évaluation
- Daftar Pustaka NewDocument2 pagesDaftar Pustaka NewRini LianingsihPas encore d'évaluation
- Addiction, Treatment, and Evidence-Based Medicine - Wilcox, SeanDocument150 pagesAddiction, Treatment, and Evidence-Based Medicine - Wilcox, Seanadu66650% (2)
- VibhorDocument21 pagesVibhorNeha ShuklaPas encore d'évaluation
- Pebc Evaluating Exam Sample QuestionDocument50 pagesPebc Evaluating Exam Sample QuestionZain zanzoonPas encore d'évaluation
- Methods of ToiletDocument180 pagesMethods of Toiletathegeha100% (2)
- PLI Proposal FormDocument8 pagesPLI Proposal FormPalakala NagarjunaPas encore d'évaluation
- Article - CVD Cardiac Arrest - Bls AclsDocument2 pagesArticle - CVD Cardiac Arrest - Bls AclsAkhosh SomarajanPas encore d'évaluation
- Farmasi Manajemen Puskesmas KaliorangDocument5 pagesFarmasi Manajemen Puskesmas KaliorangDEA REGGIANAPas encore d'évaluation
- Optimization of Granulation and Compression Process Variables of Atenolol Tablets Using Box Behnken DesignDocument9 pagesOptimization of Granulation and Compression Process Variables of Atenolol Tablets Using Box Behnken DesignnkszonePas encore d'évaluation
- PBL 1 - Post Streptococcal Rheumatic Fever PolicyDocument8 pagesPBL 1 - Post Streptococcal Rheumatic Fever PolicyAinur AbdrakhmanovaPas encore d'évaluation
- Chapter 7: Emotional and Behavioural Problems: DR Jessie EarleDocument28 pagesChapter 7: Emotional and Behavioural Problems: DR Jessie EarlejajmajPas encore d'évaluation
- CyberTherapy & Rehabilitation, Issue 3 (3), Winter 2010.Document52 pagesCyberTherapy & Rehabilitation, Issue 3 (3), Winter 2010.Giuseppe RivaPas encore d'évaluation
- Mike's Recommended Books For Paramedic StudentsDocument3 pagesMike's Recommended Books For Paramedic StudentsMichael WilsonPas encore d'évaluation
- 1005 Hemorrhage ControlDocument88 pages1005 Hemorrhage ControlZainescu Dan100% (2)
- FCBDocument26 pagesFCBsprapurPas encore d'évaluation
- Stages of Labor and DeliveryDocument4 pagesStages of Labor and DeliveryvienreyPas encore d'évaluation
- BeneFusion VP5 FP Operator's Manual V2.0 enDocument114 pagesBeneFusion VP5 FP Operator's Manual V2.0 enherbertamaya0% (1)