Académique Documents
Professionnel Documents
Culture Documents
Aerosales en VM 2015
Transféré par
césar_campos_45Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Aerosales en VM 2015
Transféré par
césar_campos_45Droits d'auteur :
Formats disponibles
CRITICAL CARE/RESPIRATORY CARE
Aerosol Drug Delivery During Mechanical
Ventilation: Devices, Selection, Delivery Technique, and
Evaluation of Clinical Response to Therapy
Arzu Ari, PhD, RRT, PT, CPFT, FAARC,
and James B. Fink, PhD, RRT, FAARC, FCCP
Abstract: Aerosolized medications are increasingly being used in
ventilator-dependent patients. There are many issues with selection and
use of aerosol delivery devices in patients receiving ventilator support.
The purpose of this paper is to explain potential problems associated
with aerosol devices, delivery technique, and clinical response to
therapy to assure patient well-being and safety during inhalation
therapy.
Key Words: nebulizers, metered-dose inhalers, aerosols, drug delivery, optimum technique, mechanical ventilation
(Clin Pulm Med 2015;22:7986)
any formulations, both solutions and suspension, such as
short-acting bronchodilators, anticholinergics, corticosteroids, mucokinetics, antibiotics, antivirals, prostanoids,
surfactants, diuretics, anticoagulants, proteins, and peptides,
have been used for the treatment of mechanically ventilated
patients.1 Drug delivery to patients receiving ventilator support
has been associated with low delivery efficiency and high
variability in dosing. There are many issues with device
selection and use of each aerosol device during mechanical
ventilation. Standard of practice is still far away from an
optimum technique that should be utilized during inhalation
therapy to mechanically ventilated patients. Therefore, the
purpose of this paper is to identify and explain potential
problems associated with aerosol devices, delivery technique,
From the Division of Respiratory Therapy, College of Health and Human
Sciences, Georgia State University, Atlanta, GA.
The study was conducted in the Aerosol Research Lab at Georgia State
University.
Disclosure: J.B.F. serves as a consultant to the biotech industry. His clients
include Aerogen, Ansun, Aridis, Bayer, Dance Biopharm, Parion,
Quark, and WHO. He currently serves as Chief Clinical Officer for
Aerogen, and Senior Fellow, Aerosol Device Development for Dance
Biopharm. He is an adjunct Professor to the Respiratory Care Programs
at Georgia State in Atlanta, and Rush Medical School in Chicago. In
addition, he has a grant from the Brazilian government to serve as a
Scholar without Borders working with the Cardiopulmonary Physiotherapy Department at Federale University of Pernumbuco in Recife,
Brazil. In all 3 academic programs he supervises graduate students in
Aerosol Research. He has involvement with the following products:
Aeroneb Pro, Solo, Go and Lab (Aerogen), PPDS system for Amikacin
(Bayer), Dance 501 Inhaler for insulin (Dance Biopharm), Prototype
nasal delivery system (Parion), and Measles vaccine delivery system
for mass campaigns in third world (WHO). A.A. declares that there are
no conflicts of interest.
Address correspondence to: Arzu Ari, PhD, RRT, PT, CPFT, FAARC,
Division of Respiratory Therapy, College of Health and Human Sciences, Georgia State University, P.O. Box 4019, Atlanta, GA 303024019. E-mail: arzuari@hotmail.com.
Copyright r 2015 Wolters Kluwer Health, Inc. All rights reserved.
ISSN: 1068-0640/15/2202-0079
DOI: 10.1097/CPM.0000000000000085
Clinical Pulmonary Medicine
and clinical response to therapy to assure optimal patient
benefit, well-being, and safety during inhalation therapy.
AEROSOL DEVICES
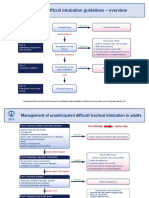
Two types of aerosol devices are used for aerosol drug
delivery to ventilator-dependent patients: (1) nebulizers and (2)
pressurized metered dose inhalers (pMDIs). Types of nebulizers used for the treatment of intubated and mechanically
ventilated patients are jet nebulizers (JNs), ultrasonic nebulizers (UNs), and vibrating mesh nebulizers (VMNs). Figure 1
shows illustrations of aerosol devices used for the treatment of
ventilator-dependent patients.
Nebulizers
JNs have been commonly used for aerosol drug delivery
during mechanical ventilation since the advent of modern
mechanical ventilation in the mid-1950s. These relatively
inexpensive nebulizers are operated using 2 to 10 L/min of
compressed gas and cause entrainment often resulting in the
injection of additional gas into the ventilator circuit. This can
lead to an increase in volumes and pressures delivered during
mechanical ventilation, especially in smaller patients, if the
ventilator does not compensate for nebulizer gas flow entering
the circuit. Therefore, clinicians may be well advised to adjust
ventilator parameters during aerosol administration and return
the ventilator to pretreatment levels after the completion of
therapy. During operation of JNs, larger particles tend to
deposit on the baffles and walls of the nebulizer. Then, they
return to the reservoir to be renebulized causing an evaporative
effect that increases concentration of medication over time,
especially with continuous nebulization. Contamination is a
risk associated with the use of JNs during mechanical ventilation because the JN reservoir is in a dependent position to
and in direct contact with the ventilator circuit. This allows
fluids, secretions, and pathogens in condensate that forms in
the circuit to drain into the reservoir of the nebulizer where it
contaminates the medication, resulting in the production of
contaminated aerosol which is then delivered to the patient.
Unfortunately these least expensive aerosol generators
tend to be the least efficient for aerosol delivery during
mechanical ventilation. As JNs have large residual volumes of
up to 2 mL, a substantial portion of drugs placed in the nebulizer stays in the reservoir and cannot be delivered to ventilator-dependent patients. Consequently, with typical dose
volumes of 3 mL, the efficiency of JNs is much less than other
aerosol device options, which have lower residual drug
remaining in the nebulizer at the conclusion of dosing.
Whereas aerosol delivery of JNs ranges from 2% to 5.4%
during mechanical ventilation, delivery efficiency of VMNs,
UNs, and pMDIs are 8.7% to 33.3%, 8.7% to 17% and 2.5% to
Volume 22, Number 2, March 2015
www.clinpulm.com |
79
Clinical Pulmonary Medicine
Ari and Fink
Jet Nebulizer (JN)
(Mistyneb)
Vibrating Mesh (VM)
(Aeroneb Pro)
Ultrasonic Nebulizer (UN)
(PB Easyneb)
Volume 22, Number 2, March 2015
Metered-dose Inhaler (pMDI)
and Spacer (AeroVent)
Aeron
eb
FIGURE 1. Variety of aerosol devices used for drug delivery to ventilator-dependent patients. From left to right: jet nebulizers, vibrating
mesh nebulizers, ultrasonic nebulizers, and pressurized metered dose inhalers.
17%, respectively, in a heated humidified ventilator circuit,
dependent on position of the aerosol generator.
The insertion and removal of nebulizers from the ventilator circuit during mechanical ventilation is often associated
with a break in the circuit with an interruption of airway
pressure and ventilation, which may cause derecruitment of
the lung resulting in lower lung volumes for an hour or longer.
In addition, breaking the circuit to insert or remove a JN,
allows contaminated fluids and secretion to be released into the
atmosphere, posing a risk to the environment, health care
providers, and other patients in the vicinity. Spring-loaded
valved T adapters may be used for the attachment of JNs to the
ventilator circuit to reduce interruption of ventilation when the
JN is attached or removed. Thus, they can reduce or eliminate
loss of pressure in the ventilator circuit during placement or
removal of a JN while eliminating nebulizer contamination
from the fluids and secretions retained in the circuit. However,
the valve system in these devices act as an additional baffle for
aerosol leaving the nebulizer and have been associated with
reduction of available aerosol to the patient by as much as 30%
compared with the standard open T adapter. In a situation
where deposition from a JN is as low as 3% of total dose, this
30% reduction is substantial.
UNs are available for use during mechanical ventilation,
but are not widely used. They tend to be expensive, bulky, and
generate more heat than other aerosol generators, which may
cause degradation of heat-sensitive materials such as proteins.
UNs may produce particles smaller than suspension, reducing
actual drug output, which may not be detectable by observing
the output of the nebulizer. Therefore, UNs are not recommended for administration of suspension. The residual volume
of UNs ranges from 0.8 to 1.2 mL. Despite their relatively
large residual drug volumes, UNs tend to be more efficient
than JNs, perhaps because they do not introduce a secondary
gas flow into the ventilator circuits. Like JNs, UN drug reservoirs and aerosol generators are position dependent to the
ventilator circuit, allowing contaminated condensate to drain
from the circuit into the reservoir.
VMNs have been associated with 3- to 5-fold higher drug
delivery efficiency than JNs with similar to greater efficiency
than UNs. This may be due in part to the smaller residual
volumes (< 0.2 mL) than other nebulizers and the lack of
additional gas added to the circuit of ventilator-dependent
patients. VMNs are the delivery of choice when clinicians need
to deliver expensive formulations and precise dosing is needed.
Contamination with pathogens and condensation in the circuit
is less of an issue with VMNs because they are positioned
superior to the ventilator circuit during therapy and their
medication reservoir is separated from the ventilator circuit by
the physical barrier of the mesh membrane. While VMNs are
80 | www.clinpulm.com
powered by battery or electricity, they tend to be small and less
noisy than JNs. As VMNs do not add heat to the medication,
risk of denaturation of proteins is minimal. With only a single
pass of medication through the aerosol generating mesh, drug
concentration is not altered over time. More viscous drugs may
reduce the rate of aerosol output, requiring longer treatment
times. Theoretically, large suspensions may clog the pores of
VMNs over time, but such incidents have not been reported.
Despite many advantages compared with other nebulizers, the
cost of VMN is an issue, being 20-fold greater than JNs.
VMNs are available as a single patient multidose disposable
nebulizer and as a more expensive multipatient, autoclavable
device. For the reusable VMNs cleaning should be gentle with
no direct contact to the mesh, to prevent damage.
Pressurized Metered Dose Inhalers
For the past 2 decades, pMDIs have been widely used for
aerosol drug delivery to mechanically ventilated patients.
pMDIs are small, single patient, multiple dose, disposable
devices that provide easy operation, short treatment time, and
consistent dosing. The pMDI consists of a canister containing
propellants, drugs, and excipients with a metering valve that
releases a precise quantity of drug and propellant with each
actuation (manually compressing the nozzle of the canister into
the seat of the actuator to release a metered dose of drug and
propellant). Virtually all pMDIs are designed for use with
ambulatory patients, with an actuator mouthpiece that is open
to atmosphere. Consequently, for use in a closed ventilator
circuit, a third-party designed spacer or low-volume adapter
with a port to accept the nozzle of the canister and spray nozzle
to disperse the emitted aerosol within the circuit must be used.
Aerosol delivery efficiency varies widely with the shape, size,
and design of these adapters. The type of adapter or spacer used
with pMDI affects aerosol drug delivery during mechanical
ventilation. Researchers report that bidirectional low-volume
adapters are more efficient than unidirectional adapters,
whereas cylindrical/chamber spacers provide 2 to 6 times
more drug delivery than unidirectional and bidirectional lowvolume adapters.24 Collapsible chamber-type spacers reduce
both the volume of the circuit and the formation of condensate
in the spacer chamber between treatments. In addition, collapsible chamber-type spacers prevent circuit disconnection and
minimize the risk of ventilator-associated pneumonia.
For effective drug delivery, the pMDI should be placed
proximal to the patient airway and must be actuated manually at
the beginning of inspiration from the ventilator. Microbial contamination of canister contents has not been reported with pMDI
use during mechanical ventilation; however, contamination of
the external surfaces of the canister may provide a vector for
communication of bacteria from care providers and other
Copyright
2015 Wolters Kluwer Health, Inc. All rights reserved.
Clinical Pulmonary Medicine
Volume 22, Number 2, March 2015
patients, especially when the pMDI is used across multiple
patients. For many years, pMDIs were considered the most costeffective drug delivery options in critical care. However, with the
introduction of hydrofluoroalkane (HFA) propellants, the higher
costs of pMDIs have made use of other types of aerosol generators using unit doses of liquid medications to appear more
cost effective. Nebulizers in general require more preparation
time to set up, cleaning, and maintenance than pMDIs. Treatment time with pMDIs is shorter than nebulizers and pMDIs
provide consistent and convenient dosing with each treatment
with reduced chances of bacterial contamination.57 Therefore,
utilization of pMDIs during mechanical ventilation has greatly
increased over the past 25 years.8,9
It is essential to track the number of doses remaining in a
pMDI either manually or with the use of a dose counter.
Otherwise, it will be impossible to determine the remaining
dose in pMDIs with potential for use of pMDIs beyond their
capacity to administer medication. Although newer pMDIs
have built-in dose counters, they may not allow removal of the
canister from the actuator or fit in standard commercial
adapter/spacers. Thus, an adapter that fits the specific pMDI
should be used.
DEVICE SELECTION
Previous evidence confirms similar therapeutic effects of
nebulizers and pMDIs with in-line adapter/spacers in ventilator-dependent patients when the drug is available in both
formats.1015 Such studies are largely based on bronchodilators. However, not all aerosol devices and interfaces provide
the same level of efficiency under all conditions. So the key
question is which device to use with which medication for any
specific ventilator circuit.
Drug Availability
The variety of drugs available with pMDIs is largely limited to bronchodilators and corticosteroids. In addition, the dose
volume of pMDIs (30 to 100 mL/actuation) is much smaller than
the 2 to 6 mL delivered with nebulizers. Nebulizers present the
opportunity for delivery of larger payloads of drugs to the lungs
with a broader range of inhaled medication including mucolytics,
mucokinetics, antivirals, antibiotics, diuretics, prostanoids, and
others. Consequently, the selection of aerosol devices for aerosol
administration during mechanical ventilation rests with the needs
of the patient, the intent of the clinician, and the desired therapeutic outcomes. In addition, if the drug is not available in a
pMDI, the nebulizer becomes the default aerosol generator
option. The need for efficient aerosol delivery increases with the
cost of any specific medication.
Target Payload and Delivery Efficiency
An expensive drug such as an antibiotic is approved for
inhalation in ambulatory CF patients using a vented breath
enhanced JN that delivers approximately 12% of the antibiotic
dose to the patients lungs. As that nebulizer cannot be used
during mechanical ventilation, the alternative aerosol device
selected for use with the ventilator should match or exceed the
lung dose achieved in ambulatory patients. Use of standard JN
with 3% efficiency might require up to 4 doses to achieve the
target 12% lung dose. In contrast, either a UN or VMN, with
efficiency of 12% to 17% during mechanical ventilation,
would provide a comparable lung dose with a single administration. In contrast, a pMDI despite 17% delivery efficiency
is not available with many formulation besides bronchodilators
and inhaled corticosteroids.
Copyright
Aerosol Drug Delivery During Mechanical Ventilation
Risk and Benefits
Although the pMDI is associated with less exhaled aerosol
than a nebulizer, all aerosol generators used in ventilatordependent patients may lead to escape of aerosol to the environment, which creates health risks to health care professionals,
caregivers, and other patients. However, the aerosols generated
by patients themselves may be the greater risk for transmission
of airborne diseases from swine flu (H1N1) and severe acute
respiratory syndrome to tuberculosis. Consequently, ventilators
should be equipped with some form of high-efficiency particulate air filter in the expiratory limb to mechanically reduce
escape of aerosol (whether generated by the patient or a nebulizer) from the ventilator circuit to the environment.
Risks such as infection with JN and an increase in drug
concentration with JN and UN should be considered during
device selection for inhalation therapy in ventilator-dependent
patients.
Cost (Both Drug and Technology)
With the transition of pMDIs from chlorofluorocarbon to
the more environmentally friendly HFA propellants, the price
of some pMDIs has increased as much as 5-fold. As the price
of a pMDI increases, the cost advantage can shift to the more
inherently expensive UN and VM technologies using less
expensive liquid formulations. The cost of pMDIs range from
$45 to $375. For instance, the ProAir HFA costs $45 for 200
puffs, whereas the price of the Advair HFA including 120 puffs
is $375 in the United States. A unit dose of albuterol/ipratropium formulation is <$0.25 per dose, whereas 4 puffs of
combivent was $5. UNs cost around $200 as opposed to VMNs
that cost from $200 to $1200. UNs, used in critical care,
require a control module ($1000), a durable aerosol generator
($200) that requires sterilization between patients, and disposable medication cups ($1) changed with each treatment.
VMN requires a controller unit ($500) with a single-patient
multiple-use aerosol generator ($45) or a multipatient use
autoclavable aerosol generator ($350). In contrast, the standard
JN may cost between $1 and $5.
The effectiveness of most inhaled drugs is based on the
amount of drug that is delivered to the lungs. If the drug was
approved in ambulatory patients with 12% dose efficiency, use of
a jet neb on a ventilator with 3% efficiency would require 4
doses to deliver a comparable mass of drug to the lung. For drugs
such as albuterol and ipratropium, the low costs per dose suggest
that JN may be cost effective, whereas other drugs ranging from
$10 to $125 per dose, use of the more efficient UN or VMN may
reduce cost of medication and more than off-setting the greater
cost of equipment ($25 to $50 per patient). Table 1 shows costs
of different drugs per dose and cost comparisons between VMN
and JN on their use of a 5-day period.
TABLE 1. Cost Comparisons Between Vibrating Mesh (VMN)
and Jet Nebulizer (JN) to Achieve Target Lung Dose During
Mechanical Ventilation With Different Drug Over a 5-Day Period
Drugs and Dose
Frequency
Tobi bid
Pulmozyme bid
Pulmicort bid
Mucomyst qid (10 mL)
Duo-Neb qid
Albuterol qid
2015 Wolters Kluwer Health, Inc. All rights reserved.
Drug Costs/
Dose
5d
VMN
5 d JN
125
89.70
10
16
0.40
0.25
1250
900
100
160
8
5
5000
3600
400
640
32
20
www.clinpulm.com |
81
Clinical Pulmonary Medicine
Ari and Fink
Volume 22, Number 2, March 2015
TABLE 2. Ventilator-related Factors, Their Effects, and
Recommendations to Optimize Bronchodilator Delivery in
Mechanically Ventilated Adults
TABLE 3. Circuit-related Factors, Their Effects, and
Recommendations to Optimize Bronchodilator Delivery in
Mechanically Ventilated Adults
Factors
Factors
Effects
Recommendations
Mode of
ventilation
The efficiency of
Prefer volume-controlled
nebulizer is lower in
ventilation when using
pressure-controlled
a nebulizer, if possible
ventilation than in
Use spontaneous modes,
volume-controlled
if tolerated by patients
ventilation
Spontaneous modes such
as CPAP increase
aerosol drug delivery
up to 23%
Tidal volume Low-tidal volume
Set tidal volume greater
decreases aerosol drug
than the volume of
delivery to the lower
tubing and ETT
respiratory tract
between the nebulizer
and the patient. For
adults it should be set to
>500 mL, if appropriate
for the patient
Inspiratory
Inspiratory time and duty Increase inspiratory time
time and
cycle are directly
while minimizing the
related to aerosol
duty cycle
degree of intrinsic
delivery during
PEEP. Duty cycle of
mechanical ventilation.
Z0.3 is recommended
As inspiratory time or
duty cycle increases,
more aerosol will be
delivered to the patient
Flow
Higher inspiratory flow
Use an inspiratory flow
increases turbulence,
of 30 to 50 L/min, if
transitional flow, and
tolerated, during
inertial impaction,
nebulization
thereby reducing
aerosol delivery
Bias flow
Bias flow dilutes aerosol Use lower bias flow
(breathgenerated proximal to
r2 L/min with
triggering
the patient but low
nebulizers when
mechanism)
flows may improve
possible
aerosol from VMNs and Synchronize actuations of
UNs placed proximal to pMDIs with inspiration
the patient
Inspiratory
Square waveform delivers Choose sinusoidal or
waveform
less aerosol than
decreasing ramp
decreasing ramp or
waveforms
sinusoidal waveforms
Reproduced with permission from Ari and Fink.16
DELIVERY TECHNIQUE
Endotracheal Drug delivery decreases
tube (ETT)
with the reduction of the
inner diameter of the
ETT
Heat and
The filter of the heat
humidity
moisture exchanger
(HME) acts as a barrier
to aerosol delivery
Placement of nebulizers
between the HME and
patient airway may
overload the HME with
exhaled aerosol and
increase work of
breathing over time
Heated humidifiers may
reduce aerosol
deposition; however,
cold dry air is a greater
problem
Turning off the humidifier
for up to 30 min does not
increase aerosol
deposition
Density of
Heliox creates the
inhaled gas
persistence of laminar
flows in the ventilator
circuit and airways
improving aerosol
deposition by decreasing
particle impaction losses
The lower density of
heliox is not as effective
in generating aerosol
with jet nebs, requiring
2-fold higher flows,
which may alter
ventilator parameters
Vibrating mesh, ultrasonic
nebs, and pMDIs
generate aerosol without
being affected by heliox
Right-angle
Using a right-angle elbow
elbow
adapter decreases
adapter
aerosol delivery from a
pMDI on a humidified
ventilator circuit but not
on a nonhumidified
circuit
Recommendations
Place the largest diameter
ETT that the patient can
safely tolerate. Keep
ETT clear of secretions
Remove the HME before
aerosol drug
administration and place
it back into the circuit
after the treatment
Do not place nebulizers
between the HME and
patient airway
Do not turn off or remove
the heated humidifier
from the circuit.
Increase the dose, as
needed for clinical
response
Use heliox 80:20 or 70:30
for optimal delivery of
aerosols through the
ventilator circuit. Do not
dilute <50:50 for effect
Use lower flow of oxygen
to power jet nebulizers.
If you do use heliox,
increase the flow rate by
2-fold
Use vibrating mesh, USN,
or pMDI with spacer
with heliox
Remove the right-angle
elbow adapter, when
using a humidified
ventilator circuit
Reproduced with permission from Ari and Fink.16
Several categories of factors affecting aerosol drug
delivery to critically ill patients receiving mechanical ventilation include: (1) ventilator-related factors, (2) circuit-related
factors, and (3) device-related factors.16 Ventilator-related
factors include mode of ventilation, tidal volume, inspiratory
time and duty cycle, flow, bias flow (breath-triggering mechanism), and inspiratory waveform. Circuit-related factors include
heat and humidity, artificial airways, and right-angle elbow
adapter. Device-related factors include placement of aerosol
device in the circuit, type of nebulizer, nature of nebulization
(intermittent vs. continuous), amount of residual drug (dead)
volume, amount of gas flow, type of adapter/spacer, as well as
shaking and actuation of pMDI. Tables 24 explain effects of
ventilator-related, circuit-related, and device-related factors,
82 | www.clinpulm.com
Effects
respectively, while providing recommendations to optimize
aerosol delivery in mechanically ventilated adults.
Successful delivery of medical aerosols to mechanically
ventilated patients can be best achieved with adequate drug
deposition at the intended site of action in the lung. As optimum drug delivery in mechanically ventilated patients is
technique dependent, careful attention to delivery technique
during mechanical ventilation is essential. Figure 2 shows an
algorithm describing steps for optimal drug administration
technique by each aerosol device.
According to previous research, placing patients in a semiFowler or seated position increases drug delivery during aerosol
Copyright
2015 Wolters Kluwer Health, Inc. All rights reserved.
Clinical Pulmonary Medicine
Volume 22, Number 2, March 2015
Aerosol Drug Delivery During Mechanical Ventilation
TABLE 4. Device-related Factors, Their Effects, and Recommendations to Optimize Bronchodilator Delivery in Mechanically Ventilated
Adults
Factors
Effects
Position of aerosol
device in circuit
Nebulizer-related
factors
pMDI-related factors
Recommendations
The location of the aerosol device in the ventilator circuit
significantly affects aerosol drug delivery
Place the jet nebulizer close to the ventilator. Position the
pMDI proximal to the patient. Vibrating mesh and
ultrasonic nebulizers in inspiratory limb near the Y
adapter, or proximal to the ventilator when using bias
flow
Nebulizer type: jet nebulizers are less efficient than
Choose the vibrating mesh nebulizer, USN, or pMDI with
vibrating mesh nebulizers, ultrasonic nebulizers, and
spacer for aerosol delivery in mechanically ventilated
pMDIs with spacer
patients
Intermittent and continuous nebulization: intermittent
Run the jet nebulizer intermittently, if ventilator has that
nebulization synchronized with expiration is more
option
efficient for aerosol delivery than continuous nebulization For continuous jet nebulizer, set the flow rate at 6 to 8 lpm
or as recommended by manufacturer and adjust the
ventilator parameters (Vt, pressure, and alarms)
Residual dead volume: the greater the dead volume, the less Use the vibrating mesh nebulizer when possible
amount of drug is nebulized. Jet nebulizers do not
In the absence of the vibrating mesh nebulizer, increase fill
aerosolize below dead volume of 1 to 2.5 mL. Vibrating
volume to 4 to 5 mL unless the jet nebulizer is
mesh nebulizers have smaller residual volumes than jet or
specifically designed for a smaller fill volume
ultrasonic nebulizers
Gas flow: the ultrasonic and vibrating nebulizers are not
Use the ultrasonic or vibrating mesh nebulizers for aerosol
influenced by gas flow as they are electrically powered.
delivery with heliox
Particle size minimally affected with heliox
Set the flow rate at 6 to 8 lpm or as recommended by
Operating the jet nebulizer at a lower flow or pressure than
manufacturer and adjust the ventilator parameters (Vt and
the design will increase particle size and reduce delivery.
pressure), if you run the jet nebulizer continuously
Gas flow inversely related to nebulization time with the
jet nebulizer
pMDI actuation: synchronized pMDI actuations with
Synchronize pMDI actuations with inspiration. Actuate at
inspiration increase aerosol delivery
Z15 s intervals
Spacer: using a chamber spacer with the pMDI reduces
Use chamber spacers with the pMDIs for aerosol
losses in the circuit and increases drug delivery up to 6administration to mechanically ventilated patients
fold
Bidirectional inline adapters are a better option than
The efficiency of a bidirectional inline adapter was higher
unidirectional low-volume inline adapters
than the efficiency of an unidirectional inline adapter and
achieved efficiency marginally less than chamber spacers
Shaking the canister: the drug in the pMDI formulations are Shake the pMDI before the first actuation of each dose
separated when standing. Therefore, not shaking a pMDI
(up to 8 puffs) administered
canister reduces total and respirable dose up to 35%
Reproduced with permission from Ari and Fink.16
therapy.1721 Therefore, when possible, clinicians should utilize
these positions to increase the efficiency and distribution of
aerosol delivery. In patients who cannot sit in the bed during
aerosol administration, the head of the bed should be elevated
between 20 and 30 degrees above horizontal.
JNs are commonly operated continuously using an external
gas source and method to meter flow and pressure (often at 50 psi).
Some ventilators offer integrated nebulization options using
internal compressors or flow diverters to drive JNs. When integrated with the software of the ventilator, these units can eliminate
the need for adjustment of ventilator parameters and activation of
ventilator alarms during aerosol drug delivery. Most compressors
operate JNs at a lower driving pressure (< 15 psi) than when using
pressurized gas (Z50 psi), which may produce larger particles and
cause a reduction in the efficiency of the JN.22,23
Historically, ventilators with integrated nebulizer outlets
synchronized nebulization with inspiration. More recently,
ventilators may offer nebulization during inspiration, expiration, or continuously through the breathing cycle. It was initially reported that nebulization during inspiration would
increase deposition compared with continuous delivery2426
with the nebulizer placed near the patient airway, with less
difference when placement was more distal from the patient.
However, more recent studies report that intermittent
Copyright
inspiratory nebulization was less efficient than either continuous or intermittent expiratory aerosol generation. Intermittent inspiratory mode did not increase lung delivery but did
dramatically increased treatment time.27,28 Ventilators with
integrated nebulizer controls often compensate for the added
flow to the nebulizer to maintain tidal volume, inspiratory
pressures, and minute ventilation during aerosol delivery,
reducing the need to adjust parameters or alarms, during and
after nebulization.
It is important to prime the pMDI before first use and
when the canister has not been used for >24 hours to avoid
separation of drug from the propellants. Similarly, the pMDI
should be shaken before first actuation for each treatment.
Otherwise, this simple mistake in delivery technique will lead
to a decrease in aerosol deposition to ventilator-dependent
patients.29 Synchronizing pMDI with the beginning of inspiration, using a chamber spacer, and placing the spacer 6 inches
from the Y adapter in the ventilator circuit increases aerosol
drug delivery during mechanical ventilation.17,30,31
Previous studies show that mistakes in delivery technique
influence aerosol drug delivery in ventilated patients.22,3240 These
mistakes in technique are specific to the delivery device used
during treatment. For instance, when nebulizers are used for aerosol delivery during mechanical ventilation, clinicians may set gas
2015 Wolters Kluwer Health, Inc. All rights reserved.
www.clinpulm.com |
83
Clinical Pulmonary Medicine
Ari and Fink
Volume 22, Number 2, March 2015
Review order identify patient and assess need for bronchodilator.
Clear the airways by suctioning, if needed.
If using an HME, remove it from the circuit.
If using a heated humidifier, do not turn off or disconnect during the
treatment.
JN:
Correctly assemble the nebulizer.
Fill the nebulizer with volume on drug
label. You may increase volume to 4-6 mL
to increase delivery.
Place the JN in the inspiratory line near
the Y adapter or proximal to the
ventilator.
VMN:
Correctly assemble the nebulizer.
Pour recommended drug volume into
the nebulizer.
Place the VMN in the inspiratory line
near the Y adapter or proximal to the
ventilator.
pMDI:
Shake and prime the pMDI.
Warm the pMDI canister to hand or
body temperature.
Place the pMDI spacer/adapter in the
inspiratory line near the Y adapter.
Correctly assemble the pMDI canister
with spacer/adapter.
Ensure that there is no leak in the circuit.
Position the patient in an upright position, if possible.
JN:
Connect the nebulizer to a gas source.
If available, use gas source on the
ventilator in order to synchronize
nebulization with inspiration
Otherwise set gas flow to the JN at 6 to 8
l/min (or flow recommended on label).
Adjust ventilator volume or pressure limit
to compensate for added flow.
VMN:
Connect the nebulizer to a power source.
Turn on the power.
pMDI:
Coordinate actuations with beginning of
inspiration.
Do not remove or shake the pMDI
between actuations.
Wait 15 seconds between actuations.
Observe aerosol cloud for adequate aerosol generation during treatment.
At the completion of treatment, remove device from the ventilator circuit.
Clean as recommended by manufacturer or institution.
Reconnect the HME.
Return ventilator settings and alarms to previous values. Ensure there
is no leak in the ventilator circuit.
Monitor vital signs, oxygen saturation and patent-ventilator
synchronization.
Monitor for adverse response.
Assess outcome and document findings.
FIGURE 2. An algorithm describing steps for optimal drug administration technique by each aerosol generator. Reproduced with
permission from Ari and Fink.16
flow improperly. Not shaking pMDI before treatment, not synchronizing pMDI actuations with the beginning of inspiration, or
not using the right type of spacer with pMDI will significantly
reduce aerosol drug delivery to ventilator-dependent patients. In
addition, improper positioning of the aerosol device in the ventilator circuit will influence efficiency of treatment during mechanical ventilation.33,34
84 | www.clinpulm.com
EVALUATION OF CLINICAL RESPONSE TO
THERAPY
There are many factors affecting the patients response to
bronchodilator delivery during mechanical ventilation. These
factors include patient airway geometry, degree of airway
responsiveness, severity of disease, quantity and nature of
secretions, and degree of airway inflammation.
Copyright
2015 Wolters Kluwer Health, Inc. All rights reserved.
Clinical Pulmonary Medicine
Volume 22, Number 2, March 2015
Aerosol Drug Delivery During Mechanical Ventilation
Evaluation of response to therapy should include heart
rate, respiratory rate, oxygen saturation, blood pressure,
patient-ventilator asynchronization, and airway resistance.
Administration of high doses of b-adrenergic bronchodilators
may result in tachycardia, atrial arrhythmias, or ventricular
arrhythmias.41 Comparisons of airway resistance and autopositive end expiratory pressure (auto-PEEP) before and after
bronchodilator administration are useful for the evaluation of
patient response to bronchodilator delivery during mechanical
ventilation.42,43 Several studies conducted on patients with
chronic obstructive pulmonary disease showed a decrease
in airway resistance and auto-PEEP after bronchodilator
administration.14,17,44
Clinicians should monitor patients before, during, and
after the administration of aerosolized bronchodilator during
mechanical ventilation. It is also important for clinicians to
stay with patients during inhalation therapy through nebulizers.
This will enable them to assure uninterrupted administration of
aerosol therapy for ventilator-dependent patients and enhance
patient safety by rapid response to complications caused by
aerosol drug delivery during mechanical ventilation.
In summary, successful aerosol delivery with metereddose inhalers and nebulizers in intubated, mechanically ventilated patients requires efficient delivery to the lower respiratory
tract. There are many issues with selection and use of aerosol
devices in ventilator-dependent patients. Once clinicians
understand potential problems and opportunities associated
with aerosol devices, delivery technique, and clinical response
to therapy, they will be able to optimize aerosol drug delivery
to patients receiving ventilator support while assuring patient
safety and well-being during inhalation therapy.
18.
REFERENCES
23.
1. Fink J, Ari A. Aerosol therapy in intubated patients. Expert Opin
Drug Deliv. 2013;10:10771093.
2. Rau J, Dunlevy C, Hill R. A comparison of inline MDI actuators
for delivery of a beta agonist and a corticosteroid with
a mechanically-ventilated lung model. Respir Care. 1998;43:
705712.
3. Rau J, Harwood R, Groff J. Evaluation of a reservoir device for
metered-dose bronchodilator delivery to intubated adults: an invitro study. Chest. 1992;102:924930.
4. Fuller HD, Dolovich MB, Turpie FH, et al. Efficiency of
bronchodilator aerosol delivery to the lungs from the metered dose
inhaler in mechanically ventilated patients. A study comparing four
different actuator devices. Chest. 1994;105:214218.
5. Hamill R, Houston E, Georghiou P. An outbreak of Burkholderia
cepacia respiratory tract colonization and infection associated with
nebulized albuterol therapy. Ann Intern Med. 1995;122:762766.
6. Craven D, Lichtenberg D, Goularte T. Contaminated medication
nebulizers in mechanical ventilator circuits. Source of bacterial
aerosols. Am J Med. 1984;77:834838.
7. Rubin B, Fink J. Optimizing aerosol delivery by pressurized
metered-dose inhalers. Respir Care. 2005;50:11911200.
8. Ballard J, Lugo RA, Salyer JW. A survey of albuterol
administration practices in intubated patients in the neonatal
intensive care unit. Respir Care. 2002;47:3138.
9. Chang L, Honiden S, Haithcock J. Utilization of bronchodilators in
ventilated patients without obstructive airways disease. Respir
Care. 2007;52:154158.
10. Dhand R. Inhalation therapy in invasive and noninvasive
mechanical ventilation. Curr Opin Crit Care. 2007;13:2738.
11. Dolovich MB, Ahrens RC, Hess DR, et al. Device selection and
outcomes of aerosol therapy: evidence-based guidelines: American
College of Chest Physicians/American College of Asthma,
Allergy, and Immunology. Chest. 2005;127:335371.
12. Duarte A, Momi K, Bidani A. Bronchodilator therapy with
metered dose inhaler and spacer versus nebulizer in mechanically
Copyright
13.
14.
15.
16.
17.
19.
20.
21.
22.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
2015 Wolters Kluwer Health, Inc. All rights reserved.
ventilated patients: comparison of magnitude and duration of
response. Respir Care. 2000;45:817823.
Gay PC, Patel HG, Nelson SB, et al. Metered dose inhalers for
bronchodilator delivery in intubated, mechanically ventilated
patients. Chest. 1991;99:6671.
Guerin C, Chevre A, Dessirier P, et al. Inhaled fenoterolipratropium bromide in mechanically ventilated patients with
chronic obstructive pulmonary disease. Am J Respir Crit Care
Med. 1999;159:10361042.
Laube BL, Janssens HM, de Jongh FH, et al. What the pulmonary
specialist should know about the new inhalation therapies. Eur
Respir J. 2011;37:13081331.
Ari A, Fink JB. Factors affecting bronchodilator delivery in
mechanically ventilated adults. Nurs Crit Care. 2010;15:192203.
Dhand R, Jubran A, Tobin MJ. Bronchodilator delivery by
metered-dose inhaler in ventilator-supported patients. Am J Respir
Crit Care Med. 1995;151:18271833.
Mouloudi E, Katsanoulas K, Anastasaki M, et al. Bronchodilator
delivery by metered-dose inhaler in mechanically ventilated
COPD patients: influence of end-inspiratory pause. Eur Respir J.
1998;12:165169.
Mouloudi E, Prinianakis G, Kondili E, et al. Bronchodilator
delivery by metered-dose inhaler in mechanically ventilated
COPD patients: influence of flow pattern. Eur Respir J. 2000;16:
263268.
Georgopoulos D, Mouloudi E, Kondili E, et al. Bronchodilator
delivery with metered-dose inhaler during mechanical ventilation.
Crit Care. 2000;4:227234.
Tzoufi M, Mentzelopoulos SD, Roussos C, et al. The effects of
nebulized salbutamol, external positive end-expiratory pressure,
and their combination on respiratory mechanics, hemodynamics,
and gas exchange in mechanically ventilated chronic obstructive
pulmonary disease patients. Anesth Analg. 2005;101:843850.
Dhand R. Aerosol delivery during mechanical ventilation: from
basic techniques to new devices. J Aerosol Med Pulm Drug Deliv.
2008;21:4560.
Ari A. Aerosol therapy for mechanically ventilated patients:
devices, issues, selection & technique. Clin Found. 2012;14:112.
Miller DD, Amin MM, Palmer LB, et al. Aerosol delivery and
modern mechanical ventilation: in vitro/in vivo evaluation. Am J
Respir Crit Care Med. 2003;168:12051209.
Dhand R. Aerosol therapy during mechanical ventilation: getting
ready for prime time. Am J Respir Crit Care Med. 2003;168:
11481149.
Hughes J, Saez J. Effects of nebulizer mode and position in a
mechanical ventilator circuit on dose efficiency. Respir Care.
1987;32:11311135.
Sidler-Moix A, Dolci U, Gryllaki M, et al. Albuterol delivery
in an in vitro pediatric ventilator lung model: comparison of jet,
ultrasonic and mesh nebulizers. Pediatr Crit Care Med. 2013;14:
15.
Wan G, Lin H, Fink J, et al. In vitro evaluation of aerosol delivery
by different nebulization modes in pediatric and mechanical
ventilator modes. Respir Care. 2014;59:14941500.
Fink J, Dhand R. Aerosol therapy in mechanically ventilated
patients: recent advances and new techniques. Semin Respir Crit
Care Med. 2000;21:183201.
Dhand R, Tobin MJ. Bronchodilator delivery with metered-dose
inhalers in mechanically-ventilated patients. Eur Respir J. 1996;
9:585595.
Diot P, Morra L, Smaldone GC. Albuterol delivery in a model of
mechanical ventilation. Comparison of metered-dose inhaler and
nebulizer efficiency. Am J Respir Crit Care Med. 1995;152:
13911394.
Dhand R, Tobin MJ. Inhaled bronchodilator therapy in mechanically ventilated patients. Am J Respir Crit Care Med. 1997;
156:310.
Ari A, Areabi H, Fink JB. Evaluation of position of aerosol device
in two different ventilator circuits during mechanical ventilation.
Respir Care. 2010;55:837844.
Ari A, Atalay OT, Harwood R, et al. Influence of nebulizer type,
position, and bias flow on aerosol drug delivery in simulated
www.clinpulm.com |
85
Clinical Pulmonary Medicine
Ari and Fink
35.
36.
37.
38.
39.
pediatric and adult lung models during mechanical ventilation.
Respir Care. 2010;55:845851.
Ari A, Fink JB. Effective bronchodilator resuscitation of children
in the emergency room: device or interface? Respir Care.
2011;56:882885.
Duarte AG. Inhaled bronchodilator administration during mechanical ventilation. Respir Care. 2004;49:623634.
Dhand R. Basic techniques for aerosol delivery during mechanical
ventilation. Respir Care. 2004;49:611622.
Dhand R. Maximizing aerosol delivery during mechanical
ventilation: go with the flow and go slow. Intensive Care Med.
2003;29:10411042.
Dhand R, Guntur VP. How best to deliver aerosol medications
to mechanically ventilated patients. Clin Chest Med. 2008;29:
277296.
86 | www.clinpulm.com
Volume 22, Number 2, March 2015
40. Guerin C, Fassier T, Bayle F, et al. Inhaled bronchodilator
administration during mechanical ventilation: How to optimize it
and for which clinical benefit? J Aerosol Med. 2008;21:8595.
41. Manthous C, Hall C, Schmidt G, et al. Metered-dose inhaler versus
nebulized salbutamol in mechanically ventilated patients. Am Rev
Resp Dis. 1993;148:15671570.
42. Bates J, Rossi A, Milic-Emili J. Analysis of the behavior of the
respiratory system with constant inspiratory flow. J Appl Physiol.
1985;58:18401848.
43. Bates J, Milic-Emili J. The flow interruption technique for
measuring respiratory resistance. J Crit Care. 1991;6:227238.
44. Dhand R, Duarte A, Jubran A, et al. Dose response to
bronchodilator delivered by metered-dose inhaler in ventilator
supported patients. Am J Respir Crit Care Med. 1996;154:
388393.
Copyright
2015 Wolters Kluwer Health, Inc. All rights reserved.
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (894)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- NCP 106Document8 pagesNCP 106yer tagalajPas encore d'évaluation
- Community Acquired Pneumonia, A Case StudyDocument26 pagesCommunity Acquired Pneumonia, A Case StudyMenggay SanDiego57% (7)
- Hesi Study GuideDocument16 pagesHesi Study Guideangie10231100% (3)
- Cameron 2016Document11 pagesCameron 2016CarmePonsPas encore d'évaluation
- Difficult Intubation Guidelines OverviewDocument3 pagesDifficult Intubation Guidelines OverviewMaufer AlPas encore d'évaluation
- q1 Social CRMDocument17 pagesq1 Social CRMcésar_campos_45Pas encore d'évaluation
- Poku2016 Q1Document4 pagesPoku2016 Q1césar_campos_45Pas encore d'évaluation
- Gru Now 2013Document18 pagesGru Now 2013césar_campos_45Pas encore d'évaluation
- Aga en Uci 2015Document5 pagesAga en Uci 2015césar_campos_45Pas encore d'évaluation
- VM Prolongada JCC 2015Document7 pagesVM Prolongada JCC 2015césar_campos_45Pas encore d'évaluation
- Insulinoterapia JCC 2015Document6 pagesInsulinoterapia JCC 2015césar_campos_45Pas encore d'évaluation
- VM Seleccionando El Peep Correcto Cocc 2015Document8 pagesVM Seleccionando El Peep Correcto Cocc 2015césar_campos_45Pas encore d'évaluation
- Prognosis GuidelinesDocument103 pagesPrognosis GuidelinesPaola MedinaPas encore d'évaluation
- Hipercapnia, Relevancia Clinica y Mecanismos Cocc 2015Document6 pagesHipercapnia, Relevancia Clinica y Mecanismos Cocc 2015césar_campos_45Pas encore d'évaluation
- Aki Inducida Por Sepsis Cocc 2014Document8 pagesAki Inducida Por Sepsis Cocc 2014césar_campos_45Pas encore d'évaluation
- Vili Cocc 2015Document6 pagesVili Cocc 2015césar_campos_45Pas encore d'évaluation
- Dar o No Dar Fluidos 2012Document8 pagesDar o No Dar Fluidos 2012césar_campos_45Pas encore d'évaluation
- ViliDocument7 pagesVilicésar_campos_45Pas encore d'évaluation
- (Inglés) Guía Infusión Insulina para Manejo Hiperglicemia Pctes Críticos (2012)Document26 pages(Inglés) Guía Infusión Insulina para Manejo Hiperglicemia Pctes Críticos (2012)césar_campos_45Pas encore d'évaluation
- ARDS New Definition - Berlin ConsensusDocument8 pagesARDS New Definition - Berlin ConsensusAndreas IoannouPas encore d'évaluation
- Problems of The Neonate Low Birth Weight BabiesDocument25 pagesProblems of The Neonate Low Birth Weight BabiesmelbourneichrcPas encore d'évaluation
- Case Study of PneumoniaDocument8 pagesCase Study of PneumoniaAnne SedanzaPas encore d'évaluation
- MODULE L3A1 - Sample Weekly Home Learning Plans - MANDIA - TEAM DENNISDocument31 pagesMODULE L3A1 - Sample Weekly Home Learning Plans - MANDIA - TEAM DENNISBernardo Jose MandiaPas encore d'évaluation
- Mojoli 2023 Tidal Lung Hysteresis To Interpret PEEP-induced Changes in Compliance in ARDS PatientsDocument10 pagesMojoli 2023 Tidal Lung Hysteresis To Interpret PEEP-induced Changes in Compliance in ARDS PatientsKhanh Ha NguyenPas encore d'évaluation
- Respiration - Behavior of GasesDocument25 pagesRespiration - Behavior of GasesSodeinde SimeonPas encore d'évaluation
- Mechanical Ventilator Management ProtocolDocument3 pagesMechanical Ventilator Management ProtocolRick Frea100% (2)
- Foreign BodyDocument11 pagesForeign BodyVania Dwi AndhaniPas encore d'évaluation
- Mechanical Ventilation:: 2. Positive Pressure VentilatorDocument3 pagesMechanical Ventilation:: 2. Positive Pressure VentilatorMurad KhairoPas encore d'évaluation
- Acute Respiratory Distress SyndromeDocument2 pagesAcute Respiratory Distress SyndromemaraPas encore d'évaluation
- Practical 4 AssignmentDocument21 pagesPractical 4 AssignmentJamalulhaslina Binti FuadPas encore d'évaluation
- Acute Respiratory InfectionsDocument34 pagesAcute Respiratory InfectionssafiebuttPas encore d'évaluation
- Form 3 Chapter 1 QuestionsDocument11 pagesForm 3 Chapter 1 QuestionsCheah Foo Kit50% (2)
- Lightening Organs of FishDocument22 pagesLightening Organs of FishHeer SheikhPas encore d'évaluation
- Respiratory Anatomy Comparison Green Leatherback Sea TurtlesDocument1 pageRespiratory Anatomy Comparison Green Leatherback Sea TurtlesAldinaPas encore d'évaluation
- Chest Tubes and ThoracentesisDocument18 pagesChest Tubes and ThoracentesisecleptosPas encore d'évaluation
- Neonatal 2Document37 pagesNeonatal 2Mateen Shukri100% (1)
- How animals survive and adapt to their environmentsDocument25 pagesHow animals survive and adapt to their environmentsLean Cristian LlobreraPas encore d'évaluation
- 3 Infeksi Saluran Pernafasan Akut (ISPA) PediatricsDocument35 pages3 Infeksi Saluran Pernafasan Akut (ISPA) PediatricsCharisma Tiara RessyaPas encore d'évaluation
- Jamb Biology Past Questions UnibenpagesDocument51 pagesJamb Biology Past Questions UnibenpagesEhigie promisePas encore d'évaluation
- Breathing Techniques For ExerciseDocument5 pagesBreathing Techniques For ExerciseHamilton DurantPas encore d'évaluation
- Nurse sees post-op appendectomy client first after endorsementDocument9 pagesNurse sees post-op appendectomy client first after endorsementMishia Renee EchonPas encore d'évaluation
- Disease ProjectDocument18 pagesDisease Projectapi-293515530Pas encore d'évaluation
- Respiratory Gas ExchangeDocument8 pagesRespiratory Gas ExchangeJohn SorianoPas encore d'évaluation
- Acute Respiratory Failure Pa Tho PhysiologyDocument4 pagesAcute Respiratory Failure Pa Tho Physiologyroseanne18100% (4)
- Respiratory System Insects 2Document4 pagesRespiratory System Insects 2KIPNGETICH FREDRICKPas encore d'évaluation
- ER RT ConsultDocument3 pagesER RT ConsultRobert BeatyPas encore d'évaluation
- Teaching Plan CopdDocument11 pagesTeaching Plan CopdMary Grace AgataPas encore d'évaluation