Académique Documents
Professionnel Documents
Culture Documents
Emotion Review 2012 Blair 133 8
Transféré par
Anca PrajanuCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Emotion Review 2012 Blair 133 8
Transféré par
Anca PrajanuDroits d'auteur :
Formats disponibles
Emotion Review
http://emr.sagepub.com/
A Cognitive Neuroscience Approach to Generalized Anxiety Disorder and Social Phobia
Karina S. Blair and R. J. R. Blair
Emotion Review 2012 4: 133
DOI: 10.1177/1754073911430251
The online version of this article can be found at:
http://emr.sagepub.com/content/4/2/133
Published by:
http://www.sagepublications.com
On behalf of:
International Society for Research on Emotion
Additional services and information for Emotion Review can be found at:
Email Alerts: http://emr.sagepub.com/cgi/alerts
Subscriptions: http://emr.sagepub.com/subscriptions
Reprints: http://www.sagepub.com/journalsReprints.nav
Permissions: http://www.sagepub.com/journalsPermissions.nav
Citations: http://emr.sagepub.com/content/4/2/133.refs.html
>> Version of Record - Apr 27, 2012
What is This?
Downloaded from emr.sagepub.com by ancuta anca on October 25, 2014
430251
EMR
A Cognitive Neuroscience Approach to Generalized
Anxiety Disorder and Social Phobia
Emotion Review
Vol. 4, No. 2 (April 2012) 133138
The Author(s) 2012
ISSN 1754-0739
DOI: 10.1177/1754073911430251
er.sagepub.com
Karina S. Blair
R. J. R. Blair
Mood & Anxiety Program, National Institute of Mental Health, National Institutes of Health, Department of Health and Human Services, USA
Abstract
Generalized anxiety disorder (GAD) and social phobia (SP) are major anxiety disorders identified by the Diagnostic and Statistical
Manual of Mental Disorders, 4th edition (DSM-IV). They are comorbid, overlap in symptoms, yet present with distinct features
(worry in GAD and fear of embarrassment in SP). Both have also been explained in terms of conditioning-based models. However,
there is little reasoning currently to believe that GAD in adulthood reflects heightened conditionability or heightened threat
processingthough patients with SP may show heightened processing of social threat stimuli. Moreover, the computational
architectures that maintain these disorders in adulthood are different. For GAD this may reflect the development of an inefficient
worrying strategy of emotional regulation. For SP this appears to reflect the atypical processing of self-referential information.
Keywords
conditioning, emotion regulation, generalized anxiety disorder, social phobia, social threat processing
Generalized anxiety disorder (GAD) and social phobia (SP) are
two highly prevalent, chronic, and disabling anxiety disorders
that are sometimes comorbid. They show some indications of
symptom overlap; for example, increased tension and thoughts
of future threat (Craske et al., 2009). However, GAD is specifically characterized by persistent and excessive worry about life
or the welfare of loved ones that is difficult to control and causes
significant distress. SP is marked by acute anxiety to social or
performance situations, related to the concern of scrutiny, or
humiliation, by others. There have been claims that a similar
neural, and presumably computational, architecture mediates
all anxiety disorders (e.g., Martin, Ressler, Binder, & Nemeroff,
2010). The current article, taking a cognitive neuroscience
perspective, suggests that this view requires modification.
GAD from a Cognitive Neuroscience
Perspective
Conditioning-based accounts have been proposed for the pathogenesis of anxiety disorders for most of the last century (Watson
& Rayner, 1920). The suggestion is that pathological anxiety
develops through classical conditioning; the individual experiences
an aversive unconditioned stimulus (US) that is associated with
an event/experience that becomes the focus of the individuals
anxiety. GAD might therefore reflect a heightened propensity
for aversive conditioning and the development of anxiety
towards a variety of stimuli. In line with this, and on the basis
of a meta-analysis of the literature, Lissek et al. concluded that
anxiety-disordered adults showed atypical conditioning (2005).
But only two studies have examined conditioning in patients
with GAD (Pitman & Orr, 1986; Thayer, Friedman, Borkovec,
Johnsen, & Molina, 2000). The first did indicate increased
responsiveness to the conditioned stimulus (CS+) in the patients
with GAD (Pitman & Orr, 1986). However, over 50% of the
patients with GAD also presented with panic disorder and it is
thus unclear whether the enhanced conditionability reflects GAD
or panic disorder. The second involved dot cues anticipating
either threat or neutral words and conditioned heart rate deceleration as the indexed conditioned response (Thayer et al., 2000).
However, this study is difficult to interpret as this conditioned
response was not shown by the healthy comparison individuals.
Moreover, the results of a third study are relevant. This study
examined the impact on startle reflex of cues which were either:
(a) predictive of aversive stimuli; (b) associated with aversive
Corresponding author: Karina S. Blair, Mood & Anxiety Program, National Institute of Mental Health, 15K North Drive, MSC 2670, Bethesda, MD 20892, USA.
Email: peschark@mail.nih.gov
Downloaded from emr.sagepub.com by ancuta anca on October 25, 2014
134 Emotion Review Vol. 4 No. 2
stimuli that were administered unpredictably; or (c) predictive of
the absence of aversive stimuli (Grillon et al., 2009). Across conditions, patients with GAD (and unlike patients with posttraumatic stress disorder [PTSD]) showed no differences from
control participants in the impact of these cues on startle reflex. If
heightened conditionability was associated with GAD, patients
with GAD should have shown an increased startle reflex following cues predictive of aversive stimuli. Yet this was not seen.
Relatedly, studies have examined the physiological
response of patients with GAD to aversive stimuli. These studies have shown either reduced, or not significantly increased,
physiological arousal in patients with GAD (Grillon et al.,
2009; Hoehn-Saric, McLeod, & Zimmerli, 1989). Similarly,
studies have examined the response of the amygdala to
emotional stimuli in patients with GAD using fMRI. Studies
with pediatric patients have indicated hyperactivity to negative emotional expression faces in GAD (McClure et al., 2007;
Monk et al., 2008); however, in contrast, three out of four
studies with adult patients have not (Blair, Shaywitz et al.,
2008; Palm, Elliott, McKie, Deakin, & Anderson, 2011;
Whalen et al., 2008). The fourth, which did find increased
amygdala response to fearful expressions in patients with
GAD, also reported increased amygdala responses to happy
expressionssuggestive of generally increased emotional
responsiveness rather than a threat-specific hyper-responsiveness (Etkin, Prater, Hoeft, Menon, & Schatzberg, 2010). A
fifth study also found no significant increased amygdala
response to the anticipation/receipt of threatening images
(though the patients with GAD did show heightened amygdala
responses to the anticipation/receipt of neutral images;
Nitschke et al., 2009). In short, currently, the literature does
not support the suggestion of heightened threat conditioning
or threat sensitivity in at least adults with GAD.
The hallmark feature of GAD is an increased propensity to
worry. It has been argued that patients with GAD resort to
worry because of an underlying abnormality in emotional regulation (Mennin, Holaway, Fresco, Moore, & Heimberg, 2007).
Imaging studies implicate a network of brain regions in both
explicit emotional regulation, where subjects are told to reduce
their emotional response (Ochsner et al., 2004), and implicit
emotional regulation, where subjects must perform attentiondemanding tasks that lead to reductions in the emotional
response (Blair et al., 2007; Pessoa, McKenna, Gutierrez, &
Ungerleider, 2002). These include lateral frontal, dorsal anterior cingulate (dACC), and parietal cortices (Ochsner et al.,
2004). These regions are implicated in topdown attention
which is thought to facilitate attention allocation to nonemotional stimulus features in both explicit and implicit tasks. In
both types of tasks, following attention theory (Desimone &
Duncan, 1995), increased attention allocation to nonemotional stimulus features should reduce representation of emotional stimulus features and consequently reduce the emotional
response.
Only two studies have investigated emotional regulation in
patients with GAD (Blair et al., under review; Etkin et al.,
2010). Etkin et al. (2010) found reduced implicit emotional
regulation and reduced regulatory activity within pregenual
anterior cingulate in patients with GAD. Blair et al. (under
review) observed reduced recruitment of dACC and parietal cortices in the patients with GAD during both implicit and explicit
emotional-regulation tasks. These data suggest that a reduced
capacity for emotional regulation might be a risk factor for the
emergence of GAD. However, it should be noted that Blair found
that this reduced recruitment of dACC and partietal cortices was
also seen in patients with SP. Moreover, other work has also
reported reduced recruitment of these regions in explicit emotional-regulation tasks in patients with SP (Goldin, Manber,
Hakimi, Canli, & Gross, 2009; Goldin, Manber-Ball, Werner,
Heimberg, & Gross, 2009). As such, dysfunctional emotional
regulation does not appear to be a specific risk factor for GAD,
but rather a more general risk factor for the development of (at
least these forms of) anxiety disorders.
Attention-based models of anxiety have also been suggested. It has been argued that anxious individuals initially
show rapid orienting of attention toward and engagement in/
difficulty disengaging from threat stimuli. This is then
followed by the eventual direction of attention away from
the threat in an effort to reduce subjective distress (Mogg &
Bradley, 2002). It is hypothesized that this vigilanceavoidance
pattern of cognitive bias is maladaptive because it enhances
sensitization and interferes with habituation, thereby maintaining anxiety (Mogg & Bradley, 2002). In line with this
view, both pediatric and adult patients with GAD have been
found to show attentional bias towards threat words and
angry faces (Bradley, Mogg, White, Groom, & de Bono, 1999;
Waters, Mogg, Bradley, & Pine, 2008), though attentional
biases away from angry faces have also been reported in
pediatric patients with GAD (e.g., Waters et al., 2008, in less
anxious patients with GAD).
A complication should be considered, however. How is this
heightened attention to threat being mediated? Emotional
attention is generally considered to reflect the interaction of the
amygdala and cortical regions (Blair et al., 2007; Pessoa &
Ungerleider, 2004). As the connections between temporal cortex and the amygdala are reciprocal (Amaral, Price, Pitkanen,
& Carmichael, 1992), the activity of neurons representing
emotional stimuli in temporal cortex is further augmented
by reciprocal feedback from the amygdala. By this account,
emotional stimuli are more likely to be attended to because
they are more likely to win the competition for representation
(Desimone & Duncan, 1995), because of the feedback from
the amygdala.
Functional magnetic resonance imaging studies have indicated amygdala hyperactivity related to negative emotional
expression faces in pediatric GAD (McClure et al., 2007; Monk
et al., 2008); however, four studies with adult GAD, consistent
with the physiological literature (Grillon et al., 2009; HoehnSaric et al., 1989), have not (Blair, Shaywitz et al., 2008;
Nitschke et al., 2009; Palm et al., 2011; Whalen et al., 2008). The
inconsistency between the pediatric and adult literature regarding responsiveness to threatening stimuli in patients with GAD
could reflect that GAD in adulthood reflects an accommodation
Downloaded from emr.sagepub.com by ancuta anca on October 25, 2014
Blair & Blair Generalized Anxiety Disorder and Social Phobia 135
to the increased responsiveness that was present when the
patients were children. As such, GAD should not be considered
an increased responsiveness to threat stimuli (this is particularly
the case since increased responsiveness to threatening facial
stimuli is seen in pediatric patients with SP who do not present
with GAD; see following lines). Rather GAD might reflect an
accommodation to this increased responsiveness to threatening
stimuli that, while pathological, is at least successful in negating
the original phenomena. In short, increased responsiveness to
threat might be a nonspecific risk factor that can, but need not,
lead to the development of GAD.
In this regard it is worth briefly returning to a consideration
of worry. As noted above, an increased propensity to worry is
the hallmark feature of GAD. As such, to understand GAD we
probably need to understand worry.
Worry has been thought to reflect an overlearned compensatory strategy for dulling emotional experience (Borkovec,
Alcaine, & Behar, 2004). However, excessive worry does not
solve objective and subjective difficulties; worrying people do
not plan complex responses to overwhelming events but rather
repeat to themselves that things will get worse (Paulesu et al.,
2010). Unfortunately, very little work has been conducted on
worry from a cognitive perspective and only two studies (both
with very small sample sizes) have investigated worry in
patients with GAD using fMRI (Hoehn-Saric, Schlund, &
Wong, 2004; Paulesu et al., 2010). Both implicated prefrontal
regions, but the regions implicated were not mutually consistent
and no computational account of worry has yet been offered.
In summary, neither heightened conditionability nor heightened threat sensitivity is likely to maintain GAD as the current
literature indicates that neither is heightened in adult patients.
However, heightened generalized threat sensitivity may play a
role in the initial development of the disorder given the literature
on youth with GAD. It is possible that this heightened generalized threat sensitivity in an individual with a reduced capacity
for emotional regulation may lead to the development of worry
(as noted, an overlearned compensatory strategy for dulling
emotional experience [Borkovec et al., 2004]). While the computational processes involved in worry remain unspecified, part
of these processes, or their consequences, likely reflect internally
driven priming of representations of potential threat. Such
priming may lead to greater and stronger semantic representations of these threats, increasing their capacity to win the competition for representation; that is, increasing their capacity to
become the focus of attention. Of course, these speculations are
very preliminary but they are currently guiding our research.
SP from a Cognitive Neuroscience Perspective
Conditioning-based theories have also been offered for SP.
Phobias have been thought to potentially reflect hypersensitivity
in the pathways that mediate innate fear. This argument has also
been made for SP (cf. Milad & Rauch, 2007), though it rests on
the assumption that social stimuli are innately fear inducing.
Three studies have examined aversive conditioning in
patients with SP (Hermann, Ziegler, Birbaumer, & Flor, 2002;
Schneider et al., 1999; Veit et al., 2002). All reported heightened
conditioning in the disorder. Moreover, patients with SP show
greater amygdala responses whilst associating neutral facial
expressions with aversive stimuli (Schneider et al., 1999).
However, some caveats should be considered.
First, these data indicate that SP is associated with a greater
preparedness to associate aversive outcomes with social stimuli rather than necessarily an increased innate fear of social
threat. To conclude the latter, we have to assume that neutral
facial expressions are innate social threats. Perhaps they are.
There are reports that neutral expressions activate the amygdala and we could assume that the amygdala is a component of
the innate response to social threat (Murphy, Nimmo-Smith, &
Lawrence, 2003). But if neutral expressions were innate social
threats and patients with SP show an increased innate fear of
social threat, we should predict that patients with SP will show
enhanced amygdala responses to neutral expressions. However,
children and adults with SP typically do not (Blair, Shaywitz
et al., 2008; Phan, Fitzgerald, Nathan, & Tancer, 2006; Stein,
Goldin, Sareen, Zorrilla, & Brown, 2002; Straube, Mentzel, &
Miltner, 2005; but see Birbaumer et al., 1998; Cooney, Atlas,
Joormann, Eugene, & Gotlib, 2006).
Second, all three studies used face stimuli as the conditioned
stimulus (CS). As such, the literature cannot disentangle
whether the effects represent a general propensity for increased
condition-ability or a specific propensity to condition towards
social stimuli. In this regard, however, it is worth considering
the literature on threat responsiveness in SP. Thus, fMRI work
has indicated heightened amygdala and temporal cortical
activity to angry (Evans et al., 2008; Phan et al., 2006; Stein et
al., 2002; Straube, Kolassa, Glauer, Mentzel, & Miltner, 2004;
Straube et al., 2005) and fearful expressions in SP (Blair,
Geraci, Korelitz et al., 2011; Blair, Shaywitz et al., 2008; but
see Stein et al., 2002). In contrast, patients with SP do not
appear to show an increased amygdala (Goldin, Manber-Ball,
et al., 2009) or physiological response (McTeague et al., 2009)
to physical threat. As such, we assume that SP does reflect a
specific propensity to condition towards social stimuli.
In this regard, it is worth noting that there are significant
disadvantages with respect to using facial expression stimuli
to understanding SP. Thus, while facial expression stimuli
serve as reinforcers (happy expressions increase the probability of the repetition of actions that elicited them while fearful/
sad expressions decrease this probability; see Blair, 2003),
they may be either primary, innately specified unconditioned
stimuli or learnt, secondary reinforcers/conditioned stimuli or
both. In other words, the heightened amygdala responses to
angry expressions in SP may reflect: (a) an innately specified
hyper-sensitivity to this expression; (b) heightened learning of
an association between aversive experiences and this expression; or (c) both. It is thus important to determine whether
patients with SP show heightened amygdala responses to
socially aversive experiences that are unlikely to be innately
specified aversive social unconditioned stimuli. In this regard,
several studies have investigated the response of patients with
SP to anticipated public speaking. Of these, two have reported
Downloaded from emr.sagepub.com by ancuta anca on October 25, 2014
136 Emotion Review Vol. 4 No. 2
increased amygdalahippocampal and temporal cortical
activity in the patients with SP (Lorberbaum et al., 2004;
Tillfors, Furmark, Marteinsdottir, & Fredrikson, 2002). Two
others did not (Nakao et al., 2011; van Ameringen et al., 2004).
However, both of these studies involved very small sample
sizes (5/6 patients with SP) and may not have had sufficient
power to detect group differences. In short, patients with SP
show heightened amygdala responses to socially aversive
experiences that are unlikely to be innately specified aversive
social unconditioned stimuli.
But is SP only a heightened propensity to condition towards
social stimuli? A core concern in SP is the fear of being negatively evaluated. These data have led to the suggestion that
disordered self-referential processing, relating to dysfunctional medial prefrontal cortex activity (MPFC), is a core component of this disorder. This was first suggested by Blair,
Geraci et al. (2008) in an fMRI study where patients were
assessed when processing self- versus other-referential criticism (e.g., Youre ugly vs. Hes ugly) and praise (e.g.,
Youre beautiful vs. Hes beautiful). This study revealed
selectively increased blood oxygen level dependent (BOLD)
responses within both the amygdala and a dorsal/lateral region
of MPFC in patients with SP to self-referential criticism. Since
then a series of studies have examined issues related to selfreferential processing in patients with SP. Thus, patients with
SP have been found to show increased amygdala responses to
self-referential statements (Blair, Geraci, Majestic, et al.,
2011), in anticipation of self-referential comments (Guyer
et al., 2008) and to negative self-beliefs (Goldin et al., 2009).
With respect to MPFC, regions proximal to the dorsal/lateral
region of MPFC noted by Blair, Geraci et al. (2008) were
identified in the context of the group main effects in two further
studies (Blair et al., 2010; Blair, Geraci, Majestic et al. 2011).
Patients with SP showed increased activity within these regions
for self-referential statements irrespective of valence and when
processing intentional, unintentional (embarrassment inducing)
and normative social interaction vignettes. But ventromedial
prefrontal cortex (VMPFC), also implicated in self-referential
processing (Northoff et al., 2006), is important. Patients with SP
have shown heightened VMPFC responses in anticipation of
self-referential comments (Guyer et al., 2008) and to negative
self-beliefs (Goldin, Manber-Ball, et al., 2009).
Recent work has potentially clarified the basis of this atypical
VMPFC activity in patients with SP. Blair et al. (2010) involved
the subjects processing intentional and unintentional (embarrassing) conventional (social disorder-based) transgressions.
Previous work with this paradigm, replicated by Blair et al.
(2010), demonstrated that healthy individuals show significantly greater activity to intentional relative to unintentional
conventional social transgressions (Berthoz, Armony, Blair, &
Dolan, 2002). This response is thought to reflect heightened
representation of the protagonists intent to challenge the
social order (Berthoz et al., 2002). However, adults with SP
showed a notably different pattern; increased activity to the
unintentional relative to intentional social transgressions. In a
second study, Blair, Geraci, Majestic et al. (2011) examined the
response of patients with SP and comparison individuals to own
(first person; e.g., Im ugly) or other individuals (second person; e.g., Youre ugly) negative, positive, and neutral opinions
about the self. They found that healthy comparison adults
showed an increased activation to first (I) relative to second
(You) viewpoints within VMPFC. In contrast, however, the
patients with SP showed significantly greater activation to
You relative to I comments.
Taken together, these data suggest a profound reorganization
of self-referential reasoning in SP. While a detailed computational
account of self-referential reasoning remains to be provided, it
appears to involve matching information to the individuals selfconcept (Berthoz et al., 2002). For healthy individuals this
appears to be particularly related to the potential status challenges
indicated by intentional social transgressions and self-generated
viewpoints (am I really like this?). In contrast, evaluations of
the self in SP primarily focus on potentially embarrassing events
and are particularly related to others viewpoints (am I really like
what this other person considers me to be?).
In summary, SP does appear to reflect a heightened propensity to condition towards social stimuli even if it is unclear, and
perhaps even doubtful, that this reflects hypersensitivity in the
pathways that mediate the innate fear of social stimuli. But SP,
at least by adulthood, is not simply this. SP also appears to be
associated with atypical processing of self-referential information and it is this impairment that likely leads to the patients
crippling concerns about potential embarrassment.
Conclusion
GAD and SP are two highly comorbid anxiety disorders, and
similar computational architectures have been proposed for
them. However, more recent data suggest that there are notable
differences in the computational impairments associated with
these disorders. For example, there is little reason, currently, to
believe that GAD in adulthood reflects heightened conditionability or heightened threat processing. In contrast, SP may
reflect such heightened threat processing, albeit only for social
stimuli.
Both disorders may share developmental risk factors, however. GAD may be associated with heightened conditionability/
threat processing in childhood and both are associated with a
deficient capacity to engage in emotional regulation. It is the
computational architectures that maintain these disorders in
adulthood that are different. For GAD this may reflect the
development of an inefficient worrying strategy of emotional
regulation (though we are clearly some way from understanding
this phenomenon). For SP this appears to reflect the atypical
processing of self-referential information.
References
Amaral, D. G., Price, J. L., Pitkanen, A., & Carmichael, S. T. (1992).
Anatomical organization of the primate amygdaloid complex. In J. P.
Aggleton (Ed.), The amygdala: Neurobiological aspects of emotion,
memory, and mental dysfunction (pp. 166). New York, NY: Wiley.
Berthoz, S., Armony, J., Blair, R. J. R., & Dolan, R. (2002). Neural correlates of violation of social norms and embarrassment. Brain, 125,
16961708.
Downloaded from emr.sagepub.com by ancuta anca on October 25, 2014
Blair & Blair Generalized Anxiety Disorder and Social Phobia 137
Birbaumer, N., Grodd, W., Diedrich, O., Klose, U., Erb, M., Lotze, M.,
... Flor, H. (1998). fMRI reveals amygdala activation to human faces in
social phobics. Neuroreport, 9, 12231226.
Blair, K. S., Geraci, M., DeVido, J., McCaffrey, D., Vythilingam, M., Ng,
P., ... Pine, D. S. (2008). Neural response to self- and other referential
praise and criticism in Generalized Social Phobia. Archives of General
Psychiatry, 65, 11761184.
Blair, K. S., Geraci, M., Hollon, N., Otero, M., DeVido, J., Majestic, C.,
... Pine, D. S. (2010). Social norm processing in adult social phobia:
Atypically increased ventromedial frontal cortex responsiveness to
unintentional (embarrassing) transgressions. The American Journal of
Psychiatry, 167, 15261532.
Blair, K. S., Geraci, M., Korelitz, K., Otero, M., Towbin, K., Ernst, M., ...
Pine, D. S. (2011). The pathology of social phobia is independent of
developmental changes in face processing. American Journal of Psychiatry, 168, 12021209.
Blair, K. S., Geraci, M., Majestic, K., Odenheimer, S., Jacobs, M., Blair,
R. J. R., & Pine, D. S. (2011). Atypical modulation of medial prefrontal cortex to self-referential comments in generalized social phobia.
Psychiatry Research, 193, 3845.
Blair, K. S., Shaywitz, J., Morton, J., Smith, B. W., Rhodes, R., Geraci, M.,
... Blair, R. J. R. (2008). Response to emotional expressions in generalized social phobia (GSP) and generalized anxiety disorder (GAD):
Evidence for separate disorders. The American Journal of Psychiatry,
165, 11931202.
Blair, K. S., Smith, B. W., Hollon, N., Geraci, M., DeVido, J., Otero, M.,
et al. Reduced dorsal anterior cingulate cortical activity during emotional regulation and top-down attentional control in Generalized
Social Phobia (GSP), Generalized Anxiety Disorder (GAD) and
comorbid GSP/GAD. Under review.
Blair, K. S., Smith, B. W., Morton, J., Mitchell, D. G., Vythilingam, M.,
Pessoa, L., ... Blair, R. J. R. (2007). Modulation of emotion by cognition and cognition by emotion. Neuroimage, 35, 430440.
Blair, R. J. R. (2003). Facial expressions, their communicatory functions
and neuro-cognitive substrates. Philosophical Transactions of the
Royal Society of London B: Biological Sciences, 358, 561572.
Borkovec, T. D., Alcaine, O., & Behar, E. (2004). Avoidance theory of
worry and generalized anxiety disorder. In R. G. Heimberg, C. L. Turk
& D. S. Mennin (Eds.), Generalized anxiety disorder: Advances in
theory and practice (pp. 77108). New York, NY: Guilford Press.
Bradley, B. P., Mogg, K., White, J., Groom, C., & de Bono, J. (1999).
Attentional bias for emotional faces in generalized anxiety disorder.
British Journal of Clinical Psychology, 38, 267278.
Cooney, R. E., Atlas, L. Y., Joormann, J., Eugene, F., & Gotlib, I. H. (2006).
Amygdala activation in the processing of neutral faces in social anxiety
disorder: Is neutral really neutral? Psychiatry Research, 148, 5559.
Craske, M. G., Rauch, S. L., Ursano, R., Prenoveau, J., Pine, D. S., &
Zinbarg, R. E. (2009). What is an anxiety disorder? Depression and
Anxiety, 26, 10661085.
Desimone, R., & Duncan, J. (1995). Neural mechanisms of selective visual
attention. Annual Review of Neuroscience, 18, 193222.
Etkin, A., Prater, K. E., Hoeft, F., Menon, V., & Schatzberg, A. F. (2010).
Failure of anterior cingulate activation and connectivity with the
amygdala during implicit regulation of emotional processing in generalized anxiety disorder. The American Journal of Psychiatry, 167,
545554.
Evans, K. C., Wright, C. I., Wedig, M. M., Gold, A. L., Pollack, M. H., &
Rauch, S. L. (2008). A functional MRI study of amygdala responses
to angry schematic faces in social anxiety disorder. Depression and
Anxiety, 25, 496505.
Goldin, P. R., Manber, T., Hakimi, S., Canli, T., & Gross, J. J. (2009).
Neural bases of social anxiety disorder: Emotional reactivity and
cognitive regulation during social and physical threat. Archives of
General Psychiatry, 66, 170180.
Goldin, P. R., Manber-Ball, T., Werner, K., Heimberg, R., & Gross, J. J.
(2009). Neural mechanisms of cognitive reappraisal of negative
self-beliefs in social anxiety disorder. Biological Psychiatry, 66,
10911099.
Grillon, C., Pine, D. S., Lissek, S., Rabin, S., Bonne, O., & Vythilingam, M.
(2009). Increased anxiety during anticipation of unpredictable aversive
stimuli in posttraumatic stress disorder but not in generalized anxiety
disorder. Biological Psychiatry, 66, 4753.
Guyer, A. E., Lau, J.Y., McClure-Tone, E. B., Parrish, J., Shiffrin, N. D.,
Reynolds, R. C., . . . Nelson, E. E. (2008). Amygdala and ventrolateral
prefrontal cortex function during anticipated peer evaluation in pediatric social anxiety. Archives of General Psychiatry, 65, 13031312.
Hermann, C., Ziegler, S., Birbaumer, N., & Flor, H. (2002). Psychophysiological and subjective indicators of aversive pavlovian conditioning in
generalized social phobia. Biological Psychiatry, 52, 328337.
Hoehn-Saric, R., McLeod, D. R., & Zimmerli, W. D. (1989). Somatic manifestations in women with generalized anxiety disorder. Psychophysiological responses to psychological stress. Archives of General Psychiatry,
46, 11131119.
Hoehn-Saric, R., Schlund, M. W., & Wong, S. H. (2004). Effects of
citalopram on worry and brain activation in patients with generalized
anxiety disorder. Psychiatry Research, 131, 1121.
Lissek, S., Powers, A. S., McClure, E. B., Phelps, E. A., Woldehawariat,
G., Grillon, C., & Pine, D. S. (2005). Classical fear conditioning in the
anxiety disorders: A meta-analysis. Behavior Research and Therapy,
43, 13911424.
Lorberbaum, J. P., Kose, S., Johnson, M. R., Arana, G. W., Sullivan, L. K.,
Hamner, M. B., ... George, M. S. (2004). Neural correlates of speech
anticipatory anxiety in generalized social phobia. Neuroreport, 15,
27012705.
Martin, E. I., Ressler, K. J., Binder, E., & Nemeroff, C. B. (2010). The
neurobiology of anxiety disorders: Brain imaging, genetics, and
psychoneuroendocrinology. Clinics in Laboratory Medicine, 30,
865891.
McClure, E. B., Monk, C. S., Nelson, E. E., Parrish, J. M., Adler, A., Blair,
R. J., ... Pine, D. S. (2007). Abnormal attention modulation of fear
circuit function in pediatric generalized anxiety disorder. Archives of
General Psychiatry, 64, 97106.
McTeague, L. M., Lang, P. J., Laplante, M. C., Cuthbert, B. N., Strauss,
C. C., & Bradley, M. M. (2009). Fearful imagery in social phobia:
Generalization, comorbidity, and physiological reactivity. Biological
Psychiatry, 65, 374382.
Mennin, D. S., Holaway, R. M., Fresco, D. M., Moore, M. T., & Heimberg,
R. G. (2007). Delineating components of emotion and its dysregulation
in anxiety and mood psychopathology. Behavior Therapy, 38, 284302.
Milad, M. R., & Rauch, S. L. (2007). The role of the orbitofrontal cortex in
anxiety disorders. Annals of the New York Academy of Sciences, 1121,
546561.
Mogg, K., & Bradley, B. P. (2002). Selective orienting of attention to
masked threat faces in social anxiety. Behavior Research and Therapy,
40, 14031414.
Monk, C. S., Telzer, E. H., Mogg, K., Bradley, B. P., Mai, X., Louro, H. M.
C., ... Pine, D. S. (2008). Amygdala and ventromedial prefrontal cortex
activation to masked angry faces in children and adolescents with generalized anxiety disorder. Archives of General Psychiatry, 65, 56876.
Murphy, F. C., Nimmo-Smith, I., & Lawrence, A. D. (2003). Functional
neuroanatomy of emotions: A meta-analysis. Cognitive, Affective, &
Behavioral Neuroscience, 3, 207233.
Nakao, T., Sanematsu, H., Yoshiura, T., Togao, O., Murayama, K., Tomita,
M., ... Kanba, S. (2011). fMRI of patients with social anxiety disorder
during a social situation task. Neuroscience Research, 69, 6772.
Nitschke, J. B., Sarinopoulos, I., Oathes, D. J., Johnstone, T., Whalen, P. J.,
Davidson, R. J., & Kalin, N. H. (2009). Anticipatory activation in the
amygdala and anterior cingulate in generalized anxiety disorder and
Downloaded from emr.sagepub.com by ancuta anca on October 25, 2014
138 Emotion Review Vol. 4 No. 2
prediction of treatment response. The American Journal of Psychiatry,
166, 302310.
Northoff, G., Heinzel, A., de Greck, M., Bermpohl, F., Dobrowolny, H.,
& Panksepp, J. (2006). Self-referential processing in our brain
A meta-analysis of imaging studies on the self. Neuroimage, 31,
440457.
Ochsner, K. N., Ray, R. D., Cooper, J. C., Robertson, E. R., Chopra, S.,
Gabrieli, J. D., & Gross, J. J. (2004). For better or for worse: Neural
systems supporting the cognitive down- and up-regulation of negative
emotion. Neuroimage, 23, 483499.
Palm, M. E., Elliott, R., McKie, S., Deakin, J. F. W., & Anderson, I. M.
(2011). Attenuated responses to emotional expressions in women with
generalized anxiety disorder. Psychological Medicine, 41, 10091018.
Paulesu, E., Sambugaro, E., Torti, T., Danelli, L., Ferri, F., Scialfa, G., ...
Sassaroli, S. (2010). Neural correlates of worry in generalized anxiety
disorder and in normal controls: A functional MRI study. Psychological Medicine, 40, 117124.
Pessoa, L., McKenna, M., Gutierrez, E., & Ungerleider, L. G. (2002).
Neural processing of emotional faces requires attention. Proceedings
of the National Academy of Sciences USA, 99, 1145811463.
Pessoa, L., & Ungerleider, L. G. (2004). Neuroimaging studies of attention and the processing of emotion-laden stimuli. Progress in Brain
Research, 144, 171182.
Phan, K. L., Fitzgerald, D. A., Nathan, P. J., & Tancer, M. E. (2006). Association between amygdala hyperactivity to harsh faces and severity of
social anxiety in generalized social phobia. Biological Psychiatry, 59,
424429.
Pitman, R. K., & Orr, S. P. (1986). Test of the conditioning model of neurosis: Differential aversive conditioning of angry and neutral facial expressions in anxiety disorder patients. Journal of Abnormal Psychology, 95,
208213.
Schneider, F., Weiss, U., Kessler, C., Muller-Gartner, H. W., Posse, S.,
Salloum, J. B., ... Birbaumer, N. (1999). Subcortical correlates of
differential classical conditioning of aversive emotional reactions in
social phobia. Biological Psychiatry, 45, 863871.
Stein, M. B., Goldin, P. R., Sareen, J., Zorrilla, L. T., & Brown, G. G.
(2002). Increased amygdala activation to angry and contemptuous
faces in generalized social phobia. Archives of General Psychiatry, 59,
10271034.
Straube, T., Kolassa, I. T., Glauer, M., Mentzel, H. J., & Miltner, W. H.
(2004). Effect of task conditions on brain responses to threatening
faces in social phobics: An event-related functional magnetic resonance
imaging study. Biological Psychiatry, 56, 921930.
Straube, T., Mentzel, H. J., & Miltner, W. H. (2005). Common and distinct brain activation to threat and safety signals in social phobia.
Neuropsychobiology, 52, 163168.
Thayer, J. F., Friedman, B. H., Borkovec, T. D., Johnsen, B. H., & Molina,
S. (2000). Phasic heart period reactions to cued threat and nonthreat stimuli in generalized anxiety disorder. Psychophysiology, 37,
361368.
Tillfors, M., Furmark, T., Marteinsdottir, I., & Fredrikson, M. (2002). Cerebral blood flow during anticipation of public speaking in social phobia:
A PET study. Biological Psychiatry, 52, 11131119.
van Ameringen, M., Mancini, C., Szechtman, H., Nahmias, C., Oakman, J.
M., Hall, G. B., ... Farvolden, P. (2004). A PET provocation study of
generalized social phobia. Psychiatry Research, 132, 1318.
Veit, R., Flor, H., Erb, M., Hermann, C., Lotze, M., Grodd, W., &
Birbaumer, N. (2002). Brain circuits involved in emotional learning
in antisocial behavior and social phobia in humans. Neuroscience
Letters, 328, 233236.
Waters, A. M., Mogg, K., Bradley, B. P., & Pine, D. S. (2008). Attentional
bias for emotional faces in children with generalized anxiety disorder.
Journal of the American Academy of Child & Adolescent Psychiatry,
47, 435442.
Watson, J. B., & Rayner, R. (1920). Conditioned emotional reactions.
Journal of Experimental Psychology, 3, 114.
Whalen, P. J., Johnstone, T., Somerville, L. H., Nitschke, J. B., Polis, S.,
Alexander, A. L., ... Kalin, N. H. (2008). A functional magnetic
resonance imaging predictor of treatment response to venlafaxine in
generalized anxiety disorder. Biological Psychiatry, 63, 858863.
Downloaded from emr.sagepub.com by ancuta anca on October 25, 2014
Vous aimerez peut-être aussi
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Facing Your Feelings - 02 - Accepting DistressDocument10 pagesFacing Your Feelings - 02 - Accepting Distressletitia2hintonPas encore d'évaluation
- The Secret Art of Self-Development - R16844525 PDFDocument142 pagesThe Secret Art of Self-Development - R16844525 PDFrarmandjr8474Pas encore d'évaluation
- Intro To Psychology Crash Course Psychology 1Document3 pagesIntro To Psychology Crash Course Psychology 1Hahaha YeahPas encore d'évaluation
- Rene Daumal You Ve Always Been Wrong PDFDocument64 pagesRene Daumal You Ve Always Been Wrong PDFb.herbin100% (2)
- Aaron BeckDocument9 pagesAaron BeckWeaam MasoodPas encore d'évaluation
- Dual Process Theory 2.0Document168 pagesDual Process Theory 2.0Douglas Popp MarinPas encore d'évaluation
- Sol Kittay, George Serban, Lawrence C. Kolb, Melvin Sabshin Auth., George Serban Eds. Psychopathology of Human AdaptationDocument385 pagesSol Kittay, George Serban, Lawrence C. Kolb, Melvin Sabshin Auth., George Serban Eds. Psychopathology of Human AdaptationVictor GuagliardiPas encore d'évaluation
- DysphasiaDocument48 pagesDysphasiaredroseeeeee100% (1)
- The Importance of Soft Skills: Emotional Intelligence: 4Ss of EIDocument3 pagesThe Importance of Soft Skills: Emotional Intelligence: 4Ss of EIchowdhurymoinPas encore d'évaluation
- Leadership Choices: Saima ButtDocument4 pagesLeadership Choices: Saima ButtSofia VillenaPas encore d'évaluation
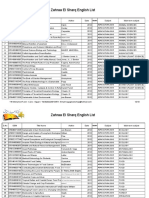
- Zahraa El Sharq List 2013-CIBF-2Document210 pagesZahraa El Sharq List 2013-CIBF-2CasPas encore d'évaluation
- Abnormal Psychology Notes: Anxiety DisordersDocument4 pagesAbnormal Psychology Notes: Anxiety DisordersAshley ChenenPas encore d'évaluation
- 1 s2.0 S0160289608000275 MainDocument9 pages1 s2.0 S0160289608000275 MainAndreea Robu-MovilaPas encore d'évaluation
- 01Document2 pages01BellaPas encore d'évaluation
- PRACTICE TEST 4 For The GiftedDocument11 pagesPRACTICE TEST 4 For The Giftedle thuong tranPas encore d'évaluation
- The Inner Shift That Changes EverythingDocument11 pagesThe Inner Shift That Changes EverythingMimi WPas encore d'évaluation
- Original PDF Intentional Interviewing and Counseling Facilitating Client Development in A Multicultural Society 9th Edition PDFDocument42 pagesOriginal PDF Intentional Interviewing and Counseling Facilitating Client Development in A Multicultural Society 9th Edition PDFshawn.hamilton470100% (34)
- EEG 2010 How To Write Report Anannit HODocument16 pagesEEG 2010 How To Write Report Anannit HOms6071086Pas encore d'évaluation
- Paperpile - May 07 JSON ExportDocument31 pagesPaperpile - May 07 JSON ExportMeaghan LinhartPas encore d'évaluation
- Content, Instructions, and Scoring of The Final Version of The Parkinson's Disease Cognitive Rating Scale (PD-CRS)Document19 pagesContent, Instructions, and Scoring of The Final Version of The Parkinson's Disease Cognitive Rating Scale (PD-CRS)Ailin Vejar GaticaPas encore d'évaluation
- Learning AssessmentDocument13 pagesLearning AssessmentAnnarizza ArceoPas encore d'évaluation
- AnsdDocument12 pagesAnsdAlok PandeyPas encore d'évaluation
- Issues in Remedial Education in MalaysiaDocument2 pagesIssues in Remedial Education in MalaysiaESWARYPas encore d'évaluation
- PSYCH-UA9029L01, Cognition: Instructor InformationDocument6 pagesPSYCH-UA9029L01, Cognition: Instructor InformationIonaPas encore d'évaluation
- Interpersonal and Intrapersonal Interventions To Manage The Stress of Living With A New RoommateDocument8 pagesInterpersonal and Intrapersonal Interventions To Manage The Stress of Living With A New RoommateAngelo PinerPas encore d'évaluation
- Neo BehaviourismDocument18 pagesNeo BehaviourismCeleste, Mark Valentene C.Pas encore d'évaluation
- Cognitive Behavioral TherapyDocument1 pageCognitive Behavioral TherapyzulkaberPas encore d'évaluation
- Theories of HRD1Document20 pagesTheories of HRD1Parameshwara AcharyaPas encore d'évaluation
- Amy L. Baylor - Development of IntuitionDocument16 pagesAmy L. Baylor - Development of IntuitionMatCultPas encore d'évaluation
- Development Economics II AssignmentDocument7 pagesDevelopment Economics II AssignmentHAMZA AYUBPas encore d'évaluation