Académique Documents
Professionnel Documents
Culture Documents
Skin Diseases
Transféré par
code-24Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Skin Diseases
Transféré par
code-24Droits d'auteur :
Formats disponibles
The skin is often referred to as the largest body organ and serves as the main protective barrier against
damage to internal tissues from trauma, ultraviolet light, temperature, toxins and bacteria. The skin is also
responsible for sensory perception, temperature regulation, production of vitamin D and excretion of waste
products. In addition to preventing harmful substances from entering the body, it also controls the loss of
vital substances from the body. It is therefore important that the skin remains intact to allow the body to
perform these essential functions. And when it cant function properly wed have a wide range of
manifestation; and here were going to talk about a few:
:Acne
Acne vulgaris usually begins at puberty
and results from hyperkeratinization of follicles,
increased sebum production, proliferation of
Propionibacterium acnes, and resulting
inflammation. Acne is classified by severity and
type as comedonal-only acne, mild-to-moderate
inflammatory acne, moderate-to-severe
inflammatory acne, and severe papulonodular
inflammatory acne. Acne is exacerbated by
creams and lotions, mechanical trauma (rubbing
from clothing, picking, and repetitive scrubbing),
medications (e.g., prednisone and progesterone), and sweating. Polycystic ovary syndrome should be
considered in women with acne, hirsutism, and acanthosis nigricans (hyperpigmentation of flexural folds).
Acne rosacea is a chronic inflammatory skin disorder of unknown etiology affecting the face,
typically the cheeks and nose, usually occurring
after the age of 30 years. On physical examination
there is erythema with telangiectasias, pustules,
and papules without comedones. Rosacea can be
differentiated from seborrheic dermatitis by the
presence of pustules. In early stages, rosacea can
present with only facial erythema and resemble
the butterfly rash of systemic lupus
erythematosus; however, the rash of systemic
lupus erythematosus typically spares the nasal
labial folds and areas under the nose and lower
lip. Rhinophyma (big irregular hyperplastic nose) can develop in some
rosacea patients.
Dermatitis (Eczematous Rashes)
Eczema denotes epidermal eruptions characterized histologically by intracellular edema. Atopic,
contact, seborrheic, and stasis dermatitis are common types of eczema, whereas nonspecific dermatitis is a
diagnosis of exclusion when no etiology is identified. Topical corticosteroids and oral antihistamines are
usually the treatment of choice for any type of eczema.
Atopic dermatitis is an allergic disorder
with genetic and immunologic components
characterized by intense itching leading to
excoriation, lichenification (epidermal
thickening), hyperpigmentation, and
papulosquamous eruption. Typical locations are
the flexural areas, head, neck, trunk, and hands.
Acute eruptions are often accompanied by
erythema, vesiculation, and oozing. In addition to
the standard treatment of dermatitis, skin
moisturizers can be used to decrease dryness and pruritis.
Contact dermatitis is precipitated by local
absorption of allergen or irritant through the
stratum corneum. Common allergens include
metals (e.g., nickel), topical anesthetics,
neomycin, poison oak, poison ivy, and strong
soaps or personal care products. The location of
eruptions may help to identify causative agents
(e.g., neck rash caused by a necklace). The
mainstay of treatment is avoidance of the
allergens and irritants.
Seborrheic dermatitis is characterized by erythematous plaques
with a dry or oily scale occurring in hair-bearing parts of the body
including scalp (dandruff), eyelashes, eyebrows, beard, chest, the external
ear canal and behind the ear, the forehead, and nasolabial folds. The precise
etiology is unknown but appears to be related to colonization with the yeast
Malassezia furfur. Scalp dermatitis is treated with selenium sulfide, coal tar,
or ketoconazole shampoos. The face can be cleansed and treated with
topical 1% hydrocortisone and 2% ketoconazole cream.
Bacterial Skin Infections
The most common skin infections observed in the outpatient setting include cellulitis, folliculitis, and
impetigo. Increasingly these infections are caused by community-acquired methicillin-resistant
Staphylococcus aureus (MRSA), especially in patients who have had close recent contact with persons
having a history of a similar infection.
Cellulitis is a deep skin (dermis) infection
most frequently caused by Staphylococcus aureus
or Group A streptococci. A well-demarcated area
of warmth, swelling, tenderness and erythema is
found on physical exam. Cellulitis can be
differentiated from contact dermatitis by absence
of vesicles or pruritis. Patients with cellulitis are
treated with oral antibiotics and analgesics;
intravenous antibiotics may be necessary for
failed outpatient treatment.
Folliculitis and furunculosis are pustular skin infections arising from hair follicles and caused by
Staphylococcus aureus and, less frequently, Group A Streptococcus. Topical antibiotics (e.g., mupirocin) and
hot compresses may be sufficient for treatment. Furuncles (boils) are pus-filled nodules requiring incision,
drainage and systemic antibiotics. Elimination of S. aureus nasal carriage using topical or intranasal
antibiotics may decrease relapses.
(Furuncle)
(Folliculitis)
Psoriasis
Psoriasis is a chronic, relapsing skin disorder characterized by discrete and well-demarcated raised
plaques or papules covered by a silvery white scale on the scalp, extensor surface of the extremities, low
back, and intergluteal cleft, and behind the ears. Symptoms are primarily cosmetic, although itching and pain
occur. Nail pitting, onycholysis, subungual hyperkeratosis, or discoloration of the nail surface occurs in up to
50% of patients. Limited chronic plaque psoriasis can be managed with sunlight, topical corticosteroids, and
tar shampoo or lotion if the scalp is involved. Topical corticosteroids should be discontinued slowly to avoid
rebound of psoriasis. Chronic plaque psoriasis involving more than 10% of the body surface, and more
severe forms of psoriasis should be referred to a dermatologist. Infection, particularly streptococcal
infections of the upper respiratory tract; injury to the skin; and medication (e.g., lithium and -blockers) can
exacerbate psoriasis. An inflammatory, seronegative spondyloarthropathy, psoriatic arthritis, can occur in up
to 25% of patients with psoriatic skin lesions. Inflammatory bowel diseaseincluding ulcerative colitis and
Crohns diseaseoccurs more commonly in patients with psoriasis.
Urticaria
Urticaria (hives) are raised, intensely pruritic red lesions
with sharp borders, typically 2-4 mm in diameter. In acute
urticaria, individual lesions may last 30 minutes to 2 hours, and an
episode usually resolves within a few days or weeks. In chronic
urticaria, individual lesions may last 4 to 36 hours. An attack
usually continues for several days or weeks, but may persist
beyond 6 weeks in one third of the patients. Common causes of
urticaria are medications, foods, viral or bacterial infection, latex
or other physical contacts, and stinging insects. Indiscriminate
laboratory testing is rarely helpful. Urticaria, in rare cases, can
precede anaphylaxis or angioedema in complement-induced
allergic reactions.
Vous aimerez peut-être aussi
- Medicine I Block Book FemaleDocument113 pagesMedicine I Block Book Femalecode-24Pas encore d'évaluation
- The Royal Victorian Eye and Ear Hospital AbbreviationsDocument7 pagesThe Royal Victorian Eye and Ear Hospital Abbreviationscode-24Pas encore d'évaluation
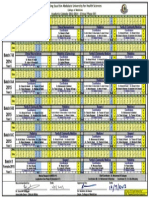
- Academic Calendar Phase III - 2013-2014Document1 pageAcademic Calendar Phase III - 2013-2014code-24Pas encore d'évaluation
- Hart of Dixie Episode Guide - Season 1 Recaps and ReviewsDocument1 pageHart of Dixie Episode Guide - Season 1 Recaps and Reviewscode-24Pas encore d'évaluation
- Antepartum HemorrhageDocument5 pagesAntepartum Hemorrhagecode-24Pas encore d'évaluation
- Skin DiseasesDocument5 pagesSkin Diseasescode-24Pas encore d'évaluation
- 2nd DraftDocument18 pages2nd Draftcode-24Pas encore d'évaluation
- KSAU-HS Female Med Student Participation Assessment FormDocument1 pageKSAU-HS Female Med Student Participation Assessment Formcode-24Pas encore d'évaluation
- Mentoring ProgramDocument1 pageMentoring Programcode-24Pas encore d'évaluation
- Access Medicine - TableDocument2 pagesAccess Medicine - Tablecode-24Pas encore d'évaluation
- Form UCE 10: Clinical Attachment Performance Feedback: DD MM DD MMDocument1 pageForm UCE 10: Clinical Attachment Performance Feedback: DD MM DD MMcode-24Pas encore d'évaluation
- 2-Year Pre-Professional Program Study Plan 2008Document5 pages2-Year Pre-Professional Program Study Plan 2008code-24Pas encore d'évaluation
- Access Medicine - Table (Hypo)Document3 pagesAccess Medicine - Table (Hypo)code-24Pas encore d'évaluation
- 12 Thediciton FINALDocument2 pages12 Thediciton FINALcode-24Pas encore d'évaluation
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- (ATB) Is This Patient Allergic To Penicillin (JAMA)Document8 pages(ATB) Is This Patient Allergic To Penicillin (JAMA)api-3697245100% (1)
- Drug EruptionsDocument11 pagesDrug EruptionsAchmad Hariyanto100% (1)
- PPE-25-Case Report of Aquagenic UrticariaDocument2 pagesPPE-25-Case Report of Aquagenic UrticariaSajin AlexanderPas encore d'évaluation
- Nalco Varidos FSK: Cigweld Pty LTDDocument10 pagesNalco Varidos FSK: Cigweld Pty LTDPouria KazemzadehPas encore d'évaluation
- Drugs Affecting Respiratory SystemDocument19 pagesDrugs Affecting Respiratory SystemRuby Ann DimayugaPas encore d'évaluation
- Drug Class Review Antihistamine (Update 5,2010)Document72 pagesDrug Class Review Antihistamine (Update 5,2010)Supalerk KowinthanaphatPas encore d'évaluation
- Opioid AllergyDocument4 pagesOpioid AllergyJay100% (1)
- Transfusion ReactionsDocument28 pagesTransfusion ReactionsRovefrances ErpeluaPas encore d'évaluation
- New 4Document38 pagesNew 4rishi guptaPas encore d'évaluation
- Cernadas-2013-Pediatric Allergy and ImmunologyDocument7 pagesCernadas-2013-Pediatric Allergy and ImmunologyMoisés PoncePas encore d'évaluation
- Katzung - AutacoidsDocument23 pagesKatzung - AutacoidsKhairul AimanPas encore d'évaluation
- Allergic Skin DiseasesDocument20 pagesAllergic Skin DiseasesRicky ChanPas encore d'évaluation
- The Flushing PatientDocument35 pagesThe Flushing Patientliu_owen17Pas encore d'évaluation
- Chapter 2Document24 pagesChapter 2edward surtidoPas encore d'évaluation
- YÖKDİL/1/İNGİLİZCE/SAĞLIK BİLİMLERİDocument28 pagesYÖKDİL/1/İNGİLİZCE/SAĞLIK BİLİMLERİSüleyman DoğanPas encore d'évaluation
- Metrogyl: New Zealand Consumer Medicine InformationDocument4 pagesMetrogyl: New Zealand Consumer Medicine InformationAnbu KrishnanPas encore d'évaluation
- Urticaria 2Document11 pagesUrticaria 2ijaldo ajahPas encore d'évaluation
- Skinhairnail Ass 1Document43 pagesSkinhairnail Ass 1Airene Aquino BusaniaPas encore d'évaluation
- Doctor Guide to Managing HivesDocument2 pagesDoctor Guide to Managing HivesSunil RathiPas encore d'évaluation
- Healing Begins With Sanctification of The HeartDocument56 pagesHealing Begins With Sanctification of The HeartMwana WaChuma100% (2)
- Food Allergy - Indian ScenarioDocument28 pagesFood Allergy - Indian ScenarioAman BansalPas encore d'évaluation
- Drug Allergy VervloetDocument450 pagesDrug Allergy VervloetGuhaKrishnaswamy100% (1)
- Flutibact Skin OintmentDocument12 pagesFlutibact Skin OintmentSowndarya100% (1)
- UtricariaDocument2 pagesUtricariaaaathavanPas encore d'évaluation
- Alsangedy Bullets For Paces Angioedema 2nd EditionDocument2 pagesAlsangedy Bullets For Paces Angioedema 2nd EditionGhulamMemonPas encore d'évaluation
- Urtikaria & Angioedema: Melinda Rambing Kong 406148015 Pembimbing: Dr. Eko Krisnarto SP - KKDocument19 pagesUrtikaria & Angioedema: Melinda Rambing Kong 406148015 Pembimbing: Dr. Eko Krisnarto SP - KKMelinda KongPas encore d'évaluation
- Paediatric Dermatology (Notes)Document24 pagesPaediatric Dermatology (Notes)Ahmad Syarafi AbdullahPas encore d'évaluation
- Emergency NursingDocument56 pagesEmergency NursingNur SanaaniPas encore d'évaluation
- Chapter 18 Thermal Injuries (Student Copy)Document31 pagesChapter 18 Thermal Injuries (Student Copy)api-287615830Pas encore d'évaluation
- ALLERGIC REACTIONS TO CHEMOTHERAPYDocument23 pagesALLERGIC REACTIONS TO CHEMOTHERAPYAmbl GeronPas encore d'évaluation