Académique Documents
Professionnel Documents
Culture Documents
Sarcopenic Obesity Predicts Instrumental Activities of Daily Living Disability in The Elderly
Transféré par
Franchesca OrtizTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Sarcopenic Obesity Predicts Instrumental Activities of Daily Living Disability in The Elderly
Transféré par
Franchesca OrtizDroits d'auteur :
Formats disponibles
Sarcopenic Obesity Predicts Instrumental
Activities of Daily Living Disability in the
Elderly
Richard N. Baumgartner,* Sharon J. Wayne,* Debra L. Waters,* Ian Janssen, Dympna Gallagher, and
John E. Morley
Abstract
BAUMGARTNER, RICHARD N., SHARON J. WAYNE,
DEBRA L. WATERS, IAN JANSSEN, DYMPNA
GALLAGHER, AND JOHN E. MORLEY. Sarcopenic
obesity predicts instrumental activities of daily living
disability in the elderly. Obes Res. 2004;12:19952004.
Objective: To determine the association of sarcopenic obesity with the onset of Instrumental Activities of Daily Living (IADL) disability in a cohort of 451 elderly men and
women followed for up to 8 years.
Research Methods and Procedures: Sarcopenic obesity
was defined at study baseline as appendicular skeletal muscle mass divided by stature squared 7.26 kg/m2 in men
and 5.45 kg/m2 in women and percentage body fat greater
than the 60th percentile of the study sample (28% body fat
in men and 40% in women). Incident disability was defined
as a loss of two or more points from baseline score on the
IADL. Subjects with disability at baseline (scores 8) were
excluded. Cox proportional hazards analysis was used to
determine the association of baseline sarcopenic obesity
with onset of IADL disability, controlling for potential
confounders.
Results: Subjects with sarcopenic obesity at baseline were
two to three times more likely to report onset of IADL
Received for review December 24, 2003.
Accepted in final form September 28, 2004.
The costs of publication of this article were defrayed, in part, by the payment of page
charges. This article must, therefore, be hereby marked advertisement in accordance with
18 U.S.C. Section 1734 solely to indicate this fact.
*Aging and Genetic Epidemiology Program, Division of Epidemiology and Preventive
Medicine, Department of Internal Medicine, University of New Mexico School of Medicine,
Albuquerque, New Mexico; Department of Community Health and Epidemiology and
School of Physical and Health Education, Queens University, Kingston, Ontario, Canada;
Obesity Research Center, St. Lukes-Roosevelt Hospital and Columbia University, New
York, New York; and Geriatric Research and Education Center, St. Louis University
VAMC, St. Louis, Missouri.
Address correspondence to R. N. Baumgartner, AGE, Surge 215, 2701 Frontier Place,
University of New Mexico School of Medicine, Albuquerque, NM 87131.
E-mail: rbaumgartner@salud.unm.edu
Copyright 2004 NAASO
disability during follow-up than lean sarcopenic or nonsarcopenic obese subjects and those with normal body composition. The relative risk for incident disability in sarcopenic
obese subjects was 2.63 (95% confidence interval, 1.19 to
5.85), adjusting for age, sex, physical activity level, length
of follow-up, and prevalent morbidity.
Discussion: This is the first study, to our knowledge, to
indicate that sarcopenic obesity is independently associated
with and precedes the onset of IADL disability in the
community-dwelling elderly. The etiology of sarcopenic
obesity is unknown but may include a combination of
decreases in anabolic signals and obesity-associated increases in catabolic signals in old age.
Key words: sarcopenic obesity, sarcopenia, obesity, Instrumental Activities of Daily Living disability, aging
Introduction
The prevalence of sarcopenia, or a relative deficiency of
skeletal muscle mass and strength, increases rapidly after 65
years of age and is significantly associated with functional
limitation and physical disability, independent of body fatness, in community-dwelling elderly (1 6). Estimates of
prevalences have varied widely across studies because of
differences in criteria for defining sarcopenia and sample
characteristics, such as age, sex, ethnicity, socioeconomic
status, health status, and body size. The strengths of associations reported have also varied because of differences in
methods of measuring functional limitation and disability
outcomes and the measurement and statistical control of
confounders. With the exception of Janssen et al. (4), who
analyzed data from NHANES III, most study samples have
been small or not strictly population-based, making results
difficult to generalize. Finally, all studies to date have been
cross-sectional, leaving open the question of whether sarcopenia and/or obesity precedes or follows the onset of
disability.
OBESITY RESEARCH Vol. 12 No. 12 December 2004
1995
Sarcopenic Obesity and Incident IADL Disability, Baumgartner et al.
Obesity has also been reported to be associated with
disability (7,8). Most studies, however, have used BMI,
which may systematically misclassify many elderly (9,10).
Some studies based on estimates of fat mass and fat-free
mass (FFM)1 have reported that increased fat mass is more
strongly associated with Instrumental Activities of Daily
Living (IADL) disability than low FFM (1113). Although
FFM is highly correlated with muscle mass, the percentage
of FFM that is appendicular skeletal muscle varies among
individuals and declines with aging (14 17). Thus, FFM
may be a less sensitive measure of sarcopenia than estimates
of muscle mass. Differences among studies in age and
ethnic composition and prevalence of overweight and obesity may also influence results for the relative strengths of
the associations of fat vs. lean body composition with disability. In any case, the various studies, taken together,
suggest that both sarcopenia and obesity are associated with
disability in community-dwelling elderly.
In a previous analysis of cross-sectional data from two
separate studies, the population-based New Mexico Elder
Health Survey (NMEHS) and the volunteer-cohort New
Mexico Aging Process Study (NMAPS), we found that the
combination of sarcopenia and obesity, or sarcopenic obesity, was more strongly associated with disability than
either body composition type alone (18,19). For example, in
the population-based NMEHS, the odds ratio for two or
more self-reported physical disabilities on the IADL was
8.72 for sarcopenic obesity in men compared with 3.78 for
pure sarcopenia and 1.34 for obesity, controlling for age,
ethnicity (Hispanic vs. non-Hispanic white), smoking, physical activity, alcohol intake, and comorbidity. The corresponding odds ratios in women were 11.98, 2.96, and 2.15,
respectively. Similar results were obtained in analyses of
data from the NMAPS (18). Sarcopenic obesity was defined
in these analyses as having a score on the relative skeletal
muscle mass index (appendicular skeletal muscle divided by
stature squared) more than 2 SD below the sex-specific
mean for a young adult reference population and percentage
body fat greater than the sex- and age-specific median.
These criteria were recognized to be somewhat arbitrary;
however, their application revealed the joint effect of sarcopenia and excess body fatness on IADL disability.
To date, we are aware of only two studies that have
attempted to replicate these findings for sarcopenic obesity.
Sternfeld et al. (13) reported a protective association for a
high lean/fat ratio, an index that is inversely correlated with
our definition of sarcopenic obesity, thereby providing indirect support. In contrast, Davison et al. (20) cross-classified 2917 men and women 70 years of age in the
NHANES III sample by predicted muscle mass and body
1
Nonstandard abbreviations: FFM, fat-free mass; IADL, Instrumental Activities of Daily
Living; NMEHS, New Mexico Elder Health Survey; NMAPS, New Mexico Aging Process
Study; NCEP ATPIII, ___; IL-6, interleukin 6; IGF-1, insulin-like growth factor 1.
1996
OBESITY RESEARCH Vol. 12 No. 12 December 2004
fat, using criteria similar to, but not identical to, ours and
found no significant associations between sarcopenic obesity and functional limitation.
In this study, we used longitudinal data from the NMAPS
cohort to test the hypothesis that sarcopenic obesity precedes, and therefore predicts, the onset of IADL disability in
community-dwelling elderly who have no disability at baseline. This is the first study that we are aware of to use
longitudinal data to determine the direction of the association between body composition and IADL disability in a
sample of community-dwelling elderly.
Research Methods and Procedures
Subjects
The subjects were members of the NMAPS, an ongoing
longitudinal cohort study of aging that began in 1980. This
study is described in detail in other publications (21). Ninety
percent of the participants are non-Hispanic white, 8% are
Hispanic, and 2% are nonwhite (black, Asian, or American Indian). To qualify for entry, subjects had to be 60 years
of age or older, free of major medical conditions, and living
independently in the Albuquerque, NM area. Enrollment
criteria were designed to exclude subjects from entry who
had significant illness that would preclude their ability to
participate in a long-term longitudinal study, such as recent
myocardial infarction, significant peripheral vascular disease, insulin-dependent diabetes, hepatic disease, history of
internal cancer requiring surgery, radiation therapy, or chemotherapy in the past 10 years, a positive test for hepatitis,
and untreated hypertension (systolic blood pressure 180
mm Hg; diastolic blood pressure 100 mm Hg). Participants were not required to maintain good health to continue
in the study. The NMAPS is a dynamic cohort in which
dropouts and deaths are replaced annually to keep the active
cohort at an average of 400 subjects per year. As a result,
the number of subjects included in a longitudinal analysis
may vary and is generally greater than the number of active
participants in any 1 year, because individuals with different
baseline years can contribute data. The dropout rate over the
20 years of the NMAPS has averaged 3.6% per year,
which is very good for a longitudinal study of elderly people
who may be expected to drop out more often because of
morbidity, IADL disability, and other causes than younger
subjects. Serious morbidity, other than dementia, has been
the main cause for dropout from the study (35%), followed
by movement from the Albuquerque area (27%).
Participants were seen annually for a thorough examination that included a blood draw, measures of body composition, a physical examination by a nurse practitioner, measures of functional and cognitive status, and nutritional
assessment. Annual assessments of cognitive and physical
functional status, balance and gait, and falls began in 1991,
and body composition measurements (other than anthro-
Sarcopenic Obesity and Incident IADL Disability, Baumgartner et al.
pometry) were initiated in 1993. A Lunar DPX DXA (GE/
Lunar Radiation Corp., Madison, WI) was used to measure
body composition, including bone mineral content and area
bone mineral density, total soft tissue mass, percent body
fat, lean soft tissue mass, and appendicular skeletal muscle
mass from standard whole body scans (20 to 40 minutes
depending on body thickness). The total dose for a whole
body scan is 1 Sv. Appendicular skeletal muscle was
defined as the sum of the lean soft tissue masses for the
arms and legs adjusted for nonmuscle components, following the method of Heymsfield et al. (22). The technical
errors of estimates of muscle mass are 3% and 2.5% for
the arm and leg, respectively; the precision of percentage
body fat is 1.5%.
Definition of Sarcopenic Obesity
Cut-points to define sarcopenic obesity were based on our
previous work (1,18). For the present analyses, subjects
were classified as sarcopenic if their relative skeletal muscle
mass was 2 SD below the mean of a sample of 229
healthy young (18 to 40 years) adults. For men, this cutpoint was 7.26 kg/m2; for women, it was 5.45 kg/m2.
Subjects were classified as obese if their percentage body
fat was above the 60th percentile of the study sample. For
men, this cut-point was 28% body fat; for women, it was
40% body fat. Based on the combination of sarcopenia and
obesity cut-points, subjects were further classified into four
groups: sarcopenic obese, sarcopenic nonobese, nonsarcopenic obese, and nonsarcopenic/nonobese.
Measurement of Incident IADL disability
The IADL questionnaire asks subjects how much help
they need to perform nine tasks considered important for
independent living: using the telephone, accessing transportation, getting groceries, making meals, doing housework,
doing handyman work, doing laundry, taking medications,
and managing money (23). There are three possible responses to each of the nine questions: need no help to
perform this task, need some help to perform this task, and
unable to do this task. Subjects were given one point for
each task they reported being able to do without help and
zero points for any tasks they were unable to do or needed
help in doing. Answers were summed for the nine responses; the maximum score of nine indicated the subject
could perform all nine tasks without help, and the minimum
score of zero indicated the subject could perform no tasks
without at least some help.
The current analysis was limited to subjects who had a
baseline IADL score of eight or nine, indicating that they
were functioning at a high level at the beginning of followup. Subjects were followed for up to 8 years (1993 to 2001)
for a drop in function, which was defined as a loss of two or
more points from baseline score. Subjects were included in
analyses if they had at least one additional IADL score
measured after baseline.
Potential Confounders
Physical activity was assessed using a modification of the
self-administered Health Insurance Plan instrument as described by Pereira et al. (24). The scores on this scale range
from 0 to 65, with higher scores indicating greater activity.
We have previously shown that physical activity scores on
this instrument are correlated with body composition (25).
Prevalent diseases were ascertained using a health history
questionnaire administered at study entry. Incident diseases
were obtained by self-report at each annual visit and verified against medical records.
Centralized obesity and the metabolic syndrome are also
potent risk factors for IADL disability and could confound
associations with sarcopenic obesity (26,27). Consequently,
we also created a variable classifying the presence of metabolic syndrome based on National Cholesterol Education
Panel, Adult Treatment Panel III criteria (28). Briefly, a
participant was considered to have the syndrome if they met
three or more of the following criteria: waist circumference
102 cm in men and 88 cm in women; serum triglycerides 150 mg/dL (1.69 mM); high-density lipoproteincholesterol 40 mg/dL (1.04 mM) in men and 50 mg/dL
(1.29 mM) in women; blood pressure 130/85 mm Hg; and
fasting glucose 110 mg/dL ( 6.1 mM).
Statistical Methods
All statistical analyses were conducted using the Statistical Analysis System (SAS Institute, Cary, NC). 2 tests for
proportions and t tests or Wilcoxon rank-sum tests for
means were used to compare body composition and drop in
IADL groups for baseline and follow-up characteristics.
Cox proportional hazards analysis was used to determine
the association of sarcopenic obesity with decline in functional status while controlling for potential confounding
variables, including age, sex, self-reported physical activity,
and morbidity. Because incident IADL disability was recorded at annual intervals, tied event times could occur. As
a result, we used a variation of the Cox model that takes into
consideration tied events caused by the use of a discrete,
rather than continuous, time-scale (SAS Ties Discrete
option). The underlying mathematics can be found in
Therneau and Grambsch (29). We did not stratify the sample for race or ethnicity because the numbers of nonwhite
and Hispanic minorities were too few for meaningful analysis.
Results
Five hundred thirty-six subjects had at least two IADL
scores between 1993 and 2001. Of these, 68 were excluded
because their baseline score was less than eight. Another 17
subjects were excluded because they had no body composition data in the year they had their first IADL score
measured. This left a final sample size of 451.
Twenty-six subjects (5.8%) were classified as sarcopenic
obese at baseline. During the 8-year follow-up period, 77
OBESITY RESEARCH Vol. 12 No. 12 December 2004
1997
Sarcopenic Obesity and Incident IADL Disability, Baumgartner et al.
Table 1. Subject characteristics by sarcopenic obesity status
By outcome
Percent with IADL drop
Mean (SD) time to IADL drop in years
Demographics
Percent male
Mean (SD) age in years at baseline
Mean (SD) activity score at baseline
Mean (SD) follow-up time in years
Prevalent conditions
Cardiovascular disease
Hypertension
Arthritis/rheumatism
Type 2 diabetes
Metabolic syndrome
Incident conditions
Stroke
Type 2 diabetes
Heart attack
Congestive heart failure
Cancer (excludes basal cell)
Hip fracture
Any fracture
Deaths
Sarcopenic
obese
(N 26)
Sarcopenic
nonobese
(N 82)
Nonsarcopenic
obese
(N 146)
Nonsarcopenic
nonobese
(N 197)
p*
38.5%
1.5 (1.1)
14.6%
2.3 (2.0)
15.1%
2.1 (1.7)
16.8%
2.4 (1.8)
0.027
0.588
61.5%
73.9 (6.6)
18.1 (4.9)
4.5 (2.5)
46.3%
74.0 (6.8)
19.8 (5.7)
4.3 (2.4)
34.2%
71.8 (5.9)
17.9 (5.9)
5.5 (2.4)
34.0%
72.7 (6.3)
20.3 (6.5)
4.7 (2.6)
0.013
0.083
0.006
0.001
11.5%
26.9%
65.4%
7.7%
19.2%
18.3%
17.1%
47.6%
1.2%
3.7%
8.2%
36.3%
50.7%
1.4%
37.5%
13.7%
20.8%
54.3%
1.0%
10.7%
0.159
0.003
0.394
0.076
0.0001
3.8%
0.0%
7.7%
7.7%
7.7%
3.8%
11.5%
7.6%
1.2%
1.2%
3.7%
1.2%
8.5%
0.0%
7.3%
13.4%
2.7%
2.1%
2.7%
0.7%
5.5%
0.0%
10.3%
6.2%
2.5%
1.5%
3.6%
1.0%
4.6%
0.5%
13.7%
10.7%
0.717
0.927
0.567
0.093
0.507
0.145
0.460
0.290
*p Value for difference between sarcopenic obesity groups in percents (2) or means (ANOVA).
Metabolic syndrome defined by NCEP ATPIII criteria.
subjects (17%) experienced a drop in functional status.
Table 1 shows that those who were sarcopenic obese at
baseline were significantly more likely to develop a loss in
functional status than those who were not (p 0.03). Time
to drop in IADL was also shorter in the sarcopenic obese
group (1.5 years) compared with the other groups (2.1 to 2.4
years). A significantly greater percentage (61.5%) of sarcopenic obese subjects was male. Sarcopenic obese and
sarcopenic nonobese groups tended to be slightly older (2
years on average) than nonsarcopenic groups. Mean baseline physical activity score was significantly higher in the
nonobese than obese groups, regardless of sarcopenia (p
0.006). The obese groups were significantly more likely to
have prevalent hypertension at baseline than the nonobese
groups, regardless of sarcopenia (p 0.003). There were
nonsignificant trends for an increased incidence of congestive heart failure and hip fracture in the sarcopenic obese
compared with the other groups. Only 1.6% (n 7) of the
1998
OBESITY RESEARCH Vol. 12 No. 12 December 2004
participants had diagnosed type 2 diabetes at baseline, and
only seven incident cases were ascertained during followup. Although the prevalence of type 2 diabetes was somewhat higher in the sarcopenic obese group (7.7%) than the
other groups (1.0% to 1.4%), this difference was not statistically significant because of the small number of cases.
Moreover, none of the incident cases of type 2 diabetes
occurred within the sarcopenic obese group. Overall, the
prevalence of the metabolic syndrome was 17.5% in men
and 19.1% in women. The prevalence was highest in the
nonsarcopenic obese group (37.5%), followed by the sarcopenic obese group (19.2%), and normal group (10.7%),
and was lowest in the sarcopenic nonobese group (3.7%).
There was no difference among the groups for any of the
other prevalent or incident morbidity conditions. A total of
43 deaths occurred during the follow-up period; however,
these were not more likely to occur in the sarcopenic obese
group (2/26, 8%) than in the other groups (41/426, 9%).
Sarcopenic Obesity and Incident IADL Disability, Baumgartner et al.
Table 2. Subject characteristics by drop in IADL
Demographics
Percent male
Mean age in years at baseline
Mean activity score at baseline
Mean follow-up time in years
Prevalent conditions
Cardiovascular disease
Hypertension
Arthritis/rheumatism
Type 2 diabetes
Metabolic syndrome
Incident conditions
Stroke
Type 2 diabetes
Heart attack
Congestive heart failure
Cancer (excludes basal cell)
Hip fracture
Any fracture
Deaths
IADL drop
(N 77)
No drop in IADL
(N 374)
p*
45.5%
78.0 (6.3)
15.8 (4.8)
5.0 (2.3)
36.6%
71.6 (5.7)
20.1 (6.2)
4.9 (2.6)
0.134
0.0001
0.0001
0.850
16.9%
36.4%
63.6%
3.9%
19.7%
11.8%
23.3%
50.3%
1.1%
18.3%
0.218
0.016
0.032
0.068
0.766
2.6%
0.0%
1.3%
1.3%
5.2%
0.0%
13.0%
28.6%
2.4%
1.9%
4.0%
1.3%
6.7%
0.5%
10.9%
5.6%
0.921
0.226
0.241
0.979
0.628
0.610
0.520
0.001
*p Value for difference between sarcopenic obesity groups in percents (2) or means (ANOVA).
Metabolic syndrome defined by NCEP ATPIII criteria.
In Table 2, subjects with a drop in IADL score are
compared with those with no drop for baseline and follow-up characteristics. A two-point drop in score, reflecting
an increase in self-reported IADL disability, was significantly associated with older age and lower physical activity
(p 0.0001). Prevalent hypertension and arthritis/rheumatism were significantly higher (p 0.05) in the IADL drop
compared with the nondrop group. The prevalence of type 2
diabetes was slightly, but not significantly, higher in the
IADL drop group (3.9%) compared with the nondrop group
(1.1%). There was no significant difference between groups
for the prevalence of the metabolic syndrome (19.7% vs.
18.3%). There was no association between drop in IADL
score and sex or any of the incident conditions listed in
Table 2. A significantly greater percentage of participants
with a drop in IADL score, however, died during follow-up
(28.6%) compared with those without a drop in IADL
(5.6%).
In a multivariate proportional hazards model simultaneously contrasting sarcopenic obese, sarcopenic nonobese,
and nonsarcopenic obese groups, with the nonsarcopenic
nonobese group as the referent category, the hazard ratio
for drop in IADL score was 2.91 (95% confidence interval, 1.36 to 6.21) for the sarcopenic obese group. Hazard
ratios for sarcopenic nonobese and nonsarcopenic obese
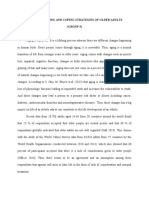
groups were not significantly different from 1.0. Figure 1
shows age-adjusted Kaplan-Meier survival curves contrasting the four body composition groups, in which the markedly shorter time to drop in IADL in the sarcopenic obese
group is clearly evident. As a result, the other three groups
were combined in the final analyses.
Table 3 shows the results of proportional hazards analyses evaluating the effect of sarcopenic obesity on time to
drop in IADL score. The unadjusted hazard ratio of 3.17
(95% confidence interval, 1.55 to 6.49) indicates a rate of
decline that was three times higher in sarcopenic obese
subjects compared with those who were not sarcopenic
obese at baseline. Adjustment for age, sex, physical activity
score, follow-up time, prevalent hypertension, and arthritis/
rheumatism reduced the hazard ratio to 2.63 (95% confidence interval, 1.19 to 5.85). Cardiovascular disease was
not included in the model because it was not associated with
either body composition type or incident IADL disability.
Sarcopenic obesity remained significantly associated with
OBESITY RESEARCH Vol. 12 No. 12 December 2004
1999
Sarcopenic Obesity and Incident IADL Disability, Baumgartner et al.
founded with age, sex, physical activity, or major prevalent morbidity.
Discussion
Figure 1: Kaplan-Meier survival curve for time to drop in IADL
by body composition type. Adjusted for age at baseline. NS, NO:
nonsarcopenic, nonobese; S, NO: sarcopenic, nonobese; NS, O:
nonsarcopenic, obese; S, O: sarcopenic, obese.
drop in IADL score (hazard ratio 2.48; 95% confidence
interval, 1.13 to 5.47) after additional inclusion in the multivariate model of metabolic syndrome (data not shown in
Table 3), which did not have a significant independent
association with incident IADL disability (hazard ratio
0.99; 95% confidence interval, 0.53 to 1.84). There was an
increased risk of incident IADL disability for prevalent type
2 diabetes, but the CI was wide because of the small number
of cases, and the association was not statistically significant
(hazard ratio 1.83; 95% confidence interval, 0.32 to
10.57). The inclusion of type 2 diabetes in the model did not
further affect the hazard ratio for sarcopenic obesity (data
not shown in Table 3). In summary, the sarcopenic obese
group had a statistically significant 2.5- to 3.0-fold increased risk compared with the other body composition
groups for new self-reported IADL disability. In multivariate analysis, this risk was not substantially con-
This is the first study, to our knowledge, to report that
sarcopenic obesity precedes and predicts the onset of IADL
disability in a sample of community-dwelling elderly. Our
data suggest that nondisabled elderly with sarcopenic obesity are 2.5 times more likely to report subsequent IADL
disability over a 7-year follow-up than individuals without
sarcopenic obesity, regardless of age, sex, level of habitual
physical activity, and morbidity. Pure sarcopenia or sarcopenic nonobesityand obesity without sarcopenia were
not significantly associated with the onset of IADL disability in this study, which contrasts somewhat with reports
from previous cross-sectional studies for significant positive
associations.
There are several limitations of this study that should be
recognized. First, the study cohort was small, and sarcopenic obesity was rare, limiting the statistical power to
detect associations. The small sample size also limited our
ability to analyze potentially confounding associations with
incident morbidity. Although our data suggest that the association of sarcopenic obesity with incident IADL disability is independent of major prevalent comorbidities, it remains possible that this association is confounded by
underlying, preclinical morbidity. Second, the method
used to define sarcopenic obesity was relatively arbitrary;
there are still no standardized definitions of sarcopenia or
obesity, in terms of percentage body fat, for communitydwelling elderly. Third, the NMAPS cohort is not strictly
population-based: it is composed of volunteers and the entry
criteria exclude those with serious diseases. Thus, our results may not be generalizable to a broader population. On
the other hand, the low prevalence and incidence of type 2
diabetes in the NMAPS cohort remove this significant obesity-related cause of IADL disability as a confounder of the
effects of sarcopenic obesity in this study.
Table 3. Hazard ratios and 95% confidence intervals for proportional hazards models evaluating the effect of
sarcopenic obesity and relevant covariates on time to drop in functional status
Unadjusted model
hazard ratio (95% CI)
Sarcopenic obesity
Age in years
Gender (men 1)
Activity score
Follow-up time in years
Prevalent hypertension
Prevalent arthritis/rheumatism
2000
3.17 (1.55, 6.49)
OBESITY RESEARCH Vol. 12 No. 12 December 2004
Intermediate model
hazard ratio (95% CI)
2.52
1.13
1.38
0.90
0.83
(1.15,
(1.08,
(0.83,
(0.86,
(0.73,
5.51)
1.18)
2.28)
0.95)
0.95)
Full model
hazard ratio (95% CI)
2.63
1.14
1.43
0.91
0.84
1.80
1.13
(1.19,
(1.09,
(0.85,
(0.87,
(0.74,
(1.06,
(0.66,
5.85)
1.19)
2.40)
0.96)
0.96)
3.06)
1.92)
Sarcopenic Obesity and Incident IADL Disability, Baumgartner et al.
We were among the first to develop and apply methods to
measure the prevalence of sarcopenia and identify risk
factors and sequelae in epidemiological studies (1). We
defined sarcopenia as having a value greater than 2 SD
below the mean of a young adult reference population for
appendicular skeletal muscle mass (measured using DXA)
divided by stature squared. Several investigators have subsequently used this index or a similar one based on total
muscle mass divided by stature squared to estimate prevalences of sarcopenia and associations with disability
(2,3,5,6). However, other researchers have used different
indices, including total muscle mass as a percentage of body
weight, FFM/stature2, FFM/fat mass ratio, and muscle mass
adjusted statistically for height and fat mass (4,13,30,31).
Thus, there is still no consensus for any standardized definition of sarcopenia. Recently, Janssen et al. (32) used
receiver-operating characteristic curve analysis to identify
optimal cut-off values for predicting physical IADL disability from total muscle mass divided by stature squared for
4449 older (60 years) participants in NHANES III. The
optimal cut-points associated with high physical IADL
disability risk were 5.75 and 8.50 kg/m2 in women and
men, respectively. Whereas we did not choose to apply
these cut-points in this paper, it should be noted that they
are closely similar to the previously defined ones that
were used (1).
The same issue applies to the definition of obesity in
the elderly; there is as yet no consensus as to its definition.
Several investigators have noted that percentage body fat is
systematically higher for any BMI in elderly compared with
young adults (9,10,33). Thus, conventional cut-off values
for defining overweight and obesity from BMI misclassify
many elderly and underestimate true prevalences of excess
body fatness, resulting in biased estimates of risk for various
outcomes associated with obesity. Gallagher et al. (33)
determined percentage body fat values corresponding to
BMI values of 25 and 30 kg/m2 in a large sample of 2639
men and women 20 to 79 years of age. A BMI 30 kg/m2
corresponded to a percentage body fat of 43% in white
women and 31% in white men 60 to 79 years of age. The
cut-points used in the present study were only slightly lower
(40% and 28% in women and men, respectively). Thus, our
criteria for classifying both sarcopenia and obesity in
this study are supported by other work.
To date, few studies of sarcopenia and sarcopenic obesity
have been conducted in population-based samples. With
regard to this study, the representativeness of the NMAPS
can be judged by comparison with the population-based
study we conducted between 1993 and 1996 in the Albuquerque area: the NMEHS (1). In 1993, the baseline year
for body composition studies, 17.5% of active NMAPS
participants had coronary heart or cardiovascular disease,
32.2% had hypertension, 72.5% had osteoarthritis, and
14.7% had cancer (other than skin cancer diagnosed subse-
quent to entry). The corresponding prevalences among nonHispanic whites in the NMEHS were as follows: coronary
heart or cardiovascular disease, 18.2%; hypertension,
32.1%, arthritis, 66.3%; history of cancer, 19.0%. The prevalence of sarcopenic obesity is also similar in the NMAPS
(5.8%) compared with the NMEHS (5%). On the other
hand, the prevalence of three or more self-reported IADL
disabilities is lower in the NAMPS (9.8%) than in the
population-based NMEHS (22%).
Whereas these results support our previously reported
finding in two separate cross-sectional studies that sarcopenic obesity is more strongly associated with IADL
disability than either obesity or sarcopenia (18), it is important to note apparently contradictory evidence. Davison et
al. (20) reported no significant association using data from
NHANES III for 2917 men and women 70 years of age.
Sarcopenia and obesity were defined using criteria similar,
but not identical, to this study; however, the outcome was
functional limitation rather than IADL disability. Functional
limitation was defined as having difficulty with at least
three of the following self-reported items: walking onequarter mile; walking up 10 steps without resting; carrying
10 lbs; stooping, crouching, or kneeling; and standing up
from an armless chair. The authors noted that an important
limitation of their study may have been that percentage
body fat and muscle mass were predicted using published
anthropometric prediction equations (1,34), rather than
measured using DXA, which could have attenuated the
associations. However, Janssen et al. (32) applied the same
prediction equation to estimate muscle mass in NHANES
III and reported significant associations between low relative muscle mass, defined as muscle mass divided by stature
squared, and IADL disability, when adjusting for body fat,
age, race, smoking, alcohol, and comorbidity. This raises
another important issue: disparities among studies for associations may also depend on the definition of the outcomes,
i.e., IADL disability as distinct from functional limitation
and the methods used to measure these. In our previous
cross-sectional studies, we found that sarcopenic obesity
was also significantly associated with abnormalities in performance-based tests of balance and gait and reported falls
in the past year (18).
Type 2 diabetes has been shown to be an important risk
factor for disability in some large cross-sectional studies
(26,27); thus, there was concern that it could be a significant
confounder of the association between sarcopenic obesity
and disability in this study. Few participants in the NMAPS
cohort had prevalent, diagnosed type 2 diabetes at baseline,
and the incidence of this disease was low. Although a
nonsignificant, increased risk for incident disability was
found for type 2 diabetes, this association was not confounded with the risk for sarcopenic obesity. Taken together, these observations strongly suggest that the association of sarcopenic obesity with incident disability is
OBESITY RESEARCH Vol. 12 No. 12 December 2004
2001
Sarcopenic Obesity and Incident IADL Disability, Baumgartner et al.
independent of type 2 diabetes. Our analyses indicate that
the association of sarcopenic obesity with incident IADL
disability is also independent of the metabolic syndrome.
Whereas the prevalence of metabolic syndrome was higher
in the sarcopenic obese group (19.2%) compared with the
normal and sarcopenic nonobese groups (10.7% and
3.7%, respectively), the prevalence was highest in the nonsarcopenic obese group (37.5%), indicating that the metabolic syndrome does not substantially overlap with our
definition of sarcopenic obesity.
Physical activity scores were significantly lower in both
sarcopenic obese and nonsarcopenic obese groups (18)
than in sarcopenic nonobese or normal groups (20) and
were substantially lower in participants with a drop in IADL
score (16) than in those with no drop (20). Physical
activity, however, was not significantly associated with
incident IADL disability independent of sarcopenic obesity
in the multivariate model. This suggests that both reduced
physical activity and incident IADL disability may be consequences of sarcopenic obesity.
The etiology of sarcopenia remains poorly understood,
and the causes of sarcopenic obesity are unknown (19).
From a physiological standpoint, it is intuitive that an individual with excess adiposity and low muscle mass would
have more difficulty accomplishing many physical activities
than an obese individual with adequate muscle mass, because muscle strength would be insufficient for body
weight. In younger adults, muscle mass is generally increased in obesity, which is assumed to be an anatomical
response to the stress imposed by increased body weight.
Bone mineral density is similarly increased in obesity.
Forbes (35) showed that changes in body weight generally
involve proportional changes in fat mass and FFM. On
average, 30% of any change in weight, gain or loss, is
comprised of FFM, mainly muscle. Certain exceptions are
recognized to this rule, including cachexia and old age.
We previously reported data showing that disproportionate
changes in fat mass and FFM occur over time in elderly
persons (36). FFM can decrease without significant weight
change, implying a simultaneous and offsetting increase in
fat mass. Thus, it would seem that the physiological relationships linking fat mass and FFM can be modified in some
elderly with advancing age, resulting in sarcopenic obesity.
Roubenoff (37) has proposed a hypothetical model in
which age-related gains in body fat and losses in muscle
mass act synergistically over time to produce sarcopenic
obesity and associated IADL disability and morbidity. The
keys to this hypothetical process are the recent recognition
that proinflammatory cytokines, such as interleukin 6 (IL6), increase with age and that adipose tissue is an active
endocrine organ that participates in the regulation of appetite, carbohydrate, and fat metabolism through the secretion
of certain cytokines, including leptin and tumor necrosis
factor , as well as IL-6. The secretion of these hormone2002
OBESITY RESEARCH Vol. 12 No. 12 December 2004
like proinflammatory cytokines is increased in obesity,
which is now considered to resemble a kind of subclinical
chronic inflammatory state. It has long been recognized that
proinflammatory cytokines, tumor necrosis factor and
IL-6 in particular, are associated with muscle wasting in
cachexia through stimulation of protein degradation through
the ubiquitinproteosome pathway. Roubenoff has proposed that chronic low levels of these cytokines caused by
age-associated increases in adiposity may result in an enhancement of the more subtle, gradual loss of muscle that
characterizes sarcopenia (37). Thus, sarcopenia may be accelerated in individuals with long-standing obesity and its
associated chronic inflammatory status, resulting in sarcopenic obesity in old age.
Data from several studies also support the hypothesis that
sarcopenia is associated with age-related decreases in anabolic signals, principally testosterone and insulin-like
growth factor 1 (IGF-1) (25,38 40). We previously noted
that sarcopenic obese men in the NMAPS had significantly
lower serum total testosterone and IGF-1 levels than other
body composition types, including sarcopenic nonobese
men (18). Unfortunately, these associations were not significant in women; thus, the role of these anabolic hormones in
sarcopenic obesity in women is less clear. Recently, Kenney
et al. (6) reported that sarcopenia was associated with serum
testosterone levels in women and that prevalences of sarcopenia were similar in women taking vs. not taking hormone replacement therapy, suggesting no association with
estrogen. Payette et al. (40) recently reported that a 2-year
loss of FFM was associated with serum IGF-1 in men and
with IL-6 production in women, 72 to 92 years of age at
baseline. Taken together, these data suggest that sarcopenic
obesity may result from the combination of decreases in
anabolic signals and obesity-associated increases in catabolic signals in old age, with possible sex differences in the
relative influences of these signals.
In summary, sarcopenic obesity in old age is more
strongly associated with IADL disability than either sarcopenia or obesity per se in the NMAPS. These findings
need to be replicated in other, larger cohort studies with
suitable data for body composition, IADL disability, and
functional status. Further research is needed on the etiology
of sarcopenic obesity as a late-life body composition disorder that is most strongly predictive of disability in old age.
Acknowledgments
This work was supported by NIH Grants R01 AG10149
and AG02049.
References
1. Baumgartner RN, Koehler KM, Gallagher D, et al. Epidemiology of sarcopenia among the elderly in New Mexico.
Am J Epidemiol. 1998;147:755 63.
Sarcopenic Obesity and Incident IADL Disability, Baumgartner et al.
2. Melton LJ, Khosla S, Crowson CS, OConnor MK,
OFallon WM, Riggs BL. Epidemiology of sarcopenia. J Am
Geriatr Soc. 2000;48:62530.
3. Tanko LB, Movsesyan L, Mouritzen U, Christiansen C,
Svendsen OL. Appendicular lean tissue mass and the prevalence of sarcopenia among healthy women. Metabolism. 2002;
51:69 74.
4. Janssen I, Heymsfield SB, Ross R. Low relative skeletal
muscle mass (sarcopenia) in older persons is associated with
functional impairment and physical IADL disability. J Am
Geriatr Soc. 2002;50:889 96.
5. Iannuzzi-Sucich M, Prestwood K, Kenny A. Prevalence of
sarcopenia and predictors of skeletal muscle mass in healthy,
older men and women. J Gerontol. 2002;57:M7727.
6. Kenney A, Dawson L, Kleppinger A, Iannuzzi-Sucich M,
Judge JO. Prevalence of sarcopenia and predictors of skeletal
muscle mass in nonobese women who are long-term users of
estrogen-replacement therapy. J Gerontol. 2003;58:436 40.
7. Jensen GL, Friedmann JM. Obesity is associated with functional decline in community-dwelling rural older persons.
J Am Geriatr Soc. 2002;50:918 23.
8. Friedman JM, Elasy T, Jensen GL. The relationship between body mass index and self-reported functional limitation
among older adults: a gender difference. J Am Geriatr Soc.
2001;49:398 403.
9. Baumgartner RN, Heymsfield SB, Roche AF. Human body
composition and chronic disease. Obes Res. 1995;3:7396.
10. Gallagher D, Visser M, Sepulveda D, Pierson RN, Harris
T, Heymsfield SB. How useful is body mass index for comparison of body fatness across age, sex, and ethnic groups?
Am J Epidemiol. 1996;143:228 39.
11. Visser M, Langlois J, Guralnik JM, et al. High body fatness, but not low fat-free mass, predicts IADL disability in
older men and women: the Cardiovascular Health Study. Am J
Clin Nutr. 1998;68:584 90.
12. Visser M, Harris TB, Langlois J, et al. Body fat and skeletal
muscle mass in relation to physical IADL disability in very old
men and women of the Framingham Heart Study. J Gerontol.
1998;53:M214 21.
13. Sternfeld B, Ngo L, Satariano WA, Tager IB. Associations
of body composition with physical performance and selfreported functional limitation in elderly men and women.
Am J Epidemiol. 2002;156:110 21.
14. Gallagher D, Visser M, deMeersman RE, et al. Appendicular skeletal muscle mass: effects of age, gender, and ethnicity. J Appl Physiol. 1997;83:229 39.
15. Janssen I, Heymsfield SB, Wang ZM, Ross R. Skeletal
muscle mass and distribution in 468 men and women aged
18 88 yr. J Appl Physiol. 2000;89:81 8.
16. Wang ZM, Heo M, Lee RC, Kotler DP, Withers RT,
Heymsfield SB. Muscularity in adult humans: proportion of
adipose tissue-free body mass as skeletal muscle. Am J Human
Biol. 2001;13:6129.
17. Kyle UG, Genton L, Hans D, Karsegard L, Slosman DO,
Pichard C. Age-related differences in fat-free mass; skeletal
muscle; body cell mass and fat mass between 18 and 94 years.
Eur J Clin Nutr. 2001;55:66372.
18. Baumgartner RN. Body composition in healthy aging. Ann N
Y Acad Sci. 2000;904:437 48.
19. Morley JE, Baumgartner RN, Roubenoff R, Mayer J, Nair
KS. Sarcopenia. J Lab Clin Med. 2001;137:231 43.
20. Davison KK, Ford ES, Cogswell ME, Dietz WH. Percentage
of body fat and body mass index are associated with mobility
limitations in people aged 70 and older from NHANES III.
J Am Geriatr Soc. 2002;50:18029.
21. Garry PJ, Owen GM, Eldridge TO. The New Mexico Aging
Process Study. Albuquerque, NM: University of New Mexico
Press; 1997.
22. Heymsfield SB, Smith R, Aulet M, et al. Appendicular
skeletal muscle massmeasurement by dual photon absorptiometry. Am J Clin Nutr. 1990;52:214 8.
23. Lawton MP, Brody EM. Assessment of older peopleself
maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179 83.
24. Pereira MA, Fitzgerald SJ, Gregg EW, et al. A collection of
physical activity questionnaires for health related research.
Med Sci Sports Exerc 1997;29:S39 40.
25. Baumgartner RN, Waters DL, Gallagher D, Morley JE,
Garry PJ. Predictors of skeletal muscle mass in elderly men
and women. Mech Ageing Dev. 1999;107:12336.
26. Gregg E, Mangione C, Cauley J, et al. Diabetes and incidence of physical IADL disability and functional decline
among older women. Diabetes. 2000;49:A192.
27. Maty SC, Fried LP, Volpato S, Williamson J, Brancati FL,
Blaum CS. Patterns of IADL disability related to diabetes
mellitus in older women. J Gerontol. 2004;59:148 53.
28. Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic
syndrome among US adults: findings from the Third National
Health and Nutrition Examination Survey. JAMA. 2002;287:
356 9.
29. Therneau TM, Grambsch PM. Modeling Survival Data:
Extending the Cox Model. New York: Springer-Verlag; 2000.
30. Castillo EM, Goodman-Gruen D, Kritz-Silverstein D,
Morton DJ, Wingard DL, Barrett-Connor E. Sarcopenia in
elderly men and womenthe Rancho Bernardo Study. Am J
Prev Med. 2003;25:226 31.
31. Newman AB, Visser M, Kupelian V, et al. Defining sarcopenia in older adults: a comparison of two approaches. The
Health Aging and Body Composition study. J Am Geriatr Soc.
2002;50:S68 S68.
32. Janssen I, Baumgartner RN, Ross R, Rosenberg IH,
Roubenoff R. Skeletal muscle cutpoints associated with elevated physical IADL disability risk in older men and women.
Am J Epidemiol. 2004;159:41321.
33. Gallagher D, Heymsfield SB, Heo M, Jebb SA, Murgatroyd PR, Sakamoto Y. Healthy percentage body fat ranges: an approach for developing guidelines based on body mass
index. Am J Clin Nutr. 2000;72:694 701.
34. Janssen I, Heymsfield SB, Baumgartner RN, Ross R. Estimation of skeletal muscle mass by bioelectrical impedance
analysis. J Appl Physiol. 2000;89:46571.
35. Forbes GB. Longitudinal changes in adult fat-free mass:
influence of body weight. Am J Clin Nutr. 1999;70:102531.
36. Gallagher D, Ruts E, Visser M, et al. Weight stability masks
sarcopenia in elderly men and women. Am J Physiol. 2000;
279:E366 75.
37. Roubenoff R. Catabolism of aging: is it an inflammatory
process? Curr Opin Clin Nutr Metab Care. 2003;6:2959.
OBESITY RESEARCH Vol. 12 No. 12 December 2004
2003
Sarcopenic Obesity and Incident IADL Disability, Baumgartner et al.
38. van den Beld AW, de Jong FH, Grobbee DE, Pols HAP,
Lamberts SWJ. Measures of bioavailable serum testosterone
and estradiol and their relationships with muscle strength,
bone density, and body composition in elderly men. J Clin
Endocrinol Metab. 2000;85:3276 82.
39. Wittert GA, Chapman IM, Haren MT, Mackintosh S,
Coates P, Morley JE. Oral testosterone supplementation
2004
OBESITY RESEARCH Vol. 12 No. 12 December 2004
increases muscle and decreases fat mass in healthy elderly
males with low-normal gonadal status. J Gerontol. 2003;
58:618 25.
40. Payette H, Roubenoff R, Jacques PF, et al. Insulin-like
growth factor-1 and interleukin 6 predict sarcopenia in very
old community-living men and women: the Framingham
Heart Study. J Am Geriatr Soc. 2003;51:1237 43.
Vous aimerez peut-être aussi
- Protein and Nutrition in Critically Ill PatientDocument43 pagesProtein and Nutrition in Critically Ill PatientTom KristiantoPas encore d'évaluation
- How To Inhibit Myostatin For Muscle Growth and Longer LifeDocument5 pagesHow To Inhibit Myostatin For Muscle Growth and Longer Lifedarthlucasx100% (3)
- Comprehensive Management SarcopeniaDocument25 pagesComprehensive Management SarcopeniaMardikaPas encore d'évaluation
- The Very Old CriticallyDocument590 pagesThe Very Old CriticallyRonei Renato RubboPas encore d'évaluation
- ESPEN Guidelines On Parenteral Nutrition. Intensive Care 2009Document38 pagesESPEN Guidelines On Parenteral Nutrition. Intensive Care 2009ERINSONPas encore d'évaluation
- Body Mass Index and Body Composition Measures by Dual X-Ray Absorptiometry in Patients Aged 10 To 21 Years With Spinal Cord InjuryDocument8 pagesBody Mass Index and Body Composition Measures by Dual X-Ray Absorptiometry in Patients Aged 10 To 21 Years With Spinal Cord InjuryJoão Pedro PontesPas encore d'évaluation
- 9 FullDocument7 pages9 FullSaudah Sii SipitPas encore d'évaluation
- Nej Mo A 1304501aasDocument12 pagesNej Mo A 1304501aasHadiyana Arief HafizPas encore d'évaluation
- Associations Between Body Weight and Personality Disorders in A Nationally Representative SampleDocument8 pagesAssociations Between Body Weight and Personality Disorders in A Nationally Representative SampleKamu Ri ChiPas encore d'évaluation
- Joernal 3Document13 pagesJoernal 3Dyra DizhwarPas encore d'évaluation
- BMC Public Health: The Validity of Self-Reported Weight in US Adults: A Population Based Cross-Sectional StudyDocument10 pagesBMC Public Health: The Validity of Self-Reported Weight in US Adults: A Population Based Cross-Sectional Studyteamfrio827Pas encore d'évaluation
- Jurnal Reading TerjemahDocument15 pagesJurnal Reading TerjemahLela Nazila ItuSayaPas encore d'évaluation
- Regular Vigorous Physical Activity and Disability Development in Healthy Overweight and Normal-Weight Seniors: A 13-Year StudyDocument6 pagesRegular Vigorous Physical Activity and Disability Development in Healthy Overweight and Normal-Weight Seniors: A 13-Year StudymartinPas encore d'évaluation
- Paper EdulcoranteDocument13 pagesPaper EdulcoranteLizbeth HidalgoPas encore d'évaluation
- Ioi80217 764 7730Document7 pagesIoi80217 764 7730kern tranhPas encore d'évaluation
- IJBTR - Bio-tech-Studies On Leptin and MC4R Gene in Obese Population of South Western Province of Saudi Arabia Final ProofedDocument10 pagesIJBTR - Bio-tech-Studies On Leptin and MC4R Gene in Obese Population of South Western Province of Saudi Arabia Final ProofedTJPRC PublicationsPas encore d'évaluation
- A Group of 500 Women Whose Health May Depart Notably From The Norm: Protocol For A Cross-Sectional SurveyDocument12 pagesA Group of 500 Women Whose Health May Depart Notably From The Norm: Protocol For A Cross-Sectional Surveyhanna.oravecz1Pas encore d'évaluation
- Cardiometabolic Risks and Severity of Obesity in Children and Young AdultsDocument11 pagesCardiometabolic Risks and Severity of Obesity in Children and Young AdultsYosie Yulanda PutraPas encore d'évaluation
- Grip Strength, Body CompositionDocument8 pagesGrip Strength, Body CompositionFPSMPas encore d'évaluation
- Total and Central Obesity Among Elderly Hispanics and The Association With Type 2 DiabetesDocument9 pagesTotal and Central Obesity Among Elderly Hispanics and The Association With Type 2 DiabetesHui LiuPas encore d'évaluation
- Associations Between Obesity and Overweight and Fall RisksDocument6 pagesAssociations Between Obesity and Overweight and Fall RisksKelas CPas encore d'évaluation
- The Insulin Resistance Atherosclerosis Study (IRAS) Family StudyDocument7 pagesThe Insulin Resistance Atherosclerosis Study (IRAS) Family StudyChikezie OnwukwePas encore d'évaluation
- Physical Activity and Abnormal Blood Glucose Among Healthy Weight AdultsDocument6 pagesPhysical Activity and Abnormal Blood Glucose Among Healthy Weight Adultssyafiqa abdullahPas encore d'évaluation
- Body Weight-For-Height Relationships Predict Mortality in Maintenance Hemodialysis PatientsDocument13 pagesBody Weight-For-Height Relationships Predict Mortality in Maintenance Hemodialysis PatientsGazelle AraceliPas encore d'évaluation
- Obesity and The Risk of Cryptogenic Ischemic Stroke in Young AdultsDocument25 pagesObesity and The Risk of Cryptogenic Ischemic Stroke in Young AdultsKhalilullah ArsyiPas encore d'évaluation
- Influence of Nutritional Factors On Prevalence of DiabetesDocument10 pagesInfluence of Nutritional Factors On Prevalence of DiabetesVictorPas encore d'évaluation
- Hruby 2016Document7 pagesHruby 2016Sam Steven Hernandez JañaPas encore d'évaluation
- Eating Behavior Correlates of Adult Weight Gain and Obesity in Healthy Women Aged 55-65 yDocument8 pagesEating Behavior Correlates of Adult Weight Gain and Obesity in Healthy Women Aged 55-65 yWahyuningsih HamidPas encore d'évaluation
- Weight Loss and Mortality Among Free-Living Frail Elders: A Prospective StudyDocument6 pagesWeight Loss and Mortality Among Free-Living Frail Elders: A Prospective StudyAle TabaskoPas encore d'évaluation
- Obesitas 2 ObesitasDocument14 pagesObesitas 2 ObesitasJeremy KerrPas encore d'évaluation
- Kushi Et Al-2006-CA: A Cancer Journal For CliniciansDocument28 pagesKushi Et Al-2006-CA: A Cancer Journal For CliniciansM MuttaPas encore d'évaluation
- Association Between A Comprehensive Movement Assesment and MetabolicallyDocument9 pagesAssociation Between A Comprehensive Movement Assesment and MetabolicallyzunigasanPas encore d'évaluation
- Misclassification of Cardiometabolic Health When Using Body Mass Index Categories in NHANES 2005-2012Document5 pagesMisclassification of Cardiometabolic Health When Using Body Mass Index Categories in NHANES 2005-2012Maria Ignacia MacariPas encore d'évaluation
- Lifestyle Behaviors and Physician Advice For Change Among Overweight and Obese Adults With Prediabetes and Diabetes in The United States, 2006Document10 pagesLifestyle Behaviors and Physician Advice For Change Among Overweight and Obese Adults With Prediabetes and Diabetes in The United States, 2006Agil SulistyonoPas encore d'évaluation
- Obesity and Type 2 Diabetes ThesisDocument6 pagesObesity and Type 2 Diabetes Thesisafhbexrci100% (1)
- Ioi70171 2461 2468Document8 pagesIoi70171 2461 2468jimmyneutron1337Pas encore d'évaluation
- Analysis of Patterns of Patient Compliance After An Abnormal Pap Smear Result The Influence of Demographic Characteristics On Patient ComplianceDocument5 pagesAnalysis of Patterns of Patient Compliance After An Abnormal Pap Smear Result The Influence of Demographic Characteristics On Patient Compliancevyvie89Pas encore d'évaluation
- (Diabetes - Metabolism Research and Reviews 2017-Dec 19 Vol. 34 Iss. 2) Hou, Xuhong - Chen, Peizhu - Hu, Gang - Chen, Yue - Chen, Siyu - Wu, - Distribution and Related Factors of CardiomDocument32 pages(Diabetes - Metabolism Research and Reviews 2017-Dec 19 Vol. 34 Iss. 2) Hou, Xuhong - Chen, Peizhu - Hu, Gang - Chen, Yue - Chen, Siyu - Wu, - Distribution and Related Factors of CardiomEshetu WondimuPas encore d'évaluation
- Lifestyle Behaviors and Physician Advice For Change Among Overweight and Obese Adults With Prediabetes and Diabetes in The United States, 2006Document9 pagesLifestyle Behaviors and Physician Advice For Change Among Overweight and Obese Adults With Prediabetes and Diabetes in The United States, 2006Agil SulistyonoPas encore d'évaluation
- Serum Alpha-Carotene Concentrations and Risk of Death Among US AdultsDocument9 pagesSerum Alpha-Carotene Concentrations and Risk of Death Among US AdultsCherry San DiegoPas encore d'évaluation
- 2 MetabolicDocument8 pages2 MetabolicMartha Patricia López PimentelPas encore d'évaluation
- The Associations of Weekend Warrior Activity Patterns With The Visceral Adiposity Index in US Adults: Repeated Cross-Sectional StudyDocument11 pagesThe Associations of Weekend Warrior Activity Patterns With The Visceral Adiposity Index in US Adults: Repeated Cross-Sectional StudyAli HPas encore d'évaluation
- Non-Cephalic Presentation in Late Pregnancy: EditorialsDocument2 pagesNon-Cephalic Presentation in Late Pregnancy: EditorialsNinosk Mendoza SolisPas encore d'évaluation
- JAPI Body FatDocument6 pagesJAPI Body FatBhupendra MahantaPas encore d'évaluation
- tmp393C TMPDocument10 pagestmp393C TMPFrontiersPas encore d'évaluation
- Estilo de VidaDocument8 pagesEstilo de Vidai_anitaPas encore d'évaluation
- Oby 21181Document13 pagesOby 21181Mayra de CáceresPas encore d'évaluation
- Implications of Body Fat Distribution in An Older Twin PopulationDocument5 pagesImplications of Body Fat Distribution in An Older Twin PopulationAle TabaskoPas encore d'évaluation
- Da QingDocument18 pagesDa QingAlina PopaPas encore d'évaluation
- (2017) Handgrip Strength CutoffDocument7 pages(2017) Handgrip Strength CutoffDaniel Caldas PinedaPas encore d'évaluation
- השמנה וכאב מפרקיDocument5 pagesהשמנה וכאב מפרקינתנאל מושקוביץPas encore d'évaluation
- Prevalence of Overweight and Obesity and Weight Loss Practice Among Beijing Adults, 2011Document10 pagesPrevalence of Overweight and Obesity and Weight Loss Practice Among Beijing Adults, 2011Aboy GunawanPas encore d'évaluation
- K Winters Lab Report 4Document13 pagesK Winters Lab Report 4api-314083880Pas encore d'évaluation
- Body Mass Index and Ischemic and Hemorrhagic Stroke: A Prospective Study in Korean MenDocument7 pagesBody Mass Index and Ischemic and Hemorrhagic Stroke: A Prospective Study in Korean MenSri Wahyuni HarliPas encore d'évaluation
- Relationshipbetween RBSandobesityDocument2 pagesRelationshipbetween RBSandobesityasdPas encore d'évaluation
- Selección de Resúmenes de Menopausia Semana Del 6 Al 12 de Agosto de 2014Document5 pagesSelección de Resúmenes de Menopausia Semana Del 6 Al 12 de Agosto de 2014rocksurPas encore d'évaluation
- IMC-Dexa-gordura-Measuring Adiposity in Patients - The Utility of Body Mass Index (BMI), Percent Body Fat, and LeptinDocument8 pagesIMC-Dexa-gordura-Measuring Adiposity in Patients - The Utility of Body Mass Index (BMI), Percent Body Fat, and LeptinFabrício Boscolo Del VecchioPas encore d'évaluation
- The Relation of Overweight To Cardiovascular Risk Factors Among Children and Adolescents: The Bogalusa Heart StudyDocument10 pagesThe Relation of Overweight To Cardiovascular Risk Factors Among Children and Adolescents: The Bogalusa Heart StudyaocuPas encore d'évaluation
- Am. J. Epidemiol.-2003-Ma-85-92Document8 pagesAm. J. Epidemiol.-2003-Ma-85-92Eima Siti NurimahPas encore d'évaluation
- Smoking and Blood Sugar Level: An Important Cause of Cardiovascular Diseases Among AustraliansDocument11 pagesSmoking and Blood Sugar Level: An Important Cause of Cardiovascular Diseases Among Australiansinflibnet inflibnetPas encore d'évaluation
- Prevalence and Associated Factors of Sarcopenia Among Elderly in Brazil: Findings From The Sabe StudyDocument7 pagesPrevalence and Associated Factors of Sarcopenia Among Elderly in Brazil: Findings From The Sabe StudyLUCAS ALVES SANTOSPas encore d'évaluation
- The Metabolic Syndrome, Diabetes, and Alzheimer's DiseaseDocument7 pagesThe Metabolic Syndrome, Diabetes, and Alzheimer's DiseaseMICHAELATTOPas encore d'évaluation
- Quality of Life of Colorectal Cancer Patients A Literature ReviewDocument6 pagesQuality of Life of Colorectal Cancer Patients A Literature Reviewddyuss90Pas encore d'évaluation
- E L B C R F U S e K D PDocument10 pagesE L B C R F U S e K D PBatta ZahranPas encore d'évaluation
- Eating Disorders in Boys and MenD'EverandEating Disorders in Boys and MenJason M. NagataPas encore d'évaluation
- Association Between Frailty Syndrome and Sedentary Behavior Among Community-Dwelling Older Adults in The Amazon Region: A Cross-Sectional StudyDocument8 pagesAssociation Between Frailty Syndrome and Sedentary Behavior Among Community-Dwelling Older Adults in The Amazon Region: A Cross-Sectional StudyFabianoBelemPas encore d'évaluation
- Effects and Mechanisms of Resveratrol On Aging and Age - Related DiseasesDocument15 pagesEffects and Mechanisms of Resveratrol On Aging and Age - Related DiseasesAna MariaPas encore d'évaluation
- KAATSU Magazine Volume 02 Issue 02 RDocument98 pagesKAATSU Magazine Volume 02 Issue 02 RKanizsa EnergetikaPas encore d'évaluation
- Antioxidants: Lipid Peroxidation-Derived Aldehydes, 4-Hydroxynonenal and Malondialdehyde in Aging-Related DisordersDocument17 pagesAntioxidants: Lipid Peroxidation-Derived Aldehydes, 4-Hydroxynonenal and Malondialdehyde in Aging-Related DisordersffwasitoPas encore d'évaluation
- Effects of Aging and Coping Strategies of Older Adults (GROUP 3)Document16 pagesEffects of Aging and Coping Strategies of Older Adults (GROUP 3)Michael AmandyPas encore d'évaluation
- Fitness Quiz:: Test Your Exercise KnowledgeDocument2 pagesFitness Quiz:: Test Your Exercise Knowledgemehak sarwanPas encore d'évaluation
- Nutritionist-Dietitian Association of The Philipiines 59th ConventionDocument36 pagesNutritionist-Dietitian Association of The Philipiines 59th ConventionOlive FactorizaPas encore d'évaluation
- The Open Orthopaedics Journal: A Review of Handgrip Strength and Its Role As A Herald of HealthDocument6 pagesThe Open Orthopaedics Journal: A Review of Handgrip Strength and Its Role As A Herald of HealthApri PerdanaPas encore d'évaluation
- Peter Collins Nutrition Support Severe Respiratory Disease 3 Slides PPDocument19 pagesPeter Collins Nutrition Support Severe Respiratory Disease 3 Slides PPKim Nana UlfaPas encore d'évaluation
- Body Composition Assessment MethodsDocument7 pagesBody Composition Assessment MethodslianaidrisPas encore d'évaluation
- Age, Gender, and Muscular Strength - Ben F. HurleyDocument4 pagesAge, Gender, and Muscular Strength - Ben F. HurleyOz FalchiPas encore d'évaluation
- The Challenges of Nutritional Assessment in Geriatric Cancer Patients - UpdatedDocument31 pagesThe Challenges of Nutritional Assessment in Geriatric Cancer Patients - Updatedsuzana78m695Pas encore d'évaluation
- Pathophysiological Background: Potential Role of Sarcopenia As A Driver of DecompensationDocument100 pagesPathophysiological Background: Potential Role of Sarcopenia As A Driver of DecompensationDiego V.G.Pas encore d'évaluation
- Frailty Assessment: From Clinical To Radiological ToolsDocument32 pagesFrailty Assessment: From Clinical To Radiological ToolsMonicaPas encore d'évaluation
- Nutrition Priorities in Obese Critically Ill.10Document11 pagesNutrition Priorities in Obese Critically Ill.10Iván OsunaPas encore d'évaluation
- Nutrition in Chronic Liver Disease EASL CPGDocument49 pagesNutrition in Chronic Liver Disease EASL CPGJack JacksonPas encore d'évaluation
- The Health Benefits of Resistance Exercise Beyond.2Document5 pagesThe Health Benefits of Resistance Exercise Beyond.2CamiloAndresRinconYPas encore d'évaluation
- Julian 2018Document14 pagesJulian 2018Harsh BohraPas encore d'évaluation
- Disfagia Sarcopenica y Fragilidad OralDocument23 pagesDisfagia Sarcopenica y Fragilidad OralPatriciaPas encore d'évaluation
- David Heber: Powerful Science ConfidenceDocument23 pagesDavid Heber: Powerful Science ConfidenceErick RiveraPas encore d'évaluation
- Global Variation in Grip Strength - A Systematic Review and Meta-Analysis of Normative DataDocument8 pagesGlobal Variation in Grip Strength - A Systematic Review and Meta-Analysis of Normative DataMárciaPereiraPas encore d'évaluation
- M8jhilClgtVjCfLCM87 PdfsDocument20 pagesM8jhilClgtVjCfLCM87 PdfsNguyễn Đình HánPas encore d'évaluation
- Narici Et Al. 2003 - EnvelhecimentoDocument7 pagesNarici Et Al. 2003 - EnvelhecimentoFábio LanferdiniPas encore d'évaluation
- 46 Dani Preventivne Medicine-Zbornik RezimeaDocument182 pages46 Dani Preventivne Medicine-Zbornik RezimeaМилош МујовићPas encore d'évaluation
- 1 s2.0 S0929664615003460 MainDocument7 pages1 s2.0 S0929664615003460 MainEva GarciaPas encore d'évaluation