Académique Documents
Professionnel Documents
Culture Documents
EOR Toxic Poison
Transféré par
sarahabdullahCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
EOR Toxic Poison
Transféré par
sarahabdullahDroits d'auteur :
Formats disponibles
Name poison
Salicylate
Paracetamol
Barbiturates
SAB & LAB
GIT
Injection sites
Liver
Absorption
Stomach
GIT
Metabolism
Liver
Excretion
Kidney
Liver
Conjugation with
glutathione
-
Toxic dose
200-300mg/kg
Fatal: >120mg%
10 grams
140mg/kg
Pathophysiology
+ respiratory center->
Glutathione depleted
resp. alkalosis
causing centrilobular
Metabolic Acidosis:
hepatic necrosis
Accumulation of
metabolites
Severe dehydration
Interfere Vita-K
Enhance G6P activity ->
hypoglycaemia
CNS: depression
GABA like-action
CVS: shock
GIT: depress smooth
muscle
Kidney: depress kidney
function
Skin: bullae; toes and
fingers
Depress CNS
Local irritant on
mucous membrane
Toxic effect on liver,
kidney and heart
Tolerance, dependence
and withdrawal
syndrome
Induce intense
stimulation of CNS
Release of
catecholamines
-epinephrine
-norepinephrine
-dopamine
Clinical picture
Hyperventilation,
sweating & acid base
disorders
Metabolic acidosis
Hypoglycaemia
Hypoprothrombinemia
Cyanosis, oliguria,
renal failure &
pulmonary oedema
S1: nausea, vomiting
and diaphoresis
S2: hepatic tenderness,
elevation of bilirubin
and prolongation of
Prothrombin time
S3: hepatic necrosis,
coagulation defects,
jaundice, renal failure
S4: death cause by
hepatic failure
CNS: stupor and deep
coma
Resp: slow and shallow
with cyanosis
CVS: arrhythmia,
hypotension
Pupil: constrict->
dilated
Nausea and vomiting
on and empty stomach
CNS: acute anxiety rxn
Euphoria, Hallucination
Aggressive and violent
CVS: tachycardia,
palpitation,
hypertension,
Muscular dyskinesia
GIT: N, V, D, dry mouth
Skin: urticaria,
erythema of the face
Investigation
Urine test
Plasma salicylates level
ABG, blood pH, acid
base status
Prothrombin level
Blood glucose
ECG, chest X-ray
Serum acetaminophen
level, 4-6hours after
Liver test
Renal test
Blood glucose test
Prothrombin test
Undetectable in
plasma
Determination of
plasma
trichloroethanol
Urine and blood test
ECG, CT, ABG
Acid base status
Electrolytes
Kidney function test
Elevation of Creatine
kinase
Treatment/
Antidote
Haemodialysis
Symptomatic
treatment
ABCD
5% dextrose IV in 10
hours
Blood/ fresh plasma
transfusion
Injection of clotting
factor or vita-K
Liver transplant
Antidote:
N-acetycysteine (NAC)
Act as glutathione
substitute
CNS: stupor->coma
CVS: clammy skin, low
BP, oliguria, weak
pulse, sweating
Respiration: slow and
shallow, cheynestokes,
cyanosis
Hypoxic paralytic
pupillary dilatation
Hypothermia
Paralytic ileus
Bullous skin
Coma +resp depress+
hypothermia
Colour test on urine
Plasma barbiturate
level
Acid base status, ABG,
ECG, Chest X-ray
Kidney function test
Artificial ventilation
and O2 inhalation
NEVER elevate the BP
to normal level
Alkalinisation of the
urine by IV NaHCO3
Symptomatic
treatment
ABC
Demulcent and
activated charcoal
Lavage or emesis are
contraindicate cause of
irritant substance
Haemoperfusion
Haemodialysis less
effective
A-B
C: hypertension by
phentolamine
D: ipecac, activated
charcoal + cathartic,
lavage
E: alkalinisation of
urine by NaHCO3
Haemodialysis
Antipsychotic drugs
Symptomatic
treatment.
SAB-poorly by renal
and good hepatic
degradation
LAB- good by renal
Read barbiturate
dependence page: 152
Chloral hydrate
Amphetamine
GIT
Oral/ IV administration
GIT and Blood
Liver
Hydroxylation and
deamination
Renal
Non-metabolized is
pH-dependent
In acidic urine only
Over 100mg
Liver, kidneys, RBC
(trichloroethanol and
trichloro-acetic acid)
Renal in urine
Theophylline
(asthma)
Oral administration
Carbon monoxide
Chloride
OPI
Lungs
External exposure and
ingestion
Liver
P450 cytochrome
oxidase
Adult: 10%unchange
Neonates: 50%
unchanged
Bound to Hb
life 4-5 hours
GIT, skin, conjunctiva,
lungs
Liver
Oxidation and
hydrolysis by esterase
Urine and faeces
Decrease metabolism
leads increase toxicity
>20ug/ml
Occurs in:
Liver and heart failure
Drug inhibit P450
Adenosine blocked-loss
heart ve feedback
Endogenous release of
catecholamine - CVS and
metabolic toxicity
Increase intracellular Cahigh contraction
GIT: N, V, D, Bleeding
CNS: seizures, lead to
rhabdomyolysis,
lethargy, coma
CVS: tachyarrhythmia,
hypotension & cardiac
arrest
Metabolic: respiratory
alkalosis, metabolic
acidosis, hypokalemia,
hyperglycaemia,
hypercalcaemia
Serum theophylline
concentration
ECG, Blood glucose,
electrolytes, ABG, acid
base status, brain CT
Myoglobin in urine
Chest X-ray
COHb level above
15%
Produce acidic
condition and
corrosive
Cl+H2O will produce
HCL and Hypochlorus
acid
Formation of
chloramine and thiol
radical
According to ChE
inhibition
Pulmonary edema
Skin bullae
Lactic metabolic
acidosis
Arrhythmia, ECG
changes
Coma, convulsion
Mucous membrane
irritation
Cough, wheezing,
haemoptysis
Nausea, vomiting,
metabolic acidosis
COHb level
ABG
Blood glucose
Electrolytes level
ECG, CT, X-ray
Evidence of exposure
Sign and symptoms
Chest X-ray
Muscarinic effect:
Wet findings due to
excessive secretion
Constricted pupil
(DUMBELS)
Nicotinic effect:
Muscle weakness
Dilated pupil
Tachycardia &
hypertension
CNS: anxiety,
convulsion, coma
Assay by erythrocyte
or plasma ChE activity
level:
20-50% mild
10-20% moderate
<10% severe
A-B
C: propranolol for
tachyarrhythmia
D: cant use ipecac
Lavage and activated
charcoal + cathartic
E: Haemoperfusion
Haemodialysis if
perfusion unavailable.
Symptomatic
treatment.
100% oxygen
inhalation
Hyperbaric oxygen
Symptomatic
treatment and relieve
treatment.
Respiratory system
Shift curve to left and
make O2 less
available
Inhibition of acetyl
cholinesterase in
nervous system and
myoneural junction
Stimulation-> paralyze
ABC: suction of
secretion and IV fluid
avoid dehydration
Antidote:
Atropine- until
atropinisation known
2mg IV repeated every
10-15 min
Oximes- break the
bond, direct react and
detox, anticholinergic
effects.
Vous aimerez peut-être aussi
- Lecture+24 +25+diureticsDocument69 pagesLecture+24 +25+diureticsGhina RizwanPas encore d'évaluation
- Acute Renal Failure Powerpoint PresentationDocument18 pagesAcute Renal Failure Powerpoint PresentationSteven Paul DaclesPas encore d'évaluation
- PoisoningDocument23 pagesPoisoningseed1876Pas encore d'évaluation
- Acute Kidney Injury: DR Hodan Ahmed Dept of Pediatrics and Child Health Amoud Medical School, AUDocument32 pagesAcute Kidney Injury: DR Hodan Ahmed Dept of Pediatrics and Child Health Amoud Medical School, AUMohamoud MohamedPas encore d'évaluation
- Obstructive Jaundice Pathophysiology and Workup: DR - Kiran Kumar.G Apollo Bgs HospitalsDocument70 pagesObstructive Jaundice Pathophysiology and Workup: DR - Kiran Kumar.G Apollo Bgs HospitalsRavinderjit SinghPas encore d'évaluation
- Acute Liver FailureDocument3 pagesAcute Liver FailureElisabeth F. OjhaPas encore d'évaluation
- Defeating Dementia - Mnemonics and Lists From EMRCS PhysiologyDocument7 pagesDefeating Dementia - Mnemonics and Lists From EMRCS PhysiologymyscribePas encore d'évaluation
- Salicylate Poisoning: WWW - Anaesthesia.co - inDocument23 pagesSalicylate Poisoning: WWW - Anaesthesia.co - inimmortalneoPas encore d'évaluation
- Interpretation of Lab Test ProfilesDocument15 pagesInterpretation of Lab Test ProfilesNicole Alexandra KhoPas encore d'évaluation
- Bu Widy - Ginjal (Patofisiologi & Penatalaksanaan GGK)Document40 pagesBu Widy - Ginjal (Patofisiologi & Penatalaksanaan GGK)Ravinder SinghPas encore d'évaluation
- Biochemisty Cheat SheetsDocument4 pagesBiochemisty Cheat SheetsNatalie KingPas encore d'évaluation
- Chronic Renal FailureDocument3 pagesChronic Renal FailureirismgallPas encore d'évaluation
- Chronic Renal FailureDocument3 pagesChronic Renal FailureIvana Yasmin Bulandres100% (2)
- Alcoholic Liver DiseaseDocument27 pagesAlcoholic Liver DiseaseIsaac MwangiPas encore d'évaluation
- Acute Liver Failure in ChildrenDocument34 pagesAcute Liver Failure in ChildrenEpahPas encore d'évaluation
- Diuretic and UtiDocument43 pagesDiuretic and UtiAmanuel MaruPas encore d'évaluation
- General Clinical ManifestationsDocument17 pagesGeneral Clinical ManifestationsYohannis AsefaPas encore d'évaluation
- MetabolicDocument23 pagesMetabolicbtidipPas encore d'évaluation
- Medical Managemen Hodgskin - SDocument18 pagesMedical Managemen Hodgskin - SbulikakoPas encore d'évaluation
- Ald 180226073505Document39 pagesAld 180226073505TianKaunangPas encore d'évaluation
- MetabolismDocument39 pagesMetabolismTiffany KnepperPas encore d'évaluation
- Hypercalcemia: Bibek Ghimire 3 Batch, PAHSDocument25 pagesHypercalcemia: Bibek Ghimire 3 Batch, PAHSBibek GhimirePas encore d'évaluation
- Patofisiologi & Penatalaksanaan Gagal Ginjal KronikDocument34 pagesPatofisiologi & Penatalaksanaan Gagal Ginjal KronikAvenaAthaliaPas encore d'évaluation
- Liver Function TestDocument5 pagesLiver Function TestAnne Sison100% (1)
- Studi Kasus Penyakit HatiDocument27 pagesStudi Kasus Penyakit HatiEfraim MangalukPas encore d'évaluation
- PENYAKIT HATI (Uas)Document27 pagesPENYAKIT HATI (Uas)Cinsy PaskalinePas encore d'évaluation
- Liver Function Tests (Sem)Document6 pagesLiver Function Tests (Sem)Francisco NiegasPas encore d'évaluation
- Electrolyte ImbalanceDocument43 pagesElectrolyte ImbalanceJoshua JoPas encore d'évaluation
- Fluids and Electrolytes, Acid-Base ImbalancesDocument15 pagesFluids and Electrolytes, Acid-Base ImbalancesJherome FernandoPas encore d'évaluation
- Alcoholic Liver DiseaseDocument22 pagesAlcoholic Liver DiseaseRaju NiraulaPas encore d'évaluation
- DiureticsDocument28 pagesDiureticsmohsen mirdamadiPas encore d'évaluation
- Off Tag Assessment (Surgery)Document19 pagesOff Tag Assessment (Surgery)Ahmad LiewPas encore d'évaluation
- Diuretics: Chris Hague, PHDDocument29 pagesDiuretics: Chris Hague, PHDranachamanPas encore d'évaluation
- Renal Failure: Manelle R. Singzon BSN 4A1-1Document30 pagesRenal Failure: Manelle R. Singzon BSN 4A1-1Manelle SingzonPas encore d'évaluation
- Alcoholic Liver Disease: Last Updated: January 19, 2024Document16 pagesAlcoholic Liver Disease: Last Updated: January 19, 2024Tselmeg TselmegPas encore d'évaluation
- IDEXX CBC Chem ExplainedDocument38 pagesIDEXX CBC Chem Explainedmmatthew74Pas encore d'évaluation
- Hyponatremia & Hypernatremia: Prof. Dr. E. J. Joseph, SPPD-KGHDocument32 pagesHyponatremia & Hypernatremia: Prof. Dr. E. J. Joseph, SPPD-KGHJeffri SetiawanPas encore d'évaluation
- Cirrhosis of LiverDocument106 pagesCirrhosis of LiveraahadPas encore d'évaluation
- ATP Production AEROBIC Metabolism: ST STDocument11 pagesATP Production AEROBIC Metabolism: ST STSiir Pwnsalot100% (1)
- CCC Gastrointestinal & DigDocument13 pagesCCC Gastrointestinal & DigChaitya DesaiPas encore d'évaluation
- 07 Liver Tunction TestsDocument41 pages07 Liver Tunction TestsPaulina PaskeviciutePas encore d'évaluation
- End-Stage Renal DiseaseDocument3 pagesEnd-Stage Renal DiseaseAkira Pongchad B100% (1)
- Fluid and Electrolyte Imbalances Part 2Document47 pagesFluid and Electrolyte Imbalances Part 2Abinaya RanganathanPas encore d'évaluation
- Renal Failure Acute and Chronic: NPN 200 Medical Surgical Nursing IDocument31 pagesRenal Failure Acute and Chronic: NPN 200 Medical Surgical Nursing IJuan ValadezPas encore d'évaluation
- Electrolyte and Metabolic Disturbances Electrolyte and Metabolic DisturbancesDocument58 pagesElectrolyte and Metabolic Disturbances Electrolyte and Metabolic DisturbancesAbdulrahman Mahmoud GhaziPas encore d'évaluation
- Exam 2 STUDY GUIDEDocument121 pagesExam 2 STUDY GUIDEJulie BrandtPas encore d'évaluation
- Acute Kidney InjuryDocument60 pagesAcute Kidney InjuryAbegail Fermanejo-GeneraoPas encore d'évaluation
- Salicylates Tca ToxicityDocument54 pagesSalicylates Tca Toxicityapi-298936498Pas encore d'évaluation
- Hepatic EncephalopathyDocument35 pagesHepatic EncephalopathyDeeksha GoyalPas encore d'évaluation
- Diabetic Ketoacidosis: Dr. Kaustuv de Fellow (3 Yr.) Critical Care MedicineDocument31 pagesDiabetic Ketoacidosis: Dr. Kaustuv de Fellow (3 Yr.) Critical Care MedicineKaustuv DePas encore d'évaluation
- Acid Base Balance and DisordersDocument25 pagesAcid Base Balance and DisordersIsmail Vokshi100% (1)
- Renal, Fluid & ElectrolyeDocument21 pagesRenal, Fluid & ElectrolyeremerosePas encore d'évaluation
- Electrolytedisturbances 111102083753 Phpapp02Document137 pagesElectrolytedisturbances 111102083753 Phpapp02bobbyfildianPas encore d'évaluation
- Chronic Renal FailureDocument54 pagesChronic Renal FailureAkia Cayasan BayaPas encore d'évaluation
- Fluid and Electrolyte Disturbance - Yoana AngelineDocument43 pagesFluid and Electrolyte Disturbance - Yoana AngelineYoana AngelinePas encore d'évaluation
- Renal Disease of Small AnimalsDocument46 pagesRenal Disease of Small AnimalsTahir KasimPas encore d'évaluation
- Pathophysiology of DMDocument5 pagesPathophysiology of DMRgn Mckl100% (3)
- Chronic Kidney Disease: DR - SarmisthaDocument19 pagesChronic Kidney Disease: DR - SarmisthaGebby MamuayaPas encore d'évaluation
- Liver Cirrhosis, A Simple Guide To The Condition, Treatment And Related DiseasesD'EverandLiver Cirrhosis, A Simple Guide To The Condition, Treatment And Related DiseasesPas encore d'évaluation
- Fatty Liver: Recipes and Guide to Prevent, Cure and Reverse Fatty Liver Disease, Lose Weight and Promote Good HealthD'EverandFatty Liver: Recipes and Guide to Prevent, Cure and Reverse Fatty Liver Disease, Lose Weight and Promote Good HealthPas encore d'évaluation
- Hizon, DrugsDocument4 pagesHizon, DrugsDan HizonPas encore d'évaluation
- Genodermatosis MCQsDocument152 pagesGenodermatosis MCQsDr.Tawheed88% (8)
- Adult DysphagiaDocument9 pagesAdult DysphagiaDevara PattyPas encore d'évaluation
- Orange Peel MSDSDocument4 pagesOrange Peel MSDSarvind kaushikPas encore d'évaluation
- Free Dive Training Schedules - Land and Pool Based Training SessionsDocument10 pagesFree Dive Training Schedules - Land and Pool Based Training Sessionssjf540100% (1)
- Drug Tariff July 2014 PDFDocument784 pagesDrug Tariff July 2014 PDFGisela Cristina MendesPas encore d'évaluation
- DLR - Tips and Tricks PDFDocument9 pagesDLR - Tips and Tricks PDFSelda CoktasarPas encore d'évaluation
- Annexure IDocument372 pagesAnnexure IsfarithaPas encore d'évaluation
- DC-TMD SQ Shortform 2013-05-12Document2 pagesDC-TMD SQ Shortform 2013-05-12Luz MendozaPas encore d'évaluation
- Ethnobotany and EthnopharmacologyDocument29 pagesEthnobotany and EthnopharmacologyJohn CaretakerPas encore d'évaluation
- Ijmrhs Vol 3 Issue 1Document228 pagesIjmrhs Vol 3 Issue 1editorijmrhsPas encore d'évaluation
- Anesthesia Drug StudyDocument3 pagesAnesthesia Drug Studyczeremar chanPas encore d'évaluation
- Basic Theories of Traditional Chinese Medicine PDFDocument194 pagesBasic Theories of Traditional Chinese Medicine PDFElanghovan Arumugam100% (31)
- Hemodynamics and Diagnosis Venous Disease-Jvs 1207Document21 pagesHemodynamics and Diagnosis Venous Disease-Jvs 1207Fahrudin ŠabanovićPas encore d'évaluation
- Gas Exchange Text Book Based Revision NoteDocument6 pagesGas Exchange Text Book Based Revision NoteJamesPas encore d'évaluation
- Art Theraphy AutismDocument2 pagesArt Theraphy AutismMatheaFiliPas encore d'évaluation
- 35521Document12 pages35521Kyle MaogPas encore d'évaluation
- Case Study GerdDocument3 pagesCase Study Gerdapi-287249002Pas encore d'évaluation
- Endocrine Methodologies Chapter 4 9-1.2012 PDFDocument26 pagesEndocrine Methodologies Chapter 4 9-1.2012 PDFLeora LiPas encore d'évaluation
- Nursing Worksheet Template 1 1Document2 pagesNursing Worksheet Template 1 1api-651287771Pas encore d'évaluation
- Benign Diseases of ThyroidDocument70 pagesBenign Diseases of ThyroidMounica MekalaPas encore d'évaluation
- PT Ortho ProblemsDocument129 pagesPT Ortho ProblemsvinaymanPas encore d'évaluation
- Case Files Pharmacology, 3rd Edition (2017!07!18 02-28-27 UTC)Document375 pagesCase Files Pharmacology, 3rd Edition (2017!07!18 02-28-27 UTC)imperiouxx100% (2)
- Clark IndigestionDocument50 pagesClark IndigestionRaveendra MungaraPas encore d'évaluation
- Psych-K Practical ApplicationsDocument10 pagesPsych-K Practical Applicationsdeluca4482% (17)
- MindfulnessDocument192 pagesMindfulnessNatalia Rojas Sattui96% (26)
- Mindfulness and Psychology-Mark WilliamsDocument7 pagesMindfulness and Psychology-Mark WilliamsssanagavPas encore d'évaluation
- Acute GastroenteritisDocument56 pagesAcute Gastroenteritisneil052298% (46)
- Downward Movement - Left Hand Only: (Figure 3-7Document20 pagesDownward Movement - Left Hand Only: (Figure 3-7mamun31Pas encore d'évaluation
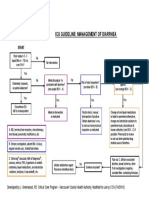
- Icu Guideline: Management of Diarrhea: StartDocument1 pageIcu Guideline: Management of Diarrhea: StartGracia VionaPas encore d'évaluation