Académique Documents
Professionnel Documents
Culture Documents
Care of Patient With Musculoskeletal Disorders
Transféré par
Bryan Mae H. DegorioCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Care of Patient With Musculoskeletal Disorders
Transféré par
Bryan Mae H. DegorioDroits d'auteur :
Formats disponibles
Care of Patient with Musculoskeletal Disorders
Bryan Mae H. Degorio, RN, MAN
I.
Fractures
- Is a disruption or break in the continuity of the structure of the bone.
- Occurs when the stress placed on the bone is greater that the bone can absorb
- Fracture maybe caused by direct blow, crushing forces, sudden twisting motion and extreme
muscle contraction
- When the bone is broken- adjacent structure are also affected resulting in soft tissue edema,
hemorrhage into the muscles and joint dislocation, ruptured tendons, severed nerves and
damage blood vessels.
-
Types of Fractures:
1. Complete Fracture
frequently
- involves a break across the entire section of the bone and is
displaced
2. Incomplete Fracture - involves the break through a part of the cross section of the bone
3. Closed Fracture
- is the one that does not cause break in the skin
4. Open Fracture
- is the one in which the skin or mucus membrane is disrupted
5. Pathologic Fracture - through an area of diseased bone
-
Pattern of Fractures
1. Greenstick Fracture
2. Transverse
3. Oblique
4. Spiral
5. Comminuted
6. Depressed
facial bones)
7. Compression
8. Avulsion
attachment
9. Impacted
- one side of the bone is broken and the other side is bent
- a fracture that is straight across the bone
- an angle across the bone
- twist around the shaft of the bone
- a fracture in which the bone has splintered into several fragments
- fragments area are driven inward (commonly seen in skull and
- bone collapse in on itself (seen in vertebral fractures)
- bone fragment has been pulled away by a tendon
- bone fragments is driven into another bone fragment
Manifestations:
1. Pain
Is continuous and increasing in severity until the bone fragment is immobilized
The spasm of the surrounding muscles serve as a temporary splints to minimize
further movement of the fracture limb.
2. Loss of function
The normal function of the muscle depends on the integrity of the bone to which
they are attached.
Pain may also contribute to the loss of function
3. Deformity
Due to displacement, angulation, or rotation of the fragments in the fracture as
seen as loss of normal bony contour.
It can be detected by comparing the injured limb with the uninjured limb.
Deformity can also be due to the soft tissue swelling
4. Shortening
Is due to the contraction of the muscles that are attached below and above the
fracture site.
The fragments overlap by as much as 2.5-5 cm (1-2 inches)
5. Crepitus
Is a grating sensation felt when bone fragments are rubbed against each other.
Note: testing for crepitus may produce further damage to the area.
6. Swelling and discoloration (ecchymosis)
Due to trauma and bleeding in the tissue
These may develop for several hours after injury.
Management:
A. Goals of Fracture Treatment:
Anatomic realignment of the bone fragment
Immobilization to maintain realignment
Restoration of normal or near normal function of the injured part
B. Three step processes in managing bone fracture:
1. Reduction- refers to the restoration of the fragments into anatomic position and
alignment (pls. refer to your notes on the general management of client with
musculoskeletal disorders)
a. Closed reduction- is a non-surgical, manual realignment of the bone. Traction
and counter traction maybe applied.
b. Open reduction- is the correction of bone alignment through a surgical
incision. It includes internal fixation of the fracture with the use of wires,
screws, pins, plates, intermedullary rods or nails.
2. Immobilization- maintaining reduction until bone healing occurs.
a. It can be achieved with use of casts, splints and tractions.
3. Rehabilitation- regaining normal function of the affected part.
C. Drug Therapy
1. Central and peripherally acting muscle relaxant can be given to relieve the pain
associated with muscle spasm.
a. It includes: carisoprodol (Soma), cyclobenzaprine (Flexeril) and methocarbamol
(Robaxin)
2. Tetanus immunoglobulins may also be given for those who has not been previously
immunized.
D. Nutritional therapy
1. Dietary therapy should include ample protein (1g/kg of body weight), vitamins (B, C
and D) and calcium, phosphorus and magnesium to ensure optimal soft tissue and
bone healing.
-
Complications of Fracture:
A. Compartment Syndrome:
Is a condition in which elevated intracompartment pressure within a confined
myofacial compartment compromises the neurovascular function of tissue within
the space.
Possible causes:
a. A reduction in the size of the muscle compartment because the enclosing
muscle fascia is too tight or a cast or dressing is constrictive.
b. An increase in the muscle compartment content because of the edema or
hemorrhage associated with variety of problems (ex: fractures and crush
injuries)
As a result, the pressure within the muscle compartment may increase to such an
extent as to decrease circulation to the area causing nerve and muscle anoxia and
necrosis.
Assessment and Diagnostics:
a. Neurovascular assessment:
paresthesia, unrelenting pain, and hypoesthesia and possible
numbness to the area.
motion is evaluated by asking the patient to move his toes or
fingers
paralysis may indicate nerve damage
peripheral circulation can be assessed by color, temperature,
capillary refill time, swelling and pulses
b. There is a deep, throbbing and unrelenting pain which is greater than
expected and is not controlled by opioids.
Management:
a. Physician must be notified immediately when suspecting for neurovascular
compromise.
b. Elevate the extremities at the level of the heart, release of restrictive
dressing (dressing or cast) or both.
c. If conservative management do not restore the tissue perfusion and relieve
pain within 1 hour, a fasciotomy compression with excision of the fibrous
membrane that covers and maybe needed to relieve the constrictive
muscle.
B. Fat Embolism Syndrome
Is characterized by the presence of the systemic fat lobules from factures that are
distributed into the tissues and organs after a traumatic skeletal injury.
Theories of the development of FES:
a. Mechanical theory- fat is released from the marrow of the injured bone and
is driven out into the circulation by the increase intramedullary pressure
causing it to lodge in the pulmonary circulation.
b. Biochemical theory- catecholamines are released at the time of trauma
mobilizing free fatty acid from the adipose tissue causing the loss of
chylomicron emulsion stability. Chylomicrons form large fat globules that
eventually lodge in the lungs.
Manifestations:
a. Hemorrhagic interstitial pneumonitis that produces signs and symptoms of
ARDS such as chest pain, tachypnea, cyanosis, dyspnea, apprehension,
tachycardia and decreases partial pressure of arterial oxygen
Management:
a. The management is directed to prevention:
immediate immobilization, minimal movement of the fracture,
adequate support for the fractured bone and maintaining fluid and
electrolyte balance.
b. Respiratory support
Administration of oxygen in high concentration.
Controlled-volume ventilation with positive end-expiratory pressure
may be used to prevent or treat pulmonary edema.
Corticosteroid to treat inflammatory lung reaction and cerebral
edema
Morphine maybe given to relive acute pain and anxiety
Vasoactive medication can be given to prevent shock and
hypotension
Vous aimerez peut-être aussi
- Cardiac AssessmentDocument7 pagesCardiac AssessmentBryan Mae H. Degorio75% (4)
- Bipolar DisordersDocument63 pagesBipolar DisorderselvinegunawanPas encore d'évaluation
- Documentation and ReportingDocument32 pagesDocumentation and ReportingBryan Mae H. Degorio100% (1)
- EmbryologyDocument26 pagesEmbryologyBryan Mae H. Degorio100% (2)
- Quiz - NeurologicalDocument3 pagesQuiz - NeurologicalRebekah HPas encore d'évaluation
- Eyes and EarsDocument17 pagesEyes and Earsdlneisha61100% (2)
- Case Studies For Bowel EliminationDocument2 pagesCase Studies For Bowel EliminationBryan Mae H. Degorio100% (2)
- Sportsnutritionguide PDFDocument543 pagesSportsnutritionguide PDFNorferatu100% (1)
- NCMB312 RLE OR Instrumentation Sutures Principles of Aseptic Techniques PDFDocument70 pagesNCMB312 RLE OR Instrumentation Sutures Principles of Aseptic Techniques PDFwokorow100% (1)
- Psychotropic Drugs: Bryan Mae H. DegorioDocument65 pagesPsychotropic Drugs: Bryan Mae H. DegorioBryan Mae H. Degorio100% (2)
- Gouty ArthritisDocument8 pagesGouty ArthritisNik2Pas encore d'évaluation
- Ear DisordersDocument5 pagesEar DisordersClara De Guzman100% (2)
- Medical ImagingDocument8 pagesMedical ImagingMansourPas encore d'évaluation
- Medical Surgical Nursing Orthopedic NursingDocument141 pagesMedical Surgical Nursing Orthopedic Nursingroger92% (12)
- Nursing Lecture OrthopedicDocument24 pagesNursing Lecture OrthopedicAedge010100% (2)
- Orthopedic NursingDocument237 pagesOrthopedic Nursingɹǝʍdןnos100% (24)
- EndocrineDocument12 pagesEndocrineAna FelPas encore d'évaluation
- Medical Surgical Nursing: By: Mr. Emerson AliswagDocument137 pagesMedical Surgical Nursing: By: Mr. Emerson AliswagMarie JhoanaPas encore d'évaluation
- Gastrointestinal Tract System NotesDocument8 pagesGastrointestinal Tract System NotesCarl Elexer Cuyugan Ano100% (1)
- The Nurse Would Evaluate That The Client Understands HisDocument10 pagesThe Nurse Would Evaluate That The Client Understands HisFilipino Nurses Central100% (1)
- Medical Surgical NursingDocument179 pagesMedical Surgical NursingLloyd Rafael EstabilloPas encore d'évaluation
- Allergies or Food Intolerances.: Therapeutic DietDocument3 pagesAllergies or Food Intolerances.: Therapeutic DietBryan Mae H. DegorioPas encore d'évaluation
- Intraoperative NursingDocument41 pagesIntraoperative NursingBryan Mae H. Degorio100% (11)
- Emergency Department Handbook PDFDocument461 pagesEmergency Department Handbook PDFdmallozziPas encore d'évaluation
- Worksheet in BloodDocument12 pagesWorksheet in BloodBryan Mae H. DegorioPas encore d'évaluation
- Medical Surgical Nursing OrthopedicDocument22 pagesMedical Surgical Nursing Orthopedicroger80% (5)
- Medical and Surgical NursingDocument4 pagesMedical and Surgical NursingCrystal Ann Monsale TadiamonPas encore d'évaluation
- Endocrine Disorders and DrugsDocument149 pagesEndocrine Disorders and DrugsJaypee Fabros Edra100% (1)
- JoyDocument5 pagesJoymichael100% (1)
- Ortho NCLEX Questions 1 PDFDocument39 pagesOrtho NCLEX Questions 1 PDFElizabella Henrietta TanaquilPas encore d'évaluation
- MS4 Midterm NCLEX BurnsDocument5 pagesMS4 Midterm NCLEX BurnsDebbie Dela Cruz100% (5)
- CA EndocrineDocument8 pagesCA EndocrineCharlie Cotoner FalgueraPas encore d'évaluation
- Final Compre Exam Key AnswersDocument14 pagesFinal Compre Exam Key Answersmj CanilangPas encore d'évaluation
- Fluid and ElectrolytesDocument21 pagesFluid and ElectrolytesMeryl RamosPas encore d'évaluation
- Neurologic Disorders - NCM 102 LecturesDocument12 pagesNeurologic Disorders - NCM 102 LecturesBernard100% (4)
- Multiple SclerosisDocument6 pagesMultiple SclerosisRonnel Alvin Antonio AdrianoPas encore d'évaluation
- Musculoskeletal DISORDERSDocument6 pagesMusculoskeletal DISORDERSJoe Stewart100% (1)
- EndoDocument8 pagesEndoAqcoh Ce Erica ParzueloPas encore d'évaluation
- Thyroid Carcinoma Case PreDocument22 pagesThyroid Carcinoma Case PreTabrrett Bethel100% (1)
- 4R's of RadiobiologyDocument32 pages4R's of Radiobiologyarif081190Pas encore d'évaluation
- Skeletal System ReviewerDocument4 pagesSkeletal System ReviewerMadelle Capending DebutonPas encore d'évaluation
- Systems of Measurement and Drug CalculationDocument13 pagesSystems of Measurement and Drug CalculationBryan Mae H. DegorioPas encore d'évaluation
- Fracture: Edfran Jed A. Serino MSN 303Document34 pagesFracture: Edfran Jed A. Serino MSN 303Edfran Jed SerinoPas encore d'évaluation
- Final NCM 116 PDFDocument20 pagesFinal NCM 116 PDFJoshua MendezPas encore d'évaluation
- Chapter 09 - Visual and Auditory ProblemsDocument7 pagesChapter 09 - Visual and Auditory ProblemscariPas encore d'évaluation
- Preceptor Handbook For Nursing EducationDocument41 pagesPreceptor Handbook For Nursing EducationBryan Mae H. Degorio0% (1)
- Addison's DiseaseDocument17 pagesAddison's DiseaseMah Jezthy100% (1)
- 04 Tissue, Glands and MembranesDocument52 pages04 Tissue, Glands and MembranesBryan Mae H. Degorio100% (1)
- Project Hospital Fin All Business SummaryDocument32 pagesProject Hospital Fin All Business Summarykanchoo100% (1)
- BurnsDocument3 pagesBurnsROBERT C. REÑA, BSN, RN, MAN (ue)67% (3)
- DISORDERS of The EYE and EARDocument8 pagesDISORDERS of The EYE and EARAnna Carmela P. MelendezPas encore d'évaluation
- The Adult LearningDocument15 pagesThe Adult LearningBryan Mae H. DegorioPas encore d'évaluation
- Medical Surgical Nursing ReviewerDocument8 pagesMedical Surgical Nursing ReviewerDavid Brillo0% (1)
- Case Studies in Nursing Fundamentals - Trueman, Margaret Sorrell - Page 170-178Document9 pagesCase Studies in Nursing Fundamentals - Trueman, Margaret Sorrell - Page 170-178Bryan Mae H. Degorio0% (3)
- Q&A FractureDocument13 pagesQ&A FractureRed JimenoPas encore d'évaluation
- Test Questions For Oncologic DisordersDocument6 pagesTest Questions For Oncologic Disorderspatzie100% (1)
- Urinary System Disorders Practice Quiz #1 (50 Questions)Document26 pagesUrinary System Disorders Practice Quiz #1 (50 Questions)Emy TandinganPas encore d'évaluation
- Eye DisordersDocument7 pagesEye DisordersClara De GuzmanPas encore d'évaluation
- Medical Surgical Nursing Test IXDocument4 pagesMedical Surgical Nursing Test IXclobregasPas encore d'évaluation
- Residual: No More Positive S/SX, Just WithdrawnDocument10 pagesResidual: No More Positive S/SX, Just WithdrawnRosie CuasitoPas encore d'évaluation
- Wound HealingDocument6 pagesWound HealingRheenz FornolesPas encore d'évaluation
- Rationale - Habon, CristineDocument21 pagesRationale - Habon, Cristinecha liPas encore d'évaluation
- Medical-Surgical Nursing Care: Caring For Clients With Diabetes MellitusDocument90 pagesMedical-Surgical Nursing Care: Caring For Clients With Diabetes MellitusJonalynCollodChewacheoPas encore d'évaluation
- Maternal and Child Health Nursing 1 Saundrs Pink EdDocument149 pagesMaternal and Child Health Nursing 1 Saundrs Pink EdVin SantosPas encore d'évaluation
- Gastrointestinal Quiz AnswersDocument3 pagesGastrointestinal Quiz AnswersLyniel Anne de AsisPas encore d'évaluation
- Cardiovascular 4416Document5 pagesCardiovascular 4416api-3703191Pas encore d'évaluation
- Renal and Urinary SystemDocument5 pagesRenal and Urinary SystemStaceyPas encore d'évaluation
- Ortho Sample QuestionsDocument4 pagesOrtho Sample QuestionsKalaMai Calalo AlvarPas encore d'évaluation
- Geron NclexDocument53 pagesGeron NclexGodfrey FrancoPas encore d'évaluation
- The Nclex-Rn Test Plan Adult Physiologal IntegrityDocument25 pagesThe Nclex-Rn Test Plan Adult Physiologal IntegrityalfreddahbiPas encore d'évaluation
- MedSurg CH 44 & 45 Study GuideDocument5 pagesMedSurg CH 44 & 45 Study GuideMichele ShepardPas encore d'évaluation
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideD'EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuidePas encore d'évaluation
- 5 Musculoskeletal TraumaDocument102 pages5 Musculoskeletal TraumaMaria Lynne Parambita100% (1)
- Principles of FractureDocument14 pagesPrinciples of Fracturezen.maree6Pas encore d'évaluation
- Ms. Elizabeth D. Cruz E.N., M.A.N.: 9.1 PathophysiologyDocument20 pagesMs. Elizabeth D. Cruz E.N., M.A.N.: 9.1 PathophysiologyAlfadz AsakilPas encore d'évaluation
- Orthopedic: Clinical Features of FracturesDocument6 pagesOrthopedic: Clinical Features of FracturesDrAyyoub AbboodPas encore d'évaluation
- Fracturesgoutosteosprain 2Document199 pagesFracturesgoutosteosprain 2Rose Cristille Yeso JocsonPas encore d'évaluation
- Effect of Injury and Immobilization On MuscleDocument19 pagesEffect of Injury and Immobilization On Musclesonali tushamerPas encore d'évaluation
- 1 Classifications of FracturesDocument33 pages1 Classifications of Fracturesرغد شاكر محمود أحمدPas encore d'évaluation
- In Practice 2012 Moores 22 6Document6 pagesIn Practice 2012 Moores 22 6ransinghPas encore d'évaluation
- MODULE 2 - THXDocument21 pagesMODULE 2 - THXZgama AbdulrahmanPas encore d'évaluation
- Musculoskeletal Disorders FRACTURESDocument10 pagesMusculoskeletal Disorders FRACTURESرافت العواضيPas encore d'évaluation
- Drug Cal - Practice TestDocument2 pagesDrug Cal - Practice TestBryan Mae H. DegorioPas encore d'évaluation
- Introduction To Change: Towards Excellence: "PHIC Accredited Health Care Provider"Document3 pagesIntroduction To Change: Towards Excellence: "PHIC Accredited Health Care Provider"Bryan Mae H. DegorioPas encore d'évaluation
- Drugs Affecting The Immune SystemDocument4 pagesDrugs Affecting The Immune SystemBryan Mae H. DegorioPas encore d'évaluation
- Sampling Process and Measurement ScaleDocument18 pagesSampling Process and Measurement ScaleBryan Mae H. DegorioPas encore d'évaluation
- Is Mentorship For YOUDocument17 pagesIs Mentorship For YOUBryan Mae H. DegorioPas encore d'évaluation
- Shock and SIRSDocument85 pagesShock and SIRSBryan Mae H. DegorioPas encore d'évaluation
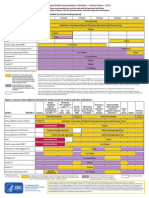
- Adult Immunization ScheduleDocument3 pagesAdult Immunization ScheduleBryan Mae H. DegorioPas encore d'évaluation
- Key (10) Principles of CST - 1 PagerDocument1 pageKey (10) Principles of CST - 1 PagerBryan Mae H. DegorioPas encore d'évaluation
- Care of Patient With Nutritional and Metabolic DisordersDocument10 pagesCare of Patient With Nutritional and Metabolic DisordersBryan Mae H. DegorioPas encore d'évaluation
- Substance AbuseDocument32 pagesSubstance AbuseBryan Mae H. Degorio100% (3)
- Slides For SeizureDocument15 pagesSlides For SeizureBryan Mae H. Degorio100% (3)
- Gestalt Sept2019 FINALDocument3 pagesGestalt Sept2019 FINALMolly ChristensenPas encore d'évaluation
- Companies Dont Test in AnimalsDocument26 pagesCompanies Dont Test in AnimalsJoao BernardoPas encore d'évaluation
- TLEDocument13 pagesTLEAnonymous lim7qKW1Pas encore d'évaluation
- West Bengal's Leather Industry OpportunitiesDocument5 pagesWest Bengal's Leather Industry OpportunitiesDeepak AgarwalPas encore d'évaluation
- Scaling Teeth TechniquesDocument12 pagesScaling Teeth TechniqueshanyPas encore d'évaluation
- Vitamin EDocument11 pagesVitamin EErvan Apsara BismakaPas encore d'évaluation
- College of Physicians and Surgeons of Ontario's Affidavit Re: Eve's Laser ClinicDocument27 pagesCollege of Physicians and Surgeons of Ontario's Affidavit Re: Eve's Laser CliniccbcottawaPas encore d'évaluation
- A Systematic Review: Optimal Management of Fatigue in Patients With Systemic Lupus ErythematosusDocument14 pagesA Systematic Review: Optimal Management of Fatigue in Patients With Systemic Lupus ErythematosusMelz Melz MutzPas encore d'évaluation
- HNS 107Document95 pagesHNS 107claudette1882Pas encore d'évaluation
- Health Benefits of HoneyDocument10 pagesHealth Benefits of HoneyMohd Idris MohiuddinPas encore d'évaluation
- Designer Babies For Reading Packet 1Document4 pagesDesigner Babies For Reading Packet 1Amirah Hadi AqilahPas encore d'évaluation
- Contribuciones de Shneidman Al Pensamiento SuicidaDocument21 pagesContribuciones de Shneidman Al Pensamiento SuicidaJuan Carlos Jaramillo100% (1)
- Gut and Psychology Syndrome - Natural Treatment For Autism, Dyspraxia, A.D.130015Document5 pagesGut and Psychology Syndrome - Natural Treatment For Autism, Dyspraxia, A.D.130015liza lizaPas encore d'évaluation
- Effective Home Remedy For AlmoranasDocument3 pagesEffective Home Remedy For AlmoranasMyk Twentytwenty NBeyondPas encore d'évaluation
- Patient Blood Management Equals Patient SafetyDocument19 pagesPatient Blood Management Equals Patient SafetyMuhammadBudiman RbcPas encore d'évaluation
- Antigens Antibodies and VaccinesDocument4 pagesAntigens Antibodies and Vaccinesapi-299996815Pas encore d'évaluation
- Case Report FinalDocument21 pagesCase Report FinalAyen FornollesPas encore d'évaluation
- 1955 Ball LauraDocument55 pages1955 Ball LauraBene BeanPas encore d'évaluation
- Wart Removal and TreatmentDocument6 pagesWart Removal and TreatmentwandaPas encore d'évaluation
- EJNSO Volume 9 Issue 1 Pages 1-10Document10 pagesEJNSO Volume 9 Issue 1 Pages 1-10doctora ranaPas encore d'évaluation
- Therapeutic CommunicationDocument7 pagesTherapeutic CommunicationJoseph Rommel Castro CortezPas encore d'évaluation