Académique Documents
Professionnel Documents
Culture Documents
Eye Disorder
Transféré par
Minlik-alew DejenieDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Eye Disorder
Transféré par
Minlik-alew DejenieDroits d'auteur :
Formats disponibles
Debre Brehan University, School of Health
Science, Program of Nursing
Review of Anatomy &
Physiology of the eye
The eye is the organ of vision which is located in a cone shaped cavity known as the
orbit.
It is highly specialized & complex structure.
It receives & sends visual data to the cerebral cortex for interpreting visual images.
Seven cranial nerves have connections to the eyes. These are;
For vision CN II.
Eye movement CN III, IV & VI.
Papillary reaction CN III.
Eyelid elevation CN III.
Eyelid closure CN VII.
Brain stem connections permit coordinated eye movement.
The eye ball is situated in the bony socket or orbit.
The eye ball is protected by: Orbit.
Eyelids (Upper & lower).
Nerves & blood vessels that supply nutrients & transmit impulses to the brain are also
present with in the orbit.
Organized bands of muscles are attached to the external eye ball.
External Structures of the eye
Grey line;
Where the skin joins palpebral conjunctivas.
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 1
Debre Brehan University, School of Health
Science, Program of Nursing
Glands: Meibomian gland;
It is found with in the tarsal plate, their ducts opening through the
palpebral conjunctiva just behind the lashes.
Produce sebaceous substance which creates the oily layer of the tear film.
Glands of moll These are sweat glands producing sebum.
Muscles:-There are three muscles supplying the eyelid.
a. Orbicularis: Oculi
Origin: Lacrimal bone.
Insertion:- Deep in the facia around the lacrimal.
Function:- to close the eye lid & to screw up the eyes & facilitate tear
drainage.
Nerve supply:- Facial nerve (CN-VII).
Its paralysis cause lag-ophthalmas (Failure to close eye).
b. Levator palpebral superioris
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 2
Debre Brehan University, School of Health
Science, Program of Nursing
Origin: around apex of orbit.
Insertion: skin of upper lid & tarsal plate.
Function: to lift the upper lid.
Nerve supply: Oculomotor (CN-III).
Its paralysis cause ptosis (dropping of eye lid).
c. Mullers muscle
This is smooth muscle.
Origin: Levator palpebral superiors.
Insertion: Tarsal plate.
Function: provide extra elevation to the upper lid.
Nerve supply: Sympathetic nervous system.
The junction of the upper & lower eyelid is called canthus/commisure.
The outer, Lateral Canthus is on the lateral temporal aspect of the eye.
The inner, Medial Canthus contains the Puncta, openings that allow tears to drain
into the upper portion of the lacrimal system.
The elliptical space between open eye lid is called palpebral fissure.
Vertical palpebral fissure = 8-11mm (More wide in female).
Horizontal palpebral fissure = 27 30 mm.
Upper eye lid is more mobile than lower eyelid.
Skin
It is the thinnest of the body.
It is freely movable.
Meibomian gland orifice in a single row.
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 3
Debre Brehan University, School of Health
Science, Program of Nursing
The anterior border of lid margin gives rise to the eye lashes.
Eye lashes:-hairs-like filament (cilia)
2 to 3 irregular row.
With 100 lashes on upper lid.
With 50 lashes on lower lid (thin & short).
It is important to trap dust particles.
Subcutaneous connective tissue
Loose & doesnt contain fat.
This cause rapid accumulation of fluid (Oedema)
Tarsus
It is called skeleton of the eyelid.
Conjunctiva
It is a mucous membrane.
Its zones are: Palpebral conjunctiva: forms inner layer of eyelid & reflects over eye
ball.
Bulbar conjunctiva;
It is extremely thin & transparent so that vessels are easily seen.
It is freely movable.
Covers the eye ball except the cornea.
Fornices: formed where bulbar & palpebral conjunctiva fold back over
each other.
Eyelids;
It is skin without subcutaneous fat.
It has 4 basic layers.
From anterior to posterior the layers are;
Skin & subcutaneous connective tissue.
Muscle.
Tarsus .
Conjunctiva.
Functions of eye lids;
Protect eye ball (globe).
Lubricate anterior surface of globe (By blinking the tear film spread over anterior
surface).
Blood supply to the lid;
Lacrimal artery & vein.
Supra orbital artery & vein (upper lid).
Superior & inferior medial palpebral artery & vein.
Lacrimal glands & Excretory System
Lacrimal glands
Location Superiorly in a shallow depression of frontal bone.
It has 2 parts:
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 4
Debre Brehan University, School of Health
Science, Program of Nursing
Orbital (lacrimal gland proper).
Numerous Excretory ducts emptying secretion to conjunctiva.
Mechanism of tear secretion is by: Reflex due to stimulation of trigeminal nerve.
Psychogenic central mechanism.
Accessory glands
Krauses gland located in the eye lid.
Meibomian gland
Basal tear secretion is constant & under sympathetic nervous system control.
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 5
Debre Brehan University, School of Health
Science, Program of Nursing
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 6
Debre Brehan University, School of Health
Science, Program of Nursing
Function of tear
Refraction: to provide an optically smooth surface to the cornea.
Lubrication of the front of eye ball.
Cleansing action by washing away dust particles from the eye.
Protection from infection by secreting the enzyme lysozyme, immuno-proteins &
antimicrobial agents.
Flow of tear is affected by;
Blinking.
Capillary attraction into the puncta.
Lacrimal pump by contraction of muscle.
Gravity.
Internal Structure of eye
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 7
Debre Brehan University, School of Health
Science, Program of Nursing
Eye Ball;
It is lined by 3 layers,
1. Outer protective layer
It is fibrous layer.
It consists;
A. Sclera
It is the white part of the eye.
Form outermost tissue of posterior & lateral (4/5)th aspects of eye ball.
It is continuous anteriorly with cornea.
Maintains the shape of the eye & gives attachment to extra ocular muscle of eye.
B. Cornea
It is the anterior continuation of sclera.
It is clear transparent & allow passage of light rays.
It is convex anteriorly & is involved in refraction or bending light rays to focus
them on retina.
It is highly sensitive.
2. Middle layer
It is Vascular organ.
It Consists;
A. Choroid
Lines the posterior (5/6)th of inner surface of sclera.
Highly vascularized.
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 8
Debre Brehan University, School of Health
Science, Program of Nursing
Light enters the eye through the pupil, stimulate the nerve endings in the retina
then is absorbed by the choroid.
Deep chocolate brown in colour.
B. Ciliary body
It is anterior continuation of the choroid & consists ciliary muscle & secretary
cells (producing aqueous humor).
It gives attachment to suspensary ligament which, at its other end, is attached to
the lens.
The ciliary muscle controls the shape of lens for focusing.
C. Iris
It is the visible coloured part of the eye & extends anteriorly from the ciliary
body, lying behind the cornea in front of the lens.
It divides the anterior segment of the eye into anterior & posterior chambers
which contain aqueous fluid secreted by ciliary body.
In the center is an aperture, the pupil.
The pupil varies in size depending upon the intensity of light.
During bright light the pupil constrict, whereas dilate during dim light .
D. Lens
It is a highly elastic circular biconvex transparent body, lying immediately behind
the pupil.
It is suspended from the ciliary body by the suspensory ligament & enclosed with
in a transparent capsule.
Its thickness is controlled by the ciliary muscle through suspensary ligament.
It bends light rays reflected by an object in front of eye.
3. Inner layer
A. Retina
It is nervous tissue layer.
Retina is especially adapted to be stimulated by light rays.
Composed of several layers of nerve cell bodies.
Rods & cones are layer highly sensitive to light.
Macula
It is an area of the retina situated to the temporal side of the optic disc.
It contains a high concentration of cones.
In its centre is the fovea centralis, a slight depression where only cones are
present.
B. Optic disc
Contains no nerve cells, so the vision cannot take place here.
This is known as the blind spot.
Structures inside the eye ball are
Aqueous humour (fluid).
Vitreous body.
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 9
Debre Brehan University, School of Health
Science, Program of Nursing
The anterior segment of the eye, i.e. the space between the cornea & the Lens, is
incompletely divided into anterior & posterior chambers by iris. Both chambers contain a
clear aqueous fluid.
Aqueous fluid
It is secreted by ciliary gland.
It passes in front of the lens, through the pupil into anterior chamber & returns to
the venous circulation in the angle between iris & cornea.
Produced continuously & drained but the IOP remains fairly constant b/n 10 to 20
mm hg.
An increase in pressure cause glaucoma.
Vitreous body
It is found behind the lens & filling the cavity of the eye ball.
Soft, colourless, transparent, jelly like substance composed of 99% water.
It maintains sufficient IOP to support the retina against the choroids & prevent the
wall of eye ball from collapsing.
The eye keeps its shape because of IOP exerted by vitreous & aqueous fluid.
Optic nerves
The fibers of optic nerve originate in the retina of the eye.
All the fibers converge to form the optic nerve about 0.5cm to the nasal side.
It pierces the choroid & sclera to pass backwards & medially through the orbital
cavity.
Passes through optic foramen of sphenoid bone, backwards & medially to meet
the nerve from the other eye at the optic chiasma.
Optic chiasma
It is situated immediately in front of & above the pituitary gland in the sphenoid
bone.
In the optic chiasma the nerve fibers of the optic nerve from the nasal side of each
retina cross over to the opposite side.
The fibers from temporal side do not cross.
Physiology of Sight
Light reflects into the eyes by objects within the field of vision.
A specific colour is perceived when only one wave length is reflected by the
object & all the others are absorbed.
E.g. an object appears red when only the red wave length is reflected.
Objects appear white when all wavelengths are reflected & black when they are
all absorbed.
In order to achieve clear vision light reflected from objects with in the visual field
is focused on the retina of both eyes.
The processes involved in producing a clear image are refraction of the light rays,
changing the size of pupils & accommodation of the eyes.
Refraction of the light rays
When light rays pass from a medium of one density to a medium of a different
density they are refracted or bent.
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 10
Debre Brehan University, School of Health
Science, Program of Nursing
Helps to focus light on retina.
Lens: - is the only structure in the eye that changes its refractive power.
Light from distant objects needs least refraction & as the objects come closer, the amount
needed is increased (i.e. ciliary muscle contract).
Size of the pupils: - control the amount of light entering to the eye.
If the pupils were dilated in a bright right, too much light would enter eye & damage
retina.
The two muscles of iris, circular muscle fiber constriction causes pupil to constrict but
constriction of radiating muscle fiber dilate pupil.
Accommodation of the eyes to light
Close Vision
In order to focus on near object i.e. with in 6 meters, the eye must make the
following adjustments.
Constriction of the pupils.
Convergence of the eye balls (Movement).
If convergence is not complete there is double vision
(diplopia).
Changing the power of lens the lens is thicker.
Distant Vision
Objects more than 6 meters away from the eyes are focused on the retina without
adjustment of the lens or convergence of the eyes.
With aging, the ability of the eye to accommodate gradually decreases because of
increased rigidity of the lens (Presbyopia).
The lens is tense able to change shape in response to visual challenge of focusing on near
objects.
Summary of eye structure
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 11
Debre Brehan University, School of Health
Science, Program of Nursing
Passage way of light rays
Light
Cornea
Pupil
Iris
Lense
AH
VH
Retina
Optic Nerve
Cerebral Cortex.
1. Assisting the patient in measurement of visual acuity
The measurement of visual acuity records the acuteness of central vision for distance, and
near or reading vision.
Visual acuity: - is the most important function of eye and it should be performed first, so
that vision is assessed before actually touching the eye.
Distance Vision
It is tested at 6m as rays of light from this distance are nearly parallel.
If the patient wears glasses constantly, vision may be recorded with & without glasses,
but this must be noted on the record.
Each eye is tested and recorded separately, the other being covered with a card held by
the examiner.
Visual acuity is tested with an eye chart called snellens chart.
Snellens Chart test type
Heavy black letters, numbers or symbols printed in black on a white background, are
arranged on a chart in grows of graded size, diminishing from above downwards. The top
letter can be read by the normal eye at a distance of 60m, and the following rows should
be read at 36, 24, 18, 12, 9, 6, 5, 4m respectively.
The patient is seated 6m from the chart, which must be adequately lit, & asked to read
down to the smallest letter he can distinguish, using one eye at a time.
Visual acuity is expressed as a fraction & abbreviated as VA.
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 12
Debre Brehan University, School of Health
Science, Program of Nursing
The numerator is the distance in meters at which a person (pt)can read a given line of
letters.
The denominator is the distance at which a person with a normal average vision can read
the same line.
Example: - If the 7th line is read at a distance of 6m this is VA 6/6. If same letters in the line are
read but not all, it is expressed as, for example, VA 6/6 -2, or VA 6/9+2.
For vision less than 6/60 the distance between the patient & the chart is reduced a meter
at a time & the vision is recorded accordingly as, for example, 5/60, 4/60, 2/60, 1/60.
If the patient cannot read the top letter at a distance of 1 meter, the examiners hand is
held at 0.9m, 0.6m or 0.3m a way against a dark background & the patient is asked to
count the number of fingers held up.
If he answers correctly, record VA= CF (Count Fingers). For less visions the hand is
moved in front of the eye at 0.3m, record VA = HM (Hand movement).
In the case of less vision, test for projection of light by shining a torch into the eye from
different directions to see if the patient can tell from which direction it comes if he sees
the light from which direction, it is noted as VA = PL(Perception of light). This test is
performed in the dark room. If no light is seen, record NO PL, which is total blindness.
A pinhole disk is used if the VA is less than 6/6, which may improve VA. If considerable
increase in vision is obtained, it may usually be assumed that there is no gross
abnormality, but a refractive error.
2. Assisting on ophthalmoscope Examination
The internal eye is called the fundus & comprises the retina, optic disc, macula, & retinal
vessels.
It can be visualized through an ophthalmoscope.
Def: - Ophthalmoscope is a hand-held instrument that projects light through a prism & bends the
light at 90 degrees, allowing the observer to view the retina.
The direct ophthalmoscope has several lenses arranged on a wheel. A lens may be chosen
by rotating the wheel with the index finger with out interrupting the inspection.
To a void a confrontation of noses, the right eye of the patient is examined with the right
eye of examiner
The room is darkened to enhance papillary dilation.
Instruct the patient to hold the eyes still & focus on a real or imagined distant object.
Grip the ophthalmoscope firmly in the hand, with the index finger resting on the lens
wheel.
The head of the ophthalmoscope is braced with in the angle made by the eye brow & the
nose.
The lens chosen for initial inspection should be the one labelled zero unless the examiner
is knowingly correcting his own defect in visual a acuity.
An examiner who wears corrective lenses should become proficient in ophthalmoscopy
while wearing the lens.
Lenses lobe led with a red numerals are for hyperopic (far sighted) patients & those with
a black numerals are for myopic (nearsighted) patients.
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 13
Debre Brehan University, School of Health
Science, Program of Nursing
The examiner stands approximately 37.5cm away & about 15 degrees to the side of the
patients gaze.
When the light is focused on the pupil, the retina glows red (or orange) through dilated
pupil opening. This is called the red reflex.
The examiner then moves closer to the patient. Placing a hand on the patients forehead,
the examiner rests his or her forehead on the hand & focuses through the
ophthalmoscope.
Examining the fundus includes evaluating: The optic disc
Retinal blood vessels
Retinal characteristics
Macular area
Vitreous hum
The disc for: Its physiologic cup & Proportional size
The blood vessels for: Size
Distribution
Crossings & colour reflection
Retinal fundus for: General Colour
Hemorrhagic
Fluid
Attachment
Macula & fovea centralis for: Colour (darker red)
Central reflection
The vitreous humor for: Colour
Foreign bodies
3. Assisting in measurements of intraocular pressure
Tonometry is a technique for measuring intra-ocular pressure (IOP) indirectly by
measuring the force necessary to flatten a 3.06mm diameter portion of the corneal
surface. The higher the IOP, the greater the force required.
Methods of measuring IOP: Digital.
Golmann applanation tonometer.
Schiotz (perkins applanation) tonometer.
Pneumotonometer.
Tonopen.
Schiotz tonometry
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 14
Debre Brehan University, School of Health
Science, Program of Nursing
Requires using a metal, hand held instrument (the tormenter) that rest on the
anesthetized cornea. The result can be variable but are a good estimate of IOP.
Goldmann applanation tonometry
it is attached to a slit lamp to measure IOP.
It is the most accurate form of measuring IOP.
Procedure
Identity the patient.
Check if the patient is wearing contact lenses, if so then remove them before
commencing the procedure.
Administer topical anaesthesia into both eyes.
Instil fluorescein stain for accurate reading.
Instruct the patient to look straight a head with both eyes wide open- if necessary, the
patients eyelids should be held apart by the examiner with out pressure being applied to
the eyeball.
The ton meter is brought into contact with the center of the cornea .
The IOP (in mm Hg) is found by multiplying the drum reading by ten.
Non contact tonometer (pneumotonometer)
It is employed by optometrists, use a puff of air blown against the eye.
It is useful when contact with the cornea is not desired.
Digital
A general determination of IOP can be made by applying gentle finger pressure
over the sclera of the closed eye.
The tips of both fore fingers are placed on the closed upper lid. One finger gently
presses inward while the adjacent finger senses the amount of pressure exerted
against it.
The examiners then compare the tension felt or perceived in the patients eye with the
pressure in their own. This requires practice.
The patient looks down wards, closing the eye.
palpate the eye ball to assess the degree of hardness.
No accurate measurement can be taken but on eye with raised pressure will feel
harder than one with normal pressure.
It is a useful initial method of assessment, especially if none of the specialized
equipment needed for measuring IOP is available.
Tonopen
Are small pen like instruments that measure pressure in a similar fashion to the
applanation method.
NB: - IOP = normal value is 10-20mmHg. Increased IOP is the cardinal sign of glaucoma
4. Assisting the patient in measurement of refractive errors
Refraction
Determination of refractive errors.
Corneal Reflections
Method: - A pen torch is held at 1/3m directly in front of both eyes. The position
of the reflection on each eye is then compared.
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 15
Debre Brehan University, School of Health
Science, Program of Nursing
Results: - The results may be: Normal Corneal reflections symmetrical.
Asymmetrical Corneal reflections.
Cover Test:-It is carried out to detect the presence of a squint, & should be used in
conjunction with observation of the corneal reflections.
Method: - A penlight is held at ~ 1/3m from the child. The child must be looking
at the height whilst the cover test is carried out.
It is important to repeat the cover test using a detailed target, e.g. a small picture
on a tongue depressor, because same squints are only present when looking at
detailed objects. The caver test should also be carried out at 6m where possible
because other squints are only present when looking into the distance, i.e.
intermittent squints.
Cover one eye, watch for any movement of the uncovered eye, remove the cover &
repeat covering the other eye & watching for any movement of uncovered eye.
The results may be: No manifest squint.
Manifest squint right convergent squint (Fig 13.6)
Manifest squint right divergent squint (Fig 13.7)
Ocular Movements
The examiner sits in front of the patient & using a pen torch, observes both eyes
moving in all eight positions of gaze.
This will include up, down, both sides & in all four corners, always returning to
the straight a head or primary position. The patients head must be held still. Any
muscle imbalance, over action & under actions are then noted.
Refractive errors
RE is a pathological condition where parallel rays of light are not brought to focus on
retina, b/c of defect in the refractive media that is cornea and lens.
Refraction is the ability of the eye to bend light rays, so that they fall on the retina.
In normal eye, parallel light rays are focused through the lens in to a sharp image on
retina, this condition termed as Emmetropia.
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 16
Debre Brehan University, School of Health
Science, Program of Nursing
Emmetropia means the light is exactly focused on the retina, not infront of it or behind it.
When the light is does not focus properly, it is called a refractive error.
Refractive errors include;
1. Myopia (Short sightedness).
2. Hyperopia or hypermetropia (Long sightedness).
3. Astigmatism (asymmetric focus).
4. Presbyopia.
5. Aphakia.
1. Myopia or short sightedness
A short sighted person has a long eyeball and the eye have excessive refracting power
(cornea and lens).
The light rays therefore come to a focus in front of the retina.
Can see near objects clearly.
Objects at a distance are blurred.
C/F = decreased distant vision.
Can be corrected by concave lens (minus), so that objects seen in the distance are focused
clearly on the retina. It bends light ray out ward.
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 17
Debre Brehan University, School of Health
Science, Program of Nursing
2. Hyperopia or long sightedness
The eye has insufficient refractive power to focus light on the retina.
The rays of light entering the eye are focused behind the retina.
The individual can see distant object clearly, but close objects are blurred (C/MImpairment of near vision).
Can be corrected by convex lens (plus) which bends light ray inward.
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 18
Debre Brehan University, School of Health
Science, Program of Nursing
3. Astigmatism
It is a refractive error in which the light rays are spread over a diffuse area rather than
sharply focused on the retina.
It results from unequal curvature of the cornea, causing horizontal and vertical rays to be
focused at two d/t pts on the retina, so that there is no point of focus of the light rays on
the retina.
C/F: - blurred vision, eye discomfort.
It can be hyperopic or myopic in relation to where the image falls.
4. Presbyopia
It is a form of hyperopia that occurs as a normal process of aging usually around the age
of about 45 years.
As the lens ages and becomes less elastic , it loses its refractive power and the eye no
longer has the ability to accommodate for near vision.
The light rays therefore fall behind the retina before coming to a focus.
Can be corrected by convex lens.
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 19
Debre Brehan University, School of Health
Science, Program of Nursing
5. Aphakia
It is the absence of crystalline lens.
The lens may be absent congenitally, cataract surgery, trauma.
Eye loses about 30% of its refractive power and no near vision.
Can be corrected by implanting intraocular lens.
External Ocular diseases
1. Hordeolum (Sty)
A Sty is an acute suppurative infection of superficial eye lid sebaceous glands.
Cause: - Staphylococcus aureus.
C/F: - Sub acute pain, redness, & swelling (edematous) of a localized area of the lid that may
rapture.
- Stys are localized to the lid margins.
- small collection of pus in the form of an abscess.
Mx
Worm, moist compresses for 10 to 15 minutes, three to four times a day, hastens the
healing process.
If the condition doesn't begin to resolve with in 48 hours, incision & drainage may be
indicated.
Application of topical antibiotics.
Analgesics.
2. Chalazion
Defn: - Chalazion is a swelling of one of the meibomian/tarsal glands due to blockage of
its duct.
It is chronic condition.
It is some times called internal hordeolum.
Cause: - Staphylococci are common causes if infected.
C/F: -Localized, firm, painless swelling that develops over period of weeks.
-Palpation usually indicates small, painless nodule in the eye lid some distance from the lid
margin.
Mx
Worm, moist compresses for 10 to 15 minutes, three to four times a day especially in the
early stage.
Massage & expression of the glandular secretions.
Antibiotic therapy (Chloramphenicol;- apply 3-4 x/d for 7-10 day, after the eye has been
steamed).
Corticosteroid drops/injection in to the chalazion lesion.
Incision is indicated if the chalazion grows larger enough to distort vision.
Nursing Care:
- Instruct the patient to apply steam to the eye.
- Instruct how to use drugs.
- Instruct the pt. to clean eye lids by using worm water.
3. Blepharitis
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 20
Debre Brehan University, School of Health
Science, Program of Nursing
C/M
It can be a cute or chronic inflammation of both eyelid margins.
It is usually bilateral.
It can take the form of;
1. Staphylococcal blepharitis:- It is usually ulcerative and more serous due to
involvement of the base of hair follicle. Permanent scaring can result. Caused by
staphylococcal chronic infection.
2. Seborrehic blepharitis:- It is chronic and usually resistant to Rx, but the milder
case can respond to lid hygiene. Caused by Seborrhoea (excessive secretion of
lipid from meibomian glands).
It may be associated with dandruff, poor hygiene, eczema.
Irritation of eye lids margins and red rimmed eyes with many scales or crusts on the lid
margin and eye lashes.
Burning.
Itching.
Photophobia.
Conjunctivitis may occur simultaneously.
Mx
o Daily meticulous cleaning of the lid margins using cotton tipped applicator, with dilute
baby shampoo: 2x/day.
o Worm Compresses.
o Application of antibiotic ointment 2-3x/d.
o Dandruff RX.
o Stop using make up or change the brand used.
o Improve hygiene.
Complication
Conjunctivitis.
Trichiasis.
Entropion or ectropion of lower lid.
Corneal Ulcer.
4. Trichiasis
It is a condition in which the eye lashes grow in words & rub on the cornea.
Cause: - blepheritis
- Trauma or surgery to the lids.
Rx: - Epilation
Complication: - Corneal abrasions
- Corneal ulceration
- Corneal Opacity
- Vascularisation of cornea
5. Entropion
Turing inward of eyelids, usually lower eye lids.
Cause: - Contraction of the palpebral conjunctiva following trauma or disease to the eye lid or
conjunctiva.
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 21
Debre Brehan University, School of Health
Science, Program of Nursing
Rx: - Transverse lid surgery and suture.
6. Ectropion
It is turning outwards of the eye lids, usually the lower lids.
Cause: - Scaring of the lid or conjunctiva
- Paralysis of facial nerve.
Rx:- Surgery
7. Ptosis
It is dropping of the upper eyelid.
Cause: - congenital.
- Oedema, tumor & scarring of eye lid
- Myasthenia gravis (Levator palpebral superioris).
- Paralysis of nerves supplying the upper lid.
Rx: - Treat underlying cause.
Disease of conjunctiva
1. Conjunctivitis
Conjunctivitis an inflammation of the conjunctiva.
It is the most common ocular disease world wide.
It is characterized by a pink appearance (hence the common term pink eye) b/c of
subcutaneous blood vessel haemorrhages.
Cause
1. Infections;
1. Bacteria (Haemophilus influenza, staph aureus).
2. Virus (Adeno virus, HSV).
3. Chlamydial.
4. Fungal.
5. Parasitic.
2. Immunologic (allergy); environmental allergens (e.g. pollens).
3. Irritant/toxic (Chemical, thermal, electrical).
4. Associated with systemic disorder.
Most conjunctivitis is bilateral; unilateral involvement suggests a toxic or chemical
origin.
1.1. Bacterial Conjunctivitis
It can be acute or chronic
Causative agents: - Streptococcus
- Staph. auerus
- Pneumococcus
C/M
Conjunctival injection, especially in the fornices where the blood supply is rich.
Hyperemia/redness.
Purulent discharge.
Pain.
Rx & Nursing Care
Take swab from affected eye for culture & sensitivity if severe.
Clean the eye using cooled, boiled water.
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 22
Debre Brehan University, School of Health
Science, Program of Nursing
Chloramphenicol or tetracycline eye drop or paint 3x/d for 3-5days.
1.2. Neonatal Conjunctivitis
Severe conjunctivitis occurring in a baby less than 28 days old is notifiable disease.
Cause: - Gonococcus
- Streptococcus
- Chlamydia
C/M: - Severe discharge
- Red, swollen eye lids
- Chemosis (edema of the conjunctiva)
- Unilateral or bilateral infection.
Rx: - Clean the eye.
- Gentamycin eye drop TID.
- Oral antibiotics.
Complication: - Conjunctival Scarring.
- Chronic blepheritis.
- Conjunctival ulceration & perforation.
- Marginal corneal ulcer.
1.3. Viral Conjunctivitis
Cause: - Measles
- Herpes Simplex
- Varicella
C/M
Red eye.
Chemosis, if severe.
Follicle may be present on the palpebral conjunctiva.
Keratitis .
Watery discharge & photophobia.
Rx: - Self limiting (with in 7-10days).
- Steroid Rx.
Mx summary for bacterial and viral conjunctivitis (highly contagious)
Hand washing.
Avoid sharing hand towels, face clothes, eye, drops.
Tissue paper should be directly discarded in to a trash can after use.
Using new tissue paper every time you wipe the discharge.
All forms of tonometry must be avoided unless medically indicated.
1.3. Allergic Conjunctivitis
Causes: - Hay fever, Eczema
C/F: - Severe chemosis
- Red eye
- Watery eye
- Sinusitis may present
- Burning sensation & severe itching
- Photophobia
Rx: - Betamethasone or hydrocortisone drop.
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 23
Debre Brehan University, School of Health
Science, Program of Nursing
-Wearing dark glass.
2. Trachoma
Trachoma is a highly contagious infectious eye disease (Chlamydia Conjunctivitis) that
affects more than 500 million people world wide and which may result in blindness.
It is the world's leading cause of preventable blindness & primarily affects people in
Africa.
Pathophysiology
Scaring of the inside of the eye lid.
The eye lid turned inward and the lash rubs the eye ball.
Scaring of the cornea.
Irreversible corneal opacities and blindness.
Cause: - Chlamydia trachomatis
Mode of transmission: Direct Contact (with eye, nose, throat secretion from the affected individual.
Fomites (towel, hand kerchiefs, fingers, wash clothes).
Insect Vector (flies).
C/M
Mild itching & irritation is principal symptom.
Red eye.
Discharge (slightly purulent).
Follicles & papillae an upper palpebral connective.
Keratitis.
Entropion and trichiasis of the upper eyelid.
Chemosis of bulbar conjunctiva.
Blurring of vision.
Photophobia.
Pannus blood vessels on the upper part of cornea.
Corneal scaring.
Complications
Scarring of eye lids.
Entropion.
Trichiasis.
Corneal trauma & ulceration.
Mx: - Good personal hygiene
- Tetracycline eye
Management
SAFE strategy;
Surgery:- trichiasis and entropion.
Antibiotic:- TTC (ointment apply TID for 3-4weeks.), sulphonamides, erythromycin.
Facial cleanness:- good hand and face washing practice.
Environmental changes:-address water shortage, eradicate flies, avoid crowded, e.t.c.
Disease of cornea
1. Keratitis
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 24
Debre Brehan University, School of Health
Science, Program of Nursing
Keratitis is an inflammation of the cornea.
Cornea is susceptible to infection and injury because of its anterior location and degree of
exposure.
Cause
Exposure (exophtalmos, lagophtalmos) keratitis as a result of drying of the cornea
because of eye lids can not protect it adequately.
Infections;
Bacteria (staph.. aureus, strep.. pneumonia, pseudomonas aergunosa).
Virus (herpes simplex, varicella zoster virus).
Fungus (Candidia, aspergillus, cephalosporium).
Parasitic organism.
Most of infections of cornea occur as a result of trauma or compromised systemic or local
defense mechanism.
C/M
Sensation of foreign baby in the eye.
Marked inflammation of glade (open space).
Muco-purulent discharge with the eyelids stuck together on awakening.
Ulceration.
Hypoyon (Pus in the anterior chamber).
Photophobia.
Blurred vision.
In advanced disease;
Perforation of cornea.
Extrusion of the iris.
End-ophthalmitis.
Dx
Identifying the ulcer by slit - lamp examination after instilling fluorescein drops to
demonstrate the shape & size of the ulcer under special light.
Mgx
Patients with severe corneal infections are usually hospitalized to allow frequent
administration (every 30 minutes) of antimicrobial drops & regular examination.
Keep the lid clean.
Cool compresses.
Monitor for sign of increased IOP.
Acetaminophen 500mg 2tabs PRN.
Cycloplegic & mydriatics to relieve pain & inflammation.
Complication
Corneal Scar.
Revascularization (new blood vessels formation) in the cornea.
2. Pterygium
Pterygium is a triangular fibro-vascular connective tissue over the growth of the intrapalpebral conjunctiva with extension to the cornea.
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 25
Debre Brehan University, School of Health
Science, Program of Nursing
Usually occurring on the nasal side, but it can be temporal.
It is thought to be an irritative and degenerative phenomenon caused by ultraviolet light.
Cause unknown.
Predisposing factors: - people who live in hot, dry climates or who work in the open air.
Rx
Surgical removal if pterygium encroaches on the visual axis or causes significant
discomfort.
In 30-50% of cases it reoccurs after surgery.
3. Corneal ulcer
It is ulceration of cornea.
Etiology
Bacteria;
Staph.. aureus, strep.. pneumonia, pseudomonas aergunosa.
Fungus
Candidia, aspergillus.
C/M
Pain.
Blurred vision.
Photophobia.
The ciliary vessel around the cornea will be dilated.
Dx
Hx.
P/E.
Culture and sensitivity.
Microscopic exam.
Mgx
Treat urgently.
Antibacterial;
Gentamycin and ciprofloxacilin eye drops.
Antifungal;
Natamycin and econazole eye drops.
Intraocular disease /disorder of the Lens/
1. Cataract
It is clouding or opacity of crystalline lens the impairs vision.
The lens is a delicate structure & any insult on it causes absorption of water, resulting in
the lens becoming opaque.
According to WHO, cataract is the leading cause of blindness in the world (2002).
Cause
From birth (congenital).
Age (senile).
Eye injury (traumatic).
Secondary to existing eye disease (e.g. uveitis).
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 26
Debre Brehan University, School of Health
Science, Program of Nursing
Drug like corticosteroids.
Cataract associated with systemic disease (DM, Hyperparathyroidism).
UV light exposure.
High dose of radiation therapy.
Degree of Cataract
Immature cataract part of the lens is opaque.
Mature cataract the whole lens is opaque & may be swollen.
Congenital Cataract
Cause
Abnormal development of the eye.
Metabolic disturbance.
Rubella or malnutrition in first trimester of pregnancy.
C/M
Unable to see.
white pupil (Unilateral or bilateral).
Rx: - Removing the cataract
Senile Cataract
Occur in patients over the age of 60 years.
They result from sclerosis of the lens due to a degenerative process.
Usually bilateral.
It is either;
Nuclear: affects the central lens & takes on a brown color.
The patient sees better in dim light when pupil is dilated.
Cortical: Affects the periphery of the lens & looks white.
Vision is usually better in bright light when the pupil is constricts.
General C/M
Gradual, progressive, and painless loss of vision.
Double vision/blurred vision/
Reduced light transmission.
Rainbow/haloes/
Previous dark pupil appear milky or white.
Dx
Hx.
P/E.
Ophtalmoscopic exam.
Slit lamp examination.
Mgx
Surgery;
surgical removal of the lens usually done under local anesthesia.
IOL (intraocular lens) are usually implanted at the time of cataract extraction.
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 27
Debre Brehan University, School of Health
Science, Program of Nursing
Nursing intervention
Preparing the pt for surgery.
Orient pt and explain the procedure and plan of care to decrease anxiety.
Instruct the pt not to touch to decrease contamination.
Administer preoperative eye drops.
Postoperative care;
Administer medication as prescribed.
Teach the pt to report sudden pain and restlessness with increased pulse.
Caution pt against coughing, sneezing, rapid movement, bending.
Encourage pt to wear shield at night to protect operated eye fro injury
while sleeping.
Diseases of sclera
1. Scleritis
It is an inflammation and swelling of sclera.
Etiology
Associated with connective tissue disorder like rheumatoid arthritis.
C/M
Severe pain.
The white part of the eye may appear red, swollen and a nodule which is painful
in touch.
Mgx
Heavy immune suppression.
Systemic corticosteroid and eye drops.
Systemic NSAIDs and treating the underlying cause.
Disease of uveal tract
1. Unveitis
Uveal tract comprises the middle vascular pigmented layer of the eye.
It is composed of three areas: The choroid.
The ciliary body.
The iris.
Def: - Uveitis is the inflammation of one or all structures of the uveal tract.
Because the uvea contains many of the blood vessels that nourish the eye and because it
borders many other parts of the eye, inflammation of this layer may threaten vision.
Cause
Bacteria ( TB).
Virus (CMV, syphilis, herpes zoster and simplex).
Fungi (toxoplasmosis, histoplasmosis, ocular candidiasis).
Chemical
Trauma
Allergy
1) Acute anterior uveitis (iritis)
Is the most common type.
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 28
Debre Brehan University, School of Health
Science, Program of Nursing
Is characterized by a history of pain, photophobia, blurring of vision, & red eye.
Rx
Dilating drops (mydriasis) are instituted immediately to prevent scar formation &
adhesion to the lens (Synechiae), which may cause glaucoma by impending aqueous
outflow.
Local corticosteroids are used to decrease the inflammation.
Wearing sunglasses.
Analgesics.
2) Intermediate uveitis (Chronic cyclitis)
It is characterized by Floating spots in the field of vision.
Rx: - Topical or injectable corticosteroids are used in severe cases.
3) Posterior uveitis (Inflammation affecting the choroid or retina)
Is usually associated with some form of systemic disease, such as AIDS,
herpes simplex or zoster, tuberculosis.
C/M
Decreased or distorted vision.
eye redness & pain.
Rx Systemic corticosteroid.
Uveitis generally categorized into two. These are;
1. Non-granulomatous
2. Granulomatous
C/M for NGU;
Have acute onset.
Pain.
Photophobia.
Conjectival ejection (congestion of blood vessel), especially around the cornea.
Pupil will be small or irregular.
Vision will be blurred.
Hypopyon in severe case.
Anterior synechia (peripheral iris adheres to cornea and impeds out flow of
aqueshumour).
Posterior synechia (adherence of the iris and lens).
C/M for GU;
Insidious onset.
Vision is markedly and adversely affected.
Conjuctival injection is diffuse.
Vitreous clouding.
Photophobia pain is minimal.
2. Sympathetic Ophthalmia
It is a rare but devastating bilateral uveitis .
Occurs after a latent period of days to years after a penetrating injury to the uveal tract.
Cause Unknown
Predisposing factor: - Allergy
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 29
Debre Brehan University, School of Health
Science, Program of Nursing
C/M
Inflammation of injured eye, followed by inflammation of the unaffected (Sympathetic)
eye.
MX
Enucleation of the sightless eye within 10 days of injury is usually recommended to
reduce the risk of sympathetic disease in the other eye.
Indication for enucleation
Blindness after penetrating injury.
Painful blind eyes that is unresponsive to the medical treatment.
Tumor of the eye.
Disease of the inner ear
1. Panophthalmitis
It is an inflammation of all tissue of the eye ball.
Etiology
Bacteria.
Virus.
Fungus.
E.t.c
Hx of recent intraocular operation.
Penetrating trauma.
Common in immune compromised pts, such as HIV/AIDS and diabetes.
C/M
Severe pain.
Loss of vision.
Redness of conjunctiva and underlying episclera.
Mgx
Medication (antimicrobial plus steroids)
Topical.
Subconjuctival.
Intravitreally.
Systemically, or in combination form.
Surgery
Enucleation.
Injuries to the eye
1. Trauma to the eye
A. Blunt contusion
It is bruising of the periorbital soft tissue.
C/M
Swelling and discoloration of the tissue.
Bleeding in to the tissue and structure of the eye.
Pain.
Mgx
Reducing swelling and pain by applying cold and warm compress.
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 30
Debre Brehan University, School of Health
Science, Program of Nursing
Refer for ophthalmologist asst.
B. Hyphema
It is the presence of blood in the anterior chamber.
C/M
Pain.
Blood in the anterior chamber.
Increase IOP.
Mgx
Usually spontaneously recovers.
If sever bed rest, and eye shield application.
C. Orbital fracture
It is fracture and dislocation of the wall of the orbit, orbital margin or both.
Cause:- Injury on the cranial area.
C/M
Rhinorrhea.
Contusion.
Diplopia.
Mgx
May heal by itself, if no displacement or infringement on the other structure.
Surgery:- repair of the orbital floor.
D. Foreign body
It is the presence of foreign material on the cornea or conjunctiva.
C/M
Severe pain with lacrimation.
Foreign body sensation.
Photophobia.
Redness.
Swelling.
Mgx
Consider a medical emergency.
Removal of foreign body through irrigation, cotton tipped applicator.
Surgical removal.
E. Laceration/Perforation.
It is cutting or penetration of soft tissue.
C/M
Pain
Bleeding
Lacrimation
Photophobia
Mgx
Consider as medical emergency.
Surgical repair- method of repair depends on the severity of injury.
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 31
Debre Brehan University, School of Health
Science, Program of Nursing
Antibiotics.
F. Ruptured globe
It is concussive injury to globe with tears in the ocular coat, usually the globe.
C/M
Pain
Altered IOP
Limitation of gaze in field of rupture
Hyphema
hemorrhage
Mgx
Consider as medical emergency.
Surgical repair
Antibiotics
Steroids
Enucleation
2.Burn of the eye
It is the destruction of the eye tissue by chemical, thermal, and ultraviolet ray.
A. Burn of chemical agent that is caused by alkali or acids.
C/M
Pain
Burning
Lacrimation
Photophobia
Mgx
Consider as medical emergency.
Copious irrigation until PH is 7.
Keratoplasty for severe scaring.
Antibiotics.
B. Burns of thermal sources
C/M
Pain
Burned skin
Blisters
Mgx
First aid-apply sterile dressing.
Pain control.
Leave fluid blebs intact.
Suture eyelid together to protect eye if perforation is possible.
Skin grafting with severe second and third degree burns.
C. Burn of UV source
C/M
Pain
Foreign body sensation
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 32
Debre Brehan University, School of Health
Science, Program of Nursing
Mgx
1.
C/M
Dx
Mgx
Lacrimation
Photophobia
Pain relief.
Bilateral patching with antibiotic ointment and cycloplegics.
Other eye condition
1. Glaucoma (Disorder of an aqueous Humor Circulation)
Glaucoma is a pathological rise in the intra ocular pressure that causes damage to the
various structure of the eye, especially the optic nerve.
It is the cause of blindness.
There are four types of glaucoma. These are;
1. Congenital .
2. Closed angle (acute).
3. Open angle (chronic)
4. Secondary.
Congenital glaucoma.
It is a rare condition that occurs in infant and neonates
The diameter of the cornea increase in size.
The cornea becomes edematous
Tonometry exam-increase IOP.
Medical-Pilocarpine drops, Acetazolamide tablet.
Surgical-Goniotomy-to incise the mesodermal membrane in the angle of anterior
chamber.
2. Closed angle glaucoma
It accounts for 10% of the primary glaucoma.
Etiology
Mechanical blockage of the anterior chamber angle.
C/M
A sudden severe pain in and around the eye.
Nausea and vomiting
Pupil mid-dilated and fixed.
Hazy appearing cornea due to corneal edema.
A sudden elevation of IOP
Dx
Slit lamp exam nation.
Tonometry examination.
Mgx
Medical
Lower the IOP as quick as possible by medical means.
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 33
Debre Brehan University, School of Health
Science, Program of Nursing
Miotics- Used to constrict the pupil and contract the ciliary muscle, thus the iris is
drawn away from cornea; aqueous humor may drain through lymph spaces
(meshwork) ion to canal of schlemm.
E.g. Pilocarpine drops 2-4% every 5 minute fro an hour, and then every hour for 12 hour
topically.
Carbonic anhydrase inhibitor-restricts action of the enzyme that is necessary to
produce aqueshumor.
E.g. Acetazolamide (diamox)250mg QID.
Hyperosmotic agents-reduce IOP by promoting diuresis.
E.g. Mannitol IV.
Surgical
Iridecomy- excision of a small portion of the iris where by AH can bypass. This
prevents the periphery of the iris blocking the angle of the anterior chamber.
Trabeculectomy-partial thickness sclera, resection with small part of trabecular
meshwork and iridectomy.
Laser iridotomy-multiple tiny laser incision to create openings for AH flow.
3. Open angle glaucoma
Makes up 90% of primary glaucoma cases.
Its incidences is increased with age.
Etiology
Degenerative changes occur in the trabecular meshwork and canal of schelmm.
Risk factors
AGE.
Familial history of glaucoma.
Diabetes
Hypertension
C/M
Mild, bilateral discomfort (tired feeling in the eyes, foggy vision).
Slowly developing impairment of peripheral vision with dilated pupil.
Progressive loss of visual field.
No pain or inflammation.
Dx
Paleness of the optic disk.
Optic nerve atrophy.
Rise in IOP.
Mgx
Medical
Reduce the IOP by medication- the medication should be continued for the rest of
the patient life
Pilocarpine drops 2-4% QID.
Adrenaline drops 1% BID.
Timolol/Timoptol/ drops ).25-0.5% BID.
Surgical
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 34
Debre Brehan University, School of Health
Science, Program of Nursing
Iridencleisis- an opening is created b/n anterior chamber and space beneath the
conjunctiva; this by pass the blocked meshwork, and AH is absorbed into conjunctival
tissues.
Cyclodiathermy/Cylocryotherapy-destruction of ciliary body with a high frequency
electrical current or supercooled probe.
4. Secondary glaucoma.
It is a type of glaucoma caused by a specific causes or pathologies.
Etiology
Hemorrhage.
Corticosteroid use.
Uveitis.
Mgx
Treat the cause.
2. Strabismus/Squint
It is the situation where by the two eyes are looking in different directions.
Etiology
Disorder of vision.
Disorder of the eye movement secondary in the abnormality on the muscle that controls
the movement.
Effects of squint
In adults
Double vision/diplopia/.
Abnormal head posture.
In children
Ambylopia/lazy eye/.
C/M
The corneal light reflex.
This is the best and simplest test of squint.
If the two eyes are straight, then the two corneal light reflexes are central and
symmetrical, but if one eye squints, then the reflex deviates from the center of the
cornea.
Testing the ocular movements.
There are six extra ocular muscle, and each one produces most of the movement
in the particular direction.
Mgx
In children
Try to correct any refractive errors and ambylopia before straightening the squint
surgically.
Patching the good eye.
Surgical correction by either weakening, straightening or realigning the extra ocular
muscles
In adults
Cosmetic surgery is the only treatment.
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 35
Debre Brehan University, School of Health
Science, Program of Nursing
3. Diabetic Retinopathy
Is a frequent complication of DM.
Occur after 20years of having DM.
Caused by damage to or occlusion of the blood vessels those nourish the retina.
Weakened blood vessels become hyper-permeable & leak, causing micro-hemorrhages,
retinal swelling, or exuadative deposits.
Progressive retinal ischemia stimulates the formation of new blood vessels
(neovascularization).
These new vessels are fragile & may rapture, causing sub retinal hemorrhage or bleeding.
The vitreous body also, they may form fibro vascular bands that contract, resulting in
traction & subsequent retinal detachment.
There are five stages of diabetic retinopathy.
Background retinopathy
Occurs in most diabetics about 20years after the onset of the disease.
Has no symptom until macula is involved.
C/M: - The fundus has dots (Micro - Aneurysms), blots (Small hemorrhage), & hard
waxy exudates (leakages of lipids from the hemorrhaging blood vessels.
Maculopathy
It is main cause of visual impairment in non insulin dependent DM.
Pre Proliferative retinopathy
Occurs in eyes with background retinopathy only.
C/M: - The retina is ischemic which causes;
Cotton wool spot
Dilation, beading, looping of blood vessels
Arteriole narrowing
Large dark blot hemorrhage
Proliferative retinopathy
Is the main cause of visual impairment in IDDM.
Advanced retinopathy
It is the end result of uncontrolled proliferative retinopathy & results in blindness.
Generally C/M of Diabetic retinopathy is;
If fluid collects at the macula, the patient notices blurred central vision.
Vitreous hemorrhage in cloudy or hazy vision of sudden onset.
Mgx
Laser photocoagulation surgery is useful. An intense beam of laser light is used to seal of
leaking blood vessels & destroy abnormal new ones.
Control DM.
4. Retinal detachment
Retinal detachment occurs when there is a separation of the neuro-sensory retina from the
underlying pigment epithelium layer of the retina.
Neurosensery retina contains: - rods & cones.
Causes: - The neural retina can be either pulled, pushes or floated off the underlying
epithelial layer
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 36
Debre Brehan University, School of Health
Science, Program of Nursing
Pulled off: - by vitreous traction, which occurs when new blood vessels
have grow in to the vitreous.
This condition con be caused by;
DM.
Retinal hemorrhage .
Vitreous hemorrhage.
Pushed off: - A lesion behind the retina . such as choroidal tumors,
hemorrhage, choroiditis & retinopathies
Floated off :- If a tear or hole appears in the retina, subretinal fluid or
vitreous fluid enters the hole, floating the neural layer off the epithelial
layer. Rhegmatagenaus ( tear induced ) detachment - is most common
type.
In general the causes can be;
congenital malformation
Metabolic disorders
Vascular disease
Neoplasm
trauma
Degenerative changes
C/F: - History of floating or flashing lights or both. The floaters are perceived as tiny
dark spots or cobwebs.
Spreading shadow or curtain moving across the field of vision, resulting in blurred vision
& loss of visual field as the retina separates
Decreased central acuity or lass or central vision
Flashing lights (photopia).
Medical-Surgical Nursing-II, Eye Disorder Prepared by Tesfa D.
(B.Sc. in Nursing)
Page 37
Vous aimerez peut-être aussi
- Congenital Corneal DisordersDocument101 pagesCongenital Corneal Disorderseyemd_in_training100% (1)
- Diabetic FootDocument104 pagesDiabetic FootadibeuutPas encore d'évaluation
- Hepatic Encephalopathy and ComaDocument19 pagesHepatic Encephalopathy and ComaJas Castro JoveroPas encore d'évaluation
- Reflective ExemplarDocument2 pagesReflective Exemplarapi-531834240Pas encore d'évaluation
- IV Therapy History and StandardsDocument31 pagesIV Therapy History and Standardsrommelrn100% (1)
- Blood Transfusion ModuleDocument45 pagesBlood Transfusion ModuleElisse RamosPas encore d'évaluation
- Pleural Fluid AnalysisDocument15 pagesPleural Fluid AnalysisNatalie Sarah MoonPas encore d'évaluation
- Case Study StrokeDocument5 pagesCase Study StrokelilutzuPas encore d'évaluation
- Pericarditis NCLEX Review: Serous Fluid Is Between The Parietal and Visceral LayerDocument2 pagesPericarditis NCLEX Review: Serous Fluid Is Between The Parietal and Visceral LayerlhenPas encore d'évaluation
- IV Fluid ChartDocument2 pagesIV Fluid Charthady920Pas encore d'évaluation
- Leadership & Management in Nursing NCLEX Practice Quiz (80 Questions)Document38 pagesLeadership & Management in Nursing NCLEX Practice Quiz (80 Questions)Mack MakaPas encore d'évaluation
- MastectomyDocument53 pagesMastectomyAngelica RelanaPas encore d'évaluation
- Ventilator Care Bundle Guidelines-LancsandsouthcumbriaDocument18 pagesVentilator Care Bundle Guidelines-LancsandsouthcumbriaPeriyarselvi VkRamuPas encore d'évaluation
- Equipments in Icu: Mr. Amol Temkar Asso. Prof College of NursingDocument46 pagesEquipments in Icu: Mr. Amol Temkar Asso. Prof College of NursingAmol TemkarPas encore d'évaluation
- Rules and Equations for Oxygen Therapy and Gas ExchangeDocument11 pagesRules and Equations for Oxygen Therapy and Gas ExchangeJenn77x1Pas encore d'évaluation
- Complications of Intravenous TherapyDocument47 pagesComplications of Intravenous TherapyKateAngeliRebosuraPas encore d'évaluation
- Formulating HypothesisDocument3 pagesFormulating HypothesisMatthew Lim MontenegroPas encore d'évaluation
- Management of Vacuum Assisted Closure TherapyDocument14 pagesManagement of Vacuum Assisted Closure TherapyVoiculescu MihaelaPas encore d'évaluation
- Cushings SyndromeDocument51 pagesCushings SyndromeTina TalmadgePas encore d'évaluation
- HIV Practice TestDocument2 pagesHIV Practice TestJoslyn GrossPas encore d'évaluation
- Blood Pressure Lesson Plan: SummaryDocument3 pagesBlood Pressure Lesson Plan: SummaryHabeeba Malik100% (1)
- Carpal Tunnel Surgery, Hand Clinics, Volume 18, Issue 2, Pages 211-368 (May 2002)Document151 pagesCarpal Tunnel Surgery, Hand Clinics, Volume 18, Issue 2, Pages 211-368 (May 2002)alinutza_childPas encore d'évaluation
- Jurnal 1 SBAR PDFDocument10 pagesJurnal 1 SBAR PDFIRFA KHIKMATUL KHULUQPas encore d'évaluation
- Operating Room Nurse Interview QuestionsDocument2 pagesOperating Room Nurse Interview Questionsali aliPas encore d'évaluation
- Superficial and Deep ReflexesDocument28 pagesSuperficial and Deep ReflexesShilpa SPas encore d'évaluation
- Cabg Case Study FormDocument9 pagesCabg Case Study FormVlad ConstantinPas encore d'évaluation
- Pulmonary CirculationDocument4 pagesPulmonary CirculationDr Md Abedur RahmanPas encore d'évaluation
- IV Complications Signs, Prevention, TreatmentDocument6 pagesIV Complications Signs, Prevention, TreatmentMercicae APas encore d'évaluation
- Perioperative Nursing - 2edited For BSN 3Document122 pagesPerioperative Nursing - 2edited For BSN 3JL D. BusiaPas encore d'évaluation
- July 2011 NLE Result: School PerformanceDocument16 pagesJuly 2011 NLE Result: School PerformanceLyle SantosPas encore d'évaluation
- Nursing Management of Common Skin and Parasitic DiseasesDocument14 pagesNursing Management of Common Skin and Parasitic Diseasesyer tagalajPas encore d'évaluation
- Chronic Renal FailureDocument29 pagesChronic Renal Failuregeorgia.langPas encore d'évaluation
- Preoperative Assessment of Diabetic PatientsDocument2 pagesPreoperative Assessment of Diabetic PatientsShilpa Pradhan100% (1)
- Sinus Rhythms: Dysrhythmia Recognition & ManagementDocument29 pagesSinus Rhythms: Dysrhythmia Recognition & Managementkamel6Pas encore d'évaluation
- CHN HandoutDocument4 pagesCHN HandoutRaymund Christopher Dela PeñaPas encore d'évaluation
- Nurse's Safety Attitudes As Perceived by Geriatric Patients in Homecare InstitutionsDocument16 pagesNurse's Safety Attitudes As Perceived by Geriatric Patients in Homecare InstitutionsGlobal Research and Development ServicesPas encore d'évaluation
- Surgical ScrubbingDocument2 pagesSurgical ScrubbingAnn Mayie100% (1)
- Blood Transfusion: Etiology of Blood CellDocument4 pagesBlood Transfusion: Etiology of Blood Cellbunso padillaPas encore d'évaluation
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideD'EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuidePas encore d'évaluation
- Haramaya University College of Health and Medical Sciences School of Nursing and Midwifery MSC in Nursing (Major in Adult Health Nursing)Document54 pagesHaramaya University College of Health and Medical Sciences School of Nursing and Midwifery MSC in Nursing (Major in Adult Health Nursing)Beyene Feleke100% (1)
- Observation Report - Hemodialysis - Kit P. RoaquinDocument15 pagesObservation Report - Hemodialysis - Kit P. Roaquineljhayar_18Pas encore d'évaluation
- Principles of CPR and CARDIAC MASSAGEDocument34 pagesPrinciples of CPR and CARDIAC MASSAGEBharat BhushanPas encore d'évaluation
- Case Study 1Document9 pagesCase Study 1andry natanel tonyPas encore d'évaluation
- Case Study PeriopDocument3 pagesCase Study PeriopSteve25% (4)
- EPILEPSY Lecture NoteDocument17 pagesEPILEPSY Lecture Notemohammed awolPas encore d'évaluation
- Basic Principles in Disaster Nursing and ShockDocument12 pagesBasic Principles in Disaster Nursing and ShockitsmyhavenPas encore d'évaluation
- Heat Stroke PatophysiologyDocument48 pagesHeat Stroke PatophysiologyMbenk NjoePas encore d'évaluation
- Mastectomy: Prepared By: Hilario, Eunice Lamoste, Jenebelle Lopez, Maria SofiaDocument34 pagesMastectomy: Prepared By: Hilario, Eunice Lamoste, Jenebelle Lopez, Maria SofiaSofia LopezPas encore d'évaluation
- Thesisproposalformat 110311092418 Phpapp01 PDFDocument23 pagesThesisproposalformat 110311092418 Phpapp01 PDFAilee MnrngPas encore d'évaluation
- Intradialytic Stretching Exercises On Fatigueand Muscle CrampsDocument6 pagesIntradialytic Stretching Exercises On Fatigueand Muscle CrampsInternational Journal of Innovative Science and Research TechnologyPas encore d'évaluation
- Who Safe Surgery Checklist: Sign inDocument3 pagesWho Safe Surgery Checklist: Sign inJann Marie IsidroPas encore d'évaluation
- Final Nursing Skills Check-OffDocument17 pagesFinal Nursing Skills Check-OffWMG 10/10100% (1)
- Fluid and ElectrolytesDocument29 pagesFluid and ElectrolytesLinh Tra100% (1)
- Cardiac SurgeryDocument27 pagesCardiac SurgeryReeti Singh100% (1)
- Neurologica L Assessment: Lijo Joseph Msc. Nursing Ist YrDocument38 pagesNeurologica L Assessment: Lijo Joseph Msc. Nursing Ist YrBibi Renu100% (2)
- MARCOS - Legal Issues of ElderlyDocument2 pagesMARCOS - Legal Issues of ElderlyArian May MarcosPas encore d'évaluation
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsD'EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsPas encore d'évaluation
- A Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsD'EverandA Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsPas encore d'évaluation
- Unit-8-Ear, Nose, Mouth, Sinus and Pharynx ExaminationDocument104 pagesUnit-8-Ear, Nose, Mouth, Sinus and Pharynx ExaminationMinlik-alew Dejenie100% (5)
- Unit-16-Integrated Physical ExaminationDocument20 pagesUnit-16-Integrated Physical ExaminationMinlik-alew DejeniePas encore d'évaluation
- Unit-15-Genitourinary ExaminationDocument110 pagesUnit-15-Genitourinary ExaminationMinlik-alew Dejenie83% (6)
- Fluid and Electrolyte ImbalanceDocument82 pagesFluid and Electrolyte ImbalanceMinlik-alew Dejenie67% (3)
- Unit-14-Neurological ExaminationDocument108 pagesUnit-14-Neurological ExaminationMinlik-alew Dejenie0% (1)
- Unit-6-Head, Neck, Thyroid and Lymph Nodes ExaminationDocument67 pagesUnit-6-Head, Neck, Thyroid and Lymph Nodes ExaminationMinlik-alew Dejenie100% (2)
- Unit-12-Heart and Blood Vessel ExaminationDocument83 pagesUnit-12-Heart and Blood Vessel ExaminationMinlik-alew DejeniePas encore d'évaluation
- Unit-13-Musculo-Skeletal ExaminationDocument79 pagesUnit-13-Musculo-Skeletal ExaminationMinlik-alew DejeniePas encore d'évaluation
- Unit-7-Eye ExaminationDocument86 pagesUnit-7-Eye ExaminationMinlik-alew Dejenie100% (5)
- Introduction To Nursing LeadershipDocument12 pagesIntroduction To Nursing LeadershipMinlik-alew DejeniePas encore d'évaluation
- Unit-5-Integumentary ExaminationDocument47 pagesUnit-5-Integumentary ExaminationMinlik-alew DejeniePas encore d'évaluation
- Unit-2-History Taking and RecordingDocument40 pagesUnit-2-History Taking and RecordingMinlik-alew DejeniePas encore d'évaluation
- Unit 7-Problem Solving, Critical Thinking, Creativity, and Decision MakingDocument127 pagesUnit 7-Problem Solving, Critical Thinking, Creativity, and Decision MakingMinlik-alew Dejenie93% (30)
- Unit 6-Time Management, Stress Managment and DelegationDocument81 pagesUnit 6-Time Management, Stress Managment and DelegationMinlik-alew DejeniePas encore d'évaluation
- Unit 3-Organizing Nursing CareDocument60 pagesUnit 3-Organizing Nursing CareMinlik-alew Dejenie100% (1)
- Unit 5-Health Management Information System (HMIS)Document47 pagesUnit 5-Health Management Information System (HMIS)Minlik-alew Dejenie91% (69)
- Unit 2-Nursing Personnel ManagementDocument60 pagesUnit 2-Nursing Personnel ManagementMinlik-alew Dejenie92% (12)
- Assessment of Knowledge, Attitude Andpractice Toward Sexually Transmitteddiseases in Boditi High School StudentsDocument56 pagesAssessment of Knowledge, Attitude Andpractice Toward Sexually Transmitteddiseases in Boditi High School StudentsMinlik-alew Dejenie88% (8)
- Asessment of Mother's Practice Towards Child Vaccination and Its Associated Factors With Child Vaccination inDocument24 pagesAsessment of Mother's Practice Towards Child Vaccination and Its Associated Factors With Child Vaccination inMinlik-alew Dejenie100% (6)
- Nursing Education, Instruction and Curriculum Development-Function of Education.Document10 pagesNursing Education, Instruction and Curriculum Development-Function of Education.Minlik-alew DejeniePas encore d'évaluation
- Nursing Education, Instruction and Curriculum-Teaching.Document10 pagesNursing Education, Instruction and Curriculum-Teaching.Minlik-alew DejeniePas encore d'évaluation
- Debre Brehan University - Nursing Program Module.Document82 pagesDebre Brehan University - Nursing Program Module.Minlik-alew Dejenie100% (3)
- CruculumDocument3 pagesCruculumMinlik-alew DejeniePas encore d'évaluation
- Nursing Education, Instruction and Curriculum Development-Assessment of Student Performance.Document22 pagesNursing Education, Instruction and Curriculum Development-Assessment of Student Performance.Minlik-alew DejeniePas encore d'évaluation
- Assessment of Knowledge, Attitude Andpractice Toward Sexually Transmitteddiseases in Boditi High School StudentsDocument56 pagesAssessment of Knowledge, Attitude Andpractice Toward Sexually Transmitteddiseases in Boditi High School StudentsMinlik-alew Dejenie88% (8)
- Nursing Education, Instruction and Curriculum Development-Assessment of Student Performance.Document22 pagesNursing Education, Instruction and Curriculum Development-Assessment of Student Performance.Minlik-alew DejeniePas encore d'évaluation
- Psychiatric Disorder.Document127 pagesPsychiatric Disorder.Minlik-alew DejeniePas encore d'évaluation
- Assessment of Psychiatric PatientDocument84 pagesAssessment of Psychiatric PatientMinlik-alew DejeniePas encore d'évaluation
- Introduction To Psychiatric NursingDocument88 pagesIntroduction To Psychiatric NursingMinlik-alew Dejenie100% (1)
- SOP-for RecallDocument3 pagesSOP-for RecallNilove PervezPas encore d'évaluation
- Nagina Cotton Mills Annual Report 2007Document44 pagesNagina Cotton Mills Annual Report 2007Sonia MukhtarPas encore d'évaluation
- CALCULUS PHYSICS MIDTERMDocument41 pagesCALCULUS PHYSICS MIDTERMMACARIO QTPas encore d'évaluation
- Differential Pulse Code ModulationDocument12 pagesDifferential Pulse Code ModulationNarasimhareddy MmkPas encore d'évaluation
- Inborn Errors of Metabolism in Infancy: A Guide To DiagnosisDocument11 pagesInborn Errors of Metabolism in Infancy: A Guide To DiagnosisEdu Diaperlover São PauloPas encore d'évaluation
- Command List-6Document3 pagesCommand List-6Carlos ArbelaezPas encore d'évaluation
- Trillium Seismometer: User GuideDocument34 pagesTrillium Seismometer: User GuideDjibril Idé AlphaPas encore d'évaluation
- Flexible Regression and Smoothing - Using GAMLSS in RDocument572 pagesFlexible Regression and Smoothing - Using GAMLSS in RDavid50% (2)
- Techniques in Selecting and Organizing InformationDocument3 pagesTechniques in Selecting and Organizing InformationMylen Noel Elgincolin ManlapazPas encore d'évaluation
- Indian Standard: Pla Ing and Design of Drainage IN Irrigation Projects - GuidelinesDocument7 pagesIndian Standard: Pla Ing and Design of Drainage IN Irrigation Projects - GuidelinesGolak PattanaikPas encore d'évaluation
- 4 Factor DoeDocument5 pages4 Factor Doeapi-516384896Pas encore d'évaluation
- Vector 4114NS Sis TDSDocument2 pagesVector 4114NS Sis TDSCaio OliveiraPas encore d'évaluation
- I Will Be Here TABSDocument7 pagesI Will Be Here TABSEric JaoPas encore d'évaluation
- Mosfet 101Document15 pagesMosfet 101Victor TolentinoPas encore d'évaluation
- CS709 HandoutsDocument117 pagesCS709 HandoutsalexPas encore d'évaluation
- Managerial EconomicsDocument3 pagesManagerial EconomicsGuruKPOPas encore d'évaluation
- THE DOSE, Issue 1 (Tokyo)Document142 pagesTHE DOSE, Issue 1 (Tokyo)Damage85% (20)
- Human Rights Alert: Corrective Actions in Re: Litigation Involving Financial InstitutionsDocument3 pagesHuman Rights Alert: Corrective Actions in Re: Litigation Involving Financial InstitutionsHuman Rights Alert - NGO (RA)Pas encore d'évaluation
- SEC QPP Coop TrainingDocument62 pagesSEC QPP Coop TrainingAbdalelah BagajatePas encore d'évaluation
- Price List PPM TerbaruDocument7 pagesPrice List PPM TerbaruAvip HidayatPas encore d'évaluation
- Worksheet 5 Communications and Privacy: Unit 6 CommunicationDocument3 pagesWorksheet 5 Communications and Privacy: Unit 6 Communicationwh45w45hw54Pas encore d'évaluation
- Ofper 1 Application For Seagoing AppointmentDocument4 pagesOfper 1 Application For Seagoing AppointmentNarayana ReddyPas encore d'évaluation
- Equilibruim of Forces and How Three Forces Meet at A PointDocument32 pagesEquilibruim of Forces and How Three Forces Meet at A PointSherif Yehia Al MaraghyPas encore d'évaluation
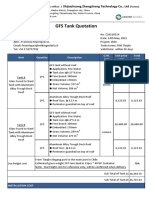
- GFS Tank Quotation C20210514Document4 pagesGFS Tank Quotation C20210514Francisco ManriquezPas encore d'évaluation
- Special Power of Attorney: Benedict Joseph M. CruzDocument1 pageSpecial Power of Attorney: Benedict Joseph M. CruzJson GalvezPas encore d'évaluation
- Nokia CaseDocument28 pagesNokia CaseErykah Faith PerezPas encore d'évaluation
- Qad Quick StartDocument534 pagesQad Quick StartMahadev Subramani100% (1)
- Baobab MenuDocument4 pagesBaobab Menuperseverence mahlamvanaPas encore d'évaluation
- Kalley Ltdn40k221twam Chassis msd6308 SM PDFDocument49 pagesKalley Ltdn40k221twam Chassis msd6308 SM PDFjulio cesar calvetePas encore d'évaluation
- Ielts Practice Tests: ListeningDocument19 pagesIelts Practice Tests: ListeningKadek Santiari DewiPas encore d'évaluation