Académique Documents
Professionnel Documents
Culture Documents
Diabetes Research Paper
Transféré par
Lysol007Description originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Diabetes Research Paper
Transféré par
Lysol007Droits d'auteur :
Formats disponibles
Running head: DIABETES MELLITUS IN OLDER ADULTS
Research Paper: Diabetes Mellitus in Older Adults
Diabetes Mellitus in Older Adults
Introduction
Diabetes mellitus encompasses a group of diseases characterized by high levels of blood
glucose resulting from the bodys failure to produce insulin (insulin-dependent Type 1) or
inability to process insulin (non-insulin-dependent Type 2). It is a metabolic disorder that affects
carbohydrate, fat and protein metabolism in the body. Type 1 is typically seen in children and
young adults, although the disease onset can begin at any age.
The main discussion will be of Type 2 diabetes as it pertains to older adults. Other
classifications include prediabetes (elevated blood glucose levels but not enough to be
considered Type 2) and gestational diabetes (develops during pregnancy). This paper examines
the etiology, epidemiology, pathophysiology, clinical manifestations, evaluation, management
and nursing concerns of diabetes mellitus in the elderly population.
Etiology
DIABETES MELLITUS IN OLDER ADULTS
The risk factors for Type 1 diabetes include genetic, autoimmune and environmental
factors. Previously called juvenile-onset diabetes, a genetic predisposition is the main cause for
this type of diabetes although environmental factors such as a virus may trigger the disease as
well. Mauk (2014) states that older age, a family history of diabetes, obesity, race (African
Americans, Hispanics Native Americans, Asian Americans, Pacific Islanders), hypertension,
decreased HDL levels, physical inactivity, polycystic ovary syndrome, and a history of
gestational or prediabetes are all risk factors for Type 2 diabetes.
People beyond age 45 are at an increased risk of getting diabetes. This is due to lifestyle
changes in older age including less regular exercise and the bodys natural decrease in muscle
mass. In this way, old age increases many other risk factors for developing diabetes.
Having a family history of diabetes means it is highly likely that the person will develop
diabetes because of the genetic link. For the older adult, this is especially important because it is
a non-modifiable risk factor and makes the person directly vulnerable to the disease regardless of
any other factors.
Mayo Clinic (2014) explains that obesity is a primary risk factor directly related to the
development of diabetes due to the added stress on the bodys ability to use insulin to properly
control blood sugar levels, which can make the body become resistant to insulin due to the
increase in the amount of fatty tissue in the body. This is a common issue with older adults who
tend to not exercise regularly leading to difficulties with managing weight, and over time, the
prolonged effects on the body can cause diabetes.
Epidemiology
Diabetes mellitus is the seventh leading cause of death among older adults (Mauk, 2014).
According to the Centers for Disease Control and Prevention (2014), 29.1 million people (9.3%
of the population) have diabetes. That is about 1 out of every 11 people just in the U.S. Of those,
21 million people are diagnosed and 8.1 million remain undiagnosed. The risk of death for adults
DIABETES MELLITUS IN OLDER ADULTS
with diabetes is 50% higher than those without diabetes. 15-30% of people with prediabetes will
develop Type 2 diabetes in five years without proper weight management and physical activity.
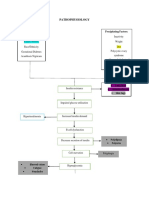
Pathophysiology
Type 1 diabetes develops when the bodys immune system destroys pancreatic beta cells,
the cells in the body responsible for making the hormone insulin to regulate blood glucose levels,
resulting in chronic hyperglycemia. However with Type 2 diabetes, a genetic predisposition
along with obesity causes insulin resistance in the body. Glucose is not properly utilized and high
levels remain in the blood causing hyperglycemia. The body then starts to produce too much
insulin and as the need for insulin increases, the pancreas gradually loses its ability to produce
insulin. Eventually the beta cells stop working properly, leading to inadequate insulin secretion
which then develops into chronic hyperglycemia in the body and diabetes (Mayo Clinic, 2014).
Clinical Manifestations
The clinical manifestations of diabetes mellitus include excessive thirst (polydipsia),
frequent urination (polyuria), blurring of vision, increased fatigue, slow healing cuts or sores, dry
and itchy skin and numbness or tingling of feet (National Institute on Aging, 2012). Unexplained
weight loss also occurs due to the increased breakdown of fat from insulin resistance. Older
adults may also have urinary incontinence related to polyuria, which can cause dehydration.
Evaluation
There are several diagnostic tests for diabetes as noted in Hale (2014). These are often
taken on two separate occasions. A random/casual glucose test is taken at any time of the day and
the criteria for diabetes is a blood glucose of 200 mg/dl or higher. A fasting glucose test is taken
after going without food for at least eight hours, and is positive for diabetes with blood glucose
126 mg/dl or higher. An oral glucose tolerance test is taken after fasting overnight and then again
two hours after ingesting glucose, with blood glucose 200 mg/dl or higher.
The hemoglobin A1C test is used to monitor the average amount of glucose in the blood
over the last few months. Glucose permanently attaches to hemoglobin in the blood, which is
DIABETES MELLITUS IN OLDER ADULTS
why this test is frequently used to determine the extent of uncontrolled blood glucose in the body
over a period of time. An A1C range of 6-7% indicates optimal glycemic control.
Management
The management of diabetes mellitus in the older adult is a combination of diet, exercise
and medications (Mauk, 2014). Meal planning and diet control helps with regulating weight and
the goal is to keep the body weight at a normal range. A higher intake of high fiber and low-fat
foods such as fruits, vegetables and whole grains and a reduction in foods high in fat and sugar
are optimal to long-term diabetes management (Mayo Clinic, 2014). Exercise burns calories,
which also helps in maintaining weight. It also stimulates proper insulin function, allowing the
bodys production of insulin to work more efficiently and improves glucose levels in older adults
(NIA, 2012). Medications may include oral hypoglycemic agents and/or insulin injections. A side
effect of insulin is hypoglycemia, so it is important for the older adult to understand the signs and
symptoms of hyperglycemia and hypoglycemia and know how to monitor blood glucose.
Some people are able to manage diabetes just through diet and exercise, while others
often need pharmacologic interventions. Mayo Clinic (2014) lists a few examples of
medications: metformin (Glucophage, Glumetza), sulfonylureas, meglitinides and insulin
therapy. Metformin is typically the first medication prescribed for Type 2 diabetes, which
improves the bodys sensitivity to insulin and also lowers glucose production in the liver.
Glyburide (DiaBeta, Glynase), glipizide (Glucotrol) and glimepiride (Amaryl) are medications in
the classification of sulfonylureas, which help the body secrete more insulin. Meglitinides such
as repaglinide (Prandin) and nateglinide (Starlix) are similar to sulfonylureas in terms of action
on the body, except these are faster-acting and have a lower risk of causing hypoglycemia.
Nursing Concerns
The main nursing concerns for diabetes fall under education, management and
prevention. The nurse works with the older adult to plan treatment goals that will prevent long
DIABETES MELLITUS IN OLDER ADULTS
term complications such as heart and kidney problems in the older adult. Older adults should also
be educated to practice good and safe self-care techniques.
It is essential for the nurse to emphasize eating healthy foods and following a diet
program, and may include a referral to a registered dietician if necessary. Other important
teaching issues include the importance of getting enough exercise and how to monitor blood
sugar in response to food, exercise, illness and medications. This includes teaching of how to
use a glucometer to check blood sugar, as well as how to assess for signs of hyperglycemia
(frequent urination, dry mouth, nausea, fatigue) and hypoglycemia (sweating, shakiness,
dizziness, hunger).
Within this area, the nurse should be able to evaluate the proficiency of the older adult in
administering medications for themselves. Nurses should consider if there are vision problems or
the client has a history of arthritis. If the older adult has anxiety about administering medications
themselves, family members and caregivers can be taught how to give insulin. Family members
are a vital part of the disease prevention process and are also required to understand care for
diabetes. For example, they need to learn about diabetes, recognize signs and symptoms and
attend diabetes education classes if needed.
Managing proper foot care is also important in the diabetic patient due to the increased
risk of infection and slow healing that occurs with the disease process, reducing the risk for
amputation (Mauk, 2014). The nurse should demonstrate proper foot care behaviors to never go
barefoot outside, always wear well-fitting shoes, prevent exposure to extreme temperatures,
inspect the feet daily and see a podiatrist for foot inspection annually.
Depending on when diabetes is diagnosed in the older adult, macrovascular and
microvascular diseases caused by diabetes may or may not have progressed. Mauk (2014) notes
that it is important to continuously monitor and assess for the development of these
complications. Coronary heart disease, stroke and peripheral vascular disease are macrovascular
DIABETES MELLITUS IN OLDER ADULTS
diseases that potentially could lead to amputation. Chronic kidney disease leading to end-stage
renal disease and diabetic neuropathy (leading factor of blindness) are some of the common
microvascular complications. Peripheral neuropathy is another concern due to the lack of
sensation, and this can also contribute to a higher risk for falls along with urinary continence due
to the increased dizziness caused by dehydration. The nurse is most concerned with the
management of pain and the maintenance of a healthy lifestyle. In this situation, physical therapy
may also be helpful to the treatment process.
Conclusion
Diabetes is one of the most dangerous and prevalent diseases affecting both the young
and old. It is important for both the healthcare professional and the client to be patient because
this is a serious lifelong disease. Planning treatment goals and establishing a diet/exercise and
medication regimen is essential to maintaining a healthy lifestyle and preventing as many
complications of the disease as possible. This allows the older adult to have responsibility and
control over his or her diabetes management.
References
Mauk, K. L. (2014). Gerontological nursing: Competencies for care (3rd ed.). Burlington, MA:
Jones and Bartlett Learning.
Centers for Disease Control and Prevention. (2014) A snapshot: Diabetes in the United States
[Data file]. Retrieved from http://www.cdc.gov/diabetes/pubs/statsreport14/diabetesinfographic.pdf
DIABETES MELLITUS IN OLDER ADULTS
National Institute on Aging. (2012) Diabetes in older people: A disease you can manage [Data
file]. Retrieved from
http://www.nia.nih.gov/sites/default/files/diabetes_in_older_people_0.pdf
Mayo Clinic Staff. (2014). Type 2 diabetes: Risk factors. Retrieved from
http://www.mayoclinic.org/diseases-conditions/type-2-diabetes/basics/risk-factors/con20031902
Vous aimerez peut-être aussi
- Management of Tuberculosis: A guide for clinicians (eBook edition)D'EverandManagement of Tuberculosis: A guide for clinicians (eBook edition)Pas encore d'évaluation
- Diabetes MellitusDocument13 pagesDiabetes Mellitusdreneavalentinstefan100% (1)
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideD'EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuidePas encore d'évaluation
- Medication Error PaperDocument6 pagesMedication Error Paperapi-272761526Pas encore d'évaluation
- Case Study of DMDocument6 pagesCase Study of DMbuzz Q0% (1)
- Diabetes Melitus 2 DkaDocument104 pagesDiabetes Melitus 2 DkaLaiza Fatima LacsonPas encore d'évaluation
- Heart Failure and CAD Case StudyDocument38 pagesHeart Failure and CAD Case StudyAbno NavarretePas encore d'évaluation
- Examining root causes of poor health and diseaseDocument1 pageExamining root causes of poor health and diseaseDONITA DALUMPINESPas encore d'évaluation
- PICO DiabetesDocument12 pagesPICO DiabetesJaclyn Strangie67% (3)
- Conley - PGC ReflectionDocument9 pagesConley - PGC Reflectionapi-458494853Pas encore d'évaluation
- Transpersonal CaringDocument46 pagesTranspersonal CaringJorie Roco100% (1)
- Influenza Health Promotion ProjectDocument8 pagesInfluenza Health Promotion Projectapi-284269118Pas encore d'évaluation
- Maximizing NICU Care Through Cost-Effective TechnologiesDocument29 pagesMaximizing NICU Care Through Cost-Effective TechnologiesVonrey Tiana73% (11)
- Compare and Contrast The Insights Into Primary Health Care Provided by DRDocument2 pagesCompare and Contrast The Insights Into Primary Health Care Provided by DRKai GamiaoPas encore d'évaluation
- Nursing ReflectionDocument5 pagesNursing Reflectionvrunda patelPas encore d'évaluation
- Personal Nursing PhilosophyDocument5 pagesPersonal Nursing PhilosophyLaura Sotomayor100% (2)
- Disease EssayDocument5 pagesDisease Essayapi-309393081Pas encore d'évaluation
- TCP HeartburnDocument12 pagesTCP HeartburnArlene NicomedezPas encore d'évaluation
- Health Teachings On CHFDocument6 pagesHealth Teachings On CHFfLOR_ZIANE_MAEPas encore d'évaluation
- Diabetes MellitusDocument93 pagesDiabetes MellitusAllen Reyes SantosPas encore d'évaluation
- Managing Status Epilepticus in an Alcoholic PatientDocument4 pagesManaging Status Epilepticus in an Alcoholic PatientKrisPas encore d'évaluation
- Community Health AssessmentDocument12 pagesCommunity Health Assessmentapi-282833536100% (2)
- NFDN 2004 Professional PortfolioDocument2 pagesNFDN 2004 Professional Portfolioapi-32048921050% (2)
- Implementing EBN to Improve Patient CareDocument7 pagesImplementing EBN to Improve Patient CareKim ViñasPas encore d'évaluation
- Personal Nursing PhilosophyDocument8 pagesPersonal Nursing PhilosophyNicole Rowland100% (1)
- Research Paper - DiabetesDocument9 pagesResearch Paper - Diabetesapi-281590163Pas encore d'évaluation
- Hypertension and ExerciseDocument8 pagesHypertension and ExercisemeyqiPas encore d'évaluation
- Portfolio NFDN 2004 1Document4 pagesPortfolio NFDN 2004 1api-306095474100% (1)
- Chapter 1 Fundamental Concepts SPSS - Descriptive StatisticsDocument4 pagesChapter 1 Fundamental Concepts SPSS - Descriptive StatisticsAvinash AmbatiPas encore d'évaluation
- Types of Anemia ExplainedDocument8 pagesTypes of Anemia ExplainedApril Mae Magos LabradorPas encore d'évaluation
- Nursing PhilosophyDocument1 pageNursing PhilosophyNene DikePas encore d'évaluation
- The Problem and Its BackgroundDocument46 pagesThe Problem and Its Backgroundharoldpaulo100% (1)
- Lect15&16 Fluids&ElectrolytesDocument77 pagesLect15&16 Fluids&Electrolyteskhurram na100% (1)
- Running Head: Pico Question: Aseptic Technique 1Document10 pagesRunning Head: Pico Question: Aseptic Technique 1api-253019091Pas encore d'évaluation
- Diabetes Nursing EducationDocument4 pagesDiabetes Nursing EducationDerick RanaPas encore d'évaluation
- Gordon's 11 Functional Health PatternsDocument4 pagesGordon's 11 Functional Health Patternsnina angelaPas encore d'évaluation
- Medication Errors FinalDocument7 pagesMedication Errors Finalapi-469407326Pas encore d'évaluation
- NFDN 2005 Report On Progress of Professional PortfolioDocument2 pagesNFDN 2005 Report On Progress of Professional Portfolioapi-304652587Pas encore d'évaluation
- PICOTDocument8 pagesPICOTRaphael Seke OkokoPas encore d'évaluation
- Diabetes Care Practice Nurse Roles Attitudes and Concerns PDFDocument8 pagesDiabetes Care Practice Nurse Roles Attitudes and Concerns PDFDiabetesBhPas encore d'évaluation
- Case Study - A Patient With Type 1 Diabetes WhoDocument4 pagesCase Study - A Patient With Type 1 Diabetes WhoWulan AnggrahiniPas encore d'évaluation
- Medication Errors in NursingDocument7 pagesMedication Errors in Nursingapi-307925878Pas encore d'évaluation
- Master's in Nursing program explores healthcare economicsDocument14 pagesMaster's in Nursing program explores healthcare economicsMatet Sales Asuncion67% (3)
- A Patient's Bill of RightsDocument4 pagesA Patient's Bill of RightsMark ElbenPas encore d'évaluation
- Health Economics Final RequirementDocument20 pagesHealth Economics Final RequirementEmergency Room Department100% (1)
- Clinical Practicum II ProposalDocument30 pagesClinical Practicum II Proposalapi-281813422Pas encore d'évaluation
- PERIOPERATIVE NURSING OVERVIEWDocument93 pagesPERIOPERATIVE NURSING OVERVIEWJoel Santos100% (1)
- Integrated Management of Childhood IllnessDocument3 pagesIntegrated Management of Childhood IllnessJanine Alexis BuenviajePas encore d'évaluation
- Diabetic Teaching PaperDocument11 pagesDiabetic Teaching PaperKisha Griffin100% (2)
- Windshield SurveyDocument7 pagesWindshield Surveyapi-267488377Pas encore d'évaluation
- Diabetes Nursing FinalDocument15 pagesDiabetes Nursing FinalAna Marie Besa Battung-ZalunPas encore d'évaluation
- Diabetis MellitusDocument25 pagesDiabetis Mellituscdamasco18Pas encore d'évaluation
- Research ProposalDocument21 pagesResearch Proposalapi-351044176Pas encore d'évaluation
- Wound Care Case Study: Managing Risks for Diabetic ClientDocument5 pagesWound Care Case Study: Managing Risks for Diabetic ClientJulia KennedyPas encore d'évaluation
- Gestational DiabetesDocument10 pagesGestational DiabetesGui NessPas encore d'évaluation
- Childhood Obesity Apa PaperDocument13 pagesChildhood Obesity Apa Paperapi-3018616020% (1)
- Diverse Culture in NursingDocument10 pagesDiverse Culture in NursingJacob Oduor100% (1)
- Psychotherapeutic Management in The Continuum of CareDocument23 pagesPsychotherapeutic Management in The Continuum of CareJohn Mark ParacadPas encore d'évaluation
- English Paper Final Research PaperDocument8 pagesEnglish Paper Final Research PaperBriana Vincent100% (1)
- Nursing AcronymsDocument17 pagesNursing AcronymsLysol007Pas encore d'évaluation
- Maternal NSG Sample QuestionsDocument29 pagesMaternal NSG Sample QuestionsLysol007Pas encore d'évaluation
- Peds Nursing ReferenceDocument6 pagesPeds Nursing ReferenceLysol007Pas encore d'évaluation
- Stroke DefinitionsDocument2 pagesStroke DefinitionsLysol007Pas encore d'évaluation
- APA FormatDocument4 pagesAPA FormatLysol007Pas encore d'évaluation
- Repositioning For The Treatment of Pressure UlcersDocument2 pagesRepositioning For The Treatment of Pressure UlcersLysol007Pas encore d'évaluation
- Elimination One PagerDocument2 pagesElimination One PagerLysol007Pas encore d'évaluation
- Stroke DefinitionsDocument2 pagesStroke DefinitionsLysol007Pas encore d'évaluation
- Rasagiline Trade Name: Azilect: ClassificationDocument3 pagesRasagiline Trade Name: Azilect: ClassificationLysol007Pas encore d'évaluation
- NandaDocument2 pagesNandaAnsu MaliyakalPas encore d'évaluation
- DiabetesDocument9 pagesDiabetesLysol007100% (1)
- Mudra Therapy For DiabetesDocument3 pagesMudra Therapy For DiabetesMeera MishraPas encore d'évaluation
- Diabetes Management GuideDocument20 pagesDiabetes Management GuideLeelanRamphalPas encore d'évaluation
- Type 2 Diabetes in Children and AdolescentsDocument16 pagesType 2 Diabetes in Children and AdolescentsCarlita Cari CclPas encore d'évaluation
- Diabetes RoadmapDocument8 pagesDiabetes Roadmapwuryan dewiPas encore d'évaluation
- Diabetes Mellitus Lesson PlanDocument6 pagesDiabetes Mellitus Lesson Planramzan aliPas encore d'évaluation
- CHN Two-Way Referral FormDocument2 pagesCHN Two-Way Referral FormCatherine PradoPas encore d'évaluation
- Diabetes Mellitus: Causes, Symptoms and TreatmentDocument34 pagesDiabetes Mellitus: Causes, Symptoms and TreatmentAru VermaPas encore d'évaluation
- Insulin Therapy: Prof. Khalifa AbdallahDocument33 pagesInsulin Therapy: Prof. Khalifa AbdallahAhmed Adel MostafaPas encore d'évaluation
- The Effect of Mangosteen (Garcinia Mangostana) Rind in The Blood Glucose Levels of Adult Patients With Type 2 Diabetes MellitusDocument4 pagesThe Effect of Mangosteen (Garcinia Mangostana) Rind in The Blood Glucose Levels of Adult Patients With Type 2 Diabetes MellitusFiqoh Puteri FauziPas encore d'évaluation
- Gestational Diabetes 97-03Document9 pagesGestational Diabetes 97-03jaenarosePas encore d'évaluation
- Mod Diabetes FinalDocument132 pagesMod Diabetes FinalOana MariaPas encore d'évaluation
- Medical Clinics of North America Volume 101 Issue 3 2017 (Doi 10.1016 - J.mcna.2016.12.011) Fayfman, Maya Pasquel, Francisco J. Umpierrez, Guillermo E. - Management of Hyperglycemic CrisesDocument20 pagesMedical Clinics of North America Volume 101 Issue 3 2017 (Doi 10.1016 - J.mcna.2016.12.011) Fayfman, Maya Pasquel, Francisco J. Umpierrez, Guillermo E. - Management of Hyperglycemic CrisesBlanca Herrera MoralesPas encore d'évaluation
- Types of Insulin: NOTE: Exact Onset, Action, and Duration Are Dependent On The Generic/brand UsedDocument3 pagesTypes of Insulin: NOTE: Exact Onset, Action, and Duration Are Dependent On The Generic/brand Usedask1400Pas encore d'évaluation
- Oral Hypoglycemic Drugs Classification and ManagementDocument26 pagesOral Hypoglycemic Drugs Classification and ManagementBansal Mohit100% (1)
- Download ebook Endocrine Secrets Pdf full chapter pdfDocument67 pagesDownload ebook Endocrine Secrets Pdf full chapter pdfjason.green261100% (23)
- Type 1 Diabetes OutlineDocument2 pagesType 1 Diabetes OutlineDominique PorterPas encore d'évaluation
- 01 Serpentina Presentation PDFDocument27 pages01 Serpentina Presentation PDFabcPas encore d'évaluation
- Activity No. 2Document3 pagesActivity No. 2Shaira Dawn D. PLANCOPas encore d'évaluation
- Epidemiology of Diabetes MellitusDocument72 pagesEpidemiology of Diabetes MellitusAnonymous RRkF0x67% (3)
- 1st Adime - HWDocument3 pages1st Adime - HWapi-243208495Pas encore d'évaluation
- JDRF School Advisory ToolkitDocument92 pagesJDRF School Advisory ToolkitLynne WilsonPas encore d'évaluation
- Case Scenario 10Document1 pageCase Scenario 10Mart Juaresa YambaoPas encore d'évaluation
- Pathophysiology: Predisposing Factors: Precipitating FactorsDocument2 pagesPathophysiology: Predisposing Factors: Precipitating FactorsJemsMei Comparativo MensuradoPas encore d'évaluation
- Meglitinide Works by Stimulating The Release of Insulin in The Presence of GlucoseDocument53 pagesMeglitinide Works by Stimulating The Release of Insulin in The Presence of GlucoseWil LesterPas encore d'évaluation
- A Step by Step Guide To Using Your Lantus Solostar PENDocument7 pagesA Step by Step Guide To Using Your Lantus Solostar PENGita Kusumadiani HaryonoPas encore d'évaluation
- Glycemic Management in The Operating RoomDocument13 pagesGlycemic Management in The Operating Room凌晓敏Pas encore d'évaluation
- Glucose Tolerance TestDocument27 pagesGlucose Tolerance Testsiya sharmaPas encore d'évaluation
- Vol 27 No 1 April 2014 Medicinus 1Document68 pagesVol 27 No 1 April 2014 Medicinus 1Natasya DelarespitaPas encore d'évaluation
- Presented By-Kamini SinghDocument52 pagesPresented By-Kamini SinghSupriyati RahayuPas encore d'évaluation
- DM Diabetic Ketoacidosis DKA Management Algorithm Adult Patients 2019Document1 pageDM Diabetic Ketoacidosis DKA Management Algorithm Adult Patients 2019Hendra AfrilaPas encore d'évaluation
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionD'EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionÉvaluation : 4 sur 5 étoiles4/5 (402)
- Why We Die: The New Science of Aging and the Quest for ImmortalityD'EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityÉvaluation : 3.5 sur 5 étoiles3.5/5 (2)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisD'EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisÉvaluation : 4 sur 5 étoiles4/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedD'EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedÉvaluation : 5 sur 5 étoiles5/5 (78)
- The Age of Magical Overthinking: Notes on Modern IrrationalityD'EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityÉvaluation : 4 sur 5 étoiles4/5 (13)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeD'EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BePas encore d'évaluation
- The Comfort of Crows: A Backyard YearD'EverandThe Comfort of Crows: A Backyard YearÉvaluation : 4.5 sur 5 étoiles4.5/5 (23)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsD'EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsÉvaluation : 3.5 sur 5 étoiles3.5/5 (3)
- Techniques Exercises And Tricks For Memory ImprovementD'EverandTechniques Exercises And Tricks For Memory ImprovementÉvaluation : 4.5 sur 5 étoiles4.5/5 (40)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsD'EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsÉvaluation : 5 sur 5 étoiles5/5 (1)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsD'EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsÉvaluation : 4.5 sur 5 étoiles4.5/5 (169)
- The Obesity Code: Unlocking the Secrets of Weight LossD'EverandThe Obesity Code: Unlocking the Secrets of Weight LossÉvaluation : 5 sur 5 étoiles5/5 (4)
- The Ultimate Guide To Memory Improvement TechniquesD'EverandThe Ultimate Guide To Memory Improvement TechniquesÉvaluation : 5 sur 5 étoiles5/5 (34)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingD'EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingÉvaluation : 5 sur 5 étoiles5/5 (4)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaD'EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsD'EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsPas encore d'évaluation
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisD'EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisÉvaluation : 5 sur 5 étoiles5/5 (8)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingD'EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (33)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.D'EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Évaluation : 4.5 sur 5 étoiles4.5/5 (110)
- Summary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisD'EverandSummary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisÉvaluation : 5 sur 5 étoiles5/5 (3)
- The Happiness Trap: How to Stop Struggling and Start LivingD'EverandThe Happiness Trap: How to Stop Struggling and Start LivingÉvaluation : 4 sur 5 étoiles4/5 (1)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeD'EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeÉvaluation : 4.5 sur 5 étoiles4.5/5 (253)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsD'EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsPas encore d'évaluation
- The Tennis Partner: A Doctor's Story of Friendship and LossD'EverandThe Tennis Partner: A Doctor's Story of Friendship and LossÉvaluation : 4.5 sur 5 étoiles4.5/5 (4)