Académique Documents
Professionnel Documents
Culture Documents
Medication Cards
Transféré par
Movaliya GhanshyamCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Medication Cards
Transféré par
Movaliya GhanshyamDroits d'auteur :
Formats disponibles
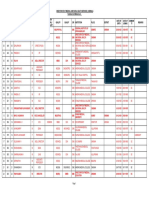
Pharmacology Drug Cards 1
Adenosine
Pharmacology Drug Cards 1
Name(s):
Class:
Actions/Uses:
Indications:
Contraindications:
Precautions:
Interactions:
Side Effects:
Routes/Dosage:
Onset/Duration:
Adenosine
Adenocard
Antidysrhythmic
A naturally occurring agent that can chemically convert PSVT to a
NSR. It has a half-life of 10 seconds and does not cause hypotension.
Narrow-complex PSVT refractory to vagal maneuvers
Hypersensitivity, 2nd and 3rd-degree heart blocks, sinus node disease, or
asthma
May cause transient dysrhythmias, COPD
Smoking : increased tachycardia ; Methylzanthines antagonize adenosine
(caffeine, theophylline); Carbamazepine may potentiate the AV nodal
blocking effect of adenosine.
Facial flushing, headache, SOB, dizziness, nausea
6 mg rapidly (1-2 sec) IV, then flush line with 20 mg NS. If ineffective,
12 mg in 1-2 min, may be repeated once. Ped: 0,1 mg/kg (1-2 sec) IV
followed by rapid NS flush, then 0.2 mg/kg in 1-2 min to max of 12 mg.
Onset: immediate; Duration: 10 seconds
Pharmacology Drug Cards 1
Albuterol
Pharmacology Drug Cards 1
Name(s):
Class:
Actions/Uses:
Indications:
Contraindications:
Precautions:
Interactions:
Side Effects:
Routes/Dosage:
Onset/Duration:
Albuterol
Proventil, Ventolin
2 sympathetic agonist, Sympathomimetic bronchodilator
A synthetic sympathomimetic that causes bronchodilation with less
cardiac effect than epinephrine and reduces mucus secretion, pulmonary
capillary leaking, and edema in the lungs during allergic reactions.
Bronchospasm and asthma in COPD
Hypersensitivity to the drug
Patient may experience tachycardia, anxiety, nausea, cough, wheezing,
and/or dizziness. Vital signs and breath sounds must be monitored; use
caution with elderly, cardiac, or hypertensive patients
Sympathomimetic may exacerbat adverse cardiovascular effects;
Antidepressants may potentiate vasodilation; beta-blockers may
antagonize alruterol; may potentiate diuretic-induced hypokalemia.
Palpations, anxiety, headache, dizziness, sweating
2 inhalations (90 mcg) via metered-dose inhaler (2 sprays) or 2.5 mg in
2-3 mL NS via nebulizer, repeat PRN. Ped: 0.15 mg/kg in 2-3 mL NS
via nebulizer, repeat PRN.
Onset: 5-15 min after inhalation; Duration 3-4 hours
Pharmacology Drug Cards 1
Amiodarone
Pharmacology Drug Cards 1
Name(s):
Class:
Actions/Uses:
Indications:
Contraindications:
Precautions:
Interactions:
Side Effects:
Routes/Dosage:
Onset/Duration:
Amiodarone
Cordarone, Pacerone
Antidysrhythmic
Prolons the duration of the action potential and refractory period and relaxes
smooth muscles, reducing peripheral vascular resistance and increasing coronary
blood flow.
Life-threatening ventricular and supraventricular dysrhythmias, frequently A-Fib
Hypersensitivity, cardiogenic shock, sever sinus bradycardia, or advanced heart
block
Hepatic impairment, pregnancy, nursing mothers, children
Bradycardia: beta blockers, calcium channel blockers; Increased anticoagulant
effects of warfarin; Increased levels of digoxin, quinidine, procainimide,
disopyramide, theophylline, phenytoin
Hypotension, nausea, anorexia, malaise, fatigue, tremors, pulmonary toxicity,
vetricular ectopic beats
150-300 mg IV over 10 min, then 1 mg/min over next 6 hours. Ped: 5 mg/kg
IV/IO, then 15 mg/kg/day
Onset: unknown; Duration: variable
Pharmacology Drug Cards 1
Aspirin
Pharmacology Drug Cards 1
Name(s):
Class:
Actions/Uses:
Indications:
Contraindications:
Precautions:
Interactions:
Side Effects:
Routes/Dosage:
Onset/Duration:
Bayer, Empirin, Alka-Seltzer
Aspirin (acetylsalicylic acid)
Analgesic, antipyretic, platelet inhibitor, anti-inflammatory,
NSAID
Inhibits the agents that cause the production of inflammation,
pain, and fever. It relieves mild to moderate pain by acting on the
peripheral nervous system, lowers body temperature in fever, and
powerfully inhibits platelet aggregation
Chest pain suggestive of an MI
Hypersensitivity to salicylates, active ulcer disease, asthma
Allergies to other NSAIDs, bleeding disorders, children or
teenagers with varicella or influenza-like symptoms.
Decreased effects with antacids and steroids; Increased effects
with anticoagulants, insulin, oral hypoglycemics, thrombolytic
agents, NSAIDs
Heartburn, nausea, vomiting, wheezing
260-325 mg PO (chewable) (4 x 81 mg chewable)
Onset: 15-30 min; Duration: 4-6 hours
Pharmacology Drug Cards 1
Atropine Sulfate
Pharmacology Drug Cards 1
Name(s):
Class:
Actions/Uses:
Indications:
Contraindications:
Precautions:
Interactions:
Side Effects:
Routes/Dosage:
Onset/Duration:
Atropine Sulfate
Parasympatholytic
Blocks the parasympathetic nervous system, specifically the vagal effects on heart
rate. It does not increase contractility but may increase myocardial oxygen
demand. Decreases airway secretions.
Hemodynamically significant bradycardia, brady asystolic arrest, and
organophosphate poisoning
None in the emergency setting
AMI, glaucoma
Use with other anticholinergic agents may increase vagal blockade, potential
adverse effects when used with digitalis, cholinergics, effects may be enhanced by
antihistamines, procainimide, quinadine, antipsychotics, antidepressants and
thiazides
Palpations, tachycardia, headache, dizziness, dry mouth, pupilary dilation, blurred
vision, urinary retention (especially in older men)
Symptomatic bradycardia: 0.5-1 mg IV (2 mg ET) q 3-5 min to 0.04 mg/kg.
Ped: 0.02 mg/kg IV (0,04 mg/kg ET) q 5 min to max 1 mg. Asystole: 1 mg IV (2
mg ET), q 3-5 min up to 0.04 mg/kg. Organophosphate poisoning: 2-5 mg
IV/IM/IO over 10-15 min; Inhalation: 0.5-1.0 mg in 2-3 mL NSS
Onset: rapid; Duration: 2-3 hours
Pharmacology Drug Cards 1
Ca l c i u m C h l o ri d e
Pharmacology Drug Cards 1
Name(s):
Class:
Actions/Uses:
Indications:
Contraindications:
Precautions:
Interactions:
Side Effects:
Routes/Dosage:
Onset/Duration:
Calcium Chloride
Electrolyte
Increases myocardial contractile force and increases ventricular
automaticity
Hyperkalemia, hypocalcemia, hypermagnesemia, and calcium channel
blocker toxicity
V-Fib, hypercalcemia, and possible digitalis toxicity
May precipitate toxicity in patients taking digoxin. Ensure the IV line is
in a large vein and flushed before and after using calcium. May
precipitate with sodium bicarbonate.
Calcium may worsen dysrhythmias secondary to digitalis; May
antagonize the peripheral vasodilatory effect of calcium channel blockers
Arrhythmias (bradycardia and asystole), hypotension
2-4 mg/kg IV (10% solution) over 10 min, repeat PRN. Ped: 20 mg/kg
IV (10% solution) over 10 min, repeat PRN; SLOW PUSH ONLY
Onset: 5-15 min; Duration: dose dependant, may persist for up to 4 hours
Pharmacology Drug Cards 1
Dexamethasone
Pharmacology Drug Cards 1
Name(s):
Class:
Actions/Uses:
Indications:
Contraindications:
Dexamethasone
Decadron
Steroid
Long-acting synthetic adrenocorticoid with intense anti-inflammatory activity. It
prevents the accumulation of inflammatory generating cells at the sites of
infection or injury.
Anaphylaxis, asthma, COPD, spinal cord edema
No absolute contraindications in the emergency setting. Relative: systemic fungal
infections, acute infections, tuberculosis, varicella, or vaccinia or live virus
vaccinations.
Precautions:
Herpes simplex, keratitis, myasthenia gravis, hepatic or renal impairment, diabetes, CHF,
seizures, physic disorders, hypothyroidism, and GI ulceration.
Interactions:
Insulinmay increase blood glucose (sugar) levels; Digitalis glycosides (heart
medicine) decrease the amount of potassium in the blood. Digitalis can increase
the risk of having an irregular heartbeat or other problems if the amount of
potassium in the blood gets too low; Sodium-containing medicinecause the
body to retain (keep) more sodium (salt) and water. Too much sodium may cause
high blood sodium, high blood pressure, and excess body water
GI bleeding, prolonged wound healing
4-24 mg IV/IM. Ped: 0.5-1 mg/kg
Side Effects:
Routes/Dosage:
Onset/Duration:
Pharmacology Drug Cards 1
Di a z e p a m
Pharmacology Drug Cards 1
Name(s):
Class:
Actions/Uses:
Indications:
Contraindications:
Diazepam
Valium
Hypnotic, anticonvulsant, sedative
A benzodiazepine sedative and skeletal muscle relaxant that reduces tremors, induces
amnesia, and reduces the incidence and recurrence of seizures. It relaxes muscle
spasms in orthopedic injuries and produces amnesia for painful procedures
(cardioversion).
Major motor seizures, status epilepticus, premedication for cardioversion, muscle
tremors due to injury, and acute anxiety
Hypersensitivity, shock, coma, acute alcoholism, depressed vital signs, obstetrical
patients, neonates
Precautions:
Interactions:
Psychoses, depression, myasthenia gravis, hepatic or renal impairment, addiction, elderly or very ill patients, or
COPD. Due to short half-life of the drug, seizures may recur.
Cigarette smoking may decrease the effectiveness of this drug. antihistamines; cimetadine; digoxin; disulfiram;
fluoxetine (Prozac); levodopa (Larodopa, Sinemet); medications for depression, seizures, pain, Parkinson's
disease, asthma, colds, or allergies; muscle relaxants; oral contraceptives; propoxyphene (Darvon); propranolol;
ranitidine; sedatives; sleeping pills; theophylline (Theo-Dur); tranquilizers; valproic acid (Depakene); and
vitamins. These medications may add to the drowsiness caused by diazepam.
Side Effects:
Routes/Dosage:
Drowsiness, hypotension, respiratory depression and apnea
Seizures: 5-10 mg IV/IM. Ped : 0.5-2 mg IV/IM. Acute anxiety: 2-5 mg IV/IM. Ped:
0.5-2 mg IM. Premedication: 5-15 mg IV. Ped: 0.2-0.5 mg/kg IV
Onset/Duration:
Pharmacology Drug Cards 1
Di l t i a z e m
Pharmacology Drug Cards 1
Name(s):
Class:
Actions/Uses:
Indications:
Contraindications:
Precautions:
Interactions:
Side Effects:
Routes/Dosage:
Onset/Duration:
1
Diltiazem
Cardizem
Calcium Channel Blocker
Slow calcium channel blocker similar to verapamil. It dilates coronary and
peripheral arteries and arterioles, thus increasing circulation to the heart and
reducing peripheral vascular resistance.
Supraventricular tachydysrhythmias (A-Fib, A-Flutter, and PSVT refractory to
adenosine) and to increase coronary artery perfusion in angina.
Hypersensitivity, sick sinus syndrome, 2nd or 3rd degree heart block, systolic BP <
90, diastolic BP < 60, wide-complex tachycardia and WPW1
CHF (especially with beta-blockers), conduction abnormalities, renal or hepatic
failure, the elderly, and nursing mothers.
Incompatible with simultaneous furosemide injection; Increased effects of
diltazem with cimetidine (Tagamet); Caution with patients receiving medications
that effect cardiac contractility and/or SA/AV node conduction.
Nausea, vomiting, hypotension, dizziness
0.25 mg/kg IV over 2 min, repeat PRN with 0.35 mg/kg followed by drip of 5-10
mg/hr, max 15 mg/hr over 24 hours
Onset: 2-5 min; Duration: 1-3 hours
Wolff-Parkinson-White syndrome: a disorder of atrioventricular conduction. It s marked by 2 atrioventricular conduction pathways.
Pharmacology Drug Cards 1
Pharmacology Drug Cards 1
Diphenhydramine
Pharmacology Drug Cards 1
Name(s):
Class:
Actions/Uses:
Indications:
Contraindications:
Precautions:
Interactions:
Side Effects:
Routes/Dosage:
Onset/Duration:
Benadryl
Diphenhydramine
Antihistamine
Blocks histamine release, thereby reducing bronchoconstriction,
vasodilation, and edema
Anaphylaxis, allergic reactions, and dystonic reactions
Asthma and other lower respiratory diseases
May induce hypotension, headache, palpitations, tachycardia,
sedation, drowsiness, and/or disturbed coordination
Monoamine oxidase (MAO) inhibitor ---these medicines
should not be used together. Anticholinergics (medicine for
abdominal or stomach spasms or cramps)Side effects,
such as dryness of mouth, of antihistamines or
anticholinergics may be more likely to occur.
Sedation, dries bronchial secretions, blurred vision, headache,
palpations
25-50 mg IV/IM
Pharmacology Drug Cards 1
Dopamine
Pharmacology Drug Cards 1
Name(s):
Class:
Actions/Uses:
Indications:
Contraindications:
Precautions:
Interactions:
Side Effects:
Routes/Dosage:
Onset/Duration:
2
Dopamine
Intropin
Sympathomimetic
A naturally occurring catecholamine that increases cardiac output without
appreciably increasing myocardial oxygen consumption. It maintains renal and
mesenteric blood flow while inducing vasoconstriction and increasing systolic
blood pressure.
Nonhypovolemic hypotension (70-100 mmHg) and cardiogenic shock
Hypovolemic hypotension without aggressive fluid resuscitation,
tachydysrhythmias, V-Fib, and pheochormocytoma2.
Occular vascular disease, cold injury, arterial embolism. Assure adequate fluid
resuscitation of the Hypovolemic patient.
Deactivated by alkaline solutions; MAOIs may potentiate the effects of
catecholamines; Beta adrenergic antagonists may blunt the inotropic response;
Sympathomimetics may exacerbate dysrhythmia response
Ventricular tachydysrhythmias, HTN, palpitations
2-5 mcg/kg/min up to 20 mcg/kg/min, titrated to effect. Ped: same as adult
Onset: 2-4 min; Duration: 10-15 min
A tumor of the adrenal gland that causes the release of too much epinephrine and norepinephrine.
Pharmacology Drug Cards 1
Epinephrine 1:1000
Pharmacology Drug Cards 1
Name(s):
Class:
Actions/Uses:
Indications:
Contraindications:
Precautions:
Interactions:
Side Effects:
Routes/Dosage:
Onset/Duration:
Epinephrine 1:1000
Adrenalin
Sympathomimetic
A naturally occurring catecholamine that increases heart rate, cardiac contractile force,
myocardial electrical activity, vascular resistance, and systolic BP, and decreases
overall airway resistance and automaticity. It also, through bronchial artery
constriction, may reduce pulmonary congestion and increases tidal volume and vital
capacity.
Bronchial asthma, exacerbation of CODP, allergic reactions pediatric cardiac arrest
Patients with underlying cardiovascular disease, HTN, pregnancy, patients with
tachyarrhythmias
Should be protected from light, BP, pulse and ECG results must be constantly
monitored
MAOIs may potentiate the effect of epinephrine; beta adrenergic antagonists may blunt
inotropic effects; sympathomimetics may exacerbate dysrhythmias response; May be
deactivated by alkaline solutions
Palpations and tachycardia, anxiousness, headache, tremors
0.3-0.5 mg SC, repeat q 5-15 min PRN, or 0.5-1 mg of 1:10,000 IV if SC dose
ineffective or severe reaction. Ped: 0.01 mg/kg of 1:1,000 SC, repeat q 10-15 min or
0.01 mg/kg of 1:10,000 IV if SC dose ineffective or severe reaction.
Onset: IV/ET 1-2 min, SQ 5-10 min (1 :1000); Duration: 5-10 min
Pharmacology Drug Cards 1
Epinephrine 1:10 000
Pharmacology Drug Cards 1
Name(s):
Class:
Actions/Uses:
Indications:
Contraindications:
Precautions:
Interactions:
Side Effects:
Routes/Dosage:
Onset/Duration:
Epinephrine 1:10 000
Adrenalin
Sympathomimetic
A naturally occurring catecholamine that increases heart rate, cardiac contractile force,
myocardial electrical activity, vascular resistance, and systolic BP, and decreases
overall airway resistance and automaticity. It also, through bronchial artery
constriction, may reduce pulmonoary congestion and increases tidal volume and vital
capacity.
Cardiac arrest, anaphylactic shock, severe airway disease
For IV or endotracheal tube (ET) use; it should not be used in patients who do not
require extensive resuscitative efforts.
Elderly, debilitated patients, HTN, diabetes, hyperthyroidism, Parkinsons disease,
tuberculosis, asthma, emphysema, and in children < 6 years of age. Can be deactivated
by alkaline solutions.
MAOIs may potentiate the effect of epinephrine; beta adrenergic antagonists may blunt inotropic effects;
sympathomimetics may exacerbate dysrhythmia response; May be deactivated by alkaline solutions
Palpations and tachycardia, anxiousness, headache, tremors
Arrest: 1 mg of 1:10,000 IV, repeat q 3-5 min (ET: 2-2.5 mg 1:1,000) Ped: 0.01 mg/kg
1:10,000 IV/IO (ET: 0.1 mg/kg 1:1,000) all subsequent doses 0.1 mg/kg IV/IO. Severe
anaphylaxis: 0.3-0.5 mg (2-5 mL); occasionally an epinephrine drip is required
Onset: IV/ET 1-2 min, SQ 5-10 min (1 :1000); Duration: 5-10 min
Pharmacology Drug Cards 1
Furosemide
Pharmacology Drug Cards 1
Name(s):
Class:
Actions/Uses:
Indications:
Contraindications:
Precautions:
Interactions:
Side Effects:
Routes/Dosage:
Onset/Duration:
Furosemide
Lasix
Diuretic
Rapid-acting, potent diuretic and antihypertensive that inhibits sodium
reabsorption by the kidney. Its vasodilating effects reduce venous return and
cardiac workload.
CHF and pulmonary edema
Hypersensitivity to furosemide or the sulfonimides, fluid and electrolyte depletion
states, hepatic coma, pregnancy (except in life-threatening circumstances)
Infants, elderly, hepatic impairment, nephrotic syndrome, cardiogenic shock
associated with acute MI, gout, or patients receiving digitalis or potassiumdepleting steroids.
Digitalis toxicity; increased ototoxic potential of aminoglycoside antibiotics;
Lithium toxicity; May potentiate therapeutic effect of other antihypertensive
drugs; Should not be administered in same line as Inocor.
Few in emergency setting; Hypokalemia; Hypercalcemia
40-120 mg slow IV. Ped: 1 mg/kg slow IV.
Onset: IV 15-20 min; Duration: 2 hours
Pharmacology Drug Cards 1
Glucagon
Pharmacology Drug Cards 1
Name(s):
Class:
Actions/Uses:
Indications:
Contraindications:
Precautions:
Interactions:
Side Effects:
Routes/Dosage:
Onset/Duration:
Glucagon
GlucaGen
Hormone, antihypoglycemic
A protein secreted by the alpha pancreatic cells that causes a breakdown
of stored glycogen into glucose and inhibits the synthesis of glycogen
from glucose.
Hypoglycemia without IV access and to reverse beta-blocker overdose.
Hypersensitivity to glucagon or protein compounds.
Cardiovascular or renal impairment. Effective only if there are sufficient
stores of glycogen in the liver.
Few in the emergency settings
Hypoglycemia: 1 mg IM/SC repeat 5-20 min. Ped: 0.01 mg/kg
IM/SC/IV for child < 10 kg; 1 mg/kg IM/SC/IV for child > 10 kg. Betablocker overdose: 50-150 mg/kg IV over 1 min. Ped: 50-150 mg/kg IV
over 1 min.
Pharmacology Drug Cards 1
Lactated Ringers
Pharmacology Drug Cards 1
Name(s):
Class:
Actions/Uses:
Indications:
Contraindications:
Precautions:
Interactions:
Side Effects:
Routes/Dosage:
Onset/Duration:
Lactated Ringers
Hartmanns solution
Isotonic crystalloid solution
Isotonic solution containing the following: Sodium (Na+)
130 mEq/L, Potassium (K+) 4 mEq/L, Calcium (Ca2+) 3
mEq/L, Chloride (Cl-) 109 mEq/L, and 28 mEq/L of lactate
(lactic acid) as a buffer. Replaces water and electrolytes.
Hypovolemic shock, and TKO
Should not be used in patients with CHF or renal failure.
Watch for signs of circulatory overload.
Few in the emergency setting
Rare in therapeutic dosages.
IV infusion; Neccesary to replace at a 3:1 rate.
Onset: immediate; Duration: variable
Pharmacology Drug Cards 1
Li doc ai ne
Pharmacology Drug Cards 1
Name(s):
Class:
Actions/Uses:
Indications:
Contraindications:
Precautions:
Interactions:
Side Effects:
Routes/Dosage:
Onset/Duration:
Lidocaine
Xylocaine
Antidysrhythmic
Suppresses automaticity and raises stimulation threshold of the ventricles. Also
causes sedation, anticonvulsant, and analgesic effects.
Pulseless V-Tach, V-Fib, V-Tach (with pulse)
Hypersensitivity to amide-type local anesthetics, supraventricular tachydysrhythmias, Stokes-Adams
syndrome, 2nd- and 3rd-degree heart blocks, and bradycardia.
Hepatic or renal impairment, CHF, hypoxia, respiratory depression, hypovolemia, myasthenia gravis, shock,
debilitated patients, elderly, family Hx of malignant hypothermia.
Metabolic clearance may be decreased in patients taking beta adrenergic blockers or in patients with
decreased cardiac output or liver impairment; Additive neurologic effects may occur with procainimide;
decreased effects of lidocaine with barbiturates.
Anxiety, drowsiness, confusion, nausea and vomiting, convulsions, widening of
QRS complex
Cardiac arrest: 1-1.5 mg.kg IV q 3-5 min up to 3 mg/kg, follow conversion with
drip of 2-4 mg/min. Ped: 1 mg/kg IV q 3-5 min up to 3 mg/kg, follow conversion
with drip of 20-50 mcg/kg/min. V-Tach (w/ pulse): 1-1.5 mg/kg slow IV. May
repeat at one-half dose q 5-10 min until conversion up to 3 mg/kg. Follow
conversion with infusion of 2-4 mg/min. Ped: 1 mg/kg, followed by a drip at 2050 mcg/kg/min.
Onset: 30-90 sec; Duration: 2-4 hours
Pharmacology Drug Cards 1
L o ra z e p a m
Pharmacology Drug Cards 1
Name(s):
Class:
Actions/Uses:
Indications:
Contraindications:
Precautions:
Interactions:
Side Effects:
Routes/Dosage:
Onset/Duration:
Ativan
Lorazepam
Benzodiazepine, sedative
The most potent benzodiazepine available. It has a strong
antianxiety, sedative, hypnotic, and skeletal muscle relaxant
properties, and a relatively short half-life.
Sedation for cardioversion and status epilepticus.
Sensitivity to benzodiazepines
Narrow angle glaucoma, depression or psychosis, coma, shock,
acute alcohol intoxication, renal or hepatic impairment, organic
brain syndrome, myasthenia gravis, GI disorders, elderly,
debilitated, limited pulmonary reserve.
Drowsiness, hypotension, respiratory depression and apnea
Sedation: 2-4 mg IM, 0.5-2 mg IV. Ped: 0.03-0.05 mg/kg
IV/IM/PR up to 5 mg. Status epilepticus: 2 mg slow IV/PR (2
mg/min). Ped: 0.1 mg/kg slow IV/PR (2-5 min).
Pharmacology Drug Cards 1
Magnesium Sulfate
Pharmacology Drug Cards 1
Name(s):
Class:
Actions/Uses:
Indications:
Contraindications:
Precautions:
Interactions:
Side Effects:
Routes/Dosage:
Onset/Duration:
Magnesium sulfate
Magnesium
Calcium channel blocker, Electrolyte
An electrolyte that acts as a calcium channel blocker, acting as a CNS depressant
and anticonvulsant. It also depresses the function of smooth, skeletal, and cardiac
muscles.
Refractory V-Fib, and pulseless V-Tach (especially Man), AMI, eclamptic
seizures.
Heart block, myocardial damage, shock, persistent HTN, and hypocalcemia.
Renal impairment, digitalized patients, other CNS depressants, or neuromuscular
blocking agents.
Serious changes in cardiac function may occur with cardiac glycosides; CNS
depressant effects may be enhanced if the patient is taking other CNS depressants.
Flushing, respiratory depression, drowsiness
V-Fib or V-Tach: 1-2 g IV over 2 min. (in 10 mL of NS) Torsade de Points: 1-2
g IV followed by infusion of 0.5-1.0 g/hr IV. AMI: 1-2 g IV over 5-30 min.
Eclampsia : 2-4 g IV/IM.
Onset: immediate; Duration: 30 min
Pharmacology Drug Cards 1
Methylprednisolone
Pharmacology Drug Cards 1
Name(s):
Class:
Actions/Uses:
Indications:
Contraindications:
Precautions:
Interactions:
Side Effects:
Routes/Dosage:
Onset/Duration:
Solu-Medrol
Methylprednisolone
Corticosteroid, Anti-inflammatory
Synthetic corticosteroid, effective as an anti-inflammatory and used in
the management of allergic reactions and in some cases of shock. It is
sometimes used in the treatment of spinal cord injury.
Spinal cord injury, asthma, severe anaphylaxis, COPD
No major contraindications in the emergency setting
Only a single dose should be given in the prehospital setting.
Hypoglycemic response to insulin & oral hypoglycemic agents may be
blunted; Potassium-depleting agents may potentiate hypokalemia
induced by corticosteroids.
GI Bleeding, prolonged wound healing, suppression of natural steroids
Asthma/COPD/Anaphylaxis: 125-250 mg IV/IM. Ped: 1-2 mg/kg/dose
IV/IM. Spinal cord injury: 30 mg/kg IV over 15 min, after 45 min an
infusion of 5.4 mg/kg/hr.
Onset: 1-2 hrs; Duration: 8-24 hrs
Pharmacology Drug Cards 1
Midazolam
Pharmacology Drug Cards 1
Name(s):
Class:
Actions/Uses:
Indications:
Contraindications:
Precautions:
Interactions:
Side Effects:
Routes/Dosage:
Onset/Duration:
Versed
Midazolam
Sedative
Short-acting benzodiazepine with CNS depressant, muscle
relaxant, anticonvulsant, and anteroretrograde amnesic effects.
To induce sedation before cardioversion or intubation.
Hypersensitivity to benzodiazepines, narrow angle glaucoma,
shock, coma, or acute alcohol intoxication.
COPD, renal impairment, CHF, elderly.
Drowsiness, hypotension, amnesia, respiratory depression and
apnea
1-2.5 mg slow IV; 0.07-0.08 mg/kg IM (usually 5 mg). Ped: 0.050.2 mg/kg IV; 0.1-0.15 mg/kg IM; 3 mg intranasal..
Pharmacology Drug Cards 1
Morphine Sulfate
Pharmacology Drug Cards 1
Name(s):
Class:
Actions/Uses:
Indications:
Contraindications:
Precautions:
Interactions:
Side Effects:
Routes/Dosage:
Onset/Duration:
Morphine Sulfate
Morphine
Narcotic Analgesic Schedule II
Potent analgesic and sedative that causes some vasodilation, reducing venous
return, and reduced myocardial demand.
Moderate to severe pain and in MI and to reduce venous return in pulmonary
edema
Hypersensitivity to opiates, undiagnosed head or abdominal injury, hypotension,
or volume depletion, acute bronchial asthma, COPD, severe respiratory
depression, or pulmonary edema due to chemical inhalation.
Elderly, children, or debilitated patients.Naloxone should be readily available to
counteract the effects of morphine.
CNS depressants may potentiate effects of morphone; Phenothiazine may
potentiate analgesia; MAOIs may cause paradoxical excitation.
Dizziness, altered level of consciousness
Pain: 2.5-15 mg IV; 5-20 mg IM/SC. Ped: 0.05-0.1 mg/kg IV; 0.1-0.2 mg/kg
IM/SC. AMI or Pulmonary edema (PE): 1-2 mg, 6-10 min to response.
Onset: 1-2 min; Duration: 2-7 hours
Pharmacology Drug Cards 1
Na l o x o n e
Pharmacology Drug Cards 1
Name(s):
Class:
Actions/Uses:
Indications:
Contraindications:
Precautions:
Interactions:
Side Effects:
Routes/Dosage:
Onset/Duration:
Narcan
Naloxone
Narcotic antagonist
Pure narcotic antagonist that blocs the effects of both natural and
synthetic narcotics and may reverse respiratory depression.
Narcotic and synthetic narcotic overdose, coma of unknown
origin.
Hypersensitivity. Non-narcotic respiratory depression.
Possible dependency (including newborns). It also has a half-life
that is shorter than most narcotics; hence, the patient may return
to the overdose state.
Rare
0.4-2 mg IV/IM (2-2.5 for ET dose), repeated q 2-3 min PRN up
to 10 mg. Ped: 0.01 mg IV/IM (2-2.5 for ET dose), repeated q 2-3
min PRN up to 10 mg.
Pharmacology Drug Cards 1
Pharmacology Drug Cards 1
Ni t ro g l y c e r i n
Pharmacology Drug Cards 1
Name(s):
Class:
Actions/Uses:
Indications:
Contraindications:
Precautions:
Interactions:
Side Effects:
Routes/Dosage:
Onset/Duration:
Nitroglycerin
Nitrostat
Nitrate
A rapid smooth muscle relaxant that reduces peripheral vascular
resistance, BP, venous return, and cardiac workload.
Chest pain associated with angina and acute myocardial infarction, and
acute pulmonary edema.
Hypersensitivity, tolerance to nitrates, severe anemia, head trauma,
hypotension, increased ICP, patients taking sildenafil, glaucoma, and
shock, under 12 years old
May induce headache that is sometimes severe. NTG is light sensitive
and will lose potency when exposed to air.
Other vasodilators may have additive hypotensive effects; May cause
severe hypotension when administered to patients who have recently
ingested alcohol.
Headache, dizziness, hypotension
1 tablet (0.4 mg) SL. May be repeated q 3-5 min up to 3 tablets, or 0.4
mg (1 spray) SL up to 3 sprays in 25 minutes.
Onset: 1-2 min; Duration: 30-60 min
Pharmacology Drug Cards 1
Nitroglycerin Paste
Pharmacology Drug Cards 1
Name(s):
Class:
Actions/Uses:
Indications:
Contraindications:
Precautions:
Interactions:
Side Effects:
Routes/Dosage:
Onset/Duration:
Nitro-Bid
Nitroglycerin
Nitrate
A rapid smooth muscle relaxant that reduces peripheral vascular
resistance, BP, venous return, and cardiac workload.
Chest pain associated with angina and acute myocardial
infarction, and acute pulmonary edema.
Hypersensitivity, tolerance to nitrates, severe anemia, head
trauma, hypotension, increased ICP, patients taking sildenafil,
glaucoma, and shock, under 12 years old
May induce headache that is sometimes severe. NTG is light
sensitive and will lose potency when exposed to air.
Other vasodilators may have additive hypotensive effects
Headache, dizziness, hypotension
to 1 inch of topical ointment
Onset: 15-60 min; Duration: 2-12 hours
Pharmacology Drug Cards 1
Normal Saline (0.9%)
Pharmacology Drug Cards 1
Name(s):
Class:
Actions/Uses:
Indications:
Contraindications:
Precautions:
Interactions:
Side Effects:
Routes/Dosage:
Onset/Duration:
Normal Saline (0.9%)
Normal Saline
Isotonic crystalloid
Normal Saline contains 154 mEq/L of sodium (Na+) and
approximately 154 mEq/L of chloride (Cl-) ions. Because this
concentration of sodium is close to that of blood, it is considered
isotonic. Normal saline replaces water and electrolytes.
Heat-related problems (Heat stroke, heat exhaustion), freshwater
drowning, hypovolemia, KVO, and diabetic ketoacidosis
CHF, because circulatory overload can be induced
Normal saline only contains Na and chloride. When large
amounts of NS are administered, it is possible to deplete other
physiologic electrolytes. In cases where large amounts of fluids
have been administered, consider Lactated Ringers
Few in the emergency setting
Rare in therapeutic dosages.
Treatment specific; 20 mL/kg
Onset: immediate; Duration: variable
Pharmacology Drug Cards 1
Oxygen
Pharmacology Drug Cards 1
Name(s):
Class:
Actions/Uses:
Oxygen
Oxidizing agent (gas)
An odorless, colorless, tasteless gas, essential for life.
It is one of the most important emergency drugs.
Indications:
Hypoxia or anticipated hypoxia, or in any medical or
trauma patient to improve respiratory efficiency.
Contraindications: There are no contraindications to oxygen therapy.
Precautions:
COPD and very prolonged administration of high
concentrations in the newborn.
Interactions:
None in prehospital setting
Side Effects:
Drying of mucous membranes
Routes/Dosage:
Hypoxia: 100% by inhalation or IPPV.
Onset/Duration:
Onset: immediate; Duration: based on metabolic rate
Pharmacology Drug Cards 1
Sodium Bicarbonate
Pharmacology Drug Cards 1
Name(s):
Class:
Actions/Uses:
Indications:
Contraindications:
Precautions:
Interactions:
Side Effects:
Routes/Dosage:
Onset/Duration:
Sodium Bicarbonate
Alkalizing Agent
NaHCO3
Provides vascular bicarbonate to assist the buffer system in reducing the
effects of metabolic acidosis and in the treatment of some overdoses.
Tricyclic antidepressant and barbiturate overdose, refractory acidosis, or
hyperkalemia.
None when used in sever hypoxia or late cardiac arrest.
May cause alkalosis if given in too large a quantity. It may also
deactivate vasopressor and may precipitate with calcium chloride.
May precipitate in calcium solutions, vasopressor may be deactivated,
alkalinization of urine may shorten elimination half-lives of certain
drugs; USE ABG WHEN POSSIBLE
Alkalosis, may worsen CHF, MAINTAIN ADEQUATE
VENTILATIONS
1mEq/kg IV, then 0.5 mEq/kg/10 min. Ped: same as adult (may be given
IO).
Onset: 2-10 min; Duration: 30-60 min
Pharmacology Drug Cards 1
Pharmacology Drug Cards 1
T e rb u t a l i n e
Pharmacology Drug Cards 1
Name(s):
Class:
Actions/Uses:
Indications:
Contraindications:
Precautions:
Interactions:
Side Effects:
Routes/Dosage:
Onset/Duration:
Terbutaline
Brethine, Bricanyl
Sympathetic Agonist
Causes bronchodilation with less cardiac effect than epinephrine.
Bronchial asthma and bronchospasm in COPD
Hypersensitivity to the drug.
Patient may experience palpitations, anxiety, nausea, and/or
dizziness. Vital signs and breath sounds must be monitored; use
caution with cardiac or HTN patients.
Increased effects with other sympathomimetics; decreased action
with beta-blockers; hypertensive crisis with MAOIs.
Palpations, tachycardia, PVCs, anxiety, tremors, headache
2 inhalations with a metered-dose inhaler, repeated once in 1 min
or 0.25 mg SQ repeated in 15-30 min.
Onset: SQ 15 min, Inh 5-30 min; Duration: SQ 1.5-4 hrs, Inh 3-6
hrs
Pharmacology Drug Cards 1
Thiamine
Pharmacology Drug Cards 1
Name(s):
Class:
Actions/Uses:
Thiamine
Vitamin B1
Vitamin
Thiamine is required to convert glucose into energy. It
is not manufactured in the body and must be
constantly provided from ingested foods or
supplements.
Indications:
Coma of unknown origin, chronic alcoholism with
associated coma, and delirium tremens.
Contraindications: None
Precautions:
Known hypersensitivity to the drug
Interactions:
Side Effects:
Routes/Dosage:
Onset/Duration:
Rare, if any
50-100 mg IV/IM. Ped: 10-25 mg IV/IM.
Pharmacology Drug Cards 1
Vasopressin
Pharmacology Drug Cards 1
Name(s):
Class:
Actions/Uses:
Indications:
Contraindications:
Precautions:
Interactions:
Side Effects:
Routes/Dosage:
Onset/Duration:
Pitressin
Vasopressin
Hormone, Vasopressor
Hormone with a strong vasopressive and antidiruretic properties
but that may precipitate angina and/or AMI.
To increase peripheral vascular resistance in arrest (CPR) or to
control bleeding from esophageal varices.
Chronic nephritis with nitrogen retention, ischemic heart disease,
PVCs, advanced arteriosclerosis, or 1st stage of labor.
Epilepsy, migraine, heart failure, angina, vascular disease,
hepatic impairment, elderly, and children.
Arrest: 40 units IV. Esophageal varicies: 0.2-0.4 units/min IV
drip.
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Individual CounselingDocument7 pagesIndividual CounselingCarla Dela CruzPas encore d'évaluation
- 2022 Arihant Political Science MCQs Term-1 Sample PapersDocument192 pages2022 Arihant Political Science MCQs Term-1 Sample PapersImran Arshad100% (4)
- Chevron Phillips Chemical Company Issued Sales SpecificationDocument1 pageChevron Phillips Chemical Company Issued Sales SpecificationSarmiento HerminioPas encore d'évaluation
- AnsdDocument12 pagesAnsdAlok PandeyPas encore d'évaluation
- Amy L. Lansky - Impossible Cure - The Promise of HomeopathyDocument295 pagesAmy L. Lansky - Impossible Cure - The Promise of Homeopathybjjman88% (17)
- Playlist AssignmentDocument7 pagesPlaylist AssignmentTimothy Matthew JohnstonePas encore d'évaluation
- Neurophysiological Effects of Spinal ManipulationDocument15 pagesNeurophysiological Effects of Spinal ManipulationBojan AnticPas encore d'évaluation
- H. Pylori IgA ELISA Package InsertDocument2 pagesH. Pylori IgA ELISA Package Inserttalha saleemPas encore d'évaluation
- Material Safety Data Sheet: 1 Identification of SubstanceDocument5 pagesMaterial Safety Data Sheet: 1 Identification of SubstanceRey AgustinPas encore d'évaluation
- Urgensi Kepemimpinan Transformasional Dan Kecerdasan Emosional Pada Perusahaan Dalam Merespons Pandemi Covid-19Document11 pagesUrgensi Kepemimpinan Transformasional Dan Kecerdasan Emosional Pada Perusahaan Dalam Merespons Pandemi Covid-19Inspektorat KubarPas encore d'évaluation
- NBR Leaflet Krynac 4955vp Ultrahigh 150dpiwebDocument2 pagesNBR Leaflet Krynac 4955vp Ultrahigh 150dpiwebSikanderPas encore d'évaluation
- Bakery Business PlanDocument31 pagesBakery Business PlanRohit Gupta93% (14)
- Kinds of Blood. Differences Between Men and WomenDocument11 pagesKinds of Blood. Differences Between Men and WomenTiagoSantosPas encore d'évaluation
- Basic Education For Autistic Children Using Interactive Video GamesDocument5 pagesBasic Education For Autistic Children Using Interactive Video GamesEwerton DuartePas encore d'évaluation
- WONCA2013 - Book of Abstracts PDFDocument830 pagesWONCA2013 - Book of Abstracts PDFBruno ZanchettaPas encore d'évaluation
- IELTS 1 Test IntroDocument1 pageIELTS 1 Test IntromichaelPas encore d'évaluation
- HIRARC - Hazard Identification Risk Assessment and Risk ControlDocument4 pagesHIRARC - Hazard Identification Risk Assessment and Risk ControlRohanPas encore d'évaluation
- AtelectasisDocument21 pagesAtelectasisshilpaPas encore d'évaluation
- Life-Long Learning Characteristics Self-Assessment: Behavioral IndicatorsDocument2 pagesLife-Long Learning Characteristics Self-Assessment: Behavioral Indicatorsapi-534534107Pas encore d'évaluation
- Vince Gironda 8x8 RoutineDocument10 pagesVince Gironda 8x8 RoutineCLAVDIVS0% (2)
- Valsalyacare Withprocuts....Document7 pagesValsalyacare Withprocuts....saumya.bsphcl.prosixPas encore d'évaluation
- VPPPA Designing For Construction Safety FINALDocument27 pagesVPPPA Designing For Construction Safety FINALKrischaEverPas encore d'évaluation
- Rule On Adoption AM NO. 02-6-02-SCDocument16 pagesRule On Adoption AM NO. 02-6-02-SCAnathea Cadagat100% (1)
- EDC Annual ReportDocument433 pagesEDC Annual ReportAngela CanaresPas encore d'évaluation
- Absorption, Distribution, Metabolism, Excretion and Mechanisms of Action of AflatoxinsDocument3 pagesAbsorption, Distribution, Metabolism, Excretion and Mechanisms of Action of AflatoxinsMaya Innaka ArhayuPas encore d'évaluation
- Model of Decision MakingDocument34 pagesModel of Decision MakingPalalikesjujubesPas encore d'évaluation
- Urbanization and HealthDocument2 pagesUrbanization and HealthsachiPas encore d'évaluation
- Behaviorism in Daily LifeDocument8 pagesBehaviorism in Daily LifeMichelleTongPas encore d'évaluation
- Part-IDocument507 pagesPart-INaan SivananthamPas encore d'évaluation
- VITA 1511 VITA 1511E Prothetikleitfaden BA en V01 Screen enDocument150 pagesVITA 1511 VITA 1511E Prothetikleitfaden BA en V01 Screen enAstri Ggamjong Xiao LuPas encore d'évaluation