Académique Documents
Professionnel Documents
Culture Documents
Maternal Cardiovascular and Hemodynamic Adaptations To Pregnancy
Transféré par
Anchalia ChandrakumaranTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Maternal Cardiovascular and Hemodynamic Adaptations To Pregnancy
Transféré par
Anchalia ChandrakumaranDroits d'auteur :
Formats disponibles
Maternal cardiovascular and hemodynamic adaptations to pregnancy
6/23/15, 4:52 AM
Official reprint from UpToDate
www.uptodate.com 2015 UpToDate
Maternal cardiovascular and hemodynamic adaptations to pregnancy
Author
Michael R Foley, MD
Section Editors
Charles J Lockwood, MD, MHCM
Bernard J Gersh, MB, ChB, DPhil,
FRCP, MACC
Deputy Editor
Kristen Eckler, MD, FACOG
All topics are updated as new evidence becomes available and our peer review process is complete.
Literature review current through: May 2015. | This topic last updated: Sep 09, 2014.
INTRODUCTION The major hemodynamic changes induced by pregnancy include an increase in cardiac output,
sodium and water retention leading to blood volume expansion, and reductions in systemic vascular resistance and
systemic blood pressure. These changes begin early in pregnancy [1], reach their peak during the second trimester, and
then remain relatively constant until delivery (figure 1). They contribute to optimal growth and development of the fetus
and help to protect the mother from the risks of delivery, such as hemorrhage. Knowledge of these cardiovascular
adaptations is required to correctly interpret hemodynamic and cardiovascular tests in the gravida, to predict the effects
of pregnancy on the woman with underlying cardiac disease, and to understand how the fetus will be affected by
maternal cardiac disorders.
The cardiovascular changes associated with normal pregnancy will be reviewed here. The management of specific
cardiac disorders, such as acquired and congenital heart disease, heart failure, and arrhythmias, are discussed
separately. (See "Acquired heart disease and pregnancy" and "Pregnancy in women with congenital heart disease:
General principles" and "Management of heart failure during pregnancy".)
CHANGES IN BLOOD VOLUME Expansion of the plasma volume and an increase in red blood cell mass begin as
early as the fourth week of pregnancy, peak at 28 to 34 weeks of gestation, and then plateau until parturition [2-4].
Plasma volume expansion is accompanied by a lesser increase in red cell volume (figure 2) [5]. As a result, there is a
modest reduction in hematocrit, with peak hemodilution occurring at 24 to 26 weeks. The blood volume in pregnant
women at term is about 100 mL/kg [6].
Plasma volume Total body volume expansion is accompanied by retention of 900 to 1000 meq of sodium and 6 to 8
liters of water, distributed among the fetus, amniotic fluid, and extracellular and intracellular spaces [7,8]. Plasma volume
increases by 10 to 15 percent at 6 to 12 weeks of gestation [9-11], expands rapidly until 30 to 34 weeks, after which
there is only a modest rise. The total gain at term averages 1100 to 1600 mL and results in a plasma volume of 4700 to
5200 mL, 30 to 50 percent above that found in nonpregnant women [4,9]. Mild edema is commonly seen.
Plasma renin activity tends to be increased and atrial natriuretic peptide levels are slightly reduced, suggesting that the
increase in plasma volume represents underfilling due to systemic vasodilatation and the ensuing rise in vascular
capacitance, rather than true blood volume expansion which would produce the opposite hormonal profile (low plasma
renin activity, elevated atrial natriuretic peptide) [12,13]. Furthermore, the degree of sodium retention is physiologically
regulated, as increasing sodium intake does not produce further volume expansion [7]. Humoral factors that contribute to
volume regulation during pregnancy are discussed separately. (See "Maternal endocrine and metabolic adaptation to
pregnancy", section on 'Adrenal gland'.)
There are no specific measures that can be taken to expand the plasma volume in pregnant women and there is no
evidence that the expansion of plasma volume would reverse or prevent associated poor pregnancy outcomes. In
principle, increasing dietary protein may improve colloid oncotic pressure (COP) which would shift extravascular fluid to
the intravascular space. Increasing maternal hydration may also act synergistically with a higher COP to improve
http://0-www.uptodate.com.elibrary.qatar-weill.cornell.edu/contents/mptions+pregnancy&selectedTitle=1%7E150&view=print&displayedView=full
Page 1 of 13
Maternal cardiovascular and hemodynamic adaptations to pregnancy
6/23/15, 4:52 AM
intravascular volume. There is also at least one anecdotal case of a patient given serial colloid infusions and furosemide
who had a successful pregnancy outcome, but we do not recommend this in the absence of data from well-designed
studies.
Red blood cell mass Red blood cell mass begins to increase at 8 to 10 weeks of gestation and steadily rises, in
women taking iron supplements, by 20 to 30 percent (250 to 450 mL) above nonpregnant levels by the end of pregnancy
[4,14-17]. Among women not on iron supplements, the red cell mass may only increase by 15 to 20 percent [18].
Increased plasma erythropoietin induces the rise in red cell mass, which partially supports the higher metabolic
requirement for oxygen during pregnancy [19].
Physiologic anemia A greater increase in intravascular volume compared to red cell mass results in the dilutional
or physiologic anemia of pregnancy. This becomes most apparent at 30 to 34 weeks of gestation when plasma volume
peaks in relation to red cell volume.
The physiologic effects of hypervolemia and anemia during pregnancy has several benefits:
Decreased blood viscosity (from greater increases in plasma volume than red cell volume) results in reduced
resistance to flow, facilitating placental perfusion and lowering cardiac work.
Total blood volume increases to approximately 50 percent above nonpregnant values near term to provide some
reserve against the normal blood loss during parturition (about 300 to 500 mL for vaginal delivery, 600 to 1000 mL
for cesarean delivery) and peripartum hemorrhage [3,4]. Following delivery, as much as 500 mL of blood
sequestered in the uteroplacental unit is autotransfused to the maternal circulation, thereby minimizing adverse
circulatory effects from blood loss at delivery.
Most of the increase in cardiac output is distributed to the placenta, kidneys, and skin to provide nutrients to the
fetus, excrete maternal and fetal waste products, and assist maternal temperature control, respectively. The
increases in renal blood flow and glomerular filtration rate during pregnancy are largely mediated by the ovarian
hormone relaxin, the release of which is increased by human chorionic gonadotropin [20]. (See "Renal and urinary
tract physiology in normal pregnancy".)
The absence of physiologic anemia appears to be harmful [21,22]. A population-based, case-control study using data
from the Swedish Medical Birth Register found that women with a hemoglobin concentration of 14.6 g/dL or higher at the
first prenatal visit were at increased risk of stillbirth (odds ratio (OR) 1.8), antepartum stillbirth without malformations (OR
2.0), and preterm and small for gestational age nonmalformed stillbirth (OR 2.7 and 4.2, respectively) [21]. The elevated
risk persisted despite a subsequent fall in hemoglobin concentration and after excluding women with preeclampsia. It is
hypothesized that high blood viscosity increases the risk of thrombosis in the uteroplacental circulation.
Assuming normal renal function, blood volume and constituents return to nonpregnant values by eight weeks
postpartum, a result of diuresis. Hemoglobin begins to increase from the third postpartum day [6].
CHANGES IN SYSTEMIC HEMODYNAMICS Maternal and fetal metabolic requirements increase as pregnancy
progresses. A change in the volume and distribution of cardiac output (the product of stroke volume and heart rate)
occurs during pregnancy to meet these demands (figure 3).
Cardiac output The cardiac output rises 30 to 50 percent (1.8 L/min) above baseline during normal pregnancy; onehalf of this increase occurs by 8 weeks of gestation [23-27]. The degree of change is acutely influenced by posture, as
the cardiac output is higher when the pregnant woman is in the left lateral decubitus position, particularly in the latter part
of pregnancy [5,28,29]. By comparison, assumption of the supine position can lower the cardiac output by as much as
25 to 30 percent due to compression of the inferior cava by the gravid uterus, leading to a substantial reduction in
venous return to the heart.
http://0-www.uptodate.com.elibrary.qatar-weill.cornell.edu/contents/mptions+pregnancy&selectedTitle=1%7E150&view=print&displayedView=full
Page 2 of 13
Maternal cardiovascular and hemodynamic adaptations to pregnancy
6/23/15, 4:52 AM
The elevation in cardiac performance results in part from changes in three important factors that determine cardiac
output:
Preload is increased due to the associated rise in blood volume
Afterload is reduced due to the decline in systemic vascular resistance (see below) [24]
Maternal heart rate rises by 15 to 20 beats/min [24].
In early pregnancy, increased cardiac output is primarily related to the rise in stroke volume; in late pregnancy, heart rate
is the major factor. The ejection fraction is unchanged from normal nonpregnant values, making it a reliable indicator of
left ventricular function during pregnancy, although the direct effect of pregnancy on left ventricular contractility remains
controversial [30]. Regardless of the mechanism, the stress induced by the increase in cardiac output can cause women
with underlying and, in some cases, asymptomatic heart disease to decompensate during the latter half of pregnancy.
(See "Management of heart failure during pregnancy".) Changes in maternal heart rate, stroke volume, and cardiac
output during pregnancy measured in the lateral and supine positions are demonstrated in the figure (figure 3).
Twin pregnancy The cardiovascular changes in women carrying twins are greater than those described above for
singleton pregnancies. Two-dimensional and M-mode echocardiography of 119 women (in the left lateral position) with
twins showed that cardiac output was 20 percent higher than in women carrying singletons, and peaked at 30 weeks of
gestation [31]. This increase was due to a 15 percent increase in stroke volume and 3.5 percent increase in heart rate.
Vascular resistance and blood pressure Systolic and diastolic blood pressure (BP) typically fall early in gestation
and are about 5 to 10 mmHg below baseline in the second trimester, declining to a mean of about 105/60 mmHg [24,3237]. In the third trimester, blood pressure gradually increases and may normalize to nonpregnant values by term.
The fall in BP is induced by a reduction in systemic vascular resistance, which in pregnancy appears to parallel changes
in afterload [38]. Both creation of a high flow, low-resistance circuit in the uteroplacental circulation and vasodilatation
contribute to the decline in vascular resistance [24]. The factors responsible for the vasodilatation are incompletely
understood, but one of the major findings is decreased vascular responsiveness to the pressor effects of angiotensin II
and norepinephrine [39-41]. Several additional mechanisms for the fall in vascular resistance have been proposed:
Increased endothelial prostacyclin [42]
Enhanced nitric oxide production [43]
Reduced aortic stiffness [44].
The possible role of humoral agents, such as estrogens, progesterone, and prolactin, in mediating the vasodilation
remains to be established [12]. In animals, as an example, estrogen and prolactin can both lower vascular resistance
and raise cardiac output [5].
Central hemodynamic changes As noted, cardiac function in the structurally normal heart is determined by preload,
afterload, heart rate, and contractility. Although changes in blood volume during pregnancy affect right ventricular
preload, central venous pressure remains in the normal nonpregnant range throughout pregnancy due to the reduction in
cardiac afterload induced by the substantial decrease in both systemic vascular resistance and pulmonary vascular
resistance (ie, afterload to the left and right heart, respectively) [45].
The inherent contractility of the myocardium is stable to slightly improved in pregnancy [46,47]. Pulmonary capillary
wedge pressure and pulmonary artery systolic and diastolic pressures remain in the normal nonpregnant range since the
hypervolemia of pregnancy is balanced by the fall in pulmonary vascular resistance.
Cerebral blood flow Several studies have reported a small increase in cerebral blood during normal pregnancy,
accompanied by a progressive decrease in cerebral vascular resistance [48-51].
Supine hypotensive syndrome Uterine enlargement beyond about 20 weeks' size can compress the inferior vena
http://0-www.uptodate.com.elibrary.qatar-weill.cornell.edu/contents/mptions+pregnancy&selectedTitle=1%7E150&view=print&displayedView=full
Page 3 of 13
Maternal cardiovascular and hemodynamic adaptations to pregnancy
6/23/15, 4:52 AM
cava (IVC), markedly reducing cardiac preload. This occurs primarily in the supine position and is relieved by displacing
the uterus to the left and off the IVC by placing a wedge under the woman's right side, having the woman lie on her left
side, or adjusting the operating table to a 30 left lateral tilt [52]. Other, less common, causes of supine hypotension
include aortic compression and neurogenic etiologies.
The reduction in preload can result in maternal hypotension, usually within 3 to 10 minutes, associated with one or more
signs and symptoms of reflex autonomic activation and/or reduced cardiac output (table 1) [52,53]. The earliest sign of
developing supine hypotension is an increase in maternal heart rate and a decrease in pulse pressure indicating
significantly reduced venous return [52]. Although these alterations are the best indicators of an impending attack, many
women remain asymptomatic.
In addition, a reduction in placental perfusion may result in nonreassuring changes in the fetal heart rate with no or
minimal decrease in upper extremity maternal blood pressure [54]. Therefore, it is important to position the parturient in
the left lateral tilt position for procedures (eg, labor and delivery, surgery, nonstress test, ultrasound) and to avoid the
supine position, even in symptom-free women.
VASCULAR CHANGES The vascular system is more compliant during pregnancy. Although not consistently found,
specific changes have been reported in the aortic media of pregnant women. [55]. These include: fragmentation of
reticular fibers; a decrease in acid mucopolysaccharides, loss of normal corrugation of elastic fibers; and hypertrophy
and hyperplasia of smooth muscle cells [56]. In addition, a small increase in the aortic diameter occurs, which increases
its compliance [57].
Aortic dissection is rare in normal young women, but when dissection occurs it usually does so during pregnancy [5860]. Dissecting aneurysm may result, in part, from the alterations described above and the occasional coincidence of
pregnancy and clinically isolated annuloaortic ectasia, even though this occurs with a 2:1 to 8:1 male predominance [61].
UTERINE BLOOD FLOW Uterine artery blood flow has been reported to increase from 50 to 60 mL/minute in the late
first trimester, to 185 mL/minute at 28 weeks, and to 450 to 750 mL/minute at term [62,63]. Cardiac output and uterine
artery diameter also increase with advancing gestation. In early pregnancy, the uterus receives 3 to 6 percent of cardiac
output; at term, the proportion is about 12 percent [62,64].
CHANGES IN SYSTEMIC COAGULATION Pregnancy is associated with changes in several coagulation factors that
result in a 20 percent reduction of prothrombin and the partial thromboplastin times [65-67]:
Resistance to activated protein C increases in the second and third trimesters [67]
Protein S decreases [68]
Factors I, II, V, VII, VIII, X, and Xll increase [68-70]
Activity of the fibrinolytic inhibitors PAI-1 and PAI-2 increases, although total fibrinolytic activity may not be impaired
[71,72]
The net effect of these pregnancy-induced changes is to produce a hypercoagulable state, which is a double-edged
sword of protection (eg, hemostasis contributing to reduced blood loss at delivery) and risk (eg, thromboembolic
phenomenon) [68]. Venous thrombosis in pregnancy occurs in approximately 0.7 per 1000 women, and is three to four
fold higher in the puerperium than during pregnancy [69,73]. The risk is increased in women with underlying inherited
thrombophilia (eg, factor V Leiden or the prothrombin gene mutation) [74-76]. (See "Deep vein thrombosis in pregnancy:
Epidemiology, pathogenesis, and diagnosis" and "Deep vein thrombosis and pulmonary embolism in pregnancy:
Prevention" and "Deep vein thrombosis and pulmonary embolism in pregnancy: Treatment" and "Inherited
thrombophilias in pregnancy".)
ARRHYTHMIAS AND PALPITATIONS The exact mechanism of increased arrhythmia burden during pregnancy is
unclear, but has been attributed to hemodynamic, hormonal, and autonomic changes related to pregnancy. (See
http://0-www.uptodate.com.elibrary.qatar-weill.cornell.edu/contents/mptions+pregnancy&selectedTitle=1%7E150&view=print&displayedView=full
Page 4 of 13
Maternal cardiovascular and hemodynamic adaptations to pregnancy
6/23/15, 4:52 AM
"Supraventricular arrhythmias during pregnancy" and "Ventricular arrhythmias during pregnancy".)
Palpitations occur frequently during pregnancy and are a common indication for cardiac evaluation during pregnancy.
The differential diagnosis of palpitations is extensive and the diagnostic evaluation of pregnant women with palpitations
does not differ from nonpregnant women. (See "Overview of palpitations in adults".)
HEMODYNAMIC CHANGES RELATED TO LABOR AND DELIVERY Normal labor and delivery is associated with
significant hemodynamic changes due to anxiety, exertion, pain, uterine contractions, uterine involution, and bleeding.
Cardiovascular effects also occur in some women due to infection, hemorrhage, or the administration of anesthesia or
analgesia.
Cardiac output Blood from the uterine sinusoids is forced into the systemic circulation with each uterine contraction,
thereby increasing preload during labor (figure 4).
Cardiac output increases by 15 percent above prelabor levels in early labor and by approximately 25 percent
during the active phase.
The additional exertion associated with pushing in the second stage results in a 50 percent rise in cardiac output.
Immediately postpartum, cardiac output increases to 80 percent above prelabor values due to significant
autotransfusion associated with uterine involution that is more pronounced than the normal blood loss of delivery.
The cardiac output and systemic vascular resistance gradually return to nonpregnant levels over a period of three
months or more [77].
Blood pressure Systolic and diastolic blood pressure increase 15 to 25 and 10 to 15 percent, respectively, during
each uterine contraction. The rise in systemic blood pressure is dependent upon the duration and intensity of uterine
contractions, position of the parturient, and the amount of pain and anxiety she is feeling. The increases in arterial
pressure associated with each uterine contraction are mirrored by a rise in pressure in the amniotic fluid, intrathoracic
venous, cerebrospinal fluid, and extradural compartments (figure 5).
Bearing down or pushing during the second stage of labor alters the blood pressure and heart rate in a similar way to the
Valsalva maneuver; these changes are less pronounced if the gravida is positioned in the left lateral versus supine
position. The hemodynamic changes resulting from a Valsalva maneuver vary with the different phases.
During phase 1, with the onset of the maneuver, there is a transient increase in left ventricular output.
During the straining phase, phase 2, there is a decrease in venous return, right and left ventricular volumes, stroke
volumes, mean arterial pressure, and pulse pressure; this is associated with a reflex increase in heart rate.
During phase 3 (release of Valsalva), which only lasts for a few cardiac cycles, there is a further reduction in left
ventricular volume.
Phase 4 is characterized by increases in stroke volume and arterial pressure and reflex slowing of heart rate (the
overshoot).
Changes in baroreceptor sensitivity during pregnancy and associated with maternal position may also play a role. As an
example, one study of normotensive pregnant women noted a marked decrease in baroreflex sensitivity for heart rate in
the supine position, but not while standing [78].
POSTPARTUM HEMODYNAMIC RESOLUTION The postpartum period is marked by significant hemodynamic
alterations. Fluctuations in cardiac output, stroke volume, and heart rate occur after delivery. Within the first ten minutes
following a term vaginal delivery, the cardiac output and stroke volume increase by 59 and 71 percent, respectively [79].
At one hour postpartum, both the cardiac output and stroke volume remain increased (by 49 and 67 percent,
http://0-www.uptodate.com.elibrary.qatar-weill.cornell.edu/contents/mptions+pregnancy&selectedTitle=1%7E150&view=print&displayedView=full
Page 5 of 13
Maternal cardiovascular and hemodynamic adaptations to pregnancy
6/23/15, 4:52 AM
respectively) while the heart rate decreases by 15 percent; blood pressure remained unchanged [80].
The increases in stroke volume and cardiac output most likely result from improved cardiac preload from auto
transfusion of utero placental blood to the intravascular space. As the uterus decompresses following delivery, a
reduction in the mechanical compression of the vena cava allows for further increases in cardiac preload.
These cardiovascular physiologic changes resolve slowly after delivery. A study that evaluated cardiac output and stroke
volume in 15 healthy nonlaboring patients at 38 weeks of gestation, and again at 2, 6, 12, and 24 weeks postpartum
demonstrated a gradual diminution in cardiac output from 7.42 L/min at 38 weeks gestation to 4.96 L/min at 24 weeks
postpartum [81]. As early as two weeks post partum there were substantial reductions in left ventricular size and
contractibility as compared to term pregnancies.
EVALUATION OF THE CARDIOVASCULAR SYSTEM IN PREGNANCY The physiologic and anatomic adaptations
to pregnancy influence the interpretation and evaluation of the gravida's cardiovascular status.
Physical examination The circulatory and respiratory changes during normal pregnancy are sometimes erroneously
attributed to heart disease. The clinician caring for the gravida should be aware of these normal maternal cardiovascular
adaptations to pregnancy.
Breathlessness (innocent hyperpnea), easy fatiguability, decreased exercise tolerance, basal rales that disappear
with cough or deep breathing, and peripheral edema commonly occur during pregnancy in normal women.
The systemic arterial pulse is characterized by a rapid rise and a brisk collapse (small water hammer) beginning in
the first trimester.
The jugular venous pulse is more conspicuous after the 20th week because brisk X and Y descents make the A
and V waves more obvious. Mean jugular venous pressure, as estimated from the superficial jugular vein, remains
normal.
The pregnant woman's heart is shifted to the left, anterior, and rotated toward a transverse position as the uterus
enlarges. As a result, the apical impulse is shifted cephalad to the fourth intercostal space and laterally to the
midclavicular line. The left ventricular impulse is relatively hyperdynamic but not sustained; the right ventricle may
be palpable because, like the left ventricle, it handles a larger volume of blood that is ejected against relatively low
resistance. As pregnancy progresses, enlargement of the breasts and abdomen makes accurate palpation of the
heart difficult, if not impossible.
Auscultatory changes accompanying normal gestation begin in the late first trimester and generally disappear
within a week after delivery. A higher basal heart rate, louder heart sounds, wide splitting of S1, splitting of S2 in
the third trimester, and a systolic ejection murmur (up to grade 2/4) over the pulmonary and tricuspid areas are
regularly detected upon cardiac auscultation. A third heart sound is present in most pregnant women; the fourth
heart sound is rarely heard. The venous hum is almost universal in normal women during gestation. The mammary
souffle (systolic or continuous) is heard over the breasts in late gestation and is peculiar to pregnancy; it is
especially common postpartum in lactating women.
Diastolic murmurs are uncommon in normal pregnant women. When they occur, they may reflect increased flow
through the tricuspid or mitral valve or physiologic dilatation of the pulmonary artery. However, these murmurs
more likely represent a pathologic condition necessitating further study [82].
Echocardiogram Physiologic multivalvular regurgitation, predominantly right-sided, is a frequent normal finding
during late gestation and may persist throughout the early post partum period [83]. In addition, chamber enlargement,
valvular annular dilatation, and a small asymptomatic pericardial effusion are frequent normal incidental findings during
late gestation [25,83,84].These findings appear to be caused by pregnancy-related hypervolemia and are important
http://0-www.uptodate.com.elibrary.qatar-weill.cornell.edu/contents/mptions+pregnancy&selectedTitle=1%7E150&view=print&displayedView=full
Page 6 of 13
Maternal cardiovascular and hemodynamic adaptations to pregnancy
6/23/15, 4:52 AM
considerations when interpreting an echocardiogram in a pregnant patient.
Electrocardiogram Normal anatomic and physiologic changes of the heart and chest wall during pregnancy cause
changes in the electrocardiogram that are unrelated to disease. The heart is rotated toward the left, resulting in a 15 to
20 left axis deviation. Marked variation in chamber volumes, especially left atrial enlargement, leads to stretching of the
cardiac conduction pathways and predisposes to alterations in cardiac rhythm. Periods of supraventricular tachycardia
and ventricular extrasystoles are a common finding. Other findings, which can be normal, include transient ST segment
and T wave changes, the presence of a Q wave and inverted T waves in lead III, an attenuated Q wave in lead AVF, and
inverted T waves in leads V1, V2 and, occasionally, V3 [46,85,86]. (See "Ventricular arrhythmias during pregnancy" and
"Supraventricular arrhythmias during pregnancy".)
Chest radiograph The left, anterior, superior rotation of the heart and hypervolemia give the illusion of ventricular
hypertrophy and cardiomegaly on chest radiographs; increased pulmonary vascular markings are also common.
Rotation of the heart may also cause an indentation of the esophagus by the left atrium and straightening of the left heart
border. The majority of these changes are temporary and return to normal by eight weeks postpartum.
SUMMARY AND RECOMMENDATIONS
Expansion of the plasma volume and an increase in red blood cell mass begin as early as the fourth week of
pregnancy, peak at 28 to 34 weeks of gestation, and then plateau. Plasma volume expansion exceeds the increase
in red cell volume, leading to "physiologic anemia". (See 'Changes in blood volume' above.)
The major hemodynamic changes induced by pregnancy include an increase in cardiac output and reductions in
systemic vascular resistance and systemic blood pressure. Cardiac output peaks a few minutes after delivery,
before gradually returning to prepregnancy levels. (See 'Changes in systemic hemodynamics' above and
'Postpartum hemodynamic resolution' above.)
Changes in several coagulation factors produce a hypercoagulable state. (See 'Changes in systemic coagulation'
above.)
Labor and delivery is associated with significant hemodynamic changes due to anxiety, exertion, pain, uterine
contractions, uterine involution, and bleeding. Infection, hemorrhage, and the administration of anesthesia or
analgesia also play a role. (See 'Hemodynamic changes related to labor and delivery' above.)
The physiologic and anatomic adaptations to pregnancy influence the interpretation and evaluation of the pregnant
woman's cardiac evaluation. (See 'Evaluation of the cardiovascular system in pregnancy' above.)
Use of UpToDate is subject to the Subscription and License Agreement.
Topic 443 Version 10.0
http://0-www.uptodate.com.elibrary.qatar-weill.cornell.edu/contents/mptions+pregnancy&selectedTitle=1%7E150&view=print&displayedView=full
Page 7 of 13
Maternal cardiovascular and hemodynamic adaptations to pregnancy
6/23/15, 4:52 AM
GRAPHICS
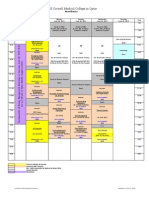
Hemodynamic changes in normal pregnancy
Normal pregnancy is characterized by an increase in cardiac output, a
reduction in systemic vascular resistance, and minimal change in mean
blood pressure. These changes are associated with a 10 to 15 beat/min
increase in heart rate.
Graphic 54685 Version 3.0
http://0-www.uptodate.com.elibrary.qatar-weill.cornell.edu/contents/mptions+pregnancy&selectedTitle=1%7E150&view=print&displayedView=full
Page 8 of 13
Maternal cardiovascular and hemodynamic adaptations to pregnancy
6/23/15, 4:52 AM
Total blood volume, plasma volume and red cell
volume in normal pregnancy
Data from Shnider SM, Levinson G. Anesthesia for Obstetrics, 3rd ed,
Williams & Wilkins, Baltimore, p. 8.
Graphic 61948 Version 2.0
http://0-www.uptodate.com.elibrary.qatar-weill.cornell.edu/contents/mptions+pregnancy&selectedTitle=1%7E150&view=print&displayedView=full
Page 9 of 13
Maternal cardiovascular and hemodynamic adaptations to pregnancy
6/23/15, 4:52 AM
Systemic hemodynamics during normal pregnancy
Data from: Bonica JJ, McDonald JS. Principles and Practice of Obstetric Analgesia
and Anesthesia, 2nd ed, Williams & Wilkins, Baltimore, 1994. p.60.
Graphic 55985 Version 2.0
http://0-www.uptodate.com.elibrary.qatar-weill.cornell.edu/contents/ptions+pregnancy&selectedTitle=1%7E150&view=print&displayedView=full
Page 10 of 13
Maternal cardiovascular and hemodynamic adaptations to pregnancy
6/23/15, 4:52 AM
Signs and symptoms attributed to supine hypotensive syndrome in
pregnancy
Faintness
Dyspnea
Dizziness
Restlessness
Nausea
Vomiting
Chest pain
Abdominal pain
Visual disturbances
Numbness
Paresthesias
Headache
Cold, clammy skin
Pallor
Cyanosis
Hypotension
Graphic 80135 Version 1.0
http://0-www.uptodate.com.elibrary.qatar-weill.cornell.edu/contents/ptions+pregnancy&selectedTitle=1%7E150&view=print&displayedView=full
Page 11 of 13
Maternal cardiovascular and hemodynamic adaptations to pregnancy
6/23/15, 4:52 AM
Cardiac output during normal labor, delivery, and
postpartum
Data from Bonica, JJ, McDonald, JS. Principles and Practice of Obstetric
Analgesia and Anesthesia, 2nd ed, Williams &Wilkins, Baltimore, 1994. p. 62.
Graphic 79834 Version 1.0
http://0-www.uptodate.com.elibrary.qatar-weill.cornell.edu/contents/ptions+pregnancy&selectedTitle=1%7E150&view=print&displayedView=full
Page 12 of 13
Maternal cardiovascular and hemodynamic adaptations to pregnancy
6/23/15, 4:52 AM
Hemodynamics with contractions
Data from: Bonica JJ, McDonald JS. Principles and Practice of Obstetric Analgesia
and Anesthesia, 2nd ed, Williams & Wilkins, Baltimore, 1994. p.66.
Graphic 69056 Version 2.0
http://0-www.uptodate.com.elibrary.qatar-weill.cornell.edu/contents/ptions+pregnancy&selectedTitle=1%7E150&view=print&displayedView=full
Page 13 of 13
Vous aimerez peut-être aussi
- Bell Single-Sleeve Shrug Crochet PatternDocument2 pagesBell Single-Sleeve Shrug Crochet PatternsicksoxPas encore d'évaluation
- Clinical Obstetrics/Gynecology Review 2023: For USMLE Step 2 CK and COMLEX-USA Level 2D'EverandClinical Obstetrics/Gynecology Review 2023: For USMLE Step 2 CK and COMLEX-USA Level 2Évaluation : 4 sur 5 étoiles4/5 (1)
- Preparation For MCAT Verbal ReasoningDocument88 pagesPreparation For MCAT Verbal ReasoningAishwarya Balasubramaniyan100% (3)
- CA-idms Ads Alive User Guide 15.0Document142 pagesCA-idms Ads Alive User Guide 15.0svdonthaPas encore d'évaluation
- AAFP QuestionsDocument509 pagesAAFP QuestionsAnchalia Chandrakumaran100% (3)
- Physiologycal Changes in PregnancyDocument66 pagesPhysiologycal Changes in PregnancyYulia RestyPas encore d'évaluation
- Combat Storm - Shipping ContainerDocument6 pagesCombat Storm - Shipping ContainermoiPas encore d'évaluation
- 1 - Maternal Physiological Changes During PregnancyDocument45 pages1 - Maternal Physiological Changes During PregnancyKholoud KholoudPas encore d'évaluation
- Physiological Changes During Pregnancy 2010Document42 pagesPhysiological Changes During Pregnancy 2010Asyhok Renault100% (1)
- Management of Pregnant Patient in DentistryDocument10 pagesManagement of Pregnant Patient in DentistryVíctor Orduña LópezPas encore d'évaluation
- Paso de Blas Lying in Clinic For NewDocument5 pagesPaso de Blas Lying in Clinic For NewNaheed Dean MustafaPas encore d'évaluation
- Practice Quiz Reflection Project Initiation and Key ComponentsDocument3 pagesPractice Quiz Reflection Project Initiation and Key ComponentsFalastin Tanani67% (3)
- Neonatal PolycythemiaDocument13 pagesNeonatal PolycythemiaMariel HuamancayoPas encore d'évaluation
- Physiology, Maternal Changes - StatPearls - NCBI Bookshelf PDFDocument5 pagesPhysiology, Maternal Changes - StatPearls - NCBI Bookshelf PDFAlejandro DiezPas encore d'évaluation
- Cambios Fisiologicos EmbarazoDocument23 pagesCambios Fisiologicos EmbarazoajanethPas encore d'évaluation
- Alterations in Physiology and Anatomy During Pregnancy PDFDocument12 pagesAlterations in Physiology and Anatomy During Pregnancy PDFAsh AmePas encore d'évaluation
- Maternal Adaptations To Pregnancy - Hematologic Changes - UpToDate PDFDocument27 pagesMaternal Adaptations To Pregnancy - Hematologic Changes - UpToDate PDFDiego Andres VasquezPas encore d'évaluation
- Shock and PregnancyDocument11 pagesShock and Pregnancy101 Andi Dwi Fahria.RPas encore d'évaluation
- Hematologic Changes in PregnancyDocument27 pagesHematologic Changes in PregnancySafinaz Inaz100% (1)
- Physiological Changes in Pregnancy - PMCDocument16 pagesPhysiological Changes in Pregnancy - PMCWidad SalsabilaPas encore d'évaluation
- Changes in PregnancyDocument9 pagesChanges in PregnancyFrankRodríguezLuisPas encore d'évaluation
- Physiology 212 Harrison AssignmentDocument3 pagesPhysiology 212 Harrison AssignmentHarrison RumePas encore d'évaluation
- Maternal Adaptations To PregnancyDocument12 pagesMaternal Adaptations To PregnancyTessa AcostaPas encore d'évaluation
- Definition:: Maternal Physiology During PregnancyDocument139 pagesDefinition:: Maternal Physiology During PregnancygibreilPas encore d'évaluation
- Maternal Adaptations To Pregnancy - Renal and Urinary Tract Physiology - UpToDateDocument9 pagesMaternal Adaptations To Pregnancy - Renal and Urinary Tract Physiology - UpToDateGrace TupiaPas encore d'évaluation
- Hematologic Changes in PregnancyDocument9 pagesHematologic Changes in PregnancyAlberto VelazquezPas encore d'évaluation
- Physiological Changes in Pregnancy: Candice K Silversides, Jack M ColmanDocument12 pagesPhysiological Changes in Pregnancy: Candice K Silversides, Jack M ColmanrinimeimeiPas encore d'évaluation
- OB I For 2nd YearDocument122 pagesOB I For 2nd YeardiribaPas encore d'évaluation
- Hematological Changes in Pregnancy The PreparatiDocument6 pagesHematological Changes in Pregnancy The Preparatiمحمد رحيم حسن محمودPas encore d'évaluation
- 1 s2.0 S2666668521001324 MainDocument5 pages1 s2.0 S2666668521001324 Mainmchojnacki81Pas encore d'évaluation
- CARDIOVASCULARDocument7 pagesCARDIOVASCULARyoungjbPas encore d'évaluation
- Obstetric AnesthesiaDocument31 pagesObstetric AnesthesiaChosenPas encore d'évaluation
- Reanimacion en La Paciente EmbarazadaDocument13 pagesReanimacion en La Paciente EmbarazadaJerry PowersPas encore d'évaluation
- Maternal Physiology in Pregnancy by ERMIDocument56 pagesMaternal Physiology in Pregnancy by ERMIHenok Y KebedePas encore d'évaluation
- Hematological Profile of Pregnant Women at St. Paul 'S Hospital Millennium Medical College, Addis Ababa, EthiopiaDocument7 pagesHematological Profile of Pregnant Women at St. Paul 'S Hospital Millennium Medical College, Addis Ababa, Ethiopiaade lydia br.siregarPas encore d'évaluation
- Maternal Physiology During PregnancyDocument60 pagesMaternal Physiology During PregnancySerge TresorPas encore d'évaluation
- Physiologic Changes of Pregnacy ADODocument55 pagesPhysiologic Changes of Pregnacy ADOTadesse MuhammedPas encore d'évaluation
- Resume Luar Negeri Dita FebriyantiDocument9 pagesResume Luar Negeri Dita FebriyantiDita FebriyantiPas encore d'évaluation
- Acute Abdomen in PregnancyDocument14 pagesAcute Abdomen in PregnancyNaila WardhanaPas encore d'évaluation
- Maternalphysiologylecture 091206194125 Phpapp01Document69 pagesMaternalphysiologylecture 091206194125 Phpapp01Ian Kirby Formeloza SolpicoPas encore d'évaluation
- Physiological Changes in Hematological Parameters During PregnancyDocument4 pagesPhysiological Changes in Hematological Parameters During PregnancyEva SihalohoPas encore d'évaluation
- Heart Disease and PregnancyDocument17 pagesHeart Disease and PregnancyDuy Nguyen CongPas encore d'évaluation
- Maternal Physiology and Complications of Multiple PregnancyDocument11 pagesMaternal Physiology and Complications of Multiple PregnancyFafaPas encore d'évaluation
- Normal PregnancyDocument150 pagesNormal Pregnancydevag0973Pas encore d'évaluation
- Thrombocytopenia in The Parturient: ReviewarticleDocument10 pagesThrombocytopenia in The Parturient: ReviewarticlesteffiesolinPas encore d'évaluation
- Presentor:-Sameeksha Sidhpuria Moderator: - Mrs. ANUPAMADocument69 pagesPresentor:-Sameeksha Sidhpuria Moderator: - Mrs. ANUPAMALakshmi PrasannaPas encore d'évaluation
- Preeclampsia: Clinical Features and DiagnosisDocument20 pagesPreeclampsia: Clinical Features and DiagnosisEdward VertizPas encore d'évaluation
- Physiologic Changes During Pregnancy and DeliveryDocument13 pagesPhysiologic Changes During Pregnancy and DeliveryBudi Khang100% (1)
- Physiological Changes in PregnancyDocument4 pagesPhysiological Changes in PregnancyMichimichi 78Pas encore d'évaluation
- Post Partum HemorrhageDocument10 pagesPost Partum HemorrhagedenekePas encore d'évaluation
- Pregnancy and Renal Function: Educational SupplementDocument3 pagesPregnancy and Renal Function: Educational SupplementIskandar HasanPas encore d'évaluation
- Critical Illness in Pregnancy Part I: An Approach To A Pregnant Patient in The ICU and Common Obstetric DisordersDocument12 pagesCritical Illness in Pregnancy Part I: An Approach To A Pregnant Patient in The ICU and Common Obstetric Disordersgustavo1rodriguesPas encore d'évaluation
- Physiological Changes in PregnancyDocument7 pagesPhysiological Changes in PregnancyFarid DjafarPas encore d'évaluation
- Hematological Changes Blood Volume: Figure 4-6Document12 pagesHematological Changes Blood Volume: Figure 4-6'aac' JujuuPas encore d'évaluation
- Physiologic Changes of PregnancyDocument8 pagesPhysiologic Changes of PregnancyAsteway MesfinPas encore d'évaluation
- Hematological Changes Blood Volume: Figure 4-6Document12 pagesHematological Changes Blood Volume: Figure 4-6'aac' JujuuPas encore d'évaluation
- Anesthesia in Pregnant Patients For Nonobstetric SurgeryDocument7 pagesAnesthesia in Pregnant Patients For Nonobstetric SurgeryBig TexPas encore d'évaluation
- Physiologic Changes During Normal Pregnancy and DeliveryDocument13 pagesPhysiologic Changes During Normal Pregnancy and DeliveryAlejandra RequesensPas encore d'évaluation
- Trauma Dalam KehamilanDocument6 pagesTrauma Dalam Kehamilaniin FzahroPas encore d'évaluation
- Fisiología en El Embarazo - Crit Care 2006Document7 pagesFisiología en El Embarazo - Crit Care 2006Fabiola Buelna GaxiolaPas encore d'évaluation
- Riñon y EmbarazoDocument20 pagesRiñon y EmbarazoMTZGEJPas encore d'évaluation
- 10.1007@s11906 020 01058 WDocument11 pages10.1007@s11906 020 01058 WMauricio Lopez MejiaPas encore d'évaluation
- Jcbfm2012210a PDFDocument14 pagesJcbfm2012210a PDFVenerandaPas encore d'évaluation
- Classification and Treatment of Ovarian Hyperstimulation SyndromeDocument7 pagesClassification and Treatment of Ovarian Hyperstimulation SyndromeGabo Bravo RodríguezPas encore d'évaluation
- Beers 2020 ACKD Kidney Physiology in PregnancyDocument6 pagesBeers 2020 ACKD Kidney Physiology in PregnancyBCR ABLPas encore d'évaluation
- Endoscopy and Sedation: DR - Malavan Habeeb Internist & GI Endoscopist Lecturer - College of Medicine University of DuhokDocument37 pagesEndoscopy and Sedation: DR - Malavan Habeeb Internist & GI Endoscopist Lecturer - College of Medicine University of DuhokMalavan MohammedPas encore d'évaluation
- Hypoglycemia in Diabetes: Pathophysiology, Prevalence, and PreventionD'EverandHypoglycemia in Diabetes: Pathophysiology, Prevalence, and PreventionPas encore d'évaluation
- Weill Cornell Medical College in Qatar: Week 18Document1 pageWeill Cornell Medical College in Qatar: Week 18Anchalia ChandrakumaranPas encore d'évaluation
- 2014Document10 pages2014Anchalia ChandrakumaranPas encore d'évaluation
- Autonomic DRUGSDocument25 pagesAutonomic DRUGSAnchalia ChandrakumaranPas encore d'évaluation
- Weill Cornell Medical College in Qatar: Week 1: AnesthesiaDocument1 pageWeill Cornell Medical College in Qatar: Week 1: AnesthesiaAnchalia ChandrakumaranPas encore d'évaluation
- LG 4Document2 pagesLG 4Anchalia ChandrakumaranPas encore d'évaluation
- Nri 3349Document13 pagesNri 3349Anchalia ChandrakumaranPas encore d'évaluation
- BOD Week 3 ScheduleDocument1 pageBOD Week 3 ScheduleAnchalia ChandrakumaranPas encore d'évaluation
- Weill Cornell Medical College in Qatar: Week 17: RheumatologyDocument1 pageWeill Cornell Medical College in Qatar: Week 17: RheumatologyAnchalia ChandrakumaranPas encore d'évaluation
- 2014Document10 pages2014Anchalia ChandrakumaranPas encore d'évaluation
- Kjim 29 281Document10 pagesKjim 29 281Anchalia ChandrakumaranPas encore d'évaluation
- Tissue Factor and Cancer Metastasis - The Role of Intracellular and Extracellular Signaling PathwaysDocument6 pagesTissue Factor and Cancer Metastasis - The Role of Intracellular and Extracellular Signaling PathwaysAnchalia ChandrakumaranPas encore d'évaluation
- MSK Path LabDocument1 pageMSK Path LabAnchalia ChandrakumaranPas encore d'évaluation
- E2559 FullDocument8 pagesE2559 FullAnchalia ChandrakumaranPas encore d'évaluation
- New CompDocument5 pagesNew CompAnchalia ChandrakumaranPas encore d'évaluation
- Amphiregulin Induces Tyrosine Phosphorylation of The Epidermal Growth Factor Receptor and p185Document8 pagesAmphiregulin Induces Tyrosine Phosphorylation of The Epidermal Growth Factor Receptor and p185Anchalia ChandrakumaranPas encore d'évaluation
- NK CellDocument11 pagesNK CellAnchalia ChandrakumaranPas encore d'évaluation
- DiagramDocument1 pageDiagramAnchalia ChandrakumaranPas encore d'évaluation
- Access Public File Serve 1Document10 pagesAccess Public File Serve 1Anchalia ChandrakumaranPas encore d'évaluation
- May 2013 SchedulesDocument72 pagesMay 2013 SchedulesAnchalia ChandrakumaranPas encore d'évaluation
- The Transcription Factor Fra-2 Promotes Mammary Tumour Progression by Changing The Adhesive Properties of Breast Cancer CellsDocument11 pagesThe Transcription Factor Fra-2 Promotes Mammary Tumour Progression by Changing The Adhesive Properties of Breast Cancer CellsAnchalia ChandrakumaranPas encore d'évaluation
- Raw TrackDocument8 pagesRaw TrackAnchalia ChandrakumaranPas encore d'évaluation
- 749 FTPDocument11 pages749 FTPAnchalia ChandrakumaranPas encore d'évaluation
- Gangliosides Expressed On Breast Cancer Cells Are E-Selectin LigandsDocument7 pagesGangliosides Expressed On Breast Cancer Cells Are E-Selectin LigandsAnchalia ChandrakumaranPas encore d'évaluation
- 8660406Document14 pages8660406Anchalia ChandrakumaranPas encore d'évaluation
- Cancer Res 2011 Julien 7683 93Document12 pagesCancer Res 2011 Julien 7683 93Anchalia ChandrakumaranPas encore d'évaluation
- The Transcription Factor Fra-2 Promotes Mammary Tumour Progression by Changing The Adhesive Properties of Breast Cancer CellsDocument11 pagesThe Transcription Factor Fra-2 Promotes Mammary Tumour Progression by Changing The Adhesive Properties of Breast Cancer CellsAnchalia ChandrakumaranPas encore d'évaluation
- 8660406Document14 pages8660406Anchalia ChandrakumaranPas encore d'évaluation
- Paper Format IJRDTDocument3 pagesPaper Format IJRDTrock starPas encore d'évaluation
- Trend in Agricultural ProductivityDocument1 pageTrend in Agricultural ProductivityGiaPas encore d'évaluation
- Panel Hospital List IGIDocument6 pagesPanel Hospital List IGIAbdul RahmanPas encore d'évaluation
- MT4 EA Installation Guide Digital - EnglishDocument7 pagesMT4 EA Installation Guide Digital - EnglishThe Trading PitPas encore d'évaluation
- Spike Magazine Cup PackDocument5 pagesSpike Magazine Cup PackBungle MarleyPas encore d'évaluation
- Gel Electrophoresis Worksheet Teacher AnswersDocument3 pagesGel Electrophoresis Worksheet Teacher AnswersChris FalokunPas encore d'évaluation
- No ApprovedDocument154 pagesNo ApprovedAnnaPas encore d'évaluation
- Hotel Voucher: Itinerary ID Hotel Santika Taman Mini Indonesia IndahDocument2 pagesHotel Voucher: Itinerary ID Hotel Santika Taman Mini Indonesia IndahSyukron PribadiPas encore d'évaluation
- English Assignment - October 6, 2020 - Group AssignmentDocument3 pagesEnglish Assignment - October 6, 2020 - Group AssignmentDaffa RaihanPas encore d'évaluation
- COSO DefinEDDocument21 pagesCOSO DefinEDRefdy AnugrahPas encore d'évaluation
- VDRL - Press. GaugesDocument9 pagesVDRL - Press. GaugesSourav RayPas encore d'évaluation
- Exam C - HANATEC142: SAP Certified Technology Associate - SAP HANA (Edition 2014)Document10 pagesExam C - HANATEC142: SAP Certified Technology Associate - SAP HANA (Edition 2014)SadishPas encore d'évaluation
- Tip Sheet March 2017Document2 pagesTip Sheet March 2017hoangvubui4632Pas encore d'évaluation
- Asme Bladder Accumulator DatasheetDocument3 pagesAsme Bladder Accumulator DatasheetSamad A BakarPas encore d'évaluation
- Engineering Mathematics Questions and AnswersDocument9 pagesEngineering Mathematics Questions and AnswersZaky Muzaffar100% (1)
- No Experience ResumeDocument2 pagesNo Experience ResumeNatalia PantojaPas encore d'évaluation
- Police Cranston School Committee Member Stole PTO FundsDocument1 pagePolice Cranston School Committee Member Stole PTO FundsashaydelinePas encore d'évaluation
- Epidemiological Triad of HIV/AIDS: AgentDocument8 pagesEpidemiological Triad of HIV/AIDS: AgentRakib HossainPas encore d'évaluation
- DD 3600 3500 3000 Parts CatalogDocument46 pagesDD 3600 3500 3000 Parts CatalogAndres Fdo Mora D100% (2)
- KirbyDocument3 pagesKirbyNorhassanah UtosabuayanPas encore d'évaluation
- Introduction To Object Oriented Database: Unit-IDocument67 pagesIntroduction To Object Oriented Database: Unit-Ipreetham rPas encore d'évaluation
- 7 ApportionmentDocument46 pages7 Apportionmentsass sofPas encore d'évaluation
- Job Sheet 1Document5 pagesJob Sheet 1Sue AzizPas encore d'évaluation
- SET UP Computer ServerDocument3 pagesSET UP Computer ServerRicHArdPas encore d'évaluation
- Bank OD Account in Tally 1Document3 pagesBank OD Account in Tally 1yashusahu180Pas encore d'évaluation