Académique Documents
Professionnel Documents
Culture Documents
Out 11
Transféré par
Andi Suchy Qumala SarieTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Out 11
Transféré par
Andi Suchy Qumala SarieDroits d'auteur :
Formats disponibles
Sleep Breath (2012) 16:881886
DOI 10.1007/s11325-011-0590-1
ORIGINAL ARTICLE
Detection of postoperative sleep-disordered breathing
using a portable monitoring device
Ian D. Weir & Khaleel Mohammed Ahmed & Steve Korbuly & Anil Achaen &
Mary OMalley & Ed OMalley & Christopher Manfredi & Dorothy B. Wakefield &
Jonathan M. Fine & Stephen M. Winter
Received: 9 November 2010 / Revised: 18 August 2011 / Accepted: 5 September 2011 / Published online: 28 September 2011
# Springer-Verlag 2011
Abstract
Purpose Adverse surgical outcomes may occur more
frequently in patients with sleep-disordered breathing
(SDB). Despite this concern, there have been no prospective studies using objective measures of postoperative SDB
to determine the scope of the problem. We designed a
prospective study to determine the feasibility of identifying
SDB in elective postoperative patients by the use of a type
IV portable monitor (PM).
Methods Patients >18 years old who presented for elective
surgery with at least one postoperative hospital night on a
non-monitored unit were enrolled and wore a type IV
device that measured nasal flow, heart rate, and oxygen
saturation on their first postoperative night. Respiratory
disturbance index (RDI) and oxygen desaturation index
(ODI) were generated for each patient.
Results Data sufficient for interpretation were collected
on 100/116 patients enrolled. SDB (RDI 5) was
observed in 51% of the study group, and 17% had a
RDI >15. An elevated ODI 5 was seen in 42%, while
17% had an ODI 15. Device malfunction occurred in
16% of the study participants.
Conclusion A type IV PM can be employed in the postoperative setting to detect and gauge the severity of SDB.
This paper is presented at the American Thoracic Society National
Meeting 2008.
I. D. Weir : K. M. Ahmed : C. Manfredi : J. M. Fine :
S. M. Winter
Section of Pulmonary and Critical Care Medicine, Internal
Medicine, Norwalk Hospital,
Norwalk, CT, USA
K. M. Ahmed
e-mail: drkhaleel99@yahoo.com
C. Manfredi
e-mail: pulmcc@aol.com
S. Korbuly
Internal Medicine, Norwalk Hospital,
Norwalk, CT, USA
e-mail: steve.korbuly@norwalkhealth.org
E. OMalley
Optimal Sleep,
Easton, CT, USA
e-mail: eddom@gmail.com
J. M. Fine
e-mail: jonathan.fine@norwalkhealth.org
S. M. Winter
e-mail: stephen.winter@norwalkhealth.org
I. D. Weir : A. Achaen : M. OMalley : C. Manfredi
Sleep Section, Internal Medicine, Norwalk Hospital,
Norwalk, CT, USA
A. Achaen
e-mail: anilachaen@gmail.com
M. OMalley
e-mail: mary.ommm@gmail.com
D. B. Wakefield
University of Connecticut Health Center,
Farmington, CT, USA
e-mail: jewakefield@snet.net
I. D. Weir (*)
Norwalk Hospital Sleep Disorders Center,
24 Stevens Street,
Norwalk, CT 06854, USA
e-mail: ian.weir@norwalkhealth.org
882
Keywords Obstructive sleep apnea . Sleep-disordered
breathing . Portable monitoring . Oxygen . Postoperative
complications
Abbreviations
OSA
Obstructive sleep apnea
SDB
Sleep-disordered breathing
RDI
Respiratory disturbance index
AHI
Apnea hypopnea index
ODI
Oxygen desaturation index
CPAP
Continuous positive airway pressure
BMI
Body mass index
MEND Morphine equivalent narcotic dose
Sleep Breath (2012) 16:881886
devices, however, is that postoperative patients frequently
receive oxygen via nasal cannula, which could obscure
the measurement of nasal flow. This barrier could be
potentially overcome by employing a dual-lumen nasal
catheter for simultaneous delivery of oxygen and measurement of air flow, although this solution has not been
well examined. In this study, we examine the feasibility
of using a type IV device, including dual-lumen nasal
catheters for patients receiving supplemental oxygen, in
postoperative patients to detect respiratory disturbances
characteristic of SDB.
Methods
Study sample
Background
Postoperative sleep-disordered breathing (SDB) has
garnered major attention due to concern that this widely
underdiagnosed disorder leads to postoperative complications and is associated with difficult intubations [1].
Screening tools have been proposed that depend on the
identification of recognized risk factors for SDB, including clinical signs such as hypertension, symptoms, and
abnormal overnight oximetry [1]. Issues exist, however,
concerning the validity of these screening tools for
identification of patients at risk for postoperative SDB.
Missing from the traditional risk factors, for example, but
present after surgery are the lingering effects of narcotics
and sedatives as well as the changes in rapid eye
movement sleep [2]. Validation of these screening tools,
moreover, has relied on association with postoperative
complications, which can be difficult to assign to SDB
rather than to related comorbid conditions or on polysomnography (PSG) prior to surgery. The underlying
assumption with the latter is that the identification of
SDB by polysomnography in the preoperative state
suffices to predict the occurrence of respiratory disturbances indicative of SDB in the immediate postoperative
state. To actually prove that this assumption is true,
postoperative SDB must be identified, which would be a
daunting task using the gold standard of PSG.
An alternative method to full-scale PSG for identifying
SDB is the use of a multichannel type IV portable testing
devices that detect respiratory disturbances characteristic of
SDB by measuring nasal air flow, oximetry, and heart rate
and an actigraph to record movement as a surrogate for
wakefulness. These type IV devices have been approved for
home testing and may be more workable in the postoperative environment because of ease of set up and minimal
intrusiveness. A potential barrier to the use of type IV
The study was approved by the institutional review board at
Norwalk Hospital. Over a 9-month period, we recruited
stable postsurgical patients older than 18 years old who
presented to a university-affiliated community teaching
hospital for an elective surgery with an expected stay on
the general surgical floor of at least one postoperative night.
Patients were excluded if they refused to participate, had
nasal packing or any other reason why nasal flow could not
be measured, were clinically unstable including requiring a
higher level of care postoperatively (telemetry or ICU), or
were currently on continuous positive airway pressure
(CPAP) at home. Enrolled patients wore a Medcare
(currently Embla) Compass type IV device (Reykjavik,
Iceland) on the first postoperative night that measured
nasal flow by a nasal pressure transducer, heart rate,
and oxygen saturation. This device shares the internal
components of the Embletta X10 device and uses
RemLogic software system. Patients were placed on
oxygen by a respiratory therapist postoperatively if
oxygen saturation was <92% on room air at the time
of device initiation. The flow rate was then titrated by
the respiratory therapist to achieve an oxygen saturation
above 92%. A dual-lumen cannula (Salter Lab, Arvin,
CA, USA) allowed nasal flow to be measured while on
supplemental oxygen (not to exceed 5 l/min). Testing of
the dual-lumen cannula in three patients undergoing
overnight polysomnography in our sleep laboratory
revealed no changes in flow signal with supplemental
oxygen up to a flow rate of 5 l/min.
Measure of postoperative respiratory disturbance index
The portable device was placed on the patient by a
respiratory therapist between the hours of 8 and
11 p.m. and removed from the patient at 7 a.m. the
Sleep Breath (2012) 16:881886
following morning. A total recording time of at least
6 h was required for the study to be considered valid.
The data collected were used to generate a respiratory
disturbance index (RDI) defined as the number of
apnea or hypopnea events per hour of recorded time
minus the movement time, and oxygen desaturation
index (ODI) defined as the number of oxygen desaturation events of greater or equal to 4% per hour of
recorded time minus the movement time. Movement
time (estimated wake time) was detected by the use of
a built-in actigraph. Nasal flow, heart rate, and oxygen
saturation data were prepared using Somologica software and scored by a physician with specialized training
in sleep medicine using preestablished criteria [3].
Apnea was defined as a greater than 90% reduction of
flow from baseline for 10 s and hypopnea was defined as a
30% reduction of flow for 10 s associated with a 4%
oxygen desaturation. Because we did not measure sleep
directly, we did not include respiratory effort-related
arousals in the RDI. Postoperative sleep-disordered
breathing was defined as a RDI 5 in accordance with
published guidelines [4].
Patient characteristics
Patient data were collected from the medical record and
included the following: patient demographics, personal
history of OSA, family history of OSA, BMI, type of
anesthesia, type of surgical procedure, length of surgery,
difficult intubation, oropharyngeal exam, neck circumference, Mallampati score, and past medical history including
cardiac and pulmonary disease. Also, abstracted was the
anesthesiologist's impression of whether OSA was present.
No formal screening tool was used. Sedative medications
including narcotics and benzodiazepines given over 24 h
from surgery were recorded. The morphine equivalent
narcotic dose (MEND) score, tabulated as milligrams of
morphine equivalent over 24 h, was calculated for each
patient.
Postoperative complications were assessed by the use of
electronic chart review and discharge diagnosis International Statistical Classification of Diseases and Related
Health Problems (ICD-9) codes. Electronic chart and ICD-9
code review were blinded to the results of the portable
monitoring. A complication was said to occur if any one
of the following occurred during the hospitalization after
the planned procedure: reintubation, acute hypercapnia
(PaCO2 >45), use of noninvasive ventilation, postoperative
pneumonia, myocardial infarction or ischemia, cardiac
arrhythmia, unplanned transfer to higher level of care
(ICU or telemetry), or death. The association between
either RDI or ODI and patient characteristics was per-
883
formed by using the Pearson chi2 bivariate analysis or two
sample t test with equal variances.
Results
Study sample and patient characteristics
A total of 214 outpatients were evaluated for inclusion in
the study. Ninety patients refused to participate in the study.
Others were excluded because of device malfunction prior
to initiation of data collection (n=3), concern for latex
allergy (n=1), and device not available (n=4). No patient
overtly refused to wear the device after being attached.
Among the 116 patients tested, 16 patients (2 with the dual
cannula) had a flow signal recording insufficient for
interpretation, resulting in 100 (86%) patients with adequate monitoring data for at least 6 h. Most were female
(77%) and the mean SD for age was 5815.4 years
(Table 1). Among the 100 patients included in the study, 44
patients required oxygen postoperatively and were studied
with a dual-lumen cannula with an average oxygen flow
rate of 2.5 l/min. The average dose of midazolam
administered over 24 h was 2.31.4 mg. Only 4 of 100
patients received midazolam in the post anesthesia care unit
or surgical ward. Twenty-one patients were included in the
study after undergoing laparoscopic banding procedures
and were not previously diagnosed with SDB or using
CPAP. The mean SD of RDI and ODI for all patients was
8.812.3 and 7.710.1, respectively. The mean SD (in
percent) for time <90% saturation and lowest oxygen
saturation for all patients was 8.0%17.5 and 85.3%6.4,
respectively (see Table 2). No consistent association was
observed between known risk factors for SDB and both
ODI >5 and RDI >5 except for age (p = .001). No
association between MEND score and RDI was observed
(p=0.43).
Fifty-one of the 100 patients evaluated had evidence of
SDB with an RDI 5, one third of whom had an RDI >15
(Table 2). One patient had a personal history of OSA and
was not using CPAP. All 100 patients were screened for
OSA by the anesthesiologist prior to surgery and 5 patients
were thought by the anesthesiologist to have OSA. There
were four difficult intubations
No increase in the serious complication rate occurred
among patients with SDB compared with those without
SDB. Five (5%) patients had postoperative complications,
two of whom had evidence of SDB (RDI 5). Postoperative
pneumonia was diagnosed in one patient with SDB and two
patients without SDB. One patient with SDB required
reintubation the following day and one patient without SDB
was transferred to telemetry due to an arrhythmia. No
884
Sleep Breath (2012) 16:881886
Table 1 Patient characteristics
All patients
Number of subjects
Age (SD)
Gender (% female)
Pulmonary disease (%)
Cardiovascular disease (%)
Sleep-disordered breathing risk factors
Hypertension (%)
Body mass index (SD)
Neck circumference 17 in. (%)
Mallampatti class of 3 or 4 (%)
Type of surgery
Orthopedic (%)
Laparoscopic band (%)
Gynecological/urological (%)
Thoracic/abdominal (%)
Other (%)
Type of anesthesia
Spinal anesthesia (%)
General anesthesia (%)
Patient-controlled anesthesia (%)
Median length of surgery (range) (h)
Morphine equivalent narcotic dose
in the first 24 h (mean mg SD)
American Society of Anesthesiologists
physical status classification>class 2
(mild systemic disease) (%)
complication was diagnosed during the recording period,
and there were no deaths among the enrolled patients.
Discussion
These results show that the use of a type IV monitoring device
to detect respiratory disturbances suggestive of SDB is
feasible in postoperative patients, including those requiring
No oxygen
100
5815.4
76
7
56
56
5715.5
68
5
54
45
31.47.7
18
15
40
30.37.3
16
16
Oxygen
44
6015.1
86
9
59
52
32.98.1
20
14
34
22
17
27
20
23
43
25
9
13
14
16
14
9
14
30
70
26
2.45 (14.5)
57.435.4
18
82
5.3
2.27 (14.5)
59.832.5
25
19
45
55
53
2.7 (1.14.4)
54.530.1
32
supplemental oxygen via nasal cannula. All patients agreeing
to participate in the study tolerated wearing the cannula and
actigraph, further supporting the use of this monitoring device.
This method, therefore, appears suitable for monitoring
postoperative patients to determine whether the types of
complications reported are plausibly related to SDB and to
give better estimates of the prevalence of this problem.
Although this was strictly a feasibility study, we
observed that among the selected patient population
Table 2 Postoperative sleep-disordered breathing and oxygenation
Classification
Sleep-disordered breathing
Respiratory disturbance index 5 (%)
Respiratory disturbance index >15 (%)
Mean RDI SD
Oxygenation
Oxygen desaturation index 5 (%)
Oxygen desaturation index >15 (%)
Mean ODI SD
Mean SD time <90% saturation (%)
Mean SD lowest oxygen saturation (%)
All patients (n=100)
No oxygen (n=56)
Oxygen (n=44)
51
17
8.812.3
62
20
10.312.5
36
14
6.89.2
42
17
7.710.1
8.017.5
85.36.4
55
21
7.511.3
14.87.3
84.67.6
25
11
4.97.5
1.42.7
85.95.6
Sleep Breath (2012) 16:881886
studied, 51% had an abnormal RDI and, among these, 33%
had an RDI greater than 15. These rates are considerably
higher than the prevalence estimate in the general outpatient
population [5]. Additionally, a recent study of patients
presenting for ambulatory surgery by Collop and colleagues
identified only 4.8% of patients at high risk for OSA [6]. Our
population of patients, however, may not be representative of
all non-critically ill postoperative patients because approximately half of the eligible patients refused to participate. No
postoperative complications, moreover, occurred among the
patients while they were being monitored. Nonetheless, the
elevated prevalence rate noted raises concern that the first
postoperative night surgical population comprises a high risk
group for sleep-disordered breathing.
Flow measurement characteristics from the dual-lumen
catheter were excellent. Although patients wearing the duallumen catheter had risk factors for SDB similar to those
wearing the single-lumen catheter, they were significantly
less likely to have an abnormal RDI. This finding is not
surprising given that the calculation of RDI is partially
dependent on oxygen saturation measurement. Whether
supplemental oxygen also provides a protective effect or
simply masquerades the apneas in this setting is unknown.
Furthermore, it is possible that oxygen may prolong apneas
by decreasing the arousal threshold and, thereby, worsen
the severity of the sleep-disordered breathing at the same
time that the RDI may be lowered.
Current recommendations from the American Society for
Anesthesiologists call for identification of OSA using
traditional risk factors, physical findings, and past medical
history and for the scoring of OSA severity based on PSG.
PSG results, in concert with the type of surgery and
postoperative narcotic use, are recommended for postoperative risk stratification [1]. In our study, anesthesiologists
preoperatively identified only 5% of the patients found to
have postoperative SDB despite screening all patients,
highlighting the poor predictive value of clinical impression
alone. The STOP-Bang scoring system has been proposed
as a screening tool for preoperative patients and has been
validated for identifying OSA patients outside of the
hospital setting with a negative predictive value of 83.6%
for apnea hypopnea index (AHI) >5 and 92.9% for AHI
>15%, among the 51% of patients agreeing to be studied
[7]. Although plausible, these methods of screening and
scoring have not been validated for the immediate
postoperative setting. The use of the type IV monitoring
device would allow the reasonable determination of
whether patients with SDB in the postoperative setting
can be accurately identified and their severity estimated
with these screening methods. It is worth noting that no
prospective study has shown that a screening program
followed by the provision of positive airway pressure
reduces the hazards associated with postoperative SDB.
885
Further studies are also needed to characterize the risk of
postoperative complications in patients with SDB and to
determine the effect of postoperative positive airway
pressure. Given the very high prevalence of SDB found in
our postoperative patients, we speculate that some of our
patients had SDB associated only with the type of
physiologic conditions associated with the postoperative
state and might not have had a diagnosis of SDB made with
measurements in the preoperative period. Further, most
known risk factors and MEND score were not associated
with SDB in this study, although our patient population
may have been underpowered to detect such associations.
Follow-up PSG data were not collected on the study
patients and, therefore, the long-term health risks from
postoperative SDB are unclear. This potential group of
patients with transient demonstration of SDB might not
share the same risk for postoperative complications as those
with more chronic cardiovascular stress. Moreover, the
absence of chronic compensatory responses may place this
population at even greater risk. This is an important
question for future studies.
Limitations of this study include our inability to
distinguish central from obstructive apneas because effort
belts could not be employed in this postoperative population. We, therefore, use the more general term of sleepdisordered breathing, accepting actigraphy as a valid
method of estimating sleep. It is also unclear if making
such a distinction between central and obstructive apneas
would be useful in assessing postoperative complication
risk. Portable devices may also overestimate or underestimate the AHI when compared to overnight PSG. [8, 9]
Although movement time was excluded, it is possible we
counted apneas or hypopneas that did not occur in sleep.
More likely, however, we may have overestimated the total
sleep time and, as a result, may have underestimated the
RDI. It should also be recognized that PM has not been
validated with PSG postoperatively and that setting specific
variables may affect the diagnostic reliability of PM. An
additional caveat is the high refusal rate to participate in
the study, which is not surprising given the expected
discomfort experienced by these patients and is a likely
issue for any postoperative study. Inadequate duration of
study and device malfunction was observed in 19 of the 116
patients agreeing to be studied, which is consistent with the
findings in other studies employing similar portable devices
[10].
In conclusion, our pilot study shows that a type IV
device can be employed in the postoperative setting to
detect and gauge the severity of SDB. For patients requiring
supplemental oxygen via nasal cannula, a dual cannula can
be employed to detect flow; however, RDI may be
artificially reduced by the prevention of oxygen desaturation by the supplemental oxygen. Further studies are
886
feasible using such methods to determine the accuracy of
proposed postoperative SDB screening tools and to determine what special risk factors for OSA that surgery may
impose.
Sleep Breath (2012) 16:881886
4.
5.
Disclosure There is no financial support, conflict of interest, and
off-label or investigational use to disclose.
References
1. American Society of Anesthesiologists Task Force on Perioperative Management of Obstructive Sleep Apnea (2006) Practice
guidelines for the perioperative management of patients with
obstructive sleep apnea: a report by the American Society of
Anesthesiologists Task Force on Perioperative Management of
patients with obstructive sleep apnea. Anesthesiology 104:1081
1093
2. Kaw R, Michota F, Jaffer A, Ghamande S, Auckley D, Golish J
(2006) Unrecognized sleep apnea in the surgical patient: implications for the perioperative setting. Chest 129:198205
3. Iber C, Ancoli-Israel S, Chesson A, Quan SF, American Academy
of Sleep Medicine (2007) The AASM manual for the scoring of
sleep and associated events: rules, terminology and technical
6.
7.
8.
9.
10.
specifications, 1st edn. American Academy of Sleep Medicine,
Westchester
American Academy of Sleep Medicine Task Force (1999) Sleeprelated breathing disorders in adults: recommendations for
syndrome definition and measurement techniques in clinical
research. Sleep 22:667689
Punjabi NM (2008) The epidemiology of adult obstructive sleep
apnea. Proc Am Thorac Soc 5:136143
Stierer TL, Wright CW, George A, Thompson RE, Wu CL, Collop
N (2010) Risk assessment of obstructive sleep apnea in a
population of patients undergoing ambulatory surgery. J Clin
Sleep Med 6(5):467472
Chung F, Yegneswaran B, Liao P, Chung SA, Vairavanathan S,
Islam S, Khajehdehi A, Shapiro CM (2008) STOP questionnaire:
a tool to screen patients for obstructive sleep apnea. Anesthesiology 108:812821
Liesching TN, Carlisle C, Marte A, Bonitati A, Millman FP
(2004) Evaluation of the accuracy of SNAP technology sleep
sonography in detecting obstructive sleep apnea in adults
compared to standard polysomnography. Chest 125:886891
Chesson AL, Berry RB, Pack A (2003) Practice parameters for the
use of portable monitoring devices in the investigation of
suspected obstructive sleep apnea in adults. Sleep 26:907913
Skomro RP, Gjevre J, Reid J, McNab B, Ghosh S, Stiles M,
Jokic R, Ward H, Cotton D (2010) Outcomes of home-based
diagnosis and treatment of obstructive sleep apnea. Chest
138:257263
Reproduced with permission of the copyright owner. Further reproduction prohibited without permission.
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1091)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Reliance Individual Mediclaim Policy ScheduleDocument1 pageReliance Individual Mediclaim Policy ScheduleKoushik Dutta38% (13)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- George P. Prigatano-Principles of Neuropsychological Rehabilitation PDFDocument375 pagesGeorge P. Prigatano-Principles of Neuropsychological Rehabilitation PDFTlaloc Gonzalez100% (7)
- TOEFL Practice Test ITP PDFDocument9 pagesTOEFL Practice Test ITP PDFAndi Suchy Qumala SariePas encore d'évaluation
- Assessment A - Project Tasks (1) CompletedDocument5 pagesAssessment A - Project Tasks (1) Completednazifa zahid100% (2)
- SPA - PRC IdDocument3 pagesSPA - PRC IdGracelyn Enriquez Bellingan67% (6)
- Starbucks Managing High Growth BrandDocument15 pagesStarbucks Managing High Growth BrandSumit BansalPas encore d'évaluation
- Physics of The Solid Earth (Phy 202)Document11 pagesPhysics of The Solid Earth (Phy 202)Gaaga British0% (1)
- Vascular TraumaDocument16 pagesVascular TraumaAndi Suchy Qumala SariePas encore d'évaluation
- 2012 Carnevale D. PI3K in Hypertension A Novel Therapeutic Target Controlling Vascular Myogenic Tone and Target Organ DamageDocument6 pages2012 Carnevale D. PI3K in Hypertension A Novel Therapeutic Target Controlling Vascular Myogenic Tone and Target Organ DamageAndi Suchy Qumala SariePas encore d'évaluation
- 2012 Akif M. Structural Basis of Peptide Recognition by The Angiotensin 1 Converting Enzyme Homologue AnCE From Drosophila MelanogasterDocument10 pages2012 Akif M. Structural Basis of Peptide Recognition by The Angiotensin 1 Converting Enzyme Homologue AnCE From Drosophila MelanogasterAndi Suchy Qumala SariePas encore d'évaluation
- 2012 Akif M. Structural Basis of Peptide Recognition by The Angiotensin 1 Converting Enzyme Homologue AnCE From Drosophila MelanogasterDocument10 pages2012 Akif M. Structural Basis of Peptide Recognition by The Angiotensin 1 Converting Enzyme Homologue AnCE From Drosophila MelanogasterAndi Suchy Qumala SariePas encore d'évaluation
- Endocrine Reviews UndanaDocument132 pagesEndocrine Reviews UndanaAndi Suchy Qumala SariePas encore d'évaluation
- BIOKIMIA Regulation of Neurotransmitters in Neuropsychiatric SystemDocument83 pagesBIOKIMIA Regulation of Neurotransmitters in Neuropsychiatric SystemAndi Suchy Qumala SariePas encore d'évaluation
- 2.syok Hipovolemik-Dr - Andi Salahuddin, SP - AnDocument37 pages2.syok Hipovolemik-Dr - Andi Salahuddin, SP - AnAndi Suchy Qumala SariePas encore d'évaluation
- Pancreatitis 1Document29 pagesPancreatitis 1Andi Suchy Qumala SariePas encore d'évaluation
- Valvular Heart Disease:: Ambulatory Monitoring and Surgical ReferralDocument56 pagesValvular Heart Disease:: Ambulatory Monitoring and Surgical ReferralAndi Suchy Qumala SariePas encore d'évaluation
- Children Infected & Affected By: Hiv/ AidsDocument13 pagesChildren Infected & Affected By: Hiv/ AidsAndi Suchy Qumala SariePas encore d'évaluation
- Nutrition: A Co-Factor in HIV Infection/AIDS Progression: Phara Jourdan Rosabelle CamposDocument54 pagesNutrition: A Co-Factor in HIV Infection/AIDS Progression: Phara Jourdan Rosabelle CamposAndi Suchy Qumala SariePas encore d'évaluation
- WSD Dextra: - Produksi: 200cc/ 24 Jam - Expiratory Bubble: - Air Bubble: - Undulasi: +Document1 pageWSD Dextra: - Produksi: 200cc/ 24 Jam - Expiratory Bubble: - Air Bubble: - Undulasi: +Andi Suchy Qumala SariePas encore d'évaluation
- Expiratory Bubble: - Respiratory Bubble: - Undulasi: +Document1 pageExpiratory Bubble: - Respiratory Bubble: - Undulasi: +Andi Suchy Qumala SariePas encore d'évaluation
- HIV/AIDS Instruction: California Comprehensive Sexual Health and HIV/AIDS Prevention Education ActDocument31 pagesHIV/AIDS Instruction: California Comprehensive Sexual Health and HIV/AIDS Prevention Education ActAndi Suchy Qumala SariePas encore d'évaluation
- Pregnancy and Heart DiseaseDocument60 pagesPregnancy and Heart DiseaseAndi Suchy Qumala SariePas encore d'évaluation
- Epsom Salt ClassDocument7 pagesEpsom Salt ClassSofia marisa fernandesPas encore d'évaluation
- Guidance ProgramDocument4 pagesGuidance ProgramShainajoy BoterPas encore d'évaluation
- DB-En 19 R-2-829 PDFDocument4 pagesDB-En 19 R-2-829 PDFashokPas encore d'évaluation
- The Logarithmic Properties Active and Passive Mandibular GrowthDocument20 pagesThe Logarithmic Properties Active and Passive Mandibular GrowthThe Reading CrabPas encore d'évaluation
- All Polyurea SystemsDocument20 pagesAll Polyurea SystemsRaheel AsgharPas encore d'évaluation
- Quarterly Test - Q3 English 9Document6 pagesQuarterly Test - Q3 English 9Rodrigl BaiganPas encore d'évaluation
- How To Wash Off Our Negative Karmas (Sins) : AbhinavDocument6 pagesHow To Wash Off Our Negative Karmas (Sins) : Abhinavmg2000105820Pas encore d'évaluation
- Lect. 2 - Silvics - Silviculture and Locaility FactorsDocument14 pagesLect. 2 - Silvics - Silviculture and Locaility FactorsNaga Varshini MeenakshisundaramPas encore d'évaluation
- Sample - Global Pharmaceutical Contract Manufacturing Outsourcing (CMO) Market - Mordor IntelligenceDocument54 pagesSample - Global Pharmaceutical Contract Manufacturing Outsourcing (CMO) Market - Mordor IntelligenceSilke IgemannPas encore d'évaluation
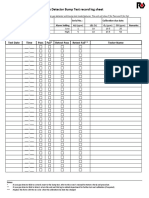
- Gas Detector Bump Test Record Log Sheet: Bump Test Result Test Date Time Pass Fail Retest Pass Retest Fail Tester NameDocument2 pagesGas Detector Bump Test Record Log Sheet: Bump Test Result Test Date Time Pass Fail Retest Pass Retest Fail Tester NameAndry Kurnia100% (2)
- Nissan RPX80 Vs Crown PE4500Document13 pagesNissan RPX80 Vs Crown PE4500Forklift Systems IncorporatedPas encore d'évaluation
- Business Ethics ANSWERSDocument3 pagesBusiness Ethics ANSWERSMỹ HàPas encore d'évaluation
- 2300 - Performing The EngagementDocument1 page2300 - Performing The EngagementAlexandra AvîrvareiPas encore d'évaluation
- Lecture 06 What Is Avalanche and Causes of Avalanche CSS PMS General Science and AbilityDocument13 pagesLecture 06 What Is Avalanche and Causes of Avalanche CSS PMS General Science and Abilityabdul samiPas encore d'évaluation
- Checklist of Eligibility Requirements For Consulting ServicesDocument2 pagesChecklist of Eligibility Requirements For Consulting ServicesAndrea BroccoliPas encore d'évaluation
- Literature Review Devin KilburnDocument4 pagesLiterature Review Devin Kilburnapi-549230129Pas encore d'évaluation
- 2015 Pri XLDocument2 pages2015 Pri XLTimmyJuriPas encore d'évaluation
- ClaireDocument24 pagesClaireMariclaire LibasPas encore d'évaluation
- Road To Sustainable SHG-Bank Linkage Programme: Formulating Strategies For Managing Credit Risk With Respect To Rural BengalDocument6 pagesRoad To Sustainable SHG-Bank Linkage Programme: Formulating Strategies For Managing Credit Risk With Respect To Rural BengalAnimesh TiwariPas encore d'évaluation
- AcknowledgementDocument2 pagesAcknowledgementSonali SinghPas encore d'évaluation
- Division of Humanities: Use and Convert To PDF File This Format Every Time You Will Submit Your Activity To VLEDocument3 pagesDivision of Humanities: Use and Convert To PDF File This Format Every Time You Will Submit Your Activity To VLEIane Jhazzlee MapilePas encore d'évaluation
- Red Oxide PrimerDocument2 pagesRed Oxide Primermarsha.fsdPas encore d'évaluation
- Dysphagia in Lateral Medullary Syndrome ObjavljenDocument10 pagesDysphagia in Lateral Medullary Syndrome ObjavljenMala MirnaPas encore d'évaluation
- TwoStep Linkage SSP9028 v10Document1 pageTwoStep Linkage SSP9028 v10David BriggsPas encore d'évaluation