Académique Documents
Professionnel Documents
Culture Documents
Cefoperazone
Transféré par
Baim FarmaDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Cefoperazone
Transféré par
Baim FarmaDroits d'auteur :
Formats disponibles
Name /bks_53161_deglins_md_disk/cefoperazone
02/19/2014 01:03PM
cefoperazone (sef-oh-per-a-zone)
to penicillins.
Use Cautiously in: Hepatic/biliary impairment or combined hepatic/biliary/renal
Classification
Therapeutic: anti-infectives
Pharmacologic: third-generation cephalosporins
Pregnancy Category B
impairment (dosep/qdosing interval recommended); Patients with poor nutritional
status, malabsorption states, or alcoholism (may be atqrisk of bleeding); History of
GI disease, especially colitis; OB, Lactation: Has been used safely.
Indications
Treatment of the following infections caused by susceptible organisms: Skin and skin
structure infections, Urinary tract infections, Gynecological infections including gonorrhea, Respiratory tract infections, Intra-abdominal infections, Septicemia.
Action
Binds to the bacterial cell wall membrane, causing cell death. Therapeutic Effects: Bactericidal action against susceptible bacteria. Spectrum: Similar to that of
second-generation cephalosporins, but activity against staphylococci is less, while
activity against gram-negative pathogens is greater, even for organisms resistant to
first- and second-generation agents. Notable is increased action against: Citrobacter,
Enterobacter, Haemophilus influenzae, Escherichia coli, Klebsiella pneumoniae,
Morganella morganii, Neisseria gonorrhoeae, Proteus, Providencia, Pseudomonas aeruginosa, Serratia. Has some activity against enterococci. Has some activity against anaerobes, includingBacteroides fragilis.
Pharmacokinetics
Absorption: Well absorbed following IM administration; IV administration results
in complete bioavailability.
Distribution: Widely distributed. Crosses the placenta; enters breast milk in low
concentrations. CSF penetration better than with first- and second-generation agents.
Protein Binding: 90%.
Metabolism and Excretion: Excreted in bile.
Half-life: 2 hr.
Adverse Reactions/Side Effects
CNS: SEIZURES (high doses). GI: PSEUDOMEMBRANOUS COLITIS, diarrhea, nausea,
vomiting. Derm: rashes, urticaria. Hemat: bleeding, eosinophilia, neutropenia.
Local: pain at IM site, phlebitis at IV site. Misc: allergic reactions including ANAPHYLAXIS, superinfection.
Interactions
Drug-Drug: Ingestion of alcohol within 48 72 hr of cefoperazone may result in a
disulfiram-like reaction. May potentiate the effects of anticoagulants andqrisk of
bleeding. Concurrent use of loop diuretics or aminoglycosides mayqrisk of
nephrotoxicity.
Route/Dosage
IM, IV (Adults): Mild to moderate infections 1 2 g every 12 hr. Severe infections 2 4 g q 8 hr or 1.5 3 g every 6 hr.
Hepatic Impairment
IV (Adults): Impaired hepatic function/biliary obstruction daily dose should
not exceed 4 g; combined hepatic and renal impairment daily dose should not
exceed 1 2 g.
NURSING IMPLICATIONS
Assessment
Assess for infection (vital signs; appearance of wound, sputum, urine, and stool;
WBC) at beginning of and throughout therapy.
Before initiating therapy, obtain a history to determine previous use of and reac-
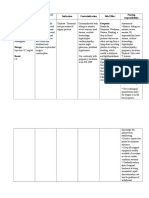
TIME/ACTION PROFILE (blood levels)
ROUTE
ONSET
PEAK
DURATION
IM
IV
rapid
rapid
12 hr
end of infusion
12 hr
12 hr
Genetic Implication.
pg 1 # 1
Contraindications/Precautions
Contraindicated in: Hypersensitivity to cephalosporins; Serious hypersensitivity
Canadian drug name.
Plate # 0-Composite
tions to penicillins or cephalosporins. Persons with a negative history of penicillin
sensitivity may still have an allergic response.
Obtain specimens for culture and sensitivity before initiating therapy. First dose
may be given before receiving results.
CAPITALS indicate life-threatening, underlines indicate most frequent.
Strikethrough Discontinued.
PDF Page #1
Name /bks_53161_deglins_md_disk/cefoperazone
02/19/2014 01:03PM
2
Observe patient for signs and symptoms of anaphylaxis (rash, pruritus,
laryngeal edema, wheezing). Discontinue the drug and notify health
care professional immediately if these symptoms occur. Keep epinephrine, an antihistamine, and resuscitation equipment close by in the event
of an anaphylactic reaction.
Monitor bowel function. Diarrhea, abdominal cramping, fever, and
bloody stools should be reported to health care professional promptly
as a sign of pseudomembranous colitis. May begin up to several weeks
following cessation of therapy.
Lab Test Considerations: May cause positive results for Coombs test.
Monitor prothrombin time and assess patient for bleeding (guaiac stools; check
for hematuria, bleeding gums, ecchymosis) daily in high-risk patients; may cause
hypoprothrombinemia.
May causeqserum AST, ALT, alkaline phosphatase, bilirubin, LDH, BUN, and creatinine.
May rarely cause neutropenia and eosinophilia.
Potential Nursing Diagnoses
Risk for infection (Indications) (Side Effects)
Diarrhea (Adverse Reactions)
Implementation
IM: Reconstitute IM doses with sterile or bacteriostatic water for injection or 0.9%
NaCl for injection. May be diluted with lidocaine to minimize injection discomfort.
Inject deep into a well-developed muscle mass; massage well.
IV Administration
pH: 4.5 6.5.
IV: Monitor injection site frequently for phlebitis (pain, redness, swelling).
Change sites every 48 72 hr to prevent phlebitis.
If aminoglycosides are administered concurrently, administer in separate sites, if
possible, at least 1 hr apart. If second site is unavailable, flush lines between medications.
Intermittent Infusion: Reconstitute each gram with 5 mL of sterile or bacteriostatic water for injection, 0.9% NaCl, or D5W. Shake vigorously and allow to stand
for visualization and clarity. Solution may be colorless to straw-colored. Diluent:
Plate # 0-Composite
pg 2 # 2
Further dilute each gram in 50 100 mL of 0.9% NaCl, D5W, D10W, D5/0.25%
NaCl, D5/0.9% NaCl, D5/LR, or lactated Ringers solution. Solution is stable for 24
hr at room temperature and 5 days if refrigerated. Rate: Administer over 15 30
min.
Y-Site Compatibility: acyclovir, alfentanil, allopurinol, aminophylline, ascorbic
acid, atropine, aztreonam, bivalirudin, bumetanide, buprenorphine, butorphanol, calcium gluconate, carboplatin, cefazolin, cefotaxime, cefotetan, cefoxitin, ceftazidime, ceftriaxone, cefuroxime, chloramphenicol, cisplatin, clindamycin,
cyanocobalamin, cyclophosphamide, cyclosporine, cytarabine, dactinomycin,
dexamethasone, dexmedetomidine, digoxin, docetaxel, enalaprilat, epinephrine,
epoetin alfa, eptifibatide, etoposide, etoposide phosphate, fenoldopam, fentanyl,
fluconazole, fludarabine, fluorouracil, folic acid, foscarnet, furosemide, glycopyrrolate, granisetron, heparin, hydrocortisone, hydromorphone, ifosfamide, imipenem/cilastatin, isoproterenol, ketorolac, lidocaine, linezolid, mannitol, mechlorethamine, melphalan, methotrexate, methylprednisolone, metoclopramide,
metoprolol, metronidazole, multivitamins, nafcillin, naloxone, nitroglycerin, nitroprusside, norepinephrine, oxacillin, oxytocin, paclitaxel, penicillin G, pentobarbital, phenobarbital, phenylephrine, phytonadione, potassium chloride, procainamide, propofol, propranolol, ranitidine, rituximab, sodium acetate, sodium
bicarbonate, streptokinase, succinylcholine, sufentanil, tacrolimus, teniposide,
theophylline, thiotepa, ticarcillin/clavulanate, vasopressin, vincristine.
Y-Site Incompatibility: amifostine, amikacin, amphotericin B cholesteryl, amphotericin B liposome, atracurium, azathioprine, benztropine, calcium chloride,
caspofungin, chlorpromazine, cimetidine, cisatracurium, codeine, dantrolene,
diazepam, diazoxide, diphenhydramine, dobutamine, dopamine, doxacurium,
doxorubicin(, doxorubicin liposome, doxycycline, epirubicin, filgrastim, ganciclovir, gemcitabine, gentamicin, haloperidol, hydralazine, hydroxyzine, idarubicin, indomethacin, insulin, labetalol, levofloxacin, meperidine, metaraminol, methoxamine, methyldopate, midazolam, mitoxantrone, nalbuphine, nesiritide,
nicardipine, ondansetron, oxaliplatin, pantoprazole, papaverine, pentamidine,
pentazocine, perphenazine, phentolamine, phenytoin, prochlorperazine, promethazine, protamine, pyridoxime, quinupristin/dalfopristin, rocuronium, sargramostim, thiamine, tobramycin, tolazoline, trastuzumab, trimetaphan, trimethoprim/sulfamethoxazole, vancomycin, verapamil, vinorelbine.
Patient/Family Teaching
Advise patient to report signs of superinfection (furry overgrowth on the tongue,
vaginal itching or discharge, loose or foul-smelling stools) and allergy.
2015 F.A. Davis Company
CONTINUED
PDF Page #2
Name /bks_53161_deglins_md_disk/cefoperazone
02/19/2014 01:03PM
Plate # 0-Composite
pg 3 # 3
3
PDF Page #3
CONTINUED
cefoperazone
Caution patients that concurrent use of alcohol with cefoperazone may cause a di-
sulfiram-like reaction (abdominal cramps, nausea, vomiting, headache, hypotension, palpitations, dyspnea, tachycardia, sweating, flushing). Alcohol and alcoholcontaining medications should be avoided during and for several days after
therapy.
Instruct patient to notify health care professional if fever and diarrhea
develop, especially if stool contains blood, pus, or mucus. Advise patient
not to treat diarrhea without consulting health care professional.
Evaluation/Desired Outcomes
Resolution of the signs and symptoms of infection. Length of time for complete res-
olution depends on the organism and site of infection.
Why was this drug prescribed for your patient?
Canadian drug name.
Genetic Implication.
CAPITALS indicate life-threatening, underlines indicate most frequent.
Strikethrough Discontinued.
Vous aimerez peut-être aussi
- CefotaximeDocument3 pagesCefotaximeMargotPas encore d'évaluation
- CeftriaxoneDocument5 pagesCeftriaxoneCastillo MikaellaPas encore d'évaluation
- AcetazolamideDocument3 pagesAcetazolamideGwyn RosalesPas encore d'évaluation
- Drug Study Dopamine HCLDocument2 pagesDrug Study Dopamine HCLA.Pas encore d'évaluation
- Metronidazole 500mg/tab 1 Tab 3xadayDocument4 pagesMetronidazole 500mg/tab 1 Tab 3xadayCrisyl LipawenPas encore d'évaluation
- Cyclobenzaprine Hydrochloride (Drug Study)Document1 pageCyclobenzaprine Hydrochloride (Drug Study)Franz.thenurse6888Pas encore d'évaluation
- Drug Study For FractureDocument4 pagesDrug Study For FractureitsmeayaPas encore d'évaluation
- Drug SDocument2 pagesDrug SJane CasiquinPas encore d'évaluation
- Pilocarpine (Drug Monograph)Document1 pagePilocarpine (Drug Monograph)Muhammad ArsalanPas encore d'évaluation
- Atropine SulfateDocument1 pageAtropine SulfateTrishaaMayolPas encore d'évaluation
- Tramadol Drug StudyDocument2 pagesTramadol Drug StudyTipey Segismundo0% (1)
- Magnesium Oxide (Antacid, Anti-Convulsant, Electrolyte, Laxative)Document1 pageMagnesium Oxide (Antacid, Anti-Convulsant, Electrolyte, Laxative)Danielle Marie SamblacenoPas encore d'évaluation
- Aspirin: Generic NameDocument4 pagesAspirin: Generic NameGwww BabababaPas encore d'évaluation
- Act Rapid 2Document2 pagesAct Rapid 2Leah Torcelino-InfantePas encore d'évaluation
- EsmololDocument2 pagesEsmololtherock316_995149Pas encore d'évaluation
- CetirizineDocument1 pageCetirizineGabby Robles PajePas encore d'évaluation
- Generic Name: Brand Name:: ClassificationsDocument2 pagesGeneric Name: Brand Name:: ClassificationsbillyktoubattsPas encore d'évaluation
- Check The Physician's Observe and Follow The 14 Warn The Mother AboutDocument2 pagesCheck The Physician's Observe and Follow The 14 Warn The Mother AboutJust nowPas encore d'évaluation
- Drug Study Bsn3aDocument3 pagesDrug Study Bsn3aEmuelle GanPas encore d'évaluation
- Duty Drug Study'sDocument7 pagesDuty Drug Study'sGrape JuicePas encore d'évaluation
- Generic Name: Classification: IndicationDocument2 pagesGeneric Name: Classification: IndicationKristine YoungPas encore d'évaluation
- Filgastrim (GCSF)Document3 pagesFilgastrim (GCSF)Kyla Barrera TabungarPas encore d'évaluation
- Nursing Care Plan ADocument6 pagesNursing Care Plan ACrystal WyattPas encore d'évaluation
- NimodipineDocument5 pagesNimodipineGwyn Rosales100% (1)
- Subcutaneous Injection: Humalog U-100 or U-200: More CommonDocument2 pagesSubcutaneous Injection: Humalog U-100 or U-200: More Commonahmad ryanPas encore d'évaluation
- Drug AnalysisDocument3 pagesDrug AnalysisAbby BorabienPas encore d'évaluation
- SHEENA Clomid Drug StudyDocument3 pagesSHEENA Clomid Drug StudyNur SetsuPas encore d'évaluation
- AldactoneDocument2 pagesAldactoneianecunarPas encore d'évaluation
- Nursing Responsibility Adverse Effects Machanism of Action Drug NameDocument2 pagesNursing Responsibility Adverse Effects Machanism of Action Drug NameSalwa ZeinPas encore d'évaluation
- Drug Mechanism of Action/side Effects Indication/ Contraindication Nursing ResponsibilitiesDocument1 pageDrug Mechanism of Action/side Effects Indication/ Contraindication Nursing ResponsibilitiesSheryhan Tahir BaylePas encore d'évaluation
- Generic Name & Brand Name Mechanism of Action Indications and Drug Rationale Contraindications Common Side Effects Nursing ConsiderationsDocument2 pagesGeneric Name & Brand Name Mechanism of Action Indications and Drug Rationale Contraindications Common Side Effects Nursing ConsiderationsMary Shine GonidaPas encore d'évaluation
- Drug Classification Mechanism of Action Indications Contraindications Side Effects/ Adverse Effects Nursing ConsiderationsDocument2 pagesDrug Classification Mechanism of Action Indications Contraindications Side Effects/ Adverse Effects Nursing ConsiderationsFranz Earl Niño AlbesaPas encore d'évaluation
- Drug Tabulation orDocument23 pagesDrug Tabulation orChin Villanueva UlamPas encore d'évaluation
- Silver Sulfadiazine Drug StudyDocument3 pagesSilver Sulfadiazine Drug StudyKenn Siasar100% (1)
- Drug Study OrthoDocument4 pagesDrug Study OrthoJhessa Curie Pitagan100% (1)
- Epirubicin 10Document1 pageEpirubicin 10PdianghunPas encore d'évaluation
- AmilorideDocument1 pageAmilorideRox San100% (1)
- CHN Drug StudyDocument17 pagesCHN Drug StudyEdmel Pamplona DuquesaPas encore d'évaluation
- Colistin/ Colistimethate SodiumDocument2 pagesColistin/ Colistimethate SodiumnonamePas encore d'évaluation
- Drug StudyDocument4 pagesDrug StudyJeboy SadioaPas encore d'évaluation
- Oraa, Jamie - Drug Study Surgical WardDocument1 pageOraa, Jamie - Drug Study Surgical WardJamie LeePas encore d'évaluation
- Urokinase Dosage WheelDocument2 pagesUrokinase Dosage WheelNidhiPas encore d'évaluation
- Drug Name Mecahnism of Action Indication Side Effects Generic NameDocument2 pagesDrug Name Mecahnism of Action Indication Side Effects Generic NamehahahaPas encore d'évaluation
- Amoxicillin Tri Hydrate Table FormatDocument3 pagesAmoxicillin Tri Hydrate Table FormatNico DonatoPas encore d'évaluation
- Noradrenaline (Norepinephrine) : 1mg/mLDocument5 pagesNoradrenaline (Norepinephrine) : 1mg/mLBrian RelsonPas encore d'évaluation
- FINAL Drug StudyDocument2 pagesFINAL Drug StudycasedraftPas encore d'évaluation
- Discharge PlanDocument4 pagesDischarge PlanVillanueva NiñaPas encore d'évaluation
- Tinidazole Drug StudyDocument2 pagesTinidazole Drug StudyEmagra AzilPas encore d'évaluation
- IsoketDocument2 pagesIsoketJaessa FelicianoPas encore d'évaluation
- Drug Study CaseDocument3 pagesDrug Study CaseKatrina Ponce100% (1)
- Drug Study 1 (Done)Document3 pagesDrug Study 1 (Done)Otaku MiyoPas encore d'évaluation
- Drug Study: Name of PatientDocument1 pageDrug Study: Name of PatientKaloy KamaoPas encore d'évaluation
- NeostigmineDocument4 pagesNeostigmineDonna Lyn B. DizonPas encore d'évaluation
- Generic Name: Mebeverine Hydrochloride Mechanism of Action Side Effects/ Adverse Reaction Nursing Responsibility Assessment & Drug EffectsDocument4 pagesGeneric Name: Mebeverine Hydrochloride Mechanism of Action Side Effects/ Adverse Reaction Nursing Responsibility Assessment & Drug EffectsNiziu BearsPas encore d'évaluation
- AcetazolamideDocument2 pagesAcetazolamideAlexandra Antondy0% (1)
- Drug Study - CefotaximeDocument5 pagesDrug Study - CefotaximeAngel laurestaPas encore d'évaluation
- CaptoprilDocument2 pagesCaptoprilJohn Louie EscardaPas encore d'évaluation
- Antibiotic Penicillin: Ampicillin Ampicillin Sodium AmpicillinDocument3 pagesAntibiotic Penicillin: Ampicillin Ampicillin Sodium AmpicillinMaria Delia SalvadoPas encore d'évaluation
- Cefoxitin Sodium MefoxinDocument3 pagesCefoxitin Sodium MefoxinKristi WrayPas encore d'évaluation
- Drug Study Mefenamic Acid and CephalexinDocument5 pagesDrug Study Mefenamic Acid and CephalexinRoselle Soriano100% (3)
- 241 245 PDFDocument5 pages241 245 PDFBaim FarmaPas encore d'évaluation
- 2014 - Guidelines For Safety in The Gastrointestinal Endoscopy Unit PDFDocument10 pages2014 - Guidelines For Safety in The Gastrointestinal Endoscopy Unit PDFBaim FarmaPas encore d'évaluation
- Helicobacter Pylori: Eradication - An Update On The Latest TherapiesDocument5 pagesHelicobacter Pylori: Eradication - An Update On The Latest TherapiesBaim FarmaPas encore d'évaluation
- Certificate of Analysis: LactoseDocument1 pageCertificate of Analysis: LactoseBaim FarmaPas encore d'évaluation
- Certificate of Analysis: C H FO 392.47 White Solid DMSO To 100 MM Store at RTDocument2 pagesCertificate of Analysis: C H FO 392.47 White Solid DMSO To 100 MM Store at RTBaim FarmaPas encore d'évaluation
- Cephalosporins Pharmacology and ChemistryDocument5 pagesCephalosporins Pharmacology and ChemistryIrfan QaisarPas encore d'évaluation
- Microbiology, Infections, and Antibiotic Therapy: Elizabeth J. Rosen, MD Francis B. Quinn, MD March 22, 2000Document86 pagesMicrobiology, Infections, and Antibiotic Therapy: Elizabeth J. Rosen, MD Francis B. Quinn, MD March 22, 2000skmvicky1483Pas encore d'évaluation
- TerrexineDocument5 pagesTerrexineWakhidatus InryaPas encore d'évaluation
- List of AntibioticsDocument10 pagesList of AntibioticsAia JavierPas encore d'évaluation
- Antibiotics For Urinary Tract Infections: Nani MaharaniDocument45 pagesAntibiotics For Urinary Tract Infections: Nani MaharaniMelinda FiskaPas encore d'évaluation
- Drug Study - CefuroximeDocument2 pagesDrug Study - CefuroximeErika Jane EsperanzaPas encore d'évaluation
- Cell Wall Synthesis - BacterialProteinSynthesis - AntimicrobialsDocument99 pagesCell Wall Synthesis - BacterialProteinSynthesis - AntimicrobialsJoslin Roz GalileaPas encore d'évaluation
- Ancef Drug CardDocument1 pageAncef Drug CardSheri490Pas encore d'évaluation
- Importance of Intrinsic ResistanceDocument2 pagesImportance of Intrinsic ResistanceGeozel ViviennePas encore d'évaluation
- Drug StudyDocument6 pagesDrug Studyjohnclement_dcPas encore d'évaluation
- Drug Study MixDocument29 pagesDrug Study MixMatty JolbitadoPas encore d'évaluation
- Analgesics & Antibiotics in Pediatric DentistryDocument77 pagesAnalgesics & Antibiotics in Pediatric DentistryJanani Gopalakrishnan100% (3)
- Community Acquired Pneumonia (CAP)Document48 pagesCommunity Acquired Pneumonia (CAP)lei2x100% (1)
- Actinomycets 1Document12 pagesActinomycets 1Manohar PattarPas encore d'évaluation
- Pulmonary PharmaDocument242 pagesPulmonary Pharmaarturo quevedoPas encore d'évaluation
- Prophylactic Antibiotics in Hip and Knee ArthroplastyDocument11 pagesProphylactic Antibiotics in Hip and Knee ArthroplastySara Aly YoussefPas encore d'évaluation
- Drug Study 68-75Document8 pagesDrug Study 68-75joshua_santiago_5Pas encore d'évaluation
- Obat - BMDocument50 pagesObat - BMNovita PermataPas encore d'évaluation
- Antibiotics Lecture 3 - CarbapenemsDocument22 pagesAntibiotics Lecture 3 - CarbapenemsRenas SalayPas encore d'évaluation
- Allergy Evaluation For Immediate Penicillin Allergy: Skin Test-Based Diagnostic Strategies and Cross-Reactivity With Other Beta-Lactam AntibioticsDocument29 pagesAllergy Evaluation For Immediate Penicillin Allergy: Skin Test-Based Diagnostic Strategies and Cross-Reactivity With Other Beta-Lactam Antibioticsthao hoangPas encore d'évaluation
- CephalosporinsDocument35 pagesCephalosporinslakshmiuniq100% (1)
- Lista Clsi 2016Document1 pageLista Clsi 2016Nelson BerriosPas encore d'évaluation
- Drug StudyDocument7 pagesDrug StudyKarol Ann RodriguezPas encore d'évaluation
- Cefuroxomine Drug StudyDocument3 pagesCefuroxomine Drug StudyNiziu BearsPas encore d'évaluation
- Ceftriaxone: Antibiotic ClassDocument2 pagesCeftriaxone: Antibiotic ClassTanjung PrabandariPas encore d'évaluation
- Drug Study - AmpicillinDocument2 pagesDrug Study - Ampicillinliza sianPas encore d'évaluation
- Degradation of: ββ-lactam antibioticsDocument12 pagesDegradation of: ββ-lactam antibioticsMuhammad Azam TahirPas encore d'évaluation
- Name and Classification of DrugDocument3 pagesName and Classification of DrugAnicas, Ralph Joshua V.Pas encore d'évaluation
- Drug Study NurseryDocument2 pagesDrug Study Nurseryjulesubayubay54280% (1)
- Cephalexin Use While BreastfeedingDocument8 pagesCephalexin Use While BreastfeedingTilahun MikiasPas encore d'évaluation