Académique Documents
Professionnel Documents
Culture Documents
Thyroid Storm: An Unusual Presentation: Case Report
Transféré par
play_wright2084Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Thyroid Storm: An Unusual Presentation: Case Report
Transféré par
play_wright2084Droits d'auteur :
Formats disponibles
C A S E
R E P O R T
JIACM 2014; 15(3-4): 222-3
Thyroid storm: An unusual presentation
NS Neki*
Abstract
A 23-year-old female patient was hospitalised with complaints of fever, diarrhoea, altered sensorium for 3 days with a rapidly
declining mental status. Before admission to the hospital, her relatives gave history of her being restless, markedly irritable with
generalised tonic-clonic seizures and a positive history of palpitations. Suspecting the diagnosis of thyroid storm clinically, she
was started on aggressive antithyroid treatment following which she showed marked clinical improvement. Thyroid storm is a
rare endocrine emergency with increased mortality risk in this otherwise fatal entity. The aim of reporting this case is to make the
physicians aware of this fatal medical disease necessitating prompt intervention. A case of thyroid storm presenting with
predominant neurological manifestations is being presented here for its rarity.
Key words: Thyroid storm, unusual presentation.
Introduction
Thyroid storm (accelerated hyperthyroidism) is a rare
manifestation of thyrotoxicosis with a wide spectrum of
clinical presentations involving multiple systems. It
generally occurs in females from the third to the sixth
decade of life, especially with Graves disease. It is usually
a life-threatening medical emergency and is fatal if left
untreated. The classic clinical presentation includes fever,
tachycardia, hypertension, tremors, nausea, vomiting,
diarrhoea, dehydration, arrhythmias, delirium, and coma1.
It usually develops in an undiagnosed hyperthyroid
patient who has a major stress or continues without
antithyroid treatment in addition to other precipitating
factors like surgery, radio-iodine therapy, trauma, acute
infection toxaemia of pregnancy, labour, excessive
palpation of the thyroid gland in hyperthyroid patients,
pulmonary thromboembolism, severe drug reactions, or
myocardial infarction, etc 2. Its early recognition and
treatment is essential in reducing the morbidity and
mortality rate in this potentially fatal disease. Only 1 - 2%
of hyperthyroid cases manifest as thyroid storm and the
mortality ranges between 20 - 30% despite treatment3.
Case report
A 23-year-old unmarried female was brought to the
hospital with complaints of fever, diarrhoea, light
headedness, altered sensorium for 3 days with a rapidly
declining mental status. Before admission, she was
reported to be restless, markedly irritable with generalised
tonic clonic seizures as well as positive history of
palpitations as narrated by relatives.
There was no history of previous illness or hospital
admission, major surgery, or antipsychotic drugs intake. On
examination, she was febrile (temp 101F), pulse rate 126/
min and regular, BP 110/70 mmHg, respiratory rate 29
breaths/mm, oxygen saturation 98% on 3L. Her pupils were
slightly dilated, mucous membranes were moist and the
she had an abrasion on the tongue consistent with biting.
JVP was normal; there was no lymphadenopathy.
Examination of the neck revealed bilateral thyroid
enlargement with diffuse toxic goitre with systolic bruit
heard over it. She had a stare with a typical anxious look.
There were no signs of meningeal irritation. Fundus
examination was normal. On neurological examination, she
responded to painful stimuli, with brisk deep tendon
reflexes and plantar flexor response. CVS examination
revealed tachycardia with regular rhythm but no murmurs.
Respiratory system and abdominal examination was
unremarkable. ECG showed sinus tachycardia. Her
laboratory results showed no abnormality of haemogram,
blood glucose levels, CSF, serum electrolytes, renal and liver
function tests. X-ray chest showed no active disease. CT
brain was normal. Blood cultures were negative. EEG
revealed bilateral frontal slow waves. Technetium scan of
thyroid showed hyperfunctioning gland with diffuse tracer
uptake (36% at 20 minutes). The constellation of signs and
symptoms suggested that this could be a case of thyroid
storm. Based on the diagnostic criteria of Burch and
Wartofsky4, she had a total score of 60, which was strongly
suggestive of thyroid storm (a score > 25 is suggestive of
thyroid storm). The patient was put on antithyroid drugs
awaiting thyroid function tests T3, T4, and TSH. She was
started on propylthiouracil 400 mg tid and propranolol 40
mg tid, IV fluids, hydrocortisone IV (later changed to oral
steroids). Her thyroid profile revealed TSH 0.02 mIU/ml, T4
28 g/dl (N 4 - 14 g/dl); T3 40 ng/dl (N = 0.8 - 2 ng/dl).
Thyroid peroxidase autoantibody was negative. Based on
*Professor of Medicine, Government Medical College, Amritsar, Punjab, and Trained Endocrinologist, Department of
Endocrinology, PGIMER, Chandigarh; and President, Geriatric Society of India.
clinical presentation and later on confirmed by results,
Lugols iodine 8 drops 8 hourly was given for 3 days. The
fever subsided, diarrhoea improved, and agitation
decreased. After considerable improvement in her
condition in about 8 days time, she was discharged in an
euthyroid state, conscious, well oriented, without tremors
and fever, and advised to continue on propylthiouracil and
propranolol. On follow-up at 3 months, she was carrying
our all routine activities with a positive frame of mind.
Discussion
Thyroid storm a dramatic exacerbation of existing
hyperthyroidism, of sudden onset associated with fever,
tachycardia, and CNS symptomatology remains a lifethreatening medical emergency if left untreated. Being a
rare endocrine emergency, all clinicians must be aware of
its clinical features and treatment so that morbidity and
mortality can be avoided. About 1 - 2% of patients with
hyperthyroidism progress to thyroid storm and the 100%
mortality reported earlier has now come down to 20 - 30%
with better recognition and treatment. It might be difficult
to distinguish between thyroid storm and infection in
thyrotoxic patients as tachycardia and fever might be
present in both. On account of an overlapping of the
symptoms, precipitating conditions and complications, a
clinical diagnosis is not easy and is often made too late.The
definitive criteria of thyroid storm laid down by Burch and
Wartotsky4 are useful. The triggering factors for thyroid
storm include surgery, major stress, noncompliance to
antithyroid drugs, infection, radio-iodine, etc2. Treatment
of thyroid storm should not be delayed if there is a high
index of suspicion, and empirical treatment should be
started on clinical grounds awaiting laboratory reports,
which was evident in our case5. Urgent thyroid function tests
is a confirmatory diagnosis. Hyperglycaemia,
hypercalcaemia, leucocytosis may co-exist. Deranged liver
functions mainly alkaline phosphatase may occur due to
increased osteoblastic activity in response to high bone
resorption. Serum thyroid hormone levels would typically
show hyperthyroidism, but due to an abrupt rise of thryoid
hormone secondary to triggering factors, the patient can
no longer adapt to the sudden metabolic stress6. An acute
elevation of FT3 or FT4 in thyrotoxic patients may produce
acute decompensation. However, no absolute levels of
serum T3 or T4 exist above which thyroid storm develops
inevitably.7 Earlier, cases of thyroid storm have been well
reported where treatment of thyroid storm was started
immediately awaiting thyroid function tests8,9. T4 may rarely
be normal or even decreasing because of co-existing
nonthyroidal illness10.
In our case, the patient presented with altered sensorium
without signs of raised intracranial tension and focal
neurological deficit. Differential diagnosis includes
Journal, Indian Academy of Clinical Medicine
neuroleptic malignant syndrome, anticholinergic poisoning,
sympathomimetic toxicity, alcohol withdrawal syndrome,
toxic/metabolic encephalopathy, hypertensive
encephalopathy, meningitis, etc. But the clinical features of
our patient in the form of hypermetabolic state made
thyroid storm a definitive diagnosis; and possibly the
triggering factor for thyroid storm in this case could be
febrile illness. Predominant neurological manifestation in
the form of altered mental status and history of tonic clonic
generalised seizures was an unusual feature in our case.
Treatment of thyroid storm includes correction of severe
thyrotoxicosis, precipitating illness, and associated active
thyroid eye disease. Patients should be monitored in the
intensive care units in the early phase. Diuretics may be
given for congestive cardiac failure (CHF). Drugs like
thionamides block hormone synthesis; iodine solution
blocks the release of thyroid hormone, beta-blockers
control adrenergic symptoms, and steroids reduce T4 to T3
conversion. Beta-blockers should be used cautiously in the
presence of CHF. Among thionamides, propylthiouracil is
preferred over methionazole as it blocks peripheral T4 to
T3 conversion. Iodinated radiocontrast iopanoic acid,
cholestyramine can also be used. Peritoneal dialysis and
plasmaphresis are used to reduce the high levels of
circulating T4 and T3 in a thyroid storm5,9,10.
Conclusion
Diagnosis may be missed on account of variable
presentation. Treatment should never be delayed. A high
index of suspicion is required for prompt recognition and
effective management of unusual presentation of thyroid
storm in order to reduce the morbidity and mortality of
this life-threatening medical disorder.
References
1.
2.
Graqvin LA. Thyroid crises. Med Clin North Am 1991; 75: 179-93.
Nqo SY, Chew HC. When the storm passes unnoticed - a case series
of thyroid storm. Resuscitation 2007; 73 (3): 485-90.
3. Waldstein SS, Slodki SJ et al. A clinical study of thyroid storm. Ann
Intern Med 1960; 52: 626-42.
4. Burch HB, Wartofsky L. Life-Threatening thyrotoxicosis: Thyroid
storm. Endocrinol Metab Clin North Am 1993; 22: 263-77.
5. Ingbar S. Management of emergencies: Thyroid storm. N Engl J
Med 1996; 274: 1253-4.
6. Hehrmann R. Thyrotoxic crisis: Pitfalls in diagnosis intensive
therapy. Fortschr Med 1996; 14 (10): 114-17.
7. Jiang YZ, Hutchinson KA et al. Thyroid storm presenting as
multiorgan dysfunction syndrome. Chest 2000; 118 (3): 877-9.
8. Bindu M, Harinarayana CV, Vengmma B. A lady with acute
confessional state and generalised tremors: a case report. JIACM
2005; 6 (1): 76-8.
9. Ahmed Rishad, Patil S, Basanagouda. Thyroid storm. An unusual
presentation. Al Am En J Med Sci 2008; 1: 55-7.
10. Birkhauser M, Busset R et al. Diagnosis of hyperthyroidism when
serum thyroxine alone is raised. Lancet 1997; 2:43.
Vol. 15, No. 3 & 4
July-December, 2014
223
Vous aimerez peut-être aussi
- Organization of NICU ServicesDocument45 pagesOrganization of NICU ServicesMonika Bagchi84% (64)
- HyperthyroidismDocument18 pagesHyperthyroidismWahyuni FatmonaPas encore d'évaluation
- Thyroid Storm: An Acute Life-Threatening Hypermetabolic StateDocument11 pagesThyroid Storm: An Acute Life-Threatening Hypermetabolic StateAndrew UtamaPas encore d'évaluation
- Electrocardiography for Healthcare ProfessionalsDocument6 pagesElectrocardiography for Healthcare ProfessionalsOasisBogo Med0% (1)
- AJMS Thyroid StormDocument3 pagesAJMS Thyroid StormHildaPas encore d'évaluation
- Thyroid Storm Diagnosis and Treatment ChallengesDocument7 pagesThyroid Storm Diagnosis and Treatment ChallengesKarl Angelo MontanoPas encore d'évaluation
- Thyroid StormDocument36 pagesThyroid StormSabrina ShalhoutPas encore d'évaluation
- Thyroid It IsDocument16 pagesThyroid It IsRoby KieranPas encore d'évaluation
- THYROID DISORDERS CASE REPORT DETAILS RARE THYROTROPIN-SECRETING PITUITARY ADENOMADocument1 pageTHYROID DISORDERS CASE REPORT DETAILS RARE THYROTROPIN-SECRETING PITUITARY ADENOMAAnca LunguPas encore d'évaluation
- Tormenta Tiroidea: Una Urgencia Endocrinológica: Thyroid Storm: An Endocrinological UrgencyDocument4 pagesTormenta Tiroidea: Una Urgencia Endocrinológica: Thyroid Storm: An Endocrinological UrgencyConstanza Moraga HerreraPas encore d'évaluation
- Hydatidiform Mole With Hyperthyroidism - Perioperative ChallengesDocument2 pagesHydatidiform Mole With Hyperthyroidism - Perioperative ChallengesAl MubartaPas encore d'évaluation
- 7381-Article Text-34752-1-10-20230316Document10 pages7381-Article Text-34752-1-10-20230316jihan OktafianiPas encore d'évaluation
- MyxedemaDocument3 pagesMyxedemaBobet ReñaPas encore d'évaluation
- Subacute, Silent, and Postpartum Thyroiditis 2012Document11 pagesSubacute, Silent, and Postpartum Thyroiditis 2012YoaNnita GoMezPas encore d'évaluation
- PDF document-CD8968C1BAE7-1Document22 pagesPDF document-CD8968C1BAE7-1Sean SialanaPas encore d'évaluation
- Thyroid Gland McqsDocument6 pagesThyroid Gland Mcqssabreena.samad.ssPas encore d'évaluation
- Endocrine CasesDocument12 pagesEndocrine Casesعلي. احمدPas encore d'évaluation
- Background: Excessive Release of Thyroid Hormones (THS) Hypertension Congestive Heart FailureDocument8 pagesBackground: Excessive Release of Thyroid Hormones (THS) Hypertension Congestive Heart FailureIkmal HazliPas encore d'évaluation
- Background: Excessive Release of Thyroid Hormones (THS) Hypertension Congestive Heart FailureDocument13 pagesBackground: Excessive Release of Thyroid Hormones (THS) Hypertension Congestive Heart FailureFebria ArmaPas encore d'évaluation
- Bao 2012Document3 pagesBao 2012Salim MichaelPas encore d'évaluation
- Thornton 2016Document5 pagesThornton 2016AfdhalRuslanPas encore d'évaluation
- Tiroides en Critico 2015 LancetDocument10 pagesTiroides en Critico 2015 LancetElias Vera RojasPas encore d'évaluation
- Thyroid Storm and Hyperthyroidism - CorePendiumDocument17 pagesThyroid Storm and Hyperthyroidism - CorePendiumSajeewaniePas encore d'évaluation
- ThyroidDocument12 pagesThyroidrpjaymaPas encore d'évaluation
- Jaundice As A Presentation of Thyrotoxic CrisisDocument3 pagesJaundice As A Presentation of Thyrotoxic CrisisRizki AmeliaPas encore d'évaluation
- Tyroid StormDocument10 pagesTyroid StormAfdhalia Khairunnisa SyammarhanPas encore d'évaluation
- Thyroid Storm May Be The Initial Presentation Of: Thyrotoxicosis in Undiagnosed Children, Particularly in NeonatesDocument8 pagesThyroid Storm May Be The Initial Presentation Of: Thyrotoxicosis in Undiagnosed Children, Particularly in NeonatesLolla MorsiPas encore d'évaluation
- Euthyroid Sick Syndrome - Endocrine and Metabolic Disorders - Merck Manuals Professional EditionDocument2 pagesEuthyroid Sick Syndrome - Endocrine and Metabolic Disorders - Merck Manuals Professional Editionram7676Pas encore d'évaluation
- Emergencias EndocrinasDocument6 pagesEmergencias EndocrinasAlex Andrés Cuevas UrriolaPas encore d'évaluation
- Thyroid+Storm+ +StatPearls+ +NCBI+Bookshelf 1666577389538Document9 pagesThyroid+Storm+ +StatPearls+ +NCBI+Bookshelf 1666577389538Novita Sri MulyatiPas encore d'évaluation
- Thyroid Storm - UpToDateDocument21 pagesThyroid Storm - UpToDateJENNYLA HAZEL SICLOTPas encore d'évaluation
- THYROID DISORDERS: CAUSES AND SYMPTOMS OF HYPOTHYROIDISMDocument4 pagesTHYROID DISORDERS: CAUSES AND SYMPTOMS OF HYPOTHYROIDISMVictor VicencioPas encore d'évaluation
- Management of Subclinical Hyperthyroidism: Special Feature EditorialDocument3 pagesManagement of Subclinical Hyperthyroidism: Special Feature EditorialimorkzonePas encore d'évaluation
- Hyperthyoidism: Anaesthetic ManagementDocument11 pagesHyperthyoidism: Anaesthetic ManagementerzaraptorPas encore d'évaluation
- Thyroid Emergencies: Siddharth N ShahDocument1 pageThyroid Emergencies: Siddharth N ShahSubramanian MurugesanPas encore d'évaluation
- Crisis ThyroidDocument10 pagesCrisis ThyroidimanPas encore d'évaluation
- Sheehan Syndrome Sarina SchragerDocument3 pagesSheehan Syndrome Sarina Schragerfreddyop72Pas encore d'évaluation
- Atow 496 00 01Document9 pagesAtow 496 00 01Nguyen Ngoc ChungPas encore d'évaluation
- Euthyroid Sick SyndromeDocument3 pagesEuthyroid Sick Syndromemonday125Pas encore d'évaluation
- 2750-Article Text-14541-1-10-20231222Document4 pages2750-Article Text-14541-1-10-20231222Asti NuriatiPas encore d'évaluation
- References: Hyperthyroidism Due To Graves-Basedow Disease in A Woman Refractory To Thyroid HormonesDocument3 pagesReferences: Hyperthyroidism Due To Graves-Basedow Disease in A Woman Refractory To Thyroid Hormoneshenry hernandezPas encore d'évaluation
- Mbs127 Slide Hyperthyroidism 1Document46 pagesMbs127 Slide Hyperthyroidism 1revita262Pas encore d'évaluation
- Thyrotoxic Periodic Paralysis-A Misleading ChallenDocument8 pagesThyrotoxic Periodic Paralysis-A Misleading ChallenBianca ChiriacPas encore d'évaluation
- Hypertension Urgency and EmergencyDocument8 pagesHypertension Urgency and EmergencySanditia GumilangPas encore d'évaluation
- Hypokalemic Periodic Paralysis CaseDocument3 pagesHypokalemic Periodic Paralysis Caseghieliyani spPas encore d'évaluation
- Krisis Tiroid FixDocument38 pagesKrisis Tiroid FixVita DesriantiPas encore d'évaluation
- Wo Week 4 (Hyperthyroidism)Document12 pagesWo Week 4 (Hyperthyroidism)Theddyon BhenliePas encore d'évaluation
- Case 8 Keracunan TCADocument8 pagesCase 8 Keracunan TCAIlham JauhariPas encore d'évaluation
- Man Passed Out Due to TCA OverdoseDocument8 pagesMan Passed Out Due to TCA OverdoseIlham JauhariPas encore d'évaluation
- Pathology I Review 10Document30 pagesPathology I Review 10i_areinamoPas encore d'évaluation
- Laboratory Assesment of Thyroid Function PMC2003Document14 pagesLaboratory Assesment of Thyroid Function PMC2003Muhammad Dadan KurniawanPas encore d'évaluation
- HypothyrodismDocument1 pageHypothyrodismkabal321Pas encore d'évaluation
- Diagnosis and treatment of hypothyroidismDocument10 pagesDiagnosis and treatment of hypothyroidismHanzla IrfanPas encore d'évaluation
- Perioperative Management of The Thyrotoxic PatientsDocument16 pagesPerioperative Management of The Thyrotoxic PatientsHub storePas encore d'évaluation
- Let's Talk About Thyroid PDFDocument92 pagesLet's Talk About Thyroid PDFEidi IdhamPas encore d'évaluation
- RTH 1Document3 pagesRTH 1Ei DrakorPas encore d'évaluation
- ThyrotoxicosisDocument16 pagesThyrotoxicosisFiorella Peña MoraPas encore d'évaluation
- Managing Thyroid Storm in a Pregnant PatientDocument10 pagesManaging Thyroid Storm in a Pregnant PatientAulia CahyaniPas encore d'évaluation
- Thyroid Gland Functions and Disorders ExplainedDocument35 pagesThyroid Gland Functions and Disorders ExplainedEdwin OkonPas encore d'évaluation
- Finalized Case Report JZS 11.20.21Document10 pagesFinalized Case Report JZS 11.20.21Gaming With ShafPas encore d'évaluation
- Euthyroid Sick Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsD'EverandEuthyroid Sick Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsPas encore d'évaluation
- Skin Cancer BrochDocument8 pagesSkin Cancer Brochplay_wright2084Pas encore d'évaluation
- TOLL FREE NOsDocument7 pagesTOLL FREE NOsSushil DhawalePas encore d'évaluation
- Thyroid Eye Disease - Protruding, IrritatedeyesDocument1 pageThyroid Eye Disease - Protruding, Irritatedeyesplay_wright2084Pas encore d'évaluation
- Ann Oncol 2012 Pacini Vii110 9Document10 pagesAnn Oncol 2012 Pacini Vii110 9play_wright2084Pas encore d'évaluation
- ATA DTC Guidelines 2009Document51 pagesATA DTC Guidelines 2009이호원Pas encore d'évaluation
- HypothyroidismDocument5 pagesHypothyroidismplay_wright2084Pas encore d'évaluation
- 9780723434276Document12 pages9780723434276Kashphia ZamanPas encore d'évaluation
- Daily Diabetes Meal Planning GuideDocument8 pagesDaily Diabetes Meal Planning GuidelilianaenPas encore d'évaluation
- The Diagnosis and Management of Primary Hypothyroidism Revised Statement 14 June 2011 2Document4 pagesThe Diagnosis and Management of Primary Hypothyroidism Revised Statement 14 June 2011 2play_wright2084Pas encore d'évaluation
- WIC PEPB 344 ThyroidDsrdrs05 11Document5 pagesWIC PEPB 344 ThyroidDsrdrs05 11play_wright2084Pas encore d'évaluation
- The Diagnosis and Management of Primary Hypothyroidism Revised Statement 14 June 2011 2Document4 pagesThe Diagnosis and Management of Primary Hypothyroidism Revised Statement 14 June 2011 2play_wright2084Pas encore d'évaluation
- Thyroid Function Tests - Managing Side Effects - ChemocareDocument4 pagesThyroid Function Tests - Managing Side Effects - Chemocareplay_wright2084Pas encore d'évaluation
- Ata Hypothyroidism BrochureDocument3 pagesAta Hypothyroidism Brochureplay_wright2084Pas encore d'évaluation
- Daily Diabetes Meal Planning GuideDocument8 pagesDaily Diabetes Meal Planning GuidelilianaenPas encore d'évaluation
- Nutritional Management of DiabetesDocument74 pagesNutritional Management of Diabetesplay_wright2084Pas encore d'évaluation
- Pink Panther - Diabetes Management - Chapter 12Document22 pagesPink Panther - Diabetes Management - Chapter 12jennmoyer100% (1)
- Negative Effects of Cabbage - Healthy Eating - SF GateDocument5 pagesNegative Effects of Cabbage - Healthy Eating - SF Gateplay_wright2084Pas encore d'évaluation
- Ashlesa NakshatraDocument8 pagesAshlesa Nakshatraplay_wright2084Pas encore d'évaluation
- Ardra NakshatraDocument8 pagesArdra NakshatraANTHONY WRITER50% (2)
- APPI Guide To Health and Nutrition 2nd EditionDocument188 pagesAPPI Guide To Health and Nutrition 2nd Editionshivshekar100% (1)
- Progeny Case StudiesDocument45 pagesProgeny Case Studiesplay_wright2084Pas encore d'évaluation
- Kempenhaeghe 13 TH Epilepsy SleepDocument8 pagesKempenhaeghe 13 TH Epilepsy Sleepplay_wright20840% (1)
- VARGA D/10 or DASAMA "MAHAT PHALAM" DASAMSA OR KARMAMSA OR SWARGAMSADocument11 pagesVARGA D/10 or DASAMA "MAHAT PHALAM" DASAMSA OR KARMAMSA OR SWARGAMSAANTHONY WRITER100% (3)
- Epilepsy Syndromes and SleepDocument24 pagesEpilepsy Syndromes and Sleepplay_wright2084Pas encore d'évaluation
- Epilepsy Syndromes and SleepDocument24 pagesEpilepsy Syndromes and Sleepplay_wright2084Pas encore d'évaluation
- Type 2 Diabetes and DietDocument3 pagesType 2 Diabetes and Dietpratyusha201Pas encore d'évaluation
- Sleep in EpilepsyDocument8 pagesSleep in Epilepsyplay_wright2084Pas encore d'évaluation
- Sleep in EpilepsyDocument8 pagesSleep in Epilepsyplay_wright2084Pas encore d'évaluation
- Final File Hypo GuidelinesDocument41 pagesFinal File Hypo Guidelinesroatfatchuri100% (1)
- ThoracentesisDocument4 pagesThoracentesisCyntia Theresia Lumintang100% (1)
- Barge Clinic Visit Report SummaryDocument42 pagesBarge Clinic Visit Report SummaryNicoMichaelPas encore d'évaluation
- Nursing Care of a Patient with AppendicitisDocument3 pagesNursing Care of a Patient with AppendicitisKeisha BartolataPas encore d'évaluation
- Clinical Nursing Skills & TechniquesDocument6 pagesClinical Nursing Skills & TechniquesTimi BCPas encore d'évaluation
- History, Diagnosis and Treatment Planning in Removable Partial DenturesDocument96 pagesHistory, Diagnosis and Treatment Planning in Removable Partial DenturesPriya BagalPas encore d'évaluation
- Surgery and Surgical NursingDocument193 pagesSurgery and Surgical NursingFan Eli100% (4)
- A J B P R: Sian Ournal of Iochemical and Harmaceutical EsearchDocument5 pagesA J B P R: Sian Ournal of Iochemical and Harmaceutical EsearchNAVNEET BAGGAPas encore d'évaluation
- Metabolic EncephalopathyDocument22 pagesMetabolic Encephalopathytricia isabellaPas encore d'évaluation
- Varicella and Herpes ZosterDocument20 pagesVaricella and Herpes ZosterzakiPas encore d'évaluation
- How To Protect Yourself and OthersDocument2 pagesHow To Protect Yourself and OtherslistmyclinicPas encore d'évaluation
- Cutaneous MelanomaDocument226 pagesCutaneous MelanomaGriskalia ChristinePas encore d'évaluation
- PALS Helpful Hints 2015 Guidelines Posted Nov 2016Document5 pagesPALS Helpful Hints 2015 Guidelines Posted Nov 2016Mj Teate100% (1)
- Machine Learning Medical Imaging Market to Top $2 BillionDocument13 pagesMachine Learning Medical Imaging Market to Top $2 BillionFrado SibaraniPas encore d'évaluation
- Kuisioner Nutrisi Mini Nutritional AssessmentDocument1 pageKuisioner Nutrisi Mini Nutritional AssessmentNaufal AhmadPas encore d'évaluation
- Krok 2 2002-2003 TherapyDocument41 pagesKrok 2 2002-2003 TherapyAli ZeeshanPas encore d'évaluation
- Olivia Millsop - Case Study Docx 1202Document11 pagesOlivia Millsop - Case Study Docx 1202api-345759649Pas encore d'évaluation
- Cali Naturals CBDDocument7 pagesCali Naturals CBDSomya MishraPas encore d'évaluation
- Assessment of The Intermediate Care Unit Triage SystemDocument6 pagesAssessment of The Intermediate Care Unit Triage SystemJHPas encore d'évaluation
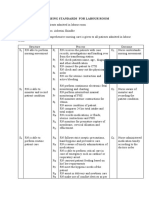
- Nursing Standards for Labour RoomDocument3 pagesNursing Standards for Labour RoomRenita ChrisPas encore d'évaluation
- 328 IndexDocument29 pages328 IndexDafi SanPas encore d'évaluation
- Lincomycin: Drug Information: ALERT: US Boxed WarningDocument12 pagesLincomycin: Drug Information: ALERT: US Boxed WarningsadiaPas encore d'évaluation
- Juvenile Idiopathic Arthritis (Jia) : IAP UG Teaching Slides 2015-16Document15 pagesJuvenile Idiopathic Arthritis (Jia) : IAP UG Teaching Slides 2015-16KathirPas encore d'évaluation
- N120 Final Review PDFDocument7 pagesN120 Final Review PDFsutopianoPas encore d'évaluation
- Nursing Diagnosis and Plan of Care for Anemia with Chronic DiseaseDocument6 pagesNursing Diagnosis and Plan of Care for Anemia with Chronic DiseaseChristine Joy FloresPas encore d'évaluation
- Infusion Pumps, Large-Volume - 040719081048Document59 pagesInfusion Pumps, Large-Volume - 040719081048Freddy Cruz BeltranPas encore d'évaluation
- Introduction To The Immune System: Lecture Day 1Document15 pagesIntroduction To The Immune System: Lecture Day 1blakePas encore d'évaluation
- Prevalence of Soil Transmitted Helminths infection in adults in North SulawesiDocument4 pagesPrevalence of Soil Transmitted Helminths infection in adults in North SulawesiSahrul hamidPas encore d'évaluation
- Medication Calculation Examination Study Guide: IV CalculationsDocument2 pagesMedication Calculation Examination Study Guide: IV Calculationswaqas_xsPas encore d'évaluation