Académique Documents
Professionnel Documents
Culture Documents
2004 - Leptin Signaling PDF
Transféré par
Cici21Description originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
2004 - Leptin Signaling PDF
Transféré par
Cici21Droits d'auteur :
Formats disponibles
Physiology & Behavior 81 (2004) 223 241
Leptin signaling
Rexford S. Ahima*, Suzette Y. Osei
Department of Medicine, Division of Endocrinology, Diabetes & Metabolism, University of Pennsylvania School of Medicine,
415 Curie Boulevard, 764 Clinical Research Building, Philadelphia, PA 19104, USA
Abstract
The discovery of leptin was a major breakthrough in our understanding of the role of adipose tissue as a storage and secretory organ.
Leptin was initially thought to act mainly to prevent obesity; however, studies have demonstrated profound effects of leptin in the response to
fasting, regulation of neuroendocrine and immune systems, hematopoiesis, bone and brain development. This review will focus on the
signaling pathways which mediate these diverse effects of leptin in the brain and other physiologic systems.
D 2004 Elsevier Inc. All rights reserved.
Keywords: Leptin; Obesity; Feeding; Hypothalamus; Neuropeptide
1. Early ideas on energy homeostasis
A connection between the brain and regulation of body
weight was first postulated, based on the observation that
tumors encroaching on the base of the brain caused
voracious appetite, morbid obesity, hypogonadism and
other hormonal abnormalities [65]. This so-called adiposus
genitalis syndrome, was initially attributed to pituitary
insufficiency; however, later studies pointed to disruption
of hypothalamic pathways [6,65,108]. Lesions of the
ventromedial hypothalamic (VMH) region resulted in
hyperphagia and morbid obesity, while lesions of the
lateral hypothalamic area (LHA) prevented spontaneous
feeding, leading to death from starvation [6,108]. These
observations provided an anatomic framework for the
dual center model of feeding regulation. It was postulated that a satiety center was present in the ventromedial hypothalamus while a feeding center was present
in the LHA [6,108]. However, the idea of discrete brain
centers for regulation of body weight was controversial, as
precise lesions of hypothalamic nuclei did not reproduce
the above phenotypes [65]. Nonetheless, these classic
experiments demonstrated a significant role of the brain
in energy homeostasis.
* Corresponding author. Tel.: +1-215-573-1872; fax: +1-215-5735809.
E-mail address: ahima@mail.med.upenn.edu (R.S. Ahima).
0031-9384/$ see front matter D 2004 Elsevier Inc. All rights reserved.
doi:10.1016/j.physbeh.2004.02.014
Humans and most mammals maintain a constant body
weight despite short-term fluctuations in feeding and energy
expenditure. Based on this observation, Kennedy [121]
proposed the existence of a physiologic system designed
to match energy intake to expenditure, with the goal of
keeping body weight, specifically fat, at a constant level.
This model was supported by studies in rodents, in which
forced overfeeding resulted in inhibition of voluntary feeding, whereas food deprivation or surgical removal of adipose tissue stimulated food intake until body weight was
restored [74,101 103]. Although it was proposed that a
factor emanating from adipose tissue signaled the brain to
regulate body weight and fat content, the chemical nature of
this substance remained elusive. Experiments by Hervey
[107] provided further insights into the link between adipose
tissue and the brain. He showed that cross-circulation
(parabiosis) between obese VMH-lesioned and normal (nonlesioned) rats resulted in suppression of feeding and weight
loss in the normal rat, while the VMH-lesioned partner
gained weight. In contrast, parabiosis of a pair of obese
VMH-lesioned rats did not prevent hyperphagia or weight
gain in either rat. These findings suggested that a circulating
satiety factor related to adipose tissue acted at the VMH to
suppress feeding and prevent obesity [107].
The notion that adipose tissue played an active role in
energy homeostasis gained further credence as a result of the
discovery of spontaneous mutations, ob (obese) and db
(diabetes), which caused hyperphagia and morbid obesity
in mice. In his classic experiments, Coleman [44,45] observed that parabiosis of ob/ob and lean (wild-type) mice
224
R.S. Ahima, S.Y. Osei / Physiology & Behavior 81 (2004) 223241
resulted in suppression of feeding and weight loss in the ob/
ob mice. In contrast, body weight was drastically reduced in
wild-type or ob/ob mice when parabiosed with db/db mice,
whereas the latter continued to gain weight [44,45]. These
seminal findings suggested that the ob locus encoded a
circulating satiety factor, while the db locus mediated the
tissue response [44,45]. More than four decades later, the ob
(Lep) gene was discovered, and its product missing in ob/ob
mice was named leptin (from the Greek root leptos
meaning thin), because it suppressed feeding and decreased
body weight when administered in mice [25,99,161,220].
On the other hand, obesity in db/db mice was linked to a
defect of the leptin receptor (LEPR) [38,129,199]. The
discovery of leptin has shed light on the complex biology
of adipose tissue [84]. Contrary to the prevailing view of
adipose tissue as merely a storage depot for triglyceride, we
now know that adipose tissue is composed of specialized
fat-storing cells (adipocytes) as well as vascular and immune cells which mediate various physiologic processes
[84,85]. Adipose tissue secretes leptin, adiponectin, resistin,
proinflammatory cytokines, complement factors, steroid
hormones and other molecules which actively regulate
energy balance, endocrine, immune and cardiovascular
systems [84,85]. An understanding of the biology of leptin
offers significant insights into the complex interrelationships
among adipose tissue, the nervous system and peripheral
organs.
2. Control of leptin production
The murine Lepob gene was discovered through positional cloning [5,220]. In mice, the leptin gene encodes a
4.5 kilobase mRNA transcript with a highly conserved 167amino acid open reading frame [220]. Leptin is remarkably
similar across species [93,105,117,118,220]. It is synthesized mainly by adipose tissue and is released into the
blood [220]. Various regulatory elements have been identified within the leptin promoter, e.g., cAMP and glucocorticoid response elements, and CCATT/enhancer and SP-1
binding sites, suggesting a direct regulation of leptin
expression through membrane and transcriptional pathways
[93,102,105,118,220]. Leptin is produced, albeit at lower
levels in other tissues, such as gastric epithelium, skeletal
muscle and placenta [7,143,144,206]. Studies have suggested physiologic roles of leptin in these tissues. For
example, leptin mRNA and protein levels are increased in
skeletal muscle following glucosamine treatment, consistent
with involvement in energy metabolism [206] (Table 1).
Leptin expression in the stomach is stimulated by feeding,
cholecystokinin and gastrin, suggesting a role in regulation
of energy balance [7] (Table 1). Placenta leptin is stimulated by hypoxia, elevated in eclampsia and may influence
fetal outcome [143,144] (Table 1). Furthermore, de novo
leptin synthesis has been demonstrated in the brain, suggesting a paracrine or autocrine action; however, the
Table 1
Factors implicated in leptin regulation
Increase leptin
Decrease leptin
Adipose tissue
Overfeeding
Obesity (except ob/ob mutation)
Insulin
Glucocorticoids
Acute infection
Proinflammatory cytokines (TNF-a, IL-1)
Placenta
Insulin
Glucocorticoids
Hypoxia/eclampsia
Skeletal muscle
Glucose
Glucosamine
Lipids
Adipose tissue
Fasting
Cold exposure
h-adrenergic agonist
Testosterone
Stomach
Feeding
Cholecystokinin
physiologic relevance of brain-derived leptin remains to
be ascertained [147,212].
In ad libitum fed animals, the levels of leptin mRNA and
protein in adipose tissue and plasma are positively correlated to body fat and adipocyte size [47,83,138]. Thus, obese
persons have higher leptin mRNA and protein levels than
lean individuals. Leptin secretion appears to occur mainly
via a constitutive mechanism, although the levels can be
regulated by various physiologic states. For example, leptin
falls during fasting, out of proportion to the decrease in
body fat [4,21,179]. Conversely, leptin mRNA and protein
are increased several hours after eating [122,179]. The
effects of nutrition are mediated, at least in part by insulin,
as shown by a direct stimulation of leptin synthesis and
release when adipocytes are cultured in the presence of
insulin [13,19,137,172]. In both humans and rodents, the
postprandial rise in leptin follows the peak insulin secretion
[79,182,188]. In contrast, insulin deficiency results in rapid
reduction of leptin mRNA and protein levels [122,179].
Leptin is regulated by steroid hormones (Table 1).
Chronic glucocorticoid exposure increases leptin synthesis
and release from cultured adipocytes and in vivo
[53,62,126,132,142,149]. A sexual dimorphism of leptin
has been demonstrated in several species [177,190]. In
humans, leptin is higher in females than males matched for
age, and the gender difference has been attributed to higher
leptin production in subcutaneous adipose tissue, stimulation
of leptin by estrogen in females and suppression of leptin by
testosterone in males [32,33,61,120,173,175,177]. Unlike
humans, leptin is higher in male rodents compared with
females [160]. The reasons for these species differences in
leptin are unclear.
Leptin is elevated during acute infection, and in response
to endotoxin and proinflammatory cytokines (Table 1)
[22,78,119,180]. In contrast, cold exposure, catecholamines
and melatonin decrease leptin [57,132,169,189,200,215].
There have been conflicting reports regarding the effects
of thyroid and growth hormone on leptin. While some
studies have reported a rise in leptin in thyroid deficiency,
R.S. Ahima, S.Y. Osei / Physiology & Behavior 81 (2004) 223241
others have demonstrated an increase in leptin in response to
hyperthyroidism or no significant effect of thyroid hormone
on leptin [69,80,140,159,163]. Similarly, the link between
growth hormone and leptin remains controversial [80,90].
Leptin level is increased in growth hormone deficiency
(GHD), presumably as a result of increased body fat [80].
However, this association has not been consistent with other
studies. For example, growth hormone treatment has been
reported to stimulate leptin, or have no significant effect on
leptin [80,90].
A nocturnal rise in leptin occurs under ad libitum fed
conditions [3,179,182]. In rodents, the increase in leptin
mRNA level and plasma leptin is prevented by fasting
[179]. Moreover, restriction of feeding to the light cycle
shifts the peak plasma leptin level from nocturnal to
diurnal [3,179]. The shift in leptin is accompanied by a
parallel shift in insulin and corticosterone; however, it is
doubtful that the latter is mediated by leptin, because a
diurnal rhythm of corticosterone occurs in ob/ob mice
despite a total absence of leptin [3,179]. As in rodents,
leptin peaks at night and declines during the day in
humans [133,134,182,188]. This pattern is thought to be
regulated mainly by insulin [182,188]. Interestingly, the
diurnal leptin rhythm appears to be blunted with aging,
and has been associated with an increase in visceral
adiposity and insulin resistance [135].
An ultradian leptin rhythm has been demonstrated following frequent blood sampling in humans [133,134].
Leptin is secreted in pulses that are inversely associated
with ACTH and cortisol, and positively correlated to gonadotropins, estradiol and thyrotropin [133,134]. Obesity is
associated not only with higher basal leptin level, but also a
blunted diurnal rhythm and dampened pulsatility [135,187].
Healthy men and women have similar leptin pulse frequency; however, leptin pulse amplitude is more than twice as
high in women [135]. The gender difference appears to be
influenced mainly by the mass or amount of leptin released
or removed per unit time, suggesting that women may be
more resistant to leptin feedback than men [135]. Potentially, this may underlie the greater susceptibility to disorders of
feeding and body weight regulation in females.
To test the hypothesis that changes in plasma leptin were
related to the levels of luteinizing hormone (LH) and
estradiol, Licinio et al. [134] sampled plasma from six
healthy women every 7 min for 24 h. Cross-correlation
analysis revealed a strong association between leptin and
LH release, with a lag time of 42 84 min. The ultradian
pattern of leptin was synchronous with LH and estradiol.
Moreover, the nocturnal leptin peak was positively correlated to LH pulses of longer duration, higher amplitude and
larger area. The nocturnal synchronicity of LH and leptin
was associated with significant coupling with estradiol,
suggesting a functional link between leptin and the hypothalamic pituitary gonadal axis [134]. The latter is consistent with the diminution of leptin amplitude and
frequency in patients with hypothalamic amenorrhea [128].
225
The timing of leptin production varies according to age.
In rodents, leptin is expressed widely during the prenatal
period. Some studies have indicated that leptin mRNA and
protein levels decrease rapidly after birth, followed by a
transient increase in the neonatal period and a steady
increase in adults [3,55,145,190]. Similar changes in plasma
leptin have been observed in longitudinal studies in prepubertal boys, in whom leptin is thought to exert a permissive
effect on sexual maturation [86,139]. However, other studies
have not observed a significant change in postnatal leptin
levels, or an association between leptin and reproductive
development [139]. So far, it is not known whether the
changes in circulating leptin with age are determined by
leptin synthesis or clearance.
Leptin gene mutations are rare. In C57Bl/6J mice, a
frameshift mutation (C-to-T) results in a stop codon at
position 105 instead of arginine, leading to production of
a truncated protein that cannot be secreted [220]. Leptin
mRNA is increased in ob/ob mice, suggesting a short
negative feedback regulation of leptin synthesis [220].
Leptin gene mutations have been identified in highly
consanguineous human families [146,158,192]. Affected
members of a Pakistani family have a deletion of guanine
in codon 133, resulting in synthesis of a truncated protein
which is degraded [146,170]. A missense leptin gene
mutation (C-to-T in codon 105) in a Turkish family results
in production of a mutant protein which cannot be secreted
[158,192]. In these cases, a lack of bioactive leptin culminates in hyperphagia, morbid obesity, hypothalamic hypogonadism and immune suppression, similar to ob/ob mice.
Moreover, heterozygousity of the leptin gene has been
associated with increased body fat in both rodents and
humans, indicating a dose effect of leptin on body fat
[41,72,104]. Nonetheless, there are significant differences
between leptin-deficient humans and rodents, as some
characteristics of leptin deficiency in C57Bl/6J mice, such
as impaired thermoregulation, elevated glucocorticoids, insulin resistance and diabetes, have not been observed in
leptin-deficient humans [70,146,158,168]. It is possible that
these disparate responses to leptin deficiency are due to
species differences in energy substrate fluxes, as well as
brown adipose tissue metabolism which is prominent in
rodents [112].
3. Leptin receptors
The first LEPR was isolated from mouse choroid plexus
by expression cloning [199]. However, because this receptor
was present in db/db mice, it was apparent that other LEPRs
had to exist [199]. To date, six splice variants of the LEPR,
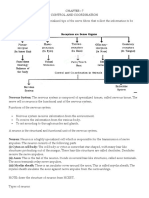
a to f, have been identified [5,198] (Fig. 1). LEPR
belongs to a family of class I cytokine receptors, which
typically contains a cytokine receptor homologous domain
in the extracellular region. Two conserved disulfide links are
present in the N-terminus, and a WSXWS motif is present in
226
R.S. Ahima, S.Y. Osei / Physiology & Behavior 81 (2004) 223241
Fig. 1. Domain structure of alternatively sliced LEPR isoforms. Terminal amino acid residues for various LEPR isoforms are denoted by the alphabet code.
Leptin receptors share a common extracellular leptin-binding domain, but differ at the carboxy-terminus intracellular domain. The long isoform, LEPRb, has
intracellular motifs necessary for JAK-STAT signaling. LEPRe lacks a transmembrane domain (TM) and intracellular domains and circulates as a soluble
receptor.
the C-terminus. LEPR shares highest sequence similarity
with receptors for interleukin-6 (IL-6), leukemia inhibitory
factor (LIF), granulocyte-colony stimulating factor (GCSF)
and oncostatin [198]. LEPR isoforms have a similar extracellular ligand-binding domain at the amino terminus, but
differ at the intracellular carboxy-terminal domain. LEPRa,
LEPRb, LEPRc, LEPRd and LEPRf have transmembrane
domains; however, only the long receptor, LEPRb, has
intracellular motifs necessary for activation of the JAKSTAT signal transduction pathway. LEPRe lacks both transmembrane and intracellular domains and circulates as a
soluble receptor [198].
The db/db mutation is caused by insertion of a premature
stop codon in the 3V-end of LEPRb mRNA transcript,
resulting in synthesis of LEPRa [38,129,198]. As expected,
db/db mice are hyperphagic, morbidly obese, sexually
immature, exhibit cold intolerance and elevated glucocorticoids, and do not respond to leptin treatment [38,129].
However, the phenotype of db/db mice is influenced by
genetic background. For example, breeding on C57BlKS/J
background results in early-onset severe diabetes, due to
apoptosis of pancreatic h cells, and a shorter life span. In
contrast, the C57Bl/6J background protects against diabetes
and promotes longevity in db/db mice. Mice homozygous
for Leprdb3J mutation fail to express all membrane LEPRs
[124]. This mutant is hyperphagic, cold intolerant, obese,
insulin resistant and infertile. Expression of a neuron-specific enolase (NSE)-LEPRb transgene restored the ability to
activate the JAK-STAT pathway in both db3J/db3J and db/
db mice, partially reversed hyperphagia, obesity, glucose
intolerance and infertility in males, and rescued the cold
intolerance in both sexes [124]. Importantly, NSE-LEPRb
was expressed mainly in the brain, confirming the importance of this organ as a target for leptin [124]. Analysis of
gene expression revealed that NSE-LEPRb restored the
ability to regulate proopiomelanocortin (POMC), agouti
gene-related protein (AGRP) and neuropeptide Y (NPY),
consistent with a significant role of these neuropeptides as
mediators of leptin action [124].
LEPR mutations have been discovered in rats [40,51,
195,212,215]. Substitution of Gln for Pro at amino acid
position 269 in the extracellular domain results in drastic
reduction of cell surface expression of LEPR and reduced
binding to leptin in Zucker fatty (fa/fa) rats [40,51,211].
These mutant rats are hyperphagic, obese and hyperlipidemic, and have increased glucocorticoids and hyperglycemia [40,51]. When expressed in Chinese hamster ovary
(CHO) cells, the fa/fa receptor not only exhibited a reduction
in leptin-binding affinity, but also performed reduced signal
transduction, as evidenced by induction of the immediate
early genes, c-fos, c-jun, and jun-B in CHO cells
[40,52,211]. Moreover, fa/fa rats are capable of responding
to high doses of leptin administered by intracerebroventricular injection, consistent with a partial function of the
receptor [51]. The obese Koletsky rat (SHROB, fak) has a
point mutation of LEPR at amino acid 763, resulting in a
premature stop codon in the extracellular domain and absence of all cell surface LEPRs [195,215]. Plasma leptin
concentration is greater than lean spontaneous hypertensive
(SHR) littermates, suggesting severe leptin resistance. Kolet-
R.S. Ahima, S.Y. Osei / Physiology & Behavior 81 (2004) 223241
sky rats are hyperphagic, morbidly obese and have various
hormonal abnormalities [195,215]. However, in contrast to
fa/fa rats, obese Koletsky rats do not respond to leptin
treatment [215].
Leptin receptor mutations are rare in humans. Affected
members of a French family have a single nucleotide
substitution (G-to-A) in the splice donor site of exon 16,
resulting in encoding of a LEPR lacking both transmembrane and intracellular domains [42]. The mutant receptor
circulates at high concentrations bound to leptin [42]. As is
the case in rodents, LEPR null humans are hyperphagic,
morbidly obese and fail to undergo normal sexual maturation [42]. Furthermore, these patients failed to respond
normally to thyrotropin-releasing hormone (TRH) and
growth-hormone-releasing hormone (GHRH) testing, suggesting a critical role of leptin in neuroendocrine regulation
[42].
4. Intracellular signal transduction of leptin
Leptin circulates as a 16-kD protein partially bound to
plasma proteins [113,187]. Most likely, protein-bound leptin exists in equilibrium with free leptin, and the latter
represent the bioactive hormone. Studies have shown that
the ratio of bound-to-free leptin is increased in obesity,
pregnancy and LEPR mutation [42,113,187]. The rise in
serum leptin in pregnancy and LEPR null humans is due to
binding to LEPRe [42,187]. An additional pool of leptin
may exist in various tissues, and contribute to the maintenance of plasma leptin [111]. As with other class I cytokine
receptors, e.g., IL-6, LIF, oncostatin M, ciliary neurotrophic
factor, growth hormone and prolactin, the leptin signal is
thought to be transmitted mainly by the JAK-STAT pathway [8,14,88,150,203]. JAKs associate constitutively with
conserved box 1 and 2 motifs in the intracellular domain of
LEPRb (Fig. 1). In mice, the box 1 motif (amino acids 6
17) is critical for JAK2 activation, and box 2 motif (amino
acids 49 60) is required for maximal activation of LEPRb.
Binding of leptin to LEPRb results in autophosphorylation
of JAK1 and JAK2, and tyrosine phosphorylation of the
cytoplasmic domain of LEPRb and downstream transcription factors, named STATs. These signaling molecules are
highly expressed in hypothalamic, brainstem and other
brain regions which control food intake, autonomic and
neuroendocrine function [98].
LEPRb has three conserved tyrosine residues in the
intracellular domain, corresponding to Y985, Y1077 and
Y1138 in mice. Leptin treatment results in phosphorylation
of the latter site, and recruitment of STAT3 via its SH2
domain. Tyrosyl-phosphorylated STAT3 undergoes homodimerization and nuclear translocation, and transactivates
target genes by binding to specific promoter elements [150].
The essential role of Y1138 was demonstrated in mice by
replacing this residue with serine [14]. Y1138S knock-in
mice (LeprS1138) were unable to activate STAT3 [14]. Like
227
db/db mice [89], LeprS1138 homozygous mice became hyperphagic and obese. However, in contrast to db/db mice,
LeprS1138 homozygotes attained normal sexual maturation,
fertility and body length [14]. Moreover, LeprS1138 homozygotes were less hyperglycemic [14]. Expression of NPY
in hypothalamus was elevated in db/db but not LeprS1138
homozygotes, whereas melanocortin expression was suppressed in both mutants [14]. These findings suggest that the
LEPRb-STAT3 signaling is required for energy balance and
regulation of melanocortins; however, a separate LEPRb
pathway, possibly involving other STATs, is likely to control
reproduction, linear growth, glucose and hypothalamic NPY
mRNA level [14].
Leptin-activated LEPRb regulates well-known insulin
targets, such as IRS-1, MAP kinase, ERK, Akt, AMP kinase
and PI3-kinase, raising the possibility that leptin pathways
act in concert with insulin to control energy metabolism and
other cellular processes [154,165]. This idea is supported by
the coexistence of LEPR, JAKs, STATs, insulin receptor and
its substrates in a variety of tissues, e.g., neurons, adipocytes, pancreatic islets, immune cells and adrenal cortex.
Leptin is able to induce the tyrosine phosphorylation of the
SH2-containing protein SHC, which associates with the
adaptor protein, Grb2. The formation of this complex may
directly link tyrosine phosphorylation events to Ras activation, and serve as a critical step in mediating the effects of
leptin and insulin on cell proliferation and differentiation
[8,20,28,150,154]. Studies have also shown that leptin and
insulin responses in the brain can both be disrupted by
inhibition of PI3 kinase, providing further proof for an
overlapping signaling pathway [154].
Although leptin enters the brain via a saturable process,
the exact structures responsible for leptin transport are
unknown [9,10]. Based on experience with other polypeptide hormones, it had been suggested that leptin was transported by receptor-mediated transcytosis across the blood
brain barrier [160]. Because short LEPRs are widely present
in brain microvessels, kidney, liver, lung and gonads, and
capable of binding, internalizing and translocating leptin, it
was suggested that these receptors mediate leptin transport
[19,20,92,202]. Cerebrospinal fluid (CSF) leptin is present
but markedly reduced in obese Koletsky rats which totally
lack membrane LEPRs, indicating that other factors besides
LEPRs are involved in brain leptin transport [195,217].
Furthermore, it is doubtful that CSF is a significant source
of leptin for neurons, because leptin concentration in CSF is
lower than plasma leptin and below the dissociation constant of the LEPR [20,27,81,92,183].
Despite the widespread distribution of LEPRs in the
brain and peripheral organs, there is little evidence in
support of an involvement of these receptors in energy
homeostasis or neuroendocrine control. Leprdb homozygous
mice lacking LEPRb but possessing a full complement of
short LEPR isoforms, develop hyperphagia, cold intolerance, obesity, insulin resistance and infertility, as is the case
with Leprdb3J homozygotes that are null for all isoforms of
228
R.S. Ahima, S.Y. Osei / Physiology & Behavior 81 (2004) 223241
LEPR [124]. In contrast, transgenic expression of NSELEPRb capable of activating JAK-STAT, partially reversed
obesity, hyperphagia, glucose and cold intolerance in male
and female db3J/db3J mice, and restored fertility in male
db3J/db3J mice, confirming the importance of LEPRb
[124].
Leptin binds to LEPRs in kidney epithelium, and the
complex is internalized and degraded [202]. A functional
role of LEPRs in leptin clearance is suggested by the
elevation of plasma leptin in patients with renal impairment [185]. Long and short LEPRs are coexpressed in
some tissues, raising the possibility that heterodimers of
these receptors may signal leptin response through the
JAK-STAT pathway. However, chimeric receptor heterodimers of LEPRa and LEPRb failed to activate JAKSTAT, whereas receptor dimers of LEPRb gave rise to
the expected ligand-dependent activation of JAK2, phosphorylation of STAT3, and increased STAT3-dependent
promoter activity [8,150]. Furthermore, site-directed mutagenesis has revealed that two hydrophobic residues
(Leu896 and Phe897) not present in LEPRa were essential
for leptin signal transduction [8].
The leptin signal is terminated by induction of SOCS-3, a
member of a family of proteins which inhibits the JAK-STAT
signaling cascade [17,66]. SOCS proteins have a variable Nterminal domain, a central SH2 domain and a C-terminal
domain, termed SOCS-box motif. They are induced by
cytokines and act in a negative feedback loop to inhibit the
receptor. Overexpression of SOCS-3 inhibits leptin-mediated
tyrosine phosphorylation of JAK-2 [17,18,66]. Protein
tyrosine phosphastase (PTP)-1B is a critical downstream
regulator of leptin signal transduction [218]. PTP-1B recognizes a specific substrate motif within JAK2. Overexpression
of PTP-1B decreased phosphorylation of JAK2 and blocked
leptin-induced transcription of SOCS-3 and c-fos. In contrast, deletion of the PTP-1B gene enhanced leptin sensitivity
in mice, thereby preventing obesity [218]. Hypothalamic
STAT-3 phosphorylation was also enhanced in PTP-1B-null
mice in response to leptin treatment, confirming the importance of PTP-1B as a mediator of in vivo leptin signaling
[183].
While these findings suggest an important role of the
JAK-STAT cascade in leptin signaling, there have been
reports of rapid effects of leptin that cannot be explained
by gene expression [49,91,114,191]. For example, leptin
inhibits NPY secretion from hypothalamic explants [91].
Application of leptin to hypothalamic slices hyperpolarizes
arcuate hypothalamic NPY neurons and depolarizes POMC
neurons [49]. In the latter case, POMC neurons are activated
in part through disinhibition by leptin-responsive NPY
neurons in the same nucleus [49]. Electrophysiologic studies
have also revealed an inhibitory response to leptin in the
supraoptic nucleus and modulation of vagal afferents in the
gut [114]. Furthermore, leptin is able to rapidly regulate
glucose-sensitive neurons in the brain and insulin secretion
from pancreatic islets [191]. These effects appear to involve
activation of ATP-sensitive potassium channels or other
membrane receptors.
5. Role of leptin in energy homeostasis
5.1. Leptin as an antiobesity hormone
At the time of its discovery, it was thought that leptin
acted as an afferent signal in the brain to suppress feeding
and increase energy expenditure [5,220]. This view was
largely based on the observation that obese (leptin-deficient)
rodents developed hyperphagia and morbid obesity, which
were reversed by leptin treatment, consistent with a feedback loop from adipose tissue to the brain [25,99,161].
However, the initial studies clearly demonstrated that leptin
replete wild-type mice were less sensitive to exogenous
leptin [25,99,161]. Subsequently, leptin mRNA and protein
levels were noted to be markedly elevated in obese rodents
(apart from ob/ob mice), and yet, the rise in leptin was
unable to suppress feeding or weight gain [33,83,138,205].
Likewise, diet-induced obesity (DIO) in humans is associated with increased leptin level and reduced sensitivity to
leptin treatment [47,109,138]. Akin to hyperinsulinemia and
insulin resistance, it has been postulated that the hyperleptinemia is indicative of leptin resistance [81].
DIO may arise from defective brain leptin transport, as
evidenced by reduced plasma-to-brain leptin transport in
obese rodents [9]. The CSF: plasma leptin ratio is reduced in
obesity compared with anorexia nervosa, and may underlie
the false perception of satiety in the latter [27,183]. Leptin
response is decreased in aged rodents, suggesting that leptin
resistance may be acquired [9]. Although no apparent
defects of LEPRb has been demonstrated in the vast
majority of obese animals, abnormalities of distal leptin
signaling molecules have been reported [17,18,28,63,66].
For example, DIO mice are unable to activate STAT-3 in the
hypothalamus following peripheral leptin injection, whereas
the response to intracerebroventricular leptin treatment is
preserved [63]. Leptin resistance may result from induction
of SOCS-3, and/or activation of SHP-2 and PTP-1B
[17,18,28,63,66,218]. SOCS-3 mRNA expression is higher
in the hypothalamus of obese agouti (Ay/a) mice and
thought to mediate leptin resistance [18]. However,
SOCS-3 is not consistently elevated in DIO, and its significance in the latter remains uncertain [63].
Susceptibility to DIO may be determined by differences
in the levels of hypothalamic neuropeptide targets of leptin
[15,167,194]. For example, the orexigenic hypothalamic
neuropeptide, NPY, is increased in C57Bl/6J mice, a strain
prone to DIO [194]. In contrast, POMC, the precursor of
the anorexigenic neuropeptide a-MSH, is elevated in
obesity-resistant A/J and SWR/J mice [15]. Expression of
genes which mediate adaptive thermogenesis, e.g., UCP-1,
UCP-3 and PGC-1, is increased in A/J and SWR/J mice,
and may prevent obesity in these strains [167,194]. Obe-
R.S. Ahima, S.Y. Osei / Physiology & Behavior 81 (2004) 223241
sity-resistant SWR/J mice are more sensitive to leptin,
compared with obesity-prone C57Bl/6J mice [194]. Moreover, susceptibility to obesity in C57Bl/6J mice is positively correlated with failure to suppress hypothalamic
NPY mRNA and blunting of brown adipose tissue UCP1 expression [167,194]. Whether these factors are involved
in the pathogenesis of DIO in humans and other primates
remains to be determined.
Reduced leptin sensitivity in DIO and aged animals
predisposes to lipid accumulation in nonadipose tissues
[201]. This condition, known as steatosis, is characterized
by excessive triglyceride accumulation in liver, pancreatic
h-cells, myocardium and skeletal muscle, resulting in lipotoxic insulin deficiency, diabetes, and impairment of
myocardium and other organs, characteristic of aging and
obesity [201]. The increase in extraadipose tissue lipid is
primarily the result of enhanced lipogenesis, although a
decrease in fatty acid oxidation also contributes (reviewed in
Ref. [201]). Consistent with this idea, pancreatic islets and
liver express high levels of lipogenic transcription factors,
e.g., SREBP-1c and PPARg, and their target genes, e.g.,
acetyl coA carboxylase (ACC), fatty acid synthase (FAS)
and glycerol phosphate acyl transferase (GPAT), as a result
of impaired leptin signaling [130,201]. Leptin slows the
progression of steatosis and its sequelae, by stimulating lipid
oxidation and preventing toxic metabolites, such as ceramide, from accumulating [130,201].
5.2. Leptin as a starvation signal
There is strong evidence showing that the dominant
action of leptin is to act as a starvation signal. Leptin
declines rapidly during fasting, and triggers a rise in
glucocorticoids, and reduction in thyroxine (T4), sex and
growth hormones [2,4]. Moreover, the characteristic decrease in thermogenesis during fasting and postfast hyperphagia is mediated, at least in part, through a decline in
leptin level [2,5]. The reduction in leptin during fasting
stimulates expression of NPY and AGRP, and suppresses
CART and POMC [2]. These fasting-induced responses
resemble the phenotypes of ob/ob and db/db mice [65].
Therefore, we reasoned that leptin deficiency was perceived
as a state of unmitigated starvation, leading to compensatory
responses, such as hyperphagia, decreased metabolic rate
and changes in hormone levels, designed to restore energy
balance [2,4,81]. In contrast to the low insulin levels
characteristic of fasting, ob/ob and db/db mice have extremely high insulin levels. Perhaps, the elevation in insulin
in these mice is commensurate with high energy efficiency,
and may contribute to excessive fat storage [81].
Chan et al. [34] have examined the role of leptin in
regulating neuroendocrine and metabolic function in fasted
humans. Placebo, low-dose recombinant-methionyl human
leptin (r-metHuLeptin) or replacement-dose r-metHuLeptin
was administered during 72-h fasting. Replacement-dose
leptin prevented the starvation-induced changes in sex
229
hormones and partially prevented the suppression of hypothalamic pituitary thyroid axis and IGF-1 binding capacity. However, unlike rodents, leptin replacement during
acute fasting did not affect fuel utilization, glucocorticoids
or growth hormone levels in humans [34]. An earlier study
by Rosenbaum et al. [176] demonstrated that chronic leptin
treatment fully prevented the reduction in energy expenditure and thyroid hormone during sustained weight reduction
in humans [150]. Taken together, these data support the idea
that leptin plays an important role in controlling the neuroendocrine and metabolic response to caloric depletion.
Studies have suggested that low leptin may predispose to
obesity in apparently healthy populations [72,84]. For
example, family members heterozygous for a leptin gene
mutation have partial leptin deficiency and excess body fat
compared with wild-type patients [72]. Similarly, mice with
heterozygous mutations of the leptin gene have increased
body fat compared with wild-type littermates [41,104].
Presumably, the reduction in leptin level signals the brain
and other targets to enhance energy storage. It has been
reported that leptin is decreased in obesity-prone Pima
Indians [171]. Moreover, cross-sectional studies have suggested that leptin is inappropriately low in 10 20% of obese
individuals, suggesting that partial leptin deficiency may
promote obesity by stimulating appetite, decreasing energy
expenditure and creating the hormone mellieu necessary for
obesity [84]. More importantly, it is possible that these
obese patients with low leptin could benefit from leptin
supplementation [84].
NPY is increased in the hypothalamus in response to
leptin deficiency, and postulated to stimulate feeding and
weight gain [5]. Although the original report discounted a
role for NPY in the leptin-mediated response to fasting, later
studies have revealed a blunted postfast hyperphagia and
weight gain in NPY-deficient mice [11,184]. Moreover,
deletion of the NPY gene partly attenuated hyperphagia,
cold intolerance, obesity and infertility in leptin-deficient
ob/ob mice, confirming the importance of NPY as a sensor
of low leptin [68]. NPY acts via a variety of receptors in the
brain and peripheral tissues. Crossing the Y2 receptor
knockout mouse onto ob/ob background attenuated obesity,
hyperglycemia and high glucocorticoids, but did not alter
hyperphagia or hypogonadism in ob/ob mice [152,153]. In
contrast, deletion of Y4 receptor did not prevent obesity,
diabetes or excess glucocorticoids, but restored sexual
maturation and fertility in ob/ob mice [152].
The fall in leptin triggers a suppression of the immune
system during starvation [136]. Conversely, leptin treatment
stimulates the immune response, e.g., reversal of splenic and
thymic atrophy, delayed hypersensitivity and lipopolysaccharide-mediated cytokine production and mortality [136].
The machinery for leptin signal transduction, i.e., LEPRb,
JAK and STAT, is present in immune cells, and leptin is
capable of directly regulating lymphocyte proliferation and
differentiation. Based on the robust responses to leptin
deficiency, it has been suggested that leptin may have
230
R.S. Ahima, S.Y. Osei / Physiology & Behavior 81 (2004) 223241
evolved as a critical signal linking adipose energy stores and
the brain and peripheral targets, as a safeguard against the
threat of starvation [81]. Reduced leptin levels promote
energy intake and limit the high energy cost of reproduction,
thyroid thermogenesis and immune response [81]. While the
leptin-mediated adaptation to energy deficiency is likely to
have been beneficial in times of food shortage, this tendency
towards efficient energy metabolism may have contributed
to the current epidemic of obesity in an environment where
food is abundant [81].
5.2.1. Lipodystrophy
Lipodystrophic syndromes comprise of a heterogeneous
group of disorders characterized by partial or generalized
loss of adipose tissue depots, and commonly associated with
severe insulin resistance, diabetes, dyslipidemia and steatosis [87]. Adipocyte-secreted proteins, e.g., leptin and adiponectin, are decreased in lipodystrophy [87]. By far the
commonest cause of acquired lipodystrophy is highly active
antiretroviral therapy (HAART)-induced lipodystrophy in
HIV patients [37]. HIV lipodystrophy results in loss of
facial and peripheral fat, preservation of visceral fat, insulin
resistance and lipid abnormalities [37]. Given the wellknown association between these metabolic alterations and
atherosclerosis, there is concern that the beneficial effect of
antiretroviral treatment would be offset by premature coronary artery disease [37]. The striking similarities between
the metabolic syndrome of obesity and lipodystrophy
have stimulated a search for common underlying mechanisms. Earlier studies attributed the metabolic changes in
lipodystrophy to the absence of adequate adipocyte storage
capacity in lipodystrophy, resulting in triglyceride accumulation in liver, skeletal and cardiac muscle, and in the
pancreatic h-cell, and culminating in impaired insulin action, diabetes and lipid abnormalities [87]. This idea was
supported by studies showing that insulin sensitivity improved following fat transplantation in mice with generalized lipodystrophy [88]. However, fat transplantation from
leptin-deficient ob/ob mice failed to reverse the metabolic
disturbance [46]. Rather, infusion or transgenic delivery of
leptin alone or in combination with adiponectin, improved
insulin resistance, glucose and lipids in lipodystrophic mice
[59,186,216]. These findings suggested that a deficiency in
adipose secreted factors, rather than decreased adipose mass
per se, contributed to the metabolic abnormalities in lipodystrophy [186,216].
Further support for a role of leptin in carbohydrate and
lipid metabolism came from experiments showing that
leptin replacement partially reversed insulin resistance,
steatosis and lipid abnormalities in lipodystrophic patients
[155,156,162]. Importantly, leptin replacement was more
effective than the standard-of-care plasmapheresis, in reducing hepatic steatosis and intramyocellular triglycerides, and
improving insulin sensitivity [155,156,162]. Interestingly,
leptin replacement restored the pituitary gonadal axis in
lipodystrophic patients, confirming the importance of leptin
as a modulator of reproduction [155]. Molecular targets for
leptin include a reduction in fatty acyl-CoA, and induction
of hepatic and muscle lipid oxidation via activation of
AMP-activated protein kinase activation [216]. In rodents,
these effects of leptin are mediated centrally through the
sympathetic nervous system and peripherally through
LEPRb [216]. The beneficial effects of leptin on glucose
and lipids occur independently of regulation of food intake
and metabolic rate per se, and have given impetus for
consideration of leptin treatment in lipodystrophy as well
as obese patients with relatively low leptin levels.
6. Leptins effects on classical hormones
6.1. Reproduction
As discussed earlier, total leptin deficiency or insensitivity is associated with hypothalamic hypogonadism in
humans and rodents. In mice, the effect of leptin deficiency
on sexual maturation is modified by genetic background, as
evidenced by spontaneous pubertal development in ob/ob
mice bred onto Balb/c background [35,70]. Similarly, menstrual cycles occurred spontaneously in a patient with leptin
gene mutation, while family members bearing the same
leptin gene mutation failed to undergo normal pubertal
development [158]. Leptin treatment restored LH secretion
and pubertal development in leptin-deficient patients, confirming its critical role in reproduction [73]. However, while
leptin is essential to puberty and reproductive cycles, studies
in ob/ob mice have indicated that it is not required for
gestation, paturition or lactation [148]. Based on studies in
rodents and nonhuman primates, leptin appears to exert a
permissive action to restore normal hypothalamic pituitary gonadal axis function during starvation [12,39,96].
These actions are likely to be mediated through stimulation
of gonadotropins, in concert with other metabolic signals
[207,214].
The link between leptin and puberty in normal animals
remains controversial [1,36,110,164]. A longitudinal study
in boys revealed elevation of prepubertal leptin levels,
preceding the rise in testosterone [139]. A transient increase
in leptin has also been noted in boys aged 5 10 years [86].
In the same study, plasma leptin was higher in girls;
however, there was no prepubertal increase [86]. Interestingly, a nocturnal rise in leptin precedes the prepubertal
increase in pulsatile LH release in monkeys [193]. This
observation is contrary to an earlier report in which there
was no change in peripubertal leptin levels in relation to the
rise in LH, FSH and testosterone [164]. Possible reasons for
these disparate results include the timing of sample collection (i.e., daytime vs. nighttime), variability of LH release
and whether intact or castrated animals were studied [110].
Leptin stimulates the synthesis and release of LH and
FSH [29,79,151,210,217]. Moreover, leptin stimulates
GnRH synthesis and potentiates the effect of insulin on
R.S. Ahima, S.Y. Osei / Physiology & Behavior 81 (2004) 223241
GnRH release [207]. Ovarian follicular cells are regulated
directly by leptin [219], indicating that leptin is able to
control the hypothalamic pituitary gonadal axis at multiple levels. Although leptin restores reproductive function in
food-deprived rodents and humans, and accelerates the
onset of sexual maturation (vaginal opening) in ad libitum
fed postnatal mice [1,36,39,96], there are no published
studies showing direct effects of leptin reproductive function in healthy humans. Current knowledge is based primarily on associations between leptin and reproductive
hormones. For example, frequent blood sampling has
revealed a positive and strong correlation between leptin
pulsatility and LH and estradiol levels in normally cycling
women [134]. In contrast, mean leptin level and diurnal
leptin rhythm are impaired in hypothalamic amenorrhea
[128]. Although leptin is elevated in association with
obesity in patients with polycystic ovarian syndrome, it
does not appear to account for menstrual abnormalities in
this population [127].
6.2. Hypothalamic pituitary adrenal axis
Leptin deficiency or insensitivity in rodents is characterized by elevated glucocorticoid levels [3]. Leptin injection
decreases corticosterone levels in ob/ob mice before significant weight loss occurs [3], indicating that leptin is able to
control the hypothalamic pituitary adrenal (HPA) axis
independently of its role in energy balance. However, unlike
ob/ob and db/db mice, humans null for leptin or LEPR
genes have normal levels of cortisol and do not exhibit
abnormalities in basal or corticotropin-releasing hormone
(CRH)-stimulated response [42]. In rats, leptin blunts the
rise in ACTH and corticosterone during restraint stress and
inhibits glucocorticoid synthesis and secretion in the adrenal
cortex [106]. Moreover, leptin prevents ACTH-stimulated
glucocorticoid secretion in adrenal cortex [22,23]. Paradoxically, intracerebroventricular leptin injection increases nocturnal glucocorticoid levels [166,204].
An interaction between leptin and the HPA axis is further
evident in the temporal relationship between plasma leptin
and glucocorticoids. Cortisol in humans and corticosterone
in rodents peak at night, coincident with the leptin nadir and
vice versa [3,4,132]. This reciprocal relationship between
leptin and the HPA axis is dependent on the feeding cycle.
Hence, a change in the timing of feeding results in a parallel
shift in glucocorticoids [3,182]. However, leptin is not
essential for establishment of the diurnal glucocorticoid
rhythm, because ob/ob mice maintain a normal rhythm,
albeit with higher basal corticosterone levels [3].
There have been conflicting reports regarding the interaction between leptin and CRH. Leptin stimulated basal
CRH secretion from hypothalamic fragments [48]; however,
another study demonstrated an inhibition of hypoglycemiainduced CRH secretion from hypothalamic explants [106].
Moreover, it has been reported that leptin increased CRH
mRNA expression in the paraventricular hypothalamic nu-
231
cleus (PVN) in fasted rats, but did not alter CRH levels in
ob/ob mice [116]. These discrepancies may be explained by
differential effects of leptin on subsets of CRH neurons in
the PVN [5,65].
6.3. Thyroid hormone
T4 and triidotyronine (T3) are both subject to negative
feedback regulation. A fall in thyroid hormone stimulates
the synthesis and secretion of TRH and TSH. Conversely, a
rise in thyroid hormone suppresses TRH and TSH. This
feedback response is disrupted during fasting and illness,
culminating in low T4 and T3 levels, low or normal TSH
and suppression of TRH. The blunting of the hypothalamic pituitary thyroid axis response during caloric deprivation or illness has been termed euthyroid sick syndrome. It
has been suggested that the dampening of hypophysiotropic
TRH neuron attenuation of the rise in TSH and T3 may have
evolved to limit energy expenditure and prevent protein
catabolism during starvation [81]. Leptin deficiency has
been associated with impairment of thyrotrope response to
TRH stimulation, while leptin replacement in leptin null
humans and during food restriction reverses the suppression
of T3, TSH and TRH mRNA levels in PVN [2,37,73,131].
Because ablation of the arcuate nucleus abolished the effect
of low leptin on PVN TRH mRNA expression, we surmised
that leptin acted indirectly via NPY, AGRP and POMC
neurons in the arcuate nucleus [131]. The latter neurons act
through melanocortin receptors (MCRs) in PVN and other
areas of the hypothalamus [75,76]. However, subsequent
studies revealed a colocalization of TRH and LEPR in PVN,
as well as direct regulation of TRH promoter activity by
leptin [100], indicating that leptin regulates thyroid function
via multiple hypothalamic circuits.
6.4. Growth hormone
Leptin and growth hormone act through a family of
cytokine receptors coupled to the JAK-STAT pathway
[198]. In rodents, growth hormone synthesis/secretion is
impaired in states of leptin deficiency or leptin insensitivity
[5,42]. Pulsatile growth hormone secretion is markedly
blunted during fasting, and restored by leptin replacement
[197], while immunoneutralization of leptin decreased
growth hormone secretion in fed rats [30,31,71,197]. To
analyze the in vivo effects of leptin on growth hormone
release, Watanobe and Habu [208] infused leptin into the
hypothalamus. Leptin was more potent in stimulating
growth hormone release in fasted than fed animals, as
manifested by increased pulse amplitudes without significant changes in the pulse frequency. Leptin increased
GHRH in fed animals, while decreasing somatostatin level
[208]. Leptin receptors and STAT3 have been colocalized
with GHRH and somatostatin, providing strong anatomical
evidence for interaction between leptin and the somatotropic
axis [97,98]. Moreover, LEPRb is expressed in somato-
232
R.S. Ahima, S.Y. Osei / Physiology & Behavior 81 (2004) 223241
trophs and stimulates growth hormone release from isolated
pituitary gland [217]. In contrast, ovine leptin acts directly
on primary cultured somatotropes, by reducing the mRNA
levels encoding growth hormone and GHRH receptor [174].
In contrast to rodents, growth secretion in humans is
enhanced by fasting and impaired in obesity and aging.
Because obesity is associated with high plasma levels of
leptin, it has been postulated that the inhibitory action of
obesity on growth hormone may be mediated by leptin
[157]. Ozata et al. [157] compared patients with missense
mutation of the leptin gene with obese and nonobese
controls. The secretion of growth hormone in response to
GHRH and GHRP-6 was negatively affected by adiposity,
but not influenced by leptin levels. Growth hormone peaks
were negatively correlated with body mass index in control
(wild-type) patients as well as leptin-deficient patients,
indicating that other adiposity factors besides leptin controlled growth hormone. Leptin is increased in GHD and
decreased in response to growth hormone treatment [5,71].
This inverse relationship is maintained in short prepubertal
children treated with growth hormone [125]. Serum leptin
concentrations were significantly reduced after 1, 3 and 12
months of growth hormone treatment. Importantly, the
growth response correlated negatively with the change in
serum leptin concentration, suggesting that short-term
changes in leptin levels in response to growth hormone
could be useful markers of growth response [125].
The effect of growth hormone on leptin levels has been
compared between patients with growth hormone insensitivity (GHI) as a result of E180 splice mutation, and
idiopathic GHD [141]. Insulin-like growth factor I (IGF-I)
and IGFBP-3 levels were lower in homozygous GHI and
GHD patients compared with either normal controls or GHI
heterozygotes. Leptin was significantly higher in homozygous GHI patients than normal controls and heterozygous
GHI and GHD patients. Leptin levels were best predicted by
gender (higher in females) and body mass index in both
homozygous GHI and normal patients [141].
6.5. Ghrelin
Ghrelin, a 28-amino acid octanoylated peptide, was
identified in the rat stomach as an endogenous ligand for
the growth hormone secretagogue receptor. Plasma ghrelin
is reduced in obesity and elevated in anorexia nervosa and
thin patients (reviewed in Ref. [115]). In contrast, leptin is
decreased in anorexia nervosa and thin patients. Both
plasma ghrelin and leptin levels return to control values in
anorexia patients after renutrition. Thus, the inverse relationship between plasma leptin and ghrelin is dependent on
body fat mass as well as nutritional status. In addition to
growth hormone-releasing properties in rodents, ghrelin
stimulates feeding following systemic or intracerebroventricular administration. Systemic ghrelin administration increased Fos expression in leptin-sensitive neurons in the
arcuate nucleus, suggesting an interaction between these
ligands [50,115]. Subsequent electrophysiologic analysis
revealed that ghrelin increased the electrical activity of the
majority of hypothalamic cells that were inhibited by leptin
[50]. Thus, the opposite effects of leptin and ghrelin on
feeding may be mediated through similar neuronal targets in
the arcuate nucleus.
There has been compelling evidence in support of
endogenous ghrelin production in the hypothalamus
[50,144]. Ghrelin-positive cells lie adjacent to the third
ventricle between the dorsal, ventral, paraventricular and
arcuate hypothalamic nuclei. These neurons send efferent
projections to NPY, AGRP, POMC and CRH neurons.
Ghrelin is bound mostly on presynaptic terminals of NPY
neurons, and stimulates the activity of arcuate NPY projections to the paraventricular nucleus [50,144]. Hence, ghrelin
produced in the hypothalamus may modulate energy balance by interacting with well-known leptin target neurons.
6.6. Prolactin
Prolactin has a major role in influencing the deposition
and mobilization of fat. The prolactin receptor belongs to
the same family as LEPR [198]. In humans, obesity diminishes the prolactin response to insulin-hypoglycemia and
thyrotrophin-releasing hormone stimulation [123]. Moreover, the spontaneous 24-h release of prolactin is dampened
in obesity [123]. Weight reduction, with accompanying
decrease in plasma insulin, improves prolactin responses
in some but not all cases [123]; hence, the molecular link
between prolactin and increased adiposity remains elusive.
Acute leptin treatment did not affect prolactin levels in fed
or fasted rats [209]. In contrast, a constant infusion of leptin in
fed rats prevented the fall in prolactin [209]. Moreover,
higher doses of leptin led to further increases in prolactin in
fasted animals. Thus, as with other pituitary hormones,
prolactin is more responsive to leptin deficiency during
fasting [2,151,197]. LEPR is very scant in lactotropes,
arguing against a significant direct effect of leptin. Moreover,
because leptin infusion into the arcuate nucleus and median
eminence complex stimulates prolactin secretion, it is likely
that leptin controls prolactin release via a hypothalamic target
[208]. Conversely, prolactin has been shown to stimulate
leptin secretion from rat adipose tissue [94].
6.7. Melatonin
Melatonin declines with aging in humans and rat, while
visceral fat, insulin and leptin levels increase [169]. In
contrast, melatonin treatment reversed the aging-associated
increase in retroperitoneal and epididymal fat, plasma insulin and leptin levels to youthful levels [169]. In the same
study, corticosterone and T4 were not significantly altered
by aging or melatonin treatment. Moreover, while plasma
testosterone, IGF-I and T3 declined by middle age, these
changes were not affected by melatonin treatment. Interestingly, melatonin decreased visceral adiposity, leptin and
R.S. Ahima, S.Y. Osei / Physiology & Behavior 81 (2004) 223241
insulin without altering food intake [213]. Taken together
with the ability of pinealectomy to increase leptin, these
findings suggest that melatonin exerts an inhibitory effect on
leptin release [26].
A rare condition known as the night-eating syndrome
(NES) may provide a link between body fat, leptin and
melatonin. NES patients are typically obese, and have
morning anorexia, evening hyperphagia and insomnia
[16]. Analysis of their neuroendocrine profile has revealed
higher cortisol level, as well as attenuation of the nocturnal
increase in plasma melatonin and leptin levels [16]. The
molecular basis of these behavioral and hormonal alterations
remains to be determined.
7. Other actions of leptin
Leptin exerts acute and long-term systemic effects,
independent of its role in body weight regulation (reviewed
in Ref. [5]). For example, peripheral or intracerebroventricular leptin administration rapidly decreases glucose and
insulin in ob/ob mice before weight loss. Leptin also
regulates glucose and lipids in wild-type rodents in part
through stimulation of gluconeogenesis and increased lipolysis. Expression of leptin in the stomach is believed to act
locally to influence satiety, through regulation of cholecystokinin and gastrin. Placental leptin increases in response to
hypoxia, and is strongly correlated with low birthweight.
Leptin regulates skeletal muscle metabolism, hematopoiesis,
immune function, angiogenesis, wound healing and brain
development. Many of these tissues express LEPRb and
downstream leptin gene targets, suggesting a direct effect of
leptin. Surprisingly, leptin deficiency is associated with
increased bone mass in rodents, despite hypogonadism
and high glucocorticoids which are well known to decrease
bone mass [58,196]. Studies have suggested that the effect
of leptin on bone in rodents is mediated through central
sympathetic neuronal pathways [196]. This finding, if
confirmed in humans, would have enormous therapeutic
implications for osteoporosis and other bone diseases.
233
the caudal regions of the nucleus ventral to the pars
compacta. LEPRb mRNA is localized mainly to the dorsomedial division of the ventromedial nucleus (VMN) with
much less hybridization in the ventrolateral VMN [64]. In
contrast, LEPRb is prominent throughout the arcuate nucleus, extending from the retrochiasmatic region to the posterior periventricular region. Moderate expression of LEPRb
is also detectable in the periventricular hypothalamic nucleus, medial mammillary nucleus and posterior hypothalamic
nucleus. A low level of LEPRb mRNA is detectable within
the parvicellular division of the PVN and LHA [64].
Unlike LEPRb, short LEPR isoforms are distributed
widely in the choroid plexus, meninges and surrounding
blood vessels in the brain parenchyma [19,64]. The presence
of LEPR mRNA in the meninges and microvessels raises
the possibility that LEPRs are responsible for transporting
leptin in or out of the brain. Leptin may enter the brain
through circumventricular organs, i.e., regions lacking a
blood brain barrier, including the median eminence, subfornical organ, organum vasculosum of the lamina terminalis, median eminence and area postrema [19]. Because the
arcuate nucleus lies adjacent to the median eminence, it is
possible that leptin diffuses to neurons in this region through
the median eminence. However, transport via the circumventricular organs cannot explain how leptin reaches deeper
structures, such as the cerebellum and thalamus, where
LEPRs have been localized [19,64]. Rather, it has been
suggested that LEPRs located in the brain microvasculature
and choroid plexus mediate leptin transport [19,64].
Hypothalamic neuropeptides involved in leptin action
have been classified into two major groups (Table 2).
Orexigenic peptides stimulate appetite, and are inhibited
by leptin and increase in response to leptin deficiency.
Anorexigenic peptides, which inhibit feeding, are stimulated by leptin and decrease in response to leptin deficiency. Orexigenic peptides include NPY, AGRP, melaninconcentrating hormone (MCH) and orexins (ORX), while
a-MSH (derived from POMC), CART and CRH are major
Table 2
Neurotransmitters and peptide targets of leptin
Stimulate feeding
Inhibit feeding
8. Central neuronal circuitry for leptin
Neuropeptide Y (NPY)
The findings discussed above indicate that leptin has
profound effects on energy homeostasis and neuroendocrine
systems. Leptin regulates specific neuronal groups within
the hypothalamus, brainstem and other regions of the brain
[5,65,95]. Here, we will focus mainly on leptin targets in the
hypothalamus. The long LEPR and LEPRb is enriched in
the hypothalamus, especially in ventrobasal hypothalamic
nuclei implicated in feeding behavior, thermogenesis and
hormone regulation [64,98]. For example, LEPRb mRNA is
present in the arcuate, dorsomedial, ventromedial and ventral premamillary hypothalamic nuclei. Within the dorsomedial nucleus (DMN), intense hybridization is present in
Agouti-related
peptide (AGRP)
Alpha-melanocyte
stimulating hormone (a-MSH)
Cocaine and
amphetamine-regulated
transcript (CART)
Corticotropin-releasing
hormone (CRH)
Neurotensin
Urocortin
Serotonin
Cholecystokinin (CCK)
Melanin-concentrating
hormone (MCH)
Orexins
Ghrelin
Galanin
Growth
hormone-releasing
hormone (GHRH)
Opioid peptides
g-Aminobutyric acid
(GABA)
Glucagon-like peptide-1 (GLP-1)
Bombesin
234
R.S. Ahima, S.Y. Osei / Physiology & Behavior 81 (2004) 223241
Fig. 2. A schematic drawing showing the connections between leptin target neurons in the hypothalamus, brainstem and peripheral targets. Leptin directly
inhibits NPY/AGRP neurons and stimulates a-MSH/CART neurons in the arcuate nucleus. These neurons project to second order neurons in the PVN and
LHA. The PVN receives input from the gastrointestinal tract via the brainstem nuclei, e.g., nucleus tractus solitarius (NTS) and lateral parabrachial nucleus
(LPB), and regulates feeding, hormone synthesis/secretion and autonomic outflow.
anorexigenic neuropeptides (Table 2). NPY, AGRP and
LEPRb mRNAs are coexpressed in the arcuate nucleus
(Figs. 2 and 3). Ablation of the arcuate nucleus disrupts
leptin response [54]. Importantly, targeted ablation of
neuronal LEPRb produced a phenotype similar to db/db
mice, suggesting that this LEPR mediates most of the
metabolic and hormonal actions of leptin in the brain [43].
Although NPY is a major leptin target, deletion of the
NPY or its receptors had little effect or did not complete-
ly reverse the obese phenotype in ob/ob mice, indicating
that other neuropeptides and neurotransmitters play significant roles in the transmission of the leptin signal
[67,68,152,153,178].
POMC neurons in the arcuate nucleus coexpress LEPRb
[5,19] (Fig. 3). The POMC gene product, a-MSH, is a
potent anorectic peptide, which acts as an agonist of
MCRs in the PVN and other regions of the hypothalamus.
AGRP (colocalized with NPY) is distributed to similar
Fig. 3. Leptin, ghrelin, NPY and melanocortin target neurons in the hypothalamus. Leptin directly regulates NPY/AGRP and POMC/CART neurons in the
arcuate nucleus. NPY stimulates feeding via Y1 and Y5 receptors. The Y2 receptor acts presynaptically to regulate NPY release at the POMC (a-MSH) neuron.
The effect of NPY is modulated by ghrelin derived from the circulation or produced locally in the hypothalamus. AGRP antagonizes a-MSH action at MC4/3
receptors, resulting in appetite stimulation, reduced energy expenditure and weight gain. GHS-R: growth hormone secretagogue receptor.
R.S. Ahima, S.Y. Osei / Physiology & Behavior 81 (2004) 223241
hypothalamic regions, such as PVN, perifornical and LHA,
and acts as an antagonist of a-MSH. Neurons containing
MC4Rs localize to the PVN (Fig. 3), DMN and LHA [65]
(Fig. 3). MC4R is thought to mediate appetite suppression,
whereas MC3R decreases body weight through stimulation
of thermogenesis. Additional molecules that contribute to
the regulation of feeding include CART, galanin, MCH
and ORX, ghrelin, GLP-1, CCK and monoamines [65]
(Table 2).
We have addressed the question of whether different
populations of hypothalamic neurons respond differently to
changes in plasma leptin concentration [2]. Leptin was
infused by constant subcutaneous infusion in ad libitum
fed rodents to mimic the rise in plasma leptin as would
occur during overfeeding and obesity [2]. Conversely, we
administered leptin by constant subcutaneous infusion to
prevent the characteristic fall in plasma leptin with fasting
[2]. Chronic leptin elevation to the mildly obese range
elicited a transient suppression of feeding and sustained
reduction in body weight. NPY mRNA expression in the
arcuate hypothalamic nucleus decreased in a dose-related
manner. Insulin, T4 and testosterone were not affected.
Moreover, major anorexigenic peptides, e.g., CRH, POMC
and CART mRNA levels, were not affected by a rise in
leptin from fed to obese levels [2]. In contrast, leptin
replacement during fasting markedly blunted the suppression of T4 and testosterone, as well as the rise in
glucocorticoids and changes in hypothalamic NPY, POMC
and CART mRNA levels [2]. Postfast hyperphagia and
weight gain were also potently attenuated by leptin replacement. Taken together, these results suggest that the
sensing of the leptin by hypothalamic neurons is skewed
towards detection of low levels during starvation [2,81].
The rise in orexigenic peptides in conjunction with reduced expression of anorexigenic peptides is likely aimed
at optimizing food intake during starvation. Leptin-sensitive hypothalamic peptides are also likely to couple gonadal, adrenal and thyroid function with alterations in
energy stores [2,81].
The PVN is uniquely positioned to transduce the leptin
signal during periods of changing energy availability, as it
possesses chemically specific projections to autonomic and
endocrine control sites involved in maintenance of homeostasis (reviewed in Refs. [5,65]; Figs. 2 and 3). For example,
the parvicellular neurons in the medial PVN control secretion of hormones, including TSH, growth hormone and
ACTH. The PVN has also been implicated in control of
feeding behavior, as lesions of the PVN induce hyperphagia
and obesity. The PVN expresses low levels of LEPR, but is
richly innervated by leptin-sensitive neurons in the arcuate
nucleus, DMN and brainstem [5,65]. Neurons in the dorsal,
ventral and lateral PVN provide autonomic preganglionic
neurons projection to the medulla and spinal cord, to control
the gastrointestinal system and brown adipose tissue [5,65].
The largest number of leptin-activated neurons that
project to the PVN is located in the DMN [5,64,65]. This
235
nucleus lies caudal to the PVN and dorsal to the VMN, and
has been implicated in regulation of ingestive behavior,
insulin secretion and cardiovascular and neuroendocrine
systems. A major target of DMN efferents is the PVN,
specifically the dorsal, ventral and lateral parvicellular
subdivisions that directly innervate parasympathetic and
sympathetic preganglionic in the medulla and spinal cord.
Lesions of the DMN alter pancreatic neural activity, while
stimulation of the DMN increases glucose, presumably
through interactions with the parasympathetic (dorsal motor
nucleus of the vagus) and sympathetic (intermediolateral
cell column of the spinal cord) preganglionic neurons.
Because the DMN contains LEPRs, expresses SOCS-3
mRNA and Fos-immunoreactive cells following leptin administration, and heavily innervates the PVN, it is plausible
that this nuclear group contributes significantly to leptins
effects on body weight, and control of the neuroendocrine
axis, insulin and glucose levels, blood pressure and body
temperature [5,65].
Ablation of VMN abolishes leptin response [181]. However, because relatively few cells in this region express
LEPR, it is likely that leptin engages the VMN via an
indirect pathway [64]. Fos immunoreactivity, a marker of
neuronal activation, is induced in the dorsomedial VMN in
response to leptin injection [64]. The dorsomedial VMN
projects to the subparaventricular zone (SPVZ) that receives
a dense innervation from the suprachiasmatic nucleus, the
circadian pacemaker of the mammalian brain [5]. The SPVZ
also interacts with PVN. Thus, input from the VMN to
SPVZ may couple leptin-mediated regulation of feeding to
sleep wake cycles to hormone rhythms, as manifested by
the link between nutrition and circadian glucocorticoid
rhythm [3,179,182]. VMN neurons also respond to glucose,
and could provide an interphase between long-term regulation of body weight by leptin and short-term effects of
nutrients [65].
The LHA is well known to regulate feeding; however,
there are very few, if any, LEPR positive cells in this
region [64]. Detailed anatomic studies have revealed that
arcuate hypothalamic NPY/AGRP and POMC/CART neurons, which respond directly to leptin, innervate the LHA,
adjacent perifornical area and zona incerta [56,64] (Figs.
2 and 3). The LHA contains two major neuropeptides,
MCH and the ORX (also called hypocretins), expressed
in separate neuronal populations [24]. Both cell groups
contribute to the lateral hypothalamic neuronal projections
from the cerebral cortex to the spinal cord to regulate
complex physiologic functions. The levels of MCH and
ORX are increased by leptin deficiency and decreased in
response to leptin treatment [65]. Apart from regulating
feeding and body weight, both MCH and ORX also
influence sleep wake cycles, and are likely to integrate
the latter with energy balance [5,65]. Ultimately, these
diverse mechanisms need to be connected to neural
networks producing specific behavioral effects of leptin,
e.g., reduction in meal size [60,82], regulation of brain
236
R.S. Ahima, S.Y. Osei / Physiology & Behavior 81 (2004) 223241
reward responses [77] and coordination of neuroendocrine
responses [5].
9. Conclusion
Advances in molecular biology and genetics have extended our understanding of mechanisms underlying feeding behavior, energy homeostasis, neuroendocrine
regulation and other complex physiologic systems. Here,
we have discussed the studies leading to the discovery of
leptin and its receptors, control of leptin production and
transport, cellular signaling and neuronal pathways for
leptin action in the brain. We have discussed how leptin
might improve glucose and lipids, aside from regulating
food intake and metabolic rate. The diverse mechanisms
linking leptin to the brain and peripheral tissues will clarify
the pathogenesis of obesity and associated diseases, and
facilitate the development of rationale therapeutic strategies.
Acknowledgements
This work was supported by grant P30DK19525 from
the National Institutes of Health.
References
[1] Ahima RS, Dushay J, Flier SN, Prabakaran D, Flier JS. Leptin
accelerates the onset of puberty in normal female mice. J Clin Invest
1997;99:91 395.
[2] Ahima RS, Kelly J, Elmquist JK, Flier JS. Distinct physiologic and
neuronal responses to decreased leptin and mild hyperleptinemia.
Endocrinology 1999;140:4923 31.
[3] Ahima RS, Prabakaran D, Flier JS. Postnatal leptin surge and regulation of circadian rhythm of leptin by feeding. Implications for
energy homeostasis and neuroendocrine function. J Clin Invest
1998;101:1020 7.
[4] Ahima RS, Prabakaran D, Mantzoros C, Qu D, Lowell B, MaratosFlier E, et al. Role of leptin in the neuroendocrine response to fasting. Nature 1996;382:250 2.
[5] Ahima RS, Saper CB, Flier JS, Elmquist JK. Leptin regulation of
neuroendocrine systems. Front Neuroendocrinol 2000;21:263 307.
[6] Anand BK, Brobeck JR. Localization of a feeding center in the
hypothalamus of the rat. Proc Soc Exp Biol Med 1951;77:323 4.
[7] Bado A, Levasseur S, Attoub S, Kermorgant S, Laigneau JP, Bortoluzzi MN, et al. The stomach is a source of leptin. Nature
1998;394:790 3.
[8] Bahrenberg G, Behrmann I, Barthel A, Hekerman P, Heinrich PC,
Joost HG, et al. Identification of the critical sequence elements in the
cytoplasmic domain of leptin receptor isoforms required for Janus
kinase/signal transducer and activator of transcription activation by
receptor heterodimers. Mol Endocrinol 2002;16:859 72.
[9] Banks WA, DiPalma CR, Farrell CL. Impaired transport of leptin
across the blood brain barrier in obesity. Peptides 1999;20:1341 5.
[10] Banks WA, Kastin AJ, Huang W, Jaspan JB, Maness LM. Leptin
enters the brain by a saturable system independent of insulin. Peptides 1996;17:305 11.
[11] Bannon AW, Seda J, Carmouche M, Francis JM, Norman MH, Karbon B, et al. Behavioral characterization of neuropeptide Y knockout
mice. Brain Res 2000;16:79 87.
[12] Barash IA, Cheung CC, Weigle DS, Ren H, Kabigting EB, Kuijper
JL, et al. Leptin is a metabolic signal to the reproductive system.
Endocrinology 1996;137:3144 7.
[13] Barr VA, Malide D, Zarnowski MJ, Taylor SI, Cushman SW. Insulin
stimulates both leptin secretion and production by rat white adipose
tissue. Endocrinology 1997;138:4463 72.
[14] Bates SH, Stearns WH, Dundon TA, Schubert M, Tso AW, Wang Y,
et al. STAT3 signalling is required for leptin regulation of energy
balance but not reproduction. Nature 2003;421:856 9.
[15] Bergen HT, Mizuno T, Taylor J, Mobbs CV. Resistance to diet-induced obesity is associated with increased proopiomelanocortin
mRNA and decreased neuropeptide Y mRNA in the hypothalamus.
Brain Res 1999;85:198 203.
[16] Birketvedt GS, Florholmen J, Sundsfjord J, Osterud B, Dinges D,
Bilker W, et al. Behavioral and neuroendocrine characteristics of the
night-eating syndrome. JAMA 1999;282:657 63.
[17] Bjorbaek C, El-Haschimi K, Frantz JD, Flier JS. The role of SOCS-3
in leptin signaling and leptin resistance. J Biol Chem 1999;274:
30059 65.
[18] Bjorbaek C, Elmquist JK, Frantz JD, Shoelson SE, Flier JS. Identification of SOCS-3 as a potential mediator of central leptin resistance. Mol Cell 1998;1:619 25.
[19] Bjorbaek C, Elmquist JK, Michl P, Ahima RS, van Bueren A,
McCall AL, et al. Expression of leptin receptor isoforms in rat brain
microvessels. Endocrinology 1998;139:3485 91.
[20] Bjorbaek C, Uotani S, da Silva B, Flier JS. Divergent signaling
capacities of the long and short isoforms of the leptin receptor. J
Biol Chem 1997;272:32686 95.
[21] Boden G, Chen X, Mozzoli M, Ryan I. Effect of fasting on serum
leptin in normal human subjects. J Clin Endocrinol Metab 1996;81:
3419 23.
[22] Bornstein SR, Licinio J, Tauchnitz R, Engelmann L, Negrao AB,
Gold P, et al. Plasma leptin levels are increased in survivors of
acute sepsis: associated loss of diurnal rhythm, in cortisol and
leptin secretion. J Clin Endocrinol Metab 1998;83:280 3.
[23] Bornstein SR, Uhlmann K, Haidan A, Ehrhart-Bornstein M, Scherbaum WA. Evidence for a novel peripheral action of leptin as a
metabolic signal to the adrenal gland: leptin inhibits cortisol release
directly. Diabetes 1997;46:1235 8.
[24] Broberger C, De Lecea L, Sutcliffe JG, Hokfelt T. Hypocretin/
orexin- and melanin-concentrating hormone-expressing cells form
distinct populations in the rodent lateral hypothalamus: relationship
to the neuropeptide Y and agouti gene-related protein systems. J
Comp Neurol 1998;402:460 74.
[25] Campfield LA, Smith FJ, Guisez Y, Devos R, Burn P. Recombinant
mouse OB protein: evidence for a peripheral signal linking adiposity
and central neural networks. Science 1995;269:546 9.
[26] Canpolat S, Sandal S, Yilmaz B, Yasar A, Kutlu S, Baydas G, et al.
Effects of pinealectomy and exogenous melatonin on serum leptin
levels in male rat. Eur J Pharmacol 2001;428:145 8.
[27] Caro JF, Kolaczynski JW, Nyce MR, Ohannesian JP, Opentanova I,
Goldman WH, et al. Decreased cerebrospinal-fluid/serum leptin ratio
in obesity: a possible mechanism for leptin resistance. Lancet 1996;
348:159 61.
[28] Carpenter LR, Farruggella TJ, Symes A, Karow ML, Yancopoulos GD, Stahl N. Enhancing leptin response by preventing SH2-containing phosphatase 2 interaction with Ob receptor. Proc Natl Acad
Sci U S A 1998;95:6061 6.
[29] Carro E, Pinilla L, Seoane LM, Considine RV, Aguilar E, Casanueva
FF, et al. Influence of endogenous leptin tone on the estrous cycle
and luteinizing hormone pulsatility in female rats. Neuroendocrinology 1997;66:375 7.
[30] Carro E, Senaris R, Considine RV, Casanueva FF, Dieguez C. Regulation of in vivo growth hormone secretion by leptin. Endocrinology 1997;138:2203 6.
[31] Carro E, Senaris RM, Seoane LM, Frohman LA, Arimura A, Casanueva FF, et al. Role of growth hormone (GH)-releasing hormone
R.S. Ahima, S.Y. Osei / Physiology & Behavior 81 (2004) 223241
[32]
[33]
[34]
[35]
[36]
[37]
[38]
[39]
[40]
[41]
[42]
[43]
[44]
[45]
[46]
[47]
[48]
[49]
[50]
[51]
and somatostatin on leptin-induced GH secretion. Neuroendocrinology 1999;69:3 10.
Casabiell X, Pineiro V, Peino R, Lage M, Camina J, Gallego R, et al.
Gender differences in both spontaneous and stimulated leptin secretion by human omental adipose tissue in vitro: dexamethasone and
estradiol stimulate leptin release in women, but not in men. J Clin
Endocrinol Metab 1998;83:2149 55.
Castracane VD, Kraemer RR, Franken MA, Kraemer GR, Gimpel T.
Serum leptin concentration in women: effect of age, obesity, and
estrogen administration. Fertil Steril 1998;70:472 7.
Chan JL, Heist K, DePaoli AM, Veldhuis JD, Mantzoros CS. The
role of falling leptin levels in the neuroendocrine and metabolic
adaptation to short-term starvation in healthy men. J Clin Invest
2003;111:1409 21.
Chehab FF, Lim ME, Lu R. Correction of the sterility defect in
homozygous obese female mice by treatment with the human recombinant leptin. Nat Genet 1996;12:318 20.
Chehab FF, Mounzih K, Lu R, Lim ME. Early onset of reproductive
function in normal female mice treated with leptin. Science
1997;275:88 90.
Chen D, Misra A, Garg A. Clinical review 153: lipodystrophy in
human immunodeficiency virus-infected patients. J Clin Endocrinol
Metab 2002;87:4845 56.
Chen H, Charlat O, Tartaglia LA, Woolf EA, Weng X, Ellis SJ, et al.
Evidence that the diabetes gene encodes the leptin receptor: identification of a mutation in the leptin receptor gene in db/db mice. Cell
1996;84:491 5.
Cheung CC, Thornton JE, Kuijper JL, Weigle DS, Clifton DK,
Steiner RA. Leptin is a metabolic gate for the onset of puberty in
the female rat. Endocrinology 1997;138:855 8.
Chua Jr SC, Chung WK, Wu-Peng XS, Zhang Y, Liu SM, Tartaglia
L, et al. Phenotypes of mouse diabetes and rat fatty due to mutations in the OB (leptin) receptor. Science 1996;271:994 6.
Chung WK, Belfi K, Chua M, Wiley J, Mackintosh R, Nicolson
M, et al. Heterozygosity for Lep(ob) or Lep(rdb) affects body
composition and leptin homeostasis in adult mice. Am J Physiol
1998;274:R985 90.
Clement K, Vaisse C, Lahlou N, Cabrol S, Pelloux V, Cassuto D, et al.
A mutation in the human leptin receptor gene causes obesity and
pituitary dysfunction. Nature 1998;392:398 401.
Cohen P, Zhao C, Cai X, Montez M, Rohani SC, Feinstein P, et al.
Selective deletion of leptin receptor in neurons leads to obesity. J
Clin Invest 2001;108:1113 21.
Coleman DL. Effects of parabiosis of obese with diabetes and normal
mice. Diabetologia 1973;9:294 8.
Coleman DL. Obese and diabetes: two mutant genes causing diabetes obesity syndromes in mice. Diabetologia 1978;14:141 8.
Colombo C, Cutson JJ, Yamauchi T, Vinson C, Kadowaki T, Gavrilova O, et al. Transplantation of adipose tissue lacking leptin is
unable to reverse the metabolic abnormalities associated with lipoatrophy. Diabetes Sep. 2002;51(9):2727 33.
Considine RV, Sinha MK, Heiman ML, Kriauciunas A, Stephens
TW, Nyce MR, et al. Serum immunoreactive-leptin concentrations
in normal-weight and obese humans. N Engl J Med 1996;
334:292 5.
Costa A, Poma A, Martignoni E, Nappi G, Ur E, Grossman A.
Stimulation of corticotrophin-releasing hormone release by the obese
(ob) gene product, leptin, from hypothalamic explants. NeuroReport
1997;8:1131 4.
Cowley MA, Smart JL, Rubinstein M, Cerdan MG, Diano S, Horvath TL, et al. Leptin activates anorexigenic POMC neurons through
a neural network in the arcuate nucleus. Nature 2001;411:480 4.
Cowley MA, Smith RG, Diano S, Tschop M, Pronchuk N, Grove
KL, et al. The distribution and mechanism of action of ghrelin in the
CNS demonstrates a novel hypothalamic circuit regulating energy
homeostasis. Neuron 2003;37:649 61.
Cusin I, Rohner-Jeanrenaud F, Stricker-Krongrad A, Jeanrenaud B.
[52]
[53]
[54]
[55]
[56]
[57]
[58]
[59]
[60]
[61]
[62]
[63]
[64]
[65]
[66]
[67]
[68]
[69]
[70]
[71]
237
The weight-reducing effect of an intracerebroventricular bolus injection of leptin in genetically obese fa/fa rats. Reduced sensitivity
compared with lean animals. Diabetes 1996;45:1446 50.
da Silva BA, Bjorbaek C, Uotani S, Flier JS. Functional properties of
leptin receptor isoforms containing the gln ! pro extracellular domain mutation of the fatty rat [see comments]. Endocrinology
1998;139:3681 90.
Dagogo-Jack S, Selke G, Melson AK, Newcomer JW. Robust leptin
secretory responses to dexamethasone in obese subjects. J Clin
Endocrinol Metab 1997;82:3230 3.
Dawson R, Pelleymounter MA, Millard WJ, Liu S, Eppler B. Attenuation of leptin-mediated effects by monosodium glutamate-induced
arcuate nucleus damage. Am J Physiol 1997;273:E202 6.
Devaskar SU, Ollesch C, Rajakumar RA, Rajakumar PA. Developmental changes in ob gene expression and circulating leptin peptide
concentrations. Biochem Biophys Res Commun 1997;238:44 7.
Diekman MJ, Romijn JA, Endert E, Sauerwein H, Wiersinga WM.
Thyroid hormones modulate serum leptin levels: observations in
thyrotoxic and hypothyroid women. Thyroid 1998;8:1081 6.
Donahoo WT, Jensen DR, Yost TJ, Eckel RH. Isoproterenol and
somatostatin decrease plasma leptin in humans: a novel mechanism regulating leptin secretion. J Clin Endocrinol Metab 1997;
82:4139 43.
Ducy P, Amling M, Takeda S, Priemel M, Schilling AF, Beil FT, et al.
Leptin inhibits bone formation through a hypothalamic relay: a central control of bone mass. Cell 2000;100:197 207.
Ebihara K, Ogawa Y, Masuzaki H, Shintani M, Miyanaga F, AizawaAbe M, et al. Transgenic overexpression of leptin rescues insulin
resistance and diabetes in a mouse model of lipoatrophic diabetes.
Diabetes 2001;50:1440 8.
Eckel LA, Langhans W, Kahler A, Campfield LA, Smith FJ, Geary
N. Chronic administration of OB protein decreases food intake by
selectively reducing meal size in female rats. Am J Physiol
1998;275:R186 93.
Elbers JM, Asscheman H, Seidell JC, Frolich M, Meinders AE,
Gooren LJ. Reversal of the sex difference in serum leptin levels
upon cross-sex hormone administration in transsexuals. J Clin Endocrinol Metab 1997;82:3267 70.
Elimam A, Knutsson U, Bronnegard M, Stierna P, Albertsson-Wikland K, Marcus C. Variations in glucocorticoid levels within the
physiological range affect plasma leptin levels. Eur J Endocrinol
1998;139:615 20.
El-Haschimi K, Pierroz DD, Hileman SM, Bjorbaek C, Flier JS. Two
defects contribute to hypothalamic leptin resistance in mice with
diet-induced obesity. J Clin Invest 2000;105:1827 32.
Elmquist JK, Bjorbaek C, Ahima RS, Flier JS, Saper CB. Distributions of leptin receptor mRNA isoforms in the rat brain. J Comp
Neurol 1998;395:535 47.
Elmquist JK, Elias CF, Saper CB. From lesions to leptin: hypothalamic control of food intake and body weight. Neuron 1999;
22:221 32.
Emilsson V, Arch JR, de Groot RP, Lister CA, Cawthorne MA.
Leptin treatment increases suppressors of cytokine signaling in central and peripheral tissues. FEBS Lett 1999;455:170 4.
Erickson JC, Clegg KE, Palmiter RD. Sensitivity to leptin and susceptibility to seizures of mice lacking neuropeptide Y. Nature 1996;
381:415 21.
Erickson JC, Hollopeter G, Palmiter RD. Attenuation of the obesity
syndrome of ob/ob mice by the loss of neuropeptide Y. Science
1996;274:1704 7.
Escobar-Morreale HF, Escobar del Rey F, Morreale de Escobar G.
Thyroid hormones influence serum leptin concentrations in the rat.
Endocrinology 1997;138:4485 8.
Ewart-Toland A, Mounzih K, Qiu J, Chehab FF. Effect of the genetic
background on the reproduction of leptin-deficient obese mice. Endocrinology 1999;140:732 8.
Fain JN, Bahouth SW. Regulation of lipolysis and leptin biosynthesis
238
[72]
[73]
[74]
[75]
[76]
[77]
[78]
[79]
[80]
[81]
[82]
[83]
[84]
[85]
[86]
[87]
[88]
[89]
[90]
[91]
R.S. Ahima, S.Y. Osei / Physiology & Behavior 81 (2004) 223241
in rodent adipose tissue by growth hormone. Metabolism 2000;49:
239 44.
Farooqi IS, Keogh JM, Kamath S, Jones S, Gibson WT, Trussell R,
et al. Partial leptin deficiency and human adiposity. Nature 2001;414:
34 5.
Farooqi IS, Matarese G, Lord GM, Keogh JM, Lawrence E, Agwu C,
et al. Beneficial effects of leptin on obesity, T cell hyporesponsiveness, and neuroendocrine/metabolic dysfunction of human congenital leptin deficiency. J Clin Invest 2002;110:1093 103.
Faust IM, Johnson PR, Hirsch J. Surgical removal of adipose tissue
alters feeding behavior and the development of obesity in rats. Science 1977;197:393 6.
Fekete C, Legradi G, Mihaly E, Huang QH, Tatro JB, Rand WM, et
al. alpha-Melanocyte-stimulating hormone is contained in nerve terminals innervating thyrotropin-releasing hormone-synthesizing neurons in the hypothalamic paraventricular nucleus and prevents
fasting-induced suppression of prothyrotropin-releasing hormone
gene expression. J Neurosci 2000;20:1550 8.
Fekete C, Sarkar S, Rand WM, Harney JW, Emerson CH, Bianco
AC, et al. Agouti-related protein (AGRP) has a central inhibitory
action on the hypothalamic pituitary thyroid (HPT) axis; comparisons between the effect of AGRP and neuropeptide Y on
energy homeostasis and the HPT axis. Endocrinology 2002;143:
3846 53.
Figlewicz DP. Adiposity signals and food reward: expanding the
CNS roles of insulin and leptin. Am J Physiol Regul Integr Comp
Physiol 2003;284:R882 92.
Finck BN, Kelley KW, Dantzer R, Johnson RW. In vivo and in vitro
evidence for the involvement of tumor necrosis factor-alpha in the
induction of leptin by lipopolysaccharide. Endocrinology 1998;139:
2278 83.
Finn PD, Cunningham MJ, Pau KY, Spies HG, Clifton DK, Steiner
RA. The stimulatory effect of leptin on the neuroendocrine reproductive axis of the monkey. Endocrinology 1998;139:4652 62.
Fisker S, Vahl N, Hansen TB, Jorgensen JO, Hagen C, Orskov H, et
al. Serum leptin is increased in growth hormone-deficient adults:
relationship to body composition and effects of placebo-controlled
growth hormone therapy for 1 year. Metabolism 1997;46:812 7.
Flier JS. Clinical review 94: whats in a name? In search of leptins
physiologic role. J Clin Endocrinol Metab 1998;83:1407 13.
Flynn MC, Scott TR, Pritchard TC, Plata-Salaman CR. Mode of action
of OB protein (leptin) on feeding. Am J Physiol 1998;275:R174 9.
Frederich RC, Hamann A, Anderson S, Lollmann B, Lowell BB, Flier
JS. Leptin levels reflect body lipid content in mice: evidence for dietinduced resistance to leptin action. Nat Med 1995;1:1311 4.
Friedman JM. Obesity in the new millennium. Nature 2000;404:
632 4.
Fruhbeck G, Gomez-Ambrosi J, Muruzabal FJ, Burrell MA. The
adipocyte: a model for integration of endocrine and metabolic signaling in energy metabolism regulation. Am J Physiol Endocrinol
Metab 2001;280:E827 47.
Garcia-Mayor RV, Andrade MA, Rios M, Lage M, Dieguez C, Casanueva FF. Serum leptin levels in normal children: relationship to age,
gender, body mass index, pituitary gonadal hormones, and pubertal
stage. J Clin Endocrinol Metab 1997;82:2849 55.
Garg A. Lipodystrophies. Am J Med 2000;108:143 52.
Gavrilova O, Marcus-Samuels B, Graham D, Kim JK, Shulman GI,
Castle AL, et al. Surgical implantation of adipose tissue reverses
diabetes in lipoatrophic mice. J Clin Invest 2000;105:271 8.
Ghilardi N, Ziegler S, Wiestner A, Stoffel R, Heim MH, Skoda RC.
Defective STAT signaling by the leptin receptor in diabetic mice.
Proc Natl Acad Sci U S A 1996;93:6231 5.
Gill MS, Toogood AA, Jones J, Clayton PE, Shalet SM. Serum leptin
response to the acute and chronic administration of growth hormone
(GH) to elderly subjects with GH deficiency. J Clin Endocrinol
Metab 1999;84:1288 95.
Glaum SR, Hara M, Bindokas VP, Lee CC, Polonsky KS, Bell GI,
[92]
[93]
[94]
[95]
[96]
[97]
[98]
[99]
[100]
[101]
[102]
[103]
[104]
[105]
[106]
[107]
[108]
[109]
[110]
[111]
[112]
[113]
[114]
et al. Leptin, the obese gene product, rapidly modulates synaptic
transmission in the hypothalamus. Mol Pharmacol 1996;50:230 5.
Golden PL, Maccagnan TJ, Pardridge WM. Human blood brain
barrier leptin receptor. Binding and endocytosis in isolated human
brain microvessels. J Clin Invest 1997;99:14 8.
Gong DW, Bi S, Pratley RE, Weintraub BD. Genomic structure and
promoter analysis of the human obese gene. J Biol Chem 1996;271:
3971 4.
Gualillo O, Lago F, Garcia M, Menendez C, Senaris R, Casanueva
FF, et al. Prolactin stimulates leptin secretion by rat white adipose
tissue. Endocrinology 1999;140:5149 53.
Grill HJ, Kaplan JM. The neuroanatomical axis for control of energy
balance. Front Neuroendocrinol 2002;23:2 40.
Gruaz NM, Lalaoui M, Pierroz DD, Englaro P, Sizonenko PC,
Blum WF, et al. Chronic administration of leptin into the lateral
ventricle induces sexual maturation in severely food-restricted female rats. J. Neuroendocrinol 1998;10:627 33.
Hakansson ML, Brown H, Ghilardi N, Skoda RC, Meister B. Leptin
receptor immunoreactivity in chemically defined target neurons of
the hypothalamus. J Neurosci 1998;18:559 72.
Hakansson ML, Meister B. Transcription factor STAT3 in leptin
target neurons of the rat hypothalamus. Neuroendocrinology 1998;
68:420 7.
Halaas JL, Gajiwala KS, Maffei M, Cohen SL, Chait BT, Rabinowitz
D, et al. Weight-reducing effects of the plasma protein encoded by
the obese gene. Science 1995;269:543 6.
Harris M, Aschkenasi C, Elias CF, Chandrankunnel A, Nillni EA,
Bjoorbaek C, et al. Transcriptional regulation of the thyrotropin-releasing hormone gene by leptin and melanocortin signaling. J Clin
Invest 2001;107:111 20.
Harris RB. Role of set-point theory in regulation of body weight.
FASEB J 1990;4:3310 8.
Harris RB, Kasser TR, Martin RJ. Dynamics of recovery of body
composition after overfeeding, food restriction or starvation of mature female rats. J Nutr 1986;116:2536 46.
Harris RB, Ramsay TG, Smith SR, Bruch RC. Early and late stimulation of ob mRNA expression in meal-fed and overfed rats. J Clin
Invest 1996;97:2020 6.
Harris RB, Zhou J, Redmann Jr SM, Smagin GN, Smith SR, Rodgers
E, et al. A leptin dose response study in obese (ob/ob) and lean (+/?)
mice. Endocrinology 1998;139:8 19.
He Y, Chen H, Quon MJ, Reitman M. The mouse obese gene. Genomic organization, promoter activity, and activation by CCAAT/enhancer-binding protein alpha. J Biol Chem 1995;270:28887 91.
Heiman ML, Ahima RS, Craft LS, Schoner B, Stephens TW, Flier
JS. Leptin inhibition of the hypothalamic pituitary adrenal axis in
response to stress. Endocrinology 1997;138:3859 63.
Hervey GR. The effects of lesions in the hypothalamus in parabiotic
rats. J Physiol (Lond) 1959;145:336 52.
Hetherington AW, Ranson SW. Hypothalamic lesions and adiposity
in the rat. Anat Rec 1940;78:149 72.
Heymsfield SB, Greenberg AS, Fujioka K, Dixon RM, Kushner R,
Hunt T, et al. Recombinant leptin for weight loss in obese and lean
adults: a randomized, controlled, dose-escalation trial. JAMA 1999;
282:1568 75.
Hileman SM, Pierroz DD, Flier JS. Leptin, nutrition, and reproduction: timing is everything. J Clin Endocrinol Metab 2000;85:804 7.
Hill RA, Margetic S, Pegg GG, Gazzola C. Leptin: its pharmacokinetics and tissue distribution. Int J Obes Relat Metab Disord 1998;22:
765 70.
Himms-Hagen J. Physiological roles of the leptin endocrine system:
differences between mice and humans. Crit Rev Clin Lab Sci
1999;36:575 655.
Houseknecht KL, Mantzoros CS, Kuliawat R, Hadro E, Flier JS, Kahn
BB. Evidence for leptin binding to proteins in serum of rodents and
humans: modulation with obesity. Diabetes 1996;45:1638 43.
Honda K, Narita K, Murata T, Higuchi T. Leptin affects the electrical
R.S. Ahima, S.Y. Osei / Physiology & Behavior 81 (2004) 223241
[115]
[116]
[117]
[118]
[119]
[120]
[121]
[122]
[123]
[124]
[125]
[126]
[127]
[128]
[129]
[130]
[131]
[132]
[133]
[134]
activity of neurones in the hypothalamic supraoptic nucleus. Brain
Res Bull 2002;57:721 5.
Horvath TL, Diano S, Sotonyi P, Heiman M, Tschop M. Minireview:
ghrelin and the regulation of energy balancea hypothalamic perspective. Endocrinology 2001;142:4163 9.
Huang Q, Rivest R, Richard D. Effects of leptin on corticotropinreleasing factor (CRF) synthesis and CRF neuron activation in the
paraventricular hypothalamic nucleus of obese (ob/ob) mice. Endocrinology 1998;139:1524 32.
Hwang CS, Mandrup S, MacDougald OA, Geiman DE, Lane MD.
Transcriptional activation of the mouse obese (ob) gene by CCAAT/
enhancer binding protein alpha. Proc Natl Acad Sci U S A
1996;93:873 7.
Isse N, Ogawa Y, Tamura N, Masuzaki H, Mori K, Okazaki T, et al.
Structural organization and chromosomal assignment of the human
obese gene. J Biol Chem 1995;270:27728 33.
Janik JE, Curti BD, Considine RV, Rager HC, Powers GC, Alvord
WG, et al. Interleukin 1 alpha increases serum leptin concentrations
in humans. J Clin Endocrinol Metab 1997;82:3084 6.
Jockenhovel F, Blum WF, Vogel E, Englaro P, Muller-Wieland D,
Reinwein D, et al. Testosterone substitution normalizes elevated serum leptin levels in hypogonadal men. J Clin Endocrinol Metab
1997;82:2510 3.
Kennedy GC. The role of depot fat in the hypothalamic control of
food intake in the rat. Proc R Soc Med 1953;140:578 96.
Kolaczynski JW, Ohannesian JP, Considine RV, Marco CC, Caro JF.
Response of leptin to short-term and prolonged overfeeding in
humans. J Clin Endocrinol Metab 1996;81:4162 5.
Kopelman PG. Physiopathology of prolactin secretion in obesity. Int
J Obes Relat Metab Disord 2000;24(Suppl. 2):S104 8.
Kowalski TJ, Liu SM, Leibel RL, Chua Jr SC. Transgenic complementation of leptin receptor deficiency: I. Rescue of the obesity/
diabetes phenotype of LEPR-null mice expressing a LEPR-B transgene. Diabetes 2001;50:425 35.
Kristrom B, Carlsson B, Rosberg S, Carlsson LM, Albertsson-Wikland K. Short-term changes in serum leptin levels provide a strong
metabolic marker for the growth response to growth hormone treatment in children. Swedish Study Group for Growth Hormone Treatment. J Clin Endocrinol Metab 1998;83:2735 41.
Larsson H, Ahren B. Short-term dexamethasone treatment increases
plasma leptin independently of changes in insulin sensitivity in
healthy women. J Clin Endocrinol Metab 1996;81:4428 32.
Laughlin GA, Morales AJ, Yen SS. Serum leptin levels in women
with polycystic ovary syndrome: the role of insulin resistance/hyperinsulinemia. J Clin Endocrinol Metab 1997;82:1692 6.
Laughlin GA, Yen SS. Hypoleptinemia in women athletes: absence
of a diurnal rhythm with amenorrhea. J Clin Endocrinol Metab
1997;82:318 21.
Lee GH, Proenca R, Montez JM, Carroll KM, Darvishzadeh JG, Lee
JJ, et al. Abnormal splicing of the leptin receptor in diabetic mice.
Nature 1996;379:632 5.
Lee Y, Wang MY, Kakuma T, Wang ZW, Babcock E, McCorkle K,
et al. Liporegulation in diet-induced obesity. The antisteatotic role
of hyperleptinemia. J Biol Chem 2001;276:5629 35.
Legradi G, Emerson CH, Ahima RS, Rand WM, Flier JS, Lechan
RM. Arcuate nucleus ablation prevents fasting-induced suppression
of ProTRH mRNA in the hypothalamic paraventricular nucleus.
Neuroendocrinology 1998;68:89 97.
Li H, Matheny M, Scarpace PJ. beta 3-Adrenergic-mediated suppression of leptin gene expression in rats. Am J Physiol 1997;272:
E1031 6.
Licinio J, Mantzoros C, Negrao AB, Cizza G, Wong ML, Bongiorno
PB, et al. Human leptin levels are pulsatile and inversely related to
pituitary adrenal function. Nat Med 1997;3:575 9.
Licinio J, Negrao AB, Mantzoros C, Kaklamani V, Wong ML,
Bongiorno PB, et al. Synchronicity of frequently sampled, 24h concentrations of circulating leptin, luteinizing hormone, and
[135]
[136]
[137]
[138]
[139]
[140]
[141]
[142]
[143]
[144]
[145]
[146]
[147]
[148]
[149]
[150]
[151]
[152]
[153]
[154]
239
estradiol in healthy women. Proc Natl Acad Sci U S A 1998;
95:2541 6.
Licinio J, Negrao AB, Mantzoros C, Kaklamani V, Wong ML, Bongiorno PB, et al. Sex differences in circulating human leptin pulse
amplitude: clinical implications. J Clin Endocrinol Metab 1998;83:
4140 7.
Lord G. Role of leptin in immunology. Nutr Rev 2002;60:S35 8.
MacDougald OA, Hwang CS, Fan H, Lane MD. Regulated expression of the obese gene product (leptin) in white adipose tissue and
3T3-L1 adipocytes. Proc Natl Acad Sci U S A 1995;92:9034 7.
Maffei M, Halaas J, Ravussin E, Pratley RE, Lee GH, Zhang Y, et al.
Leptin levels in human and rodent: measurement of plasma leptin
and ob RNA in obese and weight-reduced subjects. Nat Med 1995;1:
1155 61.
Mantzoros CS, Flier JS, Rogol AD. A longitudinal assessment of
hormonal and physical alterations during normal puberty in boys: V.
Rising leptin levels may signal the onset of puberty. J Clin Endocrinol Metab 1997;82:1066 70.
Mantzoros CS, Rosen HN, Greenspan SL, Flier JS, Moses AC.
Short-term hyperthyroidism has no effect on leptin levels in man.
J Clin Endocrinol Metab 1997;82:497 9.
Marzullo P, Buckway C, Pratt KL, Colao A, Guevara-Aguirre J,
Rosenfeld RG. Leptin concentrations in GH deficiency: the effect
of GH insensitivity. J Clin Endocrinol Metab 2002;87:540 5.
Masuzaki H, Ogawa Y, Hosoda K, Miyawaki T, Hanaoka I, Hiraoka
J, et al. Glucocorticoid regulation of leptin synthesis and secretion in
humans: elevated plasma leptin levels in Cushings syndrome. J Clin
Endocrinol Metab 1997;82:2542 7.
Masuzaki H, Ogawa Y, Sagawa N, Hosoda K, Matsumoto T, Mise H,
et al. Nonadipose tissue production of leptin: leptin as a novel placenta-derived hormone in humans. Nat Med 1997;3:1029 33.
Mise H, Sagawa N, Matsumoto T, Yura S, Nanno H, Itoh H, et al.
Augmented placental production of leptin in preeclampsia: possible
involvement of placental hypoxia. J Clin Endocrinol Metab 1998;
83:3225 9.
Mistry AM, Swick A, Romsos DR. Leptin alters metabolic rates
before acquisition of its anorectic effect in developing neonatal mice.
Am J Physiol 1999;277:R742 7.
Montague CT, Farooqi IS, Whitehead JP, Soos MA, Rau H, Wareham NJ, et al. Congenital leptin deficiency is associated with severe
early-onset obesity in humans. Nature 1997;387:903 8.
Morash B, Li A, Murphy PR, Wilkinson M, Ur E. Leptin gene
expression in the brain and pituitary gland. Endocrinology 1999;
140:5995 8.
Mounzih K, Qiu J, Ewart-Toland A, Chehab FF. Leptin is not necessary for gestation and parturition but regulates maternal nutrition via a
leptin resistance state. Endocrinology 1998;139:5259 62.
Murakami T, Iida M, Shima K. Dexamethasone regulates obese
expression in isolated rat adipocytes. Biochem Biophys Res Commun 1995;214:1260 7.
Muraoka O, Xu B, Tsurumaki T, Akira S, Yamaguchi T, Higuchi H.
Leptin-induced transactivation of NPY gene promoter mediated by
JAK1, JAK2 and STAT3 in the neural cell lines. Neurochem Int
2003;42:591 601.
Nagatani S, Guthikonda P, Thompson RC, Tsukamura H, Maeda KI,
Foster DL. Evidence for GnRH regulation by leptin: leptin administration prevents reduced pulsatile LH secretion during fasting. Neuroendocrinology 1998;67:370 6.
Naveilhan P, Hassani H, Canals JM, Ekstrand AJ, Larefalk A, Chhajlani V, et al. Normal feeding behavior, body weight and leptin response
require the neuropeptide Y Y2 receptor. Nat Med 1999;5:1188 93.
Naveilhan P, Svensson L, Nystrom S, Ekstrand AJ, Ernfors P. Attenuation of hypercholesterolemia and hyperglycemia in ob/ob mice
by NPY Y2 receptor ablation. Peptides 2002;23:1087 91.
Niswender KD, Schwartz MW. Insulin and leptin revisited: adiposity
signals with overlapping physiological and intracellular signaling
capabilities. Front Neuroendocrinol 2003;24:1 10.
240
R.S. Ahima, S.Y. Osei / Physiology & Behavior 81 (2004) 223241
[155] Oral EA, Ruiz E, Andewelt A, Sebring N, Wagner AJ, Depaoli AM,
et al. Effect of leptin replacement on pituitary hormone regulation in
patients with severe lipodystrophy. J Clin Endocrinol Metab 2002;
87:3110 7.
[156] Oral EA, Simha V, Ruiz E, Andewelt A, Premkumar A, Snell P, et al.
Leptin-replacement therapy for lipodystrophy. N Engl J Med 2002;
346:570 8.
[157] Ozata M, Dieguez C, Casanueva FF. The inhibition of growth hormone secretion presented in obesity is not mediated by the high
leptin levels: a study in human leptin deficiency patients. J Clin
Endocrinol Metab 2003;88:312 6.
[158] Ozata M, Ozdemir IC, Licinio J. Human leptin deficiency caused
by a missense mutation: multiple endocrine defects, decreased sympathetic tone, and immune system dysfunction indicate new targets
for leptin action, greater central than peripheral resistance to the
effects of leptin, and spontaneous correction of leptin-mediated
defects. J Clin Endocrinol Metab 1999;84:3686 95.
[159] Ozata M, Ozisik G, Bingol N, Corakci A, Gundogan MA. The
effects of thyroid status on plasma leptin levels in women. J Endocrinol Invest 1998;21:337 41.
[160] Pardridge WM. Receptor-mediated peptide transport through the
blood brain barrier. Endocr Rev 1986;7:314 30.
[161] Pelleymounter MA, Cullen MJ, Baker MB, Hecht R, Winters D,
Boone T, et al. Effects of the obese gene product on body weight
regulation in ob/ob mice. Science 1995;269:540 3.
[162] Petersen KF, Oral EA, Dufour S, Befroy D, Ariyan C, Yu C, et al.
Leptin reverses insulin resistance and hepatic steatosis in patients
with severe lipodystrophy. J Clin Invest 2002;109:1345 50.
[163] Pinkney JH, Goodrick SJ, Katz J, Johnson AB, Lightman SL, Coppack SW, et al. Leptin and the pituitary thyroid axis: a comparative
study in lean, obese, hypothyroid and hyperthyroid subjects. Clin
Endocrinol (Oxf) 1998;49:583 8.
[164] Plant TM, Durrant AR. Circulating leptin does not appear to provide
a signal for triggering the initiation of puberty in the male rhesus
monkey (Macaca mulatta). Endocrinology 1997;138:4505 8.
[165] Porte Jr D, Baskin DG, Schwartz MW. Leptin and insulin action in
the central nervous system. Nutr Rev 2002;60:S20 9.
[166] Pralong FP, Roduit R, Waeber G, Castillo E, Mosimann F, Thorens B,
et al. Leptin inhibits directly glucocorticoid secretion by normal human and rat adrenal gland. Endocrinology 1998;139:4264 8.
[167] Prpic V, Watson PM, Frampton IC, Sabol MA, Jezek GE, Gettys TW.
Differential mechanisms and development of leptin resistance in A/J
versus C57BL/6J mice during diet-induced obesity. Endocrinology
2003;144:1155 63.
[168] Qiu J, Ogus S, Mounzih K, Ewart-Toland A, Chehab FF. Leptindeficient mice backcrossed to the BALB/cJ genetic background have
reduced adiposity, enhanced fertility, normal body temperature, and
severe diabetes. Endocrinology 2001;142:3415 21.
[169] Rasmussen DD, Boldt BM, Wilkinson CW, Yellon SM, Matsumoto
AM. Daily melatonin administration at middle age suppresses male
rat visceral fat, plasma leptin, and plasma insulin to youthful levels.
Endocrinology 1999;140:1009 12.
[170] Rau H, Reaves BJ, ORahilly S, Whitehead JP. Truncated human
leptin (delta133) associated with extreme obesity undergoes proteasomal degradation after defective intracellular transport. Endocrinology 1999;140:1718 23.
[171] Ravussin E, Pratley RE, Maffei MM, Wang H, Friedman JM, Bennett PH, et al. Relatively low plasma leptin concentrations precede
weight gain in Pima Indians. Nat Med 1997;3:238 40.
[172] Rentsch J, Chiesi M. Regulation of ob gene mRNA levels in cultured
adipocytes. FEBS Lett 1996;379:55 9.
[173] Roemmich JN, Clark PA, Berr SS, Mai V, Mantzoros CS, Flier JS, et
al. Gender differences in leptin levels during puberty are related to
the subcutaneous fat depot and sex steroids. Am J Physiol
1998;275:E543 51.
[174] Roh SG, Nie GY, Loneragan K, Gertler A, Chen C. Direct modification of somatotrope function by long-term leptin treatment of
[175]
[176]
[177]
[178]
[179]
[180]
[181]
[182]
[183]
[184]
[185]
[186]
[187]
[188]
[189]
[190]
[191]
[192]
[193]
primary cultured ovine pituitary cells. Endocrinology 2001;142:
5167 71.
Rosenbaum M, Nicolson M, Hirsch J, Heymsfield SB, Gallagher D,
Chu F, et al. Effects of gender, body composition, and menopause on
plasma concentrations of leptin. J Clin Endocrinol Metab 1996;81:
3424 7.
Rosenbaum M, Murphy EM, Heymsfield SB, Matthews DE, Leibel
RL. Low dose leptin administration reverses effects of sustained
weight-reduction on energy expenditure and circulating concentrations of thyroid hormones. J Clin Endocrinol Metab 2002;
87:2391 4.
Saad MF, Damani S, Gingerich RL, Riad-Gabriel MG, Khan A,
Boyadjian R, et al. Sexual dimorphism in plasma leptin concentration. J Clin Endocrinol Metab 1997;82:579 84.
Sainsbury A, Schwarzer C, Couzens M, Jenkins A, Oakes SR,
Ormandy CJ, et al. Y4 receptor knockout rescues fertility in ob/ob
mice. Genes Dev 2002;16:1077 88.
Saladin R, De Vos P, Guerre-Millo M, Leturque A, Girard J, Staels
B, et al. Transient increase in obese gene expression after food intake
or insulin administration. Nature 1995;377:527 9.
Sarraf P, Frederich RC, Turner EM, Ma G, Jaskowiak NT, Rivet Jr D,
et al. Multiple cytokines and acute inflammation raise mouse leptin
levels: potential role in inflammatory anorexia. J Exp Med 1997;
185:171 5.
Satoh N, Ogawa Y, Katsuura G, Tsuji T, Masuzaki H, Hiraoka J,
et al. Pathophysiological significance of the obese gene product,
leptin, in ventromedial hypothalamus (VMH)-lesioned rats: evidence for loss of its satiety effect in VMH-lesioned rats. Endocrinology 1997;138:947 54.
Schoeller DA, Cella LK, Sinha MK, Caro JF. Entrainment of the
diurnal rhythm of plasma leptin to meal timing. J Clin Invest 1997;
100:1882 7.
Schwartz MW, Peskind E, Raskind M, Boyko EJ, Porte Jr D. Cerebrospinal fluid leptin levels: relationship to plasma levels and to
adiposity in humans. Nat Med 1996;2:589 93.
Segal-Lieberman G, Trombly DJ, Juthani V, Wang X, Maratos-Flier
E. NPY ablation in C57BL/6 mice leads to mild obesity and to an
impaired refeeding response to fasting. Am J Physiol Endocrinol
Metab 2003;284:E1131 9.
Sharma K, Considine RV, Michael B, Dunn SR, Weisberg LS, Kurnik BR, et al. Plasma leptin is partly cleared by the kidney and is
elevated in hemodialysis patients. Kidney Int 1997;51:1980 5.
Shimomura I, Hammer RE, Ikemoto S, Brown MS, Goldstein JL.
Leptin reverses insulin resistance and diabetes mellitus in mice with
congenital lipodystrophy. Nature 1999;401:73 6.
Sinha MK, Opentanova I, Ohannesian JP, Kolaczynski JW, Heiman
ML, Hale J, et al. Evidence of free and bound leptin in human
circulation. Studies in lean and obese subjects and during short-term
fasting. J Clin Invest 1996;98:1277 82.
Sinha MK, Sturis J, Ohannesian J, Magosin S, Stephens T, Heiman
ML, et al. Ultradian oscillations of leptin secretion in humans. Biochem Biophys Res Commun 1996;228:733 8.
Slieker LJ, Sloop KW, Surface PL, Kriauciunas A, LaQuier F, Manetta J, et al. Regulation of expression of ob mRNA and protein by
glucocorticoids and cAMP. J Biol Chem 1996;271:5301 4.
Smith JT, Waddell BJ. Developmental changes in plasma leptin and
hypothalamic leptin receptor expression in the rat: peripubertal
changes and the emergence of sex differences. J Endocrinol 2003;
176:313 9.
Spanswick D, Smith MA, Groppi VE, Logan SD, Ashford ML.
Leptin inhibits hypothalamic neurons by activation of ATP-sensitive
potassium channels. Nature 1997;390:521 5.
Strobel A, Issad T, Camoin L, Ozata M, Strosberg AD. A leptin
missense mutation associated with hypogonadism and morbid obesity. Nat Genet 1998;18:213 5.
Suter KJ, Pohl CR, Wilson ME. Circulating concentrations of nocturnal leptin, growth hormone, and insulin-like growth factor-I in-
R.S. Ahima, S.Y. Osei / Physiology & Behavior 81 (2004) 223241
[194]
[195]
[196]
[197]
[198]
[199]
[200]
[201]
[202]
[203]
[204]
[205]
[206]
[207]
[208]
crease before the onset of puberty in agonadal male monkeys: potential signals for the initiation of puberty. J Clin Endocrinol Metab
2000;85:808 14.
Takahashi N, Patel HR, Qi Y, Dushay J, Ahima RS. Divergent effects
of leptin in mice susceptible or resistant to obesity. Horm Metab Res
2002;34:691 7.
Takaya K, Ogawa Y, Hiraoka J, Hosoda K, Yamori Y, Nakao K, et al.
Nonsense mutation of leptin receptor in the obese spontaneously
hypertensive Koletsky rat. Nat Genet 1996;14:130 1.
Takeda S, Elefteriou F, Levasseur R, Liu X, Zhao L, Parker KL, et al.
Leptin regulates bone formation via the sympathetic nervous system.
Cell 2002;111:305 17.
Tannenbaum GS, Gurd W, Lapointe M. Leptin is a potent stimulator of spontaneous pulsatile growth hormone (GH) secretion and
the GH response to GH-releasing hormone. Endocrinology 1998;
139:3871 5.
Tartaglia LA. The leptin receptor. J Biol Chem 1997;272:6093 6.
Tartaglia LA, Dembski M, Weng X, Deng N, Culpepper J, Devos R,
et al. Identification and expression cloning of a leptin receptor, OBR. Cell 1995;83:1263 71.
Trayhurn P, Duncan JS, Rayner DV, Hardie LJ. Rapid inhibition of
ob gene expression and circulating leptin levels in lean mice by the
beta 3-adrenoceptor agonists BRL 35135A and ZD2079. Biochem
Biophys Res Commun 1996;228:605 10.
Unger RH, Orci L. Lipotoxic diseases of nonadipose tissues in obesity. Int J Obes Relat Metab Disord 2000;24(Suppl. 4):S28 32.
Uotani S, Bjorbaek C, Tornoe J, Flier JS. Functional properties of
leptin receptor isoforms: internalization and degradation of leptin
and ligand-induced receptor downregulation. Diabetes 1999;48:
279 86.
Vaisse C, Halaas JL, Horvath CM, Darnell Jr JE, Stoffel M, Friedman JM. Leptin activation of Stat3 in the hypothalamus of wild-type
and ob/ob mice but not db/db mice. Nat Genet 1996;14:95 7.
van Dijk G, Donahey JC, Thiele TE, Scheurink AJ, Steffens AB,
Wilkinson CW, et al. Central leptin stimulates corticosterone secretion at the onset of the dark phase. Diabetes 1997;46:1911 4.
Van Heek M, Compton DS, France CF, Tedesco RP, Fawzi AB,
Graziano MP, et al. Diet-induced obese mice develop peripheral,
but not central, resistance to leptin. J Clin Invest 1997;99:385 90.
Wang J, Liu R, Hawkins M, Barzilai N, Rossetti L. A nutrientsensing pathway regulates leptin gene expression in muscle and
fat. Nature 1998;393:684 8.
Watanobe H. Leptin directly acts within the hypothalamus to stimulate gonadotropin-releasing hormone secretion in vivo in rats. J Physiol 2002;545:255 68.
Watanobe H, Habu S. Leptin regulates growth hormone-releasing
factor, somatostatin, and alpha-melanocyte-stimulating hormone
[209]
[210]
[211]
[212]
[213]
[214]
[215]
[216]
[217]
[218]
[219]
[220]
241
but not neuropeptide Y release in rat hypothalamus in vivo: relation
with growth hormone secretion. J Neurosci 2002;22:6265 71.
Watanobe H, Schioth HB, Suda T. Stimulation of prolactin secretion
by chronic, but not acute, administration of leptin in the rat. Brain
Res 2000;887:426 31.
Watanobe H, Suda T, Wikberg JE, Schioth HB. Evidence that physiological levels of circulating leptin exert a stimulatory effect on
luteinizing hormone and prolactin surges in rats. Biochem Biophys
Res Commun 1999;263:162 5.
White DW, Wang D, Chua Jr SC, Morgenstern JP, Leibel RL, Baumann H, et al. Constitutive and impaired signaling of leptin receptors
containing the Gln ! Pro extracellular domain fatty mutation. Proc
Natl Acad Sci U S A 1997;94:10657 62.
Wiesner G, Vaz M, Collier G, Seals D, Kaye D, Jennings G, et al.
Leptin is released from the human brain: influence of adiposity and
gender. J Clin Endocrinol Metab 1999;84:2270 4.
Wolden-Hanson T, Mitton DR, McCants RL, Yellon SM, Wilkinson
CW, Matsumoto AM, et al. Daily melatonin administration to middle-aged male rats suppresses body weight, intraabdominal adiposity,
and plasma leptin and insulin independent of food intake and total
body fat. Endocrinology 2000;141:487 97.
Woller M, Tessmer S, Neff D, Nguema AA, Roo BV, WaechterBrulla D. Leptin stimulates gonadotropin releasing hormone release
from cultured intact hemihypothalami and enzymatically dispersed
neurons. Exp Biol Med 2001;226:591 6.
Wu-Peng XS, Chua Jr SC, Okada N, Liu SM, Nicolson M, Leibel
RL. Phenotype of the obese Koletsky (f) rat due to Tyr763Stop
mutation in the extracellular domain of the leptin receptor (Lepr):
evidence for deficient plasma-to-CSF transport of leptin in both the
Zucker and Koletsky obese rat. Diabetes 1997;46:513 8.
Yamauchi T, Kamon J, Waki H, Terauchi Y, Kubota N, Hara K, et
al. The fat-derived hormone adiponectin reverses insulin resistance
associated with both lipoatrophy and obesity. Nat Med 2001;7:
941 6.
Yu WH, Kimura M, Walczewska A, Karanth S, McCann SM. Role of
leptin in hypothalamic pituitary function. Proc Natl Acad Sci U S A
1997;94:1023 8.
Zabolotny JM, Bence-Hanulec KK, Stricker-Krongrad A, Haj F,
Wang Y, Minokoshi Y, et al. PTP1B regulates leptin signal transduction in vivo. Dev Cell 2002;2:489 95.
Zachow RJ, Magoffin DA. Direct intraovarian effects of leptin: impairment of the synergistic action of insulin-like growth factor-I on
follicle-stimulating hormone-dependent estradiol-17 beta production
by rat ovarian granulosa cells. Endocrinology 1997;138:847 50.
Zhang Y, Proenca R, Maffei M, Barone M, Leopold L, Friedman JM.
Positional cloning of the mouse obese gene and its human homologue. Nature 1994;372:425 32.
Vous aimerez peut-être aussi
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- 4 Male and Female Reproductive Organs PPTDocument71 pages4 Male and Female Reproductive Organs PPTDanica Marie Sibay100% (2)
- Step by Step Chinese CookingDocument52 pagesStep by Step Chinese CookingMarkk211Pas encore d'évaluation
- Integrative Neurobiology (CTN RF in Serbian)Document224 pagesIntegrative Neurobiology (CTN RF in Serbian)JovanaLazarevic100% (1)
- Lebanese Cooking PDFDocument52 pagesLebanese Cooking PDFCici21Pas encore d'évaluation
- 2 Evolucija GenaDocument6 254 pages2 Evolucija GenaCici21Pas encore d'évaluation
- Myogenic Satellite Cells Physiology To Molecular Biology PDFDocument18 pagesMyogenic Satellite Cells Physiology To Molecular Biology PDFCici21Pas encore d'évaluation
- Chania en PDFDocument23 pagesChania en PDFCici21Pas encore d'évaluation
- 2003 - Leptin in The CNS - Much More Than A Satiety Signal PDFDocument10 pages2003 - Leptin in The CNS - Much More Than A Satiety Signal PDFCici21Pas encore d'évaluation
- (Physiology) (17130651) Molecular Mechanisms of Insulin Resistance in Humans and Their Potential Links With Mitochondrial DysfunctionDocument7 pages(Physiology) (17130651) Molecular Mechanisms of Insulin Resistance in Humans and Their Potential Links With Mitochondrial DysfunctionAndri FerdianPas encore d'évaluation
- JEM Immunity-and-Cancer Special Issue PDFDocument74 pagesJEM Immunity-and-Cancer Special Issue PDFCici21Pas encore d'évaluation
- Eikosanoid PDFDocument3 pagesEikosanoid PDFCici21Pas encore d'évaluation
- Diabetes Mellitus Complicated PregnancyDocument21 pagesDiabetes Mellitus Complicated PregnancyanojanPas encore d'évaluation
- Notes Chapter 7Document16 pagesNotes Chapter 7KxelviiPas encore d'évaluation
- 054 Physiology MCQ ACEM Primary RenalDocument1 page054 Physiology MCQ ACEM Primary RenalYasif AbbasPas encore d'évaluation
- The Child With Endocrine/Metabolic Dysfunction: Thyroid Gland DisordersDocument17 pagesThe Child With Endocrine/Metabolic Dysfunction: Thyroid Gland DisordersMeccanazaren Susvilla BojorquePas encore d'évaluation
- Testosterone BoostersDocument2 pagesTestosterone BoostersThato SekonyanePas encore d'évaluation
- IV Push Levothyroxine Mue FinalDocument21 pagesIV Push Levothyroxine Mue Finalapi-535481376Pas encore d'évaluation
- Endocrine Physiology Case Study - BathshebaDocument6 pagesEndocrine Physiology Case Study - BathshebaMc Lindssey PascualPas encore d'évaluation
- Blood Glucose Test Worksheet: Activity 4Document3 pagesBlood Glucose Test Worksheet: Activity 4Marcelle Ann C. VillanuevaPas encore d'évaluation
- Polycystic Ovary Syndrome - PCOS - Fertility - Ultrasound - TeachMeObGynDocument4 pagesPolycystic Ovary Syndrome - PCOS - Fertility - Ultrasound - TeachMeObGynLiridon SopajPas encore d'évaluation
- Soal Physiox Endokrin Activity 2Document4 pagesSoal Physiox Endokrin Activity 2al ghiffari muhammad rayhanPas encore d'évaluation
- Management of Diabetes Mellitus A ReviewDocument11 pagesManagement of Diabetes Mellitus A ReviewEditor IJTSRDPas encore d'évaluation
- 10.11648.j.ijcd.20170102.12 2Document8 pages10.11648.j.ijcd.20170102.12 2Muhammad UmerPas encore d'évaluation
- Sodium, Water and Potassium: Michael D. PenneyDocument39 pagesSodium, Water and Potassium: Michael D. PenneyChristianus LeonardPas encore d'évaluation
- Clinical Chemistry 2: Introduction To EndocrinologyDocument3 pagesClinical Chemistry 2: Introduction To EndocrinologyYen BauzonPas encore d'évaluation
- Bedienungsanleitung Philips Lumea Precision Plus SC2008 (Deutsch - 114 Seiten)Document1 pageBedienungsanleitung Philips Lumea Precision Plus SC2008 (Deutsch - 114 Seiten)marylou.wrobelPas encore d'évaluation
- Blood Glucose Monitoring ChartDocument3 pagesBlood Glucose Monitoring Chartfazal_f1Pas encore d'évaluation
- UREMIADocument10 pagesUREMIAAkanksha TiwariPas encore d'évaluation
- Week 1 CH 48 DiabetesDocument115 pagesWeek 1 CH 48 DiabetesNeal PatelPas encore d'évaluation
- حالات سكرDocument13 pagesحالات سكرNada AliPas encore d'évaluation
- Seeleys Essentials of Anatomy and Physiology 9th Edition VanPutte Solutions Manual 1Document5 pagesSeeleys Essentials of Anatomy and Physiology 9th Edition VanPutte Solutions Manual 1marcos100% (48)
- ReportsDocument15 pagesReportsamandio silvaPas encore d'évaluation
- Urinary System ArlendsDocument55 pagesUrinary System ArlendslionioniPas encore d'évaluation
- Insulin Degludec: Dr. Taufik Hidayat Regional Medical Advisor Novo Nordisk IndonesiaDocument35 pagesInsulin Degludec: Dr. Taufik Hidayat Regional Medical Advisor Novo Nordisk IndonesiaAndi SedaPas encore d'évaluation
- Multiple Endocrine Neoplasia Type 1: Key FactsDocument3 pagesMultiple Endocrine Neoplasia Type 1: Key FactsMahfooj RahmanPas encore d'évaluation
- Reproduksi Anatomi Wanita'Document42 pagesReproduksi Anatomi Wanita'uflah_Pas encore d'évaluation
- Cells: B. Cell PhysiologyDocument29 pagesCells: B. Cell PhysiologyShyenPas encore d'évaluation
- Skin 1: The Structure and Functions of The SkinDocument4 pagesSkin 1: The Structure and Functions of The SkinJohanPas encore d'évaluation
- FLOWCHARTDocument1 pageFLOWCHARTPatrick FormosoPas encore d'évaluation
- Endometriosis PresentationDocument58 pagesEndometriosis PresentationBRI KUPas encore d'évaluation