Académique Documents
Professionnel Documents
Culture Documents
The Proinsulin/insulin (PI/I) Ratio Is Reduced by Postprandial Targeting Therapy in Type 2 Diabetes Mellitus: A Small-Scale Clinical Study
Transféré par
Soleh SundawaTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
The Proinsulin/insulin (PI/I) Ratio Is Reduced by Postprandial Targeting Therapy in Type 2 Diabetes Mellitus: A Small-Scale Clinical Study
Transféré par
Soleh SundawaDroits d'auteur :
Formats disponibles
Ohkura et al.
BMC Research Notes 2013, 6:453
http://www.biomedcentral.com/1756-0500/6/453
RESEARCH ARTICLE
Open Access
The proinsulin/insulin (PI/I) ratio is reduced by
postprandial targeting therapy in type 2 diabetes
mellitus: a small-scale clinical study
Tsuyoshi Ohkura1*, Kazuoki Inoue1, Youhei Fujioka1, Risa Nakanishi1, Hideki Shiochi1, Keisuke Sumi1, Naoya Yamamoto1,
Kazuhiko Matsuzawa2, Shoichiro Izawa1, Hiroko Ohkura2, Masahiko Kato1, Kazuhiro Yamamoto1 and Shin-ichi Taniguchi2
Abstract
Background: An elevated PI/I ratio is attributable to increased secretory demand on -cells. However, the effect of
postprandial targeting therapy on proinsulin level is unknown. We evaluated the metabolic effect of glinide and
sulfonylurea (SU) using the meal tolerance test (MTT).
Methods: MTT was applied to previously untreated Type 2 Diabetes Mellitus (T2DM) subjects. Twenty-two participants
were given a test meal (450 kcal). Plasma glucose and insulin were measured at 0 (fasting), 30, 60, 120, and 180 min.
Serum proinsulin and C-peptide immunoreactivity (CPR) were measured at 0 and 120 min. Postprandial profile was
assessed at baseline and following 3 months treatment with either mitiglinide or glimepiride.
Results: Plasma glucose level at 30, 60, 120, and 180 min was significantly improved by mitiglinide. Whereas,
glimepiride showed a significant improve plasma glucose at 0, 180 min. Peak IRI shifted from 120 to 30 min by
mitiglinide treatment. The pattern of insulin secretion was not changed by glimepiride treatment. Whereas
mitiglinide did not affect the PI/I ratio, glimepiride tended to increase the PI/I ratio. Moreover, although mitiglinide
did not affect PI/I ratio as a whole, marked reduction was noted in some patients treated by mitiglinide. PI/I ratio was
reduced significantly in the responder group. The responder subgroup exhibited less insulin resistance and higher
insulinogenic index at baseline than non-responders. Moreover, the triglyceride level of responders was significantly
lower than that of non-responders.
Conclusions: Mitiglinide improved postprandial insulin secretion pattern and thereby suppressed postprandial glucose
spike. In T2DM patients with low insulin resistance and low triglyceride, mitiglinide recovered impaired -cell function
from the viewpoint of the PI/I ratio.
Trial registration: UMIN-CTR: UMIN000010467
Keywords: Proinsulin, Meal tolerance test, Type 2 diabetes mellitus, Glinide
Background
Type 2 diabetes mellitus is a heterogeneous disease
characterized by insulin resistance and defective insulin
secretion [1]. Proinsulin is synthesized and secreted
as the precursor form of insulin. Proinsulin level is a
predictor of type 2 diabetes mellitus (T2DM), obesity,
* Correspondence: ohkura@med.tottori-u.ac.jp
Equal contributors
1
Division of Cardiovascular Medicine, Endocrinology and Metabolism,
Department of Molecular Medicine and Therapeutics, Tottori University
Faculty of Medicine, Yonago, Tottori, Japan
Full list of author information is available at the end of the article
and cardiovascular disease. The PI/I ratio reflects - cell
dysfunction associated with the onset and progression
of T2DM [2,3]. An elevated PI/I ratio is attributable to
increased secretory demand on -cells. One study reported
sulfonylurea-treated subjects had a significant elevation in
proinsulin/IRI ratio compared with diet-treated subjects,
whereas non sulfonylurea hypoglycemic agent-treated subjects (metformin, alpha-glucosidase inhibitor, troglitazone)
did not [4]. However, the effect of postprandial targeting
therapy on proinsulin level is unknown. It has been
reported that glibenclamide, but not nateglinide, induced
-cell apoptosis in cultured human islets [5]. In Japan,
2013 Ohkura et al.; licensee BioMed Central Ltd. This is an open access article distributed under the terms of the Creative
Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and
reproduction in any medium, provided the original work is properly cited.
Ohkura et al. BMC Research Notes 2013, 6:453
http://www.biomedcentral.com/1756-0500/6/453
approximately half of all patients with diabetes have a
genetic predisposition to the disease, and insulin secretion
is often impaired in lean patients with diabetes mellitus
[6,7]. Additionally, Japanese and Asian patients often
show reduced cell function. Mitiglinide is a short-acting
insulinotropic agent used in type 2 diabetes treatment.
It has a rapid stimulatory effect on insulin secretion
and reduces postprandial plasma glucose level in patients
with type 2 diabetes [8].
Based on these results, we hypothesized that glinide may
be superior to sulfonylurea about beta-cell dysfunction in
Japanese patients with type 2 diabetes mellitus. Therefore,
we evaluated the metabolic effect of glinide/sulfonylurea
(SU) using the Japan Diabetes Society-developed meal
tolerance test (MTT) in Japanese patients with type 2
diabetes mellitus, which shows a tight correlation with
glucose tolerance test.
Methods
Subjects
Twenty-two outpatients with type 2 diabetes mellitus
participated in this study at Tottori University Hospital.
Type 2 diabetes mellitus was diagnosed based on the
criteria of the Japan Diabetes Society [9]. These patients
were divided into mitiglinide group and glimepiride
group. The patients were continuously assigned to the
mitiglinide group and the glimepiride group. First 15
patients were assigned to the mitiglinide group and 7
patients who were registered thereafter were assigned
to the glimepiride group. These patients were given
mitiglinide 30 mg/day, or glimepiride 0.5 mg/day. This
study was a prospective, open label, non-randomized,
clinical study. There were fifteen patients in mitiglinide
group and seven patients in glimepiride group. There
were ten males and five females in mitiglinide group,
and six males and one female in glimepiride group. The
mean age of the patients in mitiglinide group was
58.5 years, mean BMI was 24.8 kg/m2, mean fasting
plasma glucose was 6.88 mmol/L (124 mg/dl), mean
HbA1c was 6.80% (50.8 mmol/mol) (Table 1). The mean
age of the patients in glimepiride group was 65.1 years,
mean BMI was 26.3 kg/m2, mean fasting plasma glucose
was 8.16 mmol/L (147 mg/dl), mean HbA1c was 7.60%
(59.5 mmol/mol) (Table 1). Patients with pancreatic
disease, liver disease, renal failure, or those taking
diabetogenic medications such as corticosteroids were
excluded from this study. All patients were diabetic
drug nave patients.
This study was approved by the Ethics Committee of
the Faculty of Medicine, Tottori University. Informed
consent was obtained from all of the patients using a
procedure approved by the Ethics Committee. This study
was registered in University Hospital Medical Information
Page 2 of 8
Table 1 Patient characteristics
Mitiglinide
Glimepiride
n (M/F)
15 (10/5)
7 (6/1)
Age, years
58.5 11.5
65.1 7.5
BMI, kg/m2
24.8 4.0
26.3 6.2
SBP, mmHg
137 17
132 20
DBP, mmHg
80 7
79 11
Total cholesterol, mmol/L
5.38 0.98
5.43 1.08
(mg/dL)
(208 38)
(210 42)
Triglycerides, mmol/L
1.71 1.14
1.89 0.74
(mg/dL)
(152 101)
(168 66)
HDL-C, mmol/L
1.39 0.38
1.37 0.31
(mg/dL)
(54 15)
(53 12)
Fasting glucose, mmol/L
6.88 1.27
8.16 1.05
(mg/dL)
(124 23)
(147 19)
2-h postload glucose, mmol/L
9.11 1.94
11.6 1.77
(mg/dL)
(164 35)
(209 32)
HbA1c(NGSP),%
6.80 0.54
7.60 0.63
Fasting IRI, pmol/L
52.7 53.4
49.3 36.1
(ng/mL)
(7.6 7.7)
(7.1 5.2)
HOMA-R
2.55 3.10
2.67 2.09
ISI (Matsudas index)
7.73 3.16
7.68 4.69
Insulinogenic index
0.80 0.61
0.42 0.38
CPR, nmol/L
0.59 0.30
0.57 0.17
(ng/mL)
(1.79 0.93)
(1.72 0.51)
Proinsulin, pmol/L
4.29 4.16
4.77 4.04
PI/I ratio
0.10 0.11
0.19 0.26
Data are means standard deviation.
BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood
pressure; HDL-C, high-density lipoprotein cholesterol; HbA1c, hemoglobin A1c;
NGSP, National Glycohemoglobin Standardization Program; IRI, immunoreactive
insulin; HOMA-IR, homeostasis model assessment of insulin resistance; ISI, insulin
sensitivity index; CPR, C-peptide immunoreactivity; PI/I ratio,
proinsulin/insulin ratio.
Network Clinical Trials Registry (UMIN-CTR), the ID was
UMIN000010467.
Meal tolerance test
After fasting for at least 12 h, the participants visited
the clinic in the morning and consumed a test meal
prepared by the Japan Diabetes Society (450 kcal/1882 kJ;
15% protein, 35% fat, and 50% carbohydrate; 1.6 g salt
x1.6 g) [10]. Plasma glucose and insulin were measured at
0 (fasting), 30, 60, 120, and 180 min after the test meal.
Serum C-peptide immunoreactivity (CPR) was measured
at 0 (fasting) and 120 min. Plasma glucose was measured
using the glucose oxidase method. Plasma insulin and
CPR levels were measured using chemiluminescent immunoassays (CLIA) (human insulin and CPR CLIA kits;
Kyowa Medix, Tokyo, Japan). Plasma insulin was defined
Ohkura et al. BMC Research Notes 2013, 6:453
http://www.biomedcentral.com/1756-0500/6/453
as immunoreactive insulin (IRI). Plasma proinsulin was
measured using an enzyme-linked immunosorbent assay
(ELISA) (human intact proinsulin ELISA kit; Biovendor
Heidelberg, Germany). This method of meal tolerance
test (MTT) was a well-established method in our hospital
as previously reported [11].
HbA1c (JDS: Japan Diabetes Society) was measured
by high-performance liquid chromatography and was
converted to National Glycohemoglobin Standardization
Program (NGSP) values using the following officially
certified equation: NGSP (%) = 1.02 JDS (%) + 0.25%
[12]. The reverse equation is: JDS (%) = 0.980 NGSP
(%) 0.245%.
Calculation of insulin secretion and resistance indices
Insulinogenic Index = [(insulin at 30 min) - (insulin at
0 min)]/[(glucose at 30 min) - (glucose at 0 min)] [13].
HOMA-IR = [fasting plasma glucose (FPG; mmol/L)]
[fasting IRI (F-IRI; pmol/L)]/135 [14].
ISI = 10,000/{[FPG (mmol/L) FPI (pmol/L)] [mean
glucose mean insulin during the MTT]} [15].
Self-monitoring blood glucose (SMBG)
SMBG was performed at 7 times/day (before and after
every meal, bedtime). Patients checked their blood glucose
level with a SMBG device (Freestyle, Nipro, Osaka, Japan).
Mean blood glucose of 3 days was calculated at 7 points.
Statistical analysis
Data are expressed as means standard error of the
mean. Two groups were compared using paired Students
t-test. Values of P < 0.05 were considered significant. SPSS
software version 15.0 (SPSS, Chicago, IL, USA) was used
for all analyses.
Results
Meal tolerance test
Plasma glucose level at 30, 60, 120, and 180 min was significantly improved by mitiglinide (Figure 1-a). Whereas,
glimepiride showed a significant improve plasma glucose
at 0, 180 min (Figure 1-b). Peak IRI shifted from 120 to
30 min by mitiglinide treatment, the insulin level in
30 min significantly increased (Figure 2-a). The pattern
of insulin secretion was not changed by glimepiride
treatment, and the IRI level significantly increased at 60,
120 min (Figure 2-b).
Self-monitoring blood glucose
Postprandial glucose level was significantly improved
by mitiglinide at all mealtimes (Figure 3-a). In contrast,
glimepiride reduced both pre- and post-prandial glucose
level, and there was significant reduction of blood glucose level only in before dinner time (Figure 3-b). Mitiglinide but not glimepiride improved glucose fluctuations
Page 3 of 8
difference between maximum and minimum glucose levels
(Figure 4-a,b).
Proinsulin/Insulin ratio
Whereas mitiglinide did not affect the PI/I ratio, glimepiride tended to increase PI/I ratio (Figure 5). Moreover, although mitiglinide did not affect PI/I ratio as a
whole, marked reduction was noted in some patients
treated by this agent (Figure 6). PI/I ratio was reduced
significantly in the responder group (0.084 +/ 0.064
to 0.028 +/ 0.020, P < 0.01). (Responders defined as
patients in whom PI/I ratio was reduced >10% vs baseline
by mitiglinide treatment.)
The responder subgroup exhibited significantly higher
insulin sensitivity index (9.30 +/ 2.35 vs 6.15 +/ 3.23,
P < 0.05) and higher insulinogenic index (1.01 +/ 0.69 vs
0.43 +/ 0.30, P < 0.05) at baseline than non-responders
(Table 2). The triglyceride (TG) level of responders was
significantly lower than that of non-responders (1.19
0.50 vs 2.32 1.40, P < 0.05).
Discussion
In this study, postprandial glucose level was significantly
reduced by mitiglinide treatment. After 3 months treatment, mitiglinide did not increase PI/I ratio. In contrast,
glimepiride increased PI/I ratio. Interestingly, there were
two distinct subgroups among patients treated by mitiglinide about the PI/I ratio: responders and non-responders. In the responders subgroup, marked reduction
of PI/I ratio was observed. The responder subgroup exhibited less insulin resistance and the higher insulinogenic
index at baseline than non-responders. Moreover, the
TG level of responders was significantly lower than that
of non-responders.
An elevated PI/I ratio reflects impairment of insulin
secretory capacity of -cells and cardiovascular risk in
patients with IGT or T2DM. Mitiglinide stimulates
-cells and quickly accelerates insulin secretion, which
is the physiological property of these cells. Kawai et al.
reported that treatment of GK rats with nateglinide and
glibenclamide varies in long-term effects on -cell functions; nateglinide treatment better preserved pancreatic
islet morphology than did glibenclamide treatment [16].
Laghmich et al. reported that when both normal and
GK rats were exposed to nateglinide and glibenclamide
for 7 days, insulin in islets, the secretory response to
high-glucose and basal biosynthetic activity were better
in those animals which received nateglinide [17]. Taken
together, these data suggest that short-acting nateglinide
preserves -cell functions better than the long-acting
glibenclamide does. RDER et al. reported that the
fasting PI/IRI ratio appears to be a marker of the degree of
reduced maximal acute insulin response (AIR max) in type
Ohkura et al. BMC Research Notes 2013, 6:453
http://www.biomedcentral.com/1756-0500/6/453
(a)
Page 4 of 8
(b)
Figure 1 Plasma glucose response in meal tolerance test. Plasma glucose level at 60, 120, and 180 min was significantly improved by
mitiglinide (a). Whereas, glimepiride showed a significant improve plasma glucose at only 180 min (b).
2 DM [18]. Mitiglinide reduces the levels of circulating
biomarkers of oxidative stress and inflammation caused
by postprandial hyperglycemia [19]. We speculate that
mitiglinide might rescue impairment of -cell function
possibly via preventing postprandial stress.
In this study, the insulin resistance level of responders
was significantly lower than that of non-responders.
Haffner and colleagues examined the relation between
the fasting proinsulin-to-insulin ratio with a number of
(a)
metabolic disorders believed to be associated with the
insulin resistance (IR) syndrome. In 423 subjects without
diabetes, an increased ratio was significantly associated
with hypertension, low high-density lipoprotein cholesterol,
high triglyceride levels, and impaired glucose tolerance.
These results suggest that even nondiabetic individuals
with the IR syndrome not only exhibit hyperinsulinemia
as a marker of IR, but also show elevated proinsulin
values, which may reflect relative beta-cell failure or
(b)
Figure 2 IRI response in meal tolerance test. Peak IRI shifted from 120 to 30 min by mitiglinide treatment (a). The pattern of insulin secretion
was not changed by glimepiride treatment (b).
Ohkura et al. BMC Research Notes 2013, 6:453
http://www.biomedcentral.com/1756-0500/6/453
(a)
Page 5 of 8
(b)
Figure 3 Average daily profiles of capillary blood glucose by SMBG. Postprandial glucose level was significantly improved by mitiglinide at
all mealtimes (a). In contrast, glimepiride reduced both pre- and post-prandial glucose level, and there was significant reduction of blood glucose
level in before dinner time (b).
malfunction. [20]. Another investigation explored the
predictive value of intact proinsulin in 48 T2DM patients.
There was a significant correlation between intact proinsulin values and insulin resistance measurement of
minimal model analysis [21]. These results might be able
to explain the PI/I ratio non-responder group showed
higher insulin resistance.
Next, one study reported that metformin treatment
in subjects with Type 2 diabetes mellitus significantly
reduced concentrations of proinsulin-like molecules over
a 12-week period. They conclude that short-term effects
of metformin treatment on proinsulin-like molecules
are similar to those previously observed with dietary
treatment in subjects with Type 2 diabetes but opposite
to those of sulphonylurea treatment. [22]. Furthermore,
several studies reported that treatment with pioglitazone
resulted in significant decreases in elevated proinsulin
levels in type 2 diabetes patients. This effect was inde-
Figure 4 Glucose fluctuations difference between maximum and minimum glucose levels in SMBG. Mitiglinide but not glimepiride
improved postprandial glucose level by SMBG.
Ohkura et al. BMC Research Notes 2013, 6:453
http://www.biomedcentral.com/1756-0500/6/453
Page 6 of 8
Figure 5 Change of PI/I ratio. Whereas mitiglinide did not affect the PI/I ratio, glimepiride tended to increase this parameter.
pendent from glycemic control [23]. These results suggest
that the treatment of insulin resistance is important for
reduction of PI/I ratio.
In this study, the TG level of responders was significantly lower than that of non-responders. Gama et al.
reported that fasting intact proinsulin concentrations
were similar in hypertriglyceridaemic subjects with normal glucose tolerance and control subjects but these
were lower than in hypertriglyceridaemic subjects with
impaired glucose tolerance [24]. Moreover, although
hyperproinsulinaemia has been reported in hypertriglyceridaemic subjects with type 2 diabetes mellitus, this
is probably related to their glucose intolerance rather
than their hypertriglyceridemia [25]. These results suggest
(a)
that poor controlled type 2 DM with hypertriglycemia
induce hyperproinsulinaemia. These results might be
able to explain that the TG level of responders was
lower than that of non-responders in patients with type
2 DM in this study,
RDER et al. reported that the PI/IRI ratio correlated
inversely with the acute insulin response (AIR) max in
the T2DM patients. They conclude that the magnitude of
the elevation in fasting PI/IRI is related to the reduction in
AIR max. Thus, the fasting PI/IRI ratio appears to be a
marker of the degree of reduced AIR Max in T2DM
[18]. These results might be able to explain the PI/I
ratio non-responder group showed a lower insulinogenic
index. It has been proposed that the restoration of both
(b)
Figure 6 PI/I ratio in mitiglinide responders (non-responders). PI/I ratio was reduced significantly in the responder group (a). PI/I ratio did
not change in the non-responder group (b).
Ohkura et al. BMC Research Notes 2013, 6:453
http://www.biomedcentral.com/1756-0500/6/453
Page 7 of 8
Table 2 Comparison of baseline metabolic profile
between P/I ratio responders and non-responders
Responder
Non responder
n (M/F)
8 (5/3)
7 (5/2)
BMI, kg/m2
23.6 4.2
26.4 4.1
HbA1c(NGSP),%
6.8 0.4
6.9 0.7
HOMA-R
1.85 1.18
3.90 4.58
ISI (Matsudas index)
9.30 2.35
6.15 3.23*
Insulinogenic index
1.01 0.69
0.43 0.30*
PI/I ratio
0.08 0.06
0.13 0.15
CPR, nmol/L
0.66 0.33
0.66 0.33
(ng/dL)
(2.0 1.0)
(2.0 1.0)
Total cholesterol, mmol/L
5.18 1.21
5.54 0.59
(mg/dL)
(200 47)
(214 23)
Triglyceride, mmol/L
1.19 0.50
2.32 1.40*
(mg/dL)
(106 45)
(206 124*)
HDL-C, mmol/L
1.73 0.51
1.16 0.31*
(mg/dL)
(67 20)
(45 12*)
Mean SD *P < 0.05 vs responder (paired t-test).
BMI, body mass index; HbA1c, hemoglobin A1c; NGSP, National Glycohemoglobin
Standardization Program; HOMA-IR, homeostasis model assessment of insulin
resistance; ISI, insulin sensitivity index; PI/I ratio, proinsulin/insulin ratio;
CPR, C-peptide immunoreactivity; HDL-C, high-density lipoprotein cholesterol;
IRI, immunoreactive insulin.
the early phase of insulin release and postprandial hyperglycemia have potentially significant implications in
improving metabolic control and reducing macrovascular complications [26]. Current evidence suggests that
proinsulin contributes to the excess incidence of cardiovascular disease in T2DM by stimulating plasminogen activator inhibitor-1 secretion and the consecutive
inhibition of fibrinolysis [27]. Our results suggest that
mitiglinide treatment contribute to improve metabolic
control and cardiovascular risk reduction in patients
with type 2 diabetes mellitus.
Our study had several limitations, including the small
number of patients and short term study. The major
limitation of our study is the small number of patients.
As only 15 patients participated glinide group in this
study, and PI/I responder subgroup was only 8 patients,
and the glimepride group was only 7 patients. Our study
may have biases, because of the small number of patients.
Our results require confirmation in a larger study. If
larger number of patients was observed, the PI/I ratio
of SU group might significantly increase. Furthermore,
the background between the mitiglinide group and the
glimepiride group was different. Randomized controlled
study or cross-over study is desired.
Because the term of this study was only 3 months,
our study needs longer term to confirm our results. If
longer term was observed, the PI/I ratio of SU group
might significantly increase. Despite these limitations,
we think that our study may aid routine clinical treatment
of Japanese and other Asian patients with type 2 diabetes
mellitus.
Conclusion
Mitiglinide improved postprandial insulin secretion pattern and thereby suppressed postprandial glucose spike.
In T2DM patients with low insulin resistance and low
TG, mitiglinide recovered impaired -cell function from
the viewpoint of the PI/I ratio.
Abbreviations
BMI: Body mass index; CPR: C-peptide immunoreactivity; FPG: Fasting plasma
glucose; HDL-C: High-density lipoprotein cholesterol; HOMA-IR: Homeostasis
model assessment for insulin resistance; IRI: Immunoreactive insulin;
ISI: Insulin sensitivity index; MTT: Meal tolerance test; PPG: Postprandial
plasma glucose; TG: Triglyceride.
Competing interests
The authors declare that they have no competing interests.
Authors contributions
TO and KI participated in the design of the study and performed the statistical
analysis. YF, HS, KS, NY, KM, SI, and HO collected the data. MK, KY, and ST
conceived the study, participated in its design and coordination, and helped
to draft the manuscript. All authors read and approved the final manuscript.
Author details
Tsuyoshi Ohkura, Assistant Professor, Division of Cardiovascular Medicine,
Endocrinology and Metabolism, Department of Molecular Medicine and
Therapeutics, Tottori University Faculty of Medicine, Nishi-chou 361, Yonago,
Tottori 6838504, Japan.
Tel: +81-859-38-6517; Fax: +81-859-38-6519.
Acknowledgments
This study was supported by a Tottori University Hospital Research Grant. We
thank Ms. Maki Kameda and Ms. Yoshiko Oda for her excellent technical
assistance. This work was carried out at Tottori University Faculty of
Medicine, Tottori, Japan.
Author details
1
Division of Cardiovascular Medicine, Endocrinology and Metabolism,
Department of Molecular Medicine and Therapeutics, Tottori University
Faculty of Medicine, Yonago, Tottori, Japan. 2Department of Regional
Medicine, Tottori University Faculty of Medicine, Yonago, Tottori, Japan.
Received: 3 July 2013 Accepted: 8 November 2013
Published: 11 November 2013
References
1. DeFronzo RA: Lilly lecture 1987. The triumvirate: beta-cell, muscle, liver.
A collusion responsible for NIDDM. Diabetes 1988, 37:667687.
2. Reder ME, Porte D Jr, Schwartz RS, et al: Disproportionately elevated
proinsulin levels reflect the degree of impaired B cell secretory capacity
in patients with noninsulin dependent diabetes mellitus. J Clin Endocrinol
Metab 1998, 83:604608.
3. Michael R, et al: Intact proinsulin and -cell function in lean and obese
subjects with and without type 2 diabetes. Diabetes Care 1999, 22:609614.
4. Inoguchi T, Umeda F, Kakimoto M, Sako Y, Ishii H, Noda K, Kunisaki M,
Imamura M, Yu HY, Etoh T, Yoshikawa H, Aoki T, Hashimoto T, Nawata H:
Chronic sulfonylurea treatment and hyperglycemia aggravate
disproportionately elevated plasma proinsulin levels in patients with
type 2 diabetes. Endocr J 2000, 47:763770.
5. Maedler K, Carr RD, Bosco D, Zuellig RA, Berney T, Donath MY: Sulfonylurea
induced -cell apoptosis in cultured human islets. J Clin Endocrinol Metab
2005, 90:501506.
6. Kadowaki T, Miyake Y, Kajinuma H: Risk factors for worsening to diabetes
in subjects with impaired glucose tolerance. Diabetologia 1984, 26:4449.
Ohkura et al. BMC Research Notes 2013, 6:453
http://www.biomedcentral.com/1756-0500/6/453
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
Kadowaki T, Yoshinaga H: Risk factors for the development of non-insulindependent diabetes mellitus (NIDDM) in Japan. Diabetes Res Clin Pract
1994, 24:123127.
Kitasato L, Tojo T, Hatakeyama Y, Kameda R, Hashikata T, Yamaoka-Tojo M:
Postprandial hyperglycemia and endothelial function in type 2 diabetes:
focus on mitiglinide. Cardiovasc Diabetol 2012, 11:79.
Kuzuya T, Nakagawa S, Satoh J, Kanazawa Y, Iwamoto Y, Kobayashi M,
Nanjo K, Sasaki A, Seino Y, Ito C, Shima K, Nonaka K, Kadowaki T, Committee
of the Japan Diabetes Society on the diagnostic criteria of diabetes mellitus:
Report of the Committee on the classification and diagnostic criteria of
diabetes mellitus. Diabetes Res Clin Pract 2002, 55:6585.
Yoshino G, Tominaga M, Hirano T, Shiba T, Kashiwagi A, Tanaka A, Tada N,
Onuma T, Egusa G, Kuwashima M, Sanke T, Oikawa S, Honda K, Tachikawa T:
The test meal A:a pilot model for the international standard of test meal
for an assessment of both postprandial hyperglycemia and
hyperlipidemia. J Jpn Diabetes Soc 2006, 49:361371.
Ohkura T, Shiochi H, Fujioka Y, Sumi K, Yamamoto N, Matsuzawa K, Izawa S,
Kinoshita H, Ohkura H, Kato M, Taniguchi SI, Yamamoto K: 20/(fasting
C-peptide x fasting plasma glucose) is a simple and effective index of
insulin resistance in patients with type 2 diabetes mellitus: a preliminary
report. Cardiovasc Diabetol 2013, 12:21.
Kashiwagi A, Kasuga M, Araki E, Oka Y, Hanafusa T, Ito H, Tominaga M,
Oikawa S, Noda M, Kawamura T, Sanke T, Namba M, Hashiramoto M,
Sasahara T, Nishio Y, Kuwa K, Ueki K, Takei I, Umemoto M, Murakami M,
Yamakado M, Yatomi Y, Ohashi H: Committee on the standardization of
diabetes mellitus-related laboratory testing of Japan diabetes society,
international clinical harmonization of glycated hemoglobin in Japan:
from Japan diabetes society to national glycohemoglobin
standardization program values. J Diabetes Invest 2012, 3:3940.
Seltzer HS, Allen EW, Herron AL Jr, Brennan MT: Insulin secretion in
response to glycemic stimulus: relation of delayed initial release to
carbohydrate intolerance in mild diabetes mellitus. J Clin Invest 1967,
46:323335.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC:
Homeostasis model assessment: insulin resistance and beta-cell function
from fasting plasma glucose and insulin concentrations in man.
Diabetologia 1985, 28:412419.
Matsuda M, DeFronzo RA: Insulin sensitivity indices obtained from oral
glucose tolerance testing: comparison with the euglycemic insulin
clamp. Diabetes Care 1999, 22:14621470.
Kawai J, Ohara-Imaizumi M, Nakamichi Y, Okamura T, Akimoto Y, Matsushima S,
Aoyagi K, Kawakami H, Watanabe T, Watada H, Kawamori R, Nagamatsu S:
Insulin exocytosis in Goto-Kakizaki rat beta-cells subjected to long-term
glinide or sulfonylurea treatment. Biochem J 2008, 412:93101.
Laghmich A, Ladriere L, Malaisse-Lagae F, Malaisse WJ: Long-term effects of
glibenclamide and nateglinide upon pancreatic islet function in normal
and diabetic rats. Pharmacol Res 1999, 40:475482.
Roder ME, Porte D Jr, Schwartz RS, Kahn SE: Disproportionately elevated
proinsulin levels reflect the degree of impaired B cell secretory capacity
in patients with noninsulin-dependent diabetes mellitus. J Clin Endocrinol
Metab 1997, 83:604608.
Assaloni R, Da Ros R, Quagliaro L, Piconi L, Maier A, Zuodar G, Motz E,
Ceriello A: Effects of S21403 (mitiglinide) on postprandial generation of
oxidative stress and inflammation in type 2 diabetic patients.
Diabetologia 2005, 48:19191924.
Haffner SM, Mykknen L, Valdez RA, Stern MP, Holloway DL, Monterrosa A,
Bowsher RR: Disproportionately increased proinsulin levels are associated
with the insulin resistance syndrome. J Clin Endocrinol Metab 1994,
79:18061810.
Pftzner A, Kunt T, Hohberg C, Mondok A, Pahler S, Konrad T, Lbben G,
Forst T: Fasting intact proinsulin is a highly specific predictor of insulin
resistance in type 2 diabetes. Diabetes Care 2004, 27:682687.
Nagi DK, Ali VM, Yudkin JS: Effect of metformin on intact proinsulin and
des 31, 32 proinsulin concentrations in subjects with non insulin
dependent (type2) diabetes mellitus. Diabetic Med 1996, 13:753757.
Pftzner A, Forst T: Elevated intact proinsulin levels are indicative of
Beta-cell dysfunction, insulin resistance, and cardiovascular risk: impact of
the antidiabetic agent pioglitazone. J Diabetes Sci Technol 2011, 5:784793.
Gama R, Shah S, Wright J, Marks V: Hyperinsulinaemia of
hypertriglyceridaemia: a reappraisal. Diabet Med 1995, 12:321324.
Page 8 of 8
25. Cooper MB, Tan KCB, Hales CN: Postprandial lipid metabolism and B-cell
function in non-insulin-dependent (type 2) diabetes mellitus after mixed
meals with a high fat content. Diabetic Med 1996, 13:816827.
26. Del Prato S, Tiengo A: The importance of first-phase insulin secretion:
implications for the therapy of type 2 diabetes mellitus. Diabetes Metab
Res Rev 2001, 17:164174.
27. Pftzner A, Pftzner AH, Larbig M, Forst T: Role of intact proinsulin in
diagnosis and treatment of type 2 diabetes mellitus. Diabetes Technol
Ther 2004, 6:405412.
doi:10.1186/1756-0500-6-453
Cite this article as: Ohkura et al.: The proinsulin/insulin (PI/I) ratio is
reduced by postprandial targeting therapy in type 2 diabetes mellitus: a
small-scale clinical study. BMC Research Notes 2013 6:453.
Submit your next manuscript to BioMed Central
and take full advantage of:
Convenient online submission
Thorough peer review
No space constraints or color gure charges
Immediate publication on acceptance
Inclusion in PubMed, CAS, Scopus and Google Scholar
Research which is freely available for redistribution
Submit your manuscript at
www.biomedcentral.com/submit
Vous aimerez peut-être aussi
- Jurnal DMDocument5 pagesJurnal DMratihparmadiniPas encore d'évaluation
- HPP 3 55Document9 pagesHPP 3 55AwfaPas encore d'évaluation
- The Glucose-Lowering Efficacy of Sitagliptin in Obese Japanese Patients With Type 2 DiabetesDocument9 pagesThe Glucose-Lowering Efficacy of Sitagliptin in Obese Japanese Patients With Type 2 DiabetesJavier VillavicencioPas encore d'évaluation
- v59 n1-2 p166Document8 pagesv59 n1-2 p166Auzia Tania UtamiPas encore d'évaluation
- Beta Cell Response To A Mixed Meal in Nigerian Patients With Type 2 DiabetesDocument6 pagesBeta Cell Response To A Mixed Meal in Nigerian Patients With Type 2 DiabetesEza MelindaPas encore d'évaluation
- JDM20120200002 37731682Document5 pagesJDM20120200002 37731682Raissa Andi SoekrisnoPas encore d'évaluation
- c3 Type 1 Diabetes MellitusDocument10 pagesc3 Type 1 Diabetes Mellitusjulio perezPas encore d'évaluation
- Effects of High Performance Inulin Supplementation On Glycemic Control and Antioxidant Status in Women With Type 2 DiabetesDocument9 pagesEffects of High Performance Inulin Supplementation On Glycemic Control and Antioxidant Status in Women With Type 2 DiabetesNia Tiffany HarrkaPas encore d'évaluation
- Molecular Nutrition and Diabetes: A Volume in the Molecular Nutrition SeriesD'EverandMolecular Nutrition and Diabetes: A Volume in the Molecular Nutrition SeriesDidac MauricioÉvaluation : 3 sur 5 étoiles3/5 (3)
- Type 1 Diabetes MellitusDocument10 pagesType 1 Diabetes Mellitusayu permata dewiPas encore d'évaluation
- Effect of A High-Protein, Low-Carbohydrate Diet On Blood Glucose Control in People With Type 2 DiabetesDocument8 pagesEffect of A High-Protein, Low-Carbohydrate Diet On Blood Glucose Control in People With Type 2 DiabetesFajar AgPas encore d'évaluation
- Mitigating Effects of Vildagliptin in Experimental Diabetes With Metabolic SyndromeDocument9 pagesMitigating Effects of Vildagliptin in Experimental Diabetes With Metabolic Syndromerajesh sumanPas encore d'évaluation
- Asemi 2015Document7 pagesAsemi 2015ahmad azhar marzuqiPas encore d'évaluation
- SGLT2 Inhibitors Tested to Delay Prediabetes Progression in Clinical TrialDocument5 pagesSGLT2 Inhibitors Tested to Delay Prediabetes Progression in Clinical TrialRiyan NuelPas encore d'évaluation
- 62 Ej14-0602 PDFDocument11 pages62 Ej14-0602 PDFEsteban Martin Chiotti KaneshimaPas encore d'évaluation
- Empagliflozin Monotherapy in Japanese Patients With Type 2 Diabetes Mellitus: A Randomized, 12-Week, Double-Blind, Placebo-Controlled, Phase II TrialDocument18 pagesEmpagliflozin Monotherapy in Japanese Patients With Type 2 Diabetes Mellitus: A Randomized, 12-Week, Double-Blind, Placebo-Controlled, Phase II TrialKeenan JaquesPas encore d'évaluation
- Smith 2011Document7 pagesSmith 2011sari putriPas encore d'évaluation
- Review ArticleDocument9 pagesReview ArticleottohasibuPas encore d'évaluation
- Types of Diabetes That The Dipeptidyl Peptidase-4 Inhibitor May Act Effectively and SafelyDocument5 pagesTypes of Diabetes That The Dipeptidyl Peptidase-4 Inhibitor May Act Effectively and SafelyRidha Surya NugrahaPas encore d'évaluation
- 2018 Body Mass Index 23 Is A Risk Factor For Insulin Resistance and Diabetes in Japanese PeopleDocument11 pages2018 Body Mass Index 23 Is A Risk Factor For Insulin Resistance and Diabetes in Japanese PeopleSathyanarayana SrikantaPas encore d'évaluation
- Nfs 774 Case StudyDocument37 pagesNfs 774 Case Studyapi-533845626Pas encore d'évaluation
- Effect of The GLP-1 Receptor Agonist Lixisenatide On Counter-Regulatory Responses To Hypoglycemia in Subjects With Insulin-Treated Type 2 DiabetesDocument8 pagesEffect of The GLP-1 Receptor Agonist Lixisenatide On Counter-Regulatory Responses To Hypoglycemia in Subjects With Insulin-Treated Type 2 DiabetestarietarooPas encore d'évaluation
- Antidiabetes Oral Kombinasi InsulinDocument10 pagesAntidiabetes Oral Kombinasi InsulinseptariefPas encore d'évaluation
- Insulina DM2 PDFDocument11 pagesInsulina DM2 PDFGabriel VargasPas encore d'évaluation
- Associations of Glucose Control with Insulin Sensitivity and Pancreatic β-Cell Responsiveness in Newly Presenting Type 2 DiabetesDocument6 pagesAssociations of Glucose Control with Insulin Sensitivity and Pancreatic β-Cell Responsiveness in Newly Presenting Type 2 DiabetesJoseph PositivoPas encore d'évaluation
- (20493614 - Endocrine Connections) Incretin-Based Therapies For Patients With Type 1 Diabetes - A Meta-AnalysisDocument12 pages(20493614 - Endocrine Connections) Incretin-Based Therapies For Patients With Type 1 Diabetes - A Meta-AnalysisIntan OktapiaPas encore d'évaluation
- Zhou2019 Article InsulinDegludecANovelUltra-LonDocument18 pagesZhou2019 Article InsulinDegludecANovelUltra-LonmehakPas encore d'évaluation
- Artigo 1Document7 pagesArtigo 1Maria LeonorPas encore d'évaluation
- Interleukin-1-Receptor Antagonist in Type 2 Diabetes MellitusDocument10 pagesInterleukin-1-Receptor Antagonist in Type 2 Diabetes MellitusSoleh SundawaPas encore d'évaluation
- GAD65 Antigen Therapy Fails to Preserve Beta-Cell Function in New-Onset Type 1 DiabetesDocument4 pagesGAD65 Antigen Therapy Fails to Preserve Beta-Cell Function in New-Onset Type 1 DiabetesDenniel FahreviPas encore d'évaluation
- Pharmacologic Approaches To Glycemic Treatment Standards of Medical Care in Diabetes-2018Document13 pagesPharmacologic Approaches To Glycemic Treatment Standards of Medical Care in Diabetes-2018ferrossanchezPas encore d'évaluation
- 1826 Full PDFDocument7 pages1826 Full PDFNia Tiffany HarrkaPas encore d'évaluation
- Trerapi Insulin Siip 2Document10 pagesTrerapi Insulin Siip 2Indra YudaPas encore d'évaluation
- Safety and efficacy of tofogliflozin in real-world Japanese patientsDocument12 pagesSafety and efficacy of tofogliflozin in real-world Japanese patientsnitrinitriPas encore d'évaluation
- Insulin Therapy For Type 2 Diabetes Mellitus.Document11 pagesInsulin Therapy For Type 2 Diabetes Mellitus.Clarissa CozziPas encore d'évaluation
- Improvement of Insulin Sensitivity in Patients With Type 2 Diabetes Mellitus After Oral Administration of Alpha-Lipoic AcidDocument8 pagesImprovement of Insulin Sensitivity in Patients With Type 2 Diabetes Mellitus After Oral Administration of Alpha-Lipoic AcidMaghfirahEkasariLaitjinaraPas encore d'évaluation
- Evaluación de Un Ingrediente Funcional para El Control Glicémico en HumanosDocument10 pagesEvaluación de Un Ingrediente Funcional para El Control Glicémico en HumanosDiego Gallegos lopezPas encore d'évaluation
- Jurnal Pilihan PDFDocument4 pagesJurnal Pilihan PDFIWayanSuparthanayaPas encore d'évaluation
- Insulin Pump Therapy Associated with Lower Risk of Severe HypoglycemiaDocument10 pagesInsulin Pump Therapy Associated with Lower Risk of Severe HypoglycemiaCaroline QueirogaPas encore d'évaluation
- Intensive insulin therapy maintains HbA1c levels and prevents complications in Japanese patients with type 2 diabetesDocument5 pagesIntensive insulin therapy maintains HbA1c levels and prevents complications in Japanese patients with type 2 diabetesAndreea GherasimPas encore d'évaluation
- Insulin AspartatDocument6 pagesInsulin AspartatatyPas encore d'évaluation
- Effects of growth hormone treatment on obese NIDDM patientsDocument1 pageEffects of growth hormone treatment on obese NIDDM patientsamritaryaaligarghPas encore d'évaluation
- Efficacy and Safety of Biosimilar Glargine-IMGDocument8 pagesEfficacy and Safety of Biosimilar Glargine-IMGSiddiq MohammedPas encore d'évaluation
- A Lower-Carbohydrate, Higher-Fat Diet Reduces Abdominal and Intermuscular Fat and Increases Insulin Sensitivity in Adults at Risk of Type 2 DiabetesDocument7 pagesA Lower-Carbohydrate, Higher-Fat Diet Reduces Abdominal and Intermuscular Fat and Increases Insulin Sensitivity in Adults at Risk of Type 2 DiabetesAureliaIstiQomahPas encore d'évaluation
- dmj-37-465Document10 pagesdmj-37-465sn4s7nyxcbPas encore d'évaluation
- Diabetes Artigo 04Document19 pagesDiabetes Artigo 04Júlio EpifanioPas encore d'évaluation
- Muito Baixo Dietas Com Baixo Teor CalóricDocument10 pagesMuito Baixo Dietas Com Baixo Teor CalóricDesolation FestPas encore d'évaluation
- The Effects of Licogliflozin, A Dual SGLT12 Inhibitor, On BodyDocument11 pagesThe Effects of Licogliflozin, A Dual SGLT12 Inhibitor, On BodyJose Mario HoyosPas encore d'évaluation
- yan 2019Document11 pagesyan 2019Sara ÖZGENPas encore d'évaluation
- Eficiencia y Tolerabilidad Glimepirida y MetfomrinaDocument7 pagesEficiencia y Tolerabilidad Glimepirida y MetfomrinaMarioA.VelascoCórdobaPas encore d'évaluation
- 1 AnDocument9 pages1 AnDana GrigorescuPas encore d'évaluation
- 11Document13 pages11Panji Tutut AnggraeniPas encore d'évaluation
- Effect of 1 Years Orlistat Treatment Compared To Placebo On Insulin Resistance Parameter in Patients With Type 2 DiabetesDocument9 pagesEffect of 1 Years Orlistat Treatment Compared To Placebo On Insulin Resistance Parameter in Patients With Type 2 Diabetesmuhammad ricky kurniawanPas encore d'évaluation
- Ketogenic Diet HypoglycaemiaDocument6 pagesKetogenic Diet HypoglycaemiaPeter McPhersonPas encore d'évaluation
- Sitagliptin vs. Pioglitazone As Add-On Treatments in Patients With Uncontrolled Type 2 Diabetes On The Maximal Dose of Metformin Plus SulfonylureaDocument9 pagesSitagliptin vs. Pioglitazone As Add-On Treatments in Patients With Uncontrolled Type 2 Diabetes On The Maximal Dose of Metformin Plus SulfonylureaFebi FernandaPas encore d'évaluation
- Ada WhoDocument7 pagesAda WhoHironmoy RoyPas encore d'évaluation
- Original Article: A. Kashiwagi, H. Takahashi, H. Ishikawa, S. Yoshida, K. Kazuta, A. Utsuno & E. UeyamaDocument9 pagesOriginal Article: A. Kashiwagi, H. Takahashi, H. Ishikawa, S. Yoshida, K. Kazuta, A. Utsuno & E. UeyamadbcooperdkPas encore d'évaluation
- Naplex Complete Study Outline A Topic-Wise Approach DiabetesD'EverandNaplex Complete Study Outline A Topic-Wise Approach DiabetesÉvaluation : 4 sur 5 étoiles4/5 (2)
- Effect of high-protein, low-carb diets on type 2 diabetesDocument10 pagesEffect of high-protein, low-carb diets on type 2 diabetesFirda Rizky KhoerunnissaPas encore d'évaluation
- Emerging Treatments Improve Diabetes ControlDocument10 pagesEmerging Treatments Improve Diabetes ControlAyman AleemPas encore d'évaluation
- MatfDocument1 pageMatfSoleh SundawaPas encore d'évaluation
- MatfDocument1 pageMatfSoleh SundawaPas encore d'évaluation
- Short vs Long Antibiotic Therapy for UTIs in Older WomenDocument2 pagesShort vs Long Antibiotic Therapy for UTIs in Older WomenSoleh SundawaPas encore d'évaluation
- Ovarian Germ Cell Tumors TreatmentDocument6 pagesOvarian Germ Cell Tumors TreatmentSoleh SundawaPas encore d'évaluation
- GoryuuuiDocument1 pageGoryuuuiSoleh SundawaPas encore d'évaluation
- High-Dose Rifapentine With Moxifloxacin For Pulmonary TuberculosisDocument10 pagesHigh-Dose Rifapentine With Moxifloxacin For Pulmonary TuberculosisSoleh SundawaPas encore d'évaluation
- BtsDocument1 pageBtsSoleh SundawaPas encore d'évaluation
- Down SyndromeDocument9 pagesDown SyndromeSoleh SundawaPas encore d'évaluation
- Amenaza de AbortoDocument5 pagesAmenaza de AbortoCarlos TalismannPas encore d'évaluation
- Interleukin-1-Receptor Antagonist in Type 2 Diabetes MellitusDocument10 pagesInterleukin-1-Receptor Antagonist in Type 2 Diabetes MellitusSoleh SundawaPas encore d'évaluation
- Perenc Kebutuhan SDM KeshtDocument8 pagesPerenc Kebutuhan SDM KeshtupikPas encore d'évaluation
- Akupuntur MedikDocument7 pagesAkupuntur MedikSoleh SundawaPas encore d'évaluation
- Perenc Kebutuhan SDM KeshtDocument8 pagesPerenc Kebutuhan SDM KeshtupikPas encore d'évaluation
- Zd. CataractDocument31 pagesZd. CataractSoleh SundawaPas encore d'évaluation
- Da C Rio CystitisDocument34 pagesDa C Rio CystitisSoleh SundawaPas encore d'évaluation
- CURRICULUM VITAE AND HISTORY OF INSULINDocument45 pagesCURRICULUM VITAE AND HISTORY OF INSULINDian SobaPas encore d'évaluation
- Correlation Serum Ferritin HbA1c Type2 Diabetes Patients Tertiary HealthcareDocument7 pagesCorrelation Serum Ferritin HbA1c Type2 Diabetes Patients Tertiary HealthcareSSR-IIJLS JournalPas encore d'évaluation
- Pengaruh Pendidikan Kesehatan Terhadap Kepatuhan Diet Pada Pasien DM Tipe2 Di Irna Non Bedah Penyakit Dalam Rsup Dr.M. Djamil Padang Tahun 2014Document10 pagesPengaruh Pendidikan Kesehatan Terhadap Kepatuhan Diet Pada Pasien DM Tipe2 Di Irna Non Bedah Penyakit Dalam Rsup Dr.M. Djamil Padang Tahun 2014Yeni NoviyantiPas encore d'évaluation
- Final1 Gatut-Pkb Unpad April09 - MetforminDocument32 pagesFinal1 Gatut-Pkb Unpad April09 - Metforminsuho exoPas encore d'évaluation
- Critical Thinking Exercise No.9 Nursing Management of The Client With DIABETES MELLITUS (Case Study 3)Document2 pagesCritical Thinking Exercise No.9 Nursing Management of The Client With DIABETES MELLITUS (Case Study 3)Lovie Japhet LopezPas encore d'évaluation
- 6.2 Diabetes MellitusDocument53 pages6.2 Diabetes MellitusMohammad AlrefaiPas encore d'évaluation
- Laboratory Test Report: Test Name Result Biological Reference Interval Glycosylated HaemoglobinDocument3 pagesLaboratory Test Report: Test Name Result Biological Reference Interval Glycosylated HaemoglobinSri ShivaPas encore d'évaluation
- M2C19 Types of InsulinDocument2 pagesM2C19 Types of Insulinirnumambreen15Pas encore d'évaluation
- CGM Comparison For People With Insulin Treated Research July 2023Document11 pagesCGM Comparison For People With Insulin Treated Research July 2023shahirahPas encore d'évaluation
- Inv. Virtual Conference Ryzodeg-16 JAN 2021 - Final - OKDocument4 pagesInv. Virtual Conference Ryzodeg-16 JAN 2021 - Final - OKmelyekaPas encore d'évaluation
- Dr. Osama's Guide to Treating Diabetes with Insulin, Oral Medications and Incretin TherapyDocument33 pagesDr. Osama's Guide to Treating Diabetes with Insulin, Oral Medications and Incretin Therapyمحيي الدين الكميشىPas encore d'évaluation
- Censo Sospechosos 2017Document121 pagesCenso Sospechosos 2017KarlaPas encore d'évaluation
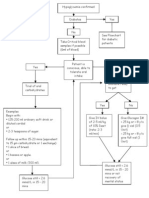
- Hypoglycaemia FlowchartDocument1 pageHypoglycaemia FlowchartMohammad SultanPas encore d'évaluation
- Diabetes in Pregnancy: Management ofDocument8 pagesDiabetes in Pregnancy: Management ofdiana rossPas encore d'évaluation
- Diet Dan Olahraga Sebagai Upaya Pengendalian Kadar Gula Darah Pada Pasien Diabetes Melitus Tipe 2 Di Poliklinik Penyakit Dalam RSUD Ulin Banjarmasin Tahun 2015Document10 pagesDiet Dan Olahraga Sebagai Upaya Pengendalian Kadar Gula Darah Pada Pasien Diabetes Melitus Tipe 2 Di Poliklinik Penyakit Dalam RSUD Ulin Banjarmasin Tahun 2015Haifatul AlimahPas encore d'évaluation
- Insulin Dosing For Fat and ProteinDocument19 pagesInsulin Dosing For Fat and Proteinapi-356625183Pas encore d'évaluation
- Week 3 Practical - Colorimetric Estimation of Blood Sugar LDocument8 pagesWeek 3 Practical - Colorimetric Estimation of Blood Sugar LBrainUniverse UnasmPas encore d'évaluation
- S51 - LPL - Bhubaneswar PURABI PLOT No. 2084/4837, Vivekananda M Arg, (Near Bhubaneswar Municipality & Mo BhubneshwarDocument4 pagesS51 - LPL - Bhubaneswar PURABI PLOT No. 2084/4837, Vivekananda M Arg, (Near Bhubaneswar Municipality & Mo BhubneshwarAnkita PriyadarsiniPas encore d'évaluation
- Why Is My Blood Sugar High in The MorningDocument4 pagesWhy Is My Blood Sugar High in The MorningRodolfo CorpuzPas encore d'évaluation
- Rbs Ogtt Final PresentDocument40 pagesRbs Ogtt Final PresentFrances GrefalPas encore d'évaluation
- Gestational DiabetesDocument21 pagesGestational DiabetesRiko Sampurna SimatupangPas encore d'évaluation
- Gudoy, Charies Jamille 12-WeierstrassDocument4 pagesGudoy, Charies Jamille 12-WeierstrasschaPas encore d'évaluation
- Diabetes Mellitus Definition, Types, Symptoms, and TreatmentDocument27 pagesDiabetes Mellitus Definition, Types, Symptoms, and Treatmentana chasanahPas encore d'évaluation
- Tugas Artikel AgustinDocument8 pagesTugas Artikel AgustinMiko WidiatmokoPas encore d'évaluation
- Latent Autoimmune Diabetes in Adults TDDocument3 pagesLatent Autoimmune Diabetes in Adults TDapi-648595816Pas encore d'évaluation
- Himawan - BPJSDocument26 pagesHimawan - BPJSAndi Upik FathurPas encore d'évaluation
- Children Presentation Nutrition and DiabetesDocument19 pagesChildren Presentation Nutrition and Diabetesapi-516120803Pas encore d'évaluation
- Investigatory Project ON Diabetes Mellitus: Name: Sagnik KulaviDocument22 pagesInvestigatory Project ON Diabetes Mellitus: Name: Sagnik Kulavisancharini kulaviPas encore d'évaluation
- Endocrine Pharmacology of Diabetes and Anti-Diabetic DrugsDocument16 pagesEndocrine Pharmacology of Diabetes and Anti-Diabetic DrugsAyro Business CenterPas encore d'évaluation
- Penerapan Asuhan Keperawatan Pada Pasien Ny. N Dengan DM Tipe Ii Dalam Pemenuhan Kebutuhan Nutrisi Di Rsud Labuang Baji MakassarDocument19 pagesPenerapan Asuhan Keperawatan Pada Pasien Ny. N Dengan DM Tipe Ii Dalam Pemenuhan Kebutuhan Nutrisi Di Rsud Labuang Baji MakassarHerman HermanPas encore d'évaluation