Académique Documents
Professionnel Documents
Culture Documents
Preserving Lean in Healthcare: Advanced Analysis in Organization Studies, Master Course, Spring 2015
Transféré par
Jonas LeoDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Preserving Lean in Healthcare: Advanced Analysis in Organization Studies, Master Course, Spring 2015
Transféré par
Jonas LeoDroits d'auteur :
Formats disponibles
Preserving Lean in Healthcare
Advanced Analysis in Organization Studies, Master Course,
Spring 2015*
Authors:
Silviu Iliesiu
Irina Popkov
Elina Rekil
*This study was conducted as our course project and it is not an official study sanctioned by Uppsala University.
This study was part of a course module and its findings should be treated as more of a prelude for possible
further study. Correspondence: Silviu.Iliesiu.1603@student.uu.se.
Silviu Iliesiu | Irina Popkov | Elina Rekil
Contents
1. Introduction
.........................................................................................................................................
3
2. Literature Review
................................................................................................................................
3
2.1 The Five Lean Principles
..............................................................................................................
4
2.2 Institutionalizing Organizational Change
......................................................................................
5
2.3 Pettigrew and Whipps Model of Strategic Management of Change
............................................
6
2.4 Summary and Analytical Framework
............................................................................................
7
3. Methodology and Research Design
.....................................................................................................
8
3.1 Data Collection Methods and Sampling
........................................................................................
8
3.2 Data Analysis Methods
.................................................................................................................
8
3.3 Validity and Reliability
.................................................................................................................
9
3.4 Limitations
..................................................................................................................................
10
4. Results and Discussion of Empirical Data
........................................................................................
10
5. Conclusions and Implications for Researchers and Practitioners
......................................................
12
Reference List
.......................................................................................................................................
13
Appendix
...............................................................................................................................................
15
AAOS Master Course, June 2015
Silviu Iliesiu | Irina Popkov | Elina Rekil
1. Introduction
In organization theory, change is seen as the result of travel of ideas (Czarniawska & Sevon,
1996). One of the most relevant examples of our time is the travel of ideas from private (e.g.
Lean management) to public sectors (e.g. healthcare). Generally speaking, Lean management
as such aims at increasing output by decreasing input (Poksinska, 2010). Lean is not just a
managerial tool, but a holistic management philosophy and a new way of working centered on
continuous improvements. The very idea behind adopting Lean is to ingrain it into an
organizations culture. In short, success with Lean arguably depends on it being
institutionalized and used continuously in the long-run (Poksinska, 2010; Womack & Jones,
1996). Placed in a broader context, the proposed project addresses the research problem of
researchers and practitioners not knowing enough about how such change management
initiatives can be successfully preserved best in healthcare organizations (HO). In order to
steer the process of finding a solution to the problem, the following research question is
formulated:
What drives the institutionalization of Lean in healthcare organizations?
In addition to the high failure rate, the theoretical framework (chapter two) will show that
there is a lack of research when it comes to how Lean management can be implemented and
institutionalized in HO successfully. Hence, building on the research question stated above,
the purpose of this study is of explanatory nature, helping academia better understand
theoretical implications of what drives preservation of change and providing practitioners
with a better understanding of conditions for lasting and successful change (Drogendijk,
2009). The following chapters contain a theoretical framework to support the study and to
demonstrate that Lean is to be seen as a holistic management philosophy, an outline of the
methodology, our analysis and discussion of empirical results, and lastly, final conclusions.
2. Literature Review
Lean is considered a management philosophy rather than a managerial tool that is centered on
creating value by understanding the process steps that add value and those that do not
(Womack & Jones, 1996). According to Miller and Womack, Jones, and Roos, Lean is
applicable to all organizations since its fundamentals revolve around improving processes
(Miller, 2005; Womack, et al., 1990). All organizations, including healthcare, are made up of
processes that are intended to create value for the customer. As such, Lean healthcare is about
AAOS Master Course, June 2015
Silviu Iliesiu | Irina Popkov | Elina Rekil
continuously improving processes by either adding value or eliminating wasteful non-value
activities (Poksinska, 2010; Radnor, 2011). Proponents have argued for adopting Lean in
healthcare, in order to cope with the increasing demand for healthcare services due to aging
populations and dire financial conditions (Poksinska, 2010).
In the healthcare sector, care processes are organized with a focus on doctors, nurses, and
other clinical staff and are often not optimized for patients (Poksinska, 2010). The care is
organized in departmental silos and the only person who sees the whole patient journey, is
often the patient. In such systems, a patient can spend hours in hospitals for little value-adding
time. Applying Lean tools and thinking has the potential to break down the silo mentality and
enable change to occur across functional boundaries. It enables HO to take a holistic view of
the entire care process, and coordinate it to identify and eliminate process steps that add no
value for the patient. As such, it comes as no surprise that Poksinska found that the five most
common applications of Lean in healthcare were (in order): process improvement, continuous
flow, value stream mapping (VSM), waste elimination, and teamwork (Poksinska, 2010).
These findings are largely congruent with Rognes and Svarts research (2012), which found
that Swedish hospitals working with Lean, mainly focused on process flow improvements as
well as teamwork (Rognes & Svarts, 2012). The focus of process improvement lies on
improving the whole process (Jones & Mitchell, 2006). This explains why working in teams
is widespread since Lean requires an interdisciplinary team approach and the integration of
different care processes into one value flow (Poksinska, 2010).
2.1 The Five Lean Principles
The core principles of Lean are based on an underlying assumption that organizations are
made up of processes, and these link to the concept of value, waste reduction, and continuous
improvement (Kaizen) into an ever-repeating process (Womack & Jones, 1996). Together,
these concepts make up the philosophy of Lean. The five Lean principles (see table 1 below)
can also be seen as a step-wise approach for organizations seeking to implement Lean
(Poksinska, 2010). Poksinskas research shows that the three first steps have a good coverage
in the Lean Healthcare literature, but the application of steps four and five are more difficult
to observe. Poksinska contends that although seeking perfection might seem as continuous
improvement (i.e. Kaizen), the concept of seeking perfection is broader than that and refers to
developing a continuous improvement culture where improvement activities become part of
the everyday work. This, she suggests, may indicate that Lean has not yet reached this level of
AAOS Master Course, June 2015
Silviu Iliesiu | Irina Popkov | Elina Rekil
maturity in HO, which in turn means that Lean has generally not yet institutionalized. One of
the most important elements of Lean is developing people and creating a continuous
improvement culture, as the real challenge is going beyond the simple application of tools to
develop a Lean culture (Poksinska, 2010).
Table 1: The Five Lean Principles
1. Specify the value desired by the customer.
2. Identify the value stream for each product/service providing that value and, challenge
all of the wasted steps.
3. Make the product/service flow continuously. Standardize processes around best practice
allowing them to run more smoothly, freeing up time for creativity and innovation.
4. Introduce pull between all steps where continuous flow is impossible. Focus upon the
demand from the customer and trigger events backwards through the value chain.
5. Manage towards perfection so that non-value adding activity will be removed from the
value chain so that the number of steps, amount of time and information needed to serve
the customer continually falls.
2.2 Institutionalizing Organizational Change
Institutionalization involves the long-term persistence of organizational change, and such
changes are part of the organizations culture (Cummings & Worley, 2009). How planned
changes become institutionalized has not received much attention in organizational change
and development literature. Buchanan et al. contend that institutionalization is underresearched since the focus lies predominantly on the ideal organization that is capable of
ongoing adaptation in changing environments. Institutionalization is therefore not regarded as
a condition to be achieved, but a problem to be solved (Buchanan, et al., 2005). However, the
successful application of Lean arguably hinges on it becoming institutionalized. Although the
goal for Lean is to reach a level of maturity and stability, the point of this stability is to
continuously improve and change in a routinely manner. In this vein, institutionalizing change
takes on increased utility than previously acknowledged by literature, and highlights the need
for further research on how management philosophies centered on continuous improvement
and change, such as Lean, can become institutionalized in organizations.
Several authors have recognized the importance of institutionalizing planned organizational
changes (cf. Kotter, 1995). Yet, 70-80% of all planned organizational change fail to
AAOS Master Course, June 2015
Silviu Iliesiu | Irina Popkov | Elina Rekil
institutionalize (Appelbaum, et al., 2012; Hughes, 2011; Jacobs, 2002). According to
Buchanan et al., most contemporary researchers consistently advocate for processualcontextual views of institutionalization, meaning that it is a process influenced by a number of
factors including the rationale behind changes, managerial support, cultural and
organizational support, and receptivity. Processual-contextual perspectives on change mainly
derive from the work of Pettigrew, who points to the many related factors influencing the
nature and outcome of change (Buchanan, et al., 2005).
2.3 Pettigrew and Whipps Model of Strategic Management of Change
Pettigrew and Whipps Context, Content, and Process model of strategic change has been
widely used in analyzing and learning retrospectively from change programs in organizations
and was based on empirical case-based organizational research (Stetler, et al., 2007). The
model focuses on the WHY of strategic change with relevance to context; the WHAT of
strategic change in terms of its content; and the HOW of strategic change processes. These
dimensions include signs and symptoms of receptivity, which are factors that drive the
institutionalization of change initiatives. WHY refers to the context behind the motivation of
the change initiative (e.g. Lean), including: environmental pressure and key people leading
change. WHAT refers to the content of the change initiative relative to organizational
elements, such as changing the way inter-organizational networks cooperate to support the
change. HOW refers to processual change initiatives, such as installing a champion (i.e. key
people leading change) to facilitate the change and setting clear objectives with the change
initiative. Although originally developed to understand private sector organizations, Pettigrew
et al. later applied it to the study of HO. In a similar vein, Stetler et al. applied Pettigrew and
Whipps framework to (1) identify what key contextual elements support and facilitate the
institutionalization of Evidence-Based Practice (EBP); and (2) to identify what strategic
processes are used to create institutionalization of EBP in HO. Results showed that the most
critical element in influencing the institutionalization of EBP were key people leading change,
which in turn affected how other factors came to be defined and become receptive towards the
change initiative (Stetler, et al., 2007; Stetler, et al., 2009). To date, Stetler et al.s study
remains one of the few studies that looked at drivers of institutionalization of planned
organizational changes in HO through an established theoretical framework in the field.
Pettigrew and Whipps framework seems suitable for studying institutionalization of Lean in
HO. The importance of installing key people leading change was shown to be crucial in
implementing Lean (Langstrand & Drotz, 2015; Poksinska, 2010). Breaking down the siloAAOS Master Course, June 2015
Silviu Iliesiu | Irina Popkov | Elina Rekil
mentality and encouraging cross-departmental cooperation is deemed as crucial for working
with Lean in order to work with VSM (Poksinska, 2010). As such, inter-organizational
networks might be an important driver for institutionalization. Environmental pressure as
well as simplicity and clarity of goals might also be important, since research has shown that
organizations with a clear rationale and goals for adopting Lean, have managed to improve in
the desired direction, whereas organizations that adopt Lean due to institutional pressures fail
in this regard (Langstrand & Drotz, 2015).
2.4 Summary and Analytical Framework
When Lean changes persist and become part of the culture, they become institutionalized, but
very little is known about what drives the institutionalization of Lean in HO. The aim of this
study is to address this research gap by identifying what drives the institutionalization of Lean
in HO. The theoretical and analytical framework for our study is Pettigrew and Whipps
Content, Context, and Process Model of Strategic Change (Pettigrew, et al., 1992). We use a
modified version (see figure 1 below) of their framework in our attempt to identify what
drives the institutionalization of Lean in HO.
Figure 1: Pettigrew and Whipp: Signs and symptoms of receptivity
Source: (Pettigrew, et al., 1992)
AAOS Master Course, June 2015
Silviu Iliesiu | Irina Popkov | Elina Rekil
3. Methodology and Research Design
This study is a partial reproduction of another organizational case study that had been
conducted in the United States, on the institutionalization of evidence-based practice (Stetler,
et al., 2009). However, instead of focusing on evidence-based practices, we focused on the
institutionalization of Lean management in HO. We analyzed institutionalization of Lean
within Capio S:t Grans Sjukhus (henceforth referred to as CStG) in Stockholm through
Pettigrew and Whipps Content, Context, and Process Model of Strategic Change. We
pursued an explanatory case study and illustrate exact methods in the following part.
3.1 Data Collection Methods and Sampling
Primary data was collected by conducting four semi-structured interviews (qualitative),
whereof three were conducted on-site and one was via telephone. Interviews followed a
format based on Stetler et al. (see appendix for interview guide). The hospital was selected
deliberately since institutionalizing changes takes approximately 5-10 years (Buchanan, et al,
2005) and CStG had worked with Lean since 2005 and represents a role model site, having
won the Swedish Lean Award in 2010 (Capio AB, 2013). Individuals were also invited
deliberately to participate in interviews to investigate the institutionalization of Lean practices
at various levels of the organization, including Sofia Palmquist (SP), the Executive Vice
President CStG, Britta Wallgren (BW), the Chief Executive Officer CStG, Jonas Leo (JL), a
surgeon who owns the acute surgery flow, and a cardiology nurse (CN) who wished to remain
anonymous.
3.2 Data Analysis Methods
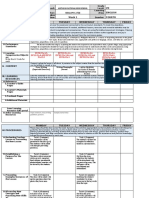
To analyze gathered data on the drivers of the institutionalization of Lean, we used
Pettigrews model of why (context), what (content) and how (process). In other words, data
from this study was summarized and compared with the studys analytical and operational
questions (see figures two and three below) based on (Stetler, et al., 2007) For this, deductive
(key terms and themes used for coding categories) and inductive (open and add to
unanticipated contextual themes identified relative to the evolution of Lean in normalization
and implementation) processes were used. Coding categories established for analysis include
environmental pressures, key people leading change, cooperative inter-organizational
networks, as well as simplicity and clarity of goals.
AAOS Master Course, June 2015
Silviu Iliesiu | Irina Popkov | Elina Rekil
What key contextual elements support and facilitate a) implementation of Lean at the project level and b)
normalization of Lean within a health care system at multiple institutional levels?
1.
2.
3.
4.
Do key contextual elements differentiate successful implementation as well as sustainability of Lean
efforts, from less successful efforts within varying levels of a hospital-based healthcare setting?
- In terms of elements either pre-existent or created through strategic change.
- In light of the interrelationship of key contextual elements over time.
Do key contextual elements differentiate successful implementation and sustainability of Lean practice
efforts from less successful efforts across similar healthcare settings interested in Lean?
Does the number of embedded units (i.e. a critical mass) within a service (and services within a
department) with key contextual elements influence the extent to which an organization has
successfully implemented and sustained Lean practice at both project level and as the norm at multiple
institutional levels?
To what extent does each of the identified models of Lean reflect the key contextual elements identified
in this study and the literature as relevant to successful and sustained implementation of Lean?
Figure 2: Key contextual elements- Core analytical general and specific research questions
What strategic approaches or implementation interventions are used to a) facilitate implementation at the
project level and b) create normalization of Lean within a healthcare system at multiple institutional levels?
1. WHY: What was/were the specific motivations for changes i.e. why did targeted
departments/ services and their embedded levels wish to implement Lean?
i.
In terms of specific projects
In general, within the department/service and other embedded levels.
2. WHAT: What was the content of related contextual change for generic, sustained Lean over time?
ii.
What key contextual elements or other entities in the system were changed to enhance or
support the routine use of evidence? E.g. alignment of infrastructure with the new purpose,
values, vision, strategy, priorities i.e. change in various operational structures, systems,
roles, job descriptions, processes and relations: budgeting; etc.
3. HOW: What was the process used to create an individual change to Lean, i.e. what was the method
used to try to get Lean implemented?
i.
Which, if any, specific implementation interventions/strategies were used to try to enable
the use of an individual, targeted piece or program of evidence? E.g. use of a dedicated
project lead? Use of a standard organizational approach to change project? Use of a
facilitator/champion? Use of Lean change strategies, e.g. audit/feedback, opinion
leadership, QI team, clinical reminder etc.?
Figure 3: Implementation interventions and strategic processes- Core operational research
questions and sample related sub-questions
3.3 Validity and Reliability
Internal validity refers to the correct conclusions, thus it was vital to analyze the results
avoiding bias, which was addressed as the data was reviewed by all three researchers.
External validity refers to the findings being generalizable to other studies (Verhoeven,
2011; Yin, 2009). In relation to this, it is necessary to consider that this study can only be
applied by HO working with Lean or wishing to implement and institutionalize it. Pettigrew
and Whipps framework was used to increase (construct) validity.
AAOS Master Course, June 2015
Silviu Iliesiu | Irina Popkov | Elina Rekil
3.4 Limitations
Limitations include that only one site was studied based on only four interviews within the
limited amount of time. Moreover, the participants were likely to provide socially desired
responses (Verhoeven, 2011; Yin, 2009), and we were aware of this fact when interpreting
and analyzing the interview data.
4. Results and Discussion of Empirical Data
The first coding category addresses environmental pressures (EP). This category helps
answering the question of what it was that motivated change and WHY the implementation of
Lean specifically, was strived for. All interviewees stated that the main motivator of and
reason for change, was the shock coming from the external environment, when Karolinska
and Huddinge hospital merged in 2005/06, which lead to an increase by 75,000 people in
CStGs patient-uptake. This EP resulted in the need to manage the patient flow more
efficiently, while still providing safe and high-quality care for patients. EP also made it
necessary to improve the working environment for staff members, since especially the
emergency department needed to manage 60,000 patients while only being built for 30,000,
and bad working conditions as well extremely long working hours, caused a 40% employee
turnover. According to all interviewees, Lean was not implemented because it was merely a
trend, but because there was a necessity to continuously be able to manage several thousands
of additional patients in the long run and improve the quality of care and patient safety. Thus,
it was an important driver for the institutionalization of Lean at CStG.
Key people leading change (KPLC) is the second coding category and was a crucial driver
for the motivation or WHY to implement Lean at CStG. KPLC were top management,
including former CEO Birgir Jakobsson who initiated the change towards adopting Lean
organization-wide, as well as early adopters of Lean within certain departments. An early
adopter was the emergency unit that had experienced a dramatic increase in its patient uptake,
in which Lean facilitators drove the motivation for change within their department as well as
others by showing that Lean could generate good results. All interviewees stated that the
change towards Lean was initiated and driven by top management and early adopters
simultaneously, and was both a top management idea and a grassroots movement, which was
crucial for driving and sustaining the motivation to adopt Lean. This suggests that KPLC were
crucial in driving and sustaining the motivation to implement Lean, which was triggered by
AAOS Master Course, June 2015
10
Silviu Iliesiu | Irina Popkov | Elina Rekil
environmental pressure. To understand WHAT KPLC did to implement Lean and support its
institutionalization and how they did it, see the following two coding categories. In short,
KPLC instituted changes such as shifting CStG from a silo to a matrix structure to enable
VSM and facilitate teamwork within and across departments. KPLC also launched
educational programs to help staff understand Lean, its goals, tools, and underlying thinking
better, which supported overcoming some of the resistance towards it. Staff came to terms
with Lean and understood that it was beneficial for themselves and the hospitals patients.
This was facilitated by the integration of Lean into CStGs strategy and goals. These findings
indicate that KPLC impacted on the institutionalization of Lean at CStG in a similar vein as in
Stetler et al.s (2009) study. Through the above mentioned change measures, KPLC impacted
on how CION and SCG came to be receptive towards change and became drivers of the
institutionalization of Lean at CStG.
The third coding category is cooperative inter-organizational networks (CION). In order to
work with VSM, it is crucial to break down the silo-mentality and encourage crossdepartmental cooperation (Poksinska, 2010). WHAT changed at CStG was that they went
from silo to matrix structure to enable VSM, in which flow owners were instated as
responsible for the entire care journey. Furthermore, to support the routine use of Lean after
the implementation phase, managerial support and education was provided to interlink the
steering groups of professional medical departments and to center more on teamwork, which
enabled better coordination across departments. This suggests that these changes enabled the
use of Lean, which in turn developed CION into a driver of the institutionalization of Lean.
The last coding category concerns simplicity and clarity of goals (SCG). Lean was initially
perceived as a managerial buzzword by parts of the staff and it was unclear how removing
waste in care processes could help the hospital improve patient care. Lean was slightly
incongruent with the staffs values. By educating staff on Lean tools and why these were
important to cope with EP and improve patient care, the goals with working with Lean
became simpler and clearer for staff to understand. CStG went from focusing on removing
waste, which was crucial to reduce lead times in the emergency unit, to focusing more on
adding value to patient care, which was more congruent with staffs values. Moreover, Lean
was integrated into CStGs strategy and goals to ensure its routine use and long-term
persistence. This indicates that these processual change initiatives to SCG enabled it to
become a driver of the institutionalization as staff came to terms with Lean and realized its
potential value.
AAOS Master Course, June 2015
11
Silviu Iliesiu | Irina Popkov | Elina Rekil
5. Conclusions and Implications for Researchers and Practitioners
The purpose of this study was to determine what drives the institutionalization of Lean in
healthcare organizations. The results and analysis show that all four factors, namely EP,
KPLC, CION, and SCG, were found to be important drivers of the institutionalization of Lean
at CStG. One tentative conclusion in line with previous research (Stetler et al., 2009), is that
KPLC play an even more crucial part in driving the institutionalization of changes within
organizations. KPLC helped sustain the motivation to implement Lean, which was triggered
by EP. Together, they shaped organizational factors like CION and SCG to become receptive
towards the change and drivers for the institutionalization of Lean. As such, all signs and
symptoms of receptivity (SOS) are interconnected, forming a pattern conducive to the
institutionalization of change initiatives in organizations, which is in line with the notion that
institutionalization is a complex process contingent on a variety of factors (Buchanan et al.,
2005). For practitioners, this demonstrates the importance of installing KPLC to drive the
change process and shape these interlinked factors to enable them to become
institutionalization drivers. Enabling CION, and integrating the goals with Lean in simple and
clear terms with the overall strategy, seem quite important. We conclude that future research
should investigate other factors in Pettigrew and Whipps framework and their influence on
the institutionalization of Lean, as the scope of this study was limited to four of the eight
factors. One suggestion is to focus on the link between the locale of the change initiative and
EP. In CStGs case, EP had a profound impact on its emergency unit, which became an early
adopter and driver of implementing Lean organization-wide. Focusing on the effect of these
two factors on the institutionalization could help further our understanding of what drives the
institutionalization of Lean in HO.
AAOS Master Course, June 2015
12
Silviu Iliesiu | Irina Popkov | Elina Rekil
Reference List
Appelbaum, S. H., Habashy, S., Malo, J. L. & Shafiq, H. (2012). Back to the future: revisiting
Kotter's 1996 change model. Journal of Management Development, 31(8), pp. 764-782.
Buchanan, D. et al. (200)5. No going back: A review of the literature on sustaining
organizational change. International Journal of Management Reviews, 7(3), pp. 189-205.
Capio AB, 2013. Capio. [Online]
Available
at:
http://capio.com/en/media/newsroom/news/2010/capio-st-gorans-hospital-
receives-awards/
[Accessed 27 March 2015].
Cummings, T. & Worley, C. (2009). Organization Development & Change. Mason, OH:
South-Western Cengage Learning.
Czarniawska, B. & Sevon, G. (1996). Translating Organizational Change. s.l.:De Gruyter.
Drogendijk, R. (2009). Writing a Thesis at the Bachelor or Master Level, Uppsala: Uppsala
University.
Hughes, M. (2011). Do 70 Per Cent of All Organizational Change Initiatives Really Fail?.
Journal of Change Management, 11(4), pp. 451-464.
Jacobs, R. L. (2002). Institutionalizing organizational change through cascade training.
Journal of European Industrial Training, Volume 26, pp. 177-182.
Jones, D. & Mitchell, A. (2006). Lean thinking for the NHS. London: NHS confederation.
Kotter, J. P. (1995). Leading change: Why transformation efforts fail. Harvard Business
Review, 73(2), pp. 59-67.
Langstrand, J. & Drotz, E. (2015). The rhetoric and reality of Lean: a multiple case study.
Total Quality Management & Business Excellence, pp. 1-15.
Miller, D. (2005). Going Lean in Health Care, Cambridge, MA: Institute for Healthcare
Improvement.
Pettigrew, A., Ferlie, E. & McKee, L. (1992). Shaping strategic change-The case of the NHS
in the 1980s. Public Money & Management, 12(3), pp. 27-31. Poksinska, B. (2010). The
current state of Lean implementation in health care: literature review. Quality Management in
Healthcare, 19(4), pp. 319-329.
AAOS Master Course, June 2015
13
Silviu Iliesiu | Irina Popkov | Elina Rekil
Radnor, Z. (2011). Implementing Lean in Health Care: Making the link between the approach,
readiness and sustainability. International Journal of Industrial Engineering and Management,
2(1), pp. 1-12.
Rognes, J. & Svarts, A. (2012). Lean i vrden: en versikt ver dagslget i Sverige. Leading
Health Care, Issue 2, pp. 18-46.
Stetler, C. B. et al. (2009). Institutionalizing evidence-based practice: an organizational case
study using a model of strategic change. Implement Science, 4(78), pp. 1-19.
Stetler, C. B. et al. (2007). Improving quality of care through routine, successful
implementation of evidence-based practice at the bedside: an organizational case study
protocol using the Pettigrew and Whipp model of strategic change.. Implement Science, 2(3).
Verhoeven, N. (2011). Doing Research. 3 ed. s.l.:Eleven International Publishing.
Womack, J., Jones, D. T. & Roos, D. (1990). The Machine That Changed the World. New
York: Simon & Schuster UK.
Womack, J. P. & Jones, D. T. (1996). Lean thinking: Banish Waste and Create Wealth In
Your Organization,. New York: Free Press.
Yin, R. K. (2009). Case Study Research: Design and Methods. 5.4 ed. s.l.:Thousand Oaks:
Sage Publications.
AAOS Master Course, June 2015
14
Silviu Iliesiu | Irina Popkov | Elina Rekil
Appendix
Interview Guide based on Stetler, et al., 2007
1. What interventions or strategic approaches are used to a) facilitate implementation at the
project level and b) create normalization of Lean within a healthcare system at multiple
institutional levels?
a. WHY (context): What was the motivation for change/s, i.e., why did targeted
departments/services and their embedded levels wish to/implement Lean?
b. WHY
(context):
What
were
the
enabling/driving
forces
and
the
restraining/hindering forces or factors, over time, to the motivation to implement
Lean
i.
Internal environment: What was the receptive capacity (i.e., key contextual
elements) to implement and sustain Lean, over time (including at the time
of the decision to initiate Lean)? E.g.,
Strong leadership (Transformational)
Clear strategic vision
Visionary staff in key positions
ii. External environment
c. HOW (process): What was the process used to create an individual change to Lean,
i.e., what was the method used to try to get Lean get implemented?
i. Which, if any, specific implementation interventions/strategies were used to
try to enable the use of an individual, targeted piece or program of Lean?
Did the processes/strategies that were used change over time?
ii. How effective were the implementation efforts?
How did you measure the process and results? (Including Lean
outcomes)
Were you able to overcome barriers and if so, how e.g., attitudes,
knowledge, lack of cooperation?
AAOS Master Course, June 2015
15
Silviu Iliesiu | Irina Popkov | Elina Rekil
iii. What were the enabling/driving factors and the restraining/hindering
factors?
d. WHAT (content): What was the content of related contextual change for targeted
Lean projects over time?
i. What in the system was changed to enhance or support the use of an
individual, targeted piece of Lean?
ii. What were the enabling/driving factors and the restraining/hindering
factors?
iii. Was successful implementation sustained?
iv. How was it sustained?
e. HOW (process): What was the process used over time to create a change to Lean as
the norm or to create routine Lean?
i. Which, if any, strategies were used to try to enable the routine use
(institutionalization) of Lean?
ii. How effective were these strategic implementation efforts, over time?
How was this assessed?
iii. What were the enabling/driving factors and the restraining/hindering
factors?
f. WHAT (content): What was the content of related contextual change for generic,
sustained Lean over time:
i. What key contextual elements or other entities in the system were changed
to enhance or support the routine use (institutionalization) of Lean?
ii. What were the enabling/driving factors and the restraining/hindering
factors?
iii. Were related goals/objectives/outcomes met?
What is/has been the degree of Lean activity (at all levels) over time,
its related success (per number of Lean outcomes); and its related
maintenance (sustainability of activity & outcomes)?
AAOS Master Course, June 2015
16
Silviu Iliesiu | Irina Popkov | Elina Rekil
iv. Was successful transformational change sustained?
How was it sustained?
AAOS Master Course, June 2015
17
Vous aimerez peut-être aussi
- Developing a Program of Research: An Essential Process for a Successful Research CareerD'EverandDeveloping a Program of Research: An Essential Process for a Successful Research CareerPas encore d'évaluation
- The Management of Chronic Diseases: Organizational Innovation and EfficiencyD'EverandThe Management of Chronic Diseases: Organizational Innovation and EfficiencyPas encore d'évaluation
- The Current State of Lean Implementation in Health Care: Literature ReviewDocument27 pagesThe Current State of Lean Implementation in Health Care: Literature ReviewGloom GomsPas encore d'évaluation
- Barriers of LeanDocument11 pagesBarriers of LeanRachanee SPas encore d'évaluation
- Improving Lean Healthcare EffectivenessDocument27 pagesImproving Lean Healthcare EffectivenessHadi P.Pas encore d'évaluation
- MQA Lab CepDocument19 pagesMQA Lab CepShaffan AbbasiPas encore d'évaluation
- Evaluating LeanDocument16 pagesEvaluating LeanKabib AbdullahPas encore d'évaluation
- Faculty Development For Educators: A Realist Evaluation: ArticleDocument18 pagesFaculty Development For Educators: A Realist Evaluation: ArticleRiry AmbarsaryPas encore d'évaluation
- QM LeanDocument2 pagesQM LeanElliePas encore d'évaluation
- Realist Synthesis: An Introduction: Ray Pawson Trisha Greenhalgh Gill Harvey Kieran WalsheDocument55 pagesRealist Synthesis: An Introduction: Ray Pawson Trisha Greenhalgh Gill Harvey Kieran WalsheDouglas SantosPas encore d'évaluation
- HealthcareDocument5 pagesHealthcaremamaadam02Pas encore d'évaluation
- Dimensions of Learning Organizations Questionnaire (DLOQ) in A Low-Resource Health Care Setting in NepalDocument8 pagesDimensions of Learning Organizations Questionnaire (DLOQ) in A Low-Resource Health Care Setting in Nepalsapit90Pas encore d'évaluation
- Lean Healthcare Literature ReviewDocument5 pagesLean Healthcare Literature Reviewea2167ra100% (1)
- Physical Therapy Tests in Stroke RehabilitationDocument22 pagesPhysical Therapy Tests in Stroke Rehabilitationmehdi.chlif4374Pas encore d'évaluation
- HospitalDocument7 pagesHospitalBENNY WAHYUDIPas encore d'évaluation
- Module 5 Self-AssessmentDocument4 pagesModule 5 Self-AssessmentJulie KiselevPas encore d'évaluation
- Trends and Lean HealtcareDocument20 pagesTrends and Lean HealtcareDwi SetiawatiPas encore d'évaluation
- The Lean Management Maturity Self-AssessDocument6 pagesThe Lean Management Maturity Self-AssessModerator HRCIPas encore d'évaluation
- ERP in Healthcare: April 2015Document11 pagesERP in Healthcare: April 2015HKS 95Pas encore d'évaluation
- Lean Dan 5S Pada Bidang Jasa (Healthcare) PDFDocument9 pagesLean Dan 5S Pada Bidang Jasa (Healthcare) PDFNisaa RahmiPas encore d'évaluation
- Using Lean Management To Leverage InnovaDocument3 pagesUsing Lean Management To Leverage InnovaFrancis ParedesPas encore d'évaluation
- The Daily Work of Lean Leaders - Lessons From Manufacturing and HealthcareDocument16 pagesThe Daily Work of Lean Leaders - Lessons From Manufacturing and HealthcareOUBAYIDIR aliPas encore d'évaluation
- Tonursj 11 108 PDFDocument16 pagesTonursj 11 108 PDFAnonymous OzgEr1FNvdPas encore d'évaluation
- Review of Related Literature and StudiesDocument30 pagesReview of Related Literature and StudiesMikha DacayananPas encore d'évaluation
- Quality Improvement ModelsDocument64 pagesQuality Improvement ModelsShahin Patowary100% (2)
- AB 1 BureaucracyDocument20 pagesAB 1 BureaucracyDanily Faith VillarPas encore d'évaluation
- Management SKILLSDocument280 pagesManagement SKILLSPulaMare201375% (4)
- 01 Koshy Et Al CH 01Document24 pages01 Koshy Et Al CH 01sandyshores492Pas encore d'évaluation
- The JBI Model of Evidence-Based Healthcare: A Model ReconsideredDocument12 pagesThe JBI Model of Evidence-Based Healthcare: A Model ReconsideredJoão AgrelosPas encore d'évaluation
- Session 5D HenrionDocument10 pagesSession 5D HenrionNCVOPas encore d'évaluation
- Application of Lean Healthcare in Hospital ServiceDocument14 pagesApplication of Lean Healthcare in Hospital ServiceRon patelPas encore d'évaluation
- Sister Blessing Project.Document41 pagesSister Blessing Project.ayanfePas encore d'évaluation
- Focus On Stage Model PoliciesDocument7 pagesFocus On Stage Model PoliciesJuzelle DiestaPas encore d'évaluation
- 01 Koshy Et Al CH 01 PDFDocument24 pages01 Koshy Et Al CH 01 PDFiamgodrajeshPas encore d'évaluation
- Change Theories in NursingDocument7 pagesChange Theories in NursingPeter Arnold Tagimacruz Tubayan100% (2)
- Determinate of Sustainability and Organizational Effectiveness inDocument14 pagesDeterminate of Sustainability and Organizational Effectiveness inYehualashet TeklemariamPas encore d'évaluation
- SECTION 3: Discussion, Conclusions and Recommendations 3.1Document30 pagesSECTION 3: Discussion, Conclusions and Recommendations 3.1John CheeversPas encore d'évaluation
- RP213Document8 pagesRP213mohamed moradPas encore d'évaluation
- 10 15405-Epsbs 2017 01 81 PDFDocument10 pages10 15405-Epsbs 2017 01 81 PDFNina KondićPas encore d'évaluation
- Integrating Evidence-Based Practice: Monica Mwaniki Aspen UniversityDocument9 pagesIntegrating Evidence-Based Practice: Monica Mwaniki Aspen Universityberrick otienoPas encore d'évaluation
- Comunity Health System Managent ManualDocument67 pagesComunity Health System Managent ManualPhilip MutuaPas encore d'évaluation
- Nestle ProjectDocument88 pagesNestle ProjectSandeep Chakkal100% (1)
- ERP in HealthcareDocument11 pagesERP in HealthcareAshik HaquePas encore d'évaluation
- 1-S2.0-S0168851015000366-Main - Lean in Healthcare A Cpmprehensive ReviewDocument13 pages1-S2.0-S0168851015000366-Main - Lean in Healthcare A Cpmprehensive ReviewRSP Universitas RiauPas encore d'évaluation
- Experience of Lean Application in Higher Education InstitutionsDocument20 pagesExperience of Lean Application in Higher Education InstitutionsIpsêêtà MängárãjPas encore d'évaluation
- My-Quyen2020 Article MindfulCo-creationOfTransforma PDFDocument25 pagesMy-Quyen2020 Article MindfulCo-creationOfTransforma PDFIgor de Castro ChieregatoPas encore d'évaluation
- Cultura OrganizationalaDocument16 pagesCultura OrganizationalaCristina IuliaPas encore d'évaluation
- 0 FrameworkDocument31 pages0 FrameworkWashington SilvaPas encore d'évaluation
- Sustaining Lean and Six Sigma Improvements in Healthcare: Results From A Pilot SurveyDocument12 pagesSustaining Lean and Six Sigma Improvements in Healthcare: Results From A Pilot SurveyRagu RajanPas encore d'évaluation
- 3586-10385-1-PB PDFDocument12 pages3586-10385-1-PB PDF'Mbem Octaviani'saiank Ndud-foreverPas encore d'évaluation
- Quality Management in Health Care: Concepts, Principles and StandardsDocument8 pagesQuality Management in Health Care: Concepts, Principles and StandardsKangen HijauPas encore d'évaluation
- Evidenced Based Nursing PracticeDocument7 pagesEvidenced Based Nursing PracticeKim ViñasPas encore d'évaluation
- 1.0 Background of The StudyDocument19 pages1.0 Background of The Studybello adetoun morePas encore d'évaluation
- The Paradox of Lean HealthcareDocument10 pagesThe Paradox of Lean HealthcarejuanitoPas encore d'évaluation
- Quality Management in Health Care: Concepts, Principles and StandardsDocument8 pagesQuality Management in Health Care: Concepts, Principles and StandardsMartin BringasPas encore d'évaluation
- Managing Healthcare OrganisationsDocument16 pagesManaging Healthcare OrganisationsSamuel Josafat Olam100% (1)
- Bereket BezabhiDocument39 pagesBereket Bezabhimubarek oumerPas encore d'évaluation
- The Lean Management Maturity Self-Assessment ToolDocument7 pagesThe Lean Management Maturity Self-Assessment Toolshekharbiswas60Pas encore d'évaluation
- 10.1108@jhom 06 2018 0176Document19 pages10.1108@jhom 06 2018 0176Karenziitah Katiuska Sosa RamirezPas encore d'évaluation
- Rec1 CPDforfacultyteachingstaffDocument12 pagesRec1 CPDforfacultyteachingstaffchiradzuluPas encore d'évaluation
- Human Factors in Surgery: Optimal Surgical Team Proficiency and Decision Making - The Bulletin of THDocument2 pagesHuman Factors in Surgery: Optimal Surgical Team Proficiency and Decision Making - The Bulletin of THJonas LeoPas encore d'évaluation
- Outcomes in Emergency General Surgery Following The Introduction of A Consultant-Led UnitDocument7 pagesOutcomes in Emergency General Surgery Following The Introduction of A Consultant-Led UnitJonas LeoPas encore d'évaluation
- Folder Ul EnglishDocument8 pagesFolder Ul EnglishJonas LeoPas encore d'évaluation
- 2 - Alvarez-Segura Et AlDocument15 pages2 - Alvarez-Segura Et AlJonas LeoPas encore d'évaluation
- 2 - Alvarez-Segura Et AlDocument15 pages2 - Alvarez-Segura Et AlJonas LeoPas encore d'évaluation
- The Dutch Health Care SystemDocument31 pagesThe Dutch Health Care SystemJonas LeoPas encore d'évaluation
- C2 - Planning A New Bed Towerlean Healthcare Facility Design 11-18-08Document44 pagesC2 - Planning A New Bed Towerlean Healthcare Facility Design 11-18-08Jonas LeoPas encore d'évaluation
- Lean Lab 2Document41 pagesLean Lab 2Jonas LeoPas encore d'évaluation
- Standardizing Operation Technic - The History of ShouldiceDocument64 pagesStandardizing Operation Technic - The History of ShouldiceJonas LeoPas encore d'évaluation
- C2 - Planning A New Bed Towerlean Healthcare Facility Design 11-18-08Document44 pagesC2 - Planning A New Bed Towerlean Healthcare Facility Design 11-18-08Jonas LeoPas encore d'évaluation
- Do Not Build A New Hospital in The Rear View MirrorDocument31 pagesDo Not Build A New Hospital in The Rear View MirrorJonas LeoPas encore d'évaluation
- C2 - Planning A New Bed Towerlean Healthcare Facility Design 11-18-08Document44 pagesC2 - Planning A New Bed Towerlean Healthcare Facility Design 11-18-08Jonas LeoPas encore d'évaluation
- Lean AccountingDocument16 pagesLean AccountingJonas LeoPas encore d'évaluation
- NHFLT Plenary TannerDocument18 pagesNHFLT Plenary TannerJonas LeoPas encore d'évaluation
- Daniels & SabinDocument15 pagesDaniels & SabinJonas LeoPas encore d'évaluation
- NHFLT Plenary WomackDocument14 pagesNHFLT Plenary WomackJonas LeoPas encore d'évaluation
- Redisigning Healthcare-Ben Tovim Flinders Adelaide AustralienDocument24 pagesRedisigning Healthcare-Ben Tovim Flinders Adelaide AustralienJonas LeoPas encore d'évaluation
- Paper Lean For LeadersDocument15 pagesPaper Lean For LeadersJonas LeoPas encore d'évaluation
- Cystic Fibrosis Action GuideDocument42 pagesCystic Fibrosis Action GuideJonas LeoPas encore d'évaluation
- Cordial Lean Study 2008 FinalDocument44 pagesCordial Lean Study 2008 FinalJonas LeoPas encore d'évaluation
- Batalden What Is Quality Improvement QSHC 2007Document3 pagesBatalden What Is Quality Improvement QSHC 2007Jonas LeoPas encore d'évaluation
- Open Cholecystectomy For All Patients in The Era of Laparoscopic Surgery-A Prospective Cohort StudyDocument6 pagesOpen Cholecystectomy For All Patients in The Era of Laparoscopic Surgery-A Prospective Cohort StudyJonas LeoPas encore d'évaluation
- George Orwell: Emotional QuotesDocument4 pagesGeorge Orwell: Emotional QuotesIrem YitmenPas encore d'évaluation
- The Philosophy of Ludwig WittgensteinDocument13 pagesThe Philosophy of Ludwig WittgensteinLuis MendezPas encore d'évaluation
- Review of Richard D. Lewis When Cultures Collide - Managing SucceDocument3 pagesReview of Richard D. Lewis When Cultures Collide - Managing SucceArhant PathardePas encore d'évaluation
- D E Harding ThesisDocument208 pagesD E Harding Thesismike100% (1)
- Existentialism and Education PDFDocument2 pagesExistentialism and Education PDFRickyPas encore d'évaluation
- Enclosure 4. Teacher-Made Learner's Home Task: 7MT-Ia-1Document3 pagesEnclosure 4. Teacher-Made Learner's Home Task: 7MT-Ia-1Carissa Mae Cañete0% (1)
- Pci Playbook IssipDocument27 pagesPci Playbook Issipsam cadanPas encore d'évaluation
- Marzano's Nine Essential Instructional StrategiesDocument2 pagesMarzano's Nine Essential Instructional StrategiesmicksoulPas encore d'évaluation
- Concept PaperDocument3 pagesConcept PaperDan Reynald Domingo SomeraPas encore d'évaluation
- Introduction To PhilosophyDocument12 pagesIntroduction To PhilosophyFria mae AbellanoPas encore d'évaluation
- Strategies and Models For Teachers - Teaching Content Andng Skills (6th Edition) - Paul D. Eggen - Don P. Kauchak PDFDocument17 pagesStrategies and Models For Teachers - Teaching Content Andng Skills (6th Edition) - Paul D. Eggen - Don P. Kauchak PDFFahri muhammad33% (3)
- Philosophical Theoretical Ground Mathematics TeachingDocument58 pagesPhilosophical Theoretical Ground Mathematics TeachingWidi Toss Muda PurwodadiPas encore d'évaluation
- Charming Intentions: Occultism, Magic and The History of ArtDocument2 pagesCharming Intentions: Occultism, Magic and The History of ArtcaptainfreakoutPas encore d'évaluation
- Introduction To Human Computer InteractionDocument16 pagesIntroduction To Human Computer InteractionDumbo YanPas encore d'évaluation
- Ca Kel 3Document14 pagesCa Kel 3esteria veronika panjaitanPas encore d'évaluation
- Husserl S Epoche and Phenomenological deDocument5 pagesHusserl S Epoche and Phenomenological deJohn O'sheaPas encore d'évaluation
- Lesson Plan Ma Famille 1110Document2 pagesLesson Plan Ma Famille 1110MonaPas encore d'évaluation
- L Aaaaaaaaaaaaaaaaaaaaaaaaaa Aaaaaaaaaaaaaaaaaaaaaaaaaa STDocument6 pagesL Aaaaaaaaaaaaaaaaaaaaaaaaaa Aaaaaaaaaaaaaaaaaaaaaaaaaa STM Noaman AkbarPas encore d'évaluation
- Science Is Not Value-Free: Archie J. B A H MDocument6 pagesScience Is Not Value-Free: Archie J. B A H MMade DeddyPas encore d'évaluation
- Public Speaking Sample Preparation FormatDocument7 pagesPublic Speaking Sample Preparation FormatRitz AiniePas encore d'évaluation
- 1915 Fabre Dolivet Hermeneutic InterpretationDocument613 pages1915 Fabre Dolivet Hermeneutic InterpretationRaphael Bahamonde Cobo de FigueroaPas encore d'évaluation
- 01.3 The Research ProcessDocument21 pages01.3 The Research ProcessSamaki AlsatPas encore d'évaluation
- Fostering Goodness & CaringDocument13 pagesFostering Goodness & CaringasmawiPas encore d'évaluation
- Learning Style InventoryDocument4 pagesLearning Style Inventoryapi-317891089Pas encore d'évaluation
- Motivation and EmotionDocument15 pagesMotivation and EmotionAasma IsmailPas encore d'évaluation
- Hofstadter and McGraw (1993) - Letter Spirit - An Emergent Model of The Perception and Creation of Alphabetic StyleDocument29 pagesHofstadter and McGraw (1993) - Letter Spirit - An Emergent Model of The Perception and Creation of Alphabetic Styleappled.apPas encore d'évaluation
- Psychology of Bilingualism The Cognitive and Emotional World of Bilinguals by Alfredo Ardila, Anna B. Cieślicka, Roberto R. Heredia, Mónica RoselliDocument318 pagesPsychology of Bilingualism The Cognitive and Emotional World of Bilinguals by Alfredo Ardila, Anna B. Cieślicka, Roberto R. Heredia, Mónica RoselliAlessandra Ale100% (1)
- The Elusive Cultural ChameleonDocument17 pagesThe Elusive Cultural ChameleonVikasPas encore d'évaluation
- In Defense of Pure ReasonDocument246 pagesIn Defense of Pure ReasonJacob Sparks100% (1)
- WORKSHOP 2 DLL - 4th QRTR - Week 1.docx Institutional OutcomesDocument8 pagesWORKSHOP 2 DLL - 4th QRTR - Week 1.docx Institutional OutcomesShalom FoxtrotPas encore d'évaluation