Académique Documents
Professionnel Documents
Culture Documents
Disturbances in Colonic Physiology
Transféré par
غسن سمن المدنCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Disturbances in Colonic Physiology
Transféré par
غسن سمن المدنDroits d'auteur :
Formats disponibles
Disturbances in Colonic Physiology
Physiology of Constipation
Constipation refers to stools that are infrequent or hard to pass (or both). Arbitrary
definitions have been used. Individuals with constipation are an incredibly
heterogeneous group. Distinct subtypes of constipation occur and require different
treatment modalities, but even within these subtypes there can be wide variability
in the clinical presentation and pathophys- iologic etiology. There may be dietary,
pharmacologic, sys- temic, or local causes. Many people have constipation caused
by dietary and lifestyle neglect. Two primary functions of the colon, solidifying
chyme into stool and laxation, are interde- pendent on adequate dietary fiber.
Dietary fiber normalizes large bowel function.77,78 Recommendations for
adequate fiber intake ranges from 20 to 35 g per day for adults.79 Fiber is generally soluble or insoluble and seems to improve stool weight by different
mechanisms. Oat bran, which is soluble, seems to increase stool weight by
providing rapidly fermenting soluble fiber to the proximal colon. This allows for
bacterial growth which is sustained until excretion. It seems that the increase in
stool mass is from higher bacterial content and increased excretion of lipid and
fat.80 Insoluble fiber such as wheat bran increases stool weight by increasing
dietary fiber (undigested plant material) in the stool. Wheat bran also increases fat
excretion, but not to the extent of oat bran.80 Interestingly, fiber intake in the
United States is low. One explanation is that to achieve 15 g of fiber intake daily, 11
servings of refined grains and 5 servings of fruit and vegetables are needed for
individu- als consuming 15002000 kcal daily.77 Additionally, constipation may be
seen more frequently in sedentary people. In fact, abdominal cramps and diarrhea
are reported more frequently in runners.81,82 Acute graded exer- cise has been
shown to actually decrease phasic colonic motor activity. However, after the
exercise, there was an increase in the number and amplitude of propagated
pressure waves. It is believed that this post-exercise pattern may increase the propagating activity and propel stool.43 Idiopathic slow transit constipation involves a
measurable delayed movement of material through the colon. These patients are
not helped (in fact may be made worse) with increased dietary fiber. They seem to
have altered colonic motor response to eating and impaired or decreased HAPCs of
the colon.50,64 This leads to reduced or absent colonic propulsive activity.83,84
Abnormalities in the neuronal network are suspected and recently a pan-colonic
decrease in the ICC has been shown.56 As with other areas of colonic study, this
one also needs much more investigation.
Irritable bowel syndrome (IBS) can manifest with multiple forms. It usually is
characterized as altered bowel habits and pain directly related to the altered bowel
habits. In one form, constipation can be the predominant feature. This may encompass about 30% of the IBS population and traditionally over- whelmingly affects
women. This group of patients can show an overlap with those having slow transit
constipation, but may have a normal transit study.85 Pharmaceutical companies
have targeted drugs that affect metabolism of serotonin, which seems to be
involved in the regulation of motility, sensitivity, and intestinal secretions. The
specific 5-hydroxytryptamine (5-HT)4 receptor is involved in intrinsic sensory
reflexes within the gut. Tegaserod is a 5-HT486 agonist that has been approved by
the Food and Drug Administration (FDA) (July 2002) for treatment of this group of
patients.87 Additionally, cholecystokinin-1 antagonists are in trials for treatment of
patients with constipation-predominant IBS.87
Obstructed Defecation
Obstructed defecation usually results from abnormalities in pelvic function versus
colonic function. Typically this prob- lem is associated with failure of the puborectalis
to relax with defecation, rectocele, perineal descent, or other pelvic- and rectalassociated issues. Failure of the rectum to evacuate may lead to marker studies
which also show marker collection in the left colon.88 This may also be associated
with colonic total inertia.89 A colonic source, which is a variant in obstructed
defeca- tion, is a sigmoidocele. Although rare, the sigmoid is seen to migrate into
the pelvis with defecation and obstruct evacua- tion of stool. This form can be
relieved and treated with a sig- moid resection, but the clinician should be aware of
other pelvic floor abnormalities.
Ogilvies Syndrome
Ogilvies syndrome was described initially in 1948. It is also known as acute colonic
pseudoobstruction. The pathophysiol- ogy is not clearly understood. Based on
evidence from phar- macologic studies, it seems that Ogilvies original hypothesis is
as correct as the current facts; namely, there seems to be an imbalance of
autonomic innervation to the gut. The parasym- pathetic nerves, which are
responsible for stimulating gut motility, have decreased function or input and the
sympathetic nerves, which are inhibitory, increase their input.90 Because of the law
of Laplace, the cecum can be the site of extreme dilata- tion (it requires the
smallest amount of pressure to increase in size and therefore increase the wall
tension). Treatment has focused on ruling out a distal obstruction with a
Gastrografin enema and if needed colonoscopic decompression. However,
pharmacologic treatment with neostigmine has been success- ful.91 This drug is a
cholinesterase inhibitor that allows more available acetylcholine for
neurotransmission in the parasym- pathetic system (excitatory) to promote
contractility.92
28 T.L. Hull
Irritable Bowel Syndrome
As stated above, IBS is characterized by altered bowel habits associated with pain.
Besides the constipation-predominant type described above, there can be a
diarrhea-predominant type and a mixed type. The pathophysiology of IBS has
received extensive study, but it remains unclear. Abnormal motility, visceral
hypersensitivity, inflammation, abnormali- ties in extrinsic autonomic innervation,
abnormal braingut interaction, and the role of psychosocial factors have been
investigated. If IBS is found in men it tends to be more diar- rhea-predominant type.
Treatment is based on the nature and severity of symptoms. Education,
reassurance, and dietary modification (elimination of foods that aggravate the problem) are the first steps. For those who do not respond, med- ication is considered.
Antispasmodics (anticholinergic) medication is considered for those with pain and
bloating that is especially aggravated by meals. Usually, antispasmodics and
anticholinergic agents are considered on an as-needed basis. Low-dose tricyclic
antidepressants may be considered when the pain is more constant and perhaps
disabling.86 Considering specific types, no good pharmacologic research is available
for the mixed-type IBS patients. However, for the diarrhea prone, 5-HT3 antagonists
have been found to be effective. Alosetron was initially FDA approved (March 2000)
only to be withdrawn after some patients suffered ischemic colitis and even
death.87 In June 2002, it was reapproved with restrictions that require the prescriber to demonstrate educational understanding regarding the drug. Additional
drugs are also undergoing trials.
Vous aimerez peut-être aussi
- CMB5Document2 pagesCMB5غسن سمن المدنPas encore d'évaluation
- CMB3Document3 pagesCMB3غسن سمن المدنPas encore d'évaluation
- CMB1Document1 pageCMB1غسن سمن المدنPas encore d'évaluation
- Acanthamoeba In-WPS OfficeDocument4 pagesAcanthamoeba In-WPS Officeغسن سمن المدنPas encore d'évaluation
- Antiplatelet THDocument3 pagesAntiplatelet THغسن سمن المدنPas encore d'évaluation
- CMB4Document2 pagesCMB4غسن سمن المدنPas encore d'évaluation
- CMB2Document1 pageCMB2غسن سمن المدنPas encore d'évaluation
- Abdominal AorticDocument6 pagesAbdominal Aorticغسن سمن المدنPas encore d'évaluation
- Dan M. Roden-WPS OfficeDocument1 pageDan M. Roden-WPS Officeغسن سمن المدنPas encore d'évaluation
- AchalasiaDocument4 pagesAchalasiaغسن سمن المدنPas encore d'évaluation
- AbortionDocument3 pagesAbortionغسن سمن المدنPas encore d'évaluation
- Acanthamoeba In-WPS OfficeDocument4 pagesAcanthamoeba In-WPS Officeغسن سمن المدنPas encore d'évaluation
- Recognizing A Pleural EffusionDocument1 pageRecognizing A Pleural Effusionغسن سمن المدنPas encore d'évaluation
- Lung CollapseDocument1 pageLung Collapseغسن سمن المدنPas encore d'évaluation
- Emergency Tintin-WPS OfficeDocument1 pageEmergency Tintin-WPS Officeغسن سمن المدنPas encore d'évaluation
- 17Document2 pages17غسن سمن المدنPas encore d'évaluation
- Not Seen in This Patient Include:: DiscussionDocument1 pageNot Seen in This Patient Include:: Discussionغسن سمن المدنPas encore d'évaluation
- Discussion: Pneumonia (Fig. 1a)Document1 pageDiscussion: Pneumonia (Fig. 1a)غسن سمن المدنPas encore d'évaluation
- Short Incubation PeriodDocument1 pageShort Incubation Periodغسن سمن المدنPas encore d'évaluation
- Laminar EffusionsDocument1 pageLaminar Effusionsغسن سمن المدنPas encore d'évaluation
- Types of AtelectasisDocument1 pageTypes of Atelectasisغسن سمن المدنPas encore d'évaluation
- Imaging of The Breast Is Undertaken As Part of A ComprehensiveDocument1 pageImaging of The Breast Is Undertaken As Part of A Comprehensiveغسن سمن المدنPas encore d'évaluation
- Recognize Partial or Complete Atelectasis of The Following On A Chest Radiograph or Computed TomographyDocument1 pageRecognize Partial or Complete Atelectasis of The Following On A Chest Radiograph or Computed Tomographyغسن سمن المدنPas encore d'évaluation
- The Primary Features of Established Illness Are Related To EndothelialDocument1 pageThe Primary Features of Established Illness Are Related To Endothelialغسن سمن المدنPas encore d'évaluation
- Learning ObjectivesDocument1 pageLearning Objectivesغسن سمن المدنPas encore d'évaluation
- The Development of The 12Document1 pageThe Development of The 12غسن سمن المدنPas encore d'évaluation
- Anatomy of Lung Lobes and FissuresDocument1 pageAnatomy of Lung Lobes and Fissuresغسن سمن المدنPas encore d'évaluation
- Isolated Heart MuscleDocument1 pageIsolated Heart Muscleغسن سمن المدنPas encore d'évaluation
- A Class I Incisor Relationship Is Defined by The British Standards Incisor Classification As FollowsDocument2 pagesA Class I Incisor Relationship Is Defined by The British Standards Incisor Classification As Followsغسن سمن المدنPas encore d'évaluation
- Anticoagulant andDocument2 pagesAnticoagulant andغسن سمن المدنPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- 2925 Ferose F 1415097720Document2 pages2925 Ferose F 1415097720iqbalmedicoPas encore d'évaluation
- Shnider and Levinsons Anesthesia For Obstetrics, 5th EdDocument879 pagesShnider and Levinsons Anesthesia For Obstetrics, 5th EdSri Hari50% (2)
- Major Incidents and Mass Casualty EventsDocument99 pagesMajor Incidents and Mass Casualty EventsJose Damian Cortes FernandezPas encore d'évaluation
- CH13 Ninenth Standard NCERT BOOKDocument26 pagesCH13 Ninenth Standard NCERT BOOKPrash ShanthPas encore d'évaluation
- Balanopostitis and Penyle Edema Atypical Manifestation of Primary SipilisDocument2 pagesBalanopostitis and Penyle Edema Atypical Manifestation of Primary SipilisTeja LaksanaPas encore d'évaluation
- Cek List Mini ICUDocument4 pagesCek List Mini ICUmichelle chiajungPas encore d'évaluation
- Nursing Care StudyDocument20 pagesNursing Care StudyAnjaliPas encore d'évaluation
- Common Oral Lesions: Aphthous Ulceration, Geographic Tongue, Herpetic GingivostomatitisDocument13 pagesCommon Oral Lesions: Aphthous Ulceration, Geographic Tongue, Herpetic GingivostomatitisFaridaFoulyPas encore d'évaluation
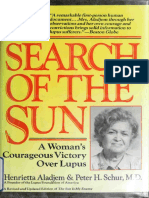
- Aladjem - The Sun Is My Enemy - in Search of The Sun - A Woman's Courageou - Aladjem, Henrietta, 1917 (Orthomolecular Medicine)Document310 pagesAladjem - The Sun Is My Enemy - in Search of The Sun - A Woman's Courageou - Aladjem, Henrietta, 1917 (Orthomolecular Medicine)Anonymous gwFqQcnaX100% (1)
- Pictotrans: Pathology of The Breast Quiz From Dra. Edna May Lasap-GoDocument32 pagesPictotrans: Pathology of The Breast Quiz From Dra. Edna May Lasap-Go2012Pas encore d'évaluation
- Stress-Related Mucosal Disease: Mitchell J. Spirt, MDDocument11 pagesStress-Related Mucosal Disease: Mitchell J. Spirt, MDnur hidayatPas encore d'évaluation
- Epilepsy Sa 1Document33 pagesEpilepsy Sa 1Kishan GoyaniPas encore d'évaluation
- Advocacy PaperDocument3 pagesAdvocacy Paperapi-478583234Pas encore d'évaluation
- Indonesia Ophthalmologic Anesthesia Society (IOAS) : Susunan Acara Pertemuan Ilmiah Tahunan Ke - 4 16 - 17 Juli 2022Document4 pagesIndonesia Ophthalmologic Anesthesia Society (IOAS) : Susunan Acara Pertemuan Ilmiah Tahunan Ke - 4 16 - 17 Juli 2022ruthameliapPas encore d'évaluation
- Prisma 2021Document10 pagesPrisma 2021Quispe RoyPas encore d'évaluation
- Covid 19 Open LetterDocument5 pagesCovid 19 Open LetterKOLD News 13Pas encore d'évaluation
- Safe syringe pump practice for patient careDocument3 pagesSafe syringe pump practice for patient careDian NoveraPas encore d'évaluation
- Question 1Document25 pagesQuestion 1Anonymous 1T0qSzPt1PPas encore d'évaluation
- Nama: Stevany Ayuningsi Aduga Nim: 150600 Kelas: Keperawatan B Questioning To Fill in Pain Assessment Form ObjectivesDocument8 pagesNama: Stevany Ayuningsi Aduga Nim: 150600 Kelas: Keperawatan B Questioning To Fill in Pain Assessment Form ObjectivesAnathasya SalamatPas encore d'évaluation
- 142 DefinitionsssDocument7 pages142 DefinitionsssAnonymous vXPYrefjGLPas encore d'évaluation
- Usp 38 Alt AkkDocument3 pagesUsp 38 Alt Akkkhoirunnissa hidayatiPas encore d'évaluation
- Prescription AnalysisDocument16 pagesPrescription AnalysisMohd Azfar HafizPas encore d'évaluation
- Certificate of DeathDocument2 pagesCertificate of DeathAlfie Omega100% (2)
- Pediatrics QuestionsDocument22 pagesPediatrics QuestionsShaik AmreenPas encore d'évaluation
- Why Advocate Re RedcopDocument34 pagesWhy Advocate Re RedcopnichiichaiiPas encore d'évaluation
- Unit 2 Mental Health AssessmentDocument60 pagesUnit 2 Mental Health AssessmentSuhana ShresthaPas encore d'évaluation
- Obstetric Nursing Study GuideDocument69 pagesObstetric Nursing Study GuideValerie100% (3)
- The Comorbidities of Dysmenorrhea: A Clinical Survey Comparing Symptom Profile in Women With and Without EndometriosisDocument14 pagesThe Comorbidities of Dysmenorrhea: A Clinical Survey Comparing Symptom Profile in Women With and Without EndometriosisSeptian WidiantoPas encore d'évaluation
- Tricorder X PrizeDocument4 pagesTricorder X PrizemariaPas encore d'évaluation
- Severe Cutaneous Adverse Drug ReactionDocument87 pagesSevere Cutaneous Adverse Drug ReactionEpi PanjaitanPas encore d'évaluation