Académique Documents
Professionnel Documents
Culture Documents
MUC5B Levels in Submandibular Gland Saliva of Patients Treated With Radiotherapy For Head-And-Neck Cancer: A Pilot Study
Transféré par
Dexter BluesTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
MUC5B Levels in Submandibular Gland Saliva of Patients Treated With Radiotherapy For Head-And-Neck Cancer: A Pilot Study
Transféré par
Dexter BluesDroits d'auteur :
Formats disponibles
Dijkema et al.
Radiation Oncology 2012, 7:91
http://www.ro-journal.com/content/7/1/91
SHORT REPORT
Open Access
MUC5B levels in submandibular gland saliva of
patients treated with radiotherapy for head-andneck cancer: A pilot study
Tim Dijkema1*, Chris H J Terhaard1, Judith M Roesink1, Cornelis P J Raaijmakers1, Petra A M van den Keijbus2,
Henk S Brand2 and Enno C I Veerman2
Abstract
Background: The salivary mucin MUC5B, present in (sero)mucous secretions including submandibular gland (SMG)
saliva, plays an important role in the lubrication of the oral mucosa and is thought to be related to the feeling of
dry mouth. We investigated if MUC5B levels in SMG saliva could distinguish between the presence or absence of
severe dry mouth complaints 12 months after radiotherapy (RT) for head-and-neck cancer (HNC).
Findings: Twenty-nine HNC patients with a residual stimulated SMG secretion rate of 0.2 ml/10 min at 12 months
after RT were analyzed. MUC5B (in U; normalized to 1) and total protein levels (mg/ml) were measured in SMG saliva at
baseline and 12 months after RT using ELISA and BCA protein assay, respectively. Overall, median MUC5B levels
decreased after RT from 0.12 to 0.03 U (p = 0.47). Patients were dichotomized into none/mild xerostomia (n = 12) and
severe xerostomia (n = 17) based on a questionnaire completed at 12 months. SMG and whole saliva flow rates
decreased after RT but were comparable in both groups. The median MUC5B level was higher in patients with no or
mild xerostomia compared to patients with severe xerostomia (0.14 vs 0.01 U, p = 0.22). Half of the patients with severe
xerostomia had no detectable MUC5B at 12 months after RT. No differences in total protein levels were observed.
Conclusions: Qualitative saliva parameters like MUC5B need further investigation in RT-induced xerostomia. This pilot
study showed a trend towards lower MUC5B levels in the SMG saliva of patients with severe xerostomia 12 months
after RT for HNC.
Keywords: Xerostomia, Head-and-neck cancer, Radiotherapy, MUC5B, Mucin, Submandibular gland
Findings
Background
Xerostomia after radiotherapy (RT) for head-and-neck
cancer (HNC) has a major impact on quality of life in
HNC survivors [1,2]. Sparing of the parotid glands (PG)
using intensity-modulated radiotherapy (IMRT) significantly improves parotid gland function in patients treated for HNC [3,4]. In some studies however, the use of
parotid gland-sparing RT alone did not improve patientreported xerostomia [4,5]. Probably the submandibular,
sublingual and minor salivary glands play an important
role in the subjective sense of moisture in between meals
[6]. They secrete glycoproteins (mucins) that cover and
* Correspondence: T. Dijkema@umcutrecht.nl
1
Department of Radiotherapy, University Medical Center Utrecht, hp Q00.118,
Heidelberglaan 100, 3584, CX, Utrecht, The Netherlands
Full list of author information is available at the end of the article
protect the underlying mucosa (MUC5B and MUC7).
The larger salivary mucin MUC5B, present in (sero)mucous secretions including submandibular gland (SMG)
saliva, is thought to be related to the perception of dry
mouth by retaining moisture in the mucosa [7,8].
Our hypothesis in this pilot study was that MUC5B
levels, as a qualitative parameter in human saliva, could
better explain xerostomia compared to quantitative saliva measurements in RT patients. For that purpose, we
investigated if MUC5B levels in SMG saliva could distinguish between the presence or absence of severe dry
mouth complaints 12 months after RT for HNC.
Patients
Twenty-nine patients were selected from a larger population, included in prospective studies on salivary gland
2012 Dijkema et al.; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative
Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and
reproduction in any medium, provided the original work is properly cited.
Dijkema et al. Radiation Oncology 2012, 7:91
http://www.ro-journal.com/content/7/1/91
function after RT for HNC at our department [9,10].
The selected patients all had a residual stimulated SMG
secretion rate of 0.2 ml/10 min at 12 months after RT.
The amount of 0.2 ml is the threshold for MUC5B analysis in saliva.
Page 2 of 4
during the day and/or the night at 12 months were
grouped together. Patients with no or mild complaints
(grade 1-3) during day- and nighttime were also grouped
together in the analyses.
Statistical analysis
Saliva flow measurements
Techniques that were used for objective saliva measurements have been described previously [3,9]. Stimulated
salivary flow rates were measured before treatment and
at one year after RT. Citric acid solution (5%) was applied on the anterior part of the tongue every 60 seconds, for 10 minutes. Saliva near Whartons duct orifices
in the floor of the mouth was collected by gentle suction
with a micropipette, representing predominantly SMG
saliva but also varying amounts from the sublingual
glands (SLG). Stimulated PG saliva was collected separately using Lashley cups. After collection, saliva samples
were stored at -20 C until analysis.
Saliva protein assays
MUC5B levels in the SMG saliva samples were determined by an enzyme-linked immunosorbent assay
(ELISA) as described previously [11,12]. The monoclonal
antibody F2 used for quantification of MUC5B specifically recognises the terminal part of the carbohydrate
moiety, sulfo-Lewisa SO3-3Gal_1-3GlcNAc. This structure is present on MUC5B secreted by the SMGs, SLGs
and palatal (minor) salivary glands. MUC5B was quantified by comparison to unstimulated whole saliva from a
pooled sample of 10 healthy staff members of a dental
faculty with optimal oral health. Each study patient was
compared to the pooled sample of these healthy volunteers. MUC5B levels were expressed in relative units,
with the MUC5B concentration in the pooled saliva of
healthy volunteers normalized to 1. 1 Unit is approximately 230 g/ml [13].
The total protein content (mg/ml) was measured in
SMG saliva using the BCA Protein Assay Reagent
(Pierce, Rockford, IL, USA) with bovine serum albumin
(BSA) as a standard.
Assessment of patient-reported xerostomia
All patients completed a xerostomia questionnaire (XQ)
before RT and 12 months after RT. The XQ contains
questions related to xerostomia and is scored on a 5point Likert scale. A score of 1 means no complaints,
while a score of 5 implies complaints are always
present. In this analysis, we utilized two questions
addressing the sensation of dry mouth during daytime
(Do you have a dry mouth during the day) and nighttime (Do you have a dry mouth at night). Xerostomia
was dichotomized into severe (grade 4-5) or none-tomild (grade 1-3). Patients who had grade 4-5 xerostomia
Patient characteristics and MUC5B/protein levels were
reported using descriptive statistics (median, ranges or
proportions; where appropriate). Correlations were calculated using Pearsons correlation coefficient (r). Paired
samples obtained before and after RT were compared
using Wilcoxon signed ranks test. Subgroup differences
in saliva flow rate, MUC5B and protein levels were analyzed using the MannWhitney U test. Fishers Exact
test was used to compare proportions within cross tabulations. All analyses were performed using SPSS version
16 (SPSS Inc, Chicago, IL, USA). A p value of <0.05 was
considered statistically significant.
Results
The 29 patients included in this pilot study had a mean
age of 58 years (range 35-82 yr) and 22 (76%) were male.
All patients had a squamous cell carcinoma of the head
and neck, with 19 oropharyngeal tumors (66%), 6 laryngeal (21%), 3 nasopharynx (10%) and 1 oral cavity (3%).
IMRT was used in 21 (72%) patients, the remainder was
treated with conventional (2D) techniques [9]. The mean
dose to the SMGs was 55.9 Gy (range 10.6-71.1 Gy).
Overall, the median MUC5B level decreased after RT
from 0.12 U to 0.03 U (p = 0.47). MUC5B levels at
12 months showed a very weak correlation with the
mean SMG dose in Gy (Pearson r = 0.18). The median
total protein content of SMG saliva decreased slightly
after treatment (1.00 and 0.82 mg/ml respectively,
p = 0.62).
Twelve months after RT, 17 patients had severe complaints of dry mouth at day- and/or nighttime, 12
patients had no or mild complaints. The SMG and whole
saliva (PG + SMG) flow rates decreased after RT but were
comparable in both groups at 12 months (Table 1).
No statistical differences were found in the baseline
MUC5B levels between the groups (median 0.12 versus
0.14 U for the group with and without severe xerostomia, respectively) nor in the change from baseline in
each individual patient (calculated as MUC5B: median
0.04 versus 0.11 U respectively, p = 0.9). MUC5B
showed a small negative correlation with the SMG mean
dose in Gy (Pearson r = -0.26).
At 12 months, the median MUC5B was higher in
patients with no or mild xerostomia compared to
patients with severe complaints, although the difference
was not statistically different at the 0.05 level (Table 1).
The group with severe complaints was characterized
mainly by undetectable MUC5B levels and a number of
Dijkema et al. Radiation Oncology 2012, 7:91
http://www.ro-journal.com/content/7/1/91
Page 3 of 4
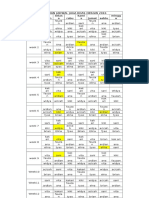
Table 1 Median saliva flow rates, MUC5B and total protein levels 12 months after RT in patients with and without
severe xerostomia during daytime and/or nighttime
No/mild xerostomia
Severe xerostomia
(n = 12)
(n = 17)
0.69
0.80
SMG flow rate
ml/10 min
WS flow rate (PG + SMG)
ml/10 min
3.35
2.80
0.82
0.14
0.01
0.22
MUC5B concentration
Undetectable MUC5B *
MUC5B x flow rate
Total protein
0.66
25
47
0.27
g/10 min
15.0
1.3
0.37
mg/ml
0.87
0.82
0.76
Abbreviations: SMG = submandibular gland, WS = whole saliva, PG = parotid gland, U = units; normalized to 1 for unstimulated saliva in healthy controls.
* MUC5B level in SMG saliva equal to 0.00 U at 12 months after RT.
The MUC5B x flow rate product (in g/10 min) was calculated by multiplying the MUC5B concentration (in U) and SMG flow rate (in ml/10 min) for each patient
at 12 months after RT and assuming 1 Unit is 230 g/ml of MUC5B [13].
outliers (Figure 1). Two of the outliers represented a 14and 123-fold increase in the MUC5B concentration from
baseline. Repeating the analyses without these two
extremes showed a borderline significant higher MUC5B
level in the patients with no or mild xerostomia (median
0.14 vs 0.00 U, p = 0.055) at 12 months.
When we combined the qualitative (MUC5B in U) and
quantitative (SMG flow rate in ml/10 min) measurements for each individual patient by multiplying both
parameters (MUC5B x flow rate; Table 1) and assumed 1
Unit is 230 g/ml of MUC5B [13], we found an approximate 10-fold lower value (in g/10 min) in the group of
patients with severe complaints of dry mouth, although
statistical difference was not reached in this small study.
The median total protein content in SMG saliva after
12 months was similar in both groups.
Discussion
This pilot study did not show a statistically significant
difference in MUC5B levels in SMG saliva of patients
MUC5B levels in relation to xerostomia
5
MUC5B (U)
4
2
0
no / mild
severe
Xerostomia
Figure 1 Comparison of MUC5B levels (in U) in patients with
and without severe xerostomia 12 months after RT, measured
using ELISA. The horizontal line represents the median for each
group.
with and without severe xerostomia 12 months after RT,
although a trend was observed towards higher MUC5B
levels in patients with fewer complaints of dry mouth.
Almost half of the patients with severe xerostomia had
no detectable MUC5B at 12 months after RT. The
results are therefore of interest and do need investigation within a larger cohort of patients. An ongoing prospective study at our department, investigating the effect
of sparing the contralateral SMG on xerostomia after
RT, is expected to yield more SMG saliva samples for future qualitative analyses [10].
As both subgroups in this study had comparable
amounts of saliva but differed in the severity of their
complaints, a case is made for qualitative saliva parameters rather than quantitative measurements in xerostomia research. The high-molecular weight salivary
mucin MUC5B contains large carbohydrate groups that
are heterogeneous and include sulfated and sialylated
oligosaccharides, retaining large amounts of water. The
unique rheological properties of MUC5B contribute to
the formation of a thin salivary film and the resulting demulcent coat is thought to hydrate and lubricate the soft
tissues of the mouth [14]. Serous acinar cells found in
the parotid glands do not produce mucins. The latter
may explain why, in RT for head-and-neck cancer, sparing of the parotid glands alone does not seem to improve patient-reported xerostomia [4].
Apart from the free MUC5B fraction measured in
SMG saliva in this study, there may be other mucinrelated factors that can explain xerostomia. First, in
stead of the free fraction, the amount of mucosa-bound
MUC5B may better explain which patients will complain
of a dry mouth. Pramanik et al. showed, that in (nonRT) dry mouth patients unable to provide a measurable
unstimulated saliva sample (zero flow), MUC5B was
often still present on all mucosal surfaces [15]. Therefore, mucins retained on the mucosa of dry mouth
patients are presumably less hydrated than in normal
subjects. In this regard, post-translational modifications
Dijkema et al. Radiation Oncology 2012, 7:91
http://www.ro-journal.com/content/7/1/91
of MUC5B synthesis and in particular sulfation levels
(rather than mucin levels per se) could result in a
reduced water content of mucins and explain the dry
mouth sensation. Loss of MUC5B sulfation was observed
in the mucous acini from labial salivary glands of
patients with Sjgren syndrome and was unrelated to
alterations in saliva quantity [7]. To what extent these
findings can be extrapolated to patients with
radiotherapy-induced xerostomia needs to be investigated. Third, differently glycosylated MUC5B species are
present in saliva. In single glandular secretions and even
in one secretory acinus different glycoforms are
expressed, pointing to a large heterogeneity in mucin
molecules [16]. Moreover, MUC5B from different glandular sources have different rheological properties that
may influence fluid retention on mucosal surfaces [17].
In this study, a specific (sulfo)glycolysation motif (sulfoLewisa) was detected, present on MUC5B secreted by the
SMGs, SLGs and palatal minor glands. Possibly, (absence
of ) other MUC5B glycoforms can better explain why
some patients with recovering SMG secretion after RT
complain of a dry mouth and others do not.
Competing interests
The authors declare that they have no competing interests.
Authors contributions
TD participated in the design of the study, performed data collection,
statistical analysis and drafted the manuscript. CT, JR and NR participated in
the design and coordination of the study and data collection. PvdK carried
out the immunoassays and protein analyses. HB and EV participated in the
design of the study and interpretation of the data, HB also assisted with the
statistical analysis. All authors read and approved the final manuscript.
Acknowledgements
This research was supported by the Dutch Cancer Society
(Grant UU 2006-3573).
Author details
1
Department of Radiotherapy, University Medical Center Utrecht, hp Q00.118,
Heidelberglaan 100, 3584, CX, Utrecht, The Netherlands. 2Section of Oral
Biochemistry, Academic Centre for Dentistry Amsterdam (ACTA), Amsterdam,
The Netherlands.
Received: 28 February 2012 Accepted: 5 June 2012
Published: 15 June 2012
References
1. Langendijk JA, Doornaert P, Verdonck-de Leeuw IM, Leemans CR,
Aaronson NK, Slotman BJ: Impact of late treatment-related toxicity on
quality of life among patients with head and neck cancer treated with
radiotherapy. J Clin Oncol 2008, 26:37703776.
2. Jellema AP, Slotman BJ, Doornaert P, Leemans CR, Langendijk JA: Impact of
radiation-induced xerostomia on quality of life after primary
radiotherapy among patients with head and neck cancer. Int J Radiat
Oncol Biol Phys 2007, 69:751760.
3. Braam PM, Terhaard CH, Roesink JM, Raaijmakers CP: Intensity-modulated
radiotherapy significantly reduces xerostomia compared with
conventional radiotherapy. Int J Radiat Oncol Biol Phys 2006, 66:975980.
4. Kam MK, Leung SF, Zee B, Chau RM, Suen JJ, Mo F, Lai M, Ho R, Cheung KY,
Yu BK, Chiu SK, Choi PH, Teo PM, Kwan WH, Chan AT: Prospective
randomized study of intensity-modulated radiotherapy on salivary gland
function in early-stage nasopharyngeal carcinoma patients. J Clin Oncol
2007, 25:48734879.
Page 4 of 4
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
Pow EH, Kwong DL, McMillan AS, Wong MC, Sham JS, Leung LH, Leung WK:
Xerostomia and quality of life after intensity-modulated radiotherapy vs.
conventional radiotherapy for early-stage nasopharyngeal carcinoma:
initial report on a randomized controlled clinical trial. Int J Radiat Oncol
Biol Phys 2006, 66:981991.
Little M, Schipper M, Feng FY, Vineberg K, Cornwall C, Murdoch-Kinch CA,
Eisbruch A: Reducing xerostomia after chemo-IMRT for head-and-neck
cancer: beyond sparing the parotid glands. Int J Radiat Oncol Biol Phys
in press.
Alliende C, Kwon YJ, Brito M, Molina C, Aguilera S, Prez P, Leyton L, Quest
AF, Mandel U, Veerman E, Espinosa M, Clausen H, Leyton C, Romo R,
Gonzlez MJ: Reduced sulfation of muc5b is linked to xerostomia in
patients with Sjgren syndrome. Ann Rheum Dis 2008, 67:14801487.
Eliasson L, Carln A: An update on minor salivary gland secretions. Eur J
Oral Sci 2010, 118:435442.
Dijkema T, Terhaard CH, Roesink JM, Braam PM, van Gils CH, Moerland MA,
Raaijmakers CP: Large cohort dose-volume response analysis of parotid
gland function after radiotherapy: intensity-modulated versus
conventional radiotherapy. Int J Radiat Oncol Biol Phys 2008, 72:11011109.
Houweling AC, Dijkema T, Roesink JM, Terhaard CH, Raaijmakers CP: Sparing
the contralateral submandibular gland in oropharyngeal cancer patients:
a planning study. Radiother Oncol 2008, 89:6470.
Silva DG, Stevens RH, Macedo JM, Hirata R, Pinto AC, Alves LM, Veerman EC,
Tinoco EM: Higher levels of salivary MUC5B and MUC7 in individuals
with gastric diseases who harbor Helicobacter pylori. Arch Oral Biol 2009,
54:8690.
Veerman ECI, Bolscher JGM, Appelmelk BJ, Bloemena E, van den Berg TK,
Nieuw Amerongen AV: A monoclonal antibody directed against high M(r)
salivary mucins recognizes the SO3-3Gal beta 1-3GlcNAc moiety of
sulfo-Lewis(a): a histochemical survey of human and rat tissue.
Glycobiology 1997, 7:3743.
Rayment SA, Liu B, Offner GD, Oppenheim FG, Troxler RF:
Immunoquantification of human salivary mucins MG1 and MG2 in
stimulated whole saliva: factors influencing mucin level. J Dent Res 2000,
79:17651772.
Tabak LA: In defense of the oral cavity: structure, biosynthesis, and
function of salivary mucins. Annu Rev Physiol 1995, 57:547564.
Pramanik R, Osailan SM, Challacombe SJ, Urquhart D, Proctor GB: Protein
and mucin retention on oral mucosal surfaces in dry mouth patients.
Eur J Oral Sci 2010, 118:245253.
Veerman ECI, van den Keijbus PAM, Nazmi K, Vos W, van der Wal JE,
Bloemena E, Bolscher JGM, Nieuw Amerongen AV: Distinct localization of
MUC5B glycoforms in the human salivary glands. Glycobiology 2003,
13:363366.
Nieuw Amerongen AV, Bolscher JGM, Veerman ECI: Salivary mucins:
protective functions in relation to their diversity. Glycobiology 1995,
5:733740.
doi:10.1186/1748-717X-7-91
Cite this article as: Dijkema et al.: MUC5B levels in submandibular gland
saliva of patients treated with radiotherapy for head-and-neck cancer: A
pilot study. Radiation Oncology 2012 7:91.
Submit your next manuscript to BioMed Central
and take full advantage of:
Convenient online submission
Thorough peer review
No space constraints or color gure charges
Immediate publication on acceptance
Inclusion in PubMed, CAS, Scopus and Google Scholar
Research which is freely available for redistribution
Submit your manuscript at
www.biomedcentral.com/submit
Vous aimerez peut-être aussi
- Emergency Psychiatry Other Than Suicide: Dr. Pooja Singh, MD Assistant ProfessorDocument45 pagesEmergency Psychiatry Other Than Suicide: Dr. Pooja Singh, MD Assistant Professorpooja singhPas encore d'évaluation
- Autonomic Nervous System: Rodina Rivera-Gorospe, M.DDocument44 pagesAutonomic Nervous System: Rodina Rivera-Gorospe, M.DPogo LocoPas encore d'évaluation
- Application Technique Traction PDFDocument25 pagesApplication Technique Traction PDFAZOZ 19Pas encore d'évaluation
- Management Flabby RidgeDocument4 pagesManagement Flabby RidgeNidya Patricia Sembiring100% (1)
- Unchallengeable Miracles of QuranDocument430 pagesUnchallengeable Miracles of QuranyoursincerefriendPas encore d'évaluation
- Leukemia EssayDocument4 pagesLeukemia EssaydanarajPas encore d'évaluation
- AACR 2022 Proceedings: Part A Online-Only and April 10D'EverandAACR 2022 Proceedings: Part A Online-Only and April 10Pas encore d'évaluation
- Nursing Care Plan: Lorma Colleges Con Template Related Learning ExperienceDocument6 pagesNursing Care Plan: Lorma Colleges Con Template Related Learning ExperiencePauline GarciaPas encore d'évaluation
- Clinical Guidelines Acute Rehab Management 2010 InteractiveDocument172 pagesClinical Guidelines Acute Rehab Management 2010 InteractivenathanaelandryPas encore d'évaluation
- Case Report Acute Otitis MediaDocument28 pagesCase Report Acute Otitis Mediamayo djitro100% (2)
- A Second-Generation Dendritic Cell Cancer Vaccine Preparing To ShineDocument19 pagesA Second-Generation Dendritic Cell Cancer Vaccine Preparing To Shinebiggercapital100% (5)
- Tai Chi LiteratureDocument2 pagesTai Chi LiteratureMichael Fong100% (1)
- JNatScBiolMed42374-2207918 003647Document5 pagesJNatScBiolMed42374-2207918 003647Ibrahim AliPas encore d'évaluation
- Tient SubtypesDocument6 pagesTient SubtypesDr-Dalya ShakirPas encore d'évaluation
- 66 68 PBDocument89 pages66 68 PBAyesha FatimaPas encore d'évaluation
- 1026 FullDocument5 pages1026 FullMuhammad Yufimar Rizza FadilahPas encore d'évaluation
- Tugas Endnote1Document7 pagesTugas Endnote1Syatirahlupphkiki XoixPas encore d'évaluation
- Document 5Document15 pagesDocument 5api-432471589Pas encore d'évaluation
- Rough Draft 1Document11 pagesRough Draft 1api-431732695Pas encore d'évaluation
- NR Endo 201421Document6 pagesNR Endo 201421Lucia VillacrizPas encore d'évaluation
- Iaft 07 I 2 P 114Document4 pagesIaft 07 I 2 P 114ashajangamPas encore d'évaluation
- The Effect of Twice Daily Kiwifruit Consumption On Periodontal and Systemic ConditionsDocument18 pagesThe Effect of Twice Daily Kiwifruit Consumption On Periodontal and Systemic ConditionsMargarita Damas PérezPas encore d'évaluation
- Background: Nivolumab For Recurrent Squamous-Cell Carcinoma of The Head and NeckDocument10 pagesBackground: Nivolumab For Recurrent Squamous-Cell Carcinoma of The Head and NeckjoitPas encore d'évaluation
- 10.1515 - CCLM 2023 7044Document112 pages10.1515 - CCLM 2023 7044sfendri17Pas encore d'évaluation
- 10.1515 - CCLM 2023 7047Document101 pages10.1515 - CCLM 2023 7047sfendri17Pas encore d'évaluation
- P ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Document4 pagesP ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Riri KumalaPas encore d'évaluation
- Actividad 2 Periodoncia Avanzada ElizabethDocument16 pagesActividad 2 Periodoncia Avanzada ElizabethElizabeth MartinezPas encore d'évaluation
- FLC in MGDocument17 pagesFLC in MGMuhammad Umer Naeem EffendiPas encore d'évaluation
- A Proteomic Approach For The Diagnosis of Bacterial Meningitisjournal - Pone.0010079Document9 pagesA Proteomic Approach For The Diagnosis of Bacterial Meningitisjournal - Pone.0010079Paijo SusenoPas encore d'évaluation
- Saliva Oral Tongue Tumor Markers CancerDocument35 pagesSaliva Oral Tongue Tumor Markers CancerAdle AboobackerPas encore d'évaluation
- Il 6 2Document28 pagesIl 6 2Herpika DianaPas encore d'évaluation
- 955 3471 1 PBDocument5 pages955 3471 1 PBOris WicaksonoPas encore d'évaluation
- Articulo OooDocument7 pagesArticulo OooPaola M. TrianaPas encore d'évaluation
- Antimicrobial Effect of Platelet Rich Plasma Against Porphyromonas GinivalisDocument15 pagesAntimicrobial Effect of Platelet Rich Plasma Against Porphyromonas GinivalisBilly TrầnPas encore d'évaluation
- Is Adjuvant Chemotherapy Useful For Women With Luminal A Breast Cancer?Document4 pagesIs Adjuvant Chemotherapy Useful For Women With Luminal A Breast Cancer?maur_jmpPas encore d'évaluation
- King's Research Portal: Citing This PaperDocument24 pagesKing's Research Portal: Citing This PaperShishirGaziPas encore d'évaluation
- Results of trialALL-BFM 90Document13 pagesResults of trialALL-BFM 90Anonymous 9dVZCnTXSPas encore d'évaluation
- Capecitabina BQQDocument8 pagesCapecitabina BQQAccelerium ClinicalPas encore d'évaluation
- Palliative Care PilocarpinaDocument7 pagesPalliative Care PilocarpinaIsteicy CortezPas encore d'évaluation
- Aging V14i5 203924Document20 pagesAging V14i5 203924Sotirios KatsamakasPas encore d'évaluation
- Adiponectin Concentration in The Orbital Fat of Patients With Graves' OphthalmopathyDocument4 pagesAdiponectin Concentration in The Orbital Fat of Patients With Graves' OphthalmopathyManuel VasquezPas encore d'évaluation
- MBC Significantly-Longer-Time-To-Deterioration-Of-QualDocument10 pagesMBC Significantly-Longer-Time-To-Deterioration-Of-QualAhmad Azhar Ab HamidPas encore d'évaluation
- Laprosy Research Paper (Ahmed Tanjimul Islam)Document7 pagesLaprosy Research Paper (Ahmed Tanjimul Islam)AHMED TANJIMUL ISLAMPas encore d'évaluation
- Is Paromomycin An Effective and Safe Treatment Against Cutaneous Leishmaniasis? A Meta-Analysis of 14 Randomized Controlled TrialsDocument10 pagesIs Paromomycin An Effective and Safe Treatment Against Cutaneous Leishmaniasis? A Meta-Analysis of 14 Randomized Controlled TrialsCarlos Alberto CastañedaPas encore d'évaluation
- Use of Therapeutic Laser For Prevention and Treatment of Oral MucositisDocument6 pagesUse of Therapeutic Laser For Prevention and Treatment of Oral Mucositishendra ardiantoPas encore d'évaluation
- Contro Pacientes DiabeticosDocument3 pagesContro Pacientes DiabeticosFrancisco Josue TinajeroPas encore d'évaluation
- Erbitux MonotherapyDocument7 pagesErbitux MonotherapyMaulik PatelPas encore d'évaluation
- Mycophenolic Acid Exposure Optimization Based On VDocument15 pagesMycophenolic Acid Exposure Optimization Based On Valfaz zamzamiPas encore d'évaluation
- Abstract Early IdentificationDocument4 pagesAbstract Early IdentificationrhezagiovPas encore d'évaluation
- Journal of Research in Pharmacy PracticeDocument6 pagesJournal of Research in Pharmacy PracticeLasiaf AlaskaPas encore d'évaluation
- 11111Document19 pages11111Nejc KovačPas encore d'évaluation
- 04.analysis of GATA1 Mutations and Leukemogenesis in Newborns With Down SyndromeDocument9 pages04.analysis of GATA1 Mutations and Leukemogenesis in Newborns With Down SyndromeCristi Daniel NeagoePas encore d'évaluation
- Efficacy and Safety of Durvalumab With Olaparib inDocument7 pagesEfficacy and Safety of Durvalumab With Olaparib inMihaela PopaPas encore d'évaluation
- The Effect of Delmopinol Mouthwash On Aphthous StomatitisDocument19 pagesThe Effect of Delmopinol Mouthwash On Aphthous StomatitisAthenaeum Scientific PublishersPas encore d'évaluation
- Expresion of GLP1 in Thyroid CarcinomaDocument9 pagesExpresion of GLP1 in Thyroid CarcinomaW Antonio Rivera MartínezPas encore d'évaluation
- p53, Cytokeratin 19 Expression in Oral Squamous Cell Carcinoma and Correlation With Histopathologic Grading: An Immunohistochemical StudyDocument9 pagesp53, Cytokeratin 19 Expression in Oral Squamous Cell Carcinoma and Correlation With Histopathologic Grading: An Immunohistochemical StudyRana PalPas encore d'évaluation
- Acute Myeloid Leukemia...Document20 pagesAcute Myeloid Leukemia...hemendre0% (1)
- Can 13 0527rDocument30 pagesCan 13 0527rData KiswaraPas encore d'évaluation
- Euromedlab 2013 Abstracts 211 and 219Document103 pagesEuromedlab 2013 Abstracts 211 and 219Jagannadha Rao PeelaPas encore d'évaluation
- Journal - Pemfigus ParaneoplastikDocument20 pagesJournal - Pemfigus ParaneoplastikAulia Rosa AmelindaPas encore d'évaluation
- Effectiveness of Periodontal Therapy On The Severity ofDocument15 pagesEffectiveness of Periodontal Therapy On The Severity ofrajeshnamburiPas encore d'évaluation
- Comparison of Whole Blood and PBMC Assays ForDocument5 pagesComparison of Whole Blood and PBMC Assays ForFani LonelygirlPas encore d'évaluation
- Xerostomia Literature ReviewDocument7 pagesXerostomia Literature Reviewaflsbdfoj100% (1)
- DeWire 2022Document14 pagesDeWire 2022docadax848Pas encore d'évaluation
- ZH 800607002314Document8 pagesZH 800607002314ekanovicaPas encore d'évaluation
- 1 s2.0 S1470204514711660 MainDocument1 page1 s2.0 S1470204514711660 MainAli Sibra MulluziPas encore d'évaluation
- Introp 1Document5 pagesIntrop 1Rima RaisyiahPas encore d'évaluation
- Combination Therapy of Rituximab and Mycophenolate Mofetil in Childhood Lupus NephritisDocument6 pagesCombination Therapy of Rituximab and Mycophenolate Mofetil in Childhood Lupus NephritisrifkyramadhanPas encore d'évaluation
- Mebendazole Compared With Secnidazole in The Treatment of Adult GiardiasisDocument16 pagesMebendazole Compared With Secnidazole in The Treatment of Adult GiardiasisJanessa DalidigPas encore d'évaluation
- How I Treat Newly Diagnosed Chronic Phase CMLDocument9 pagesHow I Treat Newly Diagnosed Chronic Phase CMLDenisse SarabiaPas encore d'évaluation
- Pamj 24 182 PDFDocument5 pagesPamj 24 182 PDFDexter BluesPas encore d'évaluation
- Activation of mTOR: A Culprit of Alzheimer's Disease?: Neuropsychiatric Disease and Treatment DoveDocument16 pagesActivation of mTOR: A Culprit of Alzheimer's Disease?: Neuropsychiatric Disease and Treatment Dovemr dexterPas encore d'évaluation
- Nejmoa1514762 PDFDocument12 pagesNejmoa1514762 PDFDexter BluesPas encore d'évaluation
- Benefits and Risks of Antiretroviral TherapyDocument12 pagesBenefits and Risks of Antiretroviral TherapyAtgy Dhita AnggraeniPas encore d'évaluation
- SDJ 2016 09 01 PDFDocument7 pagesSDJ 2016 09 01 PDFDexter BluesPas encore d'évaluation
- Ulkus Kornea Eng VerDocument15 pagesUlkus Kornea Eng VerDexter BluesPas encore d'évaluation
- Childhood IQ and Bipolar Link PDFDocument9 pagesChildhood IQ and Bipolar Link PDFDexter BluesPas encore d'évaluation
- Jurnal Anak RirinDocument10 pagesJurnal Anak RirinDexter BluesPas encore d'évaluation
- PRM2016 1658172 PDFDocument7 pagesPRM2016 1658172 PDFDexter BluesPas encore d'évaluation
- Jurnal Anak Ririn PDFDocument10 pagesJurnal Anak Ririn PDFDexter BluesPas encore d'évaluation
- Medi 96 E5795 PDFDocument5 pagesMedi 96 E5795 PDFDexter BluesPas encore d'évaluation
- Nejmoa1606356 PDFDocument10 pagesNejmoa1606356 PDFDexter BluesPas encore d'évaluation
- The Seven Cardinal MovementsDocument4 pagesThe Seven Cardinal MovementsDexter BluesPas encore d'évaluation
- Mood Dynamics in Bipolar Disorder: Research Open AccessDocument9 pagesMood Dynamics in Bipolar Disorder: Research Open AccesswulanfarichahPas encore d'évaluation
- The Seven Cardinal MovementsDocument4 pagesThe Seven Cardinal MovementsDexter BluesPas encore d'évaluation
- Referat Obgyn FixDocument29 pagesReferat Obgyn FixDexter BluesPas encore d'évaluation
- Rincian Jadwal Jaga Koas Obsgin 2016 Senin Selas A Rabu Kami S Jumat Sabtu Mingg UDocument1 pageRincian Jadwal Jaga Koas Obsgin 2016 Senin Selas A Rabu Kami S Jumat Sabtu Mingg UDexter BluesPas encore d'évaluation
- Referat Obgyn FixDocument29 pagesReferat Obgyn FixDexter BluesPas encore d'évaluation
- Fix ObgynDocument17 pagesFix ObgynDexter BluesPas encore d'évaluation
- Childhood IQ and Bipolar Link PDFDocument9 pagesChildhood IQ and Bipolar Link PDFDexter BluesPas encore d'évaluation
- The Seven Cardinal MovementsDocument3 pagesThe Seven Cardinal MovementsMaria Mandid0% (1)
- Pruritus: An Updated Look at An Old ProblemDocument7 pagesPruritus: An Updated Look at An Old ProblemThariq Mubaraq DrcPas encore d'évaluation
- QuestionsDocument1 pageQuestionsDexter BluesPas encore d'évaluation
- 1830 PDF PDFDocument5 pages1830 PDF PDFDexter BluesPas encore d'évaluation
- 10 4103@0378-6323 116725 PDFDocument14 pages10 4103@0378-6323 116725 PDFDexter BluesPas encore d'évaluation
- TSWJ2015 803752 PDFDocument8 pagesTSWJ2015 803752 PDFDexter BluesPas encore d'évaluation
- Jurnal Elderly 2 PDFDocument3 pagesJurnal Elderly 2 PDFDexter BluesPas encore d'évaluation
- Geriatric Itch PDFDocument16 pagesGeriatric Itch PDFDexter BluesPas encore d'évaluation
- Tracheostomy CareDocument7 pagesTracheostomy CareJoanna MayPas encore d'évaluation
- Spleen Diseases DiagnosisDocument2 pagesSpleen Diseases DiagnosisPraveen VontiPas encore d'évaluation
- 2.PCC Bp3iDocument36 pages2.PCC Bp3iRSUD INDRAMAYU PMKPPas encore d'évaluation
- Assessing Breasts and AxillaeDocument23 pagesAssessing Breasts and AxillaeKamile Abrahan GarciaPas encore d'évaluation
- Ineffective Health MaintenanceDocument6 pagesIneffective Health MaintenanceRYAN SAPLADPas encore d'évaluation
- Opinion WritingDocument20 pagesOpinion WritingnirmalaPas encore d'évaluation
- Application Form 1Document3 pagesApplication Form 1thienndhPas encore d'évaluation
- Assignment 4: Genes & Cancer: NameDocument2 pagesAssignment 4: Genes & Cancer: Namemiriam tidalPas encore d'évaluation
- Integrated Application Form 97 2003 Compatible PDFDocument15 pagesIntegrated Application Form 97 2003 Compatible PDFdrchughPas encore d'évaluation
- A Literary LifeDocument5 pagesA Literary LifeLayla AliPas encore d'évaluation
- Conversation Bhs Inggris Untuk 5 OrangDocument4 pagesConversation Bhs Inggris Untuk 5 OrangKurogami100% (1)
- Branches of ZoologyDocument3 pagesBranches of ZoologyVivek Morya100% (1)
- Biokimia NeurupsikiatriDocument40 pagesBiokimia Neurupsikiatrisuyudi kimikoPas encore d'évaluation
- Continuing High Mortality From Trauma Haemorrhage and Opportunities For Improvement in Transfusion Practice: A Observational StudyDocument21 pagesContinuing High Mortality From Trauma Haemorrhage and Opportunities For Improvement in Transfusion Practice: A Observational StudydanielPas encore d'évaluation
- Assignment 1Document13 pagesAssignment 1林佑邦Pas encore d'évaluation
- Oral 5Document236 pagesOral 5Iodeh1985 OdehPas encore d'évaluation
- Homoeopathic Case TakingDocument10 pagesHomoeopathic Case TakingSudhir GuptaPas encore d'évaluation
- ES V 0281 001 FinalSPCDocument4 pagesES V 0281 001 FinalSPCPankaj BeniwalPas encore d'évaluation
- History of Powerlifting Warpeha 9-4-15Document19 pagesHistory of Powerlifting Warpeha 9-4-15Treinador Bruno FerreiraPas encore d'évaluation
- Cordymax Trifold BrochureDocument2 pagesCordymax Trifold BrochureCherry San DiegoPas encore d'évaluation
- LydiaDocument219 pagesLydiatayabakhanPas encore d'évaluation