Académique Documents
Professionnel Documents
Culture Documents
Diseases of Dairy Cattle: Mastitis, Lameness, Fertility Issues
Transféré par
Junaid IjazTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Diseases of Dairy Cattle: Mastitis, Lameness, Fertility Issues
Transféré par
Junaid IjazDroits d'auteur :
Formats disponibles
9/8/2010
Diseases of Dairy Cattle
(based on Dr. Swists notes)
PATB 4110 - Diseases of Food Animals and Horses
9/8/2010
Diseases of specific concern in dairy cattle
2
The Big Three: mastitis; lameness; fertility
And three important infections:
Salmonellosis
Johnes
Tuberculosis
Retained placenta
Brisket
[personal interest]
Milk fever ( calcium)
Grass tetany ( magnesium)
Ketosis
9/8/2010
General Concepts
3
Nutritional & management problems vs. infectious disease
(contagious vs. non-contagious)
Clinical vs. subclinical disease
Cost of diseases
Veterinary & drug expenses
Loss of production (unrealized income)
Early culling/death
One animal vs. the herd
Prevalence
9/8/2010
9/8/2010
Disease can often occur in a predictable sequence or cascade
4
9/8/2010
Overconditioning
5
Optimal BCS for a cow at calving is 3.5-3.75/5
Overconditioning increases susceptibility to
all metabolic disorders
Alters hormonal balance
Greater decreases in feed intake prepartum
Faster rate of body weight loss
Rapid fat mobilization to meet energy needs
Decreased milk yields
Longer period of negative energy balance
9/8/2010
Body condition score in dairy cattle
6
9/8/2010
9/8/2010
Displaced abomasum
7
9/8/2010
Displaced abomasum
8
Repositioned abomasum from right ventral side of
abdominal cavity
Twisting from repositioning slows or stops flow of digesta
Gas buildup leads to bloat appearance
Pinging detected with stethoscope by thumping the cow near last
rib and listening on left flank
85-90% left-sided
75% occur within 1st 14 days post calving
Rare in heifers
9/8/2010
Normal Abomasum Position
Displaced Abomasum
D
A
B
C
Abomasum = A
C = Omasum
Rumen = B
D = Liver
9
9/8/2010
9/8/2010
Symptoms of DA
10
Dramatically decreased feed intake
Drastic drop in milk production
Pain (b
(back arched))
9/8/2010
Causes and Risk Factors
11
Etiology is multifactorial, although abomasal
hypomotility & gas production major contributors to
displacement or volvulus
Abomasal hypomotility:
Hypocalcemia
Mastitis/metritis-endotoxemia & decreased rumen fill
Hypomotiliy also associated with:
Ingestion high-concentrate, low-roughage diets ( VFA)
Diets also result in gas production
Changes in position of organs and fetus prior to birth
Genetic predisposition; deep-bodied cows
Ketosis
9/8/2010
Displaced Abomasum
12
Non-surgical
Removal of gas from abomasum
Rolling cow over, taking on rough trailer ride
Tethering of right hind leg
87% recovery rate
Surgical
Move abomasum into place and attach it surgically to
body wall
Open incision or blind tack
92% recovery rate
9/8/2010
9/8/2010
Displaced Abomasum
13
Prevention
Ensure rapid increase in rumen volume following calving
Feed a total mixed ration
Avoid rapid dietary changes
Maintain adequate roughage in diet
Cows should be in proper body condition at parturition
Prevent hypocalcemia & other metabolic disease
9/8/2010
Bovine Tuberculosis
14
9/8/2010
Bovine Tuberculosis (TB)
15
Historic Disease:
Bovine TB caused more losses among US farm animals in early
1900s than all other infectious diseases combined
Meat inspection: looking for TB esp.
1917, USDA/APHIS began national eradication program; 2010 TB
nearly eliminated
Highly contagious to all warm-blooded animals & humans
Reportable disease in WY & US
Wildlife can spread TB to commercial cattle (and cattle to wildlife)
Mycobacteria
M. bovis, M. avium & M. tuberculosis
9/8/2010
9/8/2010
Transmission & clinical signs
16
Transmission:
Aerosol>ingestion(milk)>intrauterine/sexual
Clinical signs: Depends on organ/location
Usuallyy chronic disease but can have acute episodes
p
General: emaciation, lethargy, weakness, anorexia, fever
Granulomatous inflammation/disease
i.e., Lung, liver, lymph nodes
9/8/2010
Emaciated Cow
Lung & liver
granulomas
17
9/8/2010
Lung & lymph node granulomas
Acid fast stain of Mycobacterium
18
9/8/2010
9/8/2010
Diagnosis TB
19
Most important diagnostic test:
Intradermal tuberculin test
Diagnosis on clinical signs alone difficult even w/advanced
cases
Other :
Radiographs, microscopic exam sputum/fluids
Meat inspection
Necropsy
Definitive diagnosis:
Isolation & ID of bacteria ~4-8wks
PCR ~2-4 days
9/8/2010
TB Tuberculin skin test
20
Animal exposed to tuberculin
Mycobacterial antigen- M. bovis or M. tuberculosis
Checked for reaction after 72 hrs
Delayed type hypersensitivity
If host
h t a reactor,
t antigen
ti
stimulates
ti l t llocall iinflammation
fl
ti c/o
/ skin
ki
swelling
Test sites vary in sensitivity & between countries ~neck, anal or
caudal fold of tail
Disadvantage: Poor specificity-cross reacts with other
Mycobacteria spp. & Nocardia spp.
9/8/2010
Control
21
#1:Test & slaughter
Only
way to assure eradication
of reactors detected by tuberculin test
In affected herd, test every 3 mo.
UM&R
Slaughter
#2: Test & segregate
#3: Chemotherapy
Elephants, nonhuman primates, humans
Routine hygiene
Clean & disinfect contaminated food, water troughs, etc.
9/8/2010
9/8/2010
Control
22
Nationwide slaughter plant surveillance activities
If positive found, trace back to herd of origin
Test
T t & slaughter
l
ht h
herd
d if necessary
Depopulation voluntary, so may quarantine
9/8/2010
Wyoming Livestock Board: Animal Import Rules
23
Import permit required on all bovines entering WY
Certificate of Veterinary Health Inspection required
Bovine originating from a state not accredited TB free must
meett USDA/APHIS requirements
i
t ffor TB
Cattle must be tested prior to movement
Based on status of state/zone and class of cattle
(breeding, sexually intact vs. spayed heifers and steers for
feeding)
9/8/2010
24
9/8/2010
9/8/2010
Mastitis
25
What is it?
Inflammation of the mammary gland
Healthy Udder & Mammary gland tissue
9/8/2010
Healthy mammary gland tissue
Mastitis
26
9/8/2010
Causes of Mastitis
27
Infectious mastitis
Invasion of bacteria into gland
Clinical or sub-clinical
Many more subclinical cases than clinical
Non
Non-infectious
infectious mastitis
Due to injury, chilling, bruising, improper milking
9/8/2010
9/8/2010
Mastitis Quick Facts
28
All dairy herds have cows w/subclinical mastitis
Varies from 15-75%
Of cows affected, 5-40% are infected in more than one quarter
On average, 2 infections per lactation
9/8/2010
Mastitis
29
Above totals are from 1996. USDA/APHIS Dairy report: From 19962007 % of cows w/clinical mastitis increased 13.4 to 16.5%. The
total economic loss is closer to $250/cow.
9/8/2010
Mastitis
30
Clinical mastitis
Visible inflammation in udder (swelling, heat, pain, redness)
Systemic-fever, anorexia & shock
Abnormal milk (e.g., color, fibrin clots)
Subclinical mastitis
Infection and inflammation without clinical mastitis or
systemic involvement (asymptomatic)
9/8/2010
10
9/8/2010
For each clinical mastitis case (Orange), 15-40
subclinical cases (Green)
31
9/8/2010
32
9/8/2010
Mastitis pathogens
33
Co
Contagious
tag ous
Environmental
9/8/2010
11
9/8/2010
Contagious mastitis
34
Pathogens colonize mammary gland
Spread by milking machines, milkers & cow to cow
Staphylococcus aureus
Streptococcus agalactiae
l i
Corynebacterium bovis
Other Streptococcus spp. & Staphylococcus spp.
Mycoplasma spp. can spread from cow to cow through
aerosol transmission
9/8/2010
35
9/8/2010
Contagious mastitis
36
Staphylococcus aureus
Worst of the contagious agents
Penetrates deep into glandular epithelium
Not very responsive to antibiotics resistance common
Immune response of cow not as successful in eliminating
infections as with other pathogens
Once established in herd, difficult/impossible to eradicate
Dry treat or cull
Survives in multiple locations in cow
Transmitted esp. by hands
Streptococcus agalactiae
Obligate infection of mammary gland
Readily eradicated with antibiotics
Multiply in milk and on mammary epithelial surfaces
Will not survive in the environment
9/8/2010
12
9/8/2010
Mycoplasma
37
Primarily respiratory pathogen
Can infect many tissues
Spreads through multiple routes
Contagious and environmental
High shedding rate
Severe purulent mastitis in multiple quarters
No treatment - identify and cull
9/8/2010
Environmental mastitis
38
Pathogens do not normally infect mammary gland
Infection when cows environment, milking machine
or teats/udder are contaminated access through
teat canal
Streptococcus uberis & other non-agalactiae Streptococcus
spp.
Escherichia coli and Klebsiella sp. (coliforms)
Arcanobacterium pyogenes
Important to maintain good sanitary conditions
9/8/2010
Environmental mastitis
39
Infect cows between milkings
Streptococcus dysgalactiae and Streptococcus
uberis
Escherichia coli
Symptoms confined to mammary gland
Easily out-competed (opportunistic)
Easily eradicated (antibiotics, immune system)
Toxins released when killed
Systemic
effects (fever, depression, death)
9/8/2010
13
9/8/2010
Pathways for Infection
40
Most common route of entry is streak canal
Smaller diameter streak canals more resistant to mastitis
If keratin plug compromised, animals more susceptible to
mastitis
9/8/2010
In udder...
41
Bacteria proliferate, destroy secretory cells
Some release toxins when killed
Destroy more secretory cells
Absorbed
Ab b d iinto bl
bloodstream
d
systemic effects (fever, low appetite)
Milk ducts blocked by clotted milk
Blood vessels dilate, slowing blood flow
Interferes with treatment access
9/8/2010
Acute mastitis:
42
Udder hot, hard, tender
Increased temperature, refusal to eat, dull eyes,
rough coat
Increased blood proteins and leukocytes in
mammary tissue and milk
Blood vessels greatly dilated
Milk ducts compressed
Treatments more likely to be unsuccessful under these conditions
9/8/2010
14
9/8/2010
43
9/8/2010
Chronic Mastitis
44
If treatment unsuccessful
Scar tissue
Ducts permanently blocked
Loss
L
off function
f
ti iin glands
l d may b
be permanentt
9/8/2010
Mastitis signs and symptoms
45
High somatic cell count (SCC) indicates mastitis
Composed of neutrophils from the blood and epithelial
secretory cells
Neutrophils in milk = response to infection
Epithelial cells in milk
Each doubling of SCC >50,000 cells.ml = loss of 0.5 kg/milk/day
In chronic mastitis, only symptom is milk thick or
lumpy
Terms you will hear:
Summer mastitis = A. pyogenes = loss of quarter
Gangranous mastitis = various causes; life-threatening
9/8/2010
15
9/8/2010
Milk quality changes
46
Altered composition
Decreased fat, protein, lactose
Increased chlorides
Lower total solids
As low as 1/3 normal milk
Poor flavor (salty)
Clumping of somatic cells
Clumpy, stringy milk
Only 2-3% of all cases show clinical symptoms
9/8/2010
Risk factors
47
Majority of new infections occur during:
First 3 weeks of dry period
Milk left in udder
First month after parturition
Immune system compromised
Frequency of milking affects risk of infection
Pathogen load decreased by evacuating milk more frequently
Position of the gland
More exposed to environment, greater the risk
Chilling on cold ground
Improper ventilation and dampness
Injury
Heritability (conformation of udder/teat)
9/8/2010
Prevention and control
48
Clean and dry environment
Clean and dry teats at milking
Good hygiene, esp. for environmental causes
Teat dips (pre- and post-milking)
Well maintained equipment
Segregate clinical cases
Early identification
Prompt treatment
Milking machine maintenance
Dry cow treatment
9/8/2010
16
9/8/2010
49
Uncomfortable free stalls increase the incidence of mastitis by increasing
exposure to environmental pathogens
9/8/2010
Latex Gloves
50
9/8/2010
51
Backflush systems reduce spread of contagious pathogens, such as S. aureus, by
sanitizing milkers between groups of cows
9/8/2010
17
9/8/2010
52
Teat dips only effective if adequate coverage of all teats
9/8/2010
53
Barrier teat dips useful to prevent mastitis in dry & transition cows
9/8/2010
54
Barrier dips block bacterial access to the animal and can be used to protect cut
areas where the skin barrier compromised.
9/8/2010
18
9/8/2010
Treatment
55
Antibiotics
During lactation
Dry period
Frequent milking
Reduce
R d
ability
bili to proliferate
lif
Oxytocin
Reduce volume of media
Reduce pathogen population
Fluid therapy for endotoxemia
9/8/2010
Treatment
56
Treatments used on dry cows most effective
method of treating Staphylococcus aureus
infections
Long-lasting antibiotic preparations
Should not be used if cows will not have full dry period
All intramammary infusions should be conducted
aseptically
Clean teat ends with alcohol
Insert infusion tube only as far as necessary
9/8/2010
57
Cannulas on commercial mastitis treatments should only be inserted one-quarter
inch into the teat end to minimize keratin removal
9/8/2010
19
9/8/2010
Treatment
58
Many reasons to avoid antibiotic contamination of
milk supply
Illegal - contamination results in financial penalties
Development of antibiotic resistance
Keep treated milk separate
Use separate equipment
9/8/2010
20
Vous aimerez peut-être aussi
- Liver Fluke An Overview For PractitionersDocument14 pagesLiver Fluke An Overview For PractitionersAli KareemPas encore d'évaluation
- Diseases of Dairy: GoatsDocument13 pagesDiseases of Dairy: GoatsalarochaPas encore d'évaluation
- Cork Pig and Poultry DiseasesDocument17 pagesCork Pig and Poultry DiseasesLeo PerezPas encore d'évaluation
- FPUK-0714-61536364: Salmonella InfectionsDocument11 pagesFPUK-0714-61536364: Salmonella InfectionsaliyahimranPas encore d'évaluation
- Emerging Mastitis Threats on Dairy FarmsDocument11 pagesEmerging Mastitis Threats on Dairy FarmsSofia ImtiazPas encore d'évaluation
- An Overview of Clostridium Species in Cattle and SheepDocument2 pagesAn Overview of Clostridium Species in Cattle and SheepRobert Marian RăureanuPas encore d'évaluation
- Dissertation CampylobacterDocument4 pagesDissertation CampylobacterCollegePaperWritingServicesMilwaukee100% (1)
- Diagnosis of Mycotoxicoses in Veterinary MedicineDocument10 pagesDiagnosis of Mycotoxicoses in Veterinary MedicineDamir SuljevicPas encore d'évaluation
- Animals: Epidemiology and Classification of MastitisDocument17 pagesAnimals: Epidemiology and Classification of Mastitisarini nashirahPas encore d'évaluation
- Salmonella in Shell Eggs Mechanisms Prevention and Detection 2155 9600 1000455Document7 pagesSalmonella in Shell Eggs Mechanisms Prevention and Detection 2155 9600 1000455mohammad khazarPas encore d'évaluation
- Puerperial PyrexiaDocument4 pagesPuerperial Pyrexiakutra3000Pas encore d'évaluation
- Vpe 311 TanuvasDocument281 pagesVpe 311 Tanuvaskaran kambojPas encore d'évaluation
- Antimicrobial Profile of Multidrug-Resistant Streptococcus Spp. Isolated From Dairy Cows With Clinical MastitisDocument12 pagesAntimicrobial Profile of Multidrug-Resistant Streptococcus Spp. Isolated From Dairy Cows With Clinical MastitisGezahegn BushoPas encore d'évaluation
- Vetmed - Vet 201511 0003Document8 pagesVetmed - Vet 201511 0003Aida GlavinicPas encore d'évaluation
- Articulo 2 paraDocument10 pagesArticulo 2 paraalex8813Pas encore d'évaluation
- Yers I NiosisDocument4 pagesYers I NiosisCharleen Joyce UsacdinPas encore d'évaluation
- First Page PDFDocument1 pageFirst Page PDFNupur SaxenaPas encore d'évaluation
- K-4 PR - Soil Transmitted HelminthiasisDocument45 pagesK-4 PR - Soil Transmitted HelminthiasissantayohanaPas encore d'évaluation
- Lecture Brucella 28-9-18Document58 pagesLecture Brucella 28-9-18Jayanthi TatineniPas encore d'évaluation
- Colibacillosis: Cause: E. ColiDocument37 pagesColibacillosis: Cause: E. ColiDianventi RiandaniPas encore d'évaluation
- Food Poisoning Fact FileDocument8 pagesFood Poisoning Fact FileAlpascaFirdausPas encore d'évaluation
- Calf Coccidiosis: DR Jonah KuttoDocument36 pagesCalf Coccidiosis: DR Jonah Kuttothanh ba matPas encore d'évaluation
- MorkzzzzDocument22 pagesMorkzzzzjd llobreraPas encore d'évaluation
- Diarrhea in Kittens and Young Cats - WSAVA2011 - VINDocument4 pagesDiarrhea in Kittens and Young Cats - WSAVA2011 - VINkukuhamru19Pas encore d'évaluation
- Aureus: Prepared By: Miss Sidra-tul-MuntahaDocument16 pagesAureus: Prepared By: Miss Sidra-tul-MuntahamuqaddasPas encore d'évaluation
- Paper 05Document8 pagesPaper 05deltanuevePas encore d'évaluation
- Metritis and Endometritis in High Yielding Dairy Cows PDFDocument9 pagesMetritis and Endometritis in High Yielding Dairy Cows PDFfranky100% (1)
- Staphylococci 222.ppsxDocument12 pagesStaphylococci 222.ppsxHaydas ChannelPas encore d'évaluation
- Botulism in Cattle: What Is Botulism and What Causes It?Document4 pagesBotulism in Cattle: What Is Botulism and What Causes It?Ali hamzaPas encore d'évaluation
- Bovine Mastitis An Evolving DiseaseDocument13 pagesBovine Mastitis An Evolving DiseaseIoana CriveiPas encore d'évaluation
- Advancements and Technologies in Pig and Poultry Bacterial Disease ControlD'EverandAdvancements and Technologies in Pig and Poultry Bacterial Disease ControlNeil FosterPas encore d'évaluation
- Staphylococcus Aureus: The Food Safety File: Staphylococcus Aureus Edition 2008 Food DoctorsDocument10 pagesStaphylococcus Aureus: The Food Safety File: Staphylococcus Aureus Edition 2008 Food DoctorsTessa Lonika EstaPas encore d'évaluation
- Avian Coccidiocis - 2016Document72 pagesAvian Coccidiocis - 2016thanh ba matPas encore d'évaluation
- Campylobacter: Features, Detection, and Prevention of Foodborne DiseaseD'EverandCampylobacter: Features, Detection, and Prevention of Foodborne DiseaseGünter KleinPas encore d'évaluation
- Food Borne Diseases Associated With Foods of Animal OriginDocument60 pagesFood Borne Diseases Associated With Foods of Animal OriginWan SyarifuddinPas encore d'évaluation
- Slavery and Slaughter of Animals for ConsumptionD'EverandSlavery and Slaughter of Animals for ConsumptionPas encore d'évaluation
- Roundworm 140120Document11 pagesRoundworm 140120Hellen HuttonPas encore d'évaluation
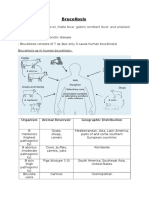
- Brucellosis: Aka: Mediterranean Fever, Malta Fever, Gastric Remittent Fever, and Undulant FeverDocument11 pagesBrucellosis: Aka: Mediterranean Fever, Malta Fever, Gastric Remittent Fever, and Undulant Feverfairuz160194Pas encore d'évaluation
- MedicalplanDocument6 pagesMedicalplanapi-341248896Pas encore d'évaluation
- Zoonotic DiseasesDocument96 pagesZoonotic DiseasesWakjira GemedaPas encore d'évaluation
- Prototheca MastitisDocument1 pagePrototheca Mastitismicrobiology kcvasPas encore d'évaluation
- Mycotoxins in Foodstuffs — 3: Invited Lectures Presented at the Third International IUPAC Symposium on Mycotoxins in Foodstuffs, Paris, France, 16 - 18 September, 1976D'EverandMycotoxins in Foodstuffs — 3: Invited Lectures Presented at the Third International IUPAC Symposium on Mycotoxins in Foodstuffs, Paris, France, 16 - 18 September, 1976M. JemmaliPas encore d'évaluation
- Mycobacterium Avium Subsp. Paratuberculosis in PowderedDocument9 pagesMycobacterium Avium Subsp. Paratuberculosis in PowderedDalonPetrelPas encore d'évaluation
- Staph Food PoisiningDocument14 pagesStaph Food PoisiningaishaPas encore d'évaluation
- Pyometrainsmallanimals: Ragnvi HagmanDocument23 pagesPyometrainsmallanimals: Ragnvi HagmansalomonPas encore d'évaluation
- Eggs and Salmonella: An Evaluation of Food Poisoning RiskDocument8 pagesEggs and Salmonella: An Evaluation of Food Poisoning RiskCarlos MarìnPas encore d'évaluation
- Mastitis ArticleDocument11 pagesMastitis ArticleHarikrishnan NamPas encore d'évaluation
- Brucellosis: By: Samira MuhyadinDocument19 pagesBrucellosis: By: Samira MuhyadinHUSNAH SULAIMANPas encore d'évaluation
- Vpe 311 Public HealthDocument354 pagesVpe 311 Public HealthshivaPas encore d'évaluation
- Microbiology: August 24, 2011 Mary Ann C. Bunyi, MDDocument5 pagesMicrobiology: August 24, 2011 Mary Ann C. Bunyi, MDLenard PlatonPas encore d'évaluation
- PoultryDocument11 pagesPoultryTawanda MandazaPas encore d'évaluation
- Milk Borne Infections 2Document83 pagesMilk Borne Infections 2Rao Qaisar Shahzad100% (1)
- Mastitis Control in Dairy HerdsDocument272 pagesMastitis Control in Dairy HerdsVladimir Huillca JaimePas encore d'évaluation
- Food Poisoning: Dr. SabirDocument29 pagesFood Poisoning: Dr. SabirciciliaPas encore d'évaluation
- Bacillus AnthracisDocument44 pagesBacillus AnthracisBalaji KrishnanPas encore d'évaluation
- BrucellosisDocument33 pagesBrucellosisعبدالرحمن محمد عبدالهاديPas encore d'évaluation
- Bovine Mastitis: Sukolrat Boonyayatra DVM, Ms Clinic For RuminantsDocument102 pagesBovine Mastitis: Sukolrat Boonyayatra DVM, Ms Clinic For RuminantsChai Yawat100% (2)
- 911 Pigeon Disease & Treatment Protocols!D'Everand911 Pigeon Disease & Treatment Protocols!Évaluation : 4 sur 5 étoiles4/5 (1)
- Diseases of Dairy Cattle: Mastitis, Lameness, Fertility IssuesDocument20 pagesDiseases of Dairy Cattle: Mastitis, Lameness, Fertility IssuesJunaid IjazPas encore d'évaluation
- Lohmann LSL LiteDocument48 pagesLohmann LSL LiteJunaid IjazPas encore d'évaluation
- Guideline For Thesis Writing (Sample) : BlackDocument10 pagesGuideline For Thesis Writing (Sample) : BlackJunaid IjazPas encore d'évaluation
- Guideline For Thesis Writing (Sample) : BlackDocument10 pagesGuideline For Thesis Writing (Sample) : BlackJunaid IjazPas encore d'évaluation
- Guideline For Thesis Writing (Sample) : BlackDocument10 pagesGuideline For Thesis Writing (Sample) : BlackJunaid IjazPas encore d'évaluation
- Maxolon Injection 5 MG / MLDocument1 pageMaxolon Injection 5 MG / MLJunaid IjazPas encore d'évaluation
- University of Veterinary & Animal Sciences, Lahore: Guideline For Synopsis Writing (Sample)Document4 pagesUniversity of Veterinary & Animal Sciences, Lahore: Guideline For Synopsis Writing (Sample)Junaid IjazPas encore d'évaluation
- Maxolon Injection 5 MG / MLDocument1 pageMaxolon Injection 5 MG / MLJunaid IjazPas encore d'évaluation
- SASO 1431 (GS 1355) SorbitolDocument5 pagesSASO 1431 (GS 1355) SorbitolakPas encore d'évaluation
- Paedo Don TicsDocument103 pagesPaedo Don TicsIana RusuPas encore d'évaluation
- LESHKOWICH 2014 American EthnologistDocument20 pagesLESHKOWICH 2014 American EthnologistJuKaschuPas encore d'évaluation
- Monthly Current Affairs Quiz - January 2023: Follow UsDocument244 pagesMonthly Current Affairs Quiz - January 2023: Follow UsSubhankar BasakPas encore d'évaluation
- Veterans Handbook 2020Document69 pagesVeterans Handbook 2020Senator Cory BookerPas encore d'évaluation
- NO Kodebarang Satuan Pakai Stock Awal Masuk Keluar Stock Akhir Harga KeteranganDocument4 pagesNO Kodebarang Satuan Pakai Stock Awal Masuk Keluar Stock Akhir Harga Keteranganruang belajar farmasiPas encore d'évaluation
- The ABO Blood Groups: Phenotypes GenotypesDocument2 pagesThe ABO Blood Groups: Phenotypes GenotypesSheila Mae CabahugPas encore d'évaluation
- Tun Razak Exchange, Retail Plot 1: APPENDIX 5 - Incident Reporting ProcedureDocument5 pagesTun Razak Exchange, Retail Plot 1: APPENDIX 5 - Incident Reporting ProcedureMatthew Mohan PerumalPas encore d'évaluation
- Unit 4 BacteriologyDocument51 pagesUnit 4 BacteriologySharmila LamisharPas encore d'évaluation
- Acy 087Document14 pagesAcy 087johnsmithdosPas encore d'évaluation
- Mapeh 10 2nd PrelimsDocument4 pagesMapeh 10 2nd PrelimsBlaize PascualPas encore d'évaluation
- Vaccinations Spina Bifida and HydrocephalusDocument6 pagesVaccinations Spina Bifida and HydrocephalusShine CharityPas encore d'évaluation
- Safe Food Handlers Course NotesDocument13 pagesSafe Food Handlers Course NotesJinky PradoPas encore d'évaluation
- Learning Kit - Q3W3 CeslDocument10 pagesLearning Kit - Q3W3 CeslJoselle Batas MagbanuaPas encore d'évaluation
- Obstetrics Case Proforma TemplateDocument4 pagesObstetrics Case Proforma TemplateSwapneelShah100% (1)
- Acute Diverticulitis-GcpDocument85 pagesAcute Diverticulitis-Gcpkuro hanabusaPas encore d'évaluation
- Managing Mental Health and Stress Online CourseDocument2 pagesManaging Mental Health and Stress Online CourseDakota624Pas encore d'évaluation
- Mozart, Beethoven, Yesudas Effect Class 2Document12 pagesMozart, Beethoven, Yesudas Effect Class 2Dr Suvarna NalapatPas encore d'évaluation
- Material Safety Data Sheet (MSDS) - Citric AcidDocument5 pagesMaterial Safety Data Sheet (MSDS) - Citric AcidMannar1Pas encore d'évaluation
- 2-1-2021 Response To LandlordDocument2 pages2-1-2021 Response To LandlordJessica SwarnerPas encore d'évaluation
- Confirmation 1068409Document3 pagesConfirmation 1068409ankiosaPas encore d'évaluation
- Cancer Lesson Plan For High SchoolDocument7 pagesCancer Lesson Plan For High SchoolUm IbrahimPas encore d'évaluation
- Less Adaptive or More Maladaptive? A Meta-Analytic Investigation of Procrastination and CopingDocument12 pagesLess Adaptive or More Maladaptive? A Meta-Analytic Investigation of Procrastination and CopingVALERIA BUSTAMANTE ALBERCOPas encore d'évaluation
- 004 General Consent English (Front)Document2 pages004 General Consent English (Front)عبدالله الرعويPas encore d'évaluation
- Immunohematology PDFDocument126 pagesImmunohematology PDFNicole Tan Calayca100% (1)
- Hospital Administrative Assistant Resume-A4Document2 pagesHospital Administrative Assistant Resume-A4Philip V AlexPas encore d'évaluation
- Internal MedicineDocument5 pagesInternal MedicineFırat GüllüPas encore d'évaluation
- Elanco Parvovirus DXTX GDocument2 pagesElanco Parvovirus DXTX Gazamkhan60Pas encore d'évaluation
- Nursing Abbreviations, Acronyms and Symbols QuizDocument3 pagesNursing Abbreviations, Acronyms and Symbols QuizAjeng Citra S SeptiyantriPas encore d'évaluation
- Bacteriological Water Analysis of Hostel's WaterDocument12 pagesBacteriological Water Analysis of Hostel's Waterapi-3705267Pas encore d'évaluation