Académique Documents
Professionnel Documents
Culture Documents
Medical Record Audit Tool PDF
Transféré par
nurhaidahDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Medical Record Audit Tool PDF
Transféré par
nurhaidahDroits d'auteur :
Formats disponibles
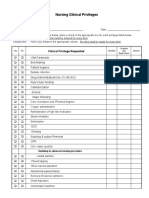
MEDICAL RECORD AUDIT TOOL
OPEN Nursing Review for Inpatient Adult and Pediatric Units
Page 1 of 4
REVIEW WITH MANAGER by the 5th of the month and FAX completed form to by the 10th of the month:
April Bowles at 982-6838 or MAIL to Box 800476.
Please audit the complete paper medical record
9CHECK THE APPROPRIATE BOX, EITHER: 9Y = Yes 9N = No 9NA = Not Applicable
Unit:
Manager Name:
CHART 1
CHART 2
Date Manager Reviewed:
CHART 3
CHART 4
Medical Record Number:
Admit Date:
Audit Date:
Reviewer(s):
Print Name
1. BLUE CHART
CHART:
Y N NA Y N NA Y N NA Y N NA
1.01 Patients name, sex, address, date of birth, admission diagnosis and
authorized representative or emergency contact are available in the record
(face sheet, EMR, database)?
1.02 If the patient is on Isolation, is there an information sheet from Infection Control in a page
protector? (NA if not on Isolation)
If the patient had a procedure(s) are the following in the chart? Check NA if no procedures
identified.
(Preprocedure checklist, Bedside form #050475, OR/Procedure #33033)
1.03 Was the Preprocedure verification section completed?
1.04 Was the Side/Body Site Verification section completed? (N/A if site verification not needed)
1.05 Is there an informed consent form? (NA if consent form not needed)
2. INFORMED CONSENT (LIP)
CHART:
Y N NA Y N NA Y N NA Y N NA
If Informed Consent was needed, consent form includes each of the following: (NA if no consent needed)
2.01 The nature of the proposed care, treatment, services, medications, interventions or procedures.
2.02 The potential benefits, risks, or side effects, including potential problems that might occur
during recuperation.
2.03 Reasonable alternatives as well as the relevant risks, benefits and side effects related to
alternatives, including the possible results of not receiving care, treatment and services.
2.04 Anesthesia type is accurately documented.
2.05 Was Informed Consent signed by patient or appropriate legal surrogate?
2.06 If applicable, blood consent obtained and includes the potential benefits, risks, side effects and
potential problems that might occur and is signed by patient or surrogate? (NA if no blood consent)
3. ADMITTING HISTORY AND PHYSICAL (LIP)
CHART:
Y N
3.01 Was an H&P completed within 30 days before or 24 hours after admission and placed in the
patients medical record within 24 hours after admission or registration but before surgery?
3.02 If H&P is less than 30 days, was updated examination completed and documented in the patients
medical record within 24 hours of admission or registration but before surgery?
Does the H&P include each of the following:
3.03 Chief complaint
3.04 Relevant past medical history
3.05 Details of present illness/injury
3.06 Social history
3.07 Allergies
3.08 Complete medication list including name, dose, route and frequency
3.09 Family history
3.10 Physical examination pertinent to diagnosis (including normal and abnormal findings
pertinent to care)
3.11 Planned course of action
2
Y N
3
Y N
4
Y N
To see related Joint Commission Standards see the Joint Commission Hospital Manual located as a computer desktop icon.
FORM 090801
NOT A CHART DOCUMENT
(REV 8/24/10)
To reorder, log onto http://www.virginia.edu/uvaprint/HSC/hs_forms.pl
MEDICAL RECORD AUDIT TOOL
4. INITIAL SCREENING (DATABASE)
CHART:
4.01 If Database blank, was at least 1 attempt made to obtain information if patient/family
unable to provide on admission? (NA if database is completed)
Note the Unit patient admitted to (information for Unit Manager)
4.02 Was initial screening by the RN initiated within 8 hours of admission to hospital and
completed within 24 hours? NOTE: IF Critical Care or L&D screening must be Initiated
AND completed within 8 hours.
4.03 If applicable, was person identified by patient notified of hospital admit? (NA if pt answers no)
Page 2 of 4
1
Y N NA Y N NA Y N NA Y N NA
4.04 For patient 18 years or older and patient able to answerIs there an answer marked to the
question, Do you have an Advance Directive? (NA if less than 18 years old)
4.05 If the patient has a resuscitative (code) status order in MIS is there a copy in the Red Page
Protector? (NA if patient is full code)
Were the following Initial screenings completed?
4.06 Learning (including barriers)
4.07 Pain
4.08 Function/Safety
4.09 Nutrition/Integumentary
4.10 Psychosocial (including abuse, neglect)
4.11 Discharge Factors and Family Strengths
5. NURSING ASSESSMENT (May be printout of electronic documentation)
Each section should show WDL, exceptions or score. Should be no NAs.
(Systems Assessment on admission and every 12 hours)
CHART:
Note the number of total number of assessments in the chart in this box.
5.01 Pain
5.02 CAM Screening complete
5.03 Neurological
5.04 Respiratory
5.05 Cardiovascular/PVS
5.06 Abdominal
5.07 Integumentary including location of lines, drains, tubes, wounds, pressure ulcers
5.08 Musculoskeletal/Mobility
5.09 Psychosocial including suicide assessment
5.10 Genitourinary
5.11 Braden Scale (completed with each assessment)
5.12 Fall Risk completed
5.13 Safety needs addressed, as appropriate
6. HAND-OFF OF CARE (HOC)
CHART:
1
Y N
2
Y N
3
Y N
4
Y N
Y N NA Y N NA Y N NA Y N NA
If patient transferred, documentation of hand-off includes: (NA if no transfer)
Note number of hand-off reports (last page with signatures) in chart (in progress notes)
6.01 Did the sending unit complete and sign the report and/or provide hand-off documentation on
the flow sheet?
6.02 Did the receiving unit complete and sign the report and/or provide hand-off documentation
on flow sheet?
6.03 If the patient returns to the sending unit (as from a test/procedure) is the hand-off report
completed by the receiving nurse and/or documentation on the flow sheet?
7. FLOWSHEET
(May be a print-out of electronic documentation)
CHART:
Note the total number of flowsheets in the chart.
For each flowsheet there should be documentation as below.
7.01 Was implementation of comfort plan initiated within 1 hour after pain identified and
assessed? (NA if no pain)
7.02 Pain Intervention was documented within 1 hour of pain score unacceptable to pt
(N/A if no pain or pain within pts comfort goal)
7.03 Were there clinical triggers noted that would indicate activation of the MET, PERT or NERT
team? (N/A if no clinical indication for a team)
7.04 Was the team activated? (See MET/PERT/NERT flowsheet) (N/A if no triggers)
Y N NA Y N NA Y N NA Y N NA
MEDICAL RECORD AUDIT TOOL
8. DAILY CARE PLAN
CHART:
Page 3 of 4
1
Note the total number of Care Plans
Y N NA Y N NA Y N NA Y N NA
8.01 Are general goals initiated or continued daily? Patient admitted to hospital
8.02 Are general goals initiated or continued daily? Patient admitted to hospital
8.03 If unique needs are identified, are corresponding interventions noted?
(NA if no unique needs)
8.04 If unique needs are identified, are corresponding interventions noted?
(NA if no unique needs)
9. PATIENT AND FAMILY EDUCATION
Nights
Days
Nights
Days
CHART:
Y N NA Y N NA Y N NA Y N NA
Patient/family/significant other are provided education specific to their needs, condition and care?
Note total number of education sessions.
When education was provided, did each session include each of the following?
9.01 Teaching is amended to address any learning barriersNoted in Comments.
(NA if no barriers.)
9.02 Learner
9.03 Method
9.04 Response
Documentation of topic taught during admission. Check any topics taught during admission:
9.05 General
9.06 Diagnosis/Illness/Injury
9.07 Before/after surgery/procedures/treatment
9.08 Safety
9.09 Activity/mobility
9.10 Self-care/ADLs
9.11 Pain management
9.12 Medications
9.13 Equipment/supplies
9.14 Diet/nutrition
9.15 Coping
9.16 Infection prevention and control
9.17 Wounds/lines/drains/airways
9.18 Discharge/followup
10. INTERDISCIPLINARY PATIENT CARE
PLANNING ROUNDS (Interdisciplinary Plan of Care,
CHART:
Social Work D/C Note, PTP, Therapy Notes/Discharge Plan)
10.01 Is there evidence of an individualized plan of care, treatment and services based on screening/
1
Y N
2
Y N
3
Y N
4
Y N
assessment that provides the opportunity to involve patients and families as appropriate?PS Goal 13
10.02 Was interdisciplinary discharge planning started within 48 hours of admission?
10.03 Coordination is noted among disciplines providing care, treatment, teaching and services.
11. OVERALL DOCUMENTATION All patient medical record entries must
be legible, complete, and authenticated (in written or electronic form) by the responsible
person, consistent with hospital policies and procedures. All documentation must have
CHART:
name/signature and/or PIC plus date/time.
11.01 Overall, does documentation meet this standard?
11.02 If there are any abbreviations, are they approved? Do not use U, IU, QD, QOD, MS,
MSO4, or MgS04
If NO is checked, note date/time/providers:
Y N
Y N
Y N
Y N
MEDICAL RECORD AUDIT TOOL
CLOSED CHART Nursing Review within 7 Days of Discharge
Page 4 of 4
12. DISCHARGE INFORMATION REVIEW FOUR CLOSED (POST-DISCHARGE) CHARTS WITHIN 7 DAYS OF DISCHARGE.
PLEASE AUDIT THE COMPLETE PAPER MEDICAL RECORD
9CHECK THE APPROPRIATE BOX, EITHER: 9Y = Yes 9N = No 9NA = Not Applicable
Unit:
CHART 1
CHART 2
CHART 3
CHART 4
Medical Record Number:
Admit Date:
Audit Date:
Reviewer(s):
(Progress Notes, SW D/C Note, D/C Instructions, Therapy Notes, Home Health Referral, CHART:
1
2
3
4
MD Discharge Summary)
Y N NA Y N NA Y N NA Y N NA
12.01 Was the patient/family given information about discharge including (as applicable):
reason, how to obtain further care, treatment and services to meet his/her needs;
pain management plan?
12.02 If applicable, did the hospital help arrange for services to meet the patients needs after
discharge? (NA if no services needed)
12.03 Was a list of medicines provided to the patient/family?
12.04 Were discharge instructions and other teaching tools given to the patient/family and did the
patient/family demonstrate understanding?
12.05 If patient does not speak English was an interpreter (live or phone) used to provide instructions?
(NA if patient spoke English)
12.06 If applicable, was patient given choice of services/agencies? (NA if no services offered)
If the patient was discharged to a facility or home with home health, clinical information was provided
including: (NA if standard discharge to home)
12.07 Reason for discharge, physical, and psychosocial status.
12.08 A summary of care, treatment, and services provided and progress toward goals.
12.09 Community resources or referrals or other specific needs after discharge
FOR PATIENTS LESS THAN 18 YEARS OLD
13. PEDIATRIC CARE ASSESSMENT ADDENDUM
CHART:
For children (under 18 years)
Does the assessment of infants, children and adolescents include?
13.02 Length/height
13.03 Weight
13.04 Immunization status
13.05 If applicable, newborn care (NA if not newborn)
13.06 Are the specific academic educational needs of the child or youth identified
and implemented?
13.07 Are family/guardian expectations for and involvement in the assessment, initial treatment,
and continuing care of the patient documented?
RELATED MEDICAL CENTER POLICIES
0125 Diagnostic Testing
0129 Hospital Education
0146 Blood Use
0153 Conscious Sedation
0159 Restraints
0197 Suicide Precautions
0213 Abuse & Neglect
Y N NA Y N NA Y N NA Y N NA
13.01 Developmental age
0024 Consent
0025 Discharge Planning
0026 Pt Rights & Responsibilities
0063 Inpatient Transfers
0091 Infection Control & Prevention
0094 Documentation
0097 Bed Assignment
0239 Pain
0259 Medications
0965 Emergency Response
0269 Patient Education
CCS Documentation Guidelines
Vous aimerez peut-être aussi
- Quality IndicatorsDocument10 pagesQuality IndicatorsKanna NikithaPas encore d'évaluation
- Medical Record Review FormDocument3 pagesMedical Record Review FormSimon Dzokoto100% (1)
- Quality and Patient Safety ChecklistDocument7 pagesQuality and Patient Safety ChecklistKarl Roble100% (4)
- Republic of The Philippines Department of Health Southern Isabela Medical CenterDocument5 pagesRepublic of The Philippines Department of Health Southern Isabela Medical Centerkrull243100% (3)
- Medical Records Audit ChecklistDocument2 pagesMedical Records Audit ChecklistAmbika Ghosh50% (2)
- Medical Case Sheet AuditDocument2 pagesMedical Case Sheet AuditSrinivas PolikepatiPas encore d'évaluation
- CLINICAL & MANAGERIAL KPIsDocument71 pagesCLINICAL & MANAGERIAL KPIsNatasha Bhasin100% (1)
- Medical Records Audit ChecklistDocument2 pagesMedical Records Audit ChecklistSrinivas Polikepati93% (42)
- Checklist For Hospital For Data CollectionDocument8 pagesChecklist For Hospital For Data CollectionMuhammad Nadeem NasirPas encore d'évaluation
- Quality Indicators 5th Edition WordDocument14 pagesQuality Indicators 5th Edition Wordtanisha100% (1)
- Nabh IdicatorsDocument61 pagesNabh IdicatorsStacy King100% (5)
- Checklist of Quality Indicators For NABH Accreditation PreparationDocument11 pagesChecklist of Quality Indicators For NABH Accreditation PreparationQUALITY SIDARTH HOSPITALSPas encore d'évaluation
- Cqi Indicators As Per Nabh 4Th Edition: S. No. Standard Ref. Deptt. KPI Formula FrequencyDocument6 pagesCqi Indicators As Per Nabh 4Th Edition: S. No. Standard Ref. Deptt. KPI Formula FrequencyNatasha BhasinPas encore d'évaluation
- Antibiotics Audit ChecklistDocument1 pageAntibiotics Audit ChecklistPrabhat Kumar100% (1)
- CSSD Audit ChecklistDocument3 pagesCSSD Audit Checklistaaminah tariq100% (3)
- Gap Analysis Report For Health Care Organnization (Hco) Hospital ProfileDocument7 pagesGap Analysis Report For Health Care Organnization (Hco) Hospital ProfileDhananjay SainiPas encore d'évaluation
- Checklist of Training Topics (Department Wise) : Top Management Training Topic Coverage Relevant ToDocument14 pagesChecklist of Training Topics (Department Wise) : Top Management Training Topic Coverage Relevant ToEka B67% (3)
- MRD Checklist: All Patient Sr. No. IPD ResponsibilitiesDocument1 pageMRD Checklist: All Patient Sr. No. IPD Responsibilitiesamit100% (4)
- Chapter-PSQ PSQ 1Document6 pagesChapter-PSQ PSQ 1balaji srinivasanPas encore d'évaluation
- NABH Traing Schedule 2Document7 pagesNABH Traing Schedule 2umeshbharti100% (1)
- Crash Cart AuditDocument1 pageCrash Cart AuditGAGANJOT85100% (1)
- 2019 Audit ChecklistDocument27 pages2019 Audit ChecklistChhaiyaAgrawalPas encore d'évaluation
- Emergency Department Crowd ManagementDocument4 pagesEmergency Department Crowd ManagementPrabhat Kumar100% (1)
- NABH QI ListDocument9 pagesNABH QI ListMangesh VirkarPas encore d'évaluation
- Audit ChecklistsDocument24 pagesAudit ChecklistsPrabhat Kumar92% (24)
- Jciinternalauditchecklist 160510164212Document14 pagesJciinternalauditchecklist 160510164212Edmund Yoong75% (4)
- MSDSDocument11 pagesMSDSPrabhat Kumar100% (1)
- 1 Procedure(s) Guide Collection, Identification, Handling, Safe Transportation, Processing and Disposal of Specimens.Document10 pages1 Procedure(s) Guide Collection, Identification, Handling, Safe Transportation, Processing and Disposal of Specimens.Sanjay KadamPas encore d'évaluation
- Er ManualDocument27 pagesEr ManualQuality Manager100% (2)
- 3.checklist of Documents For NABH Accreditation PreparationDocument4 pages3.checklist of Documents For NABH Accreditation PreparationSantosh JSE100% (3)
- ICN Nurse Job ResponsibilitiesDocument2 pagesICN Nurse Job ResponsibilitiesBirupakshya RoutPas encore d'évaluation
- Hospital Daily Monitoring - ChecklistDocument3 pagesHospital Daily Monitoring - Checklistammy_75100% (3)
- 1.checklist of Quality Indicators For NABH Accreditation PreparationDocument13 pages1.checklist of Quality Indicators For NABH Accreditation PreparationSantosh JSE100% (3)
- Mahatma Gandhi Mission Hospital: Facility Rounds ReportDocument3 pagesMahatma Gandhi Mission Hospital: Facility Rounds ReportJeevan DasmsPas encore d'évaluation
- Medical Records Department PlanningDocument4 pagesMedical Records Department PlanningSrinivas PolikepatiPas encore d'évaluation
- Nursing ICUDocument2 pagesNursing ICUKomal Tomar50% (2)
- Hic ManualDocument260 pagesHic ManualVamshi Narean Naidu100% (3)
- 2.checklist of Training Topics For NABH Accreditation PreparationDocument5 pages2.checklist of Training Topics For NABH Accreditation PreparationSantosh JSE100% (1)
- MRD ProtocolDocument27 pagesMRD ProtocolVarun Marar67% (3)
- NABH AdvantageDocument19 pagesNABH Advantagedr_vikasPas encore d'évaluation
- Clinical Audit Topics SampleDocument3 pagesClinical Audit Topics Samplebalaji srinivasanPas encore d'évaluation
- Prescription Audit ExcerciseDocument4 pagesPrescription Audit Excerciseharshananda100% (1)
- Patient SafetyDocument4 pagesPatient Safetystella rose fidelPas encore d'évaluation
- Crowd Management PolicyDocument3 pagesCrowd Management PolicyAffan sami rayeenPas encore d'évaluation
- Nursing ChecklistDocument6 pagesNursing Checklistbalaji srinivasan95% (20)
- The Healthcare Quality Book: Vision, Strategy, and Tools, Fourth EditionD'EverandThe Healthcare Quality Book: Vision, Strategy, and Tools, Fourth EditionÉvaluation : 3.5 sur 5 étoiles3.5/5 (2)
- Nursing Clinical Privileges Department: ICU /NICU /LRDocument3 pagesNursing Clinical Privileges Department: ICU /NICU /LRKUMARJIT SAHA100% (2)
- NABH Training Calendar 2020Document6 pagesNABH Training Calendar 2020balaji srinivasan100% (3)
- NABH ChecklistDocument3 pagesNABH ChecklistMargretSnehaPas encore d'évaluation
- INDICATORSDocument15 pagesINDICATORSMonish ParmarPas encore d'évaluation
- Deficiencies Observed During Pre-Assessment - Paf 2 Hospital (Full Accreditation) : Date(s) of VisitDocument8 pagesDeficiencies Observed During Pre-Assessment - Paf 2 Hospital (Full Accreditation) : Date(s) of Visitpranit mPas encore d'évaluation
- Manual Medical Records NabhDocument21 pagesManual Medical Records NabhSadaf SadafPas encore d'évaluation
- Nabh FormDocument14 pagesNabh Formakshay ranePas encore d'évaluation
- Job Description Accreditation Co-OrdinatorDocument2 pagesJob Description Accreditation Co-OrdinatorBirupakshya RoutPas encore d'évaluation
- Hospital Infection Control ManualDocument59 pagesHospital Infection Control Manualdhir.ankurPas encore d'évaluation
- Checklist For NABHDocument1 615 pagesChecklist For NABHShivani Rawat10% (10)
- In Patient Wardrs ChecklistDocument4 pagesIn Patient Wardrs ChecklistDnyanesh AitalwadPas encore d'évaluation
- MRD ChecklistDocument3 pagesMRD ChecklistSrinivas Polikepati83% (6)
- Multiple Choice Questions in Healthcare QualityD'EverandMultiple Choice Questions in Healthcare QualityÉvaluation : 4 sur 5 étoiles4/5 (8)
- Applying Quality Management in Healthcare: A Systems Approach, Fifth EditionD'EverandApplying Quality Management in Healthcare: A Systems Approach, Fifth EditionPas encore d'évaluation
- A Report On How To Stay HealthyDocument3 pagesA Report On How To Stay HealthyTharsmilaRamooPas encore d'évaluation
- SCI135 Research Project - EditedDocument4 pagesSCI135 Research Project - EditedRachael KaburuPas encore d'évaluation
- Healing by Design - Healing Gardens and Therapeutic Landscapes PDFDocument12 pagesHealing by Design - Healing Gardens and Therapeutic Landscapes PDFdumitras adelinaPas encore d'évaluation
- Alcohol Misuse: Screening and Behavioral Counseling Interventions in Primary Care GuidelinesDocument11 pagesAlcohol Misuse: Screening and Behavioral Counseling Interventions in Primary Care GuidelinesRosnerPas encore d'évaluation
- Romeo Victor M. Valderrama BSN-2A: CNS: Confusion, Depression, BeforeDocument8 pagesRomeo Victor M. Valderrama BSN-2A: CNS: Confusion, Depression, BeforeitsmeayaPas encore d'évaluation
- Early SensoryDocument6 pagesEarly SensorySteven FlynnPas encore d'évaluation
- Acute Poststreptococcal Glomerulonephritis An UpdateDocument6 pagesAcute Poststreptococcal Glomerulonephritis An UpdateJuan Antonio Herrera LealPas encore d'évaluation
- Root Canal DisinfectionDocument4 pagesRoot Canal DisinfectionKarizma TravelPas encore d'évaluation
- The Manchurian ApproachDocument2 pagesThe Manchurian ApproachArtist Metu20% (5)
- Creative JournalDocument28 pagesCreative Journalevelui02100% (1)
- Beetroot 2 PDFDocument4 pagesBeetroot 2 PDFNatasya PermataPas encore d'évaluation
- Awaken The Healer EbookDocument172 pagesAwaken The Healer Ebookrichlohdee86% (7)
- Reverse AbdominoplastyDocument3 pagesReverse AbdominoplastyongchenguanPas encore d'évaluation
- MeaslesDocument2 pagesMeaslesHari SusetyoPas encore d'évaluation
- Rebt DepressionDocument31 pagesRebt DepressionAlina Macavei100% (1)
- Otorhinolaryngology: Therapeutic Approach To Pediatric Acute Mastoiditis - An UpdateDocument9 pagesOtorhinolaryngology: Therapeutic Approach To Pediatric Acute Mastoiditis - An UpdateImelda LiePas encore d'évaluation
- Alexanders Discipline A Simple DecisionDocument150 pagesAlexanders Discipline A Simple Decisionsilviaa50% (2)
- Patho SGDDocument2 pagesPatho SGDAnna Patricia DugayPas encore d'évaluation
- Expression of Interest Build For Cancer Care Centre - 2Document5 pagesExpression of Interest Build For Cancer Care Centre - 2arakbaePas encore d'évaluation
- The Progestins All SimilarDocument23 pagesThe Progestins All SimilarVladimir KljajevicPas encore d'évaluation
- To, Ms. Sunayana Vikhe College of Pharmacy Pravara Nagar Dist. A' NagarDocument6 pagesTo, Ms. Sunayana Vikhe College of Pharmacy Pravara Nagar Dist. A' NagarSunayana VikhePas encore d'évaluation
- B32C08 Lab Report ProformaDocument13 pagesB32C08 Lab Report Proformajtoh22Pas encore d'évaluation
- Satir Family Therapy: Instructor's ManualDocument50 pagesSatir Family Therapy: Instructor's ManualDragana ĆorićPas encore d'évaluation
- Daftar Pustaka Sken 4Document4 pagesDaftar Pustaka Sken 4Allisya CarissaPas encore d'évaluation
- What Causes Pain Behind The KneeDocument7 pagesWhat Causes Pain Behind The KneeRatnaPrasadNalamPas encore d'évaluation
- IsoketDocument2 pagesIsoketGuinzaPas encore d'évaluation
- Tapping Out Trauma, Stress & Fear... Tap Into Success.: With Thought Field TherapyDocument16 pagesTapping Out Trauma, Stress & Fear... Tap Into Success.: With Thought Field TherapyRonny Deer100% (1)
- PrednisoloneDocument4 pagesPrednisoloneUmemura-san SOkmo100% (1)
- Hildegard Peplau's Theory of Interpersonal RelationsDocument20 pagesHildegard Peplau's Theory of Interpersonal RelationsSofie May Nellas100% (2)
- Sleep HygieneDocument1 pageSleep HygieneJosé Carlos FarroPas encore d'évaluation