Académique Documents
Professionnel Documents
Culture Documents
Tumor Necrosis Factor (TNF-α) and C-reactive Protein (CRP) are Positively Associated with the Risk of Chronic Kidney Disease in Patients with Type 2 Diabetes
Transféré par
Tea AgungTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Tumor Necrosis Factor (TNF-α) and C-reactive Protein (CRP) are Positively Associated with the Risk of Chronic Kidney Disease in Patients with Type 2 Diabetes
Transféré par
Tea AgungDroits d'auteur :
Formats disponibles
Original Article
DOI 10.3349/ymj.2010.51.4.519
pISSN: 0513-5796, eISSN: 1976-2437
Yonsei Med J 51(4):519-525, 2010
Tumor Necrosis Factor (TNF-) and C-reactive Protein
(CRP) are Positively Associated with the Risk of Chronic
Kidney Disease in Patients with Type 2 Diabetes
Eun-Sil Yeo,1* Ji-Yun Hwang,1* Ji Eun Park,1 Young Ju Choi,2 Kap Bum Huh,2 and Wha Young Kim1
1
Department of Nutritional Science and Food Management, Ewha Womans University, Seoul;
2
Huhs Diabetes Clinic & the 21C Diabetes and Vascular Research Institute, Seoul, Korea.
Received: August 5, 2009
Revised: September 17, 2009
Accepted: September 17, 2009
Corresponding author: Dr. Kap Bum Huh,
Huhs Diabetes Clinic & the 21C Diabetes and
Vascular Research Institute, 40-9 NogosanDong, Mapo-Gu, Seoul 121-806, Korea.
Tel: 82-2-718-1827, Fax: 82-2-704-5750
E-mail: huh7181827@hanmail.net and
Dr. Wha Young Kim,
Department of Nutritional Science and Food
Management, Ewha Womans University,
11-1 Daehyeon-dong, Seodaemun-gu,
Seoul 120-750, Korea.
Tel: 82-2-3277-3093, Fax: 82-2-3277-3103
E-mail: wykim@ewha.ac.kr
*These authors contributed equally to this
work.
The authors have no financial conflicts of
interest.
Purpose: Chronic low-grade inflammation may induce chronic kidney disease in
patients with type 2 diabetes. This study investigated the relation between
inflammatory biomarkers and chronic kidney disease in patients with type 2
diabetes, which has not yet been reported in Asian populations. Materials and
Methods: A cross-sectional study was performed in 543 patients recruited from
diabetic clinics for an ongoing, prospective study. Multivariate logistic regression
was used to evaluate the association between inflammatory biomarkers and the
presence of chronic kidney disease (estimated glomerular filtration rate < 60
mL/min per 1.73 m2 by the simplified Modification of Diet in Renal Disease
equation using plasma creatinine). Results: The risk of chronic kidney disease
increased in the highest quartiles of C-reactive protein (CRP) [multivariate odds
ratio (OR) = 3.73; 95% CI = 1.19-1.70] and tumor necrosis factor- (multivariate
OR = 4.45; 95% CI = 1.63-12.11) compared to the lowest quartiles after adjustments for age, sex, zinc intake, and other putative risk factors for chronic kidney
disease. Conclusion: Our results suggest that CRP and tumor necrosis factor-
may be independent risk factors for chronic kidney disease in patients with type 2
diabetes. A causal mechanism of this association should be evaluated in a followup study of Korean patients with type 2 diabetes.
Key Words: Type 2 diabetes, chronic kidney disease, inflammation, tumor
necrosis factor-, C-reactive protein
INTRODUCTION
Copyright:
Yonsei University College of Medicine 2010
This is an Open Access article distributed under the
terms of the Creative Commons Attribution NonCommercial License (http://creativecommons.org/
licenses/by-nc/3.0) which permits unrestricted noncommercial use, distribution, and reproduction in any
medium, provided the original work is properly cited.
The prevalence of type 2 diabetes has been rapidly rising worldwide. In Korea,
the prevalence of diabetes (95% of which were cases of type 2 diabetes) has increased from 1% of the general population in the 1970s to 13.5% of men and 10.7%
of women aged 30 years or more in 2000.1 Chronic kidney disease (CKD) is one
of the major complications of type 2 diabetes, and is the leading cause of endstage renal disease (ESRD), accounting for approximately 40% of new cases of
ESRD every year.2 Early detection and treatment of CKD in patients with type 2
diabetes can prevent or retard the progression to ESRD.
Several studies have reported positive associations between inflammatory
biomarkers and ESRD3-5 or advanced kidney failure.6 However, few studies have
Yonsei Med J http://www.eymj.org Volume 51 Number 4 July 2010
519
Eun-Sil Yeo, et al.
provided information on the relation between inflammation
and mild to moderate CKD. And to the best of our knowledge, only two studies have been performed in patients
with type 2 diabetes7,8 and no study has been performed in
Asian patients with type 2 diabetes. Type 2 diabetes is considered a chronic inflammatory condition resulting from
obesity-induced dysregulation of adipocytes, which produce
excessive inflammatory cytokines such as tumor necrosis
factor (TNF-), interleukin-6 (IL-6), and C-reactive protein
(CRP).9 This persistent inflammatory state further contributes to insulin resistance10 and abnormal endothelial vascular reactivity.11 Chronic inflammation exacerbates kidney
damage through mechanisms of vascular endothelial cell
impairments. On the other hand, adiponectin, secreted by
adipose tissue, is considered to be an important modulator of
insulin sensitivity and its concentration is reduced in patients
with type 2 diabetes and CKD, suggesting its various
protective functions as an anti-diabetic and anti-inflammatory factor.8,12 Previous studies, however, did not include
both inflammatory and anti-inflammatory biomarkers. In
addition, no attempt to assess dietary intake, which is an
important risk factor for both type 2 diabetes and CKD,2,13
was made in the aforementioned studies.
Therefore, the objective of the present study was to examine the relation between the risk of CKD and inflammatory (TNF-, IL-6, and CRP) and anti-inflammatory
(adiponectin) biomarkers in patients with type 2 diabetes.
Our hypothesis was that an inflammatory biomarker would
be positively associated and an anti-inflammatory biomarker negatively associated with the risk of CKD in patients
with type 2 diabetes.
MATERIALS AND METHODS
Study subjects
All participants were patients with type 2 diabetes who
visited one of two diabetes clinics in Seoul, Korea. For an
ongoing, prospective study of patients with type 2 diabetes,
847 subjects (439 men and 408 women, aged 40-85 years),
without coronary heart disease or cerebrovascular disease,
were randomly selected and interviewed for a baseline
investigation from September 2005 to September 2007. In
the baseline sample, 196 subjects were excluded because
no data were available on their plasma creatinine (n = 131),
body mass index (BMI) (n = 3), or dietary intake (n = 62).
Among the remaining 651 subjects, 27 were excluded due
to insufficient information on their blood parameters, and a
further 81 were excluded as a result of fasting blood glucose < 126 mg/dL or hemoglobin A1C (HbA1C) < 6.5%.
Therefore, a total of 543 Korean patients with type 2 diabetes (284 men and 259 women; aged 40-85 years) were
520
ultimately eligible for this analysis. Written informed consent to participate was obtained from each individual. The
study protocol was approved by the Institutional Review
Board of Yonsei University.
General characteristics, anthropometric
measurements, and blood pressure
All subjects were individually interviewed to obtain information about general characteristics such as age as well as
life-style behaviors such as smoking (non-, ex-, or current-)
and regular exercise (yes/no). The duration of diagnosed
type 2 diabetes, calculated by subtracting the year of
diagnosis from the year of baseline survey, was obtained
from a review of the medical record or was self-reported
with the help of an attending endocrinologist. For anthropometric measurements, height was measured with a standiometer (Seca Inc., Hamburg, Germany) attached to a wall,
weight was assessed using Inbody 4.0 (Biospace Co., Seoul,
Korea), and BMI (kg/m2) was calculated. Waist circumference was measured with a tapeline (Tanita, Seoul, Korea).
Systolic and diastolic blood pressures were measured after
the patients had rested for 10 min in a sitting position,
using an automatic blood pressure monitor (Biospace Co.,
Seoul, Korea), and were read by the attending endocrinologists. Hypertension was defined as a systolic blood pressure (SBP) > 140 mmHG, a diastolic blood pressure (DBP)
> 90 mmHG, or as taking hypertension medication.
Dietary intake
Graduate students trained in nutrition individually interviewed each subject to assess their food consumption for
the past year, using a food frequency questionnaire, which
included 114 food items and had been previously validated.14 The food intake data were analyzed using Can-Pro 3.0
software (Korean Nutrition Society, Seoul, Korea) to determine nutrient intakes for energy, fat, zinc, vitamin A,
vitamin C, vitamin E, and folate, and were compared to the
Dietary Reference Intakes for Koreans.15
Biochemical analysis
Blood samples were taken after a minimum 12-hour overnight fast, collected in EDTA-containing tubes, and centrifuged at 3,000 rpm for 20 minutes at 4C (Hanil Science
Industrial Co., Ltd, Seoul, Korea). The plasma samples
were stored at -80C until analysis. Fasting serum levels of
glucose, cholesterol, triglyceride, high-density lipoprotein
(HDL)-cholesterol, albumin, creatinine, and blood urea
nitrogen (BUN) were measured using an autoanalyzer
(Cobas Mira Roche Autoanalyzer, Hoffmann-La Roche
Ltd., Basel, Switzerland). Low-density lipoprotein (LDL)cholesterol and the atherogenic index (AI) were calculated
by employing the following equations described by Frie-
Yonsei Med J http://www.eymj.org Volume 51 Number 4 July 2010
TNF-, CRP, and Chronic Kidney Disease
dewald16 and Lauer17: LDL-cholesterol = Total cholesterol
- HDL-cholesterol-(Triglyceride/5) and AI = (Total cholesterol - HDL-cholesterol)/HDL-cholesterol, respectively.
HbA1C was measured by an HLC-723 G7 analyzer (Toche,
Japan). Serum IL-6, TNF-, and adiponectin concentrations were determined using enzyme linked immunosorbent assay kits (Quantikine, R & D Systems Inc., Minneapolis, MN, USA) according to the manufacturers instructions, and were read by an ELISA reader (Spectra Max
340, Molecular Devices, Sunnyvale, CA, USA). The measurement of malonialdehyde, a biomarker of antioxidant
status, was performed using a Lipid Peroxidation Assay kit
(Oxford Biomedical Research, Oxford, MI, USA) according to the manufacturers instructions.
Assessment of renal function
The estimation of glomerular filteration rate (GFR) using
serum creatinine concentrations is utilized as an index of
kidney function and is examined in patients with type 2
diabetes to assess for CKD. In the present study, renal
function was estimated by the simplified Modification of
Diet in Renal Disease equation, where GFR (mL/min per
1.73 m2) = 186.3[(serum creatinine, mg/dL)-1.154(age)-0.203]
0.742 (if female). The subjects were classified into a
normal kidney function group (GFR 60 mL/min per 1.73
m2) and a CKD group (GFR < 60 mL/min per 1.73 m2).18
Statistical analysis
The data were expressed as means with standard errors (adjusted for age and sex) or numbers and percentages. Variables with skewed distributions were log-transformed before
analysis and back-transformed for presenting within tables.
The differences between subjects with and without CKD
were evaluated using an analysis of covariance (ANCOVA)
2
test after adjustments for age and sex, or a
test, as appropriate. To investigate the correlations between blood
glucose indicators and inflammatory markers, a partial
correlation analysis controlling for age and sex was performed. Multivariable-adjusted logistic analysis was conducted to examine the odds ratio (OR) for CKD across
Table 1. General Characteristics and Nutrient Intakes of Study Groups
Normal
Subjects
488 (89.8)
Female (%)
231 (47.3)
Age (yrs)
56.1 0.46
Duration of diagnosed type 2 diabetes (yrs)
8.4 0.32
BMI (kg/m2)
24.6 0.14
Waist circumference (cm)
85.6 0.60
Hypertension
243 (49.7)
Regular exercise
281 (58.1)
Cigarette smoking
Non-smoker
282 (57.8)
Ex-smoker
121 (24.8)
Current smoker
85 (17.4)
Nutrient intake
Energy (kcal)
2,127.1 36.60
Fat (g)
58.7 1.56
Zinc (mg)
11.8 0.25
% below estimated average requirement
52 (10.7)
Vitamin A (gRE)
1,058.6 28.64
% below estimated average requirement
60 (12.3)
Vitamin C (mg)
143.2 3.62
% below estimated average requirement
81 (16.6)
Folate (g)
355.3 7.17
% below estimated average requirement
218 (44.7)
Vitamin E (mg)
17.5 0.47
% below estimated average requirement
73 (23.2)
CKD
55 (10.2)
28 (50.9)
64.6 1.37
11.1 0.97
24.2 0.43
87.9 1.83
35 (63.6)
34 (54.9)
p value
0.021
< 0.001
0.008
0.484
0.254
0.064
0.885
33 (60.0)
10 (18.1)
12 (21.9)
0.479
2,037.7 111.71
62.4 4.76
11.8 0.75
12 (21.8)
1,047.0 87.43
8 (14.5)
132.3 11.06
8 (14.5)
322.9 21.89
31 (56.4)
17.3 1.44
16 (29.1)
0.449
0.455
0.974
0.025
0.900
0.666
0.347
0.347
0.162
0.116
0.860
0.206
CKD, chronic kidney disease; BMI, body mass index.
Values are means SE or n (%). Continuous values were adjusted for age and sex, except for age.
Yonsei Med J http://www.eymj.org Volume 51 Number 4 July 2010
521
Eun-Sil Yeo, et al.
levels of inflammatory biomarkers continuously as well as
across quartiles of them. The first model was adjusted for
age and sex. The second model was additionally adjusted
for the duration of diagnosed type 2 diabetes, smoking,
regular exercise, hypertension, fasting blood sugar, and zinc
intake. All analyses were performed using SPSS version
12.0 software (SPSS Inc., Chicago, IL, USA). Statistical
significance was defined as p < 0.05.
RESULTS
The general characteristics and nutrient intakes of the 543
subjects with type 2 diabetes are presented in Table 1. Of
these 543 patients, 488 (89.8%) were considered to have
normal kidney function and 55 (10.2%) had CKD. It was
found that the type 2 diabetes patients with CKD were
more likely to be female (p = 0.021), were older (p < 0.001),
had a longer duration of type 2 diabetes (p = 0.008), and
were more likely to have zinc intakes less than the estimated
average requirement (p = 0.025).
For clinical characteristics, levels of GFR were lower (p
< 0.001) and levels of creatinine (p < 0.001) and BUN (p <
0.001) higher in the subjects with CKD compared to those
with normal kidney function (Table 2). Mean concentrations of fasting blood sugar were also greater in the patients with CKD (p = 0.014). In addition, the subjects with
CKD had greater levels of inflammatory biomarkers such
Table 2. Clinical Characteristics of Subjects According to Kidney Function
Normal (n = 488)
CKD (n = 55)
Kidney function
GFR (mL/min/1.73 m2)
98.1 1.41
59.5 4.30
Creatinine (mg/dL)
0.8 0.18
1.5 0.056
Blood urea nitrogen (mg/dL)
15.5 0.21
21.0 0.63
Serum albumin (g/dL)
4.4 0.20
4.3 0.60
Glucose control
Fasting blood sugar (mg/dL)
166.7 2.48
186.4 7.56
Hemoglobin A1C (%)
8.4 1.84
8.6 1.90
Blood lipids
Triglyceride (mg/dL)
142.2 3.82
158.1 11.62
Total cholesterol (mg/dL)
189.5 1.80
192.7 5.49
HDL-cholesterol (mg/dL)
49.7 0.61
47.8 1.87
LDL-cholesterol (mg/dL)
111.4 1.61
113.3 4.93
Atherogenic index
3.0 0.06
3.2 0.17
Malondialdehyde (M/L)
2.7 0.13
2.6 0.369
Inflammatory biomarkers
C-reactive protein (mg/dL)
2.1 0.34
5.0 1.12
Tumor necrosis factor- (pg/mL)
1.1 0.31
1.5 0.95
Interleukin-6 (pg/mL)
1.8 0.11
2.3 0.35
Adiponectin (g/mL)
5.9 0.24
7.9 0.74
p value
< 0.001
< 0.001
< 0.001
0.907
0.014
0.705
0.196
0.584
0.339
0.719
0.377
0.924
0.013
< 0.001
0.158
0.008
CKD, chronic kidney disease; GFR, glomerula filteration rate; HDL, high-density lipoprotein; LDL, low-density lipoprotein.
Values are means SE or n (%). Continuous values were adjusted for age and sex.
Table 3. Partial Correlation Coefficients between Indicators of Blood Glucose and Inflammatory Biomarkers
According to Kidney Function
Tumor necrosis
C-reactive protein
Interleukin-6
Adiponectin
factor-
Normal CKD Normal CKD Normal CKD Normal CKD
Fasting blood sugar 0.069
0.403
0.018
0.408
0.004
0.512*
0.026
- 0.111
HbA1C
0.037
0.453*
0.109
0.458*
0.096
0.452*
0.055
- 0.113
CKD, chronic kidney disease; HbA1C, hemoglobin A1C.
Adjusted for age and sex.
*p < 0.01.
p < 0.05 significant by partial correlation analysis.
522
Yonsei Med J http://www.eymj.org Volume 51 Number 4 July 2010
TNF-, CRP, and Chronic Kidney Disease
Table 4. Multivariable Logistic Regression Odds Ratios (OR) for an Outcome of Calculated GFR < 60 mL/min Per 1.73 m2 for
Continuous Values and for Quartile Groups of Blood Inflammatory Biomarkers
Continuous values
Quartile groups
OR ( 95%CI ) P-for-trend Q1
Q2
Q3
Q4
P-for-trend
C-reactive protein
Model 1
1.04 (1.01 - 1.07)
0.010
1 2.16 (0.99 - 1.07) 1.65 (0.99 - 1.07) 3.68 (1.77 - 10.75) 0.014
Model 2
1.04 (1.01 - 1.08)
0.013
1 2.57 (0.78 - 8.50) 2.02 (0.59 - 6.94) 3.73 (1.19 - 11.70) 0.029
Tumor necrosis factor-
Model 1
1.82 (1.32 - 2.53) < 0.001
1 1.36 (0.47 - 3.90) 1.80 (0.63 - 5.05) 3.78 (1.45 - 9.84)
0.002
Model 2
1.89 (1.33 - 2.67) < 0.001
1 1.32 (0.44 - 3.96) 2.36 (0.81 - 6.93) 4.45 (1.63 - 12.11) 0.001
Interleukin-6
Model 1
1.03 (0.91 - 1.17)
0.148
1 1.14 (0.44 - 2.96) 1.39 (0.53 - 3.70) 1.49 (0.60 - 3.70)
0.195
Model 2
1.06 (0.96 - 1.18)
0.231
1 1.06 (0.40 - 2.80) 1.30 (0.49 - 3.44) 1.18 (0.45 - 3.09)
0.484
Adiponectin
Model 1
1.05 (0.98 - 1.10)
0.008
1 1.68 (0.64 - 4.41) 1.14 (0.41 - 3.83) 2.26 (0.88 - 5.85)
0.122
Model 2
1.06 (1.01 - 1.11)
0.005
1 1.63 (0.58 - 4.60) 1.31 (0.50 - 3.83) 2.61 (0.95 - 7.16)
0.065
Model 1 is adjusted age and sex.
Model 2 is adjusted for age (continuous, yrs), sex (male/female), duration of diagnosed type 2 diabetes (continuous, yrs), cigarette smoking status (never, past, and
current), regular exercise (yes/no), hypertension (yes/no), fasting blood sugar (quartile groups), and zinc intake (below estimated average requirement: yes/no).
as CRP (p = 0.013) and TNF- (p < 0.001), as expected,
but they also had higher levels of the anti-inflammatory
biomarker adiponectin (p = 0.008) than the normal subjects, contrary to our expectation. No differences were
found in serum albumin, HbA1C, blood lipid levels, and
IL-6 between the two groups.
Elevated blood glucose levels in patients with type 2
diabetes can affect concentrations of inflammatory biomarkers. Partial correlation analysis revealed a significantly
positive correlation between blood glucose indicators and
inflammatory biomarkers (Table 3). CRP, TNF-, and IL6 were significantly positively correlated with fasting blood
sugar and HbA1C. Such a correlation did not exist for adiponectin.
The overall results relating plasma levels of inflammatory biomarkers to the risk of CKD are shown in Table 4.
The OR for CKD was positively associated with continuous values of CRP (OR = 1.04, 95% CI = 1.01-1.07; p =
0.010) and TNF- (OR = 1.82, 95% CI = 1.32-2.53; p <
0.001) after adjustments for age and sex. The association
did not change after further adjustments for duration of
type 2 diabetes, smoking, exercise, hypertension, fasting
blood sugar, and zinc intake. For quartiles of these
biomarkers, a positive association existed between CKD
risk and CRP (OR = 3.68, 95% CI = 1.77-10.75; p = 0.014)
and TNF- (OR = 3.78, 95% CI = 1.45-9.84; p = 0.002)
across the lowest to highest quartiles. Furthermore, these
trends did not change after adjusting other confounders
(OR = 3.73, 95% CI = 1.19-11.70; p = 0.029 for CRP and
OR = 4.45, 95% CI = 1.63-12.11; p = 0.001 for TNF-).
The OR for CKD tended to slightly increase with conti-
nuous values of adiponetin (OR = 1.06, 95% CI = 1.011.11; p = 0.005), but this trend disappeared when the
values were treated as quartiles.
DISCUSSION
From our data we found a strong and graded association
between CRP and TNF- and the risk of CKD in Korean
patients with type 2 diabetes. Plasma concentrations of
CRP and TNF- were significantly higher in subjects with
CKD compared to those without CKD, and the risk of
CKD was > 3-fold greater from the lowest to highest quartiles of CRP and TNF-, respectively. This association
appeared to be independent of other well-known putative
risk factors for CKD such as age, sex, duration of diagnosed
type 2 diabetes, smoking, exercise, having hypertension,
fasting blood sugar concentrations, and zinc intake, based
on multivariable-adjusted logistic analysis. Our results
suggest that high concentrations of CRP and TNF- may
be an independent risk factor for CKD in Korean patients
with type 2 diabetes.
Our findings are consistent with previously reported
results. In cross-sectional analyses from the Health Professionals Follow-Up Study of U.S. male patients with type
2 diabetes aged 40-75 years, soluble tumor necrosis factor
receptor type 2 was positively associated with the risk of
CKD (GFR < 60 mL/min per 1.73 m2).7 In a cross-sectional
study of 23 dialyzed and 16 non-dialyzed chronic renal
failure patients and 28 healthy controls in England, concentrations of CRP and TNF- were elevated in patients
Yonsei Med J http://www.eymj.org Volume 51 Number 4 July 2010
523
Eun-Sil Yeo, et al.
with chronic renal failure as compared to the controls.19
Also shown in a previous study,8 serum adiponectin concentrations were greater in patients with CKD than in
patients with normal kidney function.
Nonetheless, some studies have shown incompatible
results. Among the U.S. male patients with type 2 diabetes
from the Health Professionals Follow-Up Study, no
relation existed between CRP levels and CKD risk (GFR <
60 mL/min per 1.73 m2).7 Prior studies have reported a
positive correlation between serum adiponectin levels and
kidney function.20 Also, from another sub-study of the
Health Professionals Follow-Up Study,8 serum adiponectin concentration was negatively associated with the risk of
CKD (GFR < 60 mL/min per 1.73 m2); this is unlike our
results in which adiponectin was not associated with CKD
risk although patients with CKD had higher mean adiponectin levels than those without. Some studies have reported
elevated levels of IL-6 in patients with chronic renal failure9
or in type 2 diabetes patients with nephropathy,21 but such
a difference was not found in our study. In addition, unlike
findings from other studies showing a positive relation
between serum lipids and the risk of CKD,7 blood lipid
levels were not different between patients with CKD and
those without CKD in our study.
These inconsistent results may be attributable to differences in the ethnic origins of the study populations. In
this regard, ethnic-specific differences in risk factors of
CKD should be considered. For example, none of the
studies mentioned above, except for our current study,
included dietary intake as a confounding factor for analysis.
An intervention study has suggested the beneficial effects
of vitamin C, vitamin E, and zinc on kidney function,22
which is similar to our results where a greater proportion
of the subjects with CKD had inadequate zinc intakes.
Another possible reason for the incompatible results is the
use of different criteria for CKD. Therefore, a direct comparison is not possible due to the many differences in the
study conditions.
Several mechanisms for the effects of CRP and TNF- on
the risk of CKD have been proposed, although the mechanisms leading to the development and progression of
renal injury in type 2 diabetes are not fully understood. CRP,
produced by the liver tissue, and TNF-, synthesized
primarily by monocytes and macrophages, are cytokines
and sensitive indicators of inflammation. It is now evident
that activated innate immunity and inflammation are related
to the pathogenesis of diabetes.21 Furthermore, elevated
levels of these inflammatory markers in patients with type 2
diabetes, who have chronic low-grade inflammation, play a
critical role in the development of microvascular diabetic
complications, including CKD, by potentiating endotherial
dysfunction. Epidemiologic studies13,23 have reported that in
524
type 2 diabetes patients with CKD who had high blood
glucose levels for a prolonged period of time, poor glycemic
control was markedly associated with a rapid decline in
GFR and increased pro-inflammatory cytokines. Endothelial
dysfunction causes increases in pro-inflammatory cytokines
and anti-inflammatory cytokines.8
Consistent with our results, a positive correlation between
measures of insulin resistance and plasma concentrations
of CRP24 and TNF- 21 was previously reported in patients
with CKD. Fasting blood sugar levels were also greater in
subjects with CKD than in those without (Table 2). Overall,
our data suggest that elevated blood glucose may contribute
to increases in plasma concentrations of CRP and TNF-,
and tight blood glucose control is a top priority for patients
with type 2 diabetes to prevent and retard the progression
of diabetic complications.
Our study had several limitations that should be addressed in future studies. For example, it specifically focused
on a representative group of Korean patients with type 2
diabetes. Therefore, these results cannot easily be generalized to other populations or ethnic groups. We observed
an association between plasma concentrations of CRP and
TNF- and the risk of CKD in a cross-sectional setting.
Therefore, it was not possible to determine whether plasma
concentrations of CRP and TNF- are a cause or consequence of CKD. The causality between serum levels of
CRP and TNF- and the risk of CKD should be evaluated
in a follow-up study of the Korean population. In addition,
since the levels of CRP and TNF- increased in other
cardiac conditions complicating type 2 diabetes and subsequent microvascular changes, additional biomarkers
should be employed to clarify their specific direction of
association to CKD. Furthermore, recall bias may have
affected the subjects self-reporting of the duration of
diagnosed type 2 diabetes, although the use of a standard
protocol and well-trained interviewers minimized any bias.
This study also had several advantages. To date, no investigation has examined the association between inflammatory markers and CKD in Asian patients with type 2
diabetes, who have greater risk of CKD, and must be
targeted for its prevention in order to further inhibit the
prolonged development of type 2 diabetes complications
such as ESRD and cardiovascular disease. This study also
showed that elevated levels of CRP and TNF- in patients
with type 2 diabetes had significant effects on the risk of
CKD after adjustments for putative risk factors for CKD
including dietary intake, which is important but had not
been previously investigated.
In conclusion, our results suggest that high concentrations of CRP and TNF- may be independent risk factors
for CKD in Korean patients with type 2 diabetes. Largescale intervention studies are needed to evaluate whether
Yonsei Med J http://www.eymj.org Volume 51 Number 4 July 2010
TNF-, CRP, and Chronic Kidney Disease
lowering blood concentrations of CRP and TNF- reduces
the risk of CKD, and potential benefits of modulating CRP
or TNF- activity as therapeutic targets appear to exist in
patients with type 2 diabetes.
ACKNOWLEDGEMENTS
This work was supported by the second stage of the BK21
Project in 2009 and by Seoul R & BD Program, No. 10526.
REFERENCES
1. Kim DJ, Song KE, Park JW, Cho HK, Lee KW, Huh KB. Clinical
characteristics of Korean type 2 diabetic patients in 2005. Diabetes
Res Clin Pract 2007;77 Suppl 1:S252-7.
2. Kramer H, Molitch ME. Screening for kidney disease in adults
with diabetes. Diabetes Care 2005;28:1813-6.
3. Bolton CH, Downs LG, Victory JG, Dwight JF, Tomson CR,
Mackness MI, et al. Endothelial dysfunction in chronic renal
failure: roles of lipoprotein oxidation and pro-inflammatory
cytokines. Nephrol Dial Transplant 2001;16:1189-97.
4. Mezzano D, Pais EO, Aranda E, Panes O, Downey P, Ortiz M, et
al. Inflammation, not hyperhomocysteinemia, is related to oxidative stress and hemostatic and endothelial dysfunction in
uremia. Kidney Int 2001;60:1844-50.
5. Papayianni A, Alexopoulos E, Giamalis P, Gionanlis L, Belechri
AM, Koukoudis P, et al. Circulating levels of ICAM-1, VCAM1, and MCP-1 are increased in haemodialysis patients: association with inflammation, dyslipidaemia, and vascular events.
Nephrol Dial Transplant 2002;17:435-41.
6. Shlipak MG, Fried LF, Crump C, Bleyer AJ, Manolio TA, Tracy
RP, et al. Elevations of inflammatory and procoagulant biomarkers
in elderly persons with renal insufficiency. Circulation 2003;107:
87-92.
7. Lin J, Hu FB, Rimm EB, Rifai N, Curhan GC. The association of
serum lipids and inflammatory biomarkers with renal function in
men with type II diabetes mellitus. Kidney Int 2006;69:336-42.
8. Lin J, Hu FB, Curhan G. Serum adiponectin and renal dysfunction in men with type 2 diabetes. Diabetes Care 2007;30:
239-44.
9. Zinman B, Hanley AJ, Harris SB, Kwan J, Fantus IG. Circulating tumor necrosis factor-alpha concentrations in a native Canadian population with high rates of type 2 diabetes mellitus. J Clin
Endocrinol Metab 1999;84:272-8.
10. Pradhan AD, Manson JE, Rifai N, Buring JE, Ridker PM. Creactive protein, interleukin 6, and risk of developing type 2
diabetes mellitus. JAMA 2001;286:327-34.
krha J. Pathogenesis of angiopathy in diabetes. Acta Diabetol11. S
ogica 2003;40:S324-9.
12. Costacou T, Orchard TJ. Adiponectin: good, bad, or just plain
ugly? Kidney Int 2008;74:549-51.
13. Dalla Vestra M, Mussap M, Gallina P, Bruseghin M, Cernigoi
AM, Saller A, et al. Acute-phase markers of inflammation and
glomerular structure in patients with type 2 diabetes. J Am Soc
Nephrol 2005;16 Suppl 1:S78-82.
14. Oh SY, Kim EM, Shin MH, Lee SH, Kim JE, Lee HS, et al.
Development and validation of food frequency questionnaire for
adults. The Korean Society of Health Promotion; Annual Spring
Conference; Seoul: 2007.
15. The Korean Nutrition Society. Dietary Reference Intakes for
Koreans, Seoul: 2005.
16. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the
concentration of low density lipoprotein cholesterol in plasma,
without use of the preparative ultracentrifuge. Clin Chem 1972;
18:499-502.
17. Lauer RM, Lee J, Clarke WR. Factors affecting the relationship
between childhood and adult cholesterol levels: the Muscatine
Study. Pediatrics 1988;82:309-18.
18. National Kidney Foundation. K/DOQI clinical practice guidelines
for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 2002;39:S1-266.
19. Bolton CH, Downs LG, Victory JG, Dwight JF, Tomson CR,
Mackness MI, et al. Endothelial dysfunction in chronic renal
failure: roles of lipoprotein oxidation and pro-inflammatory
cytokines. Nephrol Dial Transplant 2001;16:1189-97.
20. Kato K, Osawa H, Ochi M, Kusunoki Y, Ebisui O, Ohno K, et
al. Serum total and high molecular weight adiponectin levels are
correlated with the severity of diabetic retinopathy and nephropathy. Clin Endocrinol (Oxf) 2008;68:442-9.
21. Navarro JF, Mora-Fernndez C. The role of TNF-alpha in diabetic nephropathy: pathogenic and therapeutic implications. Cytokine Growth Factor Rev 2006;17:441-50.
22. Rossing P, Cooper ME, Parving HH. Comparison of the effects
of vitamins and/or mineral supplementation on glomerular and
tubular dysfunction in type 2 diabetes. Diabetes Care 2006;29:
747-8.
23. Ohkubo Y, Kishikawa H, Araki E, Miyata T, Isami S, Motoyoshi
S, et al. Intensive insulin therapy prevents the progression of
diabetic microvascular complications in Japanese patients with
non-insulin-dependent diabetes mellitus: a randomized prospective 6-year study. Diabetes Res Clin Pract 1995;28:103-17.
24. Festa A, DAgostino R, Howard G, Mykknen L, Tracy RP, Haffner SM. Inflammation and microalbuminuria in nondiabetic and
type 2 diabetic subjects: The Insulin Resistance Atherosclerosis
Study. Kidney Int 2000;58:1703-10.
Yonsei Med J http://www.eymj.org Volume 51 Number 4 July 2010
525
Vous aimerez peut-être aussi
- CBLM CaregivingDocument116 pagesCBLM CaregivingGreyz Blas83% (6)
- New Frontiers SB 1Document8 pagesNew Frontiers SB 1SD CIS KOTA CIREBON JAWA BARATPas encore d'évaluation
- Jurnal Internasional Korea DMDocument9 pagesJurnal Internasional Korea DMzahradeswitamuftiPas encore d'évaluation
- 2010-High-Sensitivoty of C-Reactive Protein and CancerDocument8 pages2010-High-Sensitivoty of C-Reactive Protein and CancerThalia KarampasiPas encore d'évaluation
- Jurnal 6Document8 pagesJurnal 6OziPas encore d'évaluation
- Relationship Between C-Reactive Protein, White Blood Cell Count and Metabolic Syndrome in Nigerians With Type 2 Diabetes MellitusDocument11 pagesRelationship Between C-Reactive Protein, White Blood Cell Count and Metabolic Syndrome in Nigerians With Type 2 Diabetes MellitusPaul Gesswein FonatabaPas encore d'évaluation
- Paper Insulin Resistance and Ferritin As Major Determinants of Nonalcoholic Fatty Liver Disease in Apparently Healthy Obese PatientsDocument7 pagesPaper Insulin Resistance and Ferritin As Major Determinants of Nonalcoholic Fatty Liver Disease in Apparently Healthy Obese PatientsNike Dwi Putri LestariPas encore d'évaluation
- Generating A Reference Interval For Fasting Serum Insulin in Healthy Nondiabetic Adult Chinese MenDocument5 pagesGenerating A Reference Interval For Fasting Serum Insulin in Healthy Nondiabetic Adult Chinese MenTanveerPas encore d'évaluation
- Do Proton Pump Inhibitors Increase Mortality in Cirrhotic Patients With Spontaneous Bacterial Peritonitis?Document29 pagesDo Proton Pump Inhibitors Increase Mortality in Cirrhotic Patients With Spontaneous Bacterial Peritonitis?Muhammad Rehan AnisPas encore d'évaluation
- Expression of Renal Injury Markers Among Diabetic Patients in The University of Port Harcourt Teaching HospitalDocument8 pagesExpression of Renal Injury Markers Among Diabetic Patients in The University of Port Harcourt Teaching Hospitalijmb333Pas encore d'évaluation
- Nutrients: Nutritional Adequacy and Latent Tuberculosis Infection in End-Stage Renal Disease PatientsDocument8 pagesNutrients: Nutritional Adequacy and Latent Tuberculosis Infection in End-Stage Renal Disease PatientsMarwa AmrangPas encore d'évaluation
- Met 2019 0059Document6 pagesMet 2019 0059raihannah othmanPas encore d'évaluation
- Diabetes1 KoreaDocument10 pagesDiabetes1 KoreaJimmyPas encore d'évaluation
- 1 s2.0 S1051227620302909 MainDocument8 pages1 s2.0 S1051227620302909 MainIván OsunaPas encore d'évaluation
- Association Between Serum Cystatin C and Diabetic Peripheral Neuropathy: A Cross-Sectional Study of A Chinese Type 2 Diabetic PopulationDocument8 pagesAssociation Between Serum Cystatin C and Diabetic Peripheral Neuropathy: A Cross-Sectional Study of A Chinese Type 2 Diabetic PopulationSakdeep SinghPas encore d'évaluation
- Tight GlycemicDocument10 pagesTight GlycemicIsmail Mohammed AbdelgawadPas encore d'évaluation
- Serum Albumin Level Adjusted With C-Reactive Protein Predicts Hemodialysis Patient SurvivalDocument9 pagesSerum Albumin Level Adjusted With C-Reactive Protein Predicts Hemodialysis Patient Survivalmelda lestari haidirPas encore d'évaluation
- Metabolic Cardiovascular Disease Risk Factors and Their Clustering in Subclinical HypothyroidismDocument7 pagesMetabolic Cardiovascular Disease Risk Factors and Their Clustering in Subclinical HypothyroidismMaria Alice BourneufPas encore d'évaluation
- Study of Lipid Profile in Coronary Heart Disease Patients in LibyaDocument9 pagesStudy of Lipid Profile in Coronary Heart Disease Patients in LibyaInternational Medical PublisherPas encore d'évaluation
- Phagocytic Activity Is Impaired in Type 2 Diabetes Mellitus and Increases After Metabolic ImprovementDocument6 pagesPhagocytic Activity Is Impaired in Type 2 Diabetes Mellitus and Increases After Metabolic ImprovementJenny JennyssimaPas encore d'évaluation
- Jurnal Bu Sulis 1Document6 pagesJurnal Bu Sulis 1PitoAdhiPas encore d'évaluation
- Effect of BmiDocument5 pagesEffect of BmiSyaiful Putra RanaPas encore d'évaluation
- The Metabolic Syndrome: Comparison of Newly Proposed IDF, Modified ATP III and WHO Criteria and Their AgreementsDocument6 pagesThe Metabolic Syndrome: Comparison of Newly Proposed IDF, Modified ATP III and WHO Criteria and Their AgreementsjoelPas encore d'évaluation
- 1 s2.0 S1051227616301789 MainDocument7 pages1 s2.0 S1051227616301789 MainResearch OfficePas encore d'évaluation
- Impact of A Nurse Short Message Service Intervention For Patients With DiabetesDocument6 pagesImpact of A Nurse Short Message Service Intervention For Patients With DiabetesFatima Akbar.Pas encore d'évaluation
- s10554 014 0541 6Document11 pagess10554 014 0541 6Wami FadelPas encore d'évaluation
- The Molar Ratio of Total Branched-Chain Amino Acids To Tyrosine Predicts A Digit Symbol Test Abnormality in Cirrhotic PatientsDocument11 pagesThe Molar Ratio of Total Branched-Chain Amino Acids To Tyrosine Predicts A Digit Symbol Test Abnormality in Cirrhotic PatientsThinh VinhPas encore d'évaluation
- Habitual Coffee Intake, Genetic Polymorphisms, and Type 2 DiabetesDocument8 pagesHabitual Coffee Intake, Genetic Polymorphisms, and Type 2 DiabetesRengganis PutriPas encore d'évaluation
- Active Smoking, Passive Smoking, and Risk of Nonalcoholic Fatty Liver Disease (NAFLD) : A Population-Based Study in ChinaDocument7 pagesActive Smoking, Passive Smoking, and Risk of Nonalcoholic Fatty Liver Disease (NAFLD) : A Population-Based Study in ChinaYelvi Novita RozaPas encore d'évaluation
- Jurnal DWIDocument6 pagesJurnal DWIDwi Asti Lestari PandePas encore d'évaluation
- Manuscript Category: Original Article: DR. YUYA ITANO (Orcid ID: 0000-0001-5287-8550)Document25 pagesManuscript Category: Original Article: DR. YUYA ITANO (Orcid ID: 0000-0001-5287-8550)MarcelliaPas encore d'évaluation
- Chemistry - Ijapbcr - Study of C-Reactive Protein and - Mohd ShakeelDocument6 pagesChemistry - Ijapbcr - Study of C-Reactive Protein and - Mohd ShakeelTJPRC PublicationsPas encore d'évaluation
- Prevalence of and Factors Associated With Sarcopenia Among Elderly Individuals With HypertensionDocument10 pagesPrevalence of and Factors Associated With Sarcopenia Among Elderly Individuals With HypertensionZaskia PutriPas encore d'évaluation
- Nutrients 12 00878Document13 pagesNutrients 12 00878Ardian AshadiPas encore d'évaluation
- Serum Taurine and Risk of Coronary Heart Disease: A Prospective, Nested Case-Control StudyDocument10 pagesSerum Taurine and Risk of Coronary Heart Disease: A Prospective, Nested Case-Control StudyThalia KarampasiPas encore d'évaluation
- CIA 58682 Prognostic Value of Severity Indicators of Nursing Home Acqu 021114Document8 pagesCIA 58682 Prognostic Value of Severity Indicators of Nursing Home Acqu 021114Andres Ramos CardozoPas encore d'évaluation
- Journal Stress OksidatifDocument8 pagesJournal Stress OksidatifMiftakhur RohmahPas encore d'évaluation
- Test Thesis 2 10Document36 pagesTest Thesis 2 10adam yassinePas encore d'évaluation
- Management of Lifestyle Factors in Individuals With Cirrhosis: A Pragmatic ReviewDocument9 pagesManagement of Lifestyle Factors in Individuals With Cirrhosis: A Pragmatic ReviewsavitageraPas encore d'évaluation
- Dietary Protein Intake, Protein Energy Wasting - NUTRIENTS 2019Document12 pagesDietary Protein Intake, Protein Energy Wasting - NUTRIENTS 2019Marilu VillalobosPas encore d'évaluation
- Jurnal Kimia 8Document13 pagesJurnal Kimia 8Rizka Nurul FirdausPas encore d'évaluation
- Worldwide Trends in Diabetes Since 1980Document484 pagesWorldwide Trends in Diabetes Since 1980L P Lozada MartinezPas encore d'évaluation
- 1 s2.0 S1051227619300020 MainDocument9 pages1 s2.0 S1051227619300020 MainRomário de Macedo EspíndolaPas encore d'évaluation
- Using The EQ-5D Index Score As A Predictor of Outcomes in Patients With Type 2 Diabetes - Clarke May08Document20 pagesUsing The EQ-5D Index Score As A Predictor of Outcomes in Patients With Type 2 Diabetes - Clarke May08Haneesha MuddasaniPas encore d'évaluation
- 7decaf9c Cb18 4623 Bced Ecef2197e451Document25 pages7decaf9c Cb18 4623 Bced Ecef2197e451PrabhuPas encore d'évaluation
- 1471 2369 14 191 PDFDocument9 pages1471 2369 14 191 PDFhanifahrafaPas encore d'évaluation
- Association Between SocioeconomicDocument10 pagesAssociation Between SocioeconomicEduardo JohannesPas encore d'évaluation
- Thesis On Liver DiseaseDocument5 pagesThesis On Liver DiseaseCustomNotePaperCanada100% (1)
- Research Paper On Liver DiseaseDocument5 pagesResearch Paper On Liver Diseaseefjem40q100% (1)
- Nutrients: Micronutrient Status in 153 Patients With Anorexia NervosaDocument10 pagesNutrients: Micronutrient Status in 153 Patients With Anorexia NervosaReza Yusna HanastaPas encore d'évaluation
- Excess Protein Intake Relative To Fiber and Cardiovascular Events in Elderly Men With Chronic Kidney DiseaseDocument6 pagesExcess Protein Intake Relative To Fiber and Cardiovascular Events in Elderly Men With Chronic Kidney Diseaseluis Gomez VallejoPas encore d'évaluation
- 1nnnnn ... A Qbqn2i29191s D..... Snsjwnwbs SSWQJQKQ 1111111 60-167Document8 pages1nnnnn ... A Qbqn2i29191s D..... Snsjwnwbs SSWQJQKQ 1111111 60-167Red DiggerPas encore d'évaluation
- Assessment of Creactive Protein Lpid Profile and Body Mass Index in Type2 Diabetes Mellitus in Sudanese PatientsDocument9 pagesAssessment of Creactive Protein Lpid Profile and Body Mass Index in Type2 Diabetes Mellitus in Sudanese PatientsMotasem Sirag Mohmmed othmanPas encore d'évaluation
- Anti-Inflammatory Effects of ExerciseDocument10 pagesAnti-Inflammatory Effects of Exercisejbone918Pas encore d'évaluation
- Effect of Zinc Supplementation On Insulin Resistance and Metabolic Risk Factors in Obese Korean WomenDocument5 pagesEffect of Zinc Supplementation On Insulin Resistance and Metabolic Risk Factors in Obese Korean WomenFahmy2015Pas encore d'évaluation
- Baca IniDocument9 pagesBaca IniRahmi Annisa MaharaniPas encore d'évaluation
- Clinical PharmacyDocument6 pagesClinical PharmacyIrene KristiantiPas encore d'évaluation
- Analysis of Blood Glucose Distribution Characteristics and Its Risk Factors Among A Health Examination Population in Wuhu (China)Document9 pagesAnalysis of Blood Glucose Distribution Characteristics and Its Risk Factors Among A Health Examination Population in Wuhu (China)Aleksa CopicPas encore d'évaluation
- Higher Selenium Status Is Associated With Adverse Blood Lipid Profile in British AdultsDocument7 pagesHigher Selenium Status Is Associated With Adverse Blood Lipid Profile in British AdultsHerly Maulida SurdhawatiPas encore d'évaluation
- The Effects of Lead Exposure On Serum Uric Acid and Hyperuricemia in Chinese Adults: A Cross-Sectional StudyDocument11 pagesThe Effects of Lead Exposure On Serum Uric Acid and Hyperuricemia in Chinese Adults: A Cross-Sectional StudyriaPas encore d'évaluation
- Complementary and Alternative Medical Lab Testing Part 8: UrologyD'EverandComplementary and Alternative Medical Lab Testing Part 8: UrologyÉvaluation : 3 sur 5 étoiles3/5 (1)
- Complementary and Alternative Medical Lab Testing Part 6: Liver and GallbladderD'EverandComplementary and Alternative Medical Lab Testing Part 6: Liver and GallbladderPas encore d'évaluation
- Grade 9 DLP Week 1 Day1 2Document11 pagesGrade 9 DLP Week 1 Day1 2Rando Estañero MonsaludPas encore d'évaluation
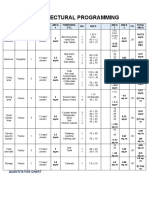
- Architectural Programming: Quantitative ChartDocument3 pagesArchitectural Programming: Quantitative Chartmiriam martinez50% (2)
- Goldenville School of Montessori, Inc.: Matimbubong, San Ildefonso, BulacanDocument4 pagesGoldenville School of Montessori, Inc.: Matimbubong, San Ildefonso, BulacanKenneth Delos SantosPas encore d'évaluation
- Recette World Chocolate Masters - InfiniteDocument1 pageRecette World Chocolate Masters - InfiniteTarak ZayaniPas encore d'évaluation
- Care Sheet - Bearded DragonDocument4 pagesCare Sheet - Bearded DragonJohn Gamesby100% (1)
- Mobile - Hyderabadi Chicken Biryani Recipe, HyderabadiDocument2 pagesMobile - Hyderabadi Chicken Biryani Recipe, HyderabadiBarath GunasekaranPas encore d'évaluation
- Cephaleuros VirescensDocument6 pagesCephaleuros VirescensAlexis Romero DobbertinPas encore d'évaluation
- Sex Tour Part DeuxDocument1 pageSex Tour Part DeuxAvel ManansalaPas encore d'évaluation
- Last Mile 5category LayoutsDocument24 pagesLast Mile 5category LayoutsManoj NakraPas encore d'évaluation
- Notes Form 2 Chapter 4Document4 pagesNotes Form 2 Chapter 4lembu_sihat7783% (6)
- S in Hort Te Ntroduc Est Ans Tion Un Wer Ke Nit, Test Eys A t1Document6 pagesS in Hort Te Ntroduc Est Ans Tion Un Wer Ke Nit, Test Eys A t1Teachers SMG eduPas encore d'évaluation
- TítDocument14 pagesTítAnhTuyet ThieuPas encore d'évaluation
- A Warm Wedding and A New Bride of Young Master LuDocument48 pagesA Warm Wedding and A New Bride of Young Master LuANNA ANETA50% (2)
- d.3. Blue Dairy Corp Vs NLRC, G.R. No. 129843, September 14, 1999Document5 pagesd.3. Blue Dairy Corp Vs NLRC, G.R. No. 129843, September 14, 1999LawrenceAltezaPas encore d'évaluation
- Shawarma Spice Blend Recipe - Minimalist Baker RecipesDocument9 pagesShawarma Spice Blend Recipe - Minimalist Baker RecipesDenis JPas encore d'évaluation
- 6 291 1477120320241 244Document4 pages6 291 1477120320241 244DarshanPas encore d'évaluation
- ISKCON Desire Tree - Vanilla Butter CakeDocument2 pagesISKCON Desire Tree - Vanilla Butter CakeISKCON desire treePas encore d'évaluation
- Student Name:: Welcome To "Introduction To ISO 22000 Food Safety Management Systems"Document15 pagesStudent Name:: Welcome To "Introduction To ISO 22000 Food Safety Management Systems"frawatPas encore d'évaluation
- Patapon 2Document59 pagesPatapon 2Dennis LubianoPas encore d'évaluation
- The Gmo in Our FoodDocument23 pagesThe Gmo in Our FoodHaiz MainePas encore d'évaluation
- Rana PackagingDocument26 pagesRana PackagingVignesh DurairajPas encore d'évaluation
- Mat Leave LetterDocument11 pagesMat Leave LetterLeshlie OrdonioPas encore d'évaluation
- 101 Essential Tips Dog Care - 2015 PDFDocument74 pages101 Essential Tips Dog Care - 2015 PDFalavanisPas encore d'évaluation
- Thesis About Pandan LeavesDocument5 pagesThesis About Pandan Leavesmelissajacksonminneapolis100% (2)
- Report of Ashapura Volclay LTDDocument33 pagesReport of Ashapura Volclay LTDNiraj Patel100% (2)
- CHAPTER 1 Investegatory ReasearchDocument3 pagesCHAPTER 1 Investegatory ReasearchAngelica Alican Cerbito50% (2)
- Graham Elizabeth Devil On Horseback PDFDocument191 pagesGraham Elizabeth Devil On Horseback PDFMaheran Aljufri81% (27)
- UNIT 12" It Really WorksDocument2 pagesUNIT 12" It Really WorksZulfa raniPas encore d'évaluation