Académique Documents
Professionnel Documents
Culture Documents
Rabies: All Mammals Are Believed To Be
Transféré par
Melissa DavidTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Rabies: All Mammals Are Believed To Be
Transféré par
Melissa DavidDroits d'auteur :
Formats disponibles
RABIES
An acute, progressive, fatal
encephalomyelitis caused by neurotropic
viruses
Always almost fatal once manifestations
develop
RHABDOVIRUS a bullet-shaped virus with
strong affinity to CNS tissues
Saliva of a rabid animal
All mammals are believed to be
susceptible, but reservoirs are carnivores
and bats.
Bite of an infected animal
Licking of open wounds by a rabid animal
Scratch of a rabid animal
Man to man transmission (10%)
Airborne (Rare)
Dogs: 1 week to 7 and months
Humans: 10 days to 1 year
Pain and numbness at the site of bite
Flu-like symptoms
Fever
Headache
Malaise/myalgia
Sore throat
Marked insomnia
Apprehensive, Restlessness
Sensitivity to light and sound
Marked excitation and apprehension
Maniacal behavior
Paranoia, Hallucinations, Delirium
Hydrophobia, Aerophobia
Drooling of saliva
Quiet and unconcscious
Spasm ceases with progressive paralysis
Tachycardia, labored respirations
Respiratory paralysis, circulatory collapse
DEATH
Isolation of virus from saliva
Detection of antibodies to virus of serum or
spinal fluid
Examination for rabies antigen in the
cutaneous nerves at the base of hair
follicles through Skin Biopsy
Clinical observation (10-14 days)
Direct Fluorescent Rabies Antibody Test
(DFRAT)
Brain Biopsy: Detection of Negri Bodies
No specific treatment
Care of the patient is symptomatic and
supportive
Clean the wound with soap and water
Antiseptic solution: Povidone-Iodine
Tetanus prophylaxis
Post-exposure prophylaxis
PASSIVE VACCINATION
1. Human Rabies Immunoglobulin (RHIg)
Rabuman, Imogam
20 IU/kg
2. Animal Serum Equine Rabies Immunoglobulin
(ASERIg)
Antirabies Serum, HyperRAB
40 IU/kg
ACTIVE VACCINATION
PVCV (Vero Rab): IM Day 0,7,21,90
PDEV (Lyssavac): ID Day 0,3,7,28,90
HDCV: IM 0,3,7,14,28
PCEV: IM 0,3,7,14,28
ACTIVE VACCINATION
PASSIVE VACCINATION
Is not required
Isolation of patients
Restrain when necessary
Darken the room and provide a quiet
environment
Stimulation of any senses by fluid is
prohibited
Wear protective barriers
Responsible Pet Ownership
Victim Immunization
Dog Immunization
Immunization
Keep away from stray animal
TETANUS
Is an infectious disease caused by
Clostridium tetani which produces potent
exotoxin with prominent systemic
neuromuscular effects
manifested by generalized spasmodic
contraction of the skeletal musculature
Lockjaw
CLOSTRIDIUM TETANI - Anaerobic, sporeforming Gram (+) rod with drumstick
appearance
Two types of toxin:
Tetanospasmin, tetanolysin
Soil
Street dust
Animal and human feces
Rusty materials
Through punctured wound that is
contaminated by dust, soil, or animal
excreta containing Clostridium tetani
Adult: 3 days 3 weeks
Newborn: 3 30 days
st
1 sign: difficulty in feeding and sucking
High grade fever
Stiffness of the jaw
Excessive crying
Muscle spasm
Convulsion
Low grade fever
Diaphoresis
Trismus
Opisthotonus
Risus sardonicus- pathognomonic sign
Abdominal rigidity
Stiffness of the extremity
Severe cases: Laryngospasm
The diagnosis is almost always made
clinically
History of wound
Lack of immunization: A factor
ANTITOXINS
Tetanus Immunoglobulin (TIG): 3,0006000 units IM
Tetanus Antitoxin (TAT): 50,000100,000 units, half IV, the rest IM
Antitetanus Serum (ATS): 40, 000 units
Antibiotic: METRONIDAZOLE- drug of
choice
Muscle Relaxant: Diazepam, Baclofen
Maintain adequate airway
Wound care: debridement
Maintain fluid and electrolyte balance
Place patient in quiet, darkened
environment
Minimal handling
Protect from injury
Exteroceptive: bright lights and noise
Interoceptive: Stress, pain
Propioceptive: Turning, touching
Ineffective breathing pattern related to
muscles spasm and neurologic impairment.
Risk for injury related to muscle spasms.
Immunization with tetanus toxoid for adults
DPT for babies and children
LEPTOSPIROSIS
1.
2.
3.
A zoonotic infectious bacterial disease
carried by animals, both domestic and wild,
whose urine contaminates water or food
which is ingested or inoculated through skin
Weils disease
Canicola Fever
Mud Fever
Hemorrhagic jaundice
Swineherds Disease
LEPTOSPIRA INTERROGANS
Spirochete, Motile, Beta-hemolytic
Chiefly saprophytic aquatic organisms
river
lake water
Sewage
sea
6-15 days
Leptospira is found in the urine between 10
to 20 days after the onset
Urine of infected animal
Reproductive fluids (RARE)
Ingestion or contact with the skin and
mucous membrane of the infected urine or
carcasses of wild and domestic animals.
Through the mucous membrane of the
eyes, nose, and mouth, and through a break
on the skin.
Direct human to human transmission is
rare.
Leptospira enters the blood to cause
damage, thereafter, in the:
Kidney
Liver
Eyes
Meninges
Occupational risk factors include
veterinarians, slaughter house workers,
farmers, and sewer workers.
Clinical course is generally biphasic and the
majority of the cases are anicteric.
Remittent fever
Chills
Headache
Anorexia
Nausea and vomiting
Prostration
Abdominal pain
Diarrhea
UNICTERIC TYPE
Conjunctival suffusion
Uveitis or iritis
Meningeal manifestations
With CSF findings of aseptic
meningitis
ICTERIC TYPE
Jaundice and renal failure (Weils
syndrome)
Hemorrhage
CHF in severe cases
th
Relapse may occur during the 4
th
to 5 week
Usually based on Serology
Culture
Blood, CSF, Urine
ELISA
MAT: the recognized standard reference
test for serologic diagnosis of leptospirosis
Antibiotic: PENICILLIN G (drug of choice)
Oral doxycycline 100mg PO every 12 hours
x 1 week (prophylactic)
Fight complications: require hospitalization
Peritoneal dialysis
Symptomatic and supportive
Isolate the patient, urine must be properly
disposed of.
Darken patients room
Observe meticulous skin care to ease
pruritus.
Keep clients under close surveillance.
Sanitation in homes, workplaces, and farms
Eradication of rats
Animals must be vaccinated (cattle, dogs,
cats, and pigs)
SCHISTOSOMIASIS
Is a parasitic disease caused by several
species of trematodes("flukes)
Primarily affects the liver and GIT.
Capable of producing obstructive jaundice
and liver cirrhosis
Second most socioeconomically devastating
parasitic disease after malaria
Schistosoma japonicum- Intestinal
schistosomiasis
Schistosoma mansoni- Intestinal
schistosomiasis
Schistosoma haematobium- Urinary
schistosomiasis
Skin penetration by cercaria
Through ingestion of contaminated water
Incubation Period
About 2-6 weeks from skin penetration
Adult female and male parasites
Ova
Miracidium infective stage in snails
Cercaria infective stage in man and
animals
Snail (Oncomelania quadrasi)
Thrives best along river banks, fresh water
streams, creeks, canals and swamps
Greenish-brown in color and is just as big as
the smallest grain of palay
Low-grade fever
Abdominal pain- due to hepatomegaly,
splenomegaly, and lymphadenopathy
Myalgia; fatigue
Cough
Bloody-mucoid stool, dysentery-like
Swimmers itch
Anemia and malnutrition
When parasites reaches the brain--- severe
headache, dizziness, and convulsion
Portal hypertension and signs of liver
cirrhosis
Hematemesis
Pulmonary hypertension
Glomerulonephritis--- Renal failure
KATO-KATZ TECHNIQUE
is a laboratory method for preparing human
stool samples prior to searching for parasite
eggs
is now most commonly used for detecting
schistosome eggs
CIRCUM OVA PRECIPITIN TEST (COPT)
Was used to detect serum antibodies
to Schistosoma mansoni, S. haematobium,
or both species by using eggs of either
species of schistosome
Praziquantel (biltricide) drug of choice;
single oral dose annually
Oxamniquine- exclusively for treating S.
mansoni
Metrifonate- exclusively for treating s.
haematobium
No vaccines are currently available
Eliminating the water-dwelling snails that
are the natural reservoir of the disease
Clearing vegetation thus exposing the snail
to sunshine
Constructing drainage to dry the land
surface where the snails thrive
Improve farming by proper irrigation and
drainage
Diminish infection rate:
Proper waste disposal
Control of stray animals
Avoid bathing in infested streams
Vous aimerez peut-être aussi
- Leptospirosis: A Bacterial Infection Spread Through Contact With Infected AnimalsDocument14 pagesLeptospirosis: A Bacterial Infection Spread Through Contact With Infected AnimalsNica Paredes MiravallesPas encore d'évaluation
- A Case HistoryDocument43 pagesA Case Historymel_pusagPas encore d'évaluation
- MedicineDocument82 pagesMedicineDr Anais AsimPas encore d'évaluation
- FINAL Snake Bite Case PresDocument48 pagesFINAL Snake Bite Case PresMonica Angelique SalayoPas encore d'évaluation
- Amphistomate & Distomate FlukeDocument12 pagesAmphistomate & Distomate FlukeJayricDepalobosPas encore d'évaluation
- Pathognomonic signs and symptoms of common communicable diseasesDocument6 pagesPathognomonic signs and symptoms of common communicable diseasesEjie Boy IsagaPas encore d'évaluation
- Peste Des Petits RuminantsDocument6 pagesPeste Des Petits RuminantsKenesaPas encore d'évaluation
- Leptospirosis: Presented By: Alexandra G de Leon Presented To: Dr. Dario V SumandeDocument15 pagesLeptospirosis: Presented By: Alexandra G de Leon Presented To: Dr. Dario V SumandealexPas encore d'évaluation
- Hemorrhagic Septicemia: An Acute, Fatal DiseaseDocument27 pagesHemorrhagic Septicemia: An Acute, Fatal DiseaseDesign worldPas encore d'évaluation
- SM SAI NS RAJ A TU N AZL AN SHA H: Human HealthDocument7 pagesSM SAI NS RAJ A TU N AZL AN SHA H: Human Healthsofea1121Pas encore d'évaluation
- 7 - LeptospirosisDocument18 pages7 - LeptospirosisCAÑADA, JOHANNELYN M.Pas encore d'évaluation
- Digenean: Schistosoma SPP.: PathologyDocument5 pagesDigenean: Schistosoma SPP.: PathologyBernard Lionel MoreusPas encore d'évaluation
- Case Study Leptospirosis PowerpointDocument17 pagesCase Study Leptospirosis Powerpointbeancent100% (2)
- Handouts Avian Salmonellosis Fall 2020Document8 pagesHandouts Avian Salmonellosis Fall 2020NabeelPas encore d'évaluation
- Anthrax: SynonymsDocument4 pagesAnthrax: SynonymsVenkatapradeepPas encore d'évaluation
- Intestinal FlukesDocument6 pagesIntestinal FlukesGillian Mae CasipitPas encore d'évaluation
- Foot and Mouth DiseaseDocument5 pagesFoot and Mouth Diseaseelvhynd beiPas encore d'évaluation
- LeptospirosisDocument10 pagesLeptospirosisjramos11067920Pas encore d'évaluation
- Mammalian Diseases Found in Captivity FinalDocument45 pagesMammalian Diseases Found in Captivity Finalapi-250146149Pas encore d'évaluation
- Zoonotic Diseases Fact SheetDocument7 pagesZoonotic Diseases Fact SheetEightch PeasPas encore d'évaluation
- Leptospirosis: Baron Lucien M, Garcia San Lazaro Hospital Olivarez College /BSN IV Group 2 Mrs. LofamiaDocument5 pagesLeptospirosis: Baron Lucien M, Garcia San Lazaro Hospital Olivarez College /BSN IV Group 2 Mrs. LofamiablucienPas encore d'évaluation
- AnthraxDocument6 pagesAnthraxeutamène ramziPas encore d'évaluation
- 2.-Schistosomiasis-Rabies-Pediculosis-Bubonic-Plague-Anthrax-HelminthesDocument92 pages2.-Schistosomiasis-Rabies-Pediculosis-Bubonic-Plague-Anthrax-Helminthesaltairejoshua.jalbayPas encore d'évaluation
- University of Perpetual HelpDocument7 pagesUniversity of Perpetual HelpchristianmozartgoPas encore d'évaluation
- Leptospirosis FDocument1 pageLeptospirosis FKeto PrehranaPas encore d'évaluation
- Leptospirosis FinalDocument5 pagesLeptospirosis FinalufriePas encore d'évaluation
- Leptospirosis: Symptoms, Causes, Statistics, PreventionDocument10 pagesLeptospirosis: Symptoms, Causes, Statistics, PreventionIrene Bodegon CuaPas encore d'évaluation
- Leptospirosis EFRIDADocument19 pagesLeptospirosis EFRIDABendy Dwi IrawanPas encore d'évaluation
- Salmonellosis and Enteric Fever: Causes, Symptoms and PreventionDocument4 pagesSalmonellosis and Enteric Fever: Causes, Symptoms and PreventionJake MillerPas encore d'évaluation
- Rodent Borne DiseaseDocument6 pagesRodent Borne DiseasecallmejusPas encore d'évaluation
- Large A.medicine 4th YearDocument285 pagesLarge A.medicine 4th YearAssefaTayachewPas encore d'évaluation
- Micro Lec 17 - YersiniaDocument24 pagesMicro Lec 17 - YersiniaJacklyn Manaog-SoPas encore d'évaluation
- Lepto Dan RabiesDocument69 pagesLepto Dan RabiesHiszom AsyhariPas encore d'évaluation
- Reptilian and Amphibious Diseases Found in Captivity FinalDocument12 pagesReptilian and Amphibious Diseases Found in Captivity Finalapi-250146149Pas encore d'évaluation
- Pasteurelosis: The Disease Due ToDocument45 pagesPasteurelosis: The Disease Due Toclarentina aristawatiPas encore d'évaluation
- Common Toxic Bites: Olowookere O.ODocument62 pagesCommon Toxic Bites: Olowookere O.OTheop AyodelePas encore d'évaluation
- Bird Diseases - Everything You Need To KnowDocument1 pageBird Diseases - Everything You Need To KnowjpgbfPas encore d'évaluation
- Avian-Parasites UpdateDocument5 pagesAvian-Parasites UpdateCody CodyPas encore d'évaluation
- Diphtheria: Respiratory SystemDocument17 pagesDiphtheria: Respiratory Systemprencess_jeny5006Pas encore d'évaluation
- Foot and Mouth Disease: AetiologyDocument6 pagesFoot and Mouth Disease: Aetiology1938 MANOJ R BHARADWAJPas encore d'évaluation
- Muhammad Usman Akram: (DVM Student at Rcvets Lahore)Document29 pagesMuhammad Usman Akram: (DVM Student at Rcvets Lahore)Usman Akram100% (1)
- TrematodesDocument56 pagesTrematodesrmukbelPas encore d'évaluation
- Lepto Spiros IsDocument5 pagesLepto Spiros IsMaEstelleJune TalampasPas encore d'évaluation
- Lepto Spiros IsDocument5 pagesLepto Spiros IsMaEstelleJune TalampasPas encore d'évaluation
- Gil P. Soriano, RN, MhpedDocument24 pagesGil P. Soriano, RN, MhpedGil Platon SorianoPas encore d'évaluation
- Prof. DR Fahim ShaltoutDocument55 pagesProf. DR Fahim ShaltoutSumit SharmaPas encore d'évaluation
- Leptospirosis in Trinidad and Grenada, With Special Reference To The Mongoose 1972Document13 pagesLeptospirosis in Trinidad and Grenada, With Special Reference To The Mongoose 1972Hugh JacobsPas encore d'évaluation
- Parasitic InfectionsDocument65 pagesParasitic InfectionsJezreel OrquinaPas encore d'évaluation
- ViralDocument49 pagesViralأحمد خيريPas encore d'évaluation
- Spirochaetta - LeptospiraDocument8 pagesSpirochaetta - Leptospiragalih suharnoPas encore d'évaluation
- Kuliah Cestode & Trematode (Hand-Out)Document13 pagesKuliah Cestode & Trematode (Hand-Out)made yogaPas encore d'évaluation
- AssignmentDocument9 pagesAssignmentDr Anais AsimPas encore d'évaluation
- Large Animal Medicine PPt2016Document221 pagesLarge Animal Medicine PPt2016kibrushe260Pas encore d'évaluation
- Exotic Animal ParasitesDocument37 pagesExotic Animal ParasitesSUTHANPas encore d'évaluation
- Cdnursing PPT 2021Document37 pagesCdnursing PPT 2021yuuki konnoPas encore d'évaluation
- Notes on Diseases of Cattle: Cause, Symptoms and TreatmentD'EverandNotes on Diseases of Cattle: Cause, Symptoms and TreatmentPas encore d'évaluation
- 911 Pigeon Disease & Treatment Protocols!D'Everand911 Pigeon Disease & Treatment Protocols!Évaluation : 4 sur 5 étoiles4/5 (1)
- Medicine Request 2020Document13 pagesMedicine Request 2020Melissa DavidPas encore d'évaluation
- CKDDocument28 pagesCKDMelissa DavidPas encore d'évaluation
- Health & Medical Services - Mid Year PresentationDocument11 pagesHealth & Medical Services - Mid Year PresentationMelissa DavidPas encore d'évaluation
- Medicines Inventory 2018Document3 pagesMedicines Inventory 2018Melissa DavidPas encore d'évaluation
- Critical Care Nursing Course MapDocument1 pageCritical Care Nursing Course MapMelissa David0% (1)
- Nursing ManagementDocument7 pagesNursing ManagementMelissa DavidPas encore d'évaluation
- Capsule The Lived Experience Rev March 30Document18 pagesCapsule The Lived Experience Rev March 30Melissa DavidPas encore d'évaluation
- Comprehensive Safety and Health Program General IndustryDocument31 pagesComprehensive Safety and Health Program General IndustryMelissa David100% (1)
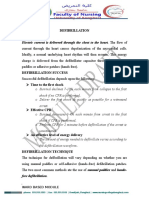
- DefibrillationDocument6 pagesDefibrillationMelissa DavidPas encore d'évaluation
- CKDDocument28 pagesCKDMelissa DavidPas encore d'évaluation
- Bangsamoro Basic Law ReasearchDocument6 pagesBangsamoro Basic Law ReasearchMelissa David100% (1)
- Otitis MediaDocument14 pagesOtitis MediaMelissa DavidPas encore d'évaluation
- AppendicitisDocument23 pagesAppendicitisMelissa DavidPas encore d'évaluation
- Remotivation TherapyDocument2 pagesRemotivation TherapyMelissa David100% (1)
- Bronchial AsthmaDocument8 pagesBronchial AsthmaBrylle CapiliPas encore d'évaluation
- Pneumonia: Causes, Signs, Symptoms and Nursing CareDocument16 pagesPneumonia: Causes, Signs, Symptoms and Nursing CareMelissa David100% (1)
- Case Study ON Acute Gastroenteritis: Submitted By: Melissa D. DavidDocument17 pagesCase Study ON Acute Gastroenteritis: Submitted By: Melissa D. DavidMelissa DavidPas encore d'évaluation
- Case Study-Congestive Heart FailureDocument71 pagesCase Study-Congestive Heart FailureKentTangcalagan92% (13)
- CHF Case StudyDocument38 pagesCHF Case StudyMelissa David100% (1)
- Nursing Care PlanDocument3 pagesNursing Care PlanMelissa DavidPas encore d'évaluation
- Drug Study ERDocument2 pagesDrug Study ERMelissa DavidPas encore d'évaluation
- Drug StudyDocument4 pagesDrug StudyMelissa DavidPas encore d'évaluation
- MsjournalDocument2 pagesMsjournalMelissa DavidPas encore d'évaluation
- Comm. Dse MOT Incub POC S/SX DX CX TX Prevent: MeaslesDocument5 pagesComm. Dse MOT Incub POC S/SX DX CX TX Prevent: MeaslesMelissa David100% (1)
- Gestational Diabetes MellitusDocument1 pageGestational Diabetes MellitusMelissa DavidPas encore d'évaluation
- CVDDocument3 pagesCVDMelissa DavidPas encore d'évaluation
- NCPDocument2 pagesNCPMelissa David100% (1)
- Milestones PediaDocument6 pagesMilestones PediaMelissa DavidPas encore d'évaluation
- NCPDocument3 pagesNCPMelissa DavidPas encore d'évaluation
- Anti Helminthic DrugsDocument3 pagesAnti Helminthic Drugsdhainey100% (2)
- (Methods in Molecular Biology 2151) David J. Timson - Schistosoma mansoni_ Methods and Protocols-Springer US_Humana (2020)Document270 pages(Methods in Molecular Biology 2151) David J. Timson - Schistosoma mansoni_ Methods and Protocols-Springer US_Humana (2020)Henry David Mogollon GarciaPas encore d'évaluation
- Rules and RegulationsDocument6 pagesRules and RegulationsMukesh MistriPas encore d'évaluation
- A Case Study On SchistosomiasisDocument154 pagesA Case Study On SchistosomiasisCarmellaDawn100% (1)
- 7 Kato Thick Smear TechniqueDocument4 pages7 Kato Thick Smear TechniqueAren SongcoPas encore d'évaluation
- Filariasis, Schistosomiasis, Leprosy Control Program and Malaria Control ProgramDocument26 pagesFilariasis, Schistosomiasis, Leprosy Control Program and Malaria Control ProgramPC NPas encore d'évaluation
- Veterinary ParasitologyDocument4 pagesVeterinary Parasitologysimran kaurPas encore d'évaluation
- Ancient Egypt and The Modern WorldDocument4 pagesAncient Egypt and The Modern WorldVanessa Reyes MontillaPas encore d'évaluation
- TrematodesDocument16 pagesTrematodesRenz Gerard AmorPas encore d'évaluation
- Importance Surveillance and DetectionDocument6 pagesImportance Surveillance and Detectionsherog ahmedPas encore d'évaluation
- TrematodesDocument20 pagesTrematodesmiguel gaquitPas encore d'évaluation
- Bank of Tanzania Academy Joining InstructionsDocument9 pagesBank of Tanzania Academy Joining InstructionsKashindye LucasPas encore d'évaluation
- BilharziaDocument4 pagesBilharziaAhmed FaizPas encore d'évaluation
- GY339 Environmental Classification of Excreta Related Disease 2017Document58 pagesGY339 Environmental Classification of Excreta Related Disease 2017Lorraine100% (1)
- CHN 1 Module 4 Communicable DiseasesDocument23 pagesCHN 1 Module 4 Communicable Diseases202270189Pas encore d'évaluation
- Para-Transes Pre-Final Exam - Unit 4Document11 pagesPara-Transes Pre-Final Exam - Unit 4Aysha AishaPas encore d'évaluation
- Trematodes 2Document4 pagesTrematodes 2Marie Petalcorin100% (1)
- Table of Different ParasitesDocument6 pagesTable of Different ParasitesYowan05Pas encore d'évaluation
- Schistosomiasis General Info IIIDocument40 pagesSchistosomiasis General Info IIIAssejanej EpracPas encore d'évaluation
- Sem in NursingDocument9 pagesSem in Nursingcrisel mayangaoPas encore d'évaluation
- ICD 10 English Indonesia Lengkap 2Document836 pagesICD 10 English Indonesia Lengkap 2DINY NOORKHAYATIPas encore d'évaluation
- Allied Health Council Examination QuestionsDocument39 pagesAllied Health Council Examination QuestionsSAMMYPas encore d'évaluation
- Helminths MCQsDocument21 pagesHelminths MCQsمحمد محمد هشام83% (18)
- Schistosomiasis Control Program PhilippinesDocument2 pagesSchistosomiasis Control Program PhilippinesDud AccPas encore d'évaluation
- Trematodes AssignmentDocument6 pagesTrematodes AssignmentJackie Lind TalosigPas encore d'évaluation
- Communicable Diseases ReviewerDocument13 pagesCommunicable Diseases ReviewerMarivic Salcedo McCreaPas encore d'évaluation
- Biology Form 3 Ecology - Knec Study Materials, Revision Kits and Past PapersDocument29 pagesBiology Form 3 Ecology - Knec Study Materials, Revision Kits and Past Paperskiraguripeter1994Pas encore d'évaluation
- Current Status of NTD PhilippinesDocument28 pagesCurrent Status of NTD PhilippinesMelody PardilloPas encore d'évaluation
- Aconitum Napellus Monkshood Anxiety Fear Anguish Mind BodyDocument26 pagesAconitum Napellus Monkshood Anxiety Fear Anguish Mind BodyvipinPas encore d'évaluation
- Communicative Skill IIDocument16 pagesCommunicative Skill IIGUDINA MENGESHA MEGNAKAPas encore d'évaluation