Académique Documents
Professionnel Documents
Culture Documents
Hysterosalpingogran
Transféré par
Sanal KumarCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Hysterosalpingogran
Transféré par
Sanal KumarDroits d'auteur :
Formats disponibles
AJR Integrative Imaging
LIFELONG LEARNING
FOR RADIOLOGY
Downloaded from www.ajronline.org by 107.167.99.125 on 12/27/14 from IP address 107.167.99.125. Copyright ARRS. For personal use only; all rights reserved
Imaging of Congenital Uterine Anomalies:
Review and Self-Assessment Module
Thomas M. Dykes1, Cary Siegel2, William Dodson1
3. Understand the clinical significance of each anomaly;
4. Make appropriate recommendations for additional imaging
or intervention.
ABSTRACT
Objective
The educational objectives of this continuing medical education activity are for the reader to exercise, self-assess, and improve skills in diagnostic radiology with regard to the
interpretation of hysterosalpingograms and magnetic resonance
imaging (MRI) of the female pelvis in the evaluation of recurrent
reproductive failure caused by congenital uterine anomalies.
Conclusion
This article reviews the common congenital uterine anomalies, characteristic imaging features of each anomaly by hysterosalpingography and MRI, and the clinical importance of
diagnosing and properly categorizing each anomaly.
INTRODUCTION
This self-assessment module on imaging of congenital uterine
anomalies has an educational component and a self-assessment
component. The educational component consists of an AJR
Teaching File article and an educational exhibit from the 2007
ARRS Annual Meeting, included as supplemental data to this
article, that the participant should review. In addition, there are
four interactive case scenarios presented in this article. The selfassessment component consists of eight multiple-choice questions with solutions. All of these materials are available on the
ARRS Website (www.arrs.org). To claim CME and SAM credit,
each participant must register and then enter his or her responses
to the questions online.
EDUCATIONAL OBJECTIVES
Upon completion of this educational activity the participant
will be able to:
1. Recognize the common congenital uterine anomalies;
2. Appropriately categorize the anomaly based on the American Fertility Society (now known as the American Society for
Reproductive Medicine) classification system;
REQUIRED ACTIVITIES
(available at www.arrs.org or www.ajronline.org)
1. Chaudry S. Infertility in a young woman. AJR 2007; 189:
S11S12.
2. Data supplement included with [1]. http://www.ajronline.org/
cgi/content/full/189/3_Supplement/S11/DC1
3. Four interactive case scenarios presented in this article.
RECOMMENDED READING
(available at www.arrs.org)
1. Lindheim SR, Sprague C, Winter TC III. Hysterosalpingography and sonohysterography: lessons in technique. AJR
2006; 186: 2429
2. Dalf AR, beda B, beda A, Monzn M, Rotger R, Ramos
R, Palacio A. Diagnostic value of hysterosalpingography in the
detection of intrauterine abnormalities: a comparison with
hysteroscopy. AJR 2004; 183: 14051409
3. Troiano RN, McCarthy SM. Mllerian duct anomalies: imaging and clinical issues. Radiology 2004; 233: 1934
4. ONeill MJ, Yoder IC, Connolly SA, Mueller PR. Imaging
evaluation and classification of developmental anomalies of
the female reproductive system with an emphasis on MR
imaging. AJR 1999; 173: 407416
INSTRUCTIONS
1. Complete the required activities and review the accompanying electronic exhibit presented as supplemental data to [1].
2. Visit www.arrs.org and go to the left-hand menu bar under
Publications/Journals/SAM articles.
3. Using your member login, order the online SAM as directed.
4. Follow the online instructions for entering your responses to
the self-assessment questions and complete the test by answering the questions online.
Keywords: congenital malformations, genitourinary tract imaging, hysterosalpingography, MR imaging, mllerian duct anomaly, womens imaging
DOI:10.2214/AJR.06.0821
Received June 22, 2006; accepted with revision August 28, 2006.
1Department of Radiology, Pennsylvania State University, Milton S. Hershey Medical Center, 500 University Drive, P.O. Box 850, Hershey, PA 17033. Address correspondence to T. M. Dykes
(tdykes@hmc.psu.edu).
2Mallinckrodt Institute of
Radiology, Washington University, St. Louis, MO.
AJR 2007;189:S1S10 0361803X/07/1893S1 American Roentgen Ray Society
AJR:189, September 2007
S1
Dykes et al.
Downloaded from www.ajronline.org by 107.167.99.125 on 12/27/14 from IP address 107.167.99.125. Copyright ARRS. For personal use only; all rights reserved
BACKGROUND
The true incidence of congenital uterine anomalies, also referred to as mllerian duct anomalies, is not accurately known,
with reports ranging from a frequency of one of 10 patients to
one of 1,600 patients [1]. Summation of data from multiple studies suggests the prevalence of these anomalies in women with a
history of multiple pregnancy loss is approximately 3% [2]. Approximately 25% of women with mllerian duct anomalies have
associated reproductive problems, compared with 10% of the
general population [2].
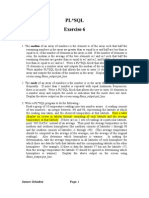
I Hypoplasia/agenesis
(a) Vaginal
After recognition of a mllerian duct anomaly, it is important to
properly classify the anomaly because the associated risks of poor
pregnancy outcome and treatment can vary widely between the
anomalies. The most common classification system for congenital
uterine anomalies is that used by the American Society for Reproductive Medicine [3]. This continuing medical education activity
focuses on types IIVI anomalies that are illustrated in Figure 1.
It is important to be mindful that this classification system is only
a framework for understanding and reporting these anomalies and
that all anomalies will not necessarily fit completely into one of the
II Unicornuate
(b) Cervical
(a) Communicating
III Didelphus
(b) Non-communicating
IV Bicornuate
(c) Fundal
(d) Tubal
(e) Combined
(c) No cavity
V Septate
(a) Complete
(d) No horn
VI Arcuate
(a) Complete
(b) Partial
VII DES drug related
(b) Partial
Fig. 1Classification system of mllerian duct anomalies used by the American Society for Reproductive Medicine [3] (Reprinted with permission). DES=diethylstilbestrol.
Fig. 2Sagittal localizer sequence in healthy patient shows imaging planes required for T2 imaging sequences.
A, T2-weighted sagittal MR localizer sequence.
B, Imaging plane prescription (white lines) for T2-weighted MR sequence parallel to the uterine long-axis.
C, Imaging plane prescription (white lines) for T2-weighted MR sequence orthogonal to the uterine long-axis.
S2
AJR:189, September 2007
Downloaded from www.ajronline.org by 107.167.99.125 on 12/27/14 from IP address 107.167.99.125. Copyright ARRS. For personal use only; all rights reserved
Imaging of Congenital Uterine Anomalies
categories. In those situations in which the identified anomaly does
not fit into a category, it is more important to accurately describe
the component parts of the anomaly rather than force it into a category that does not fully describe it [2].
A basic understanding of the embryologic model of uterovaginal development assists in understanding the anomalies that this
activity addresses. Early in gestation, the distal segments of the
paired mllerian ducts migrate caudally and medially, where
they fuse inferiorly forming the uterovaginal canal [3, 4]. There
is a residual, midline dividing septum that regresses in a caudal
to cephalad direction resulting in a single-lumen uterovaginal canal. Incomplete development of one of the mllerian ducts, failure of fusion of the mllerian ducts, or failure of septal resorption
can result in the types of anomalies presented [3, 4].
Type II anomalies (unicornuate) represent partial or complete
unilateral hypoplasia of one of the mllerian ducts. Type III
anomaly (uterus didelphus) results from near complete failure of
mllerian duct fusion. Type IV anomaly (bicornuate uterus) is
caused by incomplete fusion of the mllerian ducts at the level of
the fundus. Type V anomaly (septate) is the result of partial or
complete failure of septal resorption after fusion of the mllerian
ducts. Last, type VI anomaly (arcuate) is a result of nearly complete septal resorption with a morphology that most closely approximates normal, and it is uncertain whether the arcuate uterus
is a normal variant or a true anomaly [3].
Mllerian duct anomalies are often first identified on hysterosalpingography. Additional imaging studies such as MRI are
typically required to further evaluate and characterize these
anomalies as will be described in the scenarios of this educational
activity. MRI has a reported accuracy up to 100% in evaluation
of these anomalies [2].
Specific details concerning MRI sequences used in the evaluation
of mllerian duct anomalies can be found in the literature [3]. In general terms, the basic imaging sequences needed are:
T2-weighted localizer sequence in a sagittal orientation
to the pelvis (Fig. 2A). This aids in identifying the position and orientation of the uterus for additional imaging
sequences.
T2-weighted sequence oriented parallel to the long axis of
the uterus planned from the sagittal localizer sequence (Fig.
2B). Proper orientation of this sequence is critical because it
best depicts the external fundal contour of the uterus. T2
weighting is important because it allows identification of the
zonal anatomy of the uterus.
T2-weighted sequence oriented orthogonal to the long-axis
plane selected in the second sequence (Fig. 2C). This sequence
aids in determining the extent of a uterine septum (complete
or partial) if one is present [5].
T1-weighted sequence axial to the pelvis. T1 weighting is valuable in identification of blood products as some of these anomalies are associated with obstructive signs and symptoms.
T2-weighted, large field-of-view, coronal sequence to evaluate the kidneys. Many of the mllerian duct anomalies are
associated with renal anomalies.
Scenario 1
QUESTION 1
What type of congenital uterine anomaly is shown
in Figure 3?
A. Bicornuate uterus.
B. Unicornuate uterus without a rudimentary horn.
C. Unicornuate uterus with a communicating, cavitary,
rudimentary horn.
D. Unicornuate uterus with a noncommunicating, cavitary,
rudimentary horn.
E. Partial septate uterus.
QUESTION 2
Concerning a unicornuate uterus, which of the
following is correct?
A. It is the most common of the mllerian duct anomalies.
B. The minority of cases of unicornuate uterus have a rudimentary horn.
C. It is associated with poor pregnancy outcomes.
D. Unicornuate uterus with a rudimentary horn does not require surgical correction.
E. It is least commonly associated with renal anomalies.
AJR:189, September 2007
Clinical History
Hysterosalpingography was performed for recurrent pregnancy
loss. MRI was obtained subsequent to hysterosalpingography.
Solution to Question 1
In this case only one uterine horn is filled on the hysterosalpingogram (Fig. 3A). Bicornuate uterus is characterized by two separate uterine horns filling during hysterosalpingography, with each
horn having a fusiform appearance [4]. Septate and bicornuate
uteri can have a similar appearance on a hysterosalpingogram and
often cannot be differentiated by hysterosalpingography [4]. Option A is not the best response.
A unicornuate uterus is diagnosed on hysterosalpingography by
filling of a small, fusiform uterine cavity that tapers at its apex and
is often shifted to one side of the pelvis. It resembles one horn of a bicornuate uterus [4]. The presence of a rudimentary horn, if it is noncommunicating, cannot be determined by hysterosalpingography.
Based on the hysterosalpingogram alone, this patient could have
several possible anomalies. The patient could have a unicornuate
uterus with a noncommunicating cavitary rudimentary horn, with
a noncavitary rudimentary horn, or with no rudimentary horn [2].
Another possibility would include a uterus didelphus with only one
cervix recognized and cannulated by the physician or a uterus didelphus with a blind hemivagina (not possible to see the second cervix).
S3
Downloaded from www.ajronline.org by 107.167.99.125 on 12/27/14 from IP address 107.167.99.125. Copyright ARRS. For personal use only; all rights reserved
Dykes et al.
Fig. 3Hysterosalpingogram for recurrent pregnancy loss. MRI obtained subsequent to hysterosalpingography.
A, Hysterosalpingogram shows one uterine horn filled during injection (arrow).
B, Axial T2 MRI shows fusiform uterine cavity with typical trilaminar appearance of high-signal endometrium (star), low-signal junctional zone (long arrow), and intermediatesignal myometrium (short arrow) of uterus seen in right side of pelvis. This corresponds to cavity opacified on hysterosalpingogram.
C, Axial T2 MRI slightly lower in pelvis shows second endometrial cavity in left side of pelvis with high-signal endometrium (arrow). There is clear separation of this second
cavity from more superior cavity by intermediate-signal myometrium.
Last, a complete septate uterus with opacification of only one horn
is a possibility, although this is much less likely than a unicornuate
uterus or unrecognized uterus didelphus. The MRI (Fig. 3C) shows
two separate uterine horns, clearly separated from one another by
myometrial tissue. The smaller, left-sided uterine horn is a rudimentary horn. Option B is not the best response.
A communicating rudimentary horn of a unicornuate uterus
should be identified as filling with contrast material on the hysterosalpingogram [4] or shown to communicate with the unicornuate horn on MRI. In this case, both hysterosalpingography
and MRI clearly show that this rudimentary horn is noncommunicating. Option C is not the best response.
A rudimentary horn in a unicornuate uterus can be cavitary
(containing endometrium) or noncavitary (containing fibrous
tissue). When endometrium is present in the rudimentary horn
(cavitary), high-signal zonal anatomy can be seen on MRI [2]
(Fig. 3C). When endometrium is absent (noncavitary), generally
the tissue is fibrous and low signal on T2-weighted MR images
(Figs. 4A4C). As discussed previously, a rudimentary horn in a
unicornuate uterus can also be communicating or noncommunicating with the unicornuate horn. The combination of the hysterosalpingography and MRI confirms that this patient has a
noncommunicating rudimentary horn that has high signal intensity of endometrium (cavitary). Option D is the best response.
A partial septate uterus would have two cavities filling on hysterosalpingogram, rather than one cavity as seen on this patients examination. Option E is not the best response.
Solution to Question 2
Unicornuate uterus accounts for about 20% of mllerian duct
anomalies [2]. It is not the most common anomaly. Option A is
not the best response.
Fig. 4Hysterosalpingogram and subsequent MRI.
A, Hysterosalpingogram demonstrating filling of a left-sided unicornuate uterus (arrow).
B, Axial T2 MRI shows the unicornuate horn corresponding to that seen on the hysterosalpingogram (arrow). A low-signal-intensity fibrous rudimentary horn is seen in the
right pelvis (arrowhead).
C, Coronal T2 MRI better demonstrates the noncavitary (no high-signal endometrium) right-sided rudimentary horn attached to the left-sided unicornuate horn (arrow).
S4
AJR:189, September 2007
Downloaded from www.ajronline.org by 107.167.99.125 on 12/27/14 from IP address 107.167.99.125. Copyright ARRS. For personal use only; all rights reserved
Imaging of Congenital Uterine Anomalies
An isolated unicornuate horn (no rudimentary horn) is found in
35% of unicornuate uteri. Sixty-five percent of unicornuate uteri
have a rudimentary horn [2]. Option B is not the best response.
Although a patient with a unicornuate uterus can have a normal pregnancy, there is an increased risk of pregnancy loss and premature labor [1, 2, 4]. Spontaneous abortion rates reportedly
range between 41% and 62% and premature birth rates between
10% and 20%. Other complications include abnormal fetal lie and
intrauterine growth restriction [2]. Option C is the best response.
A noncommunicating, cavitary (contains endometrium), rudimentary horn associated with a unicornuate uterus is important
and once identified is usually surgically resected. Obstetric and nonobstetric complications associated with this anomaly include dysmenorrhea and hematometra at menarche, endometriosis, and
ectopic pregnancy implanting in the rudimentary horn [2, 6]. Pregnancy implanting in the rudimentary horn usually has a disastrous
outcome, with most resulting in uterine rupture [2, 6]. Communicating, cavitary rudimentary horns are also considered for surgical
removal because a pregnancy that implants in the rudimentary
horn rarely yields viable offspring [2]. Noncavitary (no endometrium), rudimentary horns would not have complications of
hematometra, dysmenorrhea, and endometriosis. Although a patient potentially could still have an ectopic pregnancy implant in a
Fallopian tube connected to a noncavitary, rudimentary horn, the
current recommendation for this subset of patients is that they do
not require surgical resection [2]. Most patients with rudimentary
horns require surgical correction. Option D is not the best response.
Renal anomalies are more commonly associated with unicornuate uterus than with the other mllerian duct anomalies and are
reported in up to 40% of cases. The associated renal anomaly is
typically ipsilateral to the rudimentary horn [2]. Option E is not
the best response.
Conclusion
The diagnosis in this case is unicornuate uterus with a noncommunicating, cavitary, rudimentary horn. The correct diagnosis hinges on
proper integration of hysterosalpingography and pelvic MRI. The
hysterosalpingogram identifies the typical appearance of a unicornuate uterus with opacification of a small, single uterine horn. The two
other possible diagnoses, complete septate and unrecognized uterus
didelphus, can be effectively excluded by combining the information
available from hysterosalpingography and pelvic MRI. Both horns
of a complete septate uterus will typically opacify on hysterosalpingography. On MRI, a complete septate uterus will have two separate
and relatively symmetric uterine horns rather than a hypoplastic or
absent uterine horn seen with unicornuate uterus. Only one uterine
horn may fill on hysterosalpingography in an unrecognized uterus didelphus simulating a unicornuate uterus. However, MRI can definitively distinguish between these two diagnoses, with the uterus
didelphus having two nonfused uterine horns and two cervices with
only minor degrees of fusion at the cervices.
It is important to identify whether there is a rudimentary horn
associated with the unicornuate uterus. An excellent imaging modality to accomplish this task is a pelvic MRI [2]. If MRI confirms
that the patient has a unicornuate uterus with a rudimentary horn,
it is important to determine whether the rudimentary horn has endometrial signal within it on T2 images (cavitary) or is fibrous tissue
(noncavitary). Cavitary rudimentary horns generally require surgical removal for the reasons cited previously whereas noncavitary
horns typically do not [2, 7]. It is also important to remember that
mllerian duct anomalies are frequently associated with renal
anomalies. Renal abnormalities are more commonly associated
with unicornuate uterus than any other mllerian anomaly, and
the most common abnormality is ipsilateral renal agenesis [2].
Scenario 2
cavities, usually at the uterine isthmus. A complete bicornuate
uterus has a separating cleft of tissue that extends to the internal
cervical os, while lesser degrees of separation of the two uterine
horns constitute a partial bicornuate uterus [2, 4]. This patient has
two completely separate, noncommunicating uterine horns. An
Clinical History
No clinical history was available. During hysterosalpingography two separate cervices were visualized (Fig. 5).
Solution to Question 3
A bicornuate uterus has two symmetric uterine cavities that fuse
caudally and have some degree of communication between the two
QUESTION 3
What type of congenital uterine anomaly does the
patient in Figure 5 have?
A. Complete bicornuate uterus.
B. Partial bicornuate uterus.
C. Uterus didelphus.
D. Arcuate uterus.
E. Partial septate uterus.
AJR:189, September 2007
QUESTION 4
Concerning uterus didelphus, which of the
following is correct?
A. It is the most common congenital uterine anomaly.
B. It can be confused with a unicornuate uterus on
hysterosalpingograms.
C. The minority of cases have an associated longitudinal
vaginal septum.
D. It is caused by complete failure of resorption of the
uterovaginal septum.
E. Symptoms are common in nonobstructive forms of uterus
didelphus.
S5
Dykes et al.
Downloaded from www.ajronline.org by 107.167.99.125 on 12/27/14 from IP address 107.167.99.125. Copyright ARRS. For personal use only; all rights reserved
Fig. 5Two separate cervices visualized.
A and B, Two separate injections on hysterosalpingography. Two cervices were visualized and cannulated
separately. Opacified uterine horns do not communicate and are widely divergent (arrows).
B
Fig. 6Two separate cervices visualized.
A, T2 axial MRI show two, widely separate uterine
horns in a patient with uterus didelphus (arrows).
B, T2 coronal MRI demonstrates separate, noncommunicating uterine horns (black arrows) and cervices
(arrowheads) and duplicated vagina (white arrows).
B
Fig. 7Woman with vaginal bleeding and abdominal
pain.
A, Uterus didelphus. Coronal T2 image demonstrates a
dilated right-sided uterine horn (arrow) and a nondilated left-sided uterine horn (arrowhead).
B, Uterus didelphus. Axial T2 image demonstrates the
dilated right-sided uterine horn (arrow), nondilated
left-sided uterine horn (arrowhead), and a massively
dilated, obstructed right hemivagina (star).
uncommon anomaly, the bicornuate, bicollis (two cervices) uterus
will also have some degree of communication between the uterine
horns in most cases [2]. Options A and B are not the best responses.
Uterus didelphys is caused by complete or near complete failure
of fusion of the paired mllerian ducts during embryologic development. The result is two separate, symmetric uterine cavities with
two cervices and no communication between the uterine cavities.
Injection of contrast material into each separate cervix independently opacifies a uterine horn that resembles unicornuate uterus
morphology [4]. Another uncommon anomaly that could have a
similar appearance on hysterosalpingography is a complete septate
S6
uterus with a duplicated cervix [6]. MRI distinguishes between the
complete septate which has a fused, external uterine fundal contour, and the uterus didelphys, with its widely separate uterine
horns and duplicated cervices as shown in a different patient in Figures 6A and 6B. Option C is the best response.
Arcuate uterus is characterized on hysterosalpingography as having a mild, broad indentation at the superior aspect of a single uterine cavity. Although originally classified as a mild form of bicornuate
uterus, newer classification systems place arcuate uterus into a separate category [1, 3, 8]. Arcuate uterus has little to no adverse impact on reproduction [1]. Option D is not the best response.
AJR:189, September 2007
Imaging of Congenital Uterine Anomalies
Downloaded from www.ajronline.org by 107.167.99.125 on 12/27/14 from IP address 107.167.99.125. Copyright ARRS. For personal use only; all rights reserved
A partial septate uterus would have two cavities filling on hysterosalpingography injecting a single cervix. This case required injection of two separate cervices to opacify separate uterine cavities
on hysterosalpingography. Option E is not the best response.
Solution to Question 4
Uterus didelphus constitutes only 5% of congenital uterine
anomalies [2] and is not the most common mllerian anomaly.
Option A is not the best response.
Uterus didelphus is associated with a longitudinal vaginal septum in nearly 75% of cases [2, 6]. These longitudinal vaginal septae may be further complicated by a transverse septum
obstructing one hemivagina. This combination of factors can result in nonvisualization of one of the hemivagina and the associated cervix. The resultant injection of the only visualized
cervix appears as a unicornuate uterus on hysterosalpingography [4]. MRI can help identify an obstructed uterus didelphus
[7] (Figs. 7A and 7B). Option B is the best response.
Most (75%) of cases of uterus didelphys have an associated longitudinal vaginal septum [2]. So, Option C is not the best response.
Uterus didelphys is caused by near complete failure of fusion
of the mllerian ducts, not failure of resorption once fusion has
occurred [2, 3]. Option D is not the best response.
Patients with nonobstructive forms of uterus didelphus are
usually asymptomatic, whereas patients who have obstructive
forms develop symptoms at menarche and have complications
related to retrograde menstrual flow, such as pelvic adhesions
and endometriosis [2]. Option E is not the best response.
Conclusion
Uterus didelphus is caused by complete or near-complete failure
of fusion of the paired mllerian ducts during embryologic development. The hysterosalpingography and images obtained after
injection of each cervix are characteristic. MRI demonstrates two
separate uteri with divergent horns, as expected with failure of fusion of the mllerian ducts. Two separate cervices are also seen
with no or only minor degrees of fusion (Figs. 6A and 6B) [2].
As mentioned previously, obstructive symptoms can occur
when the longitudinal vaginal septum is complicated by a transverse septum. These symptoms include hematometrocolpos and
endometriosis [2]. Uterus didelphus does have an adverse impact
on reproduction, similar to that of a unicornuate uterus [1, 9]. It
has the highest possibility for successful pregnancy of the mllerian anomalies except for arcuate uterus [9].
Solution to Question 5
Uterus didelphus is characterized on MRI as having two separate uterine cavities that are widely separate and two cervices
with little to no fusion. There is also commonly a vaginal septum.
There is no communication between the uterine cavities [2]. Figure 8 shows two uterine cavities, but there is clearly communication between the cavities in the lower uterine segment and a
single cervix. Option A is not the best response.
Septate uterus, either partial or complete, is characterized on
MRI as having two separate uterine cavities, but the external fundal contour is unified. This is seen on MRI has having either a convex or flat uterine fundal contour, or a shallow concavity (< 1 cm
depth) [2]. This case clearly has a deep fundal cleft with two separate uterine cavities. Neither option B nor C is the best response.
Partial bicornuate uterus is defined as having a tissue cleft partially separating the uterine horns with communication of the
two horns generally in the lower uterine segment. Additionally,
a bicornuate uterus will have a nonunified, external fundal contour seen as a cleft at least 1 cm deep in the external fundal contour [2]. This case shows both of these imaging features. Option
D is the best response.
QUESTION 5
QUESTION 6
Scenario 3
Clinical History
Two uterine cavities were seen on a previous hysterosalpingogram after cannulating a single cervix.
What type of congenital uterine anomaly is shown
in Figure 8?
Concerning a bicornuate uterus, which of the
following is correct?
A. Uterus didelphus.
B. Partial septate uterus.
C. Complete septate uterus.
D. Partial bicornuate uterus.
E. Complete bicornuate uterus.
A. It is more common than a septate uterus.
B. It can reliably be differentiated from a septate uterus on
routine hysterosalpingography.
C. It is differentiated from a septate uterus on MRI by identifying myometrium between the two uterine horns.
D. It is often complicated by cervical insufficiency.
E. It is caused by failure of resorption of the uterovaginal septum during fetal development.
AJR:189, September 2007
S7
Dykes et al.
Downloaded from www.ajronline.org by 107.167.99.125 on 12/27/14 from IP address 107.167.99.125. Copyright ARRS. For personal use only; all rights reserved
Fig. 8Two uterine cavities seen on previous hysterosalpingogram after cannulating single cervix.
A, T2 axial MRI shows two separate uterine cavities
(white arrows) separated by deep fundal cleft (black
arrow) at uterine fundus. Single cervix is present.
B, T2 coronal MRI shows communication of two uterine cavities in lower uterine segment (arrow).
Complete bicornuate uterus is defined as having an external
uterine fundal contour characteristic of bicornuate morphology
(described above), with separation of the two uterine horns by a
tissue cleft extending to the internal cervical os [6]. This case
shows separation of the two uterine horns only to the lower uterine
segment, where communication occurs. This tissue cleft does not
extend to the internal cervical os. Option E is not the best response.
Solution to Question 6
Bicornuate uterus accounts for approximately 10% of mllerian duct anomalies, whereas septate uterus accounts for about
55% of cases [2]. Option A is not the best response.
Two separate uterine horns are seen in both the septate uterus
and the bicornuate uterus on hysterosalpingography [4]. Typically, the uterine horns are separated by a wide angle (105 or
more) in a bicornuate uterus on hysterosalpingography, whereas
with a septate uterus the uterine horns are separated by a narrow
angle (75 or less) [4]. However, there is a large amount of overlap
in the findings of a septate and bicornuate uterus on routine hysterosalpingograms, and the reported diagnostic accuracy of hysterosalpingography alone in distinguishing between these two
anomalies is 55% [2]. Thurmond et al. [10] reported a technical innovation in hysterosalpingography, the uterine pushpull
Fig. 9Double uterine horn is present on hysterosalpingogram.
Free spill of contrast into peritoneal cavity allows direct
visualization of convex fundal contour (arrowheads)
confirming that this is septate uterus, not bicornuate.
S8
technique. Gentle cycles of manual traction-relaxation were performed using a cervical vacuum cup after free-spill of contrast material from at least one Fallopian tube in an attempt to move the
intraperitoneal contrast around the uterine fundus, allowing visualization of the fundal contour. This technique was not used with
either a balloon catheter or a tenaculum and also was not used
when patients had tubal disease or other technical problems that
limited the flow of contrast into the peritoneal cavity. Forty-four
percent of the patients in their series could not have this technique
applied (for technical and patient-related reasons), and 58% of the
patients imaged using this technique did not show adequate visualization of the fundal contour. One percent of the patients in their
series experienced moderate to severe pain and 4% had self-limited
vasovagal symptoms when this technique was attempted.
Whether this technique is used or not, when a double uterine horn
is identified on hysterosalpingography, and if intraperitoneal contrast material is seen outlining the uterine fundus, close inspection
of the fundal contour may allow distinction between septate and
bicornuate uterus (Fig. 9). Option B is not the best response.
MRI is an excellent imaging tool that can reliably differentiate
between bicornuate and septate uterine anomalies. The characteristic diagnostic feature of a bicornuate uterus is an external uterine
fundal cleft at least 1 cm deep seen on images that are acquired parallel to the long axis of the uterus. A septate uterus will have either
a shallow cleft (< 1 cm depth), a flat contour, or a convex external
uterine contour [2]. The presence or absence of myometrial tissue between the two uterine horns is not helpful in distinguishing between
septate and bicornuate uteri because it may be absent or present in
a septate uterus [2]. Option C is not the best response.
Bicornuate uterus is reported to have the highest association
with cervical insufficiency of the mllerian duct anomalies,
reaching 38%, and prophylactic cerclage may be indicated to improve fetal survival rates [2]. Option D is the best response.
Bicornuate uterus is caused embryologically by a defect in
mllerian duct fusion not resorption [1, 3]. Option E is not the
best response.
Conclusion
Bicornuate uterus is caused by a defect in mllerian duct fusion
during embryologic development. Although the diagnosis may be
AJR:189, September 2007
Downloaded from www.ajronline.org by 107.167.99.125 on 12/27/14 from IP address 107.167.99.125. Copyright ARRS. For personal use only; all rights reserved
Imaging of Congenital Uterine Anomalies
suggested on hysterosalpingography by showing opacification of
two uterine horns that are divergent from each other, there is significant overlap between this appearance and a septate uterus.
MRI is an excellent tool in both diagnosing bicornuate uterus and
differentiating it from a septate uterus. Differentiation of bicornuate from septate uterus has important implications for both prognosis and therapy. Septate uterus has higher rates of spontaneous
abortions, worse obstetric outcomes, and lower fetal survival rates
compared with bicornuate uterus [1, 2, 6]. Septate uterus is often
treated with hysteroscopic resection of the septum [1, 2, 4]. Bicornuate uterus generally does not require surgical intervention [2].
The key imaging feature to assess is the external contour of the
uterine fundus. A deep fundal cleft (> 1 cm) is consistent with a bicornuate uterus, whereas a shallow cleft, a flat contour, or a convex
fundal contour is diagnostic of a septate uterus. It is also important
to determine whether a bicornuate uterus is complete or partial because spontaneous abortion and preterm labor are reportedly
higher with a complete bicornuate compared to partial [2].
Scenario 4
Solution to Question 8
The septate uterus is characterized by uterine fundal unification,
typically seen on MRI as a flat or convex fundal contour. Bicornuate
uterus is characterized on MRI as having uterine fundal concavity
greater than 1 cm depth. It is, however, important to not interpret
slight degrees of fundal concavity (< 1 cm) as indicative of partial bicornuate morphology. Septate uterus can have slight degrees of
uterine fundal concavity [2]. Option A is not the best response.
Septate uterus constitutes about 55% of congenital uterine
anomalies [2]. It is the most common anomaly. Option B is not the
best response.
Septate uterus is associated with high rates of spontaneous abortions, ranging in the literature from 26% to 94% [1, 2, 4]. The most
common congenital uterine anomaly identified in patients presenting with recurrent, spontaneous abortions is a septate uterus [4].
Septate uterus also has the worst obstetric outcomes of the congenital uterine anomalies, with increased premature birth rates and
lower fetal survival rates [2, 4]. Option C is the best response.
Repair of a septate uterus is best done by hysteroscopic resection of the septum [1, 2, 4]. Transabdominal metroplasty is used
for correction of bicornuate anomalies [2, 6] when clinically indicated. Bicornuate uterus, however, generally does not require surgical intervention [2]. Option D is not the best response.
Resection of the septum does improve reproductive outcome
for patients with a septate uterus experiencing repeated, spontaneous abortions [2]. Option E is not the best response.
Clinical History
Recurrent pregnancy loss.
Solution to Question 7
On hysterosalpingography, a bicornuate or a septate uterine
anomaly is seen (Fig. 10A). The MRI (Fig. 10B) shows a flat to
mildly convex external uterine fundal contour that is characteristic of a septate uterus. Complete septate uterus is characterized
by a septum that separates the two uterine cavities extending to
the external cervical os [2]. T2 MR images transverse to the cervix may help in determining whether a septation is partial or
complete [5]. This case shows a septum, but it extends only to
the lower uterine segment on the hysterosalpingogram and the
MRI. Also, there is clearly no septation in the cervix on the MRI.
Option A is the best response.
The uterine septum in this case extends only to the lower uterine
segment, not to the external cervical os as would be characteristic
of a complete septate uterus. Option B is not the best response.
Although the possibility of bicornuate uterus could be considered
on the hysterosalpingogram, the MRI clearly demonstrates a uterine fundal contour consistent with a septate uterus, not bicornuate
morphology. Neither Option C nor D are the best responses.
Uterus didelphus requires cannulation of two separate cervices
to opacify the separate uterine cavities, unlike this patients hysterosalpingogram. Also, the MRI appearance of a uterus didelphus
shows complete lack of unification of the uterine horns unlike this
patients MRI (Fig. 10B) showing uterine fundal configuration
consistent with unification. Option E is not the best response.
QUESTION 8
QUESTION 7
What type of congenital uterine anomaly is shown
in Figure 10?
A. Partial septate uterus.
B. Complete septate uterus.
C. Partial bicornuate uterus.
D. Complete bicornuate uterus.
E. Uterus didelphus.
AJR:189, September 2007
Concerning a septate uterus, which of the following
is correct?
A. Diagnosis is excluded on MRI by any concavity in the external uterine fundal contour.
B. It is the least common of the congenital uterine anomalies.
C. It is associated with the worst obstetric outcomes of the
mllerian duct anomalies.
D. Surgical correction requires a transabdominal metroplasty.
E. Resection of the septum does not improve reproductive
outcome.
S9
Downloaded from www.ajronline.org by 107.167.99.125 on 12/27/14 from IP address 107.167.99.125. Copyright ARRS. For personal use only; all rights reserved
Dykes et al.
Fig. 10Woman with recurrent pregnancy loss.
A, Hysterosalpingogram with injection of one cervix demonstrates two separate uterine cavities with communication in lower uterine segment.
B, Axial T2 MRI shows flat external uterine fundal contour (arrowheads).
C, Axial T2 MRI lower in pelvis demonstrates single cervix with no septation (arrowhead).
Fig. 11No clinical history available.
A, T2 axial MRI: Septate uterus, complete. Arrowhead
demonstrates shallow (< 1 cm depth) fundal concavity,
still consistent with septate morphology.
B, T2 axial MRI slightly lower in pelvis. White arrow
shows long fibrous (low signal) septum extending to
external cervical os consistent with complete septate
uterus. Arrowhead shows shallow cleft in fundus, still
consistent with septate uterus.
Conclusion
Hysterosalpingograms cannot reliably differentiate septate
from bicornuate uterine anomalies. A cross-sectional imaging
study (sonography or MRI) is generally required to distinguish between these two anomalies that together comprise nearly two
thirds of congenital uterine anomalies. It is critical to correctly distinguish between septate and bicornuate anomalies because bicornuate uterus uncommonly needs surgical intervention, whereas
septate uterus commonly does. Also, the type of surgical intervention is different; transabdominal metroplasty for bicornuate
uterus versus hysteroscopic resection of the septum for a septate
uterus. In particular, it is important to not misinterpret slight concavity of the uterine fundal contour as bicornuate morphology.
Figures 11A and 11B are of a patient with a septate uterus with a
shallow uterine fundal cleft (< 1 cm depth) separating two uterine
cavities. This is still consistent with septate morphology.
B
References
1. Raga F, Bauset C, Remohi J, et al. Reproductive impact of congenital Mllerian anomalies. Hum Reprod 1997; 12:22772281
2. Troiano RN, McCarthy SM. Mllerian duct anomalies: imaging and clinical
issues. Radiology 2004; 233:1934
3. The American Fertility Society classifications of adnexal adhesions, distal tubal obstruction, tubal occlusion secondary to tubal ligation, tubal pregnancies,
Mllerian anomalies and intrauterine adhesions. Fertil Steril 1988; 49:944955
4. Ott DJ, Fayez JA, Zagoria RJ. Hysterosalpingography: a text and atlas, 2nd
ed. Baltimore, MD: Williams & Wilkins, 1998:67
5. Saleem SN. MR imaging diagnosis of uterovaginal anomalies: current state
of the art. RadioGraphics 2003; 23:e13
6. Cunningham FG, Leveno KJ. Williams obstetrics, 22nd ed. New York, NY.
McGraw-Hill, 2005:953956
7. Minto CL, Hollings N, Hall-Craggs M, Creighton S. Magnetic resonance imaging in the assessment of complex Mllerian anomalies. Br J Obstet Gynaecol 2001; 108:791797
8. Ubeda B, Paraira M, Alert E, Abuin RA. Hysterosalpingography: spectrum of
normal variants and nonpathologic findings. AJR 2001; 177:131135
9. Imaoka I, Wada A, Matsuo M, et al. MR imaging of disorders associated
with female infertility: use in diagnosis, treatment, and management. RadioGraphics 2003; 23:14011421
10. Thurmond AS, Jones MK, Matteri R. Using the uterine pushpull technique to
outline the fundal contour on hysterosalpingography. AJR; 175:359361
ARRS members earn free CME and SAM credit at www.arrs.org.
Go to left-hand menu bar under Publications/Journals/SAM articles.
S10
AJR:189, September 2007
Vous aimerez peut-être aussi
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Admission Prospectus2022 1 PDFDocument10 pagesAdmission Prospectus2022 1 PDFstudymba2024Pas encore d'évaluation
- Factors Influencing The Selection Of: MaterialsDocument22 pagesFactors Influencing The Selection Of: MaterialsMaulik KotadiyaPas encore d'évaluation
- Frankenstein ExtractDocument1 pageFrankenstein ExtractAnnePas encore d'évaluation
- Linberg V MakatiDocument2 pagesLinberg V MakatiChimney sweepPas encore d'évaluation
- Lotte Advanced Materials Co., LTD.: ISO 9001:2015, KS Q ISO 9001:2015Document2 pagesLotte Advanced Materials Co., LTD.: ISO 9001:2015, KS Q ISO 9001:2015Tayyab KhanPas encore d'évaluation
- 2002PCDFCADocument78 pages2002PCDFCATin NguyenPas encore d'évaluation
- Opening StrategyDocument6 pagesOpening StrategyashrafsekalyPas encore d'évaluation
- Netflix Annual Report 2010Document76 pagesNetflix Annual Report 2010Arman AliPas encore d'évaluation
- 2018-2021 VUMC Nursing Strategic Plan: Vision Core ValuesDocument1 page2018-2021 VUMC Nursing Strategic Plan: Vision Core ValuesAmeng GosimPas encore d'évaluation
- Manuall Cryton-Yamaha 2015Document57 pagesManuall Cryton-Yamaha 2015Abel PachecoPas encore d'évaluation
- Improving Radar Echo Lagrangian Extrapolation Nowcasting by Blending Numerical Model Wind Information: Statistical Performance of 16 Typhoon CasesDocument22 pagesImproving Radar Echo Lagrangian Extrapolation Nowcasting by Blending Numerical Model Wind Information: Statistical Performance of 16 Typhoon CasesLinh DinhPas encore d'évaluation
- 2017 Lecture 3 Metal Carbonyls PDFDocument28 pages2017 Lecture 3 Metal Carbonyls PDFMahnoor FatimaPas encore d'évaluation
- PL SQL Exercise6Document2 pagesPL SQL Exercise6Nishant AndhalePas encore d'évaluation
- Islami Bank Bangladesh Limited: Ibbl Ibanking ServiceDocument2 pagesIslami Bank Bangladesh Limited: Ibbl Ibanking ServiceShaikat AlamPas encore d'évaluation
- Robotech Hannibal Digital 114dpi V1.0Document119 pagesRobotech Hannibal Digital 114dpi V1.0nonfarb14thPas encore d'évaluation
- Problem Sheet 3 - External Forced Convection - WatermarkDocument2 pagesProblem Sheet 3 - External Forced Convection - WatermarkUzair KhanPas encore d'évaluation
- ITR-C (Instrument) 16cDocument1 pageITR-C (Instrument) 16cMomo ItachiPas encore d'évaluation
- RCU II Open Protocol Communication Manual FV 9 10 31 08 PDFDocument17 pagesRCU II Open Protocol Communication Manual FV 9 10 31 08 PDFAndrés ColmenaresPas encore d'évaluation
- Congenital Abnormalities of The Female Reproductive TractDocument14 pagesCongenital Abnormalities of The Female Reproductive TractMary SheshiraPas encore d'évaluation
- Syllabus Financial AccountingDocument3 pagesSyllabus Financial AccountingHusain ADPas encore d'évaluation
- Management of Odontogenic Infection of Primary Teeth in Child That Extends To The Submandibular and Submental Space Case ReportDocument5 pagesManagement of Odontogenic Infection of Primary Teeth in Child That Extends To The Submandibular and Submental Space Case ReportMel FAPas encore d'évaluation
- Yusof Ishak Secondary School Humanities Study Tour Ho Chi Minh City, VietnamDocument19 pagesYusof Ishak Secondary School Humanities Study Tour Ho Chi Minh City, Vietnamadamant751Pas encore d'évaluation
- Basic Customer Service SkillsDocument90 pagesBasic Customer Service SkillsGillian Delos ReyesPas encore d'évaluation
- A Guide To Energy Efficiency ComplianceDocument16 pagesA Guide To Energy Efficiency ComplianceOARIASCOPas encore d'évaluation
- Leading Airline Emirates Boosts Leisure Travel Sales - : Peakwork Case Study: EmiratesDocument3 pagesLeading Airline Emirates Boosts Leisure Travel Sales - : Peakwork Case Study: EmiratesAhmed AbboudPas encore d'évaluation
- Clostridium BotulinumDocument37 pagesClostridium Botulinummaria dulcePas encore d'évaluation
- Check To Make Sure You Have The Most Recent Set of AWS Simple Icons Creating DiagramsDocument48 pagesCheck To Make Sure You Have The Most Recent Set of AWS Simple Icons Creating DiagramsarunchockanPas encore d'évaluation
- Electrochemistry DPP-1Document2 pagesElectrochemistry DPP-1tarunPas encore d'évaluation
- Ajol File Journals - 404 - Articles - 66996 - Submission - Proof - 66996 4813 136433 1 10 20110608Document12 pagesAjol File Journals - 404 - Articles - 66996 - Submission - Proof - 66996 4813 136433 1 10 20110608Lovely Joy Hatamosa Verdon-DielPas encore d'évaluation
- Va797h 15 Q 0019 A00001003Document35 pagesVa797h 15 Q 0019 A00001003Hugo GranadosPas encore d'évaluation