Académique Documents
Professionnel Documents
Culture Documents
9 Ambarisha-Etal
Transféré par
editorijmrhsTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
9 Ambarisha-Etal
Transféré par
editorijmrhsDroits d'auteur :
Formats disponibles
DOI: 10.5958/2319-5886.2015.00152.
6
Open Access
Available online at: www.ijmrhs.com
Research article
ADVERSE MATERNAL AND PERINATAL OUTCOMES IN GESTATIONAL
DIABETES MELLITUS
1
2 *
Ambarisha Bhandiwad , Divyasree B , Surakshith L Gowda
ARTICLE INFO
th
Received: 5 Jun 2015
th
Revised: 24 Jul 2015
th
Accepted: 5 Sep 2015
1
Authors details:
Professor and
2,3
Head, Junior Resident Department
of OBGY, JSS Medical College, JSS
University, Mysore, India
Corresponding author: Surakshith L
Gowda
Junior Resident Department of OBGY,
JSS Medical College, JSS University,
Mysore, India
Email: surakshithlgowda@gmail.com
Keywords: Gestational Diabetes
Mellitus, Maternal and Fetal
complications, Macrosomia,
Preeclampsia
ABSTRACT
Introduction: Women with Gestational Diabetes Mellitus (GDM) are at
increased risk for many other health concerns with short and long-term
implications for both mother and child. They are at higher risk for glucosemediated macrosomia, hypertension, birth trauma, respiratory distress,
hypoglycemia, hyperbilirubinemia with increased neonatal intensive care
unit (NICU) admissions. Postpartum complications include obesity and
impaired glucose tolerance in the offspring and diabetes and cardiovascular
disease in the mothers. Objectives: To study the incidence of maternal
and fetal co-morbidities associated with GDM. Materials and Methods:
This is a retrospective observational study where cases with GDM were
analyzed for maternal and fetal complications. Results: 189 cases were
detected to be Gestational Diabetes Mellitus, out of which 63.49% cases
developed co-morbidities with GDM. 11.11% cases developed
preeclampsia, 9.52% had polyhydramnios, 5.8% patients went into preterm
labour, 3 cases had Antepartum Haemorrhage and one case had
Postpartum Haemorrhage. 19.57% cases developed macrosomia,
hypoglycemia was seen in 7.40% babies and hyperbilirubinemia in 3.70%
babies. 6 Intra Uterine Deaths and 2 still borns were documented.
Conclusion: GDM is a condition which is worth monitoring and treating,
since it has been demonstrated that good metabolic control maintained
throughout gestation can reduce maternal and fetal complications.
INTRODUCTION
Gestational Diabetes Mellitus (GDM) is commonly
defined as carbohydrate intolerance that first becomes
[1]
apparent during pregnancy. Women with GDM are at
increased risk for many other health concerns with short
and long-term implications for both mother and child.
Women with GDM are at higher risk for glucosemediated macrosomia, hypertension, adverse pregnancy
outcomes (stillbirth, birth trauma, cesarean section, preeclampsia,
eclampsia,
respiratory
distress,
hypoglycemia,
hyperbilirubinemia,
polycythemia,
hypocalcemia, increased neonatal intensive care unit
admissions) and neonatal adiposity with its long-term
[2, 3]
sequelae including childhood obesity and diabetes.
Postpartum complications include obesity and impaired
glucose tolerance in the offspring and diabetes and
[3]
cardiovascular disease in the mothers. Women who
have GDM are at higher risk of developing T2DM in the
future.This risk has been shown to be as high as 50% for
[4]
future T2DM risk.
The ADA recommends that all
women with GDM be screened at six to 12 weeks after
delivery for persistent diabetes and then every three
[5]
years thereafter
where as the DIPSI recommends to
screen women with GDM at 6 weeks, 6 months and then
yearly thereafter for persistent diabetes. This condition is
worth monitoring and treating, since it has been
demonstrated that good metabolic control maintained
throughout gestation can reduce maternal and fetal
[1]
complications.
Ambarisha et al.,
MATERIALS AND METHODS
Study design: This is a retrospective observational
study
Study period and location: The study was done
between January 2013 to December 2014, at JSS
Hospital, Mysore
Ethics approval: The study was approved by the
Institutional Ethics committee
Inclusion criteria: All antenatal patients who were
diagnosed as GDM and who delivered during the study
period available from the record section
Exclusion Criteria: Patients with oral glucose challenge
test value of <140 mg/dl, incomplete data of the patient
How GDM was diagnosed ?: All pregnant women were
screened and diagnosed with Diabetes In Pregnancy
[6]
Study group India (DIPSI) criteria i.e. irrespective of the
timing of the last meal, as and when the pregnant
women entered the antenatal clinic, she was given 75gm
oral glucose. Then two hours later, plasma glucose was
estimated by Glucose oxidase - peroxidase method. 2hr
post plasma glucose value of 140 mg/dl was diagnostic
of GDM and those patients were included in the study.
All women were screened between 24-28 weeks of
gestation and women with high risk factors such as age
>30 yrs, obesity, family history of diabetes, previous bad
obstetric history, history of GDM in previous pregnancy
were screened earlier at 12 16 weeks of gestation and
those diagnosed with GDM were included in the study,
775
Int J Med Res Health Sci. 2015;4(4):775-777
but in a normally glucose tolerant women the test was
repeated again at 32 34 weeks.
Methodology:
The incidence of maternal (i..e, Preeclampsia,
Polyhydramnios,
Preterm
labour,
Antepartum
Haemorrhage, Postpartum Haemorrhage) and fetal
complications ( i.e., Macrosomia, ICU admissions,
Hypoglycemia, Hyperbilubinemia, Intra Uterine Death,
Still born) which developed in those GDM patients were
retrospectively analyzed from the medical records and
the data was presented as percentage of complications.
RESULTS
A total of 2070 cases delivered during the study period in
which 189 cases were detected to be Gestational
Diabetes Mellitus, out of which 120 (63.49%) cases
developed co-morbidities with GDM.
Maternal complications: 21 cases (11.11%) developed
preeclampsia, 18 cases (9.52%) had polyhydramnios, 11
patients went into preterm labour i.e. 5.8%, 3 cases had
APH (1.58%) and one case had PPH.
Fetal complications: 37 cases developed macrosomia,
i.e. 19.57% (birth weight for Indian standards was taken
as >3500 gms), 22 babies were admitted to NICU and 14
developed hypoglycemia (7.40%) and 7 babies had
hyperbilirubinemia (3.70%). 6 Intra Uterine Deaths
(3.17%) and 2 still borns (1.05%) were documented.
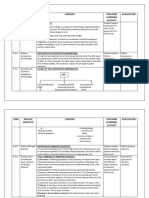
Table 1: Maternal & Fetal Complications with GDM
Maternal complications
Fetal complications
N (%)
Preeclampsia
21(11.1)
Macrosomia
37 (19.6)
Polyhydramnios 18 (9.5)
NICU
22 (11.6)
admissions
Preterm labour 11 (5.8) Hypoglycemia 14 (7.40)
Antepartum
3 (1.58)
Hyperbilirubin 7 (3.70)
Haemorrhage
emia
Postpartum
1 (0.52)
IUD
6 (3.17)
Haemorrhage
Still borns
2 (1.5)
DISCUSSION
The incidence of GDM in the present study was found to
be 9.13 %. In India the prevalence of GDM varied from
[6]
3.8 to 21% across the different regions and 63.49% of
GDM cases developed complications. Macrosomia in
this study was found to be 19.57% which is similar to a
[7]
study in which the incidence of macrosomia was 18%.
Currently, it is not known whether the overlap in GDM
and hypertensive disorders reflects a common causal
pathway. Both GDM and hypertensive disorders are
associated with factors such as insulin resistance,
[8]
inflammation, and maternal fat deposition patterns . In
a randomized MiG trial, which only included GDM
women, about 5.0% of women had gestational
[9]
hypertension and 6.3% had pre-eclampsia. However,
[10]
the randomized ACHOIS trial reported that 15% of its
GDM population had pre-eclampsia, and in the present
study Pre eclampsia was associated with GDM in
11.11% of patients.
Ambarisha et al.,
In 1987, Cousins reviewed the literature published in
English from 1965 to 1985 on the impact of diabetes on
the frequency and severity of obstetric complications.
[11]
Hydramnios was found to be 5.3%
where as it was
9.52% in the present study
Preterm delivery is usually defined as delivery <37
weeks gestation. While acknowledged as a risk of GDM,
spontaneous preterm delivery is less common compared
[3]
with other adverse outcomes. . In the present study the
incidence of preterm delivery was 5.3%. In the HAPO
study, approximately 1608 of the 23,316 participants
(6.9%) experienced preterm delivery (both induced and
spontaneous), compared with 9.6% of infants who were
LGA and 8.0% of infants who underwent intensive
[12]
neonatal care admission.
The association between
GDM and preterm delivery may be partially explained by
the coexistence of other conditions with GDM that may
lead to indicated or induced preterm delivery. Such
conditions include pre-eclampsia and hypertensiveassociated conditions, such as intrauterine growth
restriction
and
placental
abruption.
However,
spontaneous preterm birth, or birth in the absence of
conditions prompting medical intervention, accounts for
approximately three-quarters of preterm births and is not
[12, 13]
associated with GDM.
. In the present study 3 cases
had antepartum haemorrhage and one patient had post
partum haemorrhage following a cesarean section where
the neonatal birth weight was 3.9 kgs. In this study 22
babies had NICU admission and 14 babies were
admitted for neonatal hypoglycemia. The reasons for
neonatal hypoglycemia include physiologic fluctuations in
glucose seen in GDM women, apart from treatment.
Maternal hyperglycemia is thought to lead to excess fetal
glucose exposure and fetal hyperinsulinemia. In turn,
fetal hyperinsulinemia is thought to lead to hyperplasia of
fat tissue, skeletal muscle, and subsequent neonatal
[14]
hypoglycemia.
In ACHOIS, the prevalence of clinical
hypoglycemia was 7% in GDM receiving intervention and
[10]
5% in GDM not receiving intervention,
which was
similar to 7.4% in the present study.
Hyperbilirubinemia is more common among women with
GDM than in women without GDM. Maternal
hyperglycemia and the subsequent induction of fetal
hyperinsulinemia and reduced oxygenation are
hypothesized to lead to increased fetal oxygen uptake,
fetal
erythropoiesis,
and
subsequent
[15]
[12]
hyperbilirubinemia.
In the HAPO study
8.3% of the
babies were affected with hyperbilirubinemia in
comparison with 3.7% in this study. In more recent years
and in industrialized nations, stillbirth is an uncommon
outcome, even among women with glucose intolerance.
Reduced stillbirth rates have been attributed to initiation
of insulin therapy combined with closer monitoring and
[16]
subsequent induction of labor as necessary. In a study
population consisting primarily of women with GDM, the
[17]
stillbirth rate was approximately 1.4 per 1000 births. .
3.17% fetal death an 1.05% neonatal death were
documented in this study. In HAPO, only 130 women
(0.56%) of the 23,316 deliveries experienced a perinatal
death, 89 of which were fetal and 41 of which were
[12]
neonatal.
776
Int J Med Res Health Sci. 2015;4(4):775-777
The effects of GDM upon fetal health may still be
conceptualized through the framework of the Pederson
[18]
hypothesis,
which postulated that intrauterine
exposure could lead to permanent changes in fetal
metabolism. During the GDM pregnancy, the fetus may
be imprinted or programmed, resulting in excess fetal
growth, decreased insulin sensitivity, and impaired
insulin secretion. In the short term, elevated infant birth
weight confers perinatal risks, such as shoulder dystocia
and infant hypoglycemia. In the longer term, altered fetal
metabolism may be associated with impaired glucose
[19]
tolerance during early youth and adolescence.
The
reduced beta-cell reserve in GDM women can manifest
[20]
in the decade after delivery. Even among women who
have a normal postpartum glucose tolerance test, the
risk of future diabetes may be up to seven-fold higher
[21]
than in women without histories of GDM.
As many as
one-third of women with diabetes may have been
[22]
affected by prior GDM.
In turn, the increased risk of
diabetes
is
associated
with
future
maternal
[23]
cardiovascular disease.
CONCLUSION
The prevalence of GDM will continue to increase as
obesity rates rises. There are sufficient evidences to
show the association between hyperglycemia and
adverse maternal and perinatal outcomes in the mother
and offspring. A close attention to the fetal growth along
with maternal glucose and weight monitoring during
pregnancy and also in the postpartum period will
minimize adverse outcomes. GDM is a condition which is
worth monitoring and treating, since it has been
demonstrated that good metabolic control maintained
throughout gestation can reduce maternal and fetal
complications.
Conflict of Interest: None
REFERENCES
1. Metzger BE, Coustan DR (Eds.): Proceedings of the
Fourth International Workshop- Conference on
Gestational Diabetes Mellitus. Diabetes Care
1998;21(suppl. 2):B1-B167.
2. Langer O. Management of gestational diabetes:
pharmacologic treatment options and glycemic
control. Endocrinol Metab Clin North Am.
2006;35(1):53-78.
3. Gestational diabetes: risks, management, and
treatment options, Int J Womens Health. 2010; 2:
339351
4. Metzger BE. Long-term outcomes in mothers
diagnosed with gestational diabetes mellitus and
their offspring. Clin Obstet Gynecol.2007;50:972-79.
5. ADA Clinical Practice Guidelines 2011. Diabetes
Care. 2011;34(suppl 1):S4-S5.
6. Seshaiah V, Sahay BK, Das AK, Shah S, Banerjee
S, Rao PV et al. Gestational diabetes mellitus-Indian guidelines. J Indian Med Assoc. 2009
Nov;107(11):799-802, 804-806.
7. Vedavathi KJ , Swamy Rm , Kanavi Roop
Shekharappa , Venkatesh G , Veerananna HB
Influence of Gestational Diabetes Mellitus on Fetal
Ambarisha et al.,
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
growth parameters. Int J Biol Med Res. 2011; 2(3):
832-834
Seely E, Solomon C. Insulin resistance and its
potential role in pregnancy-induced hypertension. J
Clin Endocrinol Metab. 2003;88(6):23932398.
Rowan J, Hague W, Gao W, Battin M, Moore M.
MiG Trial Investigators. Metformin versus insulin for
the treatment of gestational diabetes. N Engl J Med.
2008;358(19):20032015.
Crowther C, Hiller J, Moss J, et al. Effect of
treatment of gestational diabetes mellitus on
pregnancy
outcomes.
N
Engl
J
Med.
2005;352(24):24772486.
Cousins L: Pregnancy complications among diabetic
women: review 1965-1985. Obstet Gynecol Surv ,
1987;42:140-49
HAPO Study Cooperative Research Group.
Hyperglycemia and adverse pregnancy outcomes. N
Engl J Med. 2008;358(19):19912002.
ACOG Committee on Practice Bulletins Obstetrics.
ACOG practice bulletin. Management of preterm
labor. Int J Gynaecol Obstet. 2003;82(1):127135.
HAPO Study Cooperative Research Group.
Hormonal and metabolic factors associated with
variations in insulin sensitivity in human pregnancy.
Diabetes Care. 2010;33(2):356360.
Ferrara A, Weiss N, Hedderson M, et al. Pregnancy
plasma glucose levels exceeding the American
Diabetes Association thresholds, but below the
National Diabetes Data Group thresholds for
gestational diabetes mellitus, are related to the risk
of neonatal macrosomia, hypoglycaemia, and
hyperbilirubinaemia. Diabetologia. 2007;50(2):298
306.
ACOG Practice Bulletin. Clinical management
guidelines for obstetrician-gynecologists. Obstet
Gynecol. 2001;98(3):525538.
Girz B, Divon M, Merkatz I. Sudden fetal death in
women with well-controlled intensively monitored
gestational diabetes. J Perinatol. 1992;12(3):22933
Pedersen J. Weight and length at birth in infants of
diabetic mothers. Acta Endocrinol. 1954;16(4):330
42
Catalano P, Kirwan J, Haugel-de Mouzon S, King J.
Gestational diabetes and insulin resistance: Role in
short- and long-term implications for mother and
fetus. J Nutr. 2003;133(5 Suppl 2):S1674S1683.
Kim C, Newton K, Knopp R. Gestational diabetes
and incidence of Type 2 diabetes mellitus: A
systematic
review.
Diabetes
Care.
2002;25(10):186268.
Bellamy L, Casas J, Hingorani A, Williams D. Type
2 diabetes mellitus after gestational diabetes: A
systematic review and meta-analysis. Lancet.
2009;373(9677):177379.
Cheung N, Byth K. Population health significance of
gestational
diabetes.
Diabetes
Care.
2003;26(7):200509.
Carr D, Utzschneider K, Hull R. Gestational diabetes
mellitus increases the risk of cardiovascular disease
in women with a family history of Type 2 diabetes.
Diabetes Care. 2006;29(9):207883.
777
Int J Med Res Health Sci. 2015;4(4):775-777
Vous aimerez peut-être aussi
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Ultrasound Notes For Trainees: DR Phurb DorjiDocument16 pagesUltrasound Notes For Trainees: DR Phurb DorjiooiziungiePas encore d'évaluation
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Induction of Labor With Oxytocin - UpToDateDocument54 pagesInduction of Labor With Oxytocin - UpToDateJhoseline CamposPas encore d'évaluation
- Bridging Courses for Overseas Trained DoctorsDocument7 pagesBridging Courses for Overseas Trained Doctorsphyo waiPas encore d'évaluation
- Antepartum HemorrhageDocument21 pagesAntepartum HemorrhageNidhi SharmaPas encore d'évaluation
- Radiology of Obstetrics and GynaecologyDocument61 pagesRadiology of Obstetrics and GynaecologyMUBIRU SAMUEL EDWARDPas encore d'évaluation
- Skilled Birth Attendance HandbookDocument69 pagesSkilled Birth Attendance HandbookKripa Susan100% (2)
- Ijmrhs Vol 4 Issue 2Document219 pagesIjmrhs Vol 4 Issue 2editorijmrhsPas encore d'évaluation
- 47serban Turliuc EtalDocument4 pages47serban Turliuc EtaleditorijmrhsPas encore d'évaluation
- Ijmrhs Vol 4 Issue 4Document193 pagesIjmrhs Vol 4 Issue 4editorijmrhs0% (1)
- Ijmrhs Vol 4 Issue 3Document263 pagesIjmrhs Vol 4 Issue 3editorijmrhsPas encore d'évaluation
- Ijmrhs Vol 2 Issue 3Document399 pagesIjmrhs Vol 2 Issue 3editorijmrhs100% (1)
- Ijmrhs Vol 3 Issue 3Document271 pagesIjmrhs Vol 3 Issue 3editorijmrhsPas encore d'évaluation
- Ijmrhs Vol 1 Issue 1Document257 pagesIjmrhs Vol 1 Issue 1editorijmrhsPas encore d'évaluation
- Ijmrhs Vol 3 Issue 4Document294 pagesIjmrhs Vol 3 Issue 4editorijmrhsPas encore d'évaluation
- Ijmrhs Vol 2 Issue 2Document197 pagesIjmrhs Vol 2 Issue 2editorijmrhsPas encore d'évaluation
- Ijmrhs Vol 3 Issue 1Document228 pagesIjmrhs Vol 3 Issue 1editorijmrhsPas encore d'évaluation
- 45mohit EtalDocument4 pages45mohit EtaleditorijmrhsPas encore d'évaluation
- Ijmrhs Vol 3 Issue 2Document281 pagesIjmrhs Vol 3 Issue 2editorijmrhsPas encore d'évaluation
- Ijmrhs Vol 2 Issue 4Document321 pagesIjmrhs Vol 2 Issue 4editorijmrhsPas encore d'évaluation
- Ijmrhs Vol 2 Issue 1Document110 pagesIjmrhs Vol 2 Issue 1editorijmrhs100% (1)
- Ijmrhs Vol 1 Issue 1Document257 pagesIjmrhs Vol 1 Issue 1editorijmrhsPas encore d'évaluation
- 41anurag EtalDocument2 pages41anurag EtaleditorijmrhsPas encore d'évaluation
- 48 MakrandDocument2 pages48 MakrandeditorijmrhsPas encore d'évaluation
- Pernicious Anemia in Young: A Case Report With Review of LiteratureDocument5 pagesPernicious Anemia in Young: A Case Report With Review of LiteratureeditorijmrhsPas encore d'évaluation
- 40vedant EtalDocument4 pages40vedant EtaleditorijmrhsPas encore d'évaluation
- 43chaitali EtalDocument3 pages43chaitali EtaleditorijmrhsPas encore d'évaluation
- Recurrent Cornual Ectopic Pregnancy - A Case Report: Article InfoDocument2 pagesRecurrent Cornual Ectopic Pregnancy - A Case Report: Article InfoeditorijmrhsPas encore d'évaluation
- Williams-Campbell Syndrome-A Rare Entity of Congenital Bronchiectasis: A Case Report in AdultDocument3 pagesWilliams-Campbell Syndrome-A Rare Entity of Congenital Bronchiectasis: A Case Report in AdulteditorijmrhsPas encore d'évaluation
- 38vaishnavi EtalDocument3 pages38vaishnavi EtaleditorijmrhsPas encore d'évaluation
- 36rashmipal EtalDocument6 pages36rashmipal EtaleditorijmrhsPas encore d'évaluation
- 37poflee EtalDocument3 pages37poflee EtaleditorijmrhsPas encore d'évaluation
- 35krishnasamy EtalDocument1 page35krishnasamy EtaleditorijmrhsPas encore d'évaluation
- 33 Prabu RamDocument5 pages33 Prabu RameditorijmrhsPas encore d'évaluation
- 34tupe EtalDocument5 pages34tupe EtaleditorijmrhsPas encore d'évaluation
- 32bheemprasad EtalDocument3 pages32bheemprasad EtaleditorijmrhsPas encore d'évaluation
- Biochemical Investigation in PregDocument28 pagesBiochemical Investigation in PregRana VandanaPas encore d'évaluation
- Guideline for Managing Eclampsia and Severe Pre-EclampsiaDocument15 pagesGuideline for Managing Eclampsia and Severe Pre-EclampsiaMegane YuliPas encore d'évaluation
- Tugas 2 HukKes KKIDocument12 pagesTugas 2 HukKes KKINikolasKosasihPas encore d'évaluation
- Prenatal screening testDocument2 pagesPrenatal screening testEva.linePas encore d'évaluation
- IVF TRAINING For EMBRYOLOGIST & GYNAECOLOGISTDocument3 pagesIVF TRAINING For EMBRYOLOGIST & GYNAECOLOGIST24x7emarketingPas encore d'évaluation
- Second and Third Trimester Screening For Fetal AnomalyDocument12 pagesSecond and Third Trimester Screening For Fetal AnomalyIqra NazPas encore d'évaluation
- Cervical IncompetenceDocument30 pagesCervical IncompetenceSignor ArasPas encore d'évaluation
- CLINICAL GUIDELINE FOR POSTPARTUM BLADDERDocument9 pagesCLINICAL GUIDELINE FOR POSTPARTUM BLADDERHanya BelajarPas encore d'évaluation
- English Assignment ConversationDocument4 pagesEnglish Assignment ConversationSri HalipahPas encore d'évaluation
- Rupture of UterusDocument5 pagesRupture of UterussamarbondPas encore d'évaluation
- Gynea & Obs 26-30Document6 pagesGynea & Obs 26-30Wafiyah AwaisPas encore d'évaluation
- Neonatal ResuscitationDocument36 pagesNeonatal ResuscitationDemelash SolomonPas encore d'évaluation
- Antepartum Hemorrhage Causes Fetal DistressDocument4 pagesAntepartum Hemorrhage Causes Fetal Distressvenus eugenioPas encore d'évaluation
- Mannual Removal of Placenta: Presented By-Bhawna Joshi MSC. (N) 2 YearDocument23 pagesMannual Removal of Placenta: Presented By-Bhawna Joshi MSC. (N) 2 YearBhawna JoshiPas encore d'évaluation
- Acute Uterine InversionDocument6 pagesAcute Uterine InversionBima GhovaroliyPas encore d'évaluation
- Biophysical ProfileDocument1 pageBiophysical ProfileCruz YrPas encore d'évaluation
- College of Health Sciences Yarsi Mataram DIII Midwifery Studies Program Final Project Report, July 2nd, 2019 Yana Fiqratus Shofa (037 SYEIB 16)Document3 pagesCollege of Health Sciences Yarsi Mataram DIII Midwifery Studies Program Final Project Report, July 2nd, 2019 Yana Fiqratus Shofa (037 SYEIB 16)Yana ShofaPas encore d'évaluation
- Example of Delivery NoteDocument1 pageExample of Delivery NoteRuDy RaviPas encore d'évaluation
- AC8A9EE0-EggFreezingProcesseditDocument9 pagesAC8A9EE0-EggFreezingProcesseditFrida AtallahPas encore d'évaluation
- CR3 RobbbDocument86 pagesCR3 RobbbIhsan Rasyid YuldiPas encore d'évaluation
- 1 Complications of L&D PowerDocument84 pages1 Complications of L&D PowerMarlon Glorioso II100% (1)
- MCN 209 Obgyne Rotation: Postpartum HemorrhageDocument10 pagesMCN 209 Obgyne Rotation: Postpartum HemorrhageMonique LeonardoPas encore d'évaluation
- Preliminary Offer Document (12 May 2015) PDFDocument329 pagesPreliminary Offer Document (12 May 2015) PDFInvest StockPas encore d'évaluation
- Vbac (Vaginal Birth After C-Section) : RA. Nurafrilya Fitria SariDocument13 pagesVbac (Vaginal Birth After C-Section) : RA. Nurafrilya Fitria Sariafirdha27Pas encore d'évaluation