Académique Documents
Professionnel Documents
Culture Documents
9 Hjah
Transféré par
Alex MitchellTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
9 Hjah
Transféré par
Alex MitchellDroits d'auteur :
Formats disponibles
A C TA Obstetricia et Gynecologica
AOGS M A I N R E SE A RC H A R TI C LE
Management of prolonged pregnancy by induction with a
Foley catheter
HEIDI KRUIT1, OSKARI HEIKINHEIMO1, VELI-MATTI ULANDER1, ANSA AITOKALLIO-TALLBERG1,
IRMELI NUPPONEN2, JORMA PAAVONEN1 & LEENA RAHKONEN1
1
2
Department of Obstetrics and Gynecology, University of Helsinki and Helsinki University Hospital, Helsinki, and
Childrens Hospital, University of Helsinki and Helsinki University Hospital, Helsinki, Finland
Key words
Labor induction, Foley catheter, prolonged
pregnancy, cesarean delivery rate, nulliparous
women
Correspondence
Heidi Kruit, Department of Obstetrics and
Gynecology, Helsinki University Hospital,
Haartmaninkatu 2, 00029 HUS Helsinki,
Finland.
E-mail: heidi.kruit@hus.fi
Conflict of interest
The authors have stated explicitly that there
are no conflicts of interest in connection with
this article.
Please cite this article as: Kruit H,
Heikinheimo O, Ulander V-M, AitokallioTallberg A, Nupponen I, Paavonen J, et al.
Management of prolonged pregnancy by
induction with a Foley catheter. Acta Obstet
Gynecol Scand 2015; 94: 608614.
Received: 30 December 2014
Accepted: 4 March 2015
Objectives. To describe labor outcomes in women with prolonged pregnancy
and induction of labor with a Foley catheter, as compared with women with
spontaneous onset of labor. Design. Retrospective study. Setting. Helsinki University Hospital. Sample. 553 women with uncomplicated prolonged pregnancies between January 2011 and January 2012, divided into 303 women (54.8%)
with Foley catheter induction and 250 (45.2%) with spontaneous labor. Methods. Maternal and neonatal characteristics of women with uncomplicated singleton pregnancy of 41+5 weeks of gestation were analyzed. Main outcome
measures. Cesarean delivery rates, maternal and neonatal morbidity.
Results. The cesarean delivery rate was 30.7% (n = 93/303) in women with
labor induction and 4.8% (12/250) in women with spontaneous onset of labor
(p < 0.001). The cesarean delivery rate was 37.3% (91/244) among nulliparous
women with labor induction and 8.7% (11/126) among women with spontaneous labor, a sixfold increased risk (odds ratio 6.2). Among parous women,
cesarean section rates were low and not significantly different (3.4% vs. 0.8%,
p = 0.2). There were no differences in maternal intrapartum or postpartum
infection rates or adverse neonatal outcomes between the groups. Conclusions. Foley catheter induction of labor in prolonged pregnancy did not
increase maternal or perinatal morbidity compared with spontaneous onset of
labor but was associated with a considerably increased cesarean section rate,
particularly among nulliparous women.
Abbreviations:
GBS, Group B Streptococcus agalactiae; IOL, induction of labor.
DOI: 10.1111/aogs.12632
Introduction
The World Health Organization defines post-term pregnancy as one extending to 42+0 weeks (294 days) (1).
Post-term pregnancy occurs in approximately 5% of pregnancies, varying in reported frequency from 0.4 to 8.1%
in different countries (2). In Finland, 810% of all pregnancies extend beyond 41 weeks of gestation and the rate
of post-term pregnancy has ranged between 4.2 and 4.8%
during recent years (3,4). Post-term pregnancy is associated with maternal and fetal risks, raised rates of operative delivery, and increased perinatal mortality (5,6).
608
Key Message
Labor induction with Foley catheter in prolonged
pregnancy appears as safe as spontaneous labor in
terms of perinatal morbidity but is associated with a
high rate of cesarean delivery, particularly among nulliparous women. Given the major impact of the first
cesarean delivery on subsequent pregnancies, it is
important to optimize labor induction methods, not
least for nulliparous women.
2015 Nordic Federation of Societies of Obstetrics and Gynecology, Acta Obstetricia et Gynecologica Scandinavica 94 (2015) 608614
H. Kruit et al.
Labor induction in prolonged pregnancy
Post-term pregnancy is the most common indication for
labor induction (7). Nowadays, induction of labor (IOL)
is started before 42 weeks in many countries since several
clinical practice guidelines on the management of postterm pregnancy recommend elective induction and delivery by 41 completed weeks (1,8,9). While induction rates
have increased, the rates of post-term pregnancy have
decreased (8).
There is a concern that rising rates of IOL may increase
cesarean deliveries (10,11). However, it has been debated
whether the increased cesarean section rates are related to
the IOL or to the indication(s) for induction. In a
recently published Norwegian study, only insignificant
increases in the cesarean section rate were seen after a
change to a more liberal induction policy for prolonged
pregnancies (12). Furthermore, in a recent meta-analysis
the cesarean section rate in term and post-term pregnancies was lower among women with induced labor than in
women managed expectantly (13).
The Foley catheter method has been established for
IOL since it was first described in the early 1980s. Then,
it was used in conjunction with prostaglandin administration via the catheter (14). After 1990, additional studies
on the use of the Foley catheter for labor induction were
published. Recently, the Foley catheter has been shown to
result in a comparable vaginal delivery rate to that seen
following induction with prostaglandins in low-risk
women with an unfavorable cervical score at term
(15,16).
The aim of this study was to evaluate delivery outcomes
in prolonged pregnancies induced by Foley catheter.
Material and methods
This retrospective study of women with a prolonged
pregnancy of 41+5 gestational weeks between January
2011 and January 2012 (1 year) was conducted at the
Department of Obstetrics and Gynecology, Helsinki University Hospital, Finland. According to the departmental
management guidelines, all women with an uncomplicated prolonged pregnancy receive an appointment for an
antenatal visit in the maternity outpatient clinic at 41+5
weeks of gestation. The decision on IOL or expectant
management depends on an assessment of maternal and
fetal wellbeing and on maternal preference. Fetal wellbeing was examined by cardiotocography (non-stress test)
and ultrasonographic assessment of fetal growth, fetal
movements, and amniotic fluid volume (biophysical profile). Where expectant management was chosen, IOL was
scheduled no later than 42+1 weeks (4 days later) if spontaneous labor had not commenced. Since 2010, the Foley
catheter has been the main method of labor induction in
our department (17).
A total of 798 women with an uncomplicated singleton
pregnancy 41+5 weeks of gestation were identified from
the hospital database during the study year. Duration of
pregnancy was defined by the fetal crownrump length
measurement performed at the time of first trimester
ultrasound screening. We excluded 212 women with
breech presentation, a history of cesarean section or previous rupture of membranes in the current pregnancy
(Figure 1). Since we wanted to focus on Foley catheter
induction, a relatively new IOL method in our clinic at
the time, we also excluded women in whom other induction methods were used. The final database thus contained 553 deliveries, including 303 women (54.8%) with
Foley catheter IOL and 250 women (45.2%) with spontaneous labor by 42+1 weeks of gestation. In all cases the
main indication for IOL was prolonged pregnancy. The
study protocol was approved by the local Ethics Committee (No. 268/13/03/03/2012) and the management of the
Hospital district of Helsinki and Uusimaa.
In Foley catheter induction a single balloon catheter
(R
usch 2-way Foley Couvelaire tip catheter size 22 Ch,
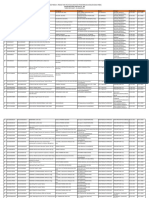
Study population
n = 798
Primary exclusion (n = 212):
Previous cesarean section n = 79
Breech presentation
n=2
Amniotomy
n = 70
Prostaglandin
n = 61
Spontaneous labor
n = 250
Primiparous
n = 126
Multiparous
n = 124
Labor induction
n = 336
Primiparous
n = 244
Secondary exclusion:
Foley catheter +
prostaglandin
n = 33
Multiparous
n = 59
Figure 1. Flow chart of the study population.
2015 Nordic Federation of Societies of Obstetrics and Gynecology, Acta Obstetricia et Gynecologica Scandinavica 94 (2015) 608614
609
Labor induction in prolonged pregnancy
Teleflex Medical, Athlone, Ireland) was used. In 139
(45.9%) cases the catheter was inserted at gestational age
41+5, in 65 women (21.5%) at 41+6, in 83 (27.4%) at
42+0 and in 16 (5.2%) at 42+1 weeks. Before inserting the
catheter, a Bishop score was determined (18). At commencement of IOL all the women had unfavorable cervical scores (Bishop score 6). The catheter was introduced
into the endocervix and towards the space between the
amniotic membrane and the lower uterine segment. The
balloon reservoir was inflated with 4050 mL of saline
and retracted so that it rested on the internal os. Light
traction was applied and the catheter was taped on to the
inner aspect of the thigh. Fetal monitoring for a minimum of 20 min was continued. After spontaneous expulsion of the balloon, amniotomy was performed if the
Bishop score was 6. If spontaneous expulsion of the Foley catheter did not occur within 24 h, the balloon was
removed. If the cervix remained unripe with a Bishop
score <6 after balloon expulsion or removal, induction
was continued with intravaginal misoprostol. These
(n = 33) the woman was excluded from the final analysis
(Figure 1). Amniotomy was performed immediately after
expulsion or at the latest, after overnight rest on the next
morning depending on delivery unit capacity. Oxytocin
augmentation was started in the absence of spontaneous
contractions. The timing of oxytocin augmentation was at
the discretion of the obstetrician and varied between 2
and 24 h. The beginning of regular contractions was
defined from the start of contractions occurring at least
every 35 min after cervical dilation of 34 cm.
Data on delivery and neonatal outcomes were collected
from the hospital records. The outcomes included the
mode of delivery, oxytocin administration, postpartum
hemorrhage, maternal and neonatal infections, umbilical
artery blood gas values, Apgar scores, and admissions to
neonatal unit or neonatal intensive care unit (NICU).
When there was more than one indication for cesarean
delivery, the primary indication was categorized using the
following hierarchy: fetal distress, infection, failure to
progress and failed induction. Data on the study population characteristics and maternal antenatal risk factors,
such as maternal age, body mass index in early pregnancy, use of in vitro fertilization, parity, Bishop score,
smoking and gestational diabetes were collected from the
antenatal clinic charts. Obesity was defined as body mass
index 30 kg/m. Gestational diabetes was diagnosed by
an oral glucose tolerance test. All women with gestational
diabetes had normoglycemia and normal fetal growth
while on dietary care.
Streptococcus agalactiae of group B (GBS) was tested
for by culture from a vaginal and perianal specimen collected at a prenatal visit 4 weeks prior to delivery, or on
admission, using a risk-based strategy for GBS screening.
610
H. Kruit et al.
Maternal infections were categorized as intrapartum or
postpartum (from delivery to discharge). The criteria for
intrapartum infection were maternal fever (38C), fetal
tachycardia (160 bpm), uterine tenderness, purulent
amniotic fluid or vaginal discharge, and a total white cell
count >20 9 109/L. At least two of these criteria had to
be met, combined with administration of antibiotics.
Postpartum infection diagnoses included endometritis (by
the above criteria), wound infection, mastitis, urinary
tract infection and puerperal fever of unknown origin.
Neonatal infections were categorized into blood culture
positive sepsis, clinical sepsis, and suspected sepsis. Neonatal clinical sepsis was defined as a blood culture negative infection with symptoms and signs consistent with
sepsis (such as respiratory distress, apnea, tachycardia,
poor capillary perfusion, low blood pressure, fever, hypoor hyperglycemia, irritability, feeding problems, lethargy
and convulsions), abnormal blood values (such as elevated levels of the C-reactive protein, leukocytosis or leukopenia,
increased
neutrophil
precursors
and
thrombocytopenia) and positive response to a minimum
of 5 days of antibiotic treatment. The cases defined as
suspected sepsis had to have at least one symptom and
one abnormal laboratory test value, and a positive
response to antibiotic treatment.
All calculations were carried out using the Microsoft
Statistical Package for Social Sciences for Windows v18.0
(SPSS Inc., Chicago, IL, USA). Categorical variables were
compared by the chi-squared and Fishers exact tests when
appropriate. Data with continuous variables were analyzed
by the t-test when the data followed normal distribution
and by a MannWhitney U-test if this was not the case.
We used univariate logistic regression to estimate relative
risks represented by odds ratios with 95% confidence
intervals. A p-value < 0.05 was considered significant.
Results
The characteristics of the study population are shown in
Table 1. The women with induced labor were more often
nulliparous (p < 0.001) and more often had an extended
gestational age of 42 weeks at the start of IOL
(p < 0.001) compared with women with spontaneous
labor onset at or after 41+5 weeks. The medians of gestational weeks at the start of IOL and spontaneous labor
were, however, similar in both groups: 41.9 (range 41.7
42.3) and 41.9 (range 41.742.6).
Maternal outcomes are shown in Table 2. The nulliparous, but not parous, women with IOL more often
received prophylactic antibiotics and epidural or spinal
analgesia than women with spontaneous labor onset did
(p < 0.001, p = 0.03, respectively). Oxytocin augmentation was more common in IOL cases than among women
2015 Nordic Federation of Societies of Obstetrics and Gynecology, Acta Obstetricia et Gynecologica Scandinavica 94 (2015) 608614
H. Kruit et al.
Labor induction in prolonged pregnancy
Table 1. Characteristics of the study population.
Maternal age 35 years
Nulliparous
IVF
Smoking
BMI (kg/m)a 30 kg/m
Gestational diabetes
Gestational age 42 weeks
Foley catheter induction
(n = 303)
Spontaneous labor
(n = 250)
p-value
65
244
7
42
34
27
197
21.5
80.5
2.3
13.9
11.2
8.9
65.0
70
126
2
35
22
22
65
28.0
50.4
0.8
14.0
8.8
8.8
26.0
0.07
<0.001
0.19
0.96
0.28
0.96
<0.001
Chi-squared test or Fishers exact probability test.
BMI, body mass index; IVF, in vitro fertilization.
a
One missing value (spontaneous labor).
Table 2. Maternal outcomes.
Primiparous
Prophylactic antibiotic
Oxytocin augmentation
Epidural/spinal analgesia
Bishop score 3 at 41+5 gestational weeksa
Bishop score 3 at start of labor inductionb
Mode of delivery
Vaginal
Vacuum extraction
Cesarean section
Indication for cesarean section
Fetal distress
Infection
Labor arrest
Failed induction
Post partum haemorrhage 1000 ml
Vaginal delivery
Cesarean delivery
Fever 38C during labor
Suspected intrapartum infection
Postpartum infection
Endometritis
Wound infection
Fever of unknown origin
Multiparous
Foley
catheter
induction
(n = 244)
Spontaneous
labor
(n = 126)
146
233
216
119
112
59.8
95.5
88.5
50.4
47.3
33
112
120
20
26.2
88.9
95.2
23.5
153
45
91
62.7
18.4
37.3
115
30
11
91.3
23.8
8.7
38
7
27
19
41.8
7.7
29.7
20.9
6
0
5
0
54.5
21
33
12
15
9
6
2
1
13.7
36.3
4.9
6.1
3.7
2.4
0.8
0.4
13
3
2
3
2
0
2
0
Foley
catheter
induction
(n = 59)
Spontaneous
labor
(n = 124)
p-value
<0.001
0.02
0.03
<0.001
9
51
48
29
24
15.3
86.4
81.4
50.9
41.4
8
60
90
18
6.5
48.4
72.6
20.5
57
4
2
96.6
6.8
3.4
123
3
1
99.2
2.4
0.8
p-value
<0.001
0.55
0.20
45.5
0.42
0.34
0.29
0
0
2
0
11.3
27.3
1.6
2.4
1.6
0.56
0.93
0.11
0.13
0.26
4
1
1
1
1
0
1
0
1.6
0.06
<0.001
0.2
<0.001
100
7.0
50
1.7
1.7
1.7
1.7
0
1
0
0
10
0
2
1
0
0
0
0
0.21
100
8.1
0.80
1.6
0.8
Chi-squared test or Fishers exact probability test.
Missing values 10 (induction) and 77 (spontaneous labor).
b
Seven missing values.
a
with spontaneous labor, among both nulliparous and parous women (p < 0.001 and p < 0.02, respectively).
The overall cesarean delivery rate was 30.7% (n = 93)
in women with IOL and 4.8% (n = 12) among women
with spontaneous labor (p < 0.001). Differences in the
cesarean delivery rates were observed in nulliparous
women (37.3 vs. 8.7%, p < 0.001) but not among the
parous women (3.4 vs. 0.8%, p = 0.2). The odds ratio for
cesarean delivery among nulliparous women was 6.2
[95% confidence interval (CI) 3.212.1]. The indications
2015 Nordic Federation of Societies of Obstetrics and Gynecology, Acta Obstetricia et Gynecologica Scandinavica 94 (2015) 608614
611
Labor induction in prolonged pregnancy
H. Kruit et al.
Table 3. Neonatal outcomes.
Primiparous
Male
Birthweight, g [mean (SD)]
Macrosomia (>4500 g)
Apgar 1 min <7
Apgar 5 min <7
Umbilical artery pH <7.05a
Umbilical artery BE 12.0a
Neonatal infection
Suspected sepsis
Clinical sepsis
Infection of unknown origin
Admission to NICU
Admission to neonatal ward
Multiparous
Foley catheter
induction
(n = 244)
Spontaneous
labor (n = 126)
135
3701
8
22
8
5
7
19
13
5
1
30
7
55.3
(428)
3.3
9.0
3.3
2.1
3.0
7.8
68.4
26.3
5.2
12.3
2.9
69
3765
4
9
1
5
6
3
2
1
0
12
2
54.8
(352)
3.2
7.1
0.8
4.0
4.8
2.4
66.7
33.3
0.92
0.45
0.96
0.50
0.23
0.32
0.40
0.04
9.5
1.6
0.45
0.43
p-value
Foley catheter
induction
(n = 244)
Spontaneous
labor (n = 126)
23
3765
3
3
0
3
1
2
2
0
0
0
2
39.0
(352)
5.1
5.1
64
3871
9
5
1
1
1
2
1
1
0
1
5
51.6
(431)
7.3
4.0
0.8
0.8
0.8
1.6
50
50
0.11
0.12
0.58
0.75
0.53
0.09
0.52
0.60
0.8
4.0
0.49
0.83
5.5
1.8
3.4
100
3.4
p-value
Chi-squared test, Fishers exact probability test or t-test.
BE, base excess; NICU, neonatal intensive care unit.
a
Eleven missing values (primiparous).
for cesarean delivery did not differ between the groups of
nulliparous women. No difference was found in the rates
of postpartum hemorrhage between the groups of nulliparous or parous women (Table 2).
The Bishop score was 3 in 50.4% (n = 119) in the
nulliparous women and in 23.5% (n = 20) in women
with spontaneous labor (p < 0.001). The corresponding
figures among parous women were 50.9% (n = 29) and
20.5% (n = 18) (p < 0.001).
Of the nulliparous women who had a Bishop score 3
at IOL, 43.8% (49/112) had a cesarean delivery compared
with 31.2% of those with a Bishop score 4 (39/125)
(p = 0.04). Of parous women with a Bishop score 3,
only two of 24 had cesarean delivery, whereas all parous
women with a higher score delivered vaginally. The rate
of cesarean delivery following IOL of labor did not differ
between obese and women with normal weight (38.2 vs.
29.7%, p = 0.31). There were no differences in the overall
intrapartum or postpartum infection rates between
women with IOL and women with spontaneous labor
onset. However, postpartum endometritis occurred only
following IOL (Table 2). No cases of blood culture-positive maternal sepsis were found. Of the nulliparous
women with intrapartum infection, 66.7% (10/15) of the
induced and 33.3% (1/3) of the spontaneous labor group
had had a cesarean delivery.
No differences were found in the adverse neonatal outcomes (low Apgar score, low umbilical artery pH or low
base excess value), NICU or neonatal unit admissions
612
between the induced and spontaneous labor groups
(Table 3). There were more neonatal infections diagnosed
after IOL than after spontaneous labor. After excluding
cases of suspected neonatal sepsis and comparing only
clinical neonatal sepsis cases, there was no difference
between the two groups (p = 0.43). No blood culturepositive cases were found. Of neonatal infections among
nulliparous women, 6/19 followed vaginal delivery and 13
(68.4%) cesarean delivery. All parous women whose neonate was diagnosed with infection (n = 4) had delivered
vaginally. Overall, GBS was tested on only 11.2%
(n = 62) of the women.
Of the 33 women (9.8%) with a Bishop score <6 after
Foley catheter and continued induction with misoprostol,
29 (87.9%) were nulliparous and had a cesarean section
rate of 51.7% (15/29) if nulliparous, whereas 25% of parous women required section.
Discussion
Our results indicate that IOL for prolonged pregnancy is
as safe when a Foley catheter is used as when awaiting
onset of spontaneous labor during a 4-day period extending just past 42 weeks. However, this is associated with a
high cesarean delivery rate among nulliparas. IOL did not
seem to increase maternal or neonatal infections and neonatal outcomes were similar following induced and spontaneous labor. Nonetheless, there are major limitations
with regard to conclusions in a retrospective study affected
2015 Nordic Federation of Societies of Obstetrics and Gynecology, Acta Obstetricia et Gynecologica Scandinavica 94 (2015) 608614
H. Kruit et al.
by a selection bias whereby more women with post-term
pregnancy ended up in the induction group and where
there was skewness towards a higher proportion of nulliparous women in group induced by Foley catheter. Large
randomized controlled trials on post-term pregnancy
management have been published (19) but we focused on
a narrow time frame (gestational length 41+5 to
42+1 weeks). The value of this study lies in the use of that
approach, which offsets to some extent our lack of power.
Alexander et al. (20) have demonstrated a 40% increase
in the cesarean delivery rate (from 14 to 19%) following
IOL compared with spontaneous labor at 41 weeks.
Overall, for induction at term, cesarean delivery rates
seem to increase three- to eightfold regardless of whether
induction is mechanical or pharmacological (21,22). In
our study the rate was sixfold higher among nulliparous
women. This is of concern given the overall 14% cesarean
rate among women aiming for vaginal delivery in our
hospital during 2012. However, some recent studies have
shown that the risk of cesarean delivery in prolonged and
post-term gestations may be lower among women with
induced labor compared with those managed expectantly
(8,12,13). The reasons for the different results are not
known but could depend on the induction method used
and the definition of prolonged pregnancy.
Nulliparity and obesity increase the risk for prolongation
of pregnancy, but they are also independent risk factors for
cesarean delivery after induced labor (20,2325). Low
Bishop scores are associated with high rates of induction
failure and operative delivery (11,26,27), also seen in our
study. The cesarean delivery rate was even higher, almost
50%, among the women in whom there was sequential use
of the Foley catheter and intravaginal misoprostol.
Cervical ripening was assessed using the Bishop score,
which was originally derived from parous women (18).
We used a score of 6 as a cut-off for the use of amniotomy and oxytocin augmentation. A more modern concept would be a Bishop score 8 (28). The exact
mechanism of cervical ripening is not completely understood. Studies have proposed that it relates to a reduction
in collagen density coupled to remodeling of the collagen
fibers (29). A recent study suggests that cell-free fetal
DNA initiates an inflammation process and with that cervical ripening, leading to onset of labor (30). What happens with the use of a Foley catheter is not known.
The most common cesarean delivery indication following IOL was failure to progress (failed induction and
labor arrest), as also noted previously (15,27,31).
In previous studies, as shown in a recent Cochrane
review, IOL by means of Foley catheter has not been
associated with increased rates of maternal infection
(15,16,32), as also found in this study, but contrasting
results have also been described (33). Likewise, clinical
Labor induction in prolonged pregnancy
neonatal infectious morbidity was not more common following induced labor, as shown previously (15). IOL itself
has, however, been linked to increased admissions to neonatal unit (34).
Our key finding was the high rate of cesarean delivery
among nulliparous women undergoing IOL by Foley
catheter between 41+5 and 42+1 weeks of gestation. Given
the major impact that the first cesarean delivery has on
subsequent pregnancies, there is a need to optimize labor
induction among nulliparous women.
Funding
This study was supported by a grant from the Finnish
Medical Society Duodecim and Helsinki University Central Hospital Research Funds.
References
1. ACOG Committee on Practice Bulletins-Obstetrics. ACOG
Practice Bulletin. Clinical management guidelines for
obstetricians-gynecologists. Number 55, September 2004
(replaces practice pattern number 6, October 1997).
Management of Postterm Pregnancy. Obstet Gynecol.
2004;104:63946.
2. Zeitlin J, Mohangoo AD, Delnord M, Cuttini M; EUROPERISTAT Scientific Committee. The second European
Perinatal Health Report: documenting changes over
6 years in the health of mothers and babies in Europe.
J Epidemiol Community Health. 2013;67:9835.
3. Vuori E, Gissler M. Perinatal statistics: parturients,
deliveries and newborns 2011. Helsinki: National Institute
of Finland for Health and Welfare, 2012.
4. Vuori E, Gissler M. Perinatal statistics: parturients,
deliveries and newborns 2013. Helsinki: National Institute
of Finland for Health and Welfare, 2014.
5. Olesen AW, Westergaard JG, Olsen J. Perinatal and
maternal complications related to postterm delivery: a
national register-based study, 19781993. Am J Obstet
Gynecol. 2003;189:2227.
6. Caughey AB, Stotland NE, Washington AE, Escobar GJ.
Maternal and obstetric complications of pregnancy are
associated with increasing gestational age at term. Am J
Obstet Gynecol. 2007;196:155.e16.
7. Briscoe D, Nguyen H, Mencer M, Gautam N, Kalb DB.
Management of pregnancy beyond 40 weeks gestation.
Am Fam Physician. 2005;71:193541.
8. Hedegaard M, Lidegaard O, Skovlund CW, Morch LS,
Hedegaard M. Reduction in stillbirths at term after new
birth induction paradigm: results of a national
intervention. BMJ Open. 2014;4:e005785.
9. NICE Guideline. Induction of labor. 2008. Available online
at: http://guidance.nice.org.uk/CG70 (accessed March 20,
2014).
2015 Nordic Federation of Societies of Obstetrics and Gynecology, Acta Obstetricia et Gynecologica Scandinavica 94 (2015) 608614
613
Labor induction in prolonged pregnancy
10. Rattigan MI, Atkinson AL, Baum JD. Delivery route
following elective induction of labor at term: analysis of
807 patients. J Clin Med Res. 2013;5:3058.
11. Beta J, Issat T, Nowicka MA, Jakimiuk AJ. Risk factors for
cesarean section after using the Foley catheter for labor
induction. Ginekol Pol. 2013;84:35962.
12. Klefstad OA, Okland I, Lindtjorn E, Rygh AB, Kaada K,
Hansen ML, et al. A more liberal approach towards
induction of labour in prolonged pregnancy does not result
in an adverse labour outcome. Dan Med J. 2014;61:A4913.
13. Mishanina E, Rogozinska E, Thatthi T, Uddin-Khan R,
Khan KS, Meads C. Use of labour induction and risk of
cesarean delivery: a systematic review and meta-analysis.
CMAJ. 2014;186:66573.
14. Saunders JR. Foley-catheter induction of labour. Br Med J.
1972;4:237.
15. Jozwiak M, Oude Rengerink K, Benthem M, van Beek E,
Dijksterhuis MG, de Graaf IM, et al. Foley catheter versus
vaginal prostaglandin E2 gel for induction of labour at
term (PROBAAT trial): an open-label, randomised
controlled trial. Lancet. 2011;378:2095103.
16. Jozwiak M, Dodd JM. Methods of term labour induction
for women with a previous caesarean section. Cochrane
Database Syst Rev. 2013;3:CD009792.
17. Panelius E, Heikinheimo O, Rahkonen L. Foley catheter
versus intravaginal misoprostol for labour induction.
Duodecim. 2012;128:2093102.
18. Bishop EH. Pelvic scoring for elective induction. Obstet
Gynecol. 1964;24:2668.
19. Heimstad R, Skogvoll E, Mattsson LA, Johansen OJ,
Eik-Nes SH, Salvesen KA. Induction of labor or serial
antenatal fetal monitoring in postterm pregnancy: a
randomized controlled trial. Obstet Gynecol.
2007;109:60917.
20. Alexander JM, MCIntire DD, Leveno KJ. Prolonged
pregnancy: induction of labor and cesarean births. Obstet
Gynecol. 2001;97:9115.
21. Maslow AS, Sweeny AL. Elective induction of labor as a
risk factor for cesarean delivery among low-risk women at
term. Obstet Gynecol. 2000;95(6 Pt 1):91722.
22. Prysak M, Castronova FC. Elective induction versus
spontaneous labor: a casecontrol analysis of safety and
efficacy. Obstet Gynecol. 1998;92:4752.
614
H. Kruit et al.
23. Caughey AB, Sundaram V, Kaimal AJ, Gienger A, Cheng
YW, McDonald KM, et al. Systematic review: elective
induction of labor versus expectant management of
pregnancy. Ann Intern Med. 2009;151:25263,
W5363.
24. Roos N, Sahlin L, Ekman-Ordeberg G, Kieler H,
Stephansson O. Maternal risk factors for postterm
pregnancy and cesarean delivery following labor induction.
Acta Obstet Gynecol Scand. 2010;89:100310.
25. ODwyer V, OKelly S, Monaghan B, Rowan A, Farah N,
Turner MJ. Maternal obesity and induction of labor. Acta
Obstet Gynecol Scand. 2013;92:14148.
26. Blackwell SC, Refuerzo J, Chadha R, Samson J. Duration
of labor induction in nulliparous women at term: how
long is long enough? Am J Perinatol. 2008;25:2059.
27. Vrouenraets FP, Roumen FJ, Dehing CJ, van den Akker
ES, Aarts MJ, Scheve EJ. Bishop score and risk of cesarean
delivery after induction of labor in nulliparous women.
Obstet Gynecol. 2005;105:6907.
28. ACOG Committee on Practice Bulletins Obstetrics.
ACOG Practice Bulletin No. 107: Induction of labor.
Obstet Gynecol. 2009;114(2 Pt 1):38697.
29. Norstrom A. Influence of prostaglandin D2 on the
biosynthesis of connective tissue constituents in the
pregnant human cervix. Prostaglandins. 1982;23:3617.
30. Phillippe M. Cell-free fetal DNA a trigger for
parturition. N Engl J Med. 2014;370:25346.
31. Jozwiak M, Bloemenkamp KW, Kelly AJ, Mol BW,
Irion O, Boulvain M. Mechanical methods for induction
of labour. Cochrane Database Syst Rev. 2012;3:
CD001233.
32. Prager M, Eneroth-Grimfors E, Edlund M, Marions L. A
randomised controlled trial of intravaginal dinoprostone,
intravaginal misoprostol and transcervical balloon catheter
for labour induction. BJOG. 2008;115:144350.
33. Heinemann J, Gillen G, Sanchez-Ramos L, Kaunitz AM.
Do mechanical methods of cervical ripening increase
infectious morbidity? A systematic review. Am J Obstet
Gynecol. 2008;199:17787.
34. Stock SJ, Ferguson E, Duffy A, Ford I, Chalmers J,
Norman JE. Outcomes of elective induction of labour
compared with expectant management: population based
study. BMJ. 2012;344:e2838.
2015 Nordic Federation of Societies of Obstetrics and Gynecology, Acta Obstetricia et Gynecologica Scandinavica 94 (2015) 608614
Vous aimerez peut-être aussi
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Health Infrastructure in India Present Challenges and Future ProspectsDocument10 pagesHealth Infrastructure in India Present Challenges and Future ProspectskasalammaPas encore d'évaluation
- Catherine Jenkins ReportDocument60 pagesCatherine Jenkins Reportjupiter stationeryPas encore d'évaluation
- Angle Orthod. 2015 85 5 881-9Document9 pagesAngle Orthod. 2015 85 5 881-9brookortontiaPas encore d'évaluation
- Maternal Pocket Book PDFDocument480 pagesMaternal Pocket Book PDFerwina nur100% (1)
- Vaccine Hesitancy Among Healthcare WorkersDocument33 pagesVaccine Hesitancy Among Healthcare WorkersFitz Jaminit100% (1)
- AdamRouilly Healthcare Education Catalogue 2015-16Document326 pagesAdamRouilly Healthcare Education Catalogue 2015-16NGUYEN HUU TRUONG TruongPas encore d'évaluation
- SGO 2016 CPT Code RVUDocument26 pagesSGO 2016 CPT Code RVUBrian SzenderPas encore d'évaluation
- Access To Mammography in New York City'Document43 pagesAccess To Mammography in New York City'NYCCouncilPas encore d'évaluation
- History of Sanitary EngineeringDocument2 pagesHistory of Sanitary EngineeringDon Matias100% (2)
- Stability Considerations in Liquid Dosage Forms Extemporaneously ...Document29 pagesStability Considerations in Liquid Dosage Forms Extemporaneously ...herryapt100% (1)
- Diagnostic ImagingDocument2 pagesDiagnostic ImagingNatalia RamírezPas encore d'évaluation
- AdhdDocument2 pagesAdhdAlexander SaladinPas encore d'évaluation
- The Impact of COVID-19 Pandemic On Dental Practice: A Questionnaire-Based ReportDocument20 pagesThe Impact of COVID-19 Pandemic On Dental Practice: A Questionnaire-Based ReportJaxine Caballero LabialPas encore d'évaluation
- Senarai Produk Yang Diluluskan Dalam PBKD380 5 Januari 2023 WebsiteDocument16 pagesSenarai Produk Yang Diluluskan Dalam PBKD380 5 Januari 2023 Websitearif azaliPas encore d'évaluation
- National Health Information System Strategic PlanDocument76 pagesNational Health Information System Strategic Plantolina chaliPas encore d'évaluation
- 1hospital ProfileDocument2 pages1hospital ProfileVenkatesh VenkatPas encore d'évaluation
- Roles and Functions of Local Government UnitsDocument3 pagesRoles and Functions of Local Government Unitsthepathfinderformercury100% (4)
- Prosthetics & Orthotics Clinic Procedures: Laaraib Nawaz Orthotist & ProsthetistDocument22 pagesProsthetics & Orthotics Clinic Procedures: Laaraib Nawaz Orthotist & ProsthetistGulzar AhmadPas encore d'évaluation
- 5 Hamad Core Comeptencies FinalDocument2 pages5 Hamad Core Comeptencies FinalvhonPas encore d'évaluation
- Suplemento mmc1Document69 pagesSuplemento mmc1ajax_telamonioPas encore d'évaluation
- Deposition Summary Sample - Litigation Support ServicesDocument10 pagesDeposition Summary Sample - Litigation Support ServicesMedico Legal Request LLCPas encore d'évaluation
- Advisory On Reiteration of Ao 2021 0012 Implementing Guidelines On The Medicine Access Program For Health 2Document7 pagesAdvisory On Reiteration of Ao 2021 0012 Implementing Guidelines On The Medicine Access Program For Health 2ncd.bulacanPas encore d'évaluation
- Resume Jessica Tundo December 2023Document2 pagesResume Jessica Tundo December 2023api-451737479Pas encore d'évaluation
- Test Bank For Tappans Handbook of Massage Therapy 6th Edition by BenjaminDocument36 pagesTest Bank For Tappans Handbook of Massage Therapy 6th Edition by Benjaminsublunardisbench.2jz85100% (39)
- Neurexan 84230 5000 5707 PDFDocument2 pagesNeurexan 84230 5000 5707 PDFAndrea Haydee Pinto HerreraPas encore d'évaluation
- SPJ Kerja BaktiDocument54 pagesSPJ Kerja BaktiRafi IrvaPas encore d'évaluation
- CertificatesDocument24 pagesCertificatesLizjasmine DimayaPas encore d'évaluation
- 05-Strategic Analysis of The Hospital Industry and HCADocument21 pages05-Strategic Analysis of The Hospital Industry and HCABhuvi VermaPas encore d'évaluation
- Ppan 2022 First Sem-General LunaDocument7 pagesPpan 2022 First Sem-General LunaroseannurakPas encore d'évaluation