Académique Documents
Professionnel Documents
Culture Documents
2ZR5YS29XX Unstable Angina Guidelines v2
Transféré par
Choi Eva Young ShineeCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
2ZR5YS29XX Unstable Angina Guidelines v2
Transféré par
Choi Eva Young ShineeDroits d'auteur :
Formats disponibles
Management of Unstable Angina and Non-ST
Elevation Myocardial Infarction Guidelines
Date: January 2009
Ref: CAR005
Version: 2
Guideline Profile
Policy Reference Number
Status
Version
Trust Leads
Implementation Date
Last Review Dates
Next Formal Review
Approval Record
Name
Clinical Governance and
Risk Committee
CAR005
Approved
2
Dr. Jagdip Sidhu
July 2005
January 2009
January 2011
Date
Feb 2009
Name
Tracker
Consultation
Dr Winston Martin
Cardiologist Consultants, A&E Consultants, Resuscitation Officer
Date
Date
July 2005
Dec 2008
References: Standards for Better Health, NHSLA, NICE Guidelines, Key Performance
Indicators (KPIs) and any other interlinking documents
NICE Clinical Guidance 48. 2007.
Guidelines for the diagnosis and
treatment of non-ST segment elevation
acute coronary syndromes. ESC, 2007.
Document Control/History
Edition No
Reason for change
V1
There have been significant changes in national and international guidelines
pertaining to the diagnosis and management of acute coronary syndromes.
Management of Unstable Angina and Non-St Elevation Myocardial Infarction Guidelines
Ref: CAR005 (v2)
January 2009
Status: Approved
Contents
Section
Page
Document Summary
1.
Introduction
2.
Purpose
3.
Aims and Objectives
4.
Definitions
5.
Accountabilities and Responsibilities
6.
Guidelines
7.
Equality Impact Assessment
8.
Training and Dissemination
9.
Monitoring Compliance with this Guideline
Appendix/Guideline
____________________________________________________________________________________________
Dartford and Gravesham NHS Trust
2
Management of Unstable Angina and Non-St Elevation Myocardial Infarction Guidelines
Ref: CAR005 (v2)
January 2009
Status: Approved
Document Summary
The guidelines for the management of Unstable Angina & ST
Elevation MI outline current best practice. The document outlines
emergency management in A&E and subsequent management in
CCU and medical wards. A risk assessment tool is included and
criteria for emergency coronary angiography are outlined. Drug
therapy, lifestyle advice and management in special patient groups
are also discussed.
____________________________________________________________________________________________
Dartford and Gravesham NHS Trust
3
Management of Unstable Angina and Non-St Elevation Myocardial Infarction Guidelines
Ref: CAR005 (v2)
January 2009
Status: Approved
1. Introduction
The Hospital Guidelines for the Management of Suspected Unstable Angina were
last published in 2005. Since that time, there have been significant changes in
national and international guidelines pertaining to the diagnosis and management of
acute coronary syndromes.
The cardiology department have decided to update the guidelines to reflect current
best practice and create two guidelines outlining:
a) Management of Acute ST elevation Myocardial Infarction (MI) and
b) Management of Unstable Angina & Non-ST elevation MI (this document)
2. Purpose
This document has been developed to update the previous guidelines and reflect
current best practice. This document is for the benefit of all staff in the Emergency
Medicine Directorate.
3. Aims and Objectives
The aim/objective of this document is to provide a concise, clinical guideline outlining
how to manage patients presenting with suspected unstable angina and Non-ST
elevation MI to DVH.
4. Definitions
A diagnosis of possible unstable angina or Non-ST elevation MI (NSTEMI) requires a
history of unrelieved ischaemic type pain, usually occurring without provocation. The
ECG may show regional ST depression or T wave inversion which is typically
reversible. However, NSTEMI/unstable angina may be associated with a normal
ECG.
Patients presenting with symptoms compatible with ischaemia and who have
elevated troponin without ST elevation on the ECG are classified as having NSTEMI.
5. Accountabilities and Responsibilities
The author will ensure that all relevant stakeholders have been consulted before this
document is submitted to the CRCG for formal approval. This includes
representatives from A&E, Acute Medical Consultants, CCU nursing staff, Specialist
Cardiac nurses and all 3 Consultant Cardiologists. All doctors and non-medical
professionals involved in the care of patients with unstable angina or NSTEMI are
responsible for following good practice as suggested in this guideline.
6. Guidelines
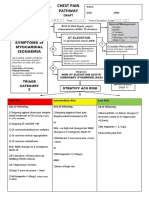
For the Management of Unstable Angina and Non ST Elevation Myocardial Infarction
see appendix A.
____________________________________________________________________________________________
Dartford and Gravesham NHS Trust
4
Management of Unstable Angina and Non-St Elevation Myocardial Infarction Guidelines
Ref: CAR005 (v2)
January 2009
Status: Approved
7. Equality Impact Assessment
The Trust aims to design and implement services, policies and measures that meet
the diverse needs of our service, population and workforce, ensuring that none are
placed at a disadvantage over others.
In order to meet these requirements, a single equality impact assessment is used to
assess all its guidelines and practices. This guidance was found to be compliant with
this philosophy.
8. Training and Dissemination
No specific training is required as there are no new practical processes/techniques in
this updated guideline. The approved document will be distributed to A&E, CCU and
emailed to all Consultants in the Emergency Medicine Directorate. Dr. Sidhu and
colleagues in the Cardiology Department will present the guidelines to A&E medical
staff and the Emergency Medicine Directorate.
No formal training is needed regarding this policy.
It is the responsibility of directorate or department to ensure that:
staff are aware of any new or newly revised policies
policies are appropriately filed and that old ones removed and destroyed
(keeping one copy for archiving purposes)
This document has been disseminated to all clinical and administration staff via
adagio and is available on the trust web site.
9. Monitoring Compliance with this Guideline
The management of NSTEMI is already audited prospectively as part of the ongoing
MINAP project. We have a dedicated specialist nurse who is responsible for this key,
national audit and performance indicator. In addition, compliance with all aspects of
this guideline will be assessed by regular audit. The first audit will be performed
within 4 months of approval of this policy and then repeated at least yearly to ensure
ongoing compliance. If an audit shows poor compliance then appropriate measures
will be taken and a re-audit performed within a shorter time frame. Initially, the
Consultant Cardiologists will take overall responsibility for auditing compliance with
the guideline.
____________________________________________________________________________________________
Dartford and Gravesham NHS Trust
5
Management of Unstable Angina and Non-St Elevation Myocardial Infarction Guidelines
Ref: CAR005 (v2)
January 2009
Status: Approved
Appendix A
Guidelines for the Management of Unstable Angina and Non ST
Elevation Myocardial Infarction
A diagnosis of NSTEMI/unstable angina requires only a history of unrelieved
ischaemic type pain, usually occurring without provocation. The ECG may show
regional ST depression or T wave inversion which are typically reversible. However,
NSTEMI/unstable angina may be associated with a normal ECG.
All patients should have serial ECG (every 15-30 minutes for 2 hours) recordings
to identify early changes (particularly ST elevation).
A Troponin I test taken 12 hours after the onset of pain, is mandatory.
Short Term Risk Assessment
The risk of progression to MI or death in the short term dictates management and
can be determined by assessing:
The likelihood of the patient having significant coronary artery disease (Tables 1 and
2)
The patients symptoms, haemodynamics and ECG (Table 3)
Cardiac troponin assay at least 12 hours after onset of pain. Patients presenting with
symptoms compatible with ischaemia and who have elevated troponin without ST
elevation on the ECG are classified as having NON ST ELEVATION MI.
Accident and Emergency Department
On arrival in the A&E department, the patient with possible cardiac chest pain should
have an ECG and be triaged category orange or in the case of direct medical referral,
the patients should be seen by the medical SHO as soon as possible.
If hypoxaemic give Oxygen therapy to keep O2 sats 94-98% (if known COPD
patient aim for O2 sats of 88-92% pending blood gas result)
Establish venous access and obtain blood samples for cardiac enzymes, U&E,
Glucose, Cholesterol and FBC. Take a Troponin I 12 hours from the onset of
symptoms
Attach patient to a cardiac monitor
Initiate emergency treatment (see below)
Obtain chest X-ray after initiating emergency treatment
Refer to medical team for assessment +/- transfer to CCU
____________________________________________________________________________________________
Dartford and Gravesham NHS Trust
6
Management of Unstable Angina and Non-St Elevation Myocardial Infarction Guidelines
Ref: CAR005 (v2)
January 2009
Status: Approved
Table 1. CV risk factor profile
Known coronary, peripheral or
cerebrovascular arterial disease
Diabetes
Smoker
Hypertension
Hypercholesterolaemia
Positive family history (parent or sibling) of premature (<60yrs) CV
death
Male sex
Central obesity
Asian race
Age Male>60/Female>70
Table 2. Likelihood of significant CHD in patients with chest pain
(modified from AHCPR guidelines)
High likelihood
Known history of documented IHD
Definite angina in M>60/F>70
Haemodynamic compromise or ECG
changes during pain
Ischaemic changes on ECG: ST elev. or
dep. >1mm or deep Twave inv.
Intermediate likelihood
Diabetes
Peripheral or cerebrovascular arterial
disease
Multiple risk factor profile
T wave inversion > 1mm (not aVr or
V1)
Asian racial group
Low likelihood
Atypical chest pain
Only 1 risk factor (NOT diabetes)
Normal ECG or T wave flattening or
inversion in isolated leads
Table 3: Short term risk of progression to death or nonfatal MI and appropriate action
(modified from AHCPR guidelines)
High risk
Moderate risk
Low risk
At least one of:
No high risk features but any of :
No high or moderate risk features but may have
any of:
With intermediate or high likelihood of CHD:
Any prolonged episode (>20 min) of rest
angina, now resolved
New onset angina at rest or minimal exertion
in the past 2 weeks
OR
Rest or nocturnal angina
Dynamic T wave changes
Pathological Q waves or resting ST dep. <
1mm in multiple leads
Recurrent angina despite starting or
increasing anti-anginal medication recently
Age >65yrs
Rest angina ongoing for >20 min
Pulmonary oedema
Hypotension
Dynamic ST changes
New deep T wave inversion
New or worsening MR
S3 or bibasal crackles
Cardiac Troponin T or I +ve
Action:
Admit to CCU
Manage as per guidelines
Consider early referral for intervention
Action:
Admit to CCU or ward with appropriate
monitoring/12-lead ECGs
Manage as per guidelines
Increased angina frequency, severity or
duration
Angina provoked at lower threshold
New onset angina beginning more than 2
weeks previously
Normal or unchanged ECG
Action:
Prescribe aspirin
Start or increase anti-anginal therapy
Arrange RACP review for outpt. assessment and
ETT
Instruct re:angina self-management
____________________________________________________________________________________________
Dartford and Gravesham NHS Trust
7
Management of Unstable Angina and Non-St Elevation Myocardial Infarction Guidelines
Ref: CAR005 (v2)
January 2009
Status: Approved
Emergency Treatment (Ref. Guidelines for the diagnosis and treatment of non-STsegment elevation acute coronary syndromes. ESC, 2007)
The aims of treatment are to relieve chest pain and to improve prognosis by
preventing progression to transmural myocardial infarction and death.
1.
2.
Nitrates
Sublingual GTN (400 mcg every 5 mins and up to 3 doses) may be given in
A&E but patients with ongoing or recurrent pain require IV GTN (50 mgs in 50
mls) infusion 1-10 mgs/hr.
The dose should be increased every 10 minutes and titrated against blood
pressure until pain is relieved, (maintain BP>100 systolic).
Beta-Blockers
These are first line drugs for pain relief in unstable angina and should be
given to all patients without specific contraindications. Treatment should be
with
Bisoprolol 2.5 uptitrated to10 mg od OR
Atenolol 25 uptitrated to 100 mgs od
Titrate up dose of beta-blocker if tolerated and resting Heart rate >70
3.
Aspirin
All patients should be treated with oral Aspirin 300 mgs initially and 75 mg od daily
thereafter.
Patients who develop dyspepsia while taking Aspirin should be prescribed:
Aspirin and PPI e.g. lansoprazole 30mg od
4.
Clopidogrel
All patients should receive 300mg of clopidogrel initially and then 75 mg od daily.
5.
Heparin
All patients should receive:
Low Molecular Weight Heparin (LMWH) by subcutaneous injection - enoxaparin
1mg/kg every 12 hours for at least 2 days. Continue for longer if the patient has
recurrent ischaemia
6.
Pain Relief
Very rarely pain is not relieved by any of the first line steps 1-5 and opiates are
needed. Give IV diamorphine (2 5 mgs)
Titrate to relieve pain and repeat every 15 minutes as necessary. IV Metoclopramide
10mgs prevents nausea and vomiting.
7.
Nicorandil
If the patient has recurrent chest pain despite the first line steps 1-5 consider adding
nicorandil. Starting dose is 10mg bd and this can be increased to 20mg bd if
necessary
8.
Calcium antagonists
These are not usually helpful in unstable angina and should only be prescribed if
asthma contraindicates -blockers or pain persists despite initial treatment. Starting
doses are Verapamil 40 mg tds or diltiazem 60 mg tds, these can be changed to od
____________________________________________________________________________________________
Dartford and Gravesham NHS Trust
8
Management of Unstable Angina and Non-St Elevation Myocardial Infarction Guidelines
Ref: CAR005 (v2)
January 2009
Status: Approved
slow release preparations prior to discharge. In patients taking beta-blockers,
Dihydropyridines (Amilodipine, Nifedipine) are preferred if heart rate is less than 60
beats per min.
Other Treatments
1.
Insulin
All known diabetic patients and those with an admission blood glucose 11 mmol/l
should receive an insulin, glucose and potassium infusion (Appendix 1).
2.
Glycoprotein IIb / IIIa Antagonists
In accordance with Guidance on the use of Glycoprotein IIb/IIIa inhibitors in the
treatment of acute coronary syndromes, from the National Institute for Clinical
Excellence.
Certain patients with unstable angina or NSTEMI are high risk:
a) with recurrent ischaemia, (either recurrent chest pain or dynamic ST segment
changes, in particular ST depression, or transient ST segment elevation)
b) with raised levels of troponin I AND continuing chest pain or dynamic ECG
changes after 12 hrs
c) who develop haemodynamic instability within observation period;
d) with major arrhythmias due to ischaemia (repetitive ventricular tachycardia,
ventricular fibrillation)
e) with early post-infarction unstable angina
These patients should be considered for treatment with Tirofiban (Aggrastat) as a
weight adjusted Infusion see BNF for contraindications, dosing and preparation.
These high risk patients should also be referred for urgent angiography and
revascularisation.
Notes:
Patients must be monitored very closely for signs of bleeding. Stop the infusion and
reported to the doctors immediately.
Low Molecular Weight Heparin to be given as standard protocol.
Check for pre-existing haemostatic abnormalities before infusion: Hb, platelet
count, creatinine, prothrombin time & activated partial thromboplastin time
Caution must be employed when used with other medical products that affect
haemostasis
Stop the infusion immediately if the patients condition changes and they
require thrombolytic therapy. Thrombolytic therapy must be initiated soon
after the Tirofiban infusion has been discontinued
For further information see data sheet
Management in CCU Secondary Prevention Treatment in CCU
Ensure that all emergency treatment has been initiated or is ongoing.
1.
Aspirin/Clopidogrel/LMWH.
LMWH can be stopped in those patients whose 12 hour troponin is negative AND
have no ischaemic ECG changes AND are painfree
2.
Beta-Blockers
If beta-blocker contraindicated consider verapamil or diltiazem
____________________________________________________________________________________________
Dartford and Gravesham NHS Trust
9
Management of Unstable Angina and Non-St Elevation Myocardial Infarction Guidelines
Ref: CAR005 (v2)
January 2009
Status: Approved
3.
Statins
All patients should receive dietary advice and a statin (simvastatin 40mg OR
atorvastatin 40mg od nocte) regardless of their actual cholesterol levels.
4.
Ace Inhibitors
All patients with NSTEMI should receive
Ramipril 2.5mg (when lying down)
Thereafter titrate Ramipril dose up to 10mg daily in single or divided
doses, blood pressure and renal function permitting
Caution
Creatinine >200 umol/l
Urea >12 mmol/l
Sodium <130mmol/l
Systolic blood pressure < 100mmHg
Diuretic dose > Frusemide 80mg/daily or equivalent
Know or suspected renal artery stenosis
Frail elderly
5.
Nicorandil (potassium channel-activator)
Patients with recurrent exertional chest pain already on a beta-blocker should receive
nicorandil in light of the reduction in mortality demonstrated in the IONA study
Initially 10mg BD for 2 weeks
Increasing to 20mg BD
6.
Eplerenone (aldosterone antagonist)
Patients with NSTEMI, confirmed by significant troponin rise, and clinical heart failure
with LV systolic dysfunction (EF<40% on echo) should receive eplerenone. The
decision to start eplerenone should be made by a consultant cardiologist as per
STEMI guidelines.
Investigations
1.
Chest x-ray
Patients who present with or develop pulmonary oedema will require further chest xrays to monitor the effects of treatment and should always have a chest x-ray
confirming resolution of lung changes.
2.
ECG
A 12 lead ECG should be obtained upon arrival in the CCU and every morning
thereafter until transfer to a general ward. Additional recordings will be necessary in
patients with ongoing or recurrent chest pain to rule out acute infarction. A final
recording should be obtained at the time of discharge from hospital and a copy
given to the patient to be taken with them should they need to return to the A&E
Department with recurrent symptoms.
3.
Blood Sampling
Samples for CK, Troponin I, U&E, Glucose, Cholesterol and FBC should already be
available from A&E. Further CK/ CK-MB should not be necessary. If the patient
experiences further pain a troponin I should be taken 12 after the symptoms.
____________________________________________________________________________________________
Dartford and Gravesham NHS Trust
10
Management of Unstable Angina and Non-St Elevation Myocardial Infarction Guidelines
Ref: CAR005 (v2)
January 2009
Status: Approved
Management in a General Ward
In most cases, patients can be transferred to a general ward or stepdown ward after
24 hours, so long as they are pain free.
1.
Mobilisation
Patients remain on full bed rest for the first 24 hours, on day 2 they may sit out of
bed. The next day they may walk to the toilet and around the ward and on day 4 they
may try the stairs. Thereafter, walking distances should gradually be extended with a
view to discharge on day 5. However, this may be varied according to capability and
risk.
2.
Lifestyle Advice and rehabilitation
All patients treated in the CCU with cardiac chest pain (AMI or unstable angina) will
be reviewed by the cardiac care nurses team who will give lifestyle advice (see
below), and an invitation to attend the rehabilitation course if appropriate. All patients
must be advised to stop smoking and to reduce total fat intake whilst increasing the
polyunsaturated to saturated fat ratio. Patients with confirmed NSTEMI should be
encouraged to eat 2 to 4 portions of oily fish per week and if patients cannot achieve
this then consider prescribing 1g daily of omega-3-acid ethyl esters licensed for
secondary prevention post MI (ref NICE 2007). Obese patients should also reduce
calorie intake. Regular aerobic exercise should be encouraged, which for most
patients will take the form of a daily walking programme, the distance increasing up
to a level appropriate for the patients physical condition.
3.
Stress Testing
Pre-discharge stress testing is only weakly predictive of risk but may be used in
selected cases (i.e. those patients whose ECGs show no ischaemia and are troponin
negative). Ischaemic ST depression early (stage 1) during exercise, or at very low
exercise tolerance may indicate increased risk of myocardial infarction and death,
and provides grounds for cardiac catheterisation. Patients pre-selected for cardiac
catheterisation on the basis that they are high or moderate risk (see Tables 2 & 3)
do not need a stress test. Clinical discretion should be used in physically frail
patients. (Appendix 2)
4.
Cardiac Catheterisation and revascularisation
The cardiology team should assess all inpatients with NSTEMI or presumed unstable
angina with a view to performing inpatient coronary angiography +/revascularisation.
Urgent catheterisation may be necessary for patients with ongoing or recurrent
chest pain.
____________________________________________________________________________________________
Dartford and Gravesham NHS Trust
11
Management of Unstable Angina and Non-St Elevation Myocardial Infarction Guidelines
Ref: CAR005 (v2)
January 2009
Status: Approved
Appendix B
Standard Regime
Check serum potassium and blood glucose before infusion
5% Dextrose (500ml) with 40mmol/l KCl (unless serum potassium >5mmol/l) plus 80
units Actrapid Insulin.
Start infusion at 15ml/hr
Aim for blood glucose of 7-10mmol/l
Check blood glucose hourly after rate change and then every 2 hours
After first hour of starting infusion, decrease infusion rate by 6mls/hr if blood glucose
now below 13mmol/l
After 10pm if blood glucose stable and < 11mmol reduce infusion rate by 50% but not
less than 3ml/hr
Check serum potassium before infusion starts and again after 6hr and 12 hr
Ensure referral to the ECG department has been made for an early echo
If Blood Glucose >22mmol/l
Bolus dose of IV Human Actrapid 8 units.
____________________________________________________________________________________________
Dartford and Gravesham NHS Trust
12
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (894)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- L3 A&p#3 With AnswersDocument7 pagesL3 A&p#3 With AnswersFergus DalePas encore d'évaluation
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Lab 10 Blood and The HeartDocument6 pagesLab 10 Blood and The Heartcindy tranPas encore d'évaluation
- Textbook of GB Madhuri For Cardio-Respiratory Cardiac Surgery and Thoracic Surgery ConditionsDocument340 pagesTextbook of GB Madhuri For Cardio-Respiratory Cardiac Surgery and Thoracic Surgery ConditionsBpt4 Kims100% (1)
- Huh Ewih EwfioewoieDocument1 pageHuh Ewih EwfioewoieChoi Eva Young ShineePas encore d'évaluation
- JKDSJHFLK WDocument1 pageJKDSJHFLK WChoi Eva Young ShineePas encore d'évaluation
- Ii WaijDocument1 pageIi WaijChoi Eva Young ShineePas encore d'évaluation
- Mekanisme Kerja Pelurus RambutDocument2 pagesMekanisme Kerja Pelurus RambutChoi Eva Young ShineePas encore d'évaluation
- 10 1002@acr 21797Document6 pages10 1002@acr 21797Choi Eva Young ShineePas encore d'évaluation
- 10 1016@j Ijcard 2015 05 023Document3 pages10 1016@j Ijcard 2015 05 023Choi Eva Young ShineePas encore d'évaluation
- Shane P. Prejean, MD, Munaib Din, BSC, Eliana Reyes, MD, PHD, and Fadi G. Hage, MD, FasncDocument8 pagesShane P. Prejean, MD, Munaib Din, BSC, Eliana Reyes, MD, PHD, and Fadi G. Hage, MD, FasncwidyadariPas encore d'évaluation
- What Is ECG?Document2 pagesWhat Is ECG?Lê Thanh HàPas encore d'évaluation
- Neonatal ShockDocument91 pagesNeonatal ShockCapricious BibekPas encore d'évaluation
- Kode Diagnosa PRBDocument21 pagesKode Diagnosa PRBRahmat GzPas encore d'évaluation
- Acls Algorithms 2012Document12 pagesAcls Algorithms 2012Prashanth KumarPas encore d'évaluation
- Case Based Discussion Astma Bronchiale, Hypertension: Chusna Helmia 01.209.5853Document26 pagesCase Based Discussion Astma Bronchiale, Hypertension: Chusna Helmia 01.209.5853helmiaPas encore d'évaluation
- CMS 251 Unit 1 Cardiovascular SystemDocument114 pagesCMS 251 Unit 1 Cardiovascular SystemAmon RicoPas encore d'évaluation
- Research Poster PresentationDocument1 pageResearch Poster Presentationapi-328441669Pas encore d'évaluation
- 9700 s02 QP 2 PDFDocument12 pages9700 s02 QP 2 PDFIG UnionPas encore d'évaluation
- Q2 Second Periodical Test 2023 2024Document12 pagesQ2 Second Periodical Test 2023 2024ALMA BANIELPas encore d'évaluation
- Abordaje de Paciente Con SoploDocument11 pagesAbordaje de Paciente Con SoploRigo rogerPas encore d'évaluation
- Igcse Biology Notes: Unit 1: Characteristics of LivingDocument50 pagesIgcse Biology Notes: Unit 1: Characteristics of Livingnana bananaPas encore d'évaluation
- Anesthetic Considerations For Ambulatory Anesthesia: Advantages of Ambulatory SurgeryDocument4 pagesAnesthetic Considerations For Ambulatory Anesthesia: Advantages of Ambulatory SurgeryIsabel CastilloPas encore d'évaluation
- European Heart Journal (2003) 24, 787-788Document2 pagesEuropean Heart Journal (2003) 24, 787-788api-26263700Pas encore d'évaluation
- Hari Sharma ChapterDocument14 pagesHari Sharma Chapterdynamic2004Pas encore d'évaluation
- ACLS Test Sinus BradycardiaDocument1 pageACLS Test Sinus BradycardiaFiya Sahrul0% (1)
- Blood Transfusion in History PDFDocument48 pagesBlood Transfusion in History PDFjozsef10Pas encore d'évaluation
- Quit Smoking BrochureDocument21 pagesQuit Smoking BrochureDumitrita NegoitaPas encore d'évaluation
- Exercise Tolerance TestDocument15 pagesExercise Tolerance TestahmedPas encore d'évaluation
- Chest Pain Pathway GuideDocument4 pagesChest Pain Pathway GuidefauzanPas encore d'évaluation
- Agricultural ErgonomicsDocument7 pagesAgricultural ErgonomicsIan Jay TumulakPas encore d'évaluation
- 2005 10 24 Review AnswersDocument30 pages2005 10 24 Review Answersaip1000Pas encore d'évaluation
- Nursing Care Plan For HypertentionDocument2 pagesNursing Care Plan For HypertentionLunnet Begg100% (1)
- CH4:Biological molecules overviewDocument34 pagesCH4:Biological molecules overviewToXicPas encore d'évaluation
- Chest X-Rays:: Case Studies From The FieldDocument12 pagesChest X-Rays:: Case Studies From The FieldRiki AntoPas encore d'évaluation
- Krok-2 2020 Previous Year Paper | 2020 Krok-2 PaperDocument2 pagesKrok-2 2020 Previous Year Paper | 2020 Krok-2 PaperEuiJinMoonPas encore d'évaluation
- Comprehensive revision test - Basics 1-5Document16 pagesComprehensive revision test - Basics 1-5drpnnreddyPas encore d'évaluation