Académique Documents
Professionnel Documents
Culture Documents
Typhoid Fever
Transféré par
adiDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Typhoid Fever
Transféré par
adiDroits d'auteur :
Formats disponibles
Indian J Med Res 131, June 2010, pp 799-803
Investigation of the outbreak of typhoid in a village of Thar Desert
Rajasthan, India
P.K. Anand & R. Ramakrishnan*
Desert Medicine Research Centre (ICMR), Jodhpur & *National Institute of Epidemiology (ICMR)
Chennai, India
Received January 15, 2009
Background & objectives: Outbreaks of typhoid have been reported from Maharashtra, Bangalore, West
Bengal and Pondicherry in India but rarely from Rajasthan. We investigated an outbreak of typhoid in
a village of Thar Desert of Rajasthan.
Methods: A retrospective cohort study was carried out during May-July 2007 in Varkana village, Pali
district, Rajasthan, to identify the risk factor for disease. The information on outbreak was collected and
then described in time, place and person characteristics to arrive at aetiological hypotheses.
Results: There were 219 cases of typhoid in village. Attack rate was 104 cases per 1000 population.
Maximum attack rate of 276 cases per 1000 population was noted in persons of 10-14 yr age group.
Forty three serum samples were reported positive for Widal agglutination test out of 70 tested. Drinking
of water from government overhead tanks was associated with disease significantly (RR= 11.1, 95%
CI= 3.7-33). Two of the three water samples from government tanks were found positive for faecal
contamination.
Interpretation & conclusion: The outbreak of typhoid in a village affected >200 persons of all age groups
and both gender. Exposure to the drinking water from government tanks was found significantly
associated with the disease. Preventive and control measures undertaken after analytical epidemiological
study helped in terminating the outbreak.
Key words Thar Desert - typhoid outbreak - water tanks
resistance in 95.1 per cent isolates of Salmonella Typhi
to chloramphenicol, ampicillin and co-trimoxazole5.
Chloramphenicol resistant isolates of Salmonella
Typhi have been reported from West Bengal6,7. Only
limited outbreaks of typhoid were subjected to proper
epidemiological investigation3,4. Kulkarni et al3
identified the role of well water in the outbreak of
typhoid fever in Katkalamba village of Nanded district
Typhoid is under regular surveillance by integrated
disease surveillance project of India1. An estimate of
annual typhoid incidence rate of 493.5 cases per 100,000
person years was reported in one study2. Outbreaks
of typhoid have been reported from Maharashtra3,4,
Bangalore5, West Bengal6,7 and Pondicherry8 in India.
Most of these outbreaks were of drug resistant strain of
Salmonella Typhi5-8. Rathish et al5 reported triple drug
799
800
INDIAN J MED RES, JUNE 2010
of Maharashtra. Sathe et al4 found massive central
contamination of the ill maintained municipal water
supply system in Maharashtra11.
Sporadic cases of typhoid have been reported from
Rajasthan9,10. We investigated an outbreak of fever
with headache and stomachache in Varkana village
of district Pali, Rajasthan in 2007. This investigation
was carried out as a field assignment under field
epidemiology training programme, at National Institute
of Epidemiology, Chennai, India.
Material & Methods
The study was carried out in village Varkana (with
a population of 2100), district Pali (24.45 - 26.75
degree North Latitude and 72.48 - 74.20 degree East
Longitude) in Rajasthan, India. It is geographically
located in vegetation and water scarce agro climate
of Thar Desert. Health care services to residents of
village Varkana are delivered through Health Ad Post
Varkana, primary health centre (PHC) Rani, community
health centre, Bali and district hospital, Pali.
Having alerted about outbreak of fever in village
Varkana on June 7, 2007, we reached the place
and collected surveillance data on patients age in
completed years, gender, locality of residence, and date
of examination at Health Ad Post Varkana. Laboratory
results of peripheral microscopic examination for
malaria parasite using Jasvant Singh & Bhattacherji
(JSB) thick and thin smears staining technique and
rapid screening Widal test, done on blood samples of
patients of Varkana village were obtained from PHC
Rani.
Operational criteria used to define suspected case
of typhoid included occurrence of sustained high grade
fever with or without headache, stomachache, diarrhoea,
and/or, constipation, vomiting, loss of appetite with
negative test result for malaria in residents of Varkana
village on any day since May 7, 2007.
Surveillance data of patients fulfilling this
operational criterion were included in study. These
cases were described in terms of time, place and person
distribution through epidemic curve, spot map and
frequency table respectively to formulate aetiological
hypotheses.
This analytical retrospective cohort study was
undertaken on a random cohort sample (n=108) of
village residents to test the significance of aetiological
hypotheses. This sample size was estimated based on
village population 2100, 50 per cent assumed proportion
of exposure, 95 per cent confidence coefficient, 10 per
cent confidence interval including 12 more residents in
anticipation of non-response during study. N= Z2 pq/d2
was used for sample size estimation.
To reach to cohort sample of 108 random village
residents, 108 households were selected through
draw of name slips prepared from the village census
list. then field team visited each selected household.
One household member, seen first among all family
members at home visit, was recruited in retrospective
analytical study from each of such selected households
leaving all other family members.
Socio-demographic data, presence or absence of
operational criterion for suspected case of typhoid,
rapid screening Widal test result and exposure to
common meal, drinking water in the preceding one
month was collected. This study was carried out during
May-July 2007.
Data were analyzed in Epiinfo (version 3.5.1).
Statistical power of the association based on normal
approximation with continuity correction was estimated
using OpenEpi software version 2.3.
Rapid screening slide test for typhoid was
performed with Typhiscreen-S (Monozyme India
Limited, Secunderabad) at primary health centre, Rani,
for those patients who could afford the price of the
test to screen the presence or absence of antibodies
against antigens of Salmonella Typhi and Salmonella
Paratyphi A and B. Presence of agglutination was
noted as positive test as per manufacturers instruction
and indicated presence of corresponding antibodies in
serum. Since this was qualitative test, antibody titre
was not measured. Results of this test were used to
formulate the diagnosis of outbreak.
Results
There was no change in surveillance system and
population movement of the affected area. The usual
rate of fever was 1-2 cases per month in affected village
in the last three years. Most of the cases were suffering
from continuous fever with stomachache, pain in
abdomen, diarrhoea or constipation and vomiting. All
cases were found to be negative for malaria. Till June
8, 2007, a total of 209 suspected typhoid cases fulfilling
operational criteria were reported through surveillance
system in Varkana village. The number rose to 219
by the time the follow up visit was made on July 4,
2007. Forty eight per cent of cases were males. Forty
three out of 70 patients serum samples sent for rapid
screening Widal test were positive.
ANAND & RAMAKRISHNAN: TYPHOID OUTBREAK IN DESERT
There was no common meal, food handler/
distributor in village in last one-month period. People
used the open place for defecation near village.
Epidemic curve began on May 18, 2007 and reached
at peak on June 6, 2007 after that it declined. In four
801
weeks duration the curve rose gradually till its peak,
declined later, making a unimodel curve (Fig. 1).
Drinking water was available either through
government supply or personal tube wells. Government
water supply was through 2 hand pumps and 3 overhead
tanks at common places. There was open well, supplying
water to all the three overhead tanks in village. Spot
map shows the clustering of cases in area supplied by
government tanks for drinking water. The Meghwal
colony, Khimawat colony, Dhani and Teachers colony
had shown a few cases. Member of these colonies were
using water either from government hand pump or
through personal tube wells (Fig. 2).
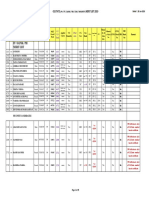
Attack rate of disease was 104 cases per 1000
population (95.45 and 114 cases per 1000 population in
male and female respectively). Attack rate was 133.33
and 276 cases per 1000 population in age groups of 5-9
and 10-14 yr respectively (Table I).
Fig. 1. Epigraph for onset of cases of typhoid in Varkana village,
district Pali, Rajasthan, India, 2007.
Among the 108 random villagers interviewed
for retrospective analytical study, 60 were found
to either have suffered from disease or suffering
currently. Relative risk of disease was 11.1 with 95
per cent confidence interval of 3.7-33.0, among those
exposed to water from government tanks as compared
Table I. Age- and gender-wise attack rates of typhoid in village
Varkana, district Pali, Rajasthan
Characteristics
Total cases
Population
Attack rate
(cases per 1000
population)
Sex:
Male
105
1100
95.45
Female
114
1000
114
0-4
15
270
55.55
5-9
34
255
133.33
10-14
69
250
276
>15
101
1325
76.22
219
2100
104.28
Age group (yr):
Fig. 2. Spot map for distribution of households of diseased (Orange
spots) and non-diseased (Blank circles) persons in village Varkana,
district Pali, Rajasthan.
Total
Table II. Relative risks of typhoid amongst persons exposed to different sources of drinking water in village Varkana, district Pali,
Rajasthan
Source of drinking water
Disease present Disease absent Incidence rate
Relative risk
95% CI
Statistical power
(%)
with continuity
correction (%)
Govt. tank
52
4
92.8
11.1
3.7-33
100
Govt. tank & hand pump & 5
11
31.2
3.75
1.02-13.8
36.49
personal well
Hand pump & personal well 3
33
8.3
Reference
Reference
Reference
802
INDIAN J MED RES, JUNE 2010
to those exposed to hand pumps and personal wells
for drinking. This association was found significant
(P<0.05; Table II).
Persons exposed to government tanks and hand
pumps and personal wells were at 3.75 times higher
risk of developing disease than the reference group with
95 per cent CI limits of 1.02-13.8. 1-tailed probability
value for Fisher Exact test found was 0.048, which was
significant.
Of the three water samples from each of
three government tanks sent to laboratory, Public
Health Engineering Department, Jodhpur for faecal
contamination test, two were positive for presumptive
coliform test. Two water samples from different hand
pump sent for test reported negative.
Discussion
The findings of the study, verified the existence of
an outbreak in village Varkana, district Pali, Rajasthan.
Clinical presentation of cases was in accordance to the
WHO criterion11. Epidemic curve with single peak and
moderate duration of about one month is suggestive of
the common source outbreak of disease with incubation
period of approximately 15 days to one month, which
is a similar requisite for typhoid11.
In high and medium incidence areas for typhoid,
maximum proportion of cases occurs in 0-4 yr age
group, however in low incidence rate areas maximum
proportion of cases belong to 20-24 yr age group12.
During this outbreak, the maximum attack rate was
noted in 10-14 yr age group suggesting low incidence
of typhoid in desert of India.
Exposure to the drinking water from government
water supply was found significantly associated
with the disease. Dose response effects observed
with the exposure of tank water add evidence for its
causality. This finding is in consistency with other
investigated outbreaks of typhoid in India where
contaminated drinking water was found as risk
factors3,4. Environmental condition around open
well supported the possibilities of its contamination.
Faecal contamination seen in water samples provided
additional evidence for the source of infection.
There were a few limitations in this study.
Drinking water was tested for faecal contamination,
which is indirect evidence for probable presence of
Salmonella Typhi in water. Microbiological testing of
water for causative bacteria was not done. Probable
case definition for typhoid was used in this outbreak.
Because of cross reactivity of antigens of Salmonella
Typhi with non-typhoidal salmonella, malaria and
dengue, false positive cases would have been included
in our study13. Malaria was excluded based on negative
blood smear examination. Though nobody presented
with retro-orbital pain, which can occur in dengue14-15,
we could not exclude it based on clinical ground.
Probability of dengue may be minimal in hot weather
of desert village, because it is mostly considered a
problem, associated with urbanization16. Non-typhoidal
salmonella could not be excluded.
Acknowledgment
Authors thank Dr Sanjeev Tak, Deputy Chief Medical &
Health Officer, Bali for his support in accessing the surveillance
and laboratory data of patients, and also thank all team members of
Ad post Varkana, community health centre, Rani, who worked with
us in this investigation.
References
1.
World Health Organization, India. Integrated disease
surveillance (IDSP). Project implementation plan. Ministry
of Health & Family Welfare, Government of India. Available
from:
http://www.whoindia.org/LinkFiles/IDSP_PIPs.pdf,
accessed on January 10, 2009.
2.
Ochiai RL, Acosta CJ, Danovaro-Holliday MC, Baiqing
D, Bhattacharya SK, Agtini MD, et al; Domi typhoid study
group. A study of typhoid fever in five Asian countries: disease
burden and implications for controls. Bull World Health Organ
2008; 86 : 260-8.
3.
Kulkarni AP, Powar RM, Mangalkar SM, Kulkarni VA,
Nagalgaonkar RN. Epidemiological investigation of an
outbreak of enteric fever in a village in Maharashtra.
J Commun Dis 1996; 28 : 117-21.
4.
Sathe PV, Karandikar VN, Gupte MD, Niphadkar KB, Joshi
BN, Polakhare JK, et al. Investigation report of an epidemic of
tyhoid fever. Int J Epidemiol 1983; 12 : 215-9.
5.
Rathish KC, Chandrashekar MR, Nagesha CN. An outbreak
of multidrug resistant typhoid fever in Bangalore. Indian J
Pediatr 1995; 62 : 445-8.
6.
Haldar KK, Basak S, Chakraborty AK, Das S. Transferable
drug resistance in Salmonella typhi strains isolated from an
outbreak at Calcutta in the recent past. J Indian Med Assoc
1995; 93 : 299-300.
7.
Sarkar AK, Ganguly S, Ganguly S. Recent outbreak of
chloramphenicol resistant typhoid fever in West Bengal.
J Indian Med Assoc 1991; 89 : 257-9.
8.
Rao RS, Amarnath SK, Sujatha S. An outbreak of typhoid due
to multidrug resistant Salmonella typhi in Pondicherry. Trans
R Soc Trop Med Hyg 1992; 86 : 204-5.
9.
Maheshwari VD, Agarwal SK. Present status of drug resistance
in cases of enteric ever in Rajasthan. J Assoc Physicians India
1996; 44 : 618-9.
ANAND & RAMAKRISHNAN: TYPHOID OUTBREAK IN DESERT
10. Saxena MM, Chhabra C. A status survey of common waterborne diseases in desert city Bikaner (NW Rajasthan, India).
J Commun Dis 2004; 36 : 53-9.
11. World Health Organization. WHO 2010. Typhoid fever;
[about 2 screens]. Available from: http://www.who.int/topics/
typhoid_fever/en/, accessed on January 10, 2009.
12. Crump JA, Luby SP, Mintz ED. The global burden of typhoid
fever. Bull World Health Organ 2004; 82 : 346-53.
13. Olopoenia LA, King AL. Widal agglutination test - 100 years
later: still plagued by controversy. Postgrad Med J 2000; 76 : 80-4.
803
14. Gulati S, Maheshwari A. Atypical manifestations of dengue.
Trop Med Int Health 2007; 12 : 1087-95.
15. World Health Organization, Regional Office for South East
Asia Region. New Delhi: Guidelines for treatment of dengue
fever/dengue hemorrhagic fever in small hospitals. Available
from: http://www.searo.who.int/LinkFiles/Dengue_Guidelinedengue.pdf, accessed on January 12, 2009.
16. Chaturvedi UC. The curse of dengue. Indian J Med Res 2006;
124 : 467-70.
Reprint requests: Dr P.K. Anand, Scientist C, Desert Medicine Research Centre (ICMR), New Pali Road
Jodhpur 342 005, Rajasthan, India
e-mail: pkanand@dmrcjodhpur.org, ananddmrc@yahoo.co.in
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Department of Pathology Pt. J. N. M. Medical College & Dr. B.R.A.M. Hospital, Raipur, C.GDocument1 pageDepartment of Pathology Pt. J. N. M. Medical College & Dr. B.R.A.M. Hospital, Raipur, C.GadiPas encore d'évaluation
- Informed Consent Form (PICF) and Participant Information Sheet (PIS), Both in English andDocument4 pagesInformed Consent Form (PICF) and Participant Information Sheet (PIS), Both in English andadiPas encore d'évaluation
- Case of Obstructive JaundiceDocument38 pagesCase of Obstructive JaundiceadiPas encore d'évaluation
- Acute Transfusion ReactionsDocument29 pagesAcute Transfusion ReactionsadiPas encore d'évaluation
- High Performance Liquid ChromatographyDocument4 pagesHigh Performance Liquid ChromatographyadiPas encore d'évaluation
- Dr. Monika NemaDocument19 pagesDr. Monika NemaadiPas encore d'évaluation
- Midterm Lecture ExamDocument5 pagesMidterm Lecture ExamMartin Clyde100% (1)
- Rapid Diagnostic Tests: Investigation Strategies and MethodsDocument35 pagesRapid Diagnostic Tests: Investigation Strategies and Methodsmuhammadalfian4258Pas encore d'évaluation
- HPLCDocument6 pagesHPLCMohammad Khaier KaliliPas encore d'évaluation
- High Performance Liquid ChromatographyDocument4 pagesHigh Performance Liquid ChromatographyadiPas encore d'évaluation
- RT-PCR AnalysisDocument37 pagesRT-PCR AnalysisKriselda May TorioPas encore d'évaluation
- 500 MCsDocument27 pages500 MCsadiPas encore d'évaluation
- Coronavirustesttes WpsofficeDocument14 pagesCoronavirustesttes WpsofficeadiPas encore d'évaluation
- High Performance Liquid ChromatographyDocument4 pagesHigh Performance Liquid ChromatographyadiPas encore d'évaluation
- Nephrology Notes Review - Passmedicine 2012Document33 pagesNephrology Notes Review - Passmedicine 2012adiPas encore d'évaluation
- CounsilingSuchna 04072019-1Document1 pageCounsilingSuchna 04072019-1adiPas encore d'évaluation
- NatNeurocon ProgrammeDocument4 pagesNatNeurocon ProgrammeadiPas encore d'évaluation
- 21जुन योगा दिवस पत्रDocument2 pages21जुन योगा दिवस पत्रadiPas encore d'évaluation
- New Doc 2019-05-29 11.56.03 - 2-3 PDFDocument1 pageNew Doc 2019-05-29 11.56.03 - 2-3 PDFadiPas encore d'évaluation
- Merit List NEET UG 2019-1Document25 pagesMerit List NEET UG 2019-1adiPas encore d'évaluation
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- Imi-Siw Monitoring FormatDocument3 pagesImi-Siw Monitoring FormatadiPas encore d'évaluation
- NEET-PG 2014 - 2015: Important One Liners For Neet - 5Document22 pagesNEET-PG 2014 - 2015: Important One Liners For Neet - 5adiPas encore d'évaluation
- Je LDwki HIp 5 V V6 JsDocument1 pageJe LDwki HIp 5 V V6 JsadiPas encore d'évaluation
- Aipgmee 2010Document34 pagesAipgmee 2010harideepPas encore d'évaluation
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- NRC Sam Chart: For Oedematous Child Admission Weight Will Be The Weight Taken On The Day The Child Has No OedemaDocument5 pagesNRC Sam Chart: For Oedematous Child Admission Weight Will Be The Weight Taken On The Day The Child Has No OedemaadiPas encore d'évaluation
- Cascade Training: Introduction of Rotavirus VaccineDocument14 pagesCascade Training: Introduction of Rotavirus VaccineadiPas encore d'évaluation
- Nephrology Notes Review - Passmedicine 2012Document33 pagesNephrology Notes Review - Passmedicine 2012adiPas encore d'évaluation
- Nephrology Notes Review - Passmedicine 2012Document33 pagesNephrology Notes Review - Passmedicine 2012adiPas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (120)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Infectous DiseaseDocument9 pagesInfectous DiseasejamikawasPas encore d'évaluation
- Pharmaceuticals 11 00094Document14 pagesPharmaceuticals 11 00094CindyGaniPas encore d'évaluation
- Extraction of Primary TeethDocument15 pagesExtraction of Primary TeethDr. Abdulsalam Awas Dental CenterPas encore d'évaluation
- AntihistaminesDocument2 pagesAntihistaminesmercywicherPas encore d'évaluation
- Drug Name Dosage, Route, Frequency Mechanism of Action Indication Contraindication Adverse Effect Nursing ResponsibilitiesDocument1 pageDrug Name Dosage, Route, Frequency Mechanism of Action Indication Contraindication Adverse Effect Nursing ResponsibilitiesJonna Mae TurquezaPas encore d'évaluation
- Reality TherapyDocument1 pageReality TherapyTinoRepaso100% (1)
- Fast Dispersible Tablet-1Document26 pagesFast Dispersible Tablet-1Hely PatelPas encore d'évaluation
- Principles of Capture - PrintableDocument51 pagesPrinciples of Capture - PrintableNguyen Thi Phuong NhiPas encore d'évaluation
- Surgical Sutures-10Document25 pagesSurgical Sutures-10badar_aqPas encore d'évaluation
- 2Document78 pages2api-3744136Pas encore d'évaluation
- Brain CTDocument83 pagesBrain CTArvind Jha100% (2)
- Physiology of HemoglobinDocument15 pagesPhysiology of HemoglobinIbrahim YahyaPas encore d'évaluation
- Mahawan Vs People of The Philippines DigestDocument1 pageMahawan Vs People of The Philippines DigestJoy Ann Ferrer100% (1)
- Proliferative EndometriumDocument4 pagesProliferative EndometriumKristine Dela CruzPas encore d'évaluation
- The Anatomical Record - 2021 - Vater - The Topographic and Systematic Anatomy of The Alpaca StomachDocument15 pagesThe Anatomical Record - 2021 - Vater - The Topographic and Systematic Anatomy of The Alpaca StomachMai Chi PhạmPas encore d'évaluation
- Jet Lag PDFDocument8 pagesJet Lag PDFIan FitzpatrickPas encore d'évaluation
- Total Protein SpinreactDocument1 pageTotal Protein Spinreactariyan khanPas encore d'évaluation
- Clinic Department InfoDocument66 pagesClinic Department InfoHumera ShaikhPas encore d'évaluation
- Timetable 1Document1 pageTimetable 1sunilbijlaniPas encore d'évaluation
- Blood Cold ChainDocument74 pagesBlood Cold Chainشريف عبد المنعمPas encore d'évaluation
- PTIDocument19 pagesPTIDick Jerzy Salazar FranciaPas encore d'évaluation
- Mindray BS-120 / BS-200 / BS-300 / BS-380 / BS-400: MTD Diagnostics, SRLDocument40 pagesMindray BS-120 / BS-200 / BS-300 / BS-380 / BS-400: MTD Diagnostics, SRLCarlos SoutoPas encore d'évaluation
- ACD/Percepta: Overview of The ModulesDocument91 pagesACD/Percepta: Overview of The ModulesTinto J AlencherryPas encore d'évaluation
- Topical Lotion Formulation PDFDocument45 pagesTopical Lotion Formulation PDFMustafa ArarPas encore d'évaluation
- Himalaya PublicationDocument20 pagesHimalaya Publicationanand1540Pas encore d'évaluation
- Precedex DosingDocument4 pagesPrecedex DosingnonemiscPas encore d'évaluation
- Universal Free Reiki PDFDocument4 pagesUniversal Free Reiki PDFSabiduria Pura100% (1)
- Intertrigo and Secondary Skin InfectionsDocument5 pagesIntertrigo and Secondary Skin Infectionskhalizamaulina100% (1)
- Pharmacy Calculations Review: Pharmacy Tech Topics™ Volume 16 Number 3 July 2011Document24 pagesPharmacy Calculations Review: Pharmacy Tech Topics™ Volume 16 Number 3 July 2011Mirumbi Kefa MomanyiPas encore d'évaluation
- Mosquitoe Repellent Plants Final 31 AugustDocument48 pagesMosquitoe Repellent Plants Final 31 AugustHomero SilvaPas encore d'évaluation