Académique Documents
Professionnel Documents
Culture Documents
Clinica Chimica Acta: Giuseppe Lippi, Elisa Danese, Gianfranco Cervellin, Martina Montagnana
Transféré par
Ria DeviTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Clinica Chimica Acta: Giuseppe Lippi, Elisa Danese, Gianfranco Cervellin, Martina Montagnana
Transféré par
Ria DeviDroits d'auteur :
Formats disponibles
Clinica Chimica Acta 430 (2014) 164170
Contents lists available at ScienceDirect
Clinica Chimica Acta
journal homepage: www.elsevier.com/locate/clinchim
Invited critical review
Laboratory diagnostics of spontaneous bacterial peritonitis
Giuseppe Lippi a,, Elisa Danese b, Gianfranco Cervellin c, Martina Montagnana b
a
b
c
Laboratory of Clinical Chemistry and Hematology, Academic Hospital of Parma, Parma, Italy
Laboratory of Clinical Chemistry and Hematology, University of Verona, Verona, Italy
Emergency Department, Academic Hospital of Parma, Parma, Italy
a r t i c l e
i n f o
Article history:
Received 1 December 2013
Received in revised form 9 January 2014
Accepted 11 January 2014
Available online 6 February 2014
Keywords:
Laboratory diagnostics
Peritonitis
Spontaneous bacterial peritonitis
Peritoneal uid
Procalcitonin
a b s t r a c t
The term peritonitis indicates an inammatory process involving the peritoneum that is most frequently infectious in nature. Primary or spontaneous bacterial peritonitis (SBP) typically occurs when a bacterial infection
spreads to the peritoneum across the gut wall or mesenteric lymphatics or, less frequently, from hematogenous
transmission in combination with impaired immune system and in absence of an identied intra-abdominal
source of infection or malignancy. The clinical presentation of SBP is variable. The condition may manifest as a
relatively insidious colonization, without signs and symptoms, or may suddenly occur as a septic syndrome.
Laboratory diagnostics play a pivotal role for timely and appropriate management of patients with bacterial peritonitis. It is now clearly established that polymorphonuclear leukocyte (PMN) in peritoneal uid is the mainstay
for the diagnosis, whereas the role of additional biochemical tests is rather controversial. Recent evidence also
suggests that automatic cell counting in peritoneal uid may be a reliable approach for early screening of patients.
According to available clinical and laboratory data, we have developed a tentative algorithm for efcient diagnosis of SBP, which is based on a reasonable integration between optimization of human/economical resources and
gradually increasing use of invasive and expensive testing. The proposed strategy entails, in sequential steps,
serum procalcitonin testing, automated cell count in peritoneal uid, manual cell count in peritoneal uid,
peritoneal uid culture and bacterial DNA testing in peritoneal uid.
2014 Elsevier B.V. All rights reserved.
Contents
1.
Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
1.1.
Primary peritonitis or spontaneous bacterial peritonitis . . . . . . . .
2.
Clinical signs and symptoms . . . . . . . . . . . . . . . . . . . . . . . .
3.
Complications and prognosis . . . . . . . . . . . . . . . . . . . . . . .
4.
Treatment . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
5.
State-of-the-art of laboratory diagnostics of spontaneous bacterial peritonitis
5.1.
Macroscopic and microscopic examination of peritoneal uid . . . . .
5.2.
Biochemical analysis of peritoneal uid . . . . . . . . . . . . . . .
5.3.
Microbiological analysis of peritoneal uid . . . . . . . . . . . . . .
6.
Future perspectives in laboratory diagnostics of peritoneal uid . . . . . . . .
7.
Conclusions . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
1. Introduction
The peritoneum is the serous membrane that forms the lining of
abdominal cavity, covers and supports most of intra-abdominal organs,
Corresponding author at: U.O. Diagnostica Ematochimica, Azienda OspedalieroUniversitaria di Parma, Via Gramsci, 14, 43126 Parma, Italy. Tel.: +39 0521 703050,
+39 0521 703791.
E-mail addresses: glippi@ao.pr.it, ulippi@tin.it (G. Lippi).
0009-8981/$ see front matter 2014 Elsevier B.V. All rights reserved.
http://dx.doi.org/10.1016/j.cca.2014.01.023
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
164
165
165
165
166
166
166
167
167
168
168
169
and also serves as a conduit for their blood and lymph vessels and
nerves. From a biological perspective, the peritoneal membrane is
a sterile, semi-permeable membrane with multiple pores, which
allows a ux of solutes and water from the vascular system to the peritoneal cavity and vice versa, mainly through a diffusion mechanism [1].
The term peritonitis designates an inammatory process involving
the peritoneum. Although peritonitis may be occasionally sterile
(e.g., due to chloridric acid or to bile salts), the most frequent cause
is represented by infections. Bacterial peritonitis (BP) is hence
G. Lippi et al. / Clinica Chimica Acta 430 (2014) 164170
dened as an inammation of the serous membrane that covers the
viscera and the peritoneal cavity due to bacterial contamination. It
is conventionally classied as (i) primary, or spontaneous BP (SBP),
when a bacterial infection spreads to the peritoneum across the gut
wall or mesenteric lymphatics or less frequently from hematogenous transmission in combination with an impaired immune system
and in absence of an identied intra-abdominal source of infection or
malignancy; (ii) secondary BP, when the infection is a consequence
of a gastro-intestinal perforation; and (iii) tertiary or recurrent BP,
dened as persistence or recurrence of intraabdominal infection in
the presence of apparently appropriate therapy [1,2]. The most important infective agents involved in different types of peritonitis
are reported in Table 1. Due to the remarkable differences existing
in clinical signicance and management of the aforementioned
forms of BP (i.e., the secondary and tertiary forms of PB are mainly of
surgical competence), this article is focused on clinical and laboratory
diagnostics of SBP.
1.1. Primary peritonitis or spontaneous bacterial peritonitis
SBP, rstly described in 1971 by Conn and Fessel [3], is the infection
of a previously sterile ascitic uid that frequently represents a complication of liver cirrhosis. It affects about one third of cirrhotic patients [4,5],
in absence of visceral perforations or other intra-abdominal infections,
as abscess, acute pancreatitis or cholecystitis [6,7]. SBP is characterized
by poor outcome and high mortality, ranging from 10 to 50% at the
rst in-hospital episode [810]. Bacterascites, which is instead dened
as the presence of a positive culture of ascitic uid without an increased
peritoneal leukocyte count, has a much lower prevalence, ranging from
2 to 3% in outpatients, but reaching 11% in hospitalized patients [5].
Portal hypertension, changes in intestinal ora and impaired immunity, typically involving cirrhotic patients, are the main causes of bacterial overgrowth and translocation from the intestinal lumen to
mesenteric lymph nodes or other extraintestinal organs and sites
[6,1113]. Changes in intestinal ora and bacterial overgrowth are
represented mainly by the increased growth of Gram-negative aerobic
bacilli from Enterobacteriaceae family (such as Escherichia coli and
Klebsiella spp.) [1416], due to failure of intestinal clearance [17], and
in association with impaired small-bowel motility and decreased
intraluminal concentration of bile salts [18,19]. Only a limited number
of intestinal bacteria can efciently translocate from the lumen of the
gut into mesenteric lymph nodes, and these include E. coli, Klebsiella
pneumoniae and other Enterobacteriaceae [2022].
Gram-positive bacteria are typically involved in 2340% of SBP and
comprise Streptococci and (less often) Staphylococci, whereas anaerobic
165
bacteria (e.g., Bacteroides, Clostridia, Lactobacillus) are more frequently
isolated from multiple organisms SBP [23]. Listeria monocytogenes has
been only occasionally identied in cases of SBP [24,25]. The third factor
predisposing to SBP in cirrhotic patients is the impaired immunity,
which is characterized by reticuloendothelial system depression, leukocyte dysfunction, and altered ascitic uid defenses [8,16].
2. Clinical signs and symptoms
Since infections in the peritoneum can be generalized or localized,
the signs and symptoms of peritonitis are then highly variable. In a
classical secondary peritonitis, these include swelling, bloating and tenderness in the abdomen. The pain may vary from dull aches to severe,
localized or diffuse, sharp pain, and is frequently accompanied by
fever (many of patients have a temperature that exceeds 38 C,
although patients with severe sepsis may become hypothermic) and
chills, loss of appetite, thirst, nausea and vomiting [2628]. Abdominal
pain is more intense with motion or touch and is often lessened when
patients take a fetal position [29]. Obstruction to gas or stool, oliguria,
low blood pressure and tachycardia may occur in the most severe
forms of generalized peritonitis.
The clinical presentation of SBP is highly variable and this condition
may manifest as a relatively insidious colonization without signs and
symptoms or it can rapidly develop as a septic syndrome [6,30].
Since suggestive symptoms and signs are frequently absent in patients
with SBP, the available guidelines suggest a diagnostic paracentesis
in all ascitic patients admitted to the hospital [5,3133]. Very rarely,
hepatic encephalopathy may be the only manifestation of SBP. Also in
tertiary peritonitis the presenting symptoms are nonspecic and insidious in onset (e.g., low-grade fever, anorexia, weight loss) [26].
3. Complications and prognosis
Despite remarkable developments in earlier detection, medical and
surgical therapy, the average mortality rate of SBP remains elevated,
approaching 30% [34,35], and ranging from b 5% in low-risk patients to
approximately 90% in those at higher risk. Most information on the predictive factors associated with poor outcome comes from studies carried
out in cirrhotic patients with SBP. In this setting well recognized indicators of mortality include advanced age [36], child score N2, the presence
of bacteremia [37], lack of infection resolution, modication of antibiotic
treatment and culture positivity [9,38], nosocomial origin [39], and the
presence of CARD15/NOD2 (nucleotide-binding oligomerization
domain-containing protein 2/caspase recruitment domain-containing
protein 15) gene variants [40], along with increased concentrations of
Table 1
The most important infective agents involved in different types of peritonitis.
Aerobic
Spontaneous bacterial peritonitis
Secondary peritonitis
Tertiary peritonitis
Gram-negative
Escherichia coli
Klebsiella
Gram-negative
Escherichia coli
Enterobacter
Klebsiella
Proteus
Fusobacterium sp.
Pseudomonas aeruginosa
Chlamydia trachomatis
Gram-positive
Streptococci
Enterococci
Staphylococci
Listeria monocytogenes
Bacteroides (B. fragilis)
Eubacteria
Clostridia
Peptostreptococci
Peptococci
Gram-negative
Pseudomonas aeruginosa
Enterobacter
Gram-positive
Streptococci
Staphylococci
Listeria monocytogenes
Anaerobic
Fungi
Bacteroides
Clostridia
Lactobacilli
Gram-positive
Enterococci
Staphylococcus
Candida
166
G. Lippi et al. / Clinica Chimica Acta 430 (2014) 164170
serum bilirubin and creatinine. In these patients, approximately half of
all deaths occur after resolution of infection and are consequent to development of complications such as upper gastrointestinal bleeding,
renal dysfunction, hepatic encephalopathy and paralytic ileus. Among
these complications, renal impairment is probably the strongest
independent predictor of mortality and occurs as a result of a decreased
arterial blood volume, mediated by vasoactive cytokines, with a resultant increased reninangiotensinaldosterone system activation [41].
In a study by Follo et al. [42], the mortality rate in 252 consecutive episodes of SBP was 100% when associated with progressive renal impairment, 31% when associated with steady renal impairment, and only 7%
in patients with preserved renal function.
The stronger predictors of poor outcome both in SBP and secondary
BP patients include the concurrent development of sepsis and subsequent multiple organ failure (MOF). Sepsis is a complex, multifactorial,
evolutive syndrome, which may progress to conditions of varying severity. Several studies have described an increased risk of death along with
transition from sepsis to severe sepsis and septic shock [43]. In the
context of BP, severe sepsis represents the virtual threshold separating
stable from critical conditions. When improperly treated, sepsis may
cause functional impairment of one or more organs or systems and
nally lead to MOF [44]. Strong correlations between mortality rates
and number of failing organs have been described in the literature
[45]. It is also noteworthy that several scoring systems have been developed to assess the clinical prognosis of patients with BP in the past
decades. The most widely used include the APACHE-II score [46],
the simplied Acute Physiology Score (SAPS)-II [47], the Mannheim
Peritonitis Index (MPI) [48], the Multiple Organ Dysfunction Score
(MODS) [49], and the Sepsis-related Organ Failure Assessment (SOFA)
score [50]. Most of these scores are based on host criteria, systemic
signs of sepsis, and complications related to organ failure. Although
valuable for comparing patient cohorts and institutions, these scores
have limited signicance in the specic, day-to-day clinical decisionmaking process for each individual patient.
4. Treatment
The current approach to BP is multidisciplinary, includes medical
and/or surgical interventions, and mainly consists of timely hemodynamic resuscitation, empirical antimicrobial therapy and source control
measures [51]. Empirical antibiotic therapy should be initiated immediately after the diagnosis of BP, or once infection is considered likely, but
should never be delayed for obtaining results of radiographic or microbiological examinations. Systemic antibiotics are administered on the
knowledge of the probable composition of the infecting ora. When
the source of contamination is unknown, coverage is usually directed
against aerobic Gram-negative organisms and anaerobes [52]. The optimal duration of antibiotic therapy must be individualized and is guided
by the underlying pathology, severity of infection, speed and effectiveness of source control, and patient response to therapy.
An appropriate source control procedure is then compulsory
for nearly all patients with intra-abdominal infection(s) and entails
physical measures undertaken to drain infected foci and modify factors
in the infectious milieu that promote microbial growth or impair host
antimicrobial defenses [53].
5. State-of-the-art of laboratory diagnostics of spontaneous
bacterial peritonitis
Due to the adverse prognosis when SBP is left untreated, the diagnosis
of disease and the identication of the underlying cause should be performed as soon as possible. As mentioned, the therapy should not be delayed until the nal diagnosis is available. Since clinical characteristics and
physician assessment are usually insufcient for establishing a certain diagnosis or for excluding SBP [54], diagnostic paracentesis with appropriate ascitic uid analysis is virtually unavoidable for a timely and accurate
diagnosis of disease, for the differential diagnosis with other conditions
that may cause ascites, and for the subsequent patient management.
5.1. Macroscopic and microscopic examination of peritoneal uid
The analysis of ascitic uid encompasses both macroscopic and microscopic examination. The macroscopic examination is aimed to dene
color (which varies from white, yellow, green, red, brown and black)
and clarity (the peritoneal uid typically ranges from clear, cloudy, or
opalescent), although the presence of abnormal ndings (i.e., haziness,
cloudiness, or bloody appearance) has a very poor sensitivity for both
diagnosing and ruling out SBP [55].
It is now universally agreed that laboratory diagnostics of SBP should
be essentially based on leukocyte count and leukocyte differential in the
ascitic uid [5]. More specically, the polymorphonuclear leukocyte
(PMN) count is the mainstay for differentiating SBP from other causes
of ascites. Some diagnostic thresholds of PMN count have been proposed, which are characterized by different values of diagnostic sensitivity and specicity. Indeed, the cut-off of 250 PMN/L is associated
with optimal sensitivity whereas, and rather understandably, higher
thresholds (e.g., 500 PMN/L) provide a much better specicity that is
however counterbalanced by a lower sensitivity. General consensus
has now been reached on the choice of the 250 PMN/L cut-off, since
this threshold would reduce the number of false negative cases [5]. It
is noteworthy, however, that even this lower cut-off may be occasionally associated with suboptimal diagnostic sensitivity. Campillo et al. performed leukocyte and PMN counts in ascitic uids from patients with
SBP [56] and found different values according to the type of infecting
bacteria. In particular, the mean PMN count in patients with peritonitis due to Staphylococcus was below the 250 PMN/mm3 threshold
(i.e., 87 200 PMN/L) and was also substantially lower than that
of patients with SBP due to other etiologies such as Staphylococcus
(650 1359 PMN/mm 3), Enterococcus (771 1686 PMN/L) or
Enterobacteriaceae (3275 8342 PMN/L). Gonzlez-Navajas et al.
also found that the percentage of PMN in ascites was substantially
lower in patients with SBP due to Gram-positive bacteria than in
those with SBP due to Gram-negative bacteria (5.3 9.2 versus
46.0 28.7%; p = 0.01) [57]. For an appropriate estimation of
PMNs, it has also been suggested that subtraction of one leukocyte per
250 red blood cells should be made to adjust for potential presence of
contaminating blood in patients with hemorrhagic ascites (i.e., with a
red blood cell count N 10 000/L).
According to the current Clinical and Laboratory Standards Institute
(CLSI) recommendations, nucleated cell count and differential should
be performed in EDTA-anticoagulated ascitic uid by means of manual
microscopy, using the same hemocytometer chamber, and after preferential staining with May-GrunwaldGiemsa [58,59]. Cytocentrifugation,
with approximately 20-fold concentration of cells, is advisable because
this minimizes cell distortion and produces a uniform monolayer of cellular elements [59]. When the specimen is excessively bloody or the nucleated cell count is markedly increased, the uid should be diluted
using isotonic saline or other appropriate uids. Although result
reporting varies widely across different laboratories, it is now accepted
that the number of nucleated cell elements may be expressed in SI
(i.e., 109/L for nucleated cell elements and 1012/L for erythrocytes)
or conventional units (i.e., cells/L) [58].
Despite optical microscopy has represented the cornerstone of ascitic
uid analysis for decades, novel opportunities have recently emerged.
Most clinical laboratories are now equipped with several types of hemocytometers and urine cytouorimeters which hold premises for the
analysis of other sample matrices such as cerebrospinal uid (CSF)
and pleural and peritoneal uids [58]. The leading drawbacks of automated ow cytometry for ascitic uid assessment are represented by
inappropriate classication of nucleated elements that may be present
in biological uids different from blood and urine (i.e., macrophages,
mesothelial cells, malignant cells and other less common elements
G. Lippi et al. / Clinica Chimica Acta 430 (2014) 164170
such as LE cells, ReedSternberg cells, mast cells and megakaryocytes),
along with the poor sensitivity for detecting pathological samples with
low cell counts, typically between 1 and 100 elements/L. On the other
hand, the use of automated instrumentation has a number of advantages compared to optical microscopy, which include fully automated
sample preparation, shortened turnaround time, less intra- and interobserver variability, major degree of standardization, and no need of
trained personnel for microscopic analysis. It is also understandable
that the use of hemocytometers and urine cytouorimeters requires
less stringent analytical criteria for the analysis of peritoneal uid
than for CSF, since the diagnostic thresholds are much higher in the
former case (e.g., 250 PMN/L in peritoneal uid versus 5 PMN/L in
CSF) [58]. It is hence not surprising that a number of studies have now
conrmed that several automated hemocytometers display high correlation with nucleated cell count by manual microscopy (e.g., correlation
coefcients comprised between 0.98 and 1.00) and very modest bias,
along with optimal agreement at SBP cut-off (from 96% to 99%)
[6062]. Similarly, recent evidence suggests that automated urine cell
analyzers also exhibit optimal performance at the conventional
diagnostic thresholds of SBP and may hence be considered a reliable
perspective for initial screening of patients [63,64].
Despite continuous evolution and improvement of instrument
software, hemocytometers and urine cytouorimeters have been specically designed for identifying (and distinguishing) nucleated cells
in blood and urine, so that their analytical performance for detecting
other cell types that may be present in pathological ascites is still unsatisfactory. Particular concern has been expressed about the risk of false
positive cases, wherein some nucleated cells may be counted as leukocytes. Moreover, not all blood and urine analyzers fulll the quality
criteria necessary for ascitic uid analysis, so manufacturers should provide a specic statement of intended use that clearly denes which
body uids have been cleared by a regulatory agency for testing [58].
Finally, the laboratory should identify the lower limits for nucleated
cell counting, below which the use of ow cytometry for the analysis
of biological uid may be unreliable. According to these limitations,
automated ow cytometry is not intended to completely replace microscopic cell counting and classication so far, but it represents a valuable
and suitable approach for initial screening of peritoneal uid in patients
with suspected SBP.
5.2. Biochemical analysis of peritoneal uid
Despite the value of cell count and differentiation in ascitic uid is
now undisputed, the role of biochemical testing is by far less certain
[65]. The biochemical tests that are conventionally performed in ascitic
uid include pH, glucose, lactate dehydrogenase (LDH) and lactate (and
corresponding arterial-ascitic gradients), although none of them has
been demonstrated to be sufciently sensitive or specic for identifying
SBP, due to the considerable overlap of values across the various forms
of peritonitis [66]. A specic algorithm however has been proposed by
Akriviadis and Runyon for differentiating secondary from SBP in
the setting of neutrocytic ascites, which include ascitic uid total
protein N10 g/L, ascitic glucose b 2.8 mmol/L (i.e., b50 mg/dL) or
LDH value greater than the upper limit of the reference range for
serum [67]. As regards ascitic glucose, although a decreased concentration has been reported in bacterial or tubercular peritonitis and
carcinomatosis, its value does not signicantly differ in the initial
phase of SBP from that of sterile peritoneal uid, so this measurement has an overall unsatisfactory sensitivity [68].
Although promising data has been published about the assessment
of leukocyte esterase in peritoneal uid, a systematic review where
the evidence of prospective clinical studies has been systematically analyzed showed that the diagnostic performance of leukocyte esterase
reagent strips varies widely, with a sensitivity comprised between
0.45 and 1.00 and a specicity comprised between 0.81 and 1.00, respectively [69]. Another more recent review of the literature concluded
167
that leukocyte esterase reagent strips are usually characterized by a
high negative predictive value (N0.95 in most studies), thus supporting
their use as a preliminary screening tool for diagnosis of SBP. Interestingly, Tllez-vila et al. recently performed a prospective study in 223
consecutive patients with ascites (49 of whom were nally diagnosed
with SBP) attending to an emergency department [70] and found that
sensitivity, specicity, negative predictive value and positive predictive
value for identifying SBP of two different leukocyte esterase reagent
strips were 0.800.78, 0.98 (for both), 0.900.91 and 0.94 (for both),
respectively. It was hence concluded that the use of leukocyte esterase
reagent strips may be a useful tool for the screening of SBP in emergency
settings.
The serum-ascites albumin gradient (SAAG), which is conventionally
dened as the difference between serum and peritoneal albumin concentration, has been proven as a reliable marker of portal hypertension, using
a diagnostic threshold of 11 g/L. However, its role in differentiating SBP
from secondary forms of disease is much more controversial [65].
According to the recent recommendations of the European Association for the Study of the Liver (EASL) [71], the ascitic total protein concentration should always be assessed because patients with protein
concentration b 15 g/L in ascitic uid have an increased risk of developing SBP (Level A1 recommendation), thus taking benet from preventive antibiotic treatment (Level A1 recommendation). This is
supported by evidence that ascitic uid proteins do not increase during
episodes of SBP, whereas patients with the lowest protein concentration
were found to be the most likely to develop peritoneal infection(s) [65].
Additional laboratory investigations, including amylase, C reactive
protein (CRP) and cytology should only be performed in cases when
the diagnosis is uncertain or in the suspicion of pancreatic disease,
cancer or tuberculosis [71].
5.3. Microbiological analysis of peritoneal uid
In general, the large majority of ascitic uid infections are spontaneous in nature, monomicrobial and characterized by low-colony-count
[72]. According to current recommendations, Gram staining is rarely
helpful for diagnosing SBP and for the accurate identication of pathogens, due to the low number of bacteria that are typically found in the
infected uid (i.e., usually b1 bacterium/mL). In particular, Chinnock
et al. retrospectively reviewed all peritoneal uid analyses performed
in an urban 3-hospital system [73] and reported that Gram stain had a
sensitivity of 0.10 and a specicity of 0.97 for detecting SBP. Similarly,
the classical culture techniques are not effective to demonstrated bacterial growth in up to two-third cases of SBP [5]. Conversely, it is currently
recommended that inoculation of ascitic uid (10 mL) in blood culture
bottles for both aerobic and anaerobic culture should be performed at
bedside in all patients with suspected SBP (i.e., bacterial growth can
be detected in up to 90% of cases when inoculation is performed at the
bedside as compared with only 40% to 60% with conventional culture)
[5,71]. The use of non-radiometric systems (e.g., colorimetric
BacTec) has also remarkably improved the time to diagnosis, since
these techniques are much faster than using conventional blood culture bottles [5]. Even inoculation of ascitic uid into blood culture
bottles is, however, not foolproof. Culture-negative neutrocytic ascites
(i.e., negative results of ascitic uid culture associated with a PMN
count of 250 cells/L) may be encountered in up to 50% of patients
with SBP [74], and this may be due to a variety of reasons. First, inappropriate preanalytical procedures (e.g. contamination or transportation
delays) as well as poor culturing techniques may impair bacterial
growth, thus generating false negative results. As mentioned, empirical
antibiotic therapy must be initiated immediately after the diagnosis of
SBP even without results of ascitic uid culture according to current
practice [5,71], so that the possibility of a false negative bacterial culture
should always be considered in patients receiving antibiotics at the time
of paracentesis. False negative results of ascitic uid culture may also be
observed in patients with late-stage resolving infections.
168
G. Lippi et al. / Clinica Chimica Acta 430 (2014) 164170
As regards nucleic acid amplication tests, a recent prospective
study including 102 consecutive patients with ascites reported a rather
poor sensitivity of this analysis for detecting SBP (i.e., bacterial DNA
could not be detected in approximately half of patients with culturenegative SBP) [75]. Controversial results were provided in separate
investigations [7678], which are mainly attributable to differences in
analytical sensitivity of various DNA extraction methods and in the
sequence of primers. Therefore, nucleic acid amplication can only be
considered as a complement, and not a substitute, of conventional
culture methods.
6. Future perspectives in laboratory diagnostics of peritoneal uid
Interesting evidence is emerging from the measurement of
procalcitonin (PCT) in serum of patients with SBP. Su et al. performed
a literature search to identify original studies that reported the diagnostic performance of PCT alone or in combination with other biomarkers
for the diagnosis of SBP [79]. The following meta-analysis showed
that serum PCT (cut-offs comprised between 0.58 and 0.75 ng/mL)
displayed a high accuracy for diagnosis of SBP, with a pooled area
under the curve (AUC) value of 0.95 (95% condence interval [95% CI],
0.820.99), a sensitivity of 0.86 (95% CI, 0.730.94), and a specicity of
0.80 (95% CI, 0.720.87). In two out of three studies included in the
meta-analysis, the sensitivity of PCT was 0.95, whereas it was 0.50 in
the remaining investigation that used a higher cut-off for supporting a
high diagnostic specicity. Even more interestingly, the positive likelihood ratio of 7.73 (95% CI, 0.9165.64) was considered to be sufciently
high for using PCT as a diagnostic test, whereas the low negative likelihood ratio (0.14; 95% CI, 0.011.89) was deemed suitable to suggest discontinuation of antibiotics therapy in combination with a negative
culture. The concentration of PCT in serum or plasma was also found
to be a better marker than CRP or Interelukin-6 for distinguishing SBP
from other causes of ascites. These results were then conrmed in two
subsequent investigations. Cekin et al. measured serum PCT and CRP
levels in 101 patients with ascites (20% of whom with infectious peritonitis) [80]. Using receiver characteristic curve (ROC) analysis,
procalcitonin (cut-off b 0.61 ng/mL) displayed an AUC of 0.98 for
diagnosing SBP. In a recent study on 84 patients with chronic severe
hepatitis B, 42 of whom with SBP, Yuan et al. reported a good diagnostic performance for both PCT (cut-off, 0.48 ng/mL; AUC, 0.89;
95% CI, 0.810.96) and CRP (cut-off, 16.15 mg/L; AUC, 0.86; 95%
CI, 0.780.94) for the identication of SBP [81]. The sensitivity and
specicity of serum PCT were 0.95 and 0.79, respectively.
Neutrophil gelatinase-associated lipocalin (NGAL) belongs to the
family of lipocalins and mainly acts as an endogenous bacteriostatic
agent that interferes with siderophore-mediated iron acquisition. The
leading endogenous sources of this protein include activated neutrophils, tubular cell of the kidney, cardiomyocytes, and epithelia of the
prostate, uterus, salivary glands, lung, liver, trachea, stomach, bowel
and colon [82]. NGAL mainly exists as a monomeric form (which is prevalently synthesized by tubular cells), along with a homodimeric form
(which is mainly released by activated neutrophils) and a heterodimeric
form, bound to matrix metalloproteinase 9 (MMP-9), which is also
prevalently present in the kidney. Owing to the fact that the current
commercial immunoassays for measuring NGAL do not distinguish
one molecular species from the others [83], and that the protein is actively released by PMN, some recent studies have assessed the potential
usefulness of NGAL for diagnosing SBP. Axelsson et al. rst described a
10-fold increase of NGAL plasma levels in patients with acute peritonitis
[84]. Leung et al. measured NGAL concentration in peritoneal dialysate
efuent in patients with continuous ambulatory peritoneal dialysisrelated peritonitis and found that the concentration of this biomarker
was higher in patients with Gram-positive or Gram-negative peritonitis
than in those with culture-negative peritonitis [85]. In a following investigation, Martino et al. observed a remarkable increased concentration
of NGAL in the peritoneal uid of dialysis patients with SBP and found
that NGAL assessment in peritoneal uid had an AUC of 0.99 [86].
Lippi et al. also measured NGAL and LDH in 111 peritoneal uids, 23%
of which from patients with SBP [87], and found an AUC of 0.88 for
LDH, 0.89 for NGAL and 0.94 for their combination (both tests positive)
for identifying bacterial infections. The sensitivity was 0.81 for LDH, 0.96
for NGAL (cut-off of 120 ng/mL) and 0.80 for their combination, whereas the specicity was 0.87 for LDH, 0.75 for NGAL and 0.95 for their combination. Interestingly, the diagnostic performance of total proteins
(AUC, 0.80) and glucose (AUC, 0.71) in peritoneal uid was consistently
worse than that of LDH, NGAL, or their combination. More recently,
Lacquaniti et al. studied 30 patients with peritonitis and 30 patients undergoing continuous ambulatory peritoneal dialysis (CAPD) [88] and reported that NGAL levels in peritoneal uid were higher compared with
baseline values at the onset of peritonitis and, even more importantly,
that the assessment of this biomarker in peritoneal uid showed a good
diagnostic performance for identifying treatment failure. Interestingly, it
has also recently been reported that the concentration of NGAL in CSFs
displayed an AUC of 0.94 (95% CI, 0.89 to 0.99) for identifying acute bacterial meningitis, with a sensitivity of 1.00 and a specicity of 0.74 at a diagnostic threshold of 13 ng/mL [89]. Taken together, this clinical evidence
suggests that NGAL in peritoneal uid may be regarded as a putative biomarker for rapid screening of patients with suspected SBP and, possibly,
for monitoring effectiveness of treatment. Further and larger studies are
needed, however, to conrm these preliminary ndings.
Additional and appareling perspectives emerge from two recent
proteomic studies. Tyan et al. performed 2-dimensional gel electrophoresis (2DE) coupled with reverse phase nano-high performance liquid
chromatography electrospray ionization tandem mass spectrometry
(RP-nano-HPLCESI-MS/MS) followed by peptide fragmentation pattern in the peritoneal dialysate of 12 patients before and after peritonitis
[90] and detected as many as 350 signicant spots. After excluding
proteins that were ultraltered from circulation, ten putative proteins
were identied as being differentially expressed (i.e., N2-fold or 50%) before and after peritonitis. More specically, downregulation was found
for apolipoprotein A-I, heat shock 70 kDa protein 1A/1B, interalphatrypsin inhibitor heavy chain H4, brinogen gamma and beta
chains, ceruloplasmin, zinc--2-glycoprotein, and -1-antitrypsin,
whereas up-regulation was observed for haptoglobin and antithrombin.
An altered plasma proteome has also been found by Thongboonkerd
et al. in plasma of pigs before and 12 h after peritonitis-induced sepsis
[91]. After resolution by 2DE and staining with SYPRO Ruby uorescence
dye, 36 spots were found to be signicantly modied in plasma. Subsequent analysis with quadrupole-time-of-ight (Q-TOF) MS and MS/MS
allowed the identication of 22 proteins which were up-regulated in
sepsis and ve proteins which were instead down-regulated.
7. Conclusions
Despite the vast array of potential analyses (Table 2), the current
laboratory diagnostics of SBP entail a limited number of conventional
investigations, which basically include PMN count in peritoneal uid
and peritoneal uid culture. However, some emerging tests may provide a signicant contribution to the diagnosis and therapeutic management of this disorder. These basically include serum procalcitonin, along
with assessment of NGAL and bacterial DNA in peritoneal uid. The use
of leukocyte esterase reagent strips is another appealing opportunity for
those healthcare settings where timely diagnosis is pivotal and conventional laboratory resources are not easily available (e.g., the emergency
department).
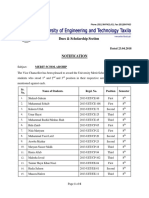
According to clinical and analytical evidence available so far, it seems
hence reasonable to suggest a tentative algorithm for rapid and efcient
diagnosis of SBP, which is based on a reasonable integration between
optimization of human/economical resources and the gradually increasing use of invasive and expensive testing (Fig. 1). Owing to the high
sensitivity, which has been reported to be approximately 0.95 using a
diagnostic threshold of 0.5 ng/mL or higher, serum PCT may help to
G. Lippi et al. / Clinica Chimica Acta 430 (2014) 164170
Table 2
Spectrum of laboratory tests for diagnosis and differential diagnosis of spontaneous
bacterial peritonitis (SBP).
Peritoneal uid analysis
1) Macroscopic and microscopic examination
a) Color and clarity
b) Leukocyte count and differential
2) Biochemical analysis
a) pH
b) Glucose
c) Lactic acid
d) Lactate dehydrogenase (LDH)
e) Leukocyte esterase
f) Total protein
g) (Serum)-ascites albumin gradient
2) Microbiological analysis
a) Gram staining
b) Peritoneal uid culture
c) Nucleic acid amplication
Serum or plasma analysis
1) Procalcitonin
2) Neutrophil gelatinase-associated lipocalin (NGAL)
3) Amylase
4) C reactive protein
Suspected SBP
Serum Procalcitonin
NO SBP
PMN <250/L
>5.0 ng/mL
Paracentesis
Automated cell count
PNM >250/L
NO SBP
PMN <250/L
Manual cell count
PMN >250/L
NO SBP
Negative
Empiric antibiotic
therapy
Peritoneal fluid culture
Positive
Nucleic acids amplification
Specific antibiotic
therapy
Negative
Positive
Consider non-bacterial
etiology
is b250 cells/L, SBP can be safely ruled out as for current guidelines,
due to the optimal agreement with optical microscopy. Owing to the
modest but still clinically meaningful number of false positive cases,
a peritoneal uid PMN value N 250 cells/L should be further conrmed with microscopic cell count. The presence of SBP may hence
be excluded when the manual PMN count is b 250 cells/L, whereas
empiric antibiotic therapy, accompanied with peritoneal uid culture,
should be immediately started when the PMN count exceeds this
threshold. In the presence of bacterial growth, targeted antibiotic therapy should be established, whereas nucleic acid amplication may be
advisable in the case of negative peritoneal uid culture. Identication
of bacterial DNA would then allow diagnosing neutrocytic ascites and
starting targeted antibiotic therapy, whereas non-bacterial etiologies
should be considered in the case of negative nucleic acid amplication.
Indeed, this diagnostic algorithm is aimed to integrate but not replace
existing guidelines and represents an innovative approach to be further
tested in large prospective studies and cost-effective analyses.
References
timely rule out SBP in those patients with concentration of this biomarker below the diagnostic cut-off. When serum PCT concentration
is N0.5 ng/mL, paracentesis should be performed and followed by
automated cell count in peritoneal uid. When the PMN count
<0.5 ng/mL
169
Neutrocytic
ascites
Fig. 1. Tentative algorithm for rapid and efcient diagnosis of spontaneous bacterial
peritonitis (SBP).
[1] Heemken R, Gandawidjaja L, Hau T. Peritonitis: pathophysiology and local defense
mechanisms. Hepatogastroenterology 1997;44:92736.
[2] Nathens AB, Rotstein OD, Marshall JC. Tertiary peritonitis: clinical features of a
complex nosocomial infection. World J Surg 1998;22:15863.
[3] Conn HO, Fessel JM. Spontaneous bacterial peritonitis in cirrhosis: variations on a
theme. Medicine 1971;50:16197.
[4] Sort P, Navasa M, Arroyo V, et al. Effect of intravenous albumin on renal impairment
and mortality in patients with cirrhosis and spontaneous bacterial peritonitis. N Engl
J Med 1999;341:4039.
[5] Wiest R, Krag A, Gerbes A. Spontaneous bacterial peritonitis: recent guidelines and
beyond. Gut 2012;61:297310.
[6] Bernardi M. Spontaneous bacterial peritonitis: from pathophysiology to prevention.
Intern Emerg Med 2010;5(Suppl. 1):S3744.
[7] Cruntu FA, Benea L. Spontaneous bacterial peritonitis: pathogenesis, diagnosis,
treatment. J Gastrointestin Liver Dis 2006;15:516.
[8] Parsi MA, Atreja A, Zein NN. Spontaneous bacterial peritonitis: recent data on
incidence and treatment. Cleve Clin J Med 2004;71:56976.
[9] Toledo C, Salmeron JM, Rimola A, et al. Spontaneous bacterial peritonitis in cirrhosis:
predictive factors of infection resolution and survival in patients treated with
cefotaxime. Hepatology 1993;17:251e7.
[10] Garcia-Tsao G. Current management of the complications of cirrhosis and portal
hypertension: variceal hemorrhage, ascites, and spontaneous bacterial peritonitis.
Gastroenterology 2001;120:72648.
[11] Garcia-Tsao G, Wiest R. Gut microora in the pathogenesis of the complications of
cirrhosis. Best Pract Res Clin Gastroenterol 2004;18:35372.
[12] Guarner C, Soriano G. Bacterial translocation and its consequences in patients with
cirrhosis. Eur J Gastroenterol Hepatol 2005;17:2731.
[13] Tripathi D, Hayes PC. Beta-blockers in portal hypertension: new developments and
controversies. Liver Int Oct 17 2013. http://dx.doi.org/10.1111/liv.12360 [Epub
ahead of print].
[14] Navasa M, Rods J. Bacterial infections in cirrhosis. Liver Int 2004;24:27780.
[15] Strauss E, Caly WR. Spontaneous bacterial peritonitis: a therapeutic update. Expert
Rev Anti Infect Ther 2006;4:24960.
[16] Riordan SM, Williams R. The intestinal ora and bacterial infection in cirrhosis. J
Hepatol 2006;45:74457.
[17] Husebye E. The pathogenesis of gastrointestinal bacterial overgrowth. Chemotherapy
2005;51(Suppl. 1):122.
[18] Pardo A, Bartoli R, Lorenzo-Zuniga V, et al. Effect of cisapride on intestinal bacterial
overgrowth and bacterial translocation in cirrhosis. Hepatology 2001;31:85863.
[19] Slocum MM, Sittig KM, Specian RD, et al. Absence of intestinal bile promotes
bacterial translocation. Am Surg 1992;58:30510.
[20] Wells CL. Relationship between intestinal microecology and the translocation of
intestinal bacteria. Antonie Van Leeuwenhoek 1990;58:8793.
[21] Wiest R, Garcia-Tsao G. Bacterial translocation (BT) in cirrhosis. Hepatology
2005;41:42233.
[22] Eaves-Pyles T, Alexander JW. Comparison of translocation of different types of
microorganisms from the intestinal tract of burned mice. Shock 2001;16:14852.
[23] Llovet JM, Planas R, Morillas R, et al. Short-term prognosis of cirrhotics with
spontaneous bacterial peritonitis: multivariate study. Am J Gastroenterol
1993;88:38892.
[24] Liatsos GD, Thanellas S, Pirounaki M, Ketikoglou I, Moulakakis A. Listeria monocytogenes
peritonitis: presentation, clinical features, treatment, and outcome. Scand J
Gastroenterol 2012;47:112940.
[25] Cardoso C, Cremers I, Oliveira AP. Spontaneous bacterial peritonitis caused by Listeria
monocytogenes: a case report and literature review. Ann Hepatol 2012;11:9557.
[26] Johnson CC, Baldessarre J, Levison ME, et al. Peritonitis: update on pathophysiology,
clinical manifestations, and management. Clin Infect Dis 1997;24:103545.
[27] Wittmann DH, Shein M, Condon RE, et al. Management of secondary peritonitis. Ann
Surg 1996;224:108.
170
G. Lippi et al. / Clinica Chimica Acta 430 (2014) 164170
[28] Laroche M, Harding G. Primary and secondary peritonitis: an update. Eur J Clin
Microbiol Infect Dis 1998;17:54250.
[29] Martin RF, Rossi RL. The acute abdomen. An overview and algorithms. Surg Clin
North Am 1997;77:122743.
[30] Alaniz C, Regal RE. Spontaneous bacterial peritonitis: a review of treatment options.
P T 2009;34:20410.
[31] Runyon BA. Management of adult patients with ascites due to cirrhosis: an update.
Hepatology 2009;49:2087107.
[32] Rimola A, Garcia-Tsao G, Navasa M, et al. Diagnosis, treatment and prophylaxis of
spontaneous bacterial peritonitis: a consensus document. International Ascites
Club. J Hepatol 2000;32:14253.
[33] Garcia-Tsao G. Bacterial infections in cirrhosis: treatment and prophylaxis. J Hepatol
2005;42(Suppl. 1):S8592.
[34] Nobre SR, Cabral JE, Gomes JJ, Leito MC. In-hospital mortality in spontaneous bacterial
peritonitis: a new predictive model. Eur J Gastroenterol Hepatol 2008;20:117681.
[35] Lamme B, Boermeester MA, Belt EJ, Van Till JWO, Gouma DJ, Obertop H. Mortality
and morbidity of planned relaparotomy versus relaparotomy on demand for
secondary peritonitis. Br J Surg 2004;91:104654.
[36] Thuluvath PJ, Morss S, Thompson R. Spontaneous bacterial peritonitisin-hospital
mortality, predictors of survival, and health care costs from 1988 to 1998. Am J
Gastroenterol 2001;96:12326.
[37] Cho JH, Park KH, Kim SH, et al. Bacteremia is a prognostic factor for poor outcome in
spontaneous bacterial peritonitis. Scand J Infect Dis 2007;39:697e702.
[38] Umgelter A, Reindl W, Miedaner M, Schmid RM, Huber W. Failure of current antibiotic rst-line regimens and mortality in hospitalized patients with spontaneous
bacterial peritonitis. Infection 2009;37:28.
[39] Cheong HS, Kang CI, Lee JA, et al. Clinical signicance and outcome of nosocomial
acquisition of spontaneous bacterial peritonitis in patients with liver cirrhosis. Clin
Infect Dis 2009;48:1230e6.
[40] Appenrodt B, Grnhage F, Gentemann MG, Thyssen L, Sauerbruch T, Lammert F.
Nucleotide-binding oligomerization domain containing 2 (NOD2) variants are
genetic risk factors for death and spontaneous bacterial peritonitis in liver cirrhosis.
Hepatology 2010;51:1327e33.
[41] Navasa M, Follo A, Filella X, et al. Tumor necrosis factor and interleukin-6 in spontaneous bacterial peritonitis in cirrhosis: relationship with the development of renal
impairment and mortality. Hepatology 1998;27:122732.
[42] Follo A, Llovet JM, Navasa M, et al. Renal impairment after spontaneous bacterial
peritonitis in cirrhosis: incidence, clinical course, predictive factors, and prognosis.
Hepatology 1994;10:1495501.
[43] Levy MM, Fink MP, Marshall JC, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International
Sepsis Denitions Conference. Crit Care Med 2003;31:12506.
[44] Bone RC, Balk RA, Cerra FB, et al. American College of Chest Physicians/Society of
Critical Care Medicine Consensus Conference: denitions for sepsis and organ
failure and guidelines for the use of innovative therapies in sepsis. Chest
1992;101:164455.
[45] Beal AL, Cerra FB. Multiple organ failure syndrome in the 1990s: systemic inammatory response and organ dysfunction. JAMA 1994;271:22633.
[46] Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease
classication system. Crit Care Med 1985;13:81829.
[47] Gall Jr Le, Lemeshow S, Saulnier F. A new Simplied Acute Physiology Score
(SAPS II) based on a European/North American multicenter study. JAMA
1993;270:295763.
[48] Wacha H, Linder MM, Feldmann U, Wesch G, Gundlach E, Steifensand RA.
Mannheim Peritonitis Index prediction of risk of death from peritonitis:
construction of a statistical and validation of an empirically based index. Theor
Surg 1987:16977.
[49] Marshall JC, Cook DJ, Christou NV, Bernard GR, Sprung CL, Sibbald WJ. Multiple organ
dysfunction score: a reliable descriptor of a complex clinical outcome. Crit Care Med
1995;23:163852.
[50] Vincent JL, Moreno R, Takala J, et al. The SOFA (Sepsis-related Organ Failure
Assessment) score to describe organ dysfunction/failure. On behalf of the Working
Group on Sepsis-Related Problems of the European Society of Intensive Care
Medicine. Intensive Care Med 1996;22:70710.
[51] Solomkin JS, Mazuski JE, Bradley JS, et al. Diagnosis and management of complicated
intra-abdominal infection in adults and children: guidelines by the Surgical
Infection Society and the Infectious Diseases Society of America. Clin Infect Dis
2010;50:13364.
[52] Mazuski JE, Sawyer RG, Nathens AB, et al. The Surgical Infection Society guidelines
on antimicrobial therapy for intra-abdominal infections: an executive summary.
Surg Infect 2002;3:16173.
[53] Marshall JC, Maier RV, Jimenez M, Dellinger EP. Source control in the management
of severe sepsis and septic shock: an evidence-based review. Crit Care Med
2004;32(11 Suppl.):S51326.
[54] Chinnock B, Afarian H, Minnigan H, Butler J, Hendey GW. Physician clinical impression does not rule out spontaneous bacterial peritonitis in patients undergoing
emergency department paracentesis. Ann Emerg Med 2008;52:26873.
[55] Chinnock B, Hendey GW, Minnigan H, Butler J, Afarian H. Clinical impression and ascites appearance do not rule out bacterial peritonitis. J Emerg Med 2013;44:9039.
[56] Campillo B, Richardet JP, Kheo T, Dupeyron C. Nosocomial spontaneous bacterial
peritonitis and bacteremia in cirrhotic patients: impact of isolate type on prognosis
and characteristics of infection. Clin Infect Dis 2002;35:110.
[57] Gonzlez-Navajas JM, Bellot P, Francs R, et al. Presence of bacterial-DNA in cirrhosis
identies a subgroup of patients with marked inammatory response not related to
endotoxin. J Hepatol 2008;48:617.
[58] Clinical and Laboratory Standards Institute. Body uid analysis for cellular composition;
approved guideline. CLSI document H56-A; 2006 [Wayne, PA].
[59] Jones CS, Cornbleet PJ. WrightGiemsa cytology of body uids. Techniques for
optimal cytocentrifuge slide preparation. Lab Med 1997;28:7136.
[60] Lippi G, Cattabiani C, Benegiamo A, et al. Evaluation of white blood cell count in peritoneal uid with ve different hemocytometers. Clin Biochem 2013;46:1736.
[61] Lippi G, Cattabiani C, Benegiamo A, et al. Evaluation of the fully automated hematological analyzer Sysmex XE-5000 for ow cytometric analysis of peritoneal uid. J
Lab Autom 2013;18:2404.
[62] Danise P, Maconi M, Rovetti A, et al. Cell counting of body uids: comparison between three automated haematology analysers and the manual microscope method.
Int J Lab Hematol 2013;35:60813.
[63] Penders J, Fiers T, Dhondt AM, Claeys G, Delanghe JR. Automated ow cytometry
analysis of peritoneal dialysis uid. Nephrol Dial Transplant 2004;19:4638.
[64] Buoro S, Gustinetti R, Dominoni P, et al. Analytical evaluation of Sysmex UF-1000i for
ow cytometric analysis of peritoneal uid. Clin Biochem 2012;45:12635.
[65] Tarn AC, Lapworth R. Biochemical analysis of ascitic (peritoneal) uid: what should
we measure? Ann Clin Biochem 2010;47(Pt 5):397407.
[66] Runyon BA, Antillon MR. Ascitic uid pH and lactate: insensitive and nonspecic
tests in detecting ascitic uid infection. Hepatology 1991;13:92935.
[67] Runyon BA, Hoefs JC. Ascitic uid analysis in the differentiation of spontaneous
bacterial peritonitis from gastrointestinal tract perforation into ascitic uid. Hepatology
1984;4:44750.
[68] Akriviadis EA, Runyon BA. Utility of an algorithm in differentiating spontaneous
from secondary bacterial peritonitis. Gastroenterology 1990;98:12733.
[69] Koulaouzidis A, Leontiadis GI, Abdullah M, et al. Leucocyte esterase reagent strips
for the diagnosis of spontaneous bacterial peritonitis: a systematic review. Eur J
Gastroenterol Hepatol 2008;20:105560.
[70] Tllez-vila FI, Chvez-Tapia NC, Franco-Guzmn AM, Uribe M, Vargas-Vorackova F.
Rapid diagnosis of spontaneous bacterial peritonitis using leukocyte esterase
reagent strips in emergency department: Uri-Quick Clini-10SG vs. Multistix
10SG. Ann Hepatol 2012;11:6969.
[71] European Association for the Study of the Liver. EASL clinical practice guidelines on
the management of ascites, spontaneous bacterial peritonitis, and hepatorenal
syndrome in cirrhosis. J Hepatol 2010;53:397417.
[72] Runyon BA, Canawati HN, Akriviadis EA. Optimization of ascitic uid culture
technique. Gastroenterology 1988;95:13515.
[73] Chinnock B, Fox C, Hendey GW. Gram's stain of peritoneal uid is rarely helpful in
the evaluation of the ascites patient. Ann Emerg Med 2009;54:7882.
[74] Runyon BA. Monomicrobial nonneutrocytic bacterascites: a variant of spontaneous
bacterial peritonitis. Hepatology 1990;12:7105.
[75] Soriano G, Esparcia O, Montemayor M, et al. Bacterial DNA in the diagnosis of
spontaneous bacterial peritonitis. Aliment Pharmacol Ther 2011;33:27584.
[76] Vieira SM, da Silveira TR, Matte U, et al. Amplication of bacterial DNA does not
distinguish patients with ascitic uid infection from those colonized by bacteria. J
Pediatr Gastroenterol Nutr 2007;44:6037.
[77] Kim SH, Jeong HS, Kim YH, et al. Evaluation of DNA extraction methods and their
clinical application for direct detection of causative bacteria in continuous ambulatory
peritoneal dialysis culture uids from patients with peritonitis by using broad-range
PCR. Ann Lab Med 2012;32:11925.
[78] Hardick J, Won H, Jeng K, et al. Identication of bacterial pathogens in ascitic uids from
patients with suspected spontaneous bacterial peritonitis by use of broad-range PCR
(16S PCR) coupled with high-resolution melt analysis. J Clin Microbiol 2012;50:242832.
[79] Su DH, Zhuo C, Liao K, Cheng WB, Cheng H, Zhao XF. Value of serum procalcitonin
levels in predicting spontaneous bacterial peritonitis. Hepatogastroenterology
2013;60:6416.
[80] Cekin Y, Cekin AH, Duman A, Yilmaz U, Yesil B, Yolcular BO. The role of serum
procalcitonin levels in predicting ascitic uid infection in hospitalized cirrhotic
and non-cirrhotic patients. Int J Med Sci 2013;10:136774.
[81] Yuan LY, Ke ZQ, Wang M, Li Y. Procalcitonin and C-reactive protein in the diagnosis
and prediction of spontaneous bacterial peritonitis associated with chronic severe
hepatitis B. Ann Lab Med 2013;33:44954.
[82] Lippi G, Plebani M. Neutrophil gelatinase-associated lipocalin (NGAL): the laboratory perspective. Clin Chem Lab Med 2012;50:14837.
[83] Lippi G, Cervellin G. Neutrophil gelatinase-associated lipocalin: a more specic assay
is needed for diagnosing renal injury. Clin Chim Acta 2012;413:11601.
[84] Axelsson L, Bergenfeldt M, Ohlsson K. Studies of the release and turnover of a human
neutrophil lipocalin. Scand J Clin Lab Invest 1995;55:57788.
[85] Leung JC, Lam MF, Tang SC, et al. Roles of neutrophil gelatinase-associated lipocalin
in continuous ambulatory peritoneal dialysis-related peritonitis. J Clin Immunol
2009;29:36578.
[86] Martino FK, Filippi I, Giavarina D, et al. Neutrophil gelatinase-associated lipocalin in
the early diagnosis of peritonitis: the case of neutrophil gelatinase-associated
lipocalin. Contrib Nephrol 2012;178:25863.
[87] Lippi G, Calef A, Pipitone S, et al. Assessment of neutrophil gelatinase-associated
lipocalin and lactate dehydrogenase in peritoneal uids for the screening of bacterial
peritonitis. Clin Chim Acta 2013;418:5962.
[88] Lacquaniti A, Chirico V, Mondello S, et al. Neutrophil gelatinase-associated
lipocalin in peritoneal dialysis reects status of peritoneum. J Nephrol May
2013;26:11519.
[89] Lippi G, Avanzini P, Calzetti C, et al. The role of neutrophil gelatinase-associated
lipocalin (NGAL) in cerebrospinal uids for screening of acute bacterial meningitis.
Clin Lab 2014;60:xx-xx. http://dx.doi.org/10.7754/Clin.Lab.2013.121239.
[90] Tyan YC, Su SB, Ting SS, Wang HY, Liao PC. A comparative proteomics analysis of
peritoneal dialysate before and after the occurrence of peritonitis episode by mass
spectrometry. Clin Chim Acta 2013;420:3444.
[91] Thongboonkerd V, Chiangjong W, Mares J, et al. Altered plasma proteome during an
early phase of peritonitis-induced sepsis. Clin Sci (Lond) 2009;116:72130.
Vous aimerez peut-être aussi
- Female Urinary Tract Infections in Clinical PracticeD'EverandFemale Urinary Tract Infections in Clinical PracticeBob YangPas encore d'évaluation
- Peritonitis: Presentan: FAUZAN AKBAR YUSYAHADI - 12100118191Document21 pagesPeritonitis: Presentan: FAUZAN AKBAR YUSYAHADI - 12100118191Fauzan Fourro100% (1)
- Colitis: A Practical Approach to Colon and Ileum Biopsy InterpretationD'EverandColitis: A Practical Approach to Colon and Ileum Biopsy InterpretationAnne Jouret-MourinPas encore d'évaluation
- PeritonitisDocument5 pagesPeritonitisdnllkzaPas encore d'évaluation
- Urinary Tract Infection in Children - Classification, Diagnosis and TreatmentD'EverandUrinary Tract Infection in Children - Classification, Diagnosis and TreatmentPas encore d'évaluation
- Primary (Spontaneous) Bacterial Peritonitis Hal 808Document4 pagesPrimary (Spontaneous) Bacterial Peritonitis Hal 808aldilla amandaPas encore d'évaluation
- Laroche 1998Document9 pagesLaroche 1998takechi takechiPas encore d'évaluation
- Peritonitis Clinical UpdateDocument11 pagesPeritonitis Clinical Updatetika tikaPas encore d'évaluation
- Peritonitis and Abdominal Sepsis: Background, Anatomy, PathophysiologyDocument16 pagesPeritonitis and Abdominal Sepsis: Background, Anatomy, PathophysiologyTias SubagioPas encore d'évaluation
- Update on Peritonitis Pathophysiology and ManagementDocument11 pagesUpdate on Peritonitis Pathophysiology and ManagementGianna_OshinPas encore d'évaluation
- Peritonitis and Abdominal Sepsis Background, Anatomy, PathophysiologyDocument1 pagePeritonitis and Abdominal Sepsis Background, Anatomy, PathophysiologyFlora Eka HeinzendorfPas encore d'évaluation
- Peritonitis and Intra-Abdominal Abscess Diagnosis TreatmentDocument16 pagesPeritonitis and Intra-Abdominal Abscess Diagnosis TreatmentPekerja KesunyianPas encore d'évaluation
- Peritonitis EmedscapeDocument38 pagesPeritonitis EmedscapeNisrina FarihaPas encore d'évaluation
- PeritonitissDocument46 pagesPeritonitissNinaPas encore d'évaluation
- Homework 4Document28 pagesHomework 4Ryan Arifin SuryantoPas encore d'évaluation
- Jurnal 3Document6 pagesJurnal 3Rafiqa Zulfi UmmiahPas encore d'évaluation
- 18 Manuscript For PeritonitisDocument8 pages18 Manuscript For Peritonitiskint manlangitPas encore d'évaluation
- لقطة شاشة 2022-04-21 في 11.10.40 صDocument55 pagesلقطة شاشة 2022-04-21 في 11.10.40 صEngi KazangyPas encore d'évaluation
- Management of Secondary Peritonitis - Surgical Treatment - NCBI BookshelfDocument10 pagesManagement of Secondary Peritonitis - Surgical Treatment - NCBI Bookshelfrahmah.hayya00Pas encore d'évaluation
- Intraabdominal InfectionsDocument17 pagesIntraabdominal InfectionsmmsPas encore d'évaluation
- Pathophysiology, Clinical Manifestation and Diagnosis of PeritonitisDocument6 pagesPathophysiology, Clinical Manifestation and Diagnosis of PeritonitisIOSRjournalPas encore d'évaluation
- PeritonitisDocument10 pagesPeritonitisDrLiyana Abu BakarPas encore d'évaluation
- International Journal of Surgery: Elroy Patrick Weledji, Marcelin Ngowe NgoweDocument6 pagesInternational Journal of Surgery: Elroy Patrick Weledji, Marcelin Ngowe NgowehhhPas encore d'évaluation
- Urinary Tract Infections (UTI)Document32 pagesUrinary Tract Infections (UTI)Ruqaya HassanPas encore d'évaluation
- Bacterial Translocation in The GutDocument29 pagesBacterial Translocation in The GutdonkeyendutPas encore d'évaluation
- 16 Abdominal Tuberculosis - Un Diagnóstico DilemaDocument3 pages16 Abdominal Tuberculosis - Un Diagnóstico Dilemajhon_4548Pas encore d'évaluation
- Pancreatic Tuberculosis Diagnosis UpdateDocument24 pagesPancreatic Tuberculosis Diagnosis UpdatesamudraandiPas encore d'évaluation
- Journal PeritonitisDocument7 pagesJournal PeritonitisEudia SiagianPas encore d'évaluation
- PeritonitisDocument78 pagesPeritonitisTan Dan100% (1)
- Association Between Liver Fluke Infection and Hepatobiliary Pathological Changes: A Systematic Review and Meta-AnalysisDocument19 pagesAssociation Between Liver Fluke Infection and Hepatobiliary Pathological Changes: A Systematic Review and Meta-AnalysistiaranindyPas encore d'évaluation
- Tuberculous Ileal Perforation in Post-Appendicectomy PeriOperative Period: A Diagnostic ChallengeDocument3 pagesTuberculous Ileal Perforation in Post-Appendicectomy PeriOperative Period: A Diagnostic ChallengeIOSRjournalPas encore d'évaluation
- Pyelonephritis: Departemen Ilmu Penyakit Dalam FK Uii YogyakartaDocument33 pagesPyelonephritis: Departemen Ilmu Penyakit Dalam FK Uii YogyakartaAndaru Tri Setyo WibowoPas encore d'évaluation
- Peritonitis and Abdominal SepsisDocument37 pagesPeritonitis and Abdominal SepsisFernando AsencioPas encore d'évaluation
- Studiu 3 Partea SpecialaDocument5 pagesStudiu 3 Partea SpecialaMara HincuPas encore d'évaluation
- Infeccion Urinaria PCNA 2019Document13 pagesInfeccion Urinaria PCNA 2019andres felipe ramirezPas encore d'évaluation
- Peritonitis: Update On Pathophysiology, Clinical Manifestations, and ManagementDocument11 pagesPeritonitis: Update On Pathophysiology, Clinical Manifestations, and ManagementerikafebriyanarPas encore d'évaluation
- Management of Septic Peritonitis Related To Mortality in IBDDocument2 pagesManagement of Septic Peritonitis Related To Mortality in IBDRafif Abdurrahman WijisaksonoPas encore d'évaluation
- PeritonitisDocument14 pagesPeritonitisAyad IdresPas encore d'évaluation
- Peritoneal Tuberculosis Mimiking Gastrointestinal Stromal TumorDocument3 pagesPeritoneal Tuberculosis Mimiking Gastrointestinal Stromal TumorIJAR JOURNALPas encore d'évaluation
- Fistulas Enterocutaneas MaingotDocument20 pagesFistulas Enterocutaneas MaingotroyvillafrancaPas encore d'évaluation
- Case 013: Fever in A Cirrhotic PatientDocument5 pagesCase 013: Fever in A Cirrhotic PatientFitri 1997Pas encore d'évaluation
- Small Animal - Nephrology and UrologyDocument3 pagesSmall Animal - Nephrology and UrologyNana juniartiPas encore d'évaluation
- Current Concept of Abdominal Sepsis: WSES Position Paper: World Journal of Emergency Surgery March 2014Document17 pagesCurrent Concept of Abdominal Sepsis: WSES Position Paper: World Journal of Emergency Surgery March 2014Muhammad Hisyam AjimulyaPas encore d'évaluation
- Jurnal DigesDocument9 pagesJurnal DigesRendy SusantoPas encore d'évaluation
- Peritonitis-Dr BrianDocument65 pagesPeritonitis-Dr BrianJhon JefriPas encore d'évaluation
- Urosepsis 1Document7 pagesUrosepsis 1Anonymous Xajh4w100% (1)
- Peritonitis Update On Pathophysiology, Clinical Manifestations, and PDFDocument11 pagesPeritonitis Update On Pathophysiology, Clinical Manifestations, and PDFAnonymous InJS6aYZ100% (1)
- Peritonitis: Update On Pathophysiology, Clinical Manifestations, and ManagementDocument11 pagesPeritonitis: Update On Pathophysiology, Clinical Manifestations, and ManagementMuhamad Chairul SyahPas encore d'évaluation
- Abdominal Tuberculosis Research ReviewDocument12 pagesAbdominal Tuberculosis Research ReviewrikarikaPas encore d'évaluation
- Perforated PeritonitisDocument5 pagesPerforated PeritonitisDeepak singh ratheePas encore d'évaluation
- AF SeedingDocument6 pagesAF SeedingdonkeyendutPas encore d'évaluation
- Frances 1Document9 pagesFrances 1Alfonn Fernandez MonescilloPas encore d'évaluation
- Peritonitis: MselemaDocument64 pagesPeritonitis: MselemaAugustus CaesarPas encore d'évaluation
- MDSCPDocument12 pagesMDSCParranyPas encore d'évaluation
- 37poflee EtalDocument3 pages37poflee EtaleditorijmrhsPas encore d'évaluation
- Causes, Types, Symptoms and Treatment of PeritonitisDocument22 pagesCauses, Types, Symptoms and Treatment of Peritonitis28 manan patelPas encore d'évaluation
- Infectious Diarrhea - Guideline For Ordering Stool SpecimensDocument8 pagesInfectious Diarrhea - Guideline For Ordering Stool Specimensgodeberta18Pas encore d'évaluation
- Theme: Peritonitis Clinocomorphological Charestics.: Vitebsk State Medical University Department of Pathological AnatomyDocument7 pagesTheme: Peritonitis Clinocomorphological Charestics.: Vitebsk State Medical University Department of Pathological AnatomyDonesan GowarippriyanPas encore d'évaluation
- Bacterial Uropathogenic Factors & Host DefensesDocument7 pagesBacterial Uropathogenic Factors & Host DefensesAtma AdiatmaPas encore d'évaluation
- Urinary Tract Infection - A Suitable Approach: Lecture NotesDocument7 pagesUrinary Tract Infection - A Suitable Approach: Lecture NotesMary Hedweg OpenianoPas encore d'évaluation
- Netter's IntestineDocument3 pagesNetter's IntestineRia DeviPas encore d'évaluation
- Jurnal DidanosineDocument8 pagesJurnal DidanosineRia DeviPas encore d'évaluation
- Spontaneous Bacterial Peritonitis (SBP) : DR - Chakravarthy, P.S, PG in Gastroenterology, Amc/KghDocument50 pagesSpontaneous Bacterial Peritonitis (SBP) : DR - Chakravarthy, P.S, PG in Gastroenterology, Amc/KghRia Devi100% (1)
- Taxonomy ReviewDocument6 pagesTaxonomy ReviewRia DeviPas encore d'évaluation
- Journal of Allergy and Clinical Immunology Volume 135 Issue 3 2015 (Doi 10.1016/j.jaci.2014.12.1910) Greenberger, Paul A. - Will A Nasal Corticosteroid Improve Control For Patients With Step 3 or HDocument2 pagesJournal of Allergy and Clinical Immunology Volume 135 Issue 3 2015 (Doi 10.1016/j.jaci.2014.12.1910) Greenberger, Paul A. - Will A Nasal Corticosteroid Improve Control For Patients With Step 3 or HRia DeviPas encore d'évaluation
- Ijms 10 01386Document21 pagesIjms 10 01386Ria DeviPas encore d'évaluation
- HBV WhoDocument166 pagesHBV WhoDuwonNay100% (1)
- 2015 Variceal HaemorrhageDocument25 pages2015 Variceal HaemorrhageRia DeviPas encore d'évaluation
- Ascites Cirrhosis 2Document13 pagesAscites Cirrhosis 2Saman AlisonPas encore d'évaluation
- Pharmaceuticals 03 01812Document30 pagesPharmaceuticals 03 01812Ria DeviPas encore d'évaluation
- Accuracy and precision of quantitative research results based on random samplingDocument9 pagesAccuracy and precision of quantitative research results based on random samplingRia DeviPas encore d'évaluation
- Yacoubi Et Al-2000-British Journal of PharmacologyDocument9 pagesYacoubi Et Al-2000-British Journal of PharmacologyRia DeviPas encore d'évaluation
- 2 - Karbhari - SHRDocument6 pages2 - Karbhari - SHRRia DeviPas encore d'évaluation
- HIV BiokimiaDocument20 pagesHIV BiokimiaRia DeviPas encore d'évaluation
- Lamivudine For Patients With Chronic Hepatitis B and Advanced Liver DiseaseDocument11 pagesLamivudine For Patients With Chronic Hepatitis B and Advanced Liver DiseaseRia DeviPas encore d'évaluation
- (Doi 10.1016/j.ijpharm.2015.01.022) T. Loftsson - Excipient Pharmacokinetics and ProfilingDocument7 pages(Doi 10.1016/j.ijpharm.2015.01.022) T. Loftsson - Excipient Pharmacokinetics and ProfilingRia DeviPas encore d'évaluation
- European Journal of Pharmaceutics and Biopharmaceutics Volume 82 Issue 3 2012 (Doi 10.1016/j.ejpb.2012.08.002) D. Velasco G. Réthoré B. Newland J. Parra C. Elvira A. Pa - Low Polydispersity (NDocument10 pagesEuropean Journal of Pharmaceutics and Biopharmaceutics Volume 82 Issue 3 2012 (Doi 10.1016/j.ejpb.2012.08.002) D. Velasco G. Réthoré B. Newland J. Parra C. Elvira A. Pa - Low Polydispersity (NRia DeviPas encore d'évaluation
- WEYHN YHLN Cirrhosis Guidance. Management of Spontaneous Bacterial PeritonitisDocument14 pagesWEYHN YHLN Cirrhosis Guidance. Management of Spontaneous Bacterial PeritonitisCempaka IrawatiPas encore d'évaluation
- Hiyama Et Al-2009-Journal of Gastroenterology and HepatologyDocument10 pagesHiyama Et Al-2009-Journal of Gastroenterology and HepatologyRia DeviPas encore d'évaluation
- Cell Mol Life Sci 2004 FisoneDocument16 pagesCell Mol Life Sci 2004 FisoneRia DeviPas encore d'évaluation
- 858 2516 1 PB PDFDocument10 pages858 2516 1 PB PDFMhuez Iz Brave'sPas encore d'évaluation
- 8Document6 pages8Nana SetiawanPas encore d'évaluation
- Should Quinolones Come First in Helicobacter Pylori Therapy?Document12 pagesShould Quinolones Come First in Helicobacter Pylori Therapy?Ria DeviPas encore d'évaluation
- Jurnal DidanosineDocument8 pagesJurnal DidanosineRia DeviPas encore d'évaluation
- GlipizideDocument2 pagesGlipizideRia DeviPas encore d'évaluation
- Short Communication: CaerulescensDocument7 pagesShort Communication: CaerulescensRia DeviPas encore d'évaluation
- Annals of Allergy, Asthma & Immunology Volume 114 Issue 1 2015 (Doi 10.1016/j.anai.2014.10.012) Hendeles, Leslie Khan, Yasmeen R. Shuster, Jonathan J. Chesro - Omalizumab Therapy For Asthma PatiDocument7 pagesAnnals of Allergy, Asthma & Immunology Volume 114 Issue 1 2015 (Doi 10.1016/j.anai.2014.10.012) Hendeles, Leslie Khan, Yasmeen R. Shuster, Jonathan J. Chesro - Omalizumab Therapy For Asthma PatiRia DeviPas encore d'évaluation
- ArticleDocument12 pagesArticleRia DeviPas encore d'évaluation
- Opioid Pharmacology: Pain Physician 2008: Opioid Special Issue: 11: S133-S153 - ISSN 1533-3159Document22 pagesOpioid Pharmacology: Pain Physician 2008: Opioid Special Issue: 11: S133-S153 - ISSN 1533-3159Suresh KumarPas encore d'évaluation
- Hidaat Alem The Medical Rights and Reform Act of 2009 University of Maryland University CollegeDocument12 pagesHidaat Alem The Medical Rights and Reform Act of 2009 University of Maryland University Collegepy007Pas encore d'évaluation
- Gcu On Wiki PediaDocument10 pagesGcu On Wiki Pediawajid474Pas encore d'évaluation
- Syllabus Sibos CLTDocument5 pagesSyllabus Sibos CLTgopimicroPas encore d'évaluation
- Extra Vocabulary: Extension Units 1 & 2Document1 pageExtra Vocabulary: Extension Units 1 & 2CeciBravoPas encore d'évaluation
- World War 2 Soldier Stories - Ryan JenkinsDocument72 pagesWorld War 2 Soldier Stories - Ryan JenkinsTaharPas encore d'évaluation
- Sigmund Freud QuotesDocument7 pagesSigmund Freud Quotesarbeta100% (2)
- MID Term VivaDocument4 pagesMID Term VivaGirik BhandoriaPas encore d'évaluation
- Bo's Coffee AprmDocument24 pagesBo's Coffee Aprmalliquemina100% (1)
- SCIENCE 5 PPT Q3 W6 - Parts of An Electric CircuitDocument24 pagesSCIENCE 5 PPT Q3 W6 - Parts of An Electric CircuitDexter Sagarino100% (1)
- Freeing Music Education From Schooling: Toward A Lifespan Perspective On Music Learning and TeachingDocument24 pagesFreeing Music Education From Schooling: Toward A Lifespan Perspective On Music Learning and TeachingRockyPas encore d'évaluation
- Harmonizing A MelodyDocument6 pagesHarmonizing A MelodyJane100% (1)
- TCW The Global CityDocument40 pagesTCW The Global CityAllen Carl100% (1)
- Team Roles EssayDocument7 pagesTeam Roles EssayCecilie Elisabeth KristensenPas encore d'évaluation
- Dues & Scholarship Section: NotificationDocument6 pagesDues & Scholarship Section: NotificationMUNEEB WAHEEDPas encore d'évaluation
- Balochistan Conservation Strategy VDocument388 pagesBalochistan Conservation Strategy VHãšãñ Trq100% (1)
- Motivation and Emotion FinalDocument4 pagesMotivation and Emotion Finalapi-644942653Pas encore d'évaluation
- NetZoom Pro v15 Install GuideDocument81 pagesNetZoom Pro v15 Install Guidescribd!!Pas encore d'évaluation
- Senarai Syarikat Berdaftar MidesDocument6 pagesSenarai Syarikat Berdaftar Midesmohd zulhazreen bin mohd nasirPas encore d'évaluation
- Introduction To Competitor AnalysisDocument18 pagesIntroduction To Competitor AnalysisSrinivas NandikantiPas encore d'évaluation
- Diabetic Foot InfectionDocument26 pagesDiabetic Foot InfectionAmanda Abdat100% (1)
- Simple Future Vs Future Continuous Vs Future PerfectDocument6 pagesSimple Future Vs Future Continuous Vs Future PerfectJocelynPas encore d'évaluation
- REMEDIOS NUGUID vs. FELIX NUGUIDDocument1 pageREMEDIOS NUGUID vs. FELIX NUGUIDDanyPas encore d'évaluation
- Treviranus ThesisDocument292 pagesTreviranus ThesisClaudio BritoPas encore d'évaluation
- Disability Election ManifestoDocument2 pagesDisability Election ManifestoDisability Rights AlliancePas encore d'évaluation
- Lab 5: Conditional probability and contingency tablesDocument6 pagesLab 5: Conditional probability and contingency tablesmlunguPas encore d'évaluation
- Common Application FormDocument5 pagesCommon Application FormKiranchand SamantarayPas encore d'évaluation
- Virtuoso 2011Document424 pagesVirtuoso 2011rraaccPas encore d'évaluation
- Kepler's Law 600 Years Before KeplerDocument7 pagesKepler's Law 600 Years Before KeplerJoe NahhasPas encore d'évaluation
- Jurnal Manajemen IndonesiaDocument20 pagesJurnal Manajemen IndonesiaThoriq MPas encore d'évaluation
- House & Garden - November 2015 AUDocument228 pagesHouse & Garden - November 2015 AUHussain Elarabi100% (3)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionD'EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionÉvaluation : 4 sur 5 étoiles4/5 (402)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingD'EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingÉvaluation : 5 sur 5 étoiles5/5 (4)
- The Age of Magical Overthinking: Notes on Modern IrrationalityD'EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityÉvaluation : 4 sur 5 étoiles4/5 (13)
- The Happiness Trap: How to Stop Struggling and Start LivingD'EverandThe Happiness Trap: How to Stop Struggling and Start LivingÉvaluation : 4 sur 5 étoiles4/5 (1)
- The Comfort of Crows: A Backyard YearD'EverandThe Comfort of Crows: A Backyard YearÉvaluation : 4.5 sur 5 étoiles4.5/5 (23)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeD'EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BePas encore d'évaluation
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsD'EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsÉvaluation : 3.5 sur 5 étoiles3.5/5 (3)
- The Obesity Code: Unlocking the Secrets of Weight LossD'EverandThe Obesity Code: Unlocking the Secrets of Weight LossÉvaluation : 5 sur 5 étoiles5/5 (3)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedD'EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedÉvaluation : 5 sur 5 étoiles5/5 (78)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisD'EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisÉvaluation : 4 sur 5 étoiles4/5 (1)
- Why We Die: The New Science of Aging and the Quest for ImmortalityD'EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityÉvaluation : 3.5 sur 5 étoiles3.5/5 (2)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsD'EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsPas encore d'évaluation
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsD'EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsÉvaluation : 4.5 sur 5 étoiles4.5/5 (169)
- The Ultimate Guide To Memory Improvement TechniquesD'EverandThe Ultimate Guide To Memory Improvement TechniquesÉvaluation : 5 sur 5 étoiles5/5 (34)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsD'EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsPas encore d'évaluation
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingD'EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (31)
- Techniques Exercises And Tricks For Memory ImprovementD'EverandTechniques Exercises And Tricks For Memory ImprovementÉvaluation : 4.5 sur 5 étoiles4.5/5 (40)
- Summary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisD'EverandSummary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisÉvaluation : 5 sur 5 étoiles5/5 (3)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.D'EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Évaluation : 4.5 sur 5 étoiles4.5/5 (110)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaD'EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeD'EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeÉvaluation : 4.5 sur 5 étoiles4.5/5 (253)
- Secure Love: Create a Relationship That Lasts a LifetimeD'EverandSecure Love: Create a Relationship That Lasts a LifetimeÉvaluation : 5 sur 5 étoiles5/5 (16)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessD'EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessÉvaluation : 4.5 sur 5 étoiles4.5/5 (327)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryD'EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryÉvaluation : 4 sur 5 étoiles4/5 (44)