Académique Documents
Professionnel Documents
Culture Documents
Intra Operative and ICU Management of Transurethral Resection of Prostrate Syndrome: A Case Report
Transféré par
IOSRjournalCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Intra Operative and ICU Management of Transurethral Resection of Prostrate Syndrome: A Case Report
Transféré par
IOSRjournalDroits d'auteur :
Formats disponibles
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS)
e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 14, Issue 11 Ver. I (Nov. 2015), PP 55-59
www.iosrjournals.org
Intra Operative and ICU Management of Transurethral
Resection of Prostrate Syndrome: A Case Report
Samit Parua*, Rupak Kundu*
*Post Graduate Trainee, Department Of Anaesthesiology And Critical Care, Gauhati Medical College And
Hospital.
Abstract: We report a case of transurethral resection of prostrate syndrome in a 56 year old man, who
underwent transurethral resection of prostrate (TURP) under spinal anaesthesia for a duration of 150 minutes
using glycine as the irrigant solution and developed nausea vomiting hypoxaemia , pulmonary oedema
intraoperatively and later in the post of period had profound hypotension, frank pulmonary oedema. Serum
electrolyte report showed sodium was 118 meq/L. Medical management consisted of diuretic therapy, volume
restriction, treatment of pulmonary oedema , mechanical ventilation. Patient received proper and timely
treatment and was finally discharged.
Introduction
TURP SYNDROME is used to describe a wide range of neurological and cardiopulmonary symptoms
that occour due to absorption of irrigation fluid used during resection into systemic circulation,specially TURP. 1
The main problems associated with it are rapid intra vascular fluid expansion , hyponatremia,
hypoosmolarity and problems due to the type of irrigation fluid used.
Case Findings And Management
A 56 year ASA I male patient weighing 60kgs underwent transurethral resection of prostrate on 15 th
may 2015 at Gauhati Medical College, Urosurgery Department. Patient gave no history of any coexisting
disease or medications. Preoperative serum Sodium was 142 meq/L, serum Potassium was 3.8 meq/L, Urea 40
mg%, Creatinine 1.8 mg%. On table vitals noted were a Heart Rate of 90 per min, Blood Pressure of 140/90 mm
Hg, a normal ECG and SpO2 of 98% with room air. Patient was adminstered spinal anaesthesia with 3ml of
Bupivacaine Heavy(0.5%), whose upper level extended to T8 dermatome, confirmed by pinprick method. Post
spinal vitals being Heart Rate of 80/min and Blood Pressure of 130/80 mm Hg. Patient was placed in lithotomy
position and surgery was started. Irrigation fluid used was 1.5% Glycine and resection was done using
monopolar instrument. The height of the irrigation fluid was kept fixed at 60 cms from the table. The
intraoperative vitals varied between 120 to 140 mm Hg Systolic and 70 to 100 mm Hg Diastolic, Heart Rate of
70 to 90 beats per minute. The whole procedure lasted 150 minutes with a estimated blood loss of 550 ml.
Intraoperatively patient received 1600 ml of isotonic saline. Just as the operation was about to end, patient
became increasingly restless, agitated with complaint of nausea vomiting and respiratory distress. Vitals noted
were Blood Pressure of 140/90 mm Hg, Heart Rate of 110/min and SpO2 of 93% with high flow oxygen. Chest
auscultation revealed bilateral mild basal crepitations. Patient was given Inj Lasix 40mg IV, surgeon was
informed about the event and the flow of the irrigation fluid was minimised. Positive pressure bag mask
ventilation was initiated. Despite positive pressure ventilation with high flow oxygen, patient SpO2 was less
than 90%, so patient had to be intubated. Electrolytes, Complete Blood Count, Urea, Creatinine were sent
urgently for evaluation. Patient was transferred post-operatively to Intensive Care Unit (ICU) . In the ICU Blood
Pressure of 110/70 mm Hg, Heart Rate of 72/min and SpO2 of 99% with 10L/min oxygen, on T piece was noted.
Patient had a GCS of 7/15 but was restless. A Central Venous Catheterization was done in right internal jugular
vein, opening CVP was 18 cm of water. Patients Blood Pressure & Heart Rate further detoriated to of 70/40
mm Hg & 50 beats per minute, chest auscultation revealed bilateral extensive crepitations. Patient was started
on infusion Dopamine and later infusion Noradrenaline was added. Even after starting inotropes patient was
persistently hypotensive. 30 minutes later pink froth was noticed through the patients endotracheal tube, his
Blood Pressure noted was 80/40 mm Hg. Patients GCS further detoriated to 4/15. Patient was immediately put
on mechanical ventilation and Dopamine & Noradrenaline infusion were increased to their maximum doseage.
30 minutes later patients Blood Pressure was 100/70 mm Hg. Over the next 3 to 4 hours patients Blood
Pressure gradually stabilized and ventilatory PEEP was added and gradually increased upto 8 cm of water.
Blood investigations showed serum Sodium of 118 meq/L, Potassium 3.8 meq/L, Urea 58 mg%, Creatinine 1.8
mg%, so it was a clear cut case of TURP syndrome with acute pulmonary odema. With medical therapy and
mechanical ventilation CVP gradually came down to 12 cm of water and pulmonary odema subsided. Blood
Pressure stabilized at 125/80 mm of Hg with Noradrenaline inf @ 10 ml/hour and Dopamine inf @ 5ml/hour.
DOI: 10.9790/0853-141115559
www.iosrjournals.org
55 | Page
Intra Operative and ICU Management of Transurethral Resection of Prostrate Syndrome
Blood investigations were sent 4 hours later revealed serum Sodium of 122 meq/L, Potassium of 3.6 meq/L,
Urea-70 mg%, Creatinine- 1.9 mg%, Haemoglobin 7.8 gm%, PCV-27%, negative Troponin t. Serum ammonia
and glycine levels could not be estimated. 100 ml of 3% hypertonic saline was started @ 20 ml per hour over the
next 5 hours. Measurement of all irrigating fluid gave a rough estimate that probably 60 liters of irrigation fluid
was used of which 5.5 L was absorbed intravascularly. Later one unit packed cell was transfused . Electrolytes
sent 12hours later showed a serum Sodium of 128 meq/L. From the second post operative day patient was fluid
restricted, and regular CVP monitoring was done. Serum Sodium report came as 134meq/L, Ammonia was 90
mg%, Troponin t was positive, inotropes were gradually tapered off and patient was extubated on the third post
operative day. Patient progressed favourably in ICU and was shifted out on 4th postoperative day and
subsequently discharged after a week.
Discussion
Wier and associates reported Water Intoxication in 1922 as excess water intake that resulted in disorders of
consciousness and convulsions.2 Transurethral resection (TUR) syndrome is an iatrogenic form of water
intoxication, a combination of fluid overload and dillusional hyponatremia that is seen in a variety of endoscopic
surgical procedures and specially after transurethral resection of prostrate. It has also been observed in other
procedures using irrigation fluid like transurethral resection of bladder tumors ( TURBT ), diagnostic
cystoscopy, percutaneus nephrolithotomy, arthroscopy and various other endoscopic gynecological
procedures.3 Recent studies show, the incidence rate of mild to moderate TURP syndrome is 0.78% and
1.4% 4,5 and Severe TURP syndrome though rare, but is associated with a high mortality rate of 25%.6 TURP
syndrome has been observed as early as 15 minutes following the start of surgical procedure7 , sometimes upto
24 hours postoperatively.8 So the patients undergoing such intervensions require thorough intraoperative and
postoperative monitoring for timely diagnosis and management of TURP syndrome.
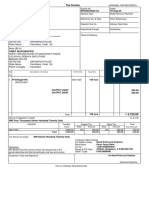
Signs And Symptoms
SIGNS AND SYMPTOMS OF TRANSURETHRAL RESECTION OF THE PROSTATE SYNDROME.3
Central Nervous System
Cardiovascular And Respiratory
Metabolic And Renal
Restlessness, headache , confusion
Hypertension, tachycardia , tachypnea
Hyponatremia,
hyperglycinemia,
intravascular haemolysis
Visual disturbances, nausea and Hypotension, bradycardia
Acute renal failure
vomiting
Convulsion and coma
Hypoxia , pulmonary oedema
TURP syndrome is mainly caused by the absorption of irrigation fluid that leads to cardiovascular,
central nervous system (CNS) and metabolic changes. The clinical picture varies according to the severity of the
condition, the type of irrigant fluid used, patient factors and surgical factors. Earliest sign consists of transient
prickling and burning sensations in the face, neck accompanied with lethargy and apprehension, often the
patient may become restless with complaint of headache. The most common signs are bradycardia and arterial
hypotension, which may be the first presentation to be detected in the perioperative period by the attending
anaesthesia team. In about 10% of patients a general nonspecific sense of being unwell is seen, which is a
commoner symptom than perioperative nausea or vomiting.9 Abdominal distention secondary to absorption of
the irrigating fluid through perforations in the prostatic capsule or secondary to bladder rupture may occour.10
In the later postoperative period visual disturbances, twitches, focal or generalized seizures with altered
state of consciousness, ranging from mild confusion to stupor & coma have been reported.11,12,13
Our patient experienced nausea vomiting, restlessness & agitation followed by respiratory distress and
subsequently developed hypoxia and hypotension intraoperatively.
Pathophysiology
The pathophysiology of TURP syndrome is complex, the typical sign and symptoms could be
explained by the following pathological changes
fluid overload, hyponatremia, hypo-osmolality,
hyperammonemia.
Fluid overload:- Small amounts of irrigant fluid continuously gets absorbed through the open prostatic venous
sinuses during TURP. If 1 L of irrigant fluid is absorbed into the circulation within 1 hour , it causes an acute
decrease in the serum sodium concentration of 5 to 8 meq/L and hence increases risk of absorption related
symptoms.14,15 Both hypertension and hypotension may be associated with TURP syndrome. Hypertension may
be due to the rapid intravascular irrigant fluid absorption . Hypotension may due to pulmonary interstitial
odema, hypovoalaemic shock16, release of endotoxins into circulation and metabolic acidosis.17,18
DOI: 10.9790/0853-141115559
www.iosrjournals.org
56 | Page
Intra Operative and ICU Management of Transurethral Resection of Prostrate Syndrome
Hyponatremia:- Serum sodium concentration of <120 meq/L is defined as severe TURP syndrome.11 This
decrease in sodium concentration builds up an osmotic gradient between intracellular and extracellular fluid
within the brain, which results in a fluid shift away from the intravascular space leading to brain edema, raised
intracranial pressure and neurologic symptoms.19 Severe and rapidly evolving hyponatremia may manifest with
seizures, coma, permanent brain damage, respiratory arrest, brain stem herniation ultimately causing death.20
Hypo-osmolality:- The blood-brain barrier is virtually impermeable to sodium but freely permeable to water. 21
The brain reacts to hypo-osmotic stress with intracellular decreases in Sodium, Potassium and Chloride. This
decrease in intracellular Sodium, Potassium, and Chloride helps to reduce intracellular osmolality and prevent
swelling.22 Brain edema is a serious issue, leading to cerebral herniation,which is the major cause of death in
these patients.21
Hyperammonemia:- Glycine ( used as irrigant during TURP) is metabolised in brain to release ammonia.
Hyperammonemic encephalopathy develops as a result of the formation of ammonia. Blood ammonia
concentrations >100 mmol/L (normal range 1035) are associated with neurologic signs and symptoms. 23
Irrigation Fluid:- An ideal irrigating fluid should be isotonic, nonhemolytic, electrically inert, nontoxic,
transparent, easy to sterilize, and inexpensive. Glycine , cytal, isotonic saline are used as irrigation fluid.
Our patient was drowsy with a detoriating GCS due to severe hyponatremia( 118 meq/l), hyperammonemia ( 90
mg%), accompanied with hypotension.
Management Of Turp Syndrome
Proper estimation of amount of irrigation fluid absorbed by
Ethanol monitoring method.
Central venous pressure measurements.
Gravimetry methods.
In our patient we did not specify the method of estimation of absorbed irrigation fluid.
Prevension of TURP syndrome.
Keeping the patient in Trendelenburg positioning on the operating table, especially in high-risk patients.24
Operative time & prostrate gland size:- It is recommended that the operative time be limited to less than 60
minutes. Mebust et al. 25 retrospectively reviewed 3885 patients who underwent TURP and found that with
a resection time more than 90 minutes, incidence of development of TURP syndrome was 2% compared
with the group with a resection time of less than 90 minutes, the incidence of intraoperative bleeding was
significantly higher (7.3%) with resection time >90 minutes as compared to 0.9% in patients with resection
time <90 minutes. In this study the incidence of TURP syndrome was 0.7%. Patients with prostrate gland
size larger than 45 g have a greater risk of development of TURP syndrome.
Madsen et al. 26 demonstrated that the pressure in the prostatic fossa and the amount of the irrigation fluid
absorbed depend on the height of the irrigating fluid above the patient and suggested that the optimum
height should be 60 cm above the patient. Performing TURP under low pressure prevents absorption of
large volumes of irrigation fluid from the open prostatic sinuses.
Operative experience:- The more experienced the surgeon the lesser is the resection time and lesser is the
chance of development of TURP syndrome.
Intraprostatic vasopressin injection:- Sharma et al.27 studied the effect of transrectal intraprostatic
vasopressin (IPVP) injection in patients who were undergoing TURP. TURP syndrome did not develop in
any of the patients, and there was reduced blood loss during the resection, which further limited the amount
of irrigant that entered the systemic circulation.
Performing a BIPOLAR TURP, LASER TURP decreases the chances of development of TURP
syndrome.3
In our patient the irrigation fluid level was maintained at 60 cms above patient and monopolar resection was
done.
Treatment of TURP Syndrome And Anaesthetic Considerations.
Prevension of development of TURP syndrome is of utmost importance. Proper timely diagnosis of
symptoms is necessary.
DOI: 10.9790/0853-141115559
www.iosrjournals.org
57 | Page
Intra Operative and ICU Management of Transurethral Resection of Prostrate Syndrome
Upon diagnosis/suspicion ask surgeon to stop/complete surgery as soon as possible with thorough
cauterization of all open prostatic venous plexuses.3
Supporting respiration and supplemental oxygenation is always necessary, and intubation and ventilation
may also be needed along with intravenous anticonvulsants. 28 Anticonvulsants mainly NMDA receptor
antagonist may be used.
Intraoperative bradycardia and hypotension to be treated using atropine, adrenergic drugs and calcium.29
Plasma volume expansion and inotrope therapy may be needed in patients with persistent hypotension.
Administer hypertonic saline 3% only if severe hyponatremia (serum Sodium < 120 mmol/L ), raising
serum Sodium concentration by 1 mmol/L/hour decreases the chances of central pontine myelinolysis. In
cases of mild to moderate hyponatremia consider volume restriction. Diuretics are specially used in a case
TURP syndrome with pulmonary odema but should be avoided if patient is haemodynamically unstable. 3
Spinal anaesthesia is the most common anesthetic technique of choice for TURP. Spinal anesthesia reduces
the risk of pulmonary edema, allows early detection of mental status.30 Spinal anesthesia however reduces
CVP, resulting in greater absorption of irrigating fluid compared to general anesthesia.31 Fluid loading
during spinal anaesthesia should be done with caution specially in elderly patients undergoing TURP.
Under general anesthesia, the diagnosis of TURP syndrome may be difficult, because patients are unable to
complain of early symptoms, and anaesthesist must solely rely on the changes in blood pressure and pulse
together with electrocardiographic changes for intraoperative diagnosis.3
The short term and long term cardiac morbidity and mortality after TURP syndrome are compareable for
general and regional anesthesia.32
Post operative ICU/ITU care is necessary for these patients.
Our patient had episodes of persistent hypotension both intraoperatively and postoperatively and had to be kept
on inotrope infusion and later one unit blood was transfused postoperatively. Our patient received postoperative
ICU care. Sodium correction in our patient was done gradually mainly by hypertonic saline infusion, diuretics
and volume restriction.
Conclusion
So we may conclude that there may be variable presentation of a patient developing intraoperative
TURP syndrome and so defining a particular protocol of management in these patients is not always feasible
and a thorough understanding of the pathophysiology of this syndrome is necessary for instituting proper and
timely treatment in these patients. Prevension of development of TURP syndrome is more important than its
management.
Disclosure Statement
No competing financial interests exist.
References
[1].
[2].
[3].
[4].
[5].
[6].
[7].
[8].
[9].
[10].
[11].
[12].
[13].
[14].
[15].
[16].
[17].
Patel SN, Patel ND. Serum sodium and serum potassium changes during transurethral resection of prostate gland in patients under
subarachnoid block. National journal of medical research 2014;4: 322-325.
Weir JF, Larson EE, Rowntree LG. Studies in diabetes insipidus water balance. Arch Intern Med 1922;29:306.
Hawary A, Mukhtar K, Sinclair A,Pearce I. Transurethral Resection of the Prostate Syndrome: Almost Gone but Not Forgotten.
Journal of endourology, december 2009;23(12): 2013-2020.
Zepnick H, Steinbach F, Schuster F. [Value of transurethral resection of the prostate (TURP) for treatment of symptomatic benign
prostatic obstruction (BPO): An analysis of efficiency and complications in 1015 cases.] (Ger) Aktuelle Urol 2008;39:369372.
Reich O, Gratzke C, Bachmann A, et al. Morbidity, mortality and early outcome of transurethral resection of the prostate: A
prospective multicenter evaluation of 10,654 patients. J Urol 2008;180:246249.
Hahn RG. Irrigating fluids in endoscopic surgery. Br J Urol 1997;79:669680.
Hurlbert BJ, Wingard DW. Water intoxication after 15 minutes of transurethral resection of the prostate. Anesthesiology
1979;50:355356.
Swaminathan R, Tormey WP. Fluid absorption during transurethral prostatectomy [letter]. Br J Urol 1981;282:317.
Hahn RG. Fluid absorption in endoscopic surgery. Br J Anaesth 2006;96:820.
Olsson J, Nilsson A, Hahn RG. Symptoms of the transurethral resection syndrome using glycine as the irrigant. J Urol
1995;154:123128.
Hatch PD. Surgical and anaesthetic considerations in transurethral resection of the prostate. Anaesth Intensive Care 1987;15:203
211.
Marx GF, Orkin LR. Complications associated with transurethral surgery. Anesthesiology 1962;23;802813.
Henderson DJ, Middleton RG. Coma from hyponatraemia following transurethral resection of the prostate. Urology 1980;15:267
271.
Olsson J, Nilsson A, Hahn RG. Symptoms of the transurethral resection syndrome using glycine as the irrigant. J Urol
1995;154:123128.
Hahn RG, Ekengren JC. Patterns of irrigating fluid absorption during transurethral resection of the prostate as indicated by ethanol.
J Urol 1993;149:502506.
Ceccarelli FE, Mantell LK. Studies on fluid and electrolyte alterations during transurethral prostatectomy. J Urol 1961; 85:7582.
Hahn RG. Acid-base status following glycine absorption in transurethral surgery. Eur J Anaesthesiol 1992;9:15.
DOI: 10.9790/0853-141115559
www.iosrjournals.org
58 | Page
Intra Operative and ICU Management of Transurethral Resection of Prostrate Syndrome
[18].
[19].
[20].
[21].
[22].
[23].
[24].
[25].
[26].
[27].
[28].
[29].
[30].
[31].
[32].
Sohn MH, Vogt C, Heinen G, et al. Fluid absorption and circulating endotoxins during transurethral resection of the prostate. Br J
Urol 1993;72:605610.
Reynolds RM, Padfield PL, Seckl JR. Disorders of sodium balance. BMJ 2006;332:702705.
Ellis SJ. Severe hyponatraemia: Complications and treatment.QJM 1995;88:905909.
Fenstermacher JD, Johnson JA. Filtration and reflection coefficients of the rabbit blood-brain barrier. Am J Physiol 1966;211:341
346.
Andrew RD. Seizure and acute osmotic change: Clinical and neurophysiological aspects. J Neurol Sci 1991;101:718.
Hoekstra PT, Kahnoski R, McCamish MA, et al. Transurethral prostatic resection syndromea new perspective: Encephalopathy
with associated hyperammonemia. J Urol 1983;130:704707.
Hulten J. Prevention of irrigating fluid absorption during transurethral resection of the prostate. Scand J Urol Nephrol
1984;82(suppl):180.
Mebust WK, Holtgrewe HL, Cocket AT, Peters PC. Transurethral prostatectomy: Immediate and postoperative complications. A
cooperative study of 13 participating institutions evaluating 3885 patients. J Urol 1989;141:243247.
Madsen PO, Naber KG. The importance of the pressure in the prostatic fossa and absorption of irrigating fluid during transurethral
resection of the prostate. J Urol 1973;109:446452.
Sharma DP, Harvey AB. Does intraprostatic vasopressin prevent the transurethral resection syndrome? BJU Int 2000; 86:223226.
Munn J. TURP syndrome. In: Allman K, Wilson I, ed. Oxford Handbook of Anaesthesia. 2nd ed. Oxford, UK: Oxford University
Press, 2006, pp. 570571.
Singer M, Patel M, Webb AR, Bullen C. Management of the transurethral prostate resection syndrome: Time for reappraisal? Crit
Care Med 1990;18:14791480.
Azar I. Transurethral prostatectomy syndrome and other complications of urological procedures. In: McLeskey CH, ed. Geriatric
Anaesthesiology. Baltimore: Williams & Wilkins, 1997, pp. 595607.
Gehring H, Nahm W, Baerwald J, et al. Irrigation fluid absorptionduring transurethral resection of the prostate:Spinal vs. general
anaesthesia. Acta Anaesthesiol Scand 1999;43:458463.
Edwards ND, Callaghan LC, White T, Reilly CS. Perioperative myocardial ischaemia in patients undergoing transurethral surgery :
A pilot study comparing general with spinal anaesthesia. Br J Anaesth 1995;74:368372.
DOI: 10.9790/0853-141115559
www.iosrjournals.org
59 | Page
Vous aimerez peut-être aussi
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- No-Vacation NationDocument24 pagesNo-Vacation NationCenter for Economic and Policy Research91% (54)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (894)
- TarotDocument21 pagesTarotKrystal Jacquot100% (2)
- Kinesics, Haptics and Proxemics: Aspects of Non - Verbal CommunicationDocument6 pagesKinesics, Haptics and Proxemics: Aspects of Non - Verbal CommunicationInternational Organization of Scientific Research (IOSR)Pas encore d'évaluation
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Linear RegressionDocument56 pagesLinear RegressionRanz CruzPas encore d'évaluation
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- A Business Development PlanDocument90 pagesA Business Development PlanRishabh Sarawagi100% (1)
- Human Rights and Dalits: Different Strands in The DiscourseDocument5 pagesHuman Rights and Dalits: Different Strands in The DiscourseInternational Organization of Scientific Research (IOSR)Pas encore d'évaluation
- Method Statement For Wall Panels InstallationDocument11 pagesMethod Statement For Wall Panels InstallationChristos LoutrakisPas encore d'évaluation
- GRADE 8 English Lesson on Indian LiteratureDocument3 pagesGRADE 8 English Lesson on Indian LiteratureErold TarvinaPas encore d'évaluation
- The Impact of Technologies On Society: A ReviewDocument5 pagesThe Impact of Technologies On Society: A ReviewInternational Organization of Scientific Research (IOSR)100% (1)
- Socio-Ethical Impact of Turkish Dramas On Educated Females of Gujranwala-PakistanDocument7 pagesSocio-Ethical Impact of Turkish Dramas On Educated Females of Gujranwala-PakistanInternational Organization of Scientific Research (IOSR)Pas encore d'évaluation
- "I Am Not Gay Says A Gay Christian." A Qualitative Study On Beliefs and Prejudices of Christians Towards Homosexuality in ZimbabweDocument5 pages"I Am Not Gay Says A Gay Christian." A Qualitative Study On Beliefs and Prejudices of Christians Towards Homosexuality in ZimbabweInternational Organization of Scientific Research (IOSR)Pas encore d'évaluation
- Assessment of The Implementation of Federal Character in Nigeria.Document5 pagesAssessment of The Implementation of Federal Character in Nigeria.International Organization of Scientific Research (IOSR)Pas encore d'évaluation
- An Evaluation of Lowell's Poem "The Quaker Graveyard in Nantucket" As A Pastoral ElegyDocument14 pagesAn Evaluation of Lowell's Poem "The Quaker Graveyard in Nantucket" As A Pastoral ElegyInternational Organization of Scientific Research (IOSR)Pas encore d'évaluation
- A Review of Rural Local Government System in Zimbabwe From 1980 To 2014Document15 pagesA Review of Rural Local Government System in Zimbabwe From 1980 To 2014International Organization of Scientific Research (IOSR)Pas encore d'évaluation
- Relationship Between Social Support and Self-Esteem of Adolescent GirlsDocument5 pagesRelationship Between Social Support and Self-Esteem of Adolescent GirlsInternational Organization of Scientific Research (IOSR)Pas encore d'évaluation
- A Proposed Framework On Working With Parents of Children With Special Needs in SingaporeDocument7 pagesA Proposed Framework On Working With Parents of Children With Special Needs in SingaporeInternational Organization of Scientific Research (IOSR)Pas encore d'évaluation
- Attitude and Perceptions of University Students in Zimbabwe Towards HomosexualityDocument5 pagesAttitude and Perceptions of University Students in Zimbabwe Towards HomosexualityInternational Organization of Scientific Research (IOSR)Pas encore d'évaluation
- The Role of Extrovert and Introvert Personality in Second Language AcquisitionDocument6 pagesThe Role of Extrovert and Introvert Personality in Second Language AcquisitionInternational Organization of Scientific Research (IOSR)Pas encore d'évaluation
- Comparative Visual Analysis of Symbolic and Illegible Indus Valley Script With Other LanguagesDocument7 pagesComparative Visual Analysis of Symbolic and Illegible Indus Valley Script With Other LanguagesInternational Organization of Scientific Research (IOSR)Pas encore d'évaluation
- Investigation of Unbelief and Faith in The Islam According To The Statement, Mr. Ahmed MoftizadehDocument4 pagesInvestigation of Unbelief and Faith in The Islam According To The Statement, Mr. Ahmed MoftizadehInternational Organization of Scientific Research (IOSR)Pas encore d'évaluation
- Importance of Mass Media in Communicating Health Messages: An AnalysisDocument6 pagesImportance of Mass Media in Communicating Health Messages: An AnalysisInternational Organization of Scientific Research (IOSR)Pas encore d'évaluation
- Edward Albee and His Mother Characters: An Analysis of Selected PlaysDocument5 pagesEdward Albee and His Mother Characters: An Analysis of Selected PlaysInternational Organization of Scientific Research (IOSR)Pas encore d'évaluation
- The Lute Against Doping in SportDocument5 pagesThe Lute Against Doping in SportInternational Organization of Scientific Research (IOSR)Pas encore d'évaluation
- Beowulf: A Folktale and History of Anglo-Saxon Life and CivilizationDocument3 pagesBeowulf: A Folktale and History of Anglo-Saxon Life and CivilizationInternational Organization of Scientific Research (IOSR)Pas encore d'évaluation
- Topic: Using Wiki To Improve Students' Academic Writing in English Collaboratively: A Case Study On Undergraduate Students in BangladeshDocument7 pagesTopic: Using Wiki To Improve Students' Academic Writing in English Collaboratively: A Case Study On Undergraduate Students in BangladeshInternational Organization of Scientific Research (IOSR)Pas encore d'évaluation
- Role of Madarsa Education in Empowerment of Muslims in IndiaDocument6 pagesRole of Madarsa Education in Empowerment of Muslims in IndiaInternational Organization of Scientific Research (IOSR)Pas encore d'évaluation
- Classical Malay's Anthropomorphemic Metaphors in Essay of Hikajat AbdullahDocument9 pagesClassical Malay's Anthropomorphemic Metaphors in Essay of Hikajat AbdullahInternational Organization of Scientific Research (IOSR)Pas encore d'évaluation
- An Exploration On The Relationship Among Learners' Autonomy, Language Learning Strategies and Big-Five Personality TraitsDocument6 pagesAn Exploration On The Relationship Among Learners' Autonomy, Language Learning Strategies and Big-Five Personality TraitsInternational Organization of Scientific Research (IOSR)Pas encore d'évaluation
- Transforming People's Livelihoods Through Land Reform in A1 Resettlement Areas in Goromonzi District in ZimbabweDocument9 pagesTransforming People's Livelihoods Through Land Reform in A1 Resettlement Areas in Goromonzi District in ZimbabweInternational Organization of Scientific Research (IOSR)Pas encore d'évaluation
- Women Empowerment Through Open and Distance Learning in ZimbabweDocument8 pagesWomen Empowerment Through Open and Distance Learning in ZimbabweInternational Organization of Scientific Research (IOSR)Pas encore d'évaluation
- Motivational Factors Influencing Littering in Harare's Central Business District (CBD), ZimbabweDocument8 pagesMotivational Factors Influencing Littering in Harare's Central Business District (CBD), ZimbabweInternational Organization of Scientific Research (IOSR)Pas encore d'évaluation
- Design Management, A Business Tools' Package of Corporate Organizations: Bangladesh ContextDocument6 pagesDesign Management, A Business Tools' Package of Corporate Organizations: Bangladesh ContextInternational Organization of Scientific Research (IOSR)Pas encore d'évaluation
- Substance Use and Abuse Among Offenders Under Probation Supervision in Limuru Probation Station, KenyaDocument11 pagesSubstance Use and Abuse Among Offenders Under Probation Supervision in Limuru Probation Station, KenyaInternational Organization of Scientific Research (IOSR)Pas encore d'évaluation
- Designing of Indo-Western Garments Influenced From Different Indian Classical Dance CostumesDocument5 pagesDesigning of Indo-Western Garments Influenced From Different Indian Classical Dance CostumesIOSRjournalPas encore d'évaluation
- Micro Finance and Women - A Case Study of Villages Around Alibaug, District-Raigad, Maharashtra, IndiaDocument3 pagesMicro Finance and Women - A Case Study of Villages Around Alibaug, District-Raigad, Maharashtra, IndiaInternational Organization of Scientific Research (IOSR)Pas encore d'évaluation
- A Study On The Television Programmes Popularity Among Chennai Urban WomenDocument7 pagesA Study On The Television Programmes Popularity Among Chennai Urban WomenInternational Organization of Scientific Research (IOSR)Pas encore d'évaluation
- Development Proposal ReportDocument37 pagesDevelopment Proposal ReportJean-Pierre RouxPas encore d'évaluation
- Drainage Pipe Unit Price AnalysisDocument9 pagesDrainage Pipe Unit Price Analysis朱叶凡Pas encore d'évaluation
- Ds B2B Data Trans 7027Document4 pagesDs B2B Data Trans 7027Shipra SriPas encore d'évaluation
- Redminote5 Invoice PDFDocument1 pageRedminote5 Invoice PDFvelmurug_balaPas encore d'évaluation
- Review Activity For The Final Test - 6 Level: 1. Match Phrasal Verbs and Match To The MeaningDocument3 pagesReview Activity For The Final Test - 6 Level: 1. Match Phrasal Verbs and Match To The MeaningGabrielle CostaPas encore d'évaluation
- Concepts of Cavity Prep PDFDocument92 pagesConcepts of Cavity Prep PDFChaithra Shree0% (1)
- Syntax - English Sentence StructureDocument2 pagesSyntax - English Sentence StructurePaing Khant KyawPas encore d'évaluation
- Soal Ulangan Harian Smester 1 Kelas 8 SMP BAHASA INGGRISDocument59 pagesSoal Ulangan Harian Smester 1 Kelas 8 SMP BAHASA INGGRISsdn6waykhilauPas encore d'évaluation
- Toe Movement - v22 Print FormatDocument10 pagesToe Movement - v22 Print FormatbensonPas encore d'évaluation
- Buckling of Thin Metal Shells 58Document1 pageBuckling of Thin Metal Shells 58pawkomPas encore d'évaluation
- 51 JointventureDocument82 pages51 JointventureCavinti LagunaPas encore d'évaluation
- TIA Portal v11 - HMI ConnectionDocument4 pagesTIA Portal v11 - HMI ConnectionasdasdasdasdasdasdasadaPas encore d'évaluation
- BLUEBOOK CITATION GUIDEDocument12 pagesBLUEBOOK CITATION GUIDEMichaela PortarcosPas encore d'évaluation
- Orbit BioscientificDocument2 pagesOrbit BioscientificSales Nandi PrintsPas encore d'évaluation
- Junior Instructor (Computer Operator & Programming Assistant) - Kerala PSC Blog - PSC Exam Questions and AnswersDocument13 pagesJunior Instructor (Computer Operator & Programming Assistant) - Kerala PSC Blog - PSC Exam Questions and AnswersDrAjay Singh100% (1)
- Situation AnalysisDocument94 pagesSituation Analysisamirafateha100% (2)
- Ass. No.1 in P.E.Document8 pagesAss. No.1 in P.E.Jessa GPas encore d'évaluation
- Heritageoil Corporategovernance AwDocument68 pagesHeritageoil Corporategovernance AwbeqsPas encore d'évaluation
- Assessment: Bipolar DisorderDocument2 pagesAssessment: Bipolar DisorderMirjana StevanovicPas encore d'évaluation
- E GCOct 2013 NsDocument0 pageE GCOct 2013 Nsvae2797Pas encore d'évaluation
- Day 3Document18 pagesDay 3SamPas encore d'évaluation
- Siege by Roxane Orgill Chapter SamplerDocument28 pagesSiege by Roxane Orgill Chapter SamplerCandlewick PressPas encore d'évaluation
- Service Manual Pioneer CDJ 2000-2 (RRV4163) (2010)Document28 pagesService Manual Pioneer CDJ 2000-2 (RRV4163) (2010)GiancaPas encore d'évaluation
- Corporation Accounting - Treasury SharesDocument4 pagesCorporation Accounting - Treasury SharesGuadaMichelleGripalPas encore d'évaluation