Académique Documents
Professionnel Documents
Culture Documents
The Tide of Antimicrobial Resistance and Selection
Transféré par
Romesh GuptaCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
The Tide of Antimicrobial Resistance and Selection
Transféré par
Romesh GuptaDroits d'auteur :
Formats disponibles
International Journal of Antimicrobial Agents 34, S3 (2009) S6 S10
The tide of antimicrobial resistance and selection
Mark H. Wilcox*
Department of Microbiology, Leeds Teaching Hospitals NHS Trust, The General Inrmary, Old Medical School, Leeds LS1 3EX, UK
ARTICLE
INFO
Keywords:
Antibiotic resistance
Selection pressure
Tigecycline
Carbapenems
Meticillin-resistant Staphylococcus
aureus
Clostridium difcile
ABSTRACT
The cumulative ecological damage, both to the individual patient and to patient populations,
secondary to antibiotic prescribing is increasingly recognised. The impact of antibiotics on
pathogens and normal ora should be a criterion for antimicrobial selection. Measures to
reduce the use of third-generation cephalosporins and uoroquinolones should be considered.
Increased reliance on carbapenems may accelerate the emergence of extremely resistant
isolates, and these antimicrobials should be restricted to key scenarios. There is a clear
need for new agents with novel modes of action and low ecological damage potential
to treat nosocomial infections. Tigecycline has a spectrum of activity that theoretically
may reduce the selection pressure for key nosocomial pathogens, and represents an
alternative to carbapenems. Further studies are needed to conrm this potentially low
selection pressure.
2009 Elsevier B.V. and the International Society of Chemotherapy. All rights reserved.
1. Antibiotic-induced ecological damage
There is clear evidence that antibiotic choice is increasingly
limited by the relentless emergence of antimicrobial resistance. The largest recent increases in resistance prevalence
have been seen in cephalosporin- and uoroquinolone-resistant
Enterobacteriaceae, and in Acinetobacter baumannii that are
resistant to almost all available antibiotics. However, this is
part of a wider phenomenon of antibiotic-induced detrimental
ecological effects. Such collateral damage includes one
or more of the following adverse effects of antibiotic
therapy: the disturbance of normal ora, potentially with
unintended consequences; the selection of drug-resistant
organisms; and colonisation or infection with multidrugresistant organisms. 1
The analogy of squeezing a balloon is sometimes used to
describe collateral damage; thus, receipt of an antibiotic
(an event on one side of the balloon) triggers a reaction
among exposed bacteria (a resultant change elsewhere).
Repeated exposure to antibiotics, either in an individual
or in a patient population, leads to an accumulation of
these trigger reactions. Cumulative antibiotic resistance
and selection pressure are analogous to the algal blooms
that occur in aquatic systems because of nutrient excess;
i.e. a tide of resistance genes and/or altered ora. This
* Tel.: +44 (0)113 392 6818; fax: +44 (0)113 343 5649.
E-mail address: Mark.Wilcox@Leedsth.nhs.uk (M.H. Wilcox).
0924-8579/ $
comparison is useful, as it emphasises the increasing ecological
cost of antibiotic prescribing resulting from selection and
resistance pressure.
It is now not uncommon to see patients colonised with
meticillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant enterococci (VRE) and multiply resistant,
extended-spectrum b-lactamase- (ESBL) producing Enterobacteriaceae, and who are at risk of Clostridium difcile
infection. A related phenomenon is the co-selection pressure
of one antimicrobial class on another (e.g. the use of
uoroquinolones being a risk factor for the selection of ESBLproducing pathogens). The most common explanation for this
phenomenon is the co-location of resistance genes on a
transposable DNA element; thus, multiple resistance genes are
acquired, despite there being only one antimicrobial resistance
selection pressure. Such effects mean that key pathogens can
typically display resistance to multiple antimicrobial classes,
as demonstrated by Table 1. 2 These European surveillance
data demonstrate that resistance to three antibiotic classes
in Klebsiella spp. is more common than to only one or two
antibiotic classes. 2 Of major concern is the accumulating
evidence for the emergence and spread of carbapenem
resistance, threatening the conventional last line of antibiotic
defence. 3 This review considers the tide of antibiotic
resistance and selection pressures that are now severely
compromising our treatment choices.
see front matter 2009 Elsevier B.V. and the International Society of Chemotherapy. All rights reserved.
M.H. Wilcox / International Journal of Antimicrobial Agents 34 (2009) S6 S10
Table 1. Resistance and co-resistance in 10 046 invasive Klebsiella
pneumoniae isolates submitted to the European Antimicrobial Resistance
Surveillance System (EARSS) in 2007 a
Resistance phenotype
Fully susceptible
Resistant to one antibiotic class
% isolates
68.4
7.9
Fluoroquinolones
3.9
Third-generation cephalosporins
2.7
Aminoglycosides
1.3
Resistant to two antibiotic classes
9.3
Fluoroquinolones + third-gen. cephalosporins
1.6
Fluoroquinolones + aminoglycosides
3.4
Third-gen. cephalosporins + aminoglycosides
Resistant to three antibiotic classes
Fluoroquinolones + third-gen. cephalosporins + aminoglycosides
4.3
14.4
14.4
100
Resistance results shown only for three antibiotic classes, as reporting of
carbapenem susceptibility was not obligatory in EARSS in 2007. 2
2. ESBL risk and antimicrobial prescribing
There has been a several-fold increase in the frequency
of cephalosporin resistance during the last decade, to
levels that now threaten the safe empirical use of these
antibiotics for severe infection. 4 In 2007 in the UK (except
Scotland), 14% and 12% of bacteraemic Klebsiella spp.
and Escherichia coli, respectively, were resistant to thirdgeneration cephalosporins, compared with 6% and 2%,
respectively, in 2000. 5 These data hide some large interhospital and inter-regional variations in resistance prevalence
resulting from clonal spread. Even higher proportions
(approximately one-third) of Enterobacter spp. and related
species are cephalosporin resistant because of the production
of derepressed b-lactamases. 5 Fluoroquinolone resistance
in E. coli over the same time period increased from
5% to 23%, 5 which has effectively curtailed the use of these
antibiotics for severe infection unless prior susceptibility
has been documented. Many studies have described the
risk factors for infection by ESBL-producing bacteria. Length
of hospital stay, severity of illness, time in the intensive
care unit, intubation and mechanical ventilation, urinary or
arterial catheterisation, and exposure to antibiotics, especially
the oxyimino b-lactams, were signicantly associated with
infection by ESBL-producing bacteria. 6,7 Similarly, Colodner
et al. 8 found that hospitalisation in the past 3 months, receipt
of antibiotics in the past 3 months, age 60 years or older,
male gender, diabetes, infection with Klebsiella spp., and
treatment with second- or third-generation cephalosporins,
uoroquinolones or penicillins were signicantly associated
with ESBL-producing isolates. Crucially, however, of all these
risk factors only the choice of antimicrobial therapy is
prospectively amenable to manipulation for a given patient,
and thus can be exploited to reduce the chance of infection
with ESBL-producing bacteria.
S7
hitherto been the role of these antibiotics. Ironically, the
threat of resistance per se increases the potential that
carbapenems are prescribed, notably in complex patients
at risk of poor outcome. For example, the Surviving Sepsis
Campaign has rightly emphasised the early prescribing of an
antibiotic as crucial for increasing the chance of survival. 9
Carbapenems have been cited as ideal antibiotics to be
used in the patient who is displaying signs of sepsis,
although these would not provide cover against MRSA, a
common nosocomial pathogen. Unfortunately, to the less
experienced prescriber, the use of a carbapenem in this
setting may erroneously be translated into a perceived need
to use these agents in any patient with potentially resistant
pathogens and/or complicated infection. Such broader-scale
prescribing, in the context of hitherto rare carbapenemresistant potential pathogens, notably Enterobacteriaceae,
Pseudomonas aeruginosa and Acinetobacter strains, will
exacerbate the selection pressure for these bacteria.
Of particular concern is the potential for rapid dissemination of carbapenem resistance. Notably, the spread
of K. pneumoniae and E. coli carrying plasmid-encoded
K. pneumoniae carbapenemase (KPC) has been reported. 10 12
In an early outbreak in New York, USA, of more than
600 K. pneumoniae that were characterised, almost half of
the isolates produced an ESBL and, of these, 3.3% were
carbapenem resistant (because of KPC-2 production). Two
hospitals experienced the rapid spread of these carbapenemresistant isolates among 58 patients. The crude 14-day
mortality in bacteraemic patients was 47%. 10 Subsequent
reports have highlighted the international occurrence of
carbapenem resistance. 3 Alerts have recently been issued in
the UK and the USA concerning the increased detection of
carbapenemase-producing bacteria. 13,14
In the UK, until the end of 2007, the Centre for Antibiotic
Resistance Monitoring and Reference Laboratory (ARMRL) in
London had only ever had eight UK isolates referred that
produced carbapenemases. This total more than doubled to
17 during 2008. 13 While these remain low numbers, there
is no place for complacency, not least because it is likely
that such isolates are far more common than this, as there
are no active surveillance schemes for carbapenemases.
Furthermore, the laboratory detection of carbapenemases
is not straightforward, and positive isolates may thus be
missed. 13,14 Of the 17 UK isolates, 16 were K. pneumoniae
(in particular two clones: ST258 and OXA-48). Most worrying,
no overseas link was identied in 12 of these 13 ; thus it would
appear that the majority of carbapenemase-producing isolates
seen in the UK are acquired and/or have their origin here.
The OXA-48 K. pneumoniae strains are only susceptible to
gentamicin, polymyxin and tigecycline.
By contrast with the relatively low numbers of carbapenemase-producing (fully carbapenem-resistant) isolates
referred to ARMRL to date, ertapenem-resistant Enterobacteriaceae are much more common (150 isolates). 13 This reects
the fact that it is biologically easier for resistance to develop
to ertapenem than to other carbapenems; production of an
ESBL coupled with impermeability secondary to porin changes
is sufcient to mediate resistance to the former.
3. Carbapenemase risk and antimicrobial prescribing
The importance of the threat of carbapenem resistance
and the selection of carbapenemase-producing bacteria is
underlined by the status of last line of defence that has
4. MRSA risk and antimicrobial prescribing
Prescribing uoroquinolones and third-generation cephalosporins provides a selection pressure for MRSA, and so, as
S8
M.H. Wilcox / International Journal of Antimicrobial Agents 34 (2009) S6 S10
these antibiotics are used more frequently, the prevalence
of MRSA in hospitalised patients increases. 15,16 Retrospective,
observational and modelling studies have described the association between MRSA and prior exposure to uoroquinolones
and cephalosporins, 15,16 but there is a lack of controlled
intervention studies to determine the effect that altering
antimicrobial prescribing has on the prevalence of MRSA. The
rate of MRSA isolation in one hospital in France decreased
signicantly, by comparison with three control hospitals, when
uoroquinolones were restricted for 1 year (32% vs. 37%
of S. aureus isolates were MRSA; odds ratio 0.82; 95% CI
0.69 0.99; P = 0.036). 17
A recent report from Switzerland examined the relationship
between MRSA incidence and both the consumption of
antibiotics and a hand-hygiene promotion campaign. 18 By using
a mathematical model to determine the effect of alcohol
hand-rub and antibiotic use on preventing and promoting,
respectively, MRSA incidence, it was estimated that these two
factors explained 57% of the variance in MRSA rates. This
nding emphasises the signicance of antimicrobial prescribing
(and conventional infection-control measures) in reducing the
risk of selecting for and disseminating nosocomial MRSA.
5. Clostridium difcile infection risk and antimicrobial
prescribing
Clostridium difcile infection (CDI) has become endemic
in many hospitals in Europe, the USA and Canada, and is
associated with excess length of stay, cost and mortality. 19
Altering antimicrobial prescribing has clearly been recognised
as a proven way to reduce the risk of CDI. Most studies
of the effectiveness of interventions to change antibiotic
prescribing are methodologically poor. 20,21 However, there is
clear evidence that restricting the use of broad-spectrum
antibiotics, specically cephalosporins or clindamycin, can
reduce CDI. 21 Crossover and long-term surveillance studies
on acute elderly medicine wards have shown that effective
restriction of third-generation cephalosporins is associated
with a reduction in incidence of CDI. 22 24
Both uoroquinolones and cephalosporins induce CDI in
a human gut model. 25,26 Conversely, neither piperacillin
tazobactam nor tigecycline cause proliferation of C. difcile
or toxin production in this model, despite clear perturbation
of gut ora secondary to their broad-spectrum activity. 27,28
The activity of piperacillin tazobactam and tigecycline (but
not uoroquinolones and cephalosporins) against common
C. difcile clones may at least partly explain this lack
of CDI induction. If an antibiotic has poor activity against
C. difcile and/or when its concentration in the gut lumen
decreases below that which will inhibit the bacteria, then
germination of C. difcile spores, if present, can occur.
Vegetative cells may then produce toxin before they enter the
next sporulation phase. It is possible that some antibiotics may
directly stimulate toxin production by C. difcile. It is also
evident that the relative resistance of a C. difcile strain to
an antibiotic may affect the population risk of selecting for
C. difcile.
The propensity of new antimicrobial agents to induce CDI
is often unclear given the limitations of prelicensing studies,
especially as these are not normally carried out in settings
endemic for C. difcile, and uncommonly include patients at
high risk of CDI. Nevertheless, clinical trial database searches
for evidence of CDI were performed on four phase 2 and
nine phase 3 studies of tigecycline. 29 CDI was very uncommon
following tigecycline administration, was associated with prior
exposure to other antibiotics, and was of a similar frequency
to that seen with comparator antibiotics (~0.2% of study
recipients). Further clinical data are desirable to conrm that
the extended broad-spectrum activity of tigecycline does not
result in increased risk of CDI.
6. Ecological damage potential affects antibiotic choice
As the consequences of the ecological damage caused by
antimicrobial therapy have become better understood, the
realisation has grown that these issues may be important
differentiators when choosing between antibiotics. Thus, the
traditional main factors that affect antibiotic choice (drug
activity, pharmacokinetics, adverse-effect prole) should be
augmented by consideration of the potential for ecological
damage. Unfortunately, this creates a complex matrix of
risk issues that should be considered. The reality is that
such complexity requires specialist advice (e.g. from medical
microbiologists or infectious disease physicians). Specialist
advice is particularly needed when choosing therapy for
the treatment of infection in patients at increased risk of
multiply antibiotic-resistant pathogens, typically because of
prior multiple antibiotic exposure, or known presence of
and/or contact with such bacteria.
However, the ecological damage caused by an antibiotic
prescription may extend far beyond the patient receiving the
drug. The potential for pathogen transmission means that
collateral damage may affect other individuals beyond the
index case, most evidently in the hospital setting. Thus,
highly transmissible bacteria and suboptimal infection control,
sometimes including insufcient capacity to isolate patients,
conspire to exacerbate the ecological damage associated with
antibiotic prescribing.
7. The (missing) antibiotic care-bundle
The recognition of the powerful effect of altering or restricting
antimicrobial prescribing in the control of CDI has not
been fully exploited to control other healthcare-associated
pathogens. Thus, conventional infection-control measures to
reduce the prevalence of healthcare-associated pathogens
have generally not included altering antimicrobial prescribing.
To their credit, Cooke and Holmes 30 coined the term missing
care-bundle when recognising this omission, in recognition
of the vogue for using healthcare bundles. These are key
elements that, when implemented together, improve the
delivery of clinical care. In the present context, optimisation
of antimicrobial prescribing can be considered to represent
the missing care-bundle to reduce the risk of healthcareassociated infection. The antibiotic care-bundle aims to
optimise treatment of the infection, and at the same time to
reduce the selective pressure for key pathogens in the index
patient and others. The antibiotic care-bundle comprises the
use of monotherapy, whenever possible, for initial (empirical)
treatment, optimising the dose and duration of antimicrobial
therapy (which requires daily review of the patient), and
performing a regular risk assessment to monitor the impact
of the antimicrobial prescribing policy (to identify special
problems that may need intervention).
M.H. Wilcox / International Journal of Antimicrobial Agents 34 (2009) S6 S10
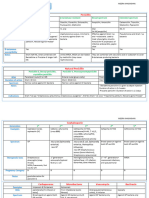
MRSA
VRE
ESBL
MDR PA
S9
C.
difficile
Carbapenems
Piperacillintazobactam
3rd generation
cephalosporins
Fluoroquinolones
Clear evidence of
selection risk
No clinical activity;
potential to select
Borderline clinical activity
and/or selection risk
Fig. 1. Potential selection risks associated with the prescribing of major antimicrobial classes. 1,21,22,24,31 35 ESBL, extended-spectrum b-lactamase; MDR-PA,
multidrug-resistant Pseudomonas aeruginosa; MRSA, meticillin-resistant Staphylococcus aeruginosa; VRE, vancomycin-resistant enterococci.
Figure 1 illustrates the complexity of issues that need to
be taken into account when considering the potential for
resistance selection. These have been considered for the major
broad-spectrum antibiotic classes, with the exception of the
glycylcycline, tigecycline. The capacity of an antibiotic to
select for resistance is determined by multiple factors. Is
the antibiotic active against the main potential pathogens?
Does it reach the site where potential pathogens either
colonise or infect the patient? What is the risk of spontaneous
(mutational) resistance, acquisition of resistance genes
(plasmids, transposons, insertion sequences) or derepression
of resistance? What are the deleterious effects of the
antibiotic on commensal bacteria that may provide resistance
to colonisation and/or expansion of potential pathogens?
Figure 1 summarises the evidence for resistance selection pressure that exists for the common antimicrobial
classes. 1,21,22,24,31 35 Using MRSA as an example, cephalosporins
(excluding the anti-MRSA cephalosporins) and uoroquinolones
lack activity against (all or most, respectively) of the common
strains. Coupled with their broad-spectrum activity against
commensal bacterial ora, this creates a selection pressure
for MRSA that is already present, or soon acquired, to
proliferate. Such theoretical potential to select for MRSA
exists for piperacillin tazobactam and carbapenems, as these
agents are inherently inactive against these bacteria. However,
there is no robust evidence to substantiate this risk, possibly
reecting the differences in the effects on key commensal
ora of piperacillin tazobactam and carbapenems compared
with cephalosporins and uoroquinolones. Resistance selection
risks are not well dened for tigecycline, given that it has not
been available as long as the other classes. Also, tigecycline
has a unique spectrum of activity that includes Grampositive resistant pathogens (including MRSA and VRE), Gramnegative resistant pathogens (including most ESBL-producing
bacteria, but excluding Pseudomonas spp., Proteus spp.,
Providencia spp. and Morganella spp.), atypical bacteria and
anaerobes. This means that the theoretical risk of selection
of resistant pathogens should be lower with tigecycline than
with other broad-spectrum antibiotic classes, possibly helped
by the option of monotherapy with tigecycline, avoiding the
use of two- or three-drug combinations that incorporate the
other major broad-spectrum antibiotic classes. Clearly, further
experience with tigecycline will be required to conrm this
theoretical potential for low resistance selection pressure.
There is a clear need for new agents with novel modes of
action and low potential to cause ecological damage for the
treatment nosocomial infections.
Funding: MHW received an honorarium for writing this
article from Wyeth Pharmaceuticals.
Competing interests: MHW has received honoraria for
consultancy work, nancial support to attend meetings
and research funding from Bayer, Genzyme, Nabriva,
Novacta, Pzer, Targanta Therapeutics, ViroPharma and
Wyeth.
Ethics approval: Not required.
References
1. Paterson DL. Collateral damage from cephalosporin or quinolone antibiotic
therapy. Clin Infect Dis 2004;38(Suppl 4):S341 5.
2. EARSS Annual Report 2007. Bilthoven, the Netherlands: European Antimicrobial Resistance Surveillance System; October 2008. http://www.rivm.nl/
earss/Images/EARSS%202007_FINAL_tcm61-55933.pdf [accessed 27 April
2009].
3. Schwaber MJ, Carmeli Y. Carbapenem-resistant enterobacteriaceae: a
potential threat. JAMA 2008;300:2911 3.
4. Pitout JD, Laupland KB. Extended-spectrum beta-lactamase-producing
Enterobacteriaceae: an emerging public-health concern. Lancet Infect Dis
2008;8:159 66.
5. Health Protection Agency. Antimicrobial resistance and prescribing in England, Wales and Northern Ireland, 2008. London: Health Protection Agency;
2008. http://www.hpa.org.uk/web/HPAwebFile/HPAweb_C/1216798080469
[accessed 27 April 2009].
6. Bradford PA. Extended-spectrum beta-lactamases in the 21st century:
characterization, epidemiology, and detection of this important resistance
threat. Clin Microbiol Rev 2001;14:933 51.
7. Graffunder EM, Preston KE, Evans AM, Venezia RA. Risk factors associated
with extended-spectrum beta-lactamase-producing organisms at a tertiary
care hospital. J Antimicrob Chemother 2005;56:139 45.
8. Colodner R, Rock W, Chazan B, Keller N, Guy N, Sakran W, et al.
Risk factors for the development of extended-spectrum beta-lactamaseproducing bacteria in nonhospitalized patients. Eur J Clin Microbiol Infect
Dis 2004;23:163 7.
9. Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, et al.
Surviving Sepsis Campaign: international guidelines for management of
severe sepsis and septic shock: 2008. Crit Care Med 2008;36:296 327.
S10
M.H. Wilcox / International Journal of Antimicrobial Agents 34 (2009) S6 S10
10. Bratu S, Landman D, Haag R, Recco R, Eramo A, Alam M, et al. Rapid spread of
carbapenem-resistant Klebsiella pneumoniae in New York City: a new threat
to our antibiotic armamentarium. Arch Intern Med 2005;165:1430 5.
11. Bratu S, Brooks S, Burney S, Kochar S, Gupta J, Landman D, et al. Detection
and spread of Escherichia coli possessing the plasmid-borne carbapenemase
KPC-2 in Brooklyn, New York. Clin Infect Dis 2007;44:972 5.
12. Urban C, Bradford PA, Tuckman M, Segal-Maurer S, Wehbeh W,
Grenner L, et al. Carbapenem-resistant Escherichia coli harboring Klebsiella
pneumoniae carbapenemase beta-lactamases associated with long-term
care facilities. Clin Infect Dis 2008;46:e127 30.
13. Health Protection Agency. Health Protection Report 2009;3(4). http://
www.hpa.org.uk/hpr/archives/2009/news0409.htm#enterora [accessed 27
April 2009].
14. Centers for Disease Control and Prevention. Guidance for control
of infections with carbapenem-resistant or carbapenemase-producing
Enterobacteriaceae in acute care facilities. MMWR Morb Mortal Wkly Rep
2009;58:256 60.
15. Wilcox MH. Antibiotic prescribing as a risk factor for MRSA. Br J Hosp Med
2005;66:180 4.
16. Tacconelli E, De Angelis G, Cataldo MA, Pozzi E, Cauda R. Does antibiotic
exposure increase the risk of methicillin-resistant Staphylococcus aureus
isolation? A systematic review and meta-analysis. J Antimicrob Chemother
2008;61:26 38.
17. Charbonneau P, Parienti JJ, Thibon P, Ramakers M, Daubin C, du Cheyron D,
et al. Fluoroquinolone use and methicillin-resistant Staphylococcus aureus
isolation rates in hospitalized patients: a quasi experimental study. Clin
Infect Dis 2006;42:778 84.
18. Vernaz N, Sax H, Pittet D, Bonnabry P, Schrenzel J, Harbarth S. Temporal
effects of antibiotic use and hand rub consumption on the incidence of MRSA
and Clostridium difcile. J Antimicrob Chemother 2008;62:601 7.
19. Rupnik M, Wilcox MH, Gerding DN. Clostridium difcile infection: new
developments in epidemiology and pathogenesis. Nature Med. Forthcoming
2009.
20. Davey P, Brown E, Fenelon L, Finch R, Gould I, Hartman G, et al.
Interventions to improve antibiotic prescribing practices for hospital
inpatients. Cochrane Database Syst Rev 2005;4:CD003543.
21. Davey P, Brown E, Fenelon L, Finch R, Gould I, Holmes A, et al. Systematic
review of antimicrobial drug prescribing in hospitals. Emerg Infect Dis 2006;
12:211 6.
22. Settle CD, Wilcox MH, Fawley WN, Corrado OJ, Hawkey PM. Prospective study
of the risk of Clostridium difcile diarrhoea in elderly patients following
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
treatment with cefotaxime or piperacillin tazobactam. Aliment Pharmacol
Ther 1998;12:1217 23.
Stone S, Kibbler C, How A, Balstrini A. Feedback is necessary in strategies
to reduce hospital acquired infection. BMJ 2000;321:302 3.
Wilcox MH. Descriptive study of intravenous immunoglobulin for the
treatment of recurrent Clostridium difcile diarrhoea. J Antimicrob
Chemother 2004;53:882 4.
Freeman J, ONeill FJ, Wilcox MH. Effects of cefotaxime and desacetylcefotaxime upon Clostridium difcile proliferation and toxin production in
a triple-stage chemostat model of the human gut. J Antimicrob Chemother
2003;52:96 102.
Saxton K, Baines SD, Freeman J, OConnor R, Wilcox MH. Effects of exposure
of Clostridium difcile PCR ribotypes 027 and 001 to uoroquinolones in a
human gut model. Antimicrob Agents Chemother 2009;53:412 20.
Baines SD, Freeman J, Wilcox MH. Effects of piperacillin/tazobactam on
Clostridium difcile growth and toxin production in a human gut model.
J Antimicrob Chemother 2005;55:974 82.
Baines SD, Saxton K, Freeman J, Wilcox MH. Tigecycline does not induce
proliferation or cytotoxin production by epidemic Clostridium difcile
strains in a human gut model. J Antimicrob Chemother 2006;58:1062 5.
Wilcox MH. Evidence for low risk of Clostridium difcile infection associated
with tigecycline. Clin Microbiol Infect 2007;13:949 52.
Cooke FJ, Holmes AH. The missing care bundle: antibiotic prescribing in
hospitals. Int J Antimicrob Agents 2007;30:25 9.
Cao B, Wang H, Sun H, Zhu Y, Chen M. Risk factors and clinical outcomes of
nosocomial multi-drug resistant Pseudomonas aeruginosa infections. J Hosp
Infect 2004;57:112 8.
Gerding DN. Is there a relationship between vancomycin-resistant
enterococcal infection and Clostridium difcile infection? Clin Infect Dis
1997;25(Suppl):S206 10.
Padiglione AA, Wolfe R, Grabsch EA, Olden D, Pearson S, Franklin C, et al.
Risk factors for new detection of vancomycin-resistant enterococci in acutecare hospitals that employ strict infection control procedures. Antimicrob
Agents Chemother 2003;47:2492 8.
Carsenti-Etesse H, Cavallo JD, Roger PM, Ziha-Zari I, Plesiat P, Garrab
e E,
et al. Effect of beta-lactam antibiotics on the in vitro development of
resistance in Pseudomonas aeruginosa. Clin Microbiol Infect 2001;7:144 51.
Carmeli Y, Eliopoulos GM, Samore MH. Antecedent treatment with different
antibiotic agents as a risk factor for vancomycin-resistant Enterococcus.
Emerg Infect Dis 2002;8:802 7.
Vous aimerez peut-être aussi
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Antimicrobial Stewardship HandbookDocument65 pagesAntimicrobial Stewardship HandbookHhaPas encore d'évaluation
- Naplex Infectiious Disease QuestionsDocument4 pagesNaplex Infectiious Disease QuestionsSARANYAPas encore d'évaluation
- Sutton - PDA .2012Document5 pagesSutton - PDA .2012Romesh GuptaPas encore d'évaluation
- Cosmetic Microbiology - A Practical ApproachDocument311 pagesCosmetic Microbiology - A Practical Approachtrantam456100% (9)
- Paint Production ProcessDocument2 pagesPaint Production ProcessRomesh Gupta100% (1)
- Drugs of choice for suspected or proved microbial pathogensDocument10 pagesDrugs of choice for suspected or proved microbial pathogensRavi Amin100% (1)
- A Study of Features Used in The DiagnosisDocument14 pagesA Study of Features Used in The DiagnosisRomesh GuptaPas encore d'évaluation
- Changes in Preservative Sensitivity For TheDocument8 pagesChanges in Preservative Sensitivity For TheRomesh GuptaPas encore d'évaluation
- Site of Action of Polymyxin On PseudomonasDocument9 pagesSite of Action of Polymyxin On PseudomonasRomesh GuptaPas encore d'évaluation
- Butyramide Utilizing MutantsDocument13 pagesButyramide Utilizing MutantsRomesh GuptaPas encore d'évaluation
- Light-Mediated Changes in Pigmentation ofDocument6 pagesLight-Mediated Changes in Pigmentation ofRomesh GuptaPas encore d'évaluation
- Our season-long test on 12 antifouls cultivates interesting resultsDocument5 pagesOur season-long test on 12 antifouls cultivates interesting resultsRomesh GuptaPas encore d'évaluation
- Antimicrob. Agents Chemother. 2011 Dec 55 (12) 5753-60, Fig. 6Document1 pageAntimicrob. Agents Chemother. 2011 Dec 55 (12) 5753-60, Fig. 6Romesh GuptaPas encore d'évaluation
- Natural Preservatives OriginalDocument33 pagesNatural Preservatives OriginalSudip GhoshPas encore d'évaluation
- Intrinsic Resistance and Unusual Phenotypes Tables v3.2 20200225Document12 pagesIntrinsic Resistance and Unusual Phenotypes Tables v3.2 20200225Roy MontoyaPas encore d'évaluation
- Antifungal Agents: LipopeptidesDocument8 pagesAntifungal Agents: LipopeptidesCristian QuitoPas encore d'évaluation
- Side Effects of VancomycinDocument20 pagesSide Effects of VancomycinSiti Hajar Mohd ZaidiPas encore d'évaluation
- Clinical review of novel anionic fluoroquinolone delafloxacinDocument13 pagesClinical review of novel anionic fluoroquinolone delafloxacinMuhammad RamzanPas encore d'évaluation
- Aerobic vs Anaerobic Bacteria: Understanding Their DifferencesDocument2 pagesAerobic vs Anaerobic Bacteria: Understanding Their DifferenceschandramohanvinPas encore d'évaluation
- Tigecycline Alone or in CombinationDocument13 pagesTigecycline Alone or in CombinationSanjay NavalePas encore d'évaluation
- Tetracyclines, Macrolides & OthersDocument3 pagesTetracyclines, Macrolides & OthersJaybee SarmientoPas encore d'évaluation
- AntibioticsDocument9 pagesAntibiotics7aith22Pas encore d'évaluation
- Tetracycline's: Jagir R. Patel Asst Prof Dept. Pharmacology Anand Pharmacy CollegeDocument21 pagesTetracycline's: Jagir R. Patel Asst Prof Dept. Pharmacology Anand Pharmacy CollegeJagirPas encore d'évaluation
- Microbewiki - Kenyon.edu Index - PHP Enterobacter CloacaeDocument4 pagesMicrobewiki - Kenyon.edu Index - PHP Enterobacter Cloacaehari.suryanto8417Pas encore d'évaluation
- IDSA Guidelines for Managing Complicated Intra-abdominal InfectionsDocument32 pagesIDSA Guidelines for Managing Complicated Intra-abdominal InfectionsSylvain ColluraPas encore d'évaluation
- 6811 PDFDocument11 pages6811 PDFMaileth Carolina Anillo ArrietaPas encore d'évaluation
- 31041313Document10 pages31041313carolinapolotorresPas encore d'évaluation
- AntibiotikDocument10 pagesAntibiotikmayaPas encore d'évaluation
- DVM Achu MercyDocument70 pagesDVM Achu MercynjonjichakunteoliverPas encore d'évaluation
- Jurnal Antibiotik Resistensi Pada Kasus OMSKDocument10 pagesJurnal Antibiotik Resistensi Pada Kasus OMSKAnonymous a2nxIq5Pas encore d'évaluation
- Acinetobacter BaumanniiDocument12 pagesAcinetobacter BaumanniiKenneth Smith IIPas encore d'évaluation
- Antibiotic Resistance in Diabetic Foot Soft Tissue Infections: A Series From GreeceDocument5 pagesAntibiotic Resistance in Diabetic Foot Soft Tissue Infections: A Series From GreeceBelinda AngelPas encore d'évaluation
- Evaluation of Bacterial Agents Isolated From Aspirate Cultures of Covid 19 General Intensivecare Patients Compared To Pre Pandemic ConditionsDocument8 pagesEvaluation of Bacterial Agents Isolated From Aspirate Cultures of Covid 19 General Intensivecare Patients Compared To Pre Pandemic ConditionsRicardo ZúñigaPas encore d'évaluation
- Guoying Wang, Guo ZhaoDocument17 pagesGuoying Wang, Guo ZhaoHQ HQPas encore d'évaluation
- Artigo Produtos NaturaisDocument39 pagesArtigo Produtos NaturaisMillygoPas encore d'évaluation
- Antimicrobial Agents and Chemotherapy-2016-Oshima-e02056-16.fullDocument9 pagesAntimicrobial Agents and Chemotherapy-2016-Oshima-e02056-16.fullI Made AryanaPas encore d'évaluation
- 26 Tetracyclines Glycylcyc 2015 Mandell Douglas and Bennett S PrincipleDocument24 pages26 Tetracyclines Glycylcyc 2015 Mandell Douglas and Bennett S PrincipleHelen DyPas encore d'évaluation
- Sun 2015Document10 pagesSun 2015sarah assegafPas encore d'évaluation
- Drug Bug TableDocument1 pageDrug Bug TableLes SangaPas encore d'évaluation
- Discromii 1Document4 pagesDiscromii 1defineyoung5Pas encore d'évaluation
- Antibiotics for Pneumonia Treatment GuidelinesDocument52 pagesAntibiotics for Pneumonia Treatment GuidelinesAndy DazPas encore d'évaluation