Académique Documents
Professionnel Documents
Culture Documents
"Scared Stiff": Catatonia As An Evolutionary-Based Fear Response
Transféré par
eduardobar2000Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
"Scared Stiff": Catatonia As An Evolutionary-Based Fear Response
Transféré par
eduardobar2000Droits d'auteur :
Formats disponibles
Psychological Review
2004, Vol. 111, No. 4, 984 1002
Copyright 2004 by the American Psychological Association
0033-295X/04/$12.00 DOI: 10.1037/0033-295X.111.4.984
Scared Stiff: Catatonia as an Evolutionary-Based Fear Response
Andrew K. Moskowitz
University of Auckland
Catatonia, long viewed as a motor disorder, may be better understood as a fear response, akin to the
animal defense strategy tonic immobility (after G. G. Gallup & J. D. Maser, 1977). This proposal,
consistent with K. L. Kahlbaums (1874/1973) original conception, is based on similarities between
catatonia and tonic immobility (death feint) as well as evidence that catatonia is associated with anxiety
and agitated depression and responds dramatically to benzodiazepines. It is argued that catatonia
originally derived from ancestral encounters with carnivores whose predatory instincts were triggered by
movement but is now inappropriately expressed in very different modern threat situations. Found in a wide
range of psychiatric and serious medical conditions, catatonia may represent a common end state response
to feelings of imminent doom and can serve as a template to understand other psychiatric disorders.
Catatonia is clearly one of the most perplexing of all psychiatric
syndromes. For no apparent reason, a person may become mute,
freeze for minutes or hours on end without any discernable awareness of the outside world, appear seemingly impervious to pain,
and allow their limbs to be bent in all sorts of awkward positions.
How can such a strange response, found in a wide range of
psychiatric and medical conditions, be understood? Is it simply due
to something having gone terribly wrong in the persons brain,
perhaps in areas responsible for movement? Or is the response one
that has been bred into the human species for generations on end
but was designed to deal with very different situations from the
ones in which it is currently expressed? Although these are clearly
not mutually exclusive possibilities, it is the latter perspective,
rarely considered, that will be emphasized here.
like facies, the eyes focused at a distance; he seems devoid of any will
to move or react to any stimuli; there may be fully developed waxen
flexibility, as in cataleptic states, or only indications, distinct, nevertheless, of this striking phenomenon. The general impression conveyed
by such patients is one of profound mental anguish, or an immobility
induced by severe mental shock. (Kahlbaum, 1874/1973, p. 8)
As is obvious from the above quotes, Kahlbaum (1874/1973)
was not unaware that persons with catatonia gave the appearance
of having been frightened. Indeed, an alternate translation of the
same passage, quoted (but not referenced) in Goldar and Starkstein
(1995), reads: All in all, these patients give the impression of the
deepest mental pain, of being frozen after a great fright (p. 202).
In a milder form, of course, this experience is not unknown to the
general population, as reflected in the common expression being
scared stiff.
The thesis that catatonia may primarily be a fear reaction,
closely related to the animal defense strategy tonic immobility (TI;
immobility characterized by muscular tension), is not a new one.
Although TI has occasionally been referred to as catatonic in the
animal literature (as opposed to the more common usage of cataleptic) and proposed in passing as a potential model for catatonia
(Klemm, 1971; Svorad, 1957), the first (and only) sustained exploration of the relation between these two conditions was
mounted in 1977 by animal researcher Gordon Gallup and psychiatrist Jack Maser.1 Noting the numerous behavioral parallels between TI and catatonia (such as immobility, decreased vocalization, analgesia, waxy flexibility, and evidence of alertness), they
concluded that catatonia could contain evolutionary-based fragments
of primitive defenses against predators that now misfire under conditions of exaggerated stress (Gallup & Maser, 1977, p. 357).
This position was later taken up by Perkins, who, in a 1982
article entitled Catatonia: The Ultimate Response to Fear?, characterized catatonia as a primitive form of expression released
under conditions of extreme stress. Subsequently, Orland and
Historical Overview
The concept of catatonia originated with the German physician
Karl Kahlbaum, who coined the term in 1869 and described it in
detail in his 1874 monograph Die Katatonia oder das Spannungsirresein, which has been translated as Catatonia or the TensionInsanity (Mora, 1973). Kahlbaum (1874/1973) based the concept
of catatonia on a previously described condition, melancholia
attonitaastonished or thunderstruck melancholiaso-called
because of the astonished expression often seen on sufferers faces
(Goldar, 1988; J. Johnson, 1984). He viewed catatonia as a progressive disorder with strong links to affective and organic conditions, usually beginning with a change of mood but sometimes
starting abruptly, particularly after very severe physical or mental
stress . . . [such as] a very terrifying experience (Kahlbaum,
1874/1973, p. 31). Kahlbaum described the primary characteristics
of catatonia as follows:
The typical signs . . . may be described as a state in which the patient
remains entirely motionless, without speaking, and with a rigid, mask-
Correspondence concerning this article should be addressed to Andrew
K. Moskowitz, Department of Psychology, University of Auckland,
Private Bag 92019, Auckland, New Zealand. E-mail: a.moskowitz@
auckland.ac.nz
Even so, Gallup and Masers (1977) contribution is primarily about TI.
Just a small portion of the chapter is dedicated to a discussion of catatonia,
and only seven references on catatonia, three from prior to 1950 and one
from a textbook, are cited.
984
CATATONIA AS A FEAR RESPONSE
Daghestani (1987), in a case study, raised the possibility that
organically based catatonias could be psychological reaction(s) to
overwhelming fear and the stress of the organic brain disease state
itself (p. 490). Berrios (1981), reviewing the historical concept of
stupor (one of the core components of catatonia), wondered
whether it might be a vestigial ethological response (p. 474) and
proposed freezing in animals as a research model. Finally, Krystal
(1993) argued that catalepsy or catatanoid reactions seen in humans under conditions of profound helplessness were akin to
animal immobility, both of which he characterized as surrender
responses in the face of unavoidable danger.
However, none of these writings appears to have had much
influence on the concept of catatonia. The notion of catatonia as a
fear reaction has been given short shrift, as the view of catatonia
as a motor disorder remains overwhelmingly dominant. As an
indication of this, Perkinss (1982) article has been cited only once
in the 20 years since its publication (by Orland & Daghestani,
1987) according to the Social Sciences Citation Index (which
references only articles and hence not Gallup & Masers, 1977,
contribution). Although Perkinss article is largely a review of
several case studies, this lack of citation no doubt reflects limited
interest in the question posed by his title. As this thesis, appearing
in various forms over the past 25 years, has generated so little
interest, why should it be reconsidered now? There are a number
of compelling reasons to do so.
First, the last 15 years has seen a resurgence of interest in
catatonia, with the resulting developments:
1.
Catatonia is no longer viewed solely as a subtype of
schizophrenia. Rather, it is now seen as a largely nonspecific syndrome, present in close to 10% of psychiatricprimarily affectively disorderedinpatients (Taylor
& Fink, 2003) and appearing in a wide range of serious
medical conditions (Carroll, Kennedy, & Goforth, 2000;
Fink, 2001; Fink & Taylor, 2003; Peralta, Cuesta, Serrano, & Martinez-Larrea, 2001; Pfuhlmann & Stoeber,
2001). This is reflected in the inclusion of catatonia as a
modifier for both affective disorders and medical conditions as well as a subtype of schizophrenia in the Diagnostic and Statistical Manual of Mental Disorders (4th
ed.; DSMIV; American Psychiatric Association, 1994).
2.
Benzodiazepines (BZs) have been found to be extremely
effective in treating catatonia, in some cases completely
relieving symptoms within a matter of minutes (Bush,
Fink, Petrides, Dowling, & Francis, 1996b; Schmider,
Standhart, Deuschle, Drancoli, & Heuser, 1999; Ungvari,
Kau, Wai-Kwong, & Shing, 2001). Although the mechanisms underlying this response have been debated
(Menza & Harris, 1989), it appears most likely that it is
the powerful antianxiety properties of BZs (as opposed to
their anticonvulsant or muscle relaxant properties, for
example) that are implicated (Northoff, Steinke, et al.,
1999; Northoff et al., 1995; Rosebush & Mazurek, 1999).
3.
The subjective state of many persons undergoing catatonic experiences is reported to be one of intense anxiety
(Northoff, Krill, et al., 1998; Rosebush, Hildebrand, Furlong, & Mazurek, 1990; Rosebush & Stewart, 1989);
985
despite their apparent unresponsiveness, they often have
a surprising level of awareness of events going on around
them (Rosebush & Mazurek, 1999).
In addition, recent research on catatonia has revealed further
areas of overlap with TI in animalssuch as frontal dysfunction
(Klemm, 1971; Northoff, 2002; Taylor, 1990)not previously
noted. Advances in understanding the role of the orbitofrontal
cortex, specifically implicated in catatonia (Northoff, 2002), in
regulating affect and emotionally driven behavior is also of relevance, as is Porgess (1995, 1997, 2001) polyvagal theory of the
role of the vagus nerve and autonomic nervous system in regulating emotion, conflict, and communication. Finally, the burgeoning
field of evolutionary psychology and psychiatry, and in particular
evolutionary factors proposed to underlie depressive disorders,
provides an appropriate framework for such an exploration (Brune,
2002; Buss, 1995; Dixon, 1998; Gilbert, 2001; Gilbert & Allan,
1998; Jones & Blackshaw, 2000). Thus, the time appears right for
a reconsideration of the role of fear in catatonia, with special focus
on its relation to the animal defense strategy TI.
Initial Formulation
The thesis put forward here is that catatonia is a relic of ancient
defensive strategies, developed during an extended period of evolution in which humans had to face predators in much the same
way many animals do today and designed to maximize an individuals chances of surviving a potentially lethal attack. It is
argued that catatonic episodes reflect an inappropriate expression
of these strategies, primarily in situations in which the individual
feels himself or herself to be under profound threatfrom either
internal (i.e., toxic reactions) or external sources.
Specifically, it is proposed that different components of catatonia are differentially related to particular animal defense strategies.
Thus, the core catatonic symptoms of stupor, mutism, and immobility are directly linked to TI. However, catatonia, as it is currently formulated, consists of more than just these symptoms,
which make up catatonic stupor (also called akinetic or retarded
catatonia). Catatonic excitement (apparently purposeless agitation
not influenced by external stimuli; American Psychiatric Association, 2000, p. 764) is not infrequently seen, as are behavioral or
communicative abnormalities such as repeating an examiners
movements or statements (echopraxia or echolalia) or negativism
(apparently motiveless resistance to instructions or attempts to be
moved; American Psychiatric Association, 2000, p. 765). It is
proposed that catatonic excitement (or hyperkinetic catatonia),
although not directly related to TI, is related to the sympathetically
mediated fightflight responses that typically precede or follow
TI.2 The remaining associated features, which I have termed
behavioral communicative symptoms, although having no direct
2
For the purposes of consistency and historical continuity, I use the
terms catatonic stupor and catatonic excitement throughout, except when
referencing other authors, despite the slight confusion entailed by the
former concept including symptoms of mutism and immobility along with
the symptom of stupor. The latter is defined as unresponsiveness, hypoactivity, and reduced or altered arousal (Fink & Taylor, 2003, p. 20).
Although stupor typically co-occurs with mutism and immobility, mutism
may occur without stupor (Fink & Taylor, 2003).
MOSKOWITZ
986
analogue in animal defense strategies, are nonetheless not inconsistent with the proposed model. They may represent primitive
attempts at communication or submissive behavior (a form of
defense) consistent with a regression to fightflight and immobility defense strategies. Indeed, the capacity to use more sophisticated forms of human interaction and communication may be lost
when such forms of defense are engaged (Porges, 1997).
Although the catatonic stuporTI connection forms the central
argument of this article, the other components of catatonia are also
important. The model, including a discussion of all three components, is presented in detail following a discussion of animal
defense reactions, evolutionary psychology, and recent research on
catatonia.
Evolutionary Perspectives
Animal Defense Reactions of Immobility
TI is one of several animal defense reactions that have been
documented for hundreds of years (Ratner, 1967). In addition to
the classic fightflight response, the most familiar of defense
reactions, animals may also freeze in response to danger (Ratner,
1967). This freezing takes two forms, which have been contrasted
as freezing and immobility (Ratner, 1967) or attentive and tonic
immobility (Marks, 1987).
TI (or unresponsive immobility) has been defined by Marks
(1987) as the sudden onset of prolonged stillness and decreased
responsivity in a previously active animal in the face of threatening
stimulation (p .60). Documented since the 17th century, TI was
known as animal hypnosis for a long time, mistakenly linked to the
phenomenon of hypnosis in humans (Gallup & Rager, 1996;
Ratner, 1967). It is now well established as a fear response, which
can be elicited in a wide range of vertebrates and invertebrates,
ranging from arthropods to fish, amphibians, reptiles, birds, and
mammals (including monkeys; Hennig, 1978; Holcombe, Sterman, Goodman, & Fairchild, 1979), and is established most easily
through some form of restraint or physical inversion (Gallup,
1977; Ratner, 1967). Some have previously argued for its presence
in humans as well, in immobility responses seen in some rape
cases (Galliano, Noble, Travis, & Puechl, 1993; Suarez & Gallup,
1979) and airline disasters (D. Johnson, 1984, cited in Gallup &
Rager, 1996), both of which include components of strong fear and
physical restraint, considered central to eliciting TI (Gallup &
Rager, 1996). Nonetheless, although restraint typically involves
physical containment, TI can be induced without any tactile pressure on the organism, leading Ratner (1967) to argue it is the
perception of entrapment, with or without physical restraint, that is
most important.
TI is characterized most prominently by a lack of movement,
which can last, depending on the species and the situation, from a
few seconds to many hours (Gallup, 1977). During this time, the
animal maintains an unusual posture, with muscular rigidity and
waxy flexibility of limbs. Vocal behavior is typically suppressed,
and the animal is unresponsive to even intense or painful stimulation (Gallup & Rager, 1996; Ratner, 1967). TI is presumed to
have developed because many predators are triggered by movement and lose interest when their prey remains motionless for a
period of time. This strategy increases the chances of animals
escaping alive (Ewell & Cullen, 1981; Sargeant & Eberhardt,
1975; Thompson et al., 1981). In addition, some predators, such as
hawks, actively avoid eating dead meat and thus may refrain from
eating an animal that appears to be dead (Marks, 1987).
Although TI is sometimes loosely called freezing, it should be
distinguished from attentive immobility, for which the term freezing is more appropriately reserved (Marks, 1987; Ratner, 1967).
Attentive immobility is primarily a transient defense strategy,
preliminary to fighting or fleeing, in which the animal stops
moving to avoid detection and shifts resources to perceptual and
executive functions to better locate the predator and plan escape. A
classic example of attentive immobility would be antelopes freezing and pricking up their ears on the African veldt at the first sign
of a lions approach. In contrast to TI, the freezing animal is highly
responsive to stimuli, such as touch, and remains in the alert
posture typical for that species (Marks, 1987); in TI, the posture,
which may be held for long periods of time, often appears bizarre,
and the animal is unresponsive to even painful stimulation (Gallup
& Rager, 1996; Ratner, 1967).
In contrasting TI and attentive immobility, Ratner (1967) proposed that their expression is a function of the distance between
predator and prey, a concept he refers to as defensive distance. 3
Specifically, Ratner stated that the initial response of potential prey
when a predator is first detected is to freeze. Then, having identified the danger and calculated the best means to escape, the
animal typically flees. If it is unable to successfully flee and the
predator is upon it, it will initially fight. However, when there is
clearly no chance for successfully fleeing or fighting, the animal
may resort to TI, in the hope that the predator will lose interest.
Should the opportunity then present itself, the animal will attempt
to escape.
Evolutionary Psychology and Psychiatry
It is noteworthy that Kahlbaum (1874/1973) himself had a
strong interest in Darwin and came to believe that psychiatric
research should be based on evolutionary grounds (Brune, 2000).
More recently, there have been arguments for an evolutionarybased definition of mental disorder (Wakefield, 1992, 1999), calls
for psychiatry to adopt an evolutionary framework (Brune, 2002;
Jones & Blackshaw, 2000), and evolutionary explanations for
anxiety disorders (Marks & Nesse, 1994) and depression (Gilbert,
2001; Gilbert & Allan, 1998). Indeed, interest has grown in this
area to such an extent that an entire recent issue of the British
Journal of Medical Psychology (Gilbert, 1998) was dedicated to
evolutionary approaches to psychopathology.
One of the basic tenets of evolutionary psychology is that
biological evolution, as reflected by changes in our genetic structure, lags far behind cultural and societal evolution (Nesse &
Williams, 1994; Tooby & Cosmides, 1990). As such, physical and
mental disorders can result from a mismatch between the environments in which behaviors were developed and the current
environment in which they are expressed (Cosmides & Tooby,
1999; Nesse & Williams, 1994). In the case of catatonia, the
argument would be that this reaction developed to deal with
situations in which our ancestors found themselves on a regular
basis, namely, face to face with a predator. As the failure to
3
This is also known as predatory imminence (Fanselow & Lester, 1988).
CATATONIA AS A FEAR RESPONSE
develop effective coping mechanisms in such situations would
lead to likely death, it is easy to see why there would be strong
selection pressures favoring those genes coding for effective strategies, such as TI. Further, such genetic adaptations would likely
include high tolerance for false positives; the consequences of
mistakenly responding with a fear response to an innocuous situation are far outweighed (evolutionarily) by the adaptive consequences of not responding to a genuine danger situation (Nesse &
Williams, 1994). Nesse (2001) has referred to this as the smoke
detector principle (p. 75).
Tooby and Cosmides (1990) considered the emotions generated
in such situations as crucially important, arguing that they carry
signals or codes for the expression of behavioral programs developed in our ancestral past; the operation of human psychological
mechanisms are orchestrated by emotions that frame present circumstances in terms of the evolutionary past (p. 420).
There is clear behavioral evidence of such relics in some human
responses to fear and danger. Perhaps most obvious in this regard
is piloerection: the hair on the nape of our necks standing up when
we are frightened or enraged. Although this serves no obvious
adaptive purpose in humans, it allows other species, such as
canines, to appear larger and more imposing to opponents. Likewise, Marks (1987) argued that stranger anxiety is largely a relic
from our developmental history or from the history of species
phylogenetically related to us, in which infants were at risk of
being killed by strange males hoping to induce ovulation in their
mother.
Among anxiety disorders, both phobias and panic disorder have
been linked to evolutionary forces. Several researchers have argued that phobias, which tend to cluster around themes of animals
(particularly spiders and snakes), social situations, blood or injuries, and open spaces, represent common danger cues in human
evolution (Ohman, 1992; Seligman, 1971). Likewise, panic disorder, in one prominent theory, is proposed to result from the
misfiring of an evolutionary-based suffocation alarm (Klein,
1993).
Most important for this thesis, depression has been hypothesized
to relate to animal defense responses in general and TI in particular
(Dixon, 1998; Gilbert & Allan, 1998). In this formulation, TI (or
in Dixons, 1998, term, arrested flight)4 is linked with aspects of
depression, such as social withdrawal, reduced eye contact, and
psychomotor retardation (Dixon, 1998; Gilbert & Allan, 1998).
Dixon (1998) characterized arrested flightTI as a last resort
defense strategy triggered by conditions of inescapable proximal
threat and characterized by cryptic immobile postures, a lack of
overt surveillance, and cutoffs. This latter behavior is designed to
minimize aversive stimulation (i.e., the predator), thereby reducing
arousal levels, and is typically manifested by the threatened animal
closing its eyes or averting its head. Dixon considered arrested
flightTI to be the behavioral hallmark of the severely depressed
individual (p. 436). Gilbert and Allan (1998) have argued that this
link is mediated by feelings of entrapment and defeat, concepts
which they have found, in a sample of students and depressed
individuals, to more strongly predict depression than the concept
of helplessness; the latter does not convey what they consider
central to the phenomenology of depressiona strong motivation
for flight that is blocked by internal or external factors.
Thus, several forms of anxiety and depression have been linked
to ancestral conditions from which they may have derived. Could
987
catatonia be another, perhaps more direct, link? To answer this
question, a brief review of catatonia and TI is required.
An Overview of Catatonia
Catatonic behavior is defined in the Diagnostic and Statistical
Manual of Mental Disorders (4th ed., text rev.; American Psychiatric Association, 2000) as the following:
Marked motor abnormalities including: [1] motoric immobility (i.e.,
catalepsy or stupor), [2] certain types of excessive motor activity
(apparently purposeless agitation not influenced by external stimuli),
[3] extreme negativism (apparently motiveless resistance to instructions or attempts to be moved) or mutism, [4] posturing or stereotyped
movements, and [5] echolalia or echopraxia. (pp. 764 765; numerals
added; reprinted with permission from the Diagnostic and Statistical
Manual of Mental Disorders, 4th ed., text. rev., Copyright 2000 by the
American Psychiatric Association)
Catalepsy is the maintenance of postures, often odd in appearance,
for long periods of time; whereas stupor is unresponsiveness,
hypoactivity, and reduced or altered arousalapparent analgesia
to painful stimuli may be present in severe cases (Fink & Taylor,
2003). Echolalia and echopraxia involve the copying or mimicking of the examiners utterances or movements, respectively. In the
DSMIV, two of the above symptom clusters are required for
catatonic schizophrenia or affective disorders with catatonic features, whereas only one is required for catatonic features due to a
medical condition.
There has been a recent proliferation of scales and approaches
for diagnosing catatonia (Braeunig, Krueger, Shugar, Hoeffler, &
Boerner, 2000; Bush, Fink, Petrides, Dowling, & Francis, 1996a;
Fink & Taylor, 2003; Northoff, Koch, et al., 1999; Peralta &
Cuesta, 2001). The closest to the DSMIV approach would be that
of Bush et al. (1996a) and Peralta and Cuesta (2001), who require
two or three symptoms, respectively, from among those listed in
the DSMIV or others, including verbigeration (repetition of
phrases or sentences), mannerisms (odd, apparently purposeful
movements), or waxy flexibility (initial resistance followed by
submission to limbs being repositionedlikened to the bending of
a warm candle). As can be noted, some signs of catatonia
immobility, posturing, mutism, or excitement, for example can
be observed, whereas otherssuch as waxy flexibility, echolalia,
or negativism can only be demonstrated through interaction with
others.
Fink and Taylor (2003), who have long argued for the acceptance of catatonia as a distinct diagnostic entity (see Fink &
Taylor, 1991), took a different tack, distinguishing between different forms of catatonia. Their criteria are:
A.
Immobility, mutism, or stupor of at least 1 hr duration,
associated with at least one of the following: catalepsy,
automatic obedience, or posturing, observed or elicited
on two or more occasions.
Dixons (1998) description of arrested flight leaves little doubt that he
is describing the same phenomenon as TI. He prefers the term arrested
flight to emphasize that this condition arises in situations in which the
animal wishes to escape but cannot, as all escape routes are blocked.
MOSKOWITZ
988
B.
In the absence of immobility, mutism, or stupor, at least
two of the following, which can be observed or elicited
on two or more occasions: stereotypy, echophenomena,
catalepsy, automatic obedience, posturing, negativism,
or ambitendency (Fink & Taylor, 2003, p. 116).
Automatic obedience is defined as an exaggerated cooperation with the examiners request, whereas ambitendency is
appearing motorically stuck in indecisive, hesitant movements (Bush et al., 1996a, p. 135).5 Fink and Taylor (2003)
allowed for three subtypes of catatonia to be generated from
these criteria. Retarded or akinetic catatonia (which they refer
to as nonmalignant catatonia) is characterized by the A criteria
above, excited catatonia (or delirious mania in their terminology) consists of the B criteria above plus severe mania or
excitement, and malignant catatonia consists of the A criteria
plus fever and autonomic instability (Fink & Taylor, 2003). In
so doing, they sensibly distinguished between the form of
catatonia excited or retardedand the seriousness or level of
riskmalignant (or lethal) or nonmalignant (or benign).
Their approach also emphasizes the centrality of immobility,
mutism, and stupor to a diagnosis of catatonia. These symptoms
have consistently been found to be the most common in catatonic
populations (Bush et al., 1996a; Morrison, 1973; Peralta & Cuesta,
2001; Rosebush et al., 1990). Most factor analytic studies conducted on catatonic symptoms confirm Fink and Taylors (2003)
approach, finding factors corresponding to stupor, mutism, and
immobility on the one hand (unrelated to diagnosis) and other
catatonic symptoms (including excitement or correlated with excitement or mania) on the other (Abrams, Taylor, & Coleman
Stolurow, 1979; Peralta et al., 2001; Starkstein et al., 1996).6
Although some had thought catatonia to be quite rare (Mahendra,
1981), four recent well-designed studies found prevalence rates of
between 7% and 9% on acute inpatient psychiatric units (Bush et
al., 1996a; Peralta & Cuesta, 2001; Rosebush et al., 1990; Ungvari,
Leung, Wong, & Lau, 1994).
Catatonia has been the subject of numerous reviews over the last
30 years, most of which were published since 1990, demonstrating
renewed interest in the disorder (Clark & Rickards, 1999; Fink,
1997; Fink & Taylor, 1991, 2001; Gelenberg, 1976; L. R. Gjessing, 1974; Goldar & Starkstein, 1995; J. Johnson, 1993; Peralta,
Cuesta, Serrano, & Mata, 1997; Pfuhlmann & Stoeber, 2001; Ries,
1985; Taylor & Fink, 2003). Indeed, this resurgence of interest
appears to be accelerating, as the last few years have seen an entire
journal issuethe European Archives of Psychiatry and Clinical
Neurosciences (Stoeber & Ungvari, 2001) dedicated to catatonia, the publication of a Behavioral and Brain Sciences review
(Northoff, 2002), and the release of two major books related to
catatonia (Fink & Taylor, 2003; Mann, Caroff, Keck, & Lazarus,
2003).
This renewal of interest revolves primarily around four areas:
(a) the appropriate placement of catatonia in psychiatric nosology,
(b) the relationship among catatonia, lethal catatonia, and neuroleptic malignant syndrome (NMS), (c) the treatment of catatonia
with BZs and/or electroconvulsive therapy (ECT), and (d) brain
functioning and neurochemistry. These issues, along with the
phenomenology of catatonia, are discussed in turn.
Catatonias Placement in Psychiatric Nosology
The history of the concept of catatonia has been well reviewed
elsewhere (Berrios, 1981; Gelenberg, 1976; Goldar & Starkstein,
1995; J. Johnson, 1993) and is not discussed in detail here. Briefly,
Kahlbaum (1874/1973) believed that catatonia was an organically
based degenerative condition, similar to general paresis, which
passed through a number of largely affective phases ultimately
leading to dementia. He thought the typical pattern to be an initial
melancholia, followed by mania (also described as rage, frenzy,
and excitement) and then stupor, but noted that the stuporous phase
could progress directly from melancholia, or even out of the
blue, after particularly severe stress. Stressors, according to Kahlbaum, were not uncommon antecedents to catatonia and could
include the death of a loved one, conflictual relationships, or
financial problems.
Ignoring Kahlbaums (1874/1973) association of catatonia with
affective conditions, Kraepelin (1899) co-opted it into his dementia praecox construct. Later, Bleuler (1911/1950) included it as a
component of schizophrenia. Despite protests that catatonia was
linked to affective conditions (Hoch, 1921; Kirby, 1913), it was
widely viewed as pathognomic for schizophrenia for most of the
20th century, appearing only as a subtype of schizophrenia for all
editions of the American Psychiatric Associations Diagnostic and
Statistical Manual of Mental Disorders until the publication of the
DSMIV in 1994 (American Psychiatric Association, 1994). The
change in the DSMIV, which allowed for the presence of catatonia in affective disorders and medical conditions, followed a series
of publications in which catatonia was found more commonly in
affective disorders than in schizophrenia (Abrams & Taylor, 1976;
Abrams et al., 1979; Gelenberg, 1976; J. Johnson, 1984; Morrison,
1973; Ries, 1985)7 and in a wide range of serious medical conditions, including various neurological conditions (such as encephalitis), toxic conditions, metabolic disorders, and idiosyncratic
responses to drugs or medications (Barnes, Saunders, Walls, Saunders, & Kirk, 1986; Carroll, 1992; Gelenberg, 1976; Popkin &
Tucker, 1992). Early reviews suggested that the syndrome of
catatonia was expressed similarly whether it was associated with
various psychiatric disorders or with medical conditions (Fein &
McGrath, 1990; Gelenberg, 1976). A recent exhaustive review by
Carroll et al. (2000) confirmed this perception, concluding that
5
Of note, in an approach dating back to Kraepelin (1899), Bush et al.
(1996a) recommended that automatic obedience be tested by asking the
person to stick out their tongue so the examiner can stick a pin in it.
Ambitendency is tested by the examiner extending his or her hand and
firmly stating, Do not shake my hand!
6
However, there is also evidence that catatonia as a whole, including
retarded and excited components, can be thought of as a syndrome. Abrams
and Taylor (1976) found neither the subtype of catatonia (excited vs.
retarded) nor the number of symptoms predictive of either associated
diagnosis or treatment response, and Oulis et al. (1997) found evidence for
one factor underlying both excited and retarded forms of catatonia.
7
Whereas early studies emphasized a link between catatonia and mania
(Abrams & Taylor, 1976; Abrams et al., 1979), more recent studies have
found that catatonia in mania is overwhelmingly associated with mixed
manic states (admixtures of mania and depression or rapid fluctuations in
mood; Braeunig, Krueger, & Shugar, 1999; Krueger & Braeunig, 2000).
This suggests that it may be the depressive component of both manic and
depressive disorders that is linked with catatonia.
CATATONIA AS A FEAR RESPONSE
psychiatric and medical catatonias are essentially indistinguishable
from each other.
NMS and LethalMalignant Catatonia
NMS is a potentially lethal condition, characterized by severe
akinesia, muscular rigidity, autonomic dysfunction, and fever,
occurring after treatment with neuroleptic (antipsychotic) medications. A mortality rate of 19% has been reported (76% in cases
reported prior to 1970), most strongly associated with cardiovascular collapse or arrhythmias (Caroff, 1980) or renal failure (Shalev, Hermesh, & Munitz, 1989). It was originally felt to be an
idiosyncratic toxic reaction to medications, sharing some symptoms with, but distinct from, catatonia (Caroff, 1980). However, in
1986, Mann et al. conducted an exhaustive historical review of
so-called lethal catatonia, drawing similarities to NMS.
Lethal catatonia had been described since the early 1830s as a
condition with no clear medical etiology, characterized typically
by extreme hyperactivity followed by stuporous exhaustion (or
occasionally only stupor without hyperactivity), with fever and
autonomic instability (Ljubisavlijevic & Schneider, 2002; Mann et
al., 2003). It could develop in a wide range of organic and
functional conditions, including various psychiatric disorders, cerebrovascular disorders, tumors, head trauma, infections, metabolic disorders, toxic disorders, and seizure disorders (Mann et al.,
2003).
The mortality rate has improved over the years, from 75%
100% in the historical (pre-1960) series to 62% in cases reported
between 1960 and 1986 (Mann et al., 1986). Most dramatically,
the rate has fallen to 9% for cases reported since 1986. This
substantial decrease in mortality, attributed to timely and appropriate interventions (Mann et al., 2003), has led some to propose
the term lethal be replaced with the term malignant (Fink &
Taylor, 2003; Mann et al., 2003).
Causes of death in early cases, typically occurring during a
stuporous phase with extreme hyperthermia, have been attributed
to cardiovascular collapse (Mann et al., 1986), vagal hypotonia
and cardiac arrest (Billig & Freeman, 1944; Shulack, 1944, cited
in Mann et al., 1986), or adrenocortical insufficiency due to
mental and physical stress (Lingjaerde, 1963, cited in Mann et al.,
1986). Of the more recent cases of death, negative results have
been found in almost 80% of the autopsies, leading Mann et al.
(2003) to characterize them as psychogenic in nature.
The relationship between NMS and malignant catatonia has
been the basis for some controversy. Although Mann et al. (1986,
2003) have argued on the basis of similarities in presentation,
physiological abnormalitiessuch as elevated creatine phosphokinase and reduced serum iron (Philbrick & Rummans, 1994; White,
1992)and mortality, that NMS is simply an iatrogenic form of
malignant catatonia, others have disagreed (Castillo, Rubin, &
Holsboer-Trachsler, 1989; Fleischhacker, Unterweger, Kane, &
Hinterhuber, 1990). However, the variant of catatonia position
has been bolstered by recent research, such as White and Robinss
(2000) finding that 17 consecutive NMS patients had histories of
catatonic episodes unassociated with medication use; the majority
of those in the field now appear to accept this position (Ahuja &
Nehru, 1990; Fink, 1996; Fink & Taylor, 2003; Fricchione, 1985;
Fricchione, Mann, & Caroff, 2000).
989
Phenomenology
There are three published studies that have commented on the
subjective state of catatonia at lengthRosebush and Stewart
(1989), Rosebush et al. (1990), and Northoff, Krill, et al. (1998).
Rosebush and Stewart (1989) identified 20 individuals who experienced 24 episodes of NMS over a period of 6 years. They
reported observing a striking, frightened facial expression in all
cases. Eleven of the 20 patients were later able to describe feeling
at the time a desire to speak but an inability to do so and a sense
of impending doom along with overwhelming anxiety. Rosebush
and Stewart did not report whether the remaining patients denied
anxiety or could not recall their mental state.
In a subsequent study, Rosebush et al. (1990) located 12 catatonic subjects out of 140 consecutive admissions (8.6%). Ten of
the 12 patients (83%) responded dramatically to lorazepam, with
complete resolution of the catatonic symptoms after one dose.
Rosebush et al. reported that all 10 responders described feeling
intense anxiety during the course of the catatonic episode. Of the
2 nonresponders, 1 did not endorse anxiety and the other could not
recall the episode. In some cases, the anxiety appeared related to
the extrapyramidal side effects of the antipsychotic medications
they had received. Thus, 3 patients misinterpreted such extrapyramidal side effects symptoms as their being controlled or turned
into a robot. Summarizing their findings in a recent editorial,
Rosebush and Mazurek (1999) concluded that the vast majority of
persons experiencing catatonic stupor report feeling frozen or
petrified and experience extreme fear during the episode (pp.
396 397).
Northoff and colleagues (Northoff, Krill, et al., 1998; Northoff
et al., 1995, 2000) researches have led them to similar conclusions.
In a study of the subjective state of persons experiencing catatonic
stupor, Northoff, Krill, et al. (1998) found, on the basis of assessments prior to treatment (including the Hamilton Anxiety Scale;
Hamilton, 1959), that BZ responders (defined by the complete
resolution of catatonic symptoms within 24 hr59% of the sample) reported significantly more anxiety, intense feelings, and
blockade of movements by emotions than did nonresponders
(Northoff, Krill, et al., 1998). In a more recent study, also using the
Hamilton Anxiety Scale, Northoff et al. (2000) found strong and
significant correlations between anxiety and catatonic symptoms
(r .60 .68).
As these studies have all retrospectively assessed emotional
experiences during catatonic episodes, they have been unable to
determine whether the anxiety preceded the catatonic episodes or
developed subsequent to them, perhaps in response to an inability
to move.8 Although Rosebush and Mazurek (1999) contend that
the fear precedes the immobility in most of their cases, no relevant
studies have been conducted; this is perhaps understandable, as it
is very difficult to predict when someone will enter a catatonic
state. There have, however, been case reports of individuals developing stupor after reports of anxiety (Chandler, 1991; Wetzel,
Heuser, & Benkert, 1987). Particularly illustrative is that of Wetzel
et al. (1987), who described the complete alleviation of symptoms
of catatonia with one dose of a BZ, followed by their reinstatement
8
This possibility, however, appears unlikely in the light of research on
catatonic stupor, which has found persons strikingly unaware of their
unusual body positions or movements (Northoff, Krill, et al., 1998).
MOSKOWITZ
990
after administration of a BZ antagonist (Ro 15-1788; PerkinElmer,
Boston). They reported,
Almost immediately after injection, the patient complained of subsequently occurring dizziness, nausea, increasing anxiety, and overwhelming fears concerning accidents of family members. These fears
condensed to certainty. Two minutes later, the patient was in a state
identical to that before application of lorazepam, being mute and
stuporous. (Wetzel et al., 1987, pp. 240 241)
Thus, although limited research has been conducted to date,
severe anxiety has been reported in psychiatric (Chandler, 1991;
Northoff, Krill, et al., 1998; Rosebush et al., 1990; Wetzel et al.,
1987), iatrogenic (Rosebush & Stewart, 1989), and medical (Orland & Daghestani, 1987) catatonias. All studies that have asked
persons subsequent to episodes of catatonic stupor what they
experienced at the time found the majority to report intense anxiety, which abated with BZ treatment.
Treatment
The resurgence of interest in catatonia has perhaps been most
stimulated by the discovery that BZs such as lorazepam alleviate
catatonic symptoms in 70%90% of acute cases (Ungvari et al.,
2001). This was initially reported in the treatment of NMS or
neuroleptic-induced catatonia (Fricchione, Cassem, Hooberman,
& Hobson, 1983; Lew & Tollefson, 1983) but was quickly discovered to be true for both psychiatric and medically related
catatonias as well (Bernstein & Levin, 1993; Delisle, 1991; Greenfeld, Conrad, Kincare, & Bowers, 1987; Harris & Menza, 1989;
Menza & Harris, 1989; Salam, Pillai, & Beresford, 1987). Several
dozen case studies have now confirmed the efficacy of BZ in not
only retarded but also excited forms of catatonia (e.g., Cottencin,
Thomas, Vaiva, Rascle, & Goudemand, 1999; Harris & Menza,
1989; Lee, Schwartz, & Hallmayer, 2000; Ungvari, Leung, & Lee,
1994). In one controlled study of BZ in catatonia, complete resolution of catatonic signs to the first dose occurred in 83% of the
sample (Rosebush et al., 1990); in another study, one dose of
lorazepam resulted in 22% demonstrating a dramatic resolution
of symptoms and the remaining 78% experiencing clinically
significant relief (Ungvari, Leung, Wong, & Lau, 1994). Of note,
the improvement appears to relate only to catatonic signs; concomitant psychotic symptoms remain largely unchanged (Ungvari
et al., 2001).
Most authors have concluded that BZs are beneficial in catatonia by virtue of their antianxiety properties (Northoff, Steinke, et
al., 1999; Rosebush & Mazurek, 1999; Wetzel, Heuser, & Benkert,
1988). Consistent with this, those who respond to BZ consistently
report more anxiety pretreatment than those who do not (Northoff,
Krill, et al., 1998; Northoff et al., 1995; Rosebush et al., 1990), and
BZ-mediated improvement in catatonic symptoms (and amantadine as well; Northoff, Eckert, & Fritze, 1997) coincides with
substantial decreases in reported anxiety (Northoff, Krill, et al.,
1998; Northoff et al., 1995; Wetzel et al., 1987). However, it is not
possible to rule out, on a pharmacological basis, that BZs efficacy
in catatonia may be anticonvulsantas opposed to antianxietyin
nature, as some have contended (Fink & Taylor, 2003; Kritzinger
& Jordaan, 2001; Raitiere, 1986). Most BZs have potent anticonvulsant effects, and ECT, which is effective in catatonia (Bush et
al., 1996b; Escobar et al., 2000; Rohland, Carroll, & Jacoby,
1993), raises the threshold for seizures; antiseizure medications,
such as carbamazepine and amobarbital, also appear to be effective
in catatonia (Kritzinger & Jordaan, 2001; McCall, Shelp, & McDonald, 1992; Rankel & Rankel, 1988). Conversely, zolpidem,
which has little anticonvulsant activity (Salva & Costa, 1995), also
appears to improve catatonia (Thomas, Rascle, Mastain, Maron, &
Vaiva, 1997; Zaw & Bates, 1997).
Moreover, although BZ and ECT both appear to be effective in
catatonia, there are several reasons to believe that their mechanisms of action may be different: (a) Six to eight sessions of ECT
are typically required to produce improvement in catatonic symptoms (Escobar et al., 2000), whereas BZs effects may be seen
within minutes (Rosebush et al., 1990); (b) ECT may improve
depression associated with catatonia (Bush et al., 1996b), whereas
BZ appears to affect only the catatonic symptoms (Ungvari et al.,
2001); (c) ECT appears to be effective in reducing catatonic
symptoms in individuals who do not respond to BZ (Bush et al.,
1996b); and (d) a combination of BZ and ECT, either sequentially
or concurrently, appears more effective than either alone (Petrides,
Divadeenam, Bush, & Francis, 1997).
Further, it appears likely that ECTs potency in catatonia is due
more to its antidepressant than anticonvulsant properties. Catatonia
is associated with severe depression (Krueger & Braeunig, 2000;
Starkstein et al., 1996), the primary psychiatric indication for ECT
(Rasmussen, 2003; UK ECT Review Group, 2003), and severe
psychomotor retardation in depression is particularly predictive of
a positive response to ECT (Rasmussen, 2003). In addition, ECT
is more effective in alleviating catatonic symptoms in affective
disorders than in schizophrenia (Abrams & Taylor, 1977; Escobar
et al., 2000; Rohland et al., 1993), and the anticonvulsant carbamazepine, effective in catatonia (Kritzinger & Jordaan, 2001;
Rankel & Rankel, 1988), is used as a treatment for mood disorders
as well (Birkhimer, Curtis, & Jann, 1985; Israel & Beaudry, 1988).
Thus, a feasible alternative to the suggestion that both BZ and ECT
act as anticonvulsants is that catatonia contains components of
both anxiety and depression in varying degrees (or that there are
catatonia subgroups with different proportions of anxiety and
depression)9 and that BZ acts primarily on anxiety symptoms
whereas ECT acts primarily on depressive symptoms.
Brain Functioning and Neurochemistry
It has been argued that both BZ and ECT as well as most other
substances effective in catatonia (e.g., valproic acid, amobarbital)
9
This argument is bolstered by the fact that anxiety and depression often
appear together. One quarter to over 60% of individuals with bipolar
disorder also meet criteria for an anxiety disorder (Henry et al., 2003;
McElroy et al., 2001; Tamam & Ozpoyraz, 2002), and anxiety is present in
both manic and depressed states (Young, Cooke, Robb, Levitt, & Joffe,
1993). Half of those diagnosed with major depression also have an anxiety
disorder (Sanderson, Beck, & Beck, 1990; Zimmerman, Chelminski, &
McDermut, 2002), and one third of those with an anxiety disorder have
comorbid dysthmia or major depression (Sanderson, DiNardo, Rapee, &
Barlow, 1990). Further, as anxiety increases with the severity of depression
(Krishnan, 2003) and catatonia is associated with more severe depressive
symptoms in both manic (Krueger & Braeunig, 2000) and depressive
(Starkstein et al., 1996) disorders, it is particularly likely that anxiety is
common in the depressive states that accompany catatonia.
CATATONIA AS A FEAR RESPONSE
improve catatonia via their action on the gamma-aminobutyric
acid (GABA) inhibitory system, and specifically through GABAA
receptors (Carroll, 1999; McCall et al., 1992; Northoff, Steinke, et
al., 1999). Indeed, Carroll (1999) has argued that GABAA receptors play a crucial role in catatonia, noting that GABAA agonists
other than BZ, such as zolpidem, also appear to improve catatonia.
Fink and Taylor (2003) agreed, noting that too much GABAB or
too little GABAA activity contributes to the expression of catatonia (p. 187). However, other substances effective in catatonia,
such as amantadine, do not directly interact with GABA but rather
decrease glutamate and increase dopamine transmission (Northoff,
Eckert, & Fritze, 1997). Further, medications that produce NMS, a
variant of catatonia, block dopamine, and almost all drugs that
increase serotonin produce a toxic reaction some have linked to
catatonia (Fink & Taylor, 2003). As a consequence, Mann et al.
(2003), while arguing for a primary role for dopamine in malignant
catatonia, acknowledged that other neurotransmitters, including
GABA, are directly or indirectly involved, and Fink and Taylor
(2003) caution that it would be oversimplified to consider any one
neurotransmitter to be the basis for catatonia. Northoff (2002)
came to a similar conclusion, noting that changes in other neurotransmitter systems, such as dopamine or serotonin, can develop
secondarily to changes in the GABA system.
Until the last few years, the only studies to systematically assess
physiological functioning or biochemistry in catatonia involved
individuals suffering from periodic catatoniasuccessive episodes
of stupor, excitement, or both. In a remarkable series of studies
conducted by the Norwegian psychiatrist R. Gjessing in the 1920s
and 1930s, summarized in a 1938 article (R. Gjessing, 1938), and
subsequent studies conducted by his son, Leiv Gjessing, summarized in a 1974 article (L. R. Gjessing, 1974), individuals suffering
from periodic catatonia were assessed on a daily basis, over
periods of months and years, on numerous physiological indices
such as pulse, blood pressure, oxygen consumption, temperature,
leucocytes, nitrogen balance, and levels of various metabolites
before, during, and after episodes of catatonic excitement and
stupor. Both researchers found reliable increases in heart rate,
temperature, blood pressure, and oxygen consumption, in both
excitement and stupor phases (L. R. Gjessing, 1974; R. Gjessing,
1938), and L. R. Gjessing (1974) found increases in a number of
metabolites, particularly adrenergicnoradrenergic. L. R. Gjessing
(1974) characterized catatonic stupor as having a more rapid onset
and greater autonomic instability (demonstrated by frequently
changing pupil widths) than catatonic excitement. These were not
insignificant changes, as R. Gjessing (1938) reported, for example,
sustained increases in pulse rate from 60 70 to 110 120 beats per
minute. Strikingly, these changes were noted even when stupor set
in during sleep and were sometimes maintained for several days
despite an almost complete lack of movement.
Both researchers concluded that overactivity of the sympathetic
nervous system (SNS) was central to the onset of periodic catatonic episodes; R. Gjessing (1938) characterized this as an
adrenal-sympathetic impulse similar to Cannons emergency
reaction, whereas L. R. Gjessing (1974) noted similarities to reactions to adrenaline injections. Of note, these changes are consistently described as coinciding with the onset of the stupor (and
excitement) and in one publication are described as occurring
during the transition into the catatonic phase (Takahashi & Gjessing, 1972).
991
Such a formulation is consistent with that recently put forward
by Gurrera (1999) on NMS. Gurrera argued that a hyperactive
and unregulated SNS, released from inhibition by the frontal
cortex (via the hypothalamus), explains most, if not all, of the signs
and symptoms of NMS.
A primary dysfunction of the frontal lobes has been more
strongly emphasized by others. Taylor (1990) noted that the symptoms of catatonia were often described in the neurological literature as evidence for frontal lobe disease or dysfunction. He proposed that catatonia might be due to a dopamine imbalance in a
frontal lobe basal ganglia brainstem system (Taylor, 1990, p.
65). Northoff and colleagues (Northoff, Braus, et al., 1999;
Northoff et al., 2001; Northoff et al., in press; Northoff, Steinke et
al., 1998, 1999; Northoff et al., 2000), who have conducted an
important series of regional cerebral blood flow, single photon
emission computed tomography, and functional magnetic resonance imaging studies on brain functioning in catatonia, took a
somewhat different tack. In a recently published Behavioral and
Brain Sciences review, Northoff (2002) argued that reduced right
orbitofrontal cortex functioning, mediated by the GABAergic system, is a hallmark of catatonia and leads to an inability to inhibit
subcortical structures such as the basal ganglia. Of note, this
reduced right orbitofrontal activity (left-hemisphere functioning
appears largely unaffected) correlates significantly with measures
of anxiety in these patients and is reversed by BZ (Northoff, 2002).
Further, Northoff discovered that in currently nonsymptomatic
catatonic patients, connectivity between orbitofrontal cortex and
premotormotor cortex was functional at baseline but became
impaired during negative emotional stimulation (i.e., distressing
photographs; Northoff et al., in press, cited in Northoff, 2002). He
speculated that this occurs via connections between the orbitofrontal cortex, limbic system, and prefrontal cortexwhich modulates
the motor cortex and premotor area (Northoff, 2002). Finally,
Northoff acknowledged that the deficits in right orbitofrontal functioning found in catatonia may derive from activity in the amygdala, with which it is strongly reciprocally connected.
Catatonia and TI
Behavioral Characteristics
Catatonia shares a number of behavioral characteristics with TI,
first noted by Gallup and Maser (1977). Specifically, both catatonic stupor and TI are characterized by (a) immobility; (b) posturing; (c) stupor (lack of response); (d) waxy flexibility; (e)
reduced or absent vocalization; (f) fixed, unfocused gaze or stare;
(g) analgesia; and (h) evidence of alertness, despite unresponsiveness (Bush et al., 1996a; Fink & Taylor, 2003; Gallup, 1974;
Gallup, Boren, Suarez, Wallnau, & Gagliardi, 1980; L. R. Gjessing, Harding, Jenner, & Johannessen, 1967; Kahlbaum, 1874/
1973; Klemm, 1971, 2001; Ratner, 1958, 1967; Rosebush &
Mazurek, 1999; Taylor, 1990). In addition, TI demonstrates an
abrupt onset, almost invariably subsequent to struggling or fighting
behavior, and often terminates with spirited struggle or escape
(Hofer, 1970; Sargeant & Eberhardt, 1975); likewise, catatonic
stupor often begins abruptly and is not infrequently preceded or
followed by hyperactivity or excitement (American Psychiatric
Association, 2000; Fink & Taylor, 2003; L. R. Gjessing, 1974;
Morrison, 1973). This hyperactivity often includes assaultive be-
992
MOSKOWITZ
havior, at times directly out of a stuporous state (Bush et al.,
1996a; Fink & Taylor, 2003; Kahlbaum, 1874/1973; Morrison,
1973). In contrast to the motor symptoms of catatonia, the
behavioral communicative symptoms, such as echophenomena
and ambitendency, do not show any clear parallels to TI obviously, those involving spoken language could not.
Mortality
There is evidence that TI can, in and of itself, be fatal (Gallup,
1977; Hofer, 1970). Gallup (1977) discovered, during the course of
his research, that chickens occasionally died while immobilized; in
all instances, the chickens had received manipulations designed to
increase fear. Likewise, Hofer (1970), working with wild rodents,
discovered that over 25% died without apparent cause during the
first week of captivity. The deaths appeared related to pronounced
arrhythmias of vagal origin that developed during prolonged states
of immobility and not to captivity per se.
The deaths arising from NMS and malignant catatonia appear
not dissimilar to those described above, attributed to factors such
as renal failure (Shalev et al., 1989), cardiovascular collapse, or
arrythmias (Caroff, 1980; Mann et al., 1986). Of note, although
such states are often characterized by hyperactivity, the deaths
typically occur during a final stuporous phase (Mann et al., 1986,
2003).
Physiology and Neurochemistry
Significant changes in heart rate and respiration are found in TI,
with heart rate dropping or initially rising and then dropping below
baseline (Carli, 1977; Hofer, 1970; Nash, Gallup, & Czech, 1976;
Ratner, 1967)though in some species, such as pigeons, it remains high (Ratner, 1967)and respiration typically increasing
(Hofer, 1970; Nash et al., 1976). Core temperature also usually
drops (Eddy & Gallup, 1990; Whishaw, Schallert, & Kolb, 1979),
and pupils are dilated (Gallup & Maser, 1977). Thus, one sees a
combination of sympathetic and parasympathetic activation in TI.
Catatonia, in both excited and stupor phases, appears to be
characterized by autonomic instability, with sympathetic activation
predominating (L. R. Gjessing, 1974; R. Gjessing, 1938). There is
also evidence, however, of some parasympathetic activation in
stupor (L. R. Gjessing, 1974), and when catatonia proceeds to
death, it is largely parasympathetically mediated (Mann et al.,
1986; Shalev et al., 1989).
One study has found morphine to induce TI in rats, in a form
that appears similar to behaviorally induced or naturally occurring
TI (de Ryck & Teitelbaum, 1984). (In contrast, neurolepticinduced catalepsy appears to have some significant differences
from TI and may be more akin to attentive immobility.) This has
led some researchers to posit a role for endogenous opiates in TI
(Leite-Panissi, Rodrigues, Brentegani, & Menescal-de-Oliveira,
2001). Specifically, de Ryck & Teitelbaum (1984) found rats
administered morphine to demonstrate rigid immobility with insensitivity to pain, alternating with explosive bursts of uncontrolled locomotion. Morphine injections into the amygdala or the
midbrain periaquaductal gray (PAG) facilitate this response
(Klemm, 1989). Although there is not direct evidence for endogenous opiate activity in catatonia, Taylor (1990) has speculated
that the insensitivity to pain seen in catatonic stupor may be opioid
mediated.
The GABA system appears to play a prominent role in TI, as the
GABAergic agonist muscimol decreases TI, whereas the GABAergic antagonist bicuculline increases it (Monassi, Leite-Panissi, &
Menescal-de-Oliveira, 1999). However, there is little evidence at
this point that BZs (which are well-known to exert their anxiolitic
effects via the GABA system) decrease TI; although they reliably
decrease attentive immobility (Kalin, 1993), two studies found BZ
to actually increase TI in chickens (Rager, Gallup, & Beckstead,
1986) and guinea pigs (Olsen, Hogg, & Lapiz, 2002). The serotonergic system, closely entwined with the GABA system (Graeff,
1993; Kahn, van Pragg, Wetzler, Asnis, & Barr, 1988), has also
been implicated in TI (Gallup & Rager, 1996; Olsen et al., 2002).
Thus, at this point, it can only be stated that TI appears to result
from a complex, not yet understood, interplay between GABAergic, opioid, and serotonergic systems. As noted above, most researchers see catatonic disturbances as being GABA mediated
(Carroll, 1999; Fink & Taylor, 2003; McCall et al., 1992; Northoff,
Steinke, et al., 1999), though some accord a prominent role to
dopamine as well (Fink & Taylor, 2003; Mann et al., 2003; Taylor,
1990).
Brain Functioning
The structures most involved in the functioning (or inhibition)
of TI appear to be the frontal lobes, limbic system, and brainstem.
Svorad first noted in 1957 that TI was most common in species
with limited development of cerebral cortex and appeared in
higher species only under pathological conditions. Klemm (1971)
agreed with Svorads position, further noting that decorticated rats
expressed immobility after surgery but not before and that immobility was common in the young of some species, before the cortex
was fully developed, but rare at maturity. He concluded that the
neocortex inhibited TI. Subsequently, Klemm (1989) proposed
that this disinhibition of cortical areas was facilitated by limbic
activity, most likely the amygdala, which controlled the opioidbased expression of TI through the GABA systems influence on
lower brain structures.
Other researchers have largely endorsed Klemms (1989) proposal, noting further that the amygdala projects to the PAG in the
brainstem and could thus potentiate the activity of the latter
(Fanselow, 1991; Ramos, Leite-Panissi, Monassi, & Menescal-deOliveira, 1999). The PAG is believed by many researchers to be
the brain structure most directly responsible for the expression of
TI as well as other evolutionary-based defense reactions, as direct
stimulation of certain portions of the PAG (as well as microinjections of morphine, as noted above) produce behavior largely indistinguishable from TI (Fanselow, 1991; Fendt & Fanselow,
1999; Gray & McNaughton, 2000; Leite-Panissi, Coimbra, &
Menescal-de-Oliveira, 2003; Monassi et al., 1999).
Catatonia has also been hypothesized to result from a dysfunction of the frontal lobes (Taylor, 1990), in particular the right
orbitofrontal lobe (Northoff, 2002). It is argued that such a dysfunction releases cortical and subcortical motor control regions
(Northoff, 2002; Taylor, 1990) and that brainstem areas may also
be involved (Taylor, 1990). In addition, Northoff (2002) and to a
lesser extent Fink and Taylor (2003) appear to recognize that such
disturbances may be partially or primarily driven by limbic inter-
CATATONIA AS A FEAR RESPONSE
ference in general (Fink & Taylor, 2003) or by the amygdala in
particular (Northoff, 2002). Finally, although Taylor (1990) implicated the brainstem in general, there is no evidence to date implicating PAG activity in catatonia.
Summary
A summary of the main findings resulting from this comparison
of catatonia with TI can be seen in Table 1. Catatonia shares with
TI a significant number of behavioral characteristics, most of
which appear to be GABA mediated. They are also both occasionally punctuated by bursts of explosive activity and in some cases
lead to death, which appears largely vagal mediated. In addition,
both have been hypothesized to involve frontal lobe dysfunction or
disinhibition, releasing motor control regions, possibly under the
influence of the amygdala. Thus, there are substantial similarities
between TI and catatonia, strongly suggesting that the latter is
derived from the former.
However, there are some important differences as well. There is
evidence that dopamine may play a role in catatonia but not in TI,
whereas the role of serotonin is more clearly demonstrated in the
latter than in the former. Further, catatonia responds to BZ,
whereas TI does not (though only two studies on BZ in TI have
been located). If TI is to be thought of as an appropriate model for
catatonia, how can this important difference be reconciled? Clues
come from focusing on catatonia as an inappropriate expression of
TI.
The Nature of Catatonia
Animal Defense Strategies and Varieties of Catatonia
As stated before, it is not catatonia, properly speaking, that is
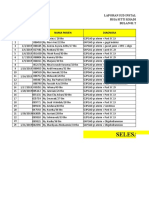
associated with TI but only one form of catatoniaakinetic cataTable 1
Comparison of Catatonia With Tonic Immobility
Domains
Behavioral characteristics
Immobility
Mutism
Stupor
Catelepsy
Excitement
Analgesia
Echolaliaechopraxia
Automatic obedience
Stereotypies
Physiology and neurochemistry
Sympathetic activitation
Parasympathetic activation
GABA involved
Opioid involved
Dopamine involved
Serotonin involved
BZ response
Brain functioning
Frontal dysfunction
Amygdala involvement
Periaquaductal graybrainstem involvement
Catatonia
Tonic
immobility
x
x
x
x
x
x
x
x
x
x
x
x
x
x
x
x
x
x
?
x
?
x
x
x
x
x
x
?
?
x
x
x
Note. x present; not present; ? limited or conflicting evidence;
GABA gamma-aminobutyric acid; BZ benzodiazepine.
993
tonia or catatonic stupor. However, other components of catatonia
may be related to other animal defense strategies, namely, fight
or flight. The three components of catatonia described above
catatonic stupor, catatonic excitement, and the behavioral
communicative featuresas well as one form of catatoniamalignant catatoniaare related to animal defense strategies and
autonomic functioning (drawing heavily on Porgess, 1995, 1997,
2001, polyvagal theory) in Table 2 and in the sections below.
Catatonic stupor as an inappropriate expression of TI. Catatonic stupor responds robustly to BZ, whereas TI does not. This
apparent discrepancy could be explained if TI is conceptualized as
a fear response and catatonic stupor is conceptualized as an anxiety
response. Although fear and anxiety have been used somewhat
interchangeably throughout this article, this distinction now becomes critical to an understanding of catatonia. Summarizing a
wealth of data in The Neuropsychology of Anxiety, Gray and
McNaughton (2000) argued that BZs are uniquely effective in
reducing anxiety but are ineffective against fear states; in fact, BZ
response forms a core component of their definition of anxiety. So,
they argued that generalized anxiety disorder, which does respond
to BZ, is appropriately considered an anxiety response, whereas
phobias, which do not respond to BZ (and have a clearly identifiable object), are best considered a fear response (Gray & McNaughton, 2000). Blanchard and Blanchard (1990) related fear to
a present threat and anxiety to a potential threat; it is important to
note that this distinction partly rests on whether the fear-producing
source can be localized. Although the source of danger is generally
not an issue in naturally occurring or experimentally induced TI, it
may be an issue in catatonia, in which the danger, despite being
experienced as present and overwhelming, may be impossible to
localize. That is, in catatonia, the fear response, evolutionarily
appropriate in situations of confrontation with a predator, is triggered in situations in which no predator can be found. The sensation of imminent doom in the absence of any localizable source of
danger transforms the fear response into an anxiety response.
Thus, in this hypothesis, catatonic stupor would be seen as an
anxiety response and predicted to respond to BZ, whereas TI
would be seen as a fear response and unresponsive to BZwhich
is what has been found. Nonetheless, this should be considered
speculative, as only two studies have explored the impact of BZ on
TI, and in both studies, the dangerin the form of the experimenter who induced TIwas localizable (Olsen et al., 2002;
Rager et al., 1986); it remains to be seen whether TI, induced
electrically or pharmacologically, which would present no object
from which to flee, would be responsive to BZ.
Catatonic excitement as an inappropriate expression of fight
flight. Aspects of catatonic excitement can also be understood as
an artifact of an inability to localize the source of danger. Indeed,
the DSMIV definition of catatonic excitementapparently purposeless [italics added] agitation not influenced by external stimuli (American Psychiatric Association, 2000, p. 764)is entirely
consistent with this. Further, assaultiveness, common in catatonic
excitement (American Psychiatric Association, 2000; Fink & Taylor, 2003; Morrison, 1973), is described as undirected or unfocussed (American Psychiatric Association, 2000). Combativeness,
a component of a prominent catatonia rating scale, is described as
being expressed usually in an undirected manner, with no, or only
a facile explanation afterwards (Bush et al., 1996a, p. 135). This
behavior is understandable if, as I propose, the catatonic individual
MOSKOWITZ
994
Table 2
Components of Catatonia Related to Autonomic Functioning and Animal Defense Reactions
Components of catatonia
Catatonic stupor
Catatonic excitement
Behavioralcommunicative
featuresa
Malignant catatonia
Relevant autonomic nervous system functioning
Animal defense reaction
Autonomic instability, with predominantly
sympathetic activity
Sympathetic activity
Loss of parasympatheticventral vagal complex
activityb
Sympathetic to parasympatheticdorsal vagal
complex activity with increasing mortalityc
Tonic immobility
Fightflight
Fightflight to tonic
immobility
Negativism, automatic obediance, echolalia, etc. b A system Porges (1995, 1997) argued is central to
high-level interpersonal communication utilizing words and gestures (see text for further explanation). c According to Porges (1995, 1997), extended utilization of the dorsal vagal complex, evolutionarily designed for
reptiles, is often fatal in mammals (see text for further explanation).
experiences a palpable sense of danger in a situation in which there
is no clearly recognizable object to attack or from which to fleea
consequence of this behavioral pattern being elicited in an evolutionary inappropriate threat situation. Under such circumstances,
unsuspecting passersby may be attacked for no apparent reason
(Fink & Taylor, 2003). Consistent with this hypothesis, uncharacteristic undirected escape behavior can be produced in rats (i.e.,
running off a 1 m high table) following morphine injections into
the PAG (de Ryck & Teitelbaum, 1984), triggering a flight response in a situation lacking a suitable object from which to flee.
Associated catatonia features and communication deficits.
Engagement of the SNS in catatonic excitement or stupor may also
affect the type of communicative behavior available to an individual. According to Porgess polyvagal theory of emotion and defensive behavior (so-called because he believes mammals have
evolved two dissociable vagal systems; Porges, 1995, 1997, 2001),
sympathetic activation results in an inhibition of the ventral vagal
complex (VVC), a parasympathetic component of the autonomic
nervous system unique to mammals that allows for rapid and
subtle cardiac modulation in situations perceived as safe and
innervates the muscles of the face and vocal system. Thus, inhibition of the VVC results in a decreased capacity to use sophisticated forms of communication with words and gesturesthe first
line of defense in situations of conflict. The loss of such capacity
would be consistent with the mutism frequently seen in catatonia
as well as symptoms such as negativism, automatic obedience, or
echolalia and echopraxia.10 If ones capacity to communicate is
severely curtailed, imitating an examiner (echophenomena) or
routinely obeying (automatic obedience) or denying (negativism)
requests may be the level at which one can interact. In addition,
several of these behaviors (waxy flexibility, automatic obedience)
appear submissive, which would also be consistent with a defense
reaction.
These symptoms (which would meet DSMIV criteria for catatonic behavior but not, in the absence of motor excitement, Fink
and Taylors, 2003, criteria for catatonia) are not typically viewed
as communicative but rather are seen as evidence of stimulusbound behavior arising from frontal lobe dysfunction (Mann et al.,
2003; Taylor & Fink, 2003). However, most can be elicited only
through interaction with another person making requests of the
individual or manipulating his or her limbs (Taylor & Fink, 2003).
As these individuals are often mute or demonstrate little productive speech, it is not unreasonable to suggest that these symptoms,
arising in the context of a social interaction, be broadly considered
communicative in nature.
In and of themselves, these symptoms, which do not have
analogues in animal defense reactions, are likely less related to
anxiety than states of stupor or excitability. Chronic catatonic
patients, who primarily exhibit these symptoms, do not demonstrate autonomic instability or respond to BZ (Bush, Petrides, &
Francis, 1997; Ungvari, Chiu, Chow, Lau, & Tang, 1999).
In addition, though admittedly speculative, it is possible that
some of the postures seen in catatoniasuch as psychological
pillowmay contain fragments of a fear response. For example,
one is better able to perceive potential dangers while lying in bed
with ones head raised, as in psychological pillow, than if one were
completely supine. Further, the twisted odd head positions frequently seen in catatonic stupor (as well as the fixed eye gaze)
could conceivably derive from the cutoff positions of TI (Dixon,
1998), reducing visual input from the predator and thereby decreasing distress and arousal.
Malignant catatonia: Scared to death? In almost 80% of the
autopsied deaths in cases of malignant catatonia since 1960, no
medical cause of death could be found (Mann et al., 2003). Mann
et al. (2003) have characterized cases such as these as psychogenic, or psychologically caused, which likely indicates that death
is due to a vagal surge (Porges, 1997, 2001). As the deaths in Mann
et al.s (1986) older series also appear to have been overwhelmingly vagal in natureas were the animal deaths during fearinducing procedures in TI studies (Gallup, 1977; Hofer, 1970)
the possibility that these individuals could have been scared to
death cannot be discounted.
The typical pattern seen in malignant catatonia (and in NMS) of
an extended period of frenetic activity followed by stupor and then
death is entirely consistent with Porgess (1995, 1997, 2001)
model of a progression from sympathetic activation to vagal (dorsal vagal complex [DVC])-mediated immobility and death in situations of extreme threat. The DVC, evolutionary designed for
reptiles for whom bradycardia and apnea are adaptive during
lengthy periods of submersion under water, is primarily used in
mammals for digestive purposes but also becomes engaged when
10
Consistent with this, patients in Rosebush and Stewarts (1989) study
who exhibited frightened faces and reported overwhelming anxiety spoke
of wishing to speak but feeling unable to do so.
CATATONIA AS A FEAR RESPONSE
metabolic resources are scarce or when immobilization is required.
However, in mammals, DVC engagement cannot be tolerated for
long and as such is used only as a last resort, after engagement of
the sympathetic system (i.e., flightfight) fails to resolve the conflict (Porges, 1997). It is proposed that this is precisely what occurs
in malignant catatonia, in which extended sympathetic activity
fails to resolve the problem however that might be perceived exposing the individual to a relatively undiluted DVC
response, which, as Porges (1997) noted, is associated with feelings of extreme terror and fatal heart abnormalities. Indeed, Porges
(1997, 2001) and Marks (1987) both speculated that so-called
voodoo death (Cannon, 1957), which is characterized by prolonged motionless prior to death, results from a similar
mechanism.
Affect and Etiology
In most cases catatonia is preceded by grief and anxiety, and in
general by depressive moods and affects aimed against the patient by
himself. Very common are anguish related to unhappy love, or selfreproach resulting from secret sexual misdemeanors. (Kahlbaum,
1874/1973, p. 33)
Despite Kahlbaums (1874/1973) observations, and the current
acceptance of catatonias association with affective disorders, the
possible role of affect in the genesis of catatonic symptoms has
been largely overlooked. Indeed, Fink and Taylor (2003), on the
basis of ECTs efficacy in catatonia, have proposed that catatonia
may be related to seizure disorders; however, a few swipes of
Occams razor should be sufficient to see that severe depression,
alleviated by ECT and strongly associated with catatonia, is a
much more likely candidate.11 Further, recent models proposed for
catatonias pathophysiology place little emphasis on affect (Fink &
Taylor, 2003; Gurrera, 1999; Mann et al., 2003; Northoff, 2002),
thoughas will be seen in the next sectionsuch considerations
are not inconsistent with any of them.
When catatonia develops in the context of a medical condition,
it is typically serious and often life threatening. Catatonia does not
arise alongside relatively mild or benign medical conditions. The
fact that the expression of catatonia does not vary whether it is
associated with life-threatening medical conditions or profoundly
dysphoric affective states (Carroll et al., 2000) and may respond to
treatments that do not affect the underlying condition (Fink &
Taylor, 1991; Ungvari et al., 2001) suggests that catatonia may
best be viewed not as a component of these various conditions but
as a reaction to them. Such a position is consonant with that of
Patricia Rosebush (2003), who leads the largest prospective study
of catatonia in the world, following 95 patients through 120
catatonic episodes to date. In a recent editorial, Rosebush and
Mazurek (1999) stated An important precipitating factor appears
to be intense anxiety . . . . Intense fear may be the common factor
in catatonic states occurring in a disparate range of medical and
neurological as well as psychiatric disorders (pp. 396 397).
Thus, catatonia may be an evolutionary-based fear response,
originally associated with serious risk to life in the context of
attack from a predator, but which has become generalized to very
different modern threat situationssuch as those listed by Kahlbaum (1874/1973) above constituting a mismatch between the
ancestral environments that bred the response and the current
995
situations that trigger it (Nesse & Williams, 1994). The mechanism
mediating this response may well be the emotions themselves, a
particular admixture of anxiety and depression, carrying the
code, as Tooby and Cosmides (1990) contend, for this ancient
behavioral pattern. Clearly, it may not be inappropriate to have a
sense of impending doom when afflicted with a serious medical
condition, as ones life may well literally be at risk.12 Although
this may not objectively be the case in psychiatric conditions,
profound depression, overwhelming anxiety, or intense psychotic
symptoms can no doubt trigger similar perceptions of inescapable
proximal threat (Dixon, 1998). Further, this perception need not be
a conscious one, as fear and anxiety can be produced solely
through nonconscious mechanisms (Armony & LeDoux, 1997;
Nadel & Jacobs, 1996; Robinson, 1998). I would suggest that the
anxious depression underlying catatonia is associated with a specific cluster of experiencesa perception of inescapable but at the
same time amorphous danger, a sense of defeat and entrapment,
and a sensation of imminent doom. Dixons (1998) notion of
arrested flightwith all escape routes being blockedis also of
relevance. Recall that the perception of entrapmentnot limited to
physical contact has been proposed to underlie not only TI in
animals (Ratner, 1967) but also depression in humans (Dixon,
1998; Gilbert & Allan, 1998).
There are, of course, alternative explanations for the presence of
anxiety in persons experiencing catatonic symptoms. Theoretically, the anxiety might simply be an epiphenomenon of biologically based changes, accompanying, but not driving, sympathetic
activation or altered orbitofrontal functioning. However, Rosebush
and Mazureks (1999) observation that experiences of fear typically precede the development of catatonic symptoms, confirmed
in case studies (Chandler, 1991; Wetzel et al., 1987), argues
against this formulation. Alternatively, as suggested by Northoff
(2002), the experience of overwhelming anxiety may be due to the
loss of a cognitive capacity to contain (or extinguish) normal
anxieties, consistent with decreased functioning of the orbitofrontal cortex. Thus, anxieties that might normally be managed in the
course of daily life, such as worries that a loved one might die
(Orland & Daghestani, 1987), could take on gargantuan proportions and lead to catatonic symptoms. Of course, this possibility is
not inconsistent with the notion of catatonia as a fear response but
does not require the presence of anything other than normal
anxieties or fears.
However, none of the above is to suggest that catatonia could
not develop in the absence of anxiety, as a significant minority of
affected individuals in Northoff et al.s (1998) and Rosebush and
Stewarts (1989) studies did not report it. This should be viewed
with caution, however, as in Rosebush and Stewarts study, all 20
NMS sufferers exhibited striking, frightened facial expressions
despite only 11 later describing experiencing overwhelming anxiety at the time. This, along with reports of amnesia for catatonic
11
In all fairness to Fink and Taylor (2003), these are not necessarily
mutually exclusive possibilities. Some (e.g., Post, Putnam, Contel, &
Goldman, 1984) have posited that ECT exerts its action in depression
through anticonvulsantantikindling effects in the amygdala.
12
This would also be true of traumatic situations, such as World War I
battles, which have been reported to trigger episodes of catatonic stupor
(Kardiner & Speigel, 1947).
MOSKOWITZ
996
episodes (Rosebush et al., 1990), suggests that some individuals
who do not recall anxiety may nonetheless have been anxious
during the catatonic episode. Even so, it is certainly conceivable
that abnormalities in the motor loop, for example, in and of
themselves could cause catatonic symptoms. However, it appears
likely that in the majority of cases of catatonia, anxiety plays a
major causative role.
Models of Pathophysiology
The mechanism through which affect may produce catatonia can
be seen by an exploration of the various models of pathophysiology proposed, presented in Table 3. All models posit a primary
role for the frontal cortex, with Northoffs (2002) strongly emphasizing the right orbitofrontal cortex. Although the orbitofrontal
cortex has a wide range of functions, one of the most important,
particularly in the right hemisphere, is regulation of affective
experience (Joseph, 1999; Schore, 1994, 2001, 2002). The orbitofrontal cortex has strong reciprocal connections with the limbic
system, hypothalamus, and vagal nerve (Nauta, 1971, 1979),
which are all more pronounced in the right hemisphere than in the
left (Porges, Doussard-Roosevelt, & Maita, 1994; Schore, 1994,
2001, 2002). Through these connections, the orbitofrontal cortex
monitors and modulates all aspects of affective experience, including the intensity and duration of emotions experienced and autonomic functioning (Dias, Robbins, & Roberts, 1996; Nauta, 1971,
1979; Schore, 1994). It is possible that the orbitofrontal cortex has
a similar role in catatonia, as Northoffs (2002) findings of decreased right orbitofrontal functioning reversed by BZ administration closely mirror work on panic disorder (Malizia, 2000, cited in
Nutt & Malizia, 2001; Malizia et al., 1998). Indeed, Malizia et al.
(1998) have argued that the right orbitofrontal cortex is central to
the mediation of anxiety.
For his part, Northoff (2002) appears to have some recognition
of this, as he accorded a primary role to anxiety in his conception
of catatonia and allowed for the possibility that the deficit in right
orbitofrontal functioning could be due to amygdala activity. He
goes further in his response to commentaries on his Behavioral
and Brain Sciences review, four of which emphasize the amygdala
(Aleman & Kahn, 2002; Miu & Olteanu, 2002; Platek & Gallup,
2002; Savodnik, 2002), by stating that he presumes that the amygdalawhose primary role lies in processing fear stimuli and
coordinating fear responses (Fendt & Fanselow, 1999; LeDoux,
1998)plays a role in the pathophysiology of catatonia (Northoff,
2002, p. 593). The other models of pathophysiology presented in
Table 3 are not so explicit on this point, but would all potentially
allow a role for the amygdala. Fink and Taylor (2003) noted that
intense mood states can lead to limbic interference in the
pathophysiological circuit they propose, whereas Mann et al.
(2003), Fink and Taylor (2003), and Gurrera (1999) all allowed a
role for stress in the precipitation of catatonic episodes. Gurrera
went so far as to suggest that acute psychic distress may be
responsible for the frontal impairment underlying the disinhibition
of the SNS. Although no studies have yet evaluated amygdala
functioning in catatonia, the fact that both BZ and N-methyl-Daspartate (NMDA)-antagonists block freezing when injected into
the amygdala (Fendt & Fanselow, 1999) and improve catatonic
symptoms (Northoff et al., 1997; Ungvari et al., 2001) is
suggestive.
Finally, it is important to recall that R. Gjessing (1938), more
than 65 years ago, linked physiological changes in catatonia to the
Table 3
Models of Pathophysiology in Catatonia
Fink & Taylor (2003)
Mann et al. (2003)
Northoff (2002)
Gurrera (1999)
Key components
Prefrontal cortex
Anterior cingulate
Thalamus
Basal ganglia
Frontal cortex
Thalamus
Basal ganglia
Orbitofrontal cortex
Anterior cingulate
Basal ganglia
Frontal cortex
Hypothalamus
SNS
Proposed mechanism
Frontal (motor) circuit dysfunction.
Disconnection between motor
regulatory and perceptualintegrating systems.
Dysfunction in multiple basal
gangliathalamocortical
circuits.
Deficit in right orbitofrontal cortex
leading to abnormal modulation
of basal ganglia.
Disruption in inhibition from frontal
cortex (via hypothalamus) leading to
dysregulated SNS hyperactivity.
Neurotransmitters emphasized
DopamineGABA
Dopamine
GABA
Dopamine
Role for amygdala?
Implicit, as model allows for
limbic interference due to
intense mood states. Acute
severe stress is also implicated.
Potential, as circuits may be
disrupted by acute stress.
Explicit, though unproven.
Amygdala could be responsible for
orbitofrontal cortex deficit.
Note. SNS sympathetic nervous system; GABA gamma-aminobutyric acid.
Potential, as acute psychic distress
may be responsible for frontal
cortex impairment.
CATATONIA AS A FEAR RESPONSE
sympathically mediated emergency or stress reactions described
by Cannon (1928); among contemporary theorists, autonomic dysfunction or sympathetic hyperactivity is emphasized by Fink and
Taylor (2003) and is central to Gurreras (1999) formulation of
NMS.
Implications and Future Directions
When Kahlbaum (1874/1973) first proposed the concept of
catatonia over 125 years ago, there was an awareness of its
connection to stressful and frightening events. That awareness was
lost until a few decades ago, when Gallup and Maser (1977) and
Perkins (1982) reintroduced it. The current conceptualization of
catatonia as a fear response deriving from TI is consistent with
their positions as well as with Kahlbaums original formulation,
evolutionary-based conceptions of depression, and much of the
recent research on the phenomenology, treatment response, and
pathophysiology of catatonia. In addition, positions recently articulated by Georg Northoff (2002), the most prominent cognitive
neuroscientist working in this area, and Patricia Rosebush (2003;
see also Rosebush & Mazurek, 1999), who has the largest corpus
of catatonia cases, are entirely consistent with this thesis. Although
this position thus has significant empirical support, many questions
remain.
First, the prevalence and precise nature of the affect underlying
catatonia is still to be determined. If catatonia is overwhelmingly
associated with mixed affective states in mania, as Krueger and
Braeunig (2000) asserted, is it the depression that drives the
response? Does anxiety or agitation underlie irritability when the
latter is seen in mania with catatonic features? Is anxiety often
missed in catatonic stupor because psychomotor retardation does
not typically suggest anxiety? Systematic research, involving both
rating scales and interviews, is clearly needed to address these
questions.
Second, as there are strain differences in the propensity for
expression of TI (Gallup, Ledbetter, & Maser, 1976; Mills &
Faure, 1991), there may well be personality or physiological
predispositions to catatonia. Gurrera (1999) suggested a genetically based sensitivity to stress could lead to the hyperactive SNS
seen in NMS, which Fink and Taylor (2003) endorsed for malignant catatonia. If such a predisposition exists, however, it need not
be genetic. Heim and Nemeroff (2001) have found adverse childhood experiences to induce a persistent sensitization of stressresponsive neural circuits (p. 1024), particularly related to mixed
depressionanxiety states (Heim et al., 2000). Further, early adverse experiences may lead to not only increased SNS sensitivity
but, as Schore (2001) contended, excessively pruned connections
between the right orbitofrontal cortex and the amygdala and hypothalamus, making it more difficult for the former to modulate
the latter structures. The consequences of this would be that even
low-level stressors could generate unmodulated terrifying and
painful emotional experiences, triggering fear-freeze behavioral responses (Schore, 2001, p. 227). Future research will need to
establish whether early adverse experiences, common in major
depression (Kendler, Kessler, Neale, Heath, & Eaves, 1993), are
also frequent in individuals who manifest catatonic states.
Additionally, if catatonia is primarily a fear response as hypothesized, attempts to code the facial expressions of persons in the
midst of catatonic episodes, with an approach such as the Facial
997
Action Coding System (Ekman & Friesen, 1978), should result in
a preponderance of anxious or fearful expressions. It should be
recalled that the frequent presence of fearful faces inspired the
name for the condition on which Kahlbaum (1874/1973) based his
concept of catatoniamelancholia attonita.
Finally, if Porgess polyvagal theory does apply to catatonia as
proposed, there should be evidence for decreased VVC activity in
catatonia. VVC activity can reliably be measured by assessing an
individuals respiratory sinus arrhythmia rate (Porges, 2001; Sahar, Shalev, & Porges, 2001). Respiratory sinus arrythmias are
minor fluctuations in heart rate, coincident with respiratory
rhythms, which allow an individual to engage and disengage from
the social environment with minimal energy expenditure. One
would predict low activity during catatonic states and possibly
between episodes, as low VVC activity could indicate a vulnerability to catatonic episodes.
Catatonia is not the only possible link between psychiatric
conditions and animal defense reactions. There are aspects of other
disorders potentially explainable by a progression from fight
flight to TI, with perceived changes in level of danger, or predatory
imminence. Nijenhuis, Vanderlinden, and Spinhoven (1998) have
proposed just such a model for dissociative disorders, and posttraumatic stress disorder, with its cyclic alterations between intrusive and avoidance symptoms, seems a good fit as well (Horowitz,
1978). Indeed, both dissociation and avoidance symptoms, which
allow the avoidance of distressing and arousing information,
would appear to be the psychological equivalent of Dixons (1998)
cutoff behaviors in TI. Finally, could bipolar disorder, which some
see as integrally related to catatonia (Fink & Taylor, 2003; Ries,
1985), also be modeled on alterations between episodes of TI and
fightflight? Depression has already been linked to TI (Dixon,
1998), and as some see manic excitement as parallel to catatonic
excitement (Fink & Taylor, 2003), such a proposal could clearly be
mounted. Thus, catatonia may be the best but is certainly not the
only example of the usefulness of exploring animal and evolutionary models of behavior as a means to understand psychiatric
disorders.
It is proposed here that the concept of catatonia as a fear
response provides more explanatory power than the dominant view
of catatonia as a motor disorder. Although the latter is superficially
accurate, it is unable to adequately explain many aspects of catatonia, such as the presence of anxious and fearful expressions, the
potential lethality, the communicative abnormalities, and the presence of undirected aggressive behavior. Catatonia as a fear response can explain all of the above in addition to the motor
disturbances. Conceptualizing catatonia as a motor disorder is a
relic of black box materialism, deriving from an inability to see
humans as responsive to the situations in which they find themselveswhether these situations are predatory attacks, profoundly
dysphoric mood states, or potentially life-threatening medical conditions. Responses to these situationswhich need not be consciously mediatedmay include catatonia. Recognition of this fact
is crucial to advancing our understanding and treatment of this
bizarre and frightful condition.
References
Abrams, R., & Taylor, M. A. (1976). Catatonia. A prospective clinical
study. Archives of General Psychiatry, 33, 579 581.
998
MOSKOWITZ
Abrams, R., & Taylor, M. A. (1977). Catatonia: Prediction of response to
somatic treatments. American Journal of Psychiatry, 134, 78 80.
Abrams, R., Taylor, M. A., & Coleman Stolurow, K. A. (1979). Catatonia
and mania: Patterns of cerebral dysfunction. Biological Psychiatry, 14,
111117.
Ahuja, N., & Nehru, R. (1990). Neuroleptic malignant syndrome: A
subtype of lethal catatonia? [Letter to the editor]. Acta Psychiatrica
Scandinavica, 82, 398.
Aleman, A., & Kahn, R. S. (2002). Top-down modulation, emotion, and
hallucination. Behavioral and Brain Sciences, 25, 578.
American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: Author.
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text. rev.). Washington, DC: Author.
Armony, J. L., & LeDoux, J. E. (1997). How the brain processes emotional
information. In A. C. McFarlane (Ed.), Psychobiology of posttraumatic
stress disorder (Vol. 821, pp. 259 270). New York: New York Academy of Sciences.
Barnes, M. P., Saunders, M., Walls, T. J., Saunders, I., & Kirk, C. A.
(1986). The syndrome of Karl Ludwig Kahlbaum. Journal of Neurology,
Neurosurgery & Psychiatry, 49, 991996.
Bernstein, L., & Levin, R. (1993). Catatonia responsive to intravenous
lorazepam in a patient with cyclosporine neurotoxicity and hypomagnesemia. Psychosomatics, 34, 102103.
Berrios, G. E. (1981). Stupor revisited. Comprehensive Psychiatry, 22,
466 478.
Billig, O., & Freeman, W. T. (1944). Fatal catatonia. American Journal of
Psychiatry, 100, 633 638.
Birkhimer, L. J., Curtis, J. L., & Jann, M. W. (1985). Use of carbamazepine
in psychiatric disorders. Clinical Pharmacy, 4, 425 434.
Blanchard, R. J., & Blanchard, D. C. (1990). An ethoexperimental analysis
of defense, fear, and anxiety. In G. Andrews (Ed.), Anxiety (Vol. 1, pp.
124 133). New Zealand: University of Otago Press.
Bleuler, E. (1950). Dementia praecox or the group of schizophrenias (J.
Zinkin, Trans.). New York: International Universities Press. (Original
work published 1911)
Braeunig, P., Krueger, S., & Shugar, G. (1999). Prevalence and clinical
significance of catatonic symptoms in mania. Fortschritte der
Neurologie-Psychiatrie, 67, 306 317.
Braeunig, P., Krueger, S., Shugar, G., Hoeffler, J., & Boerner, I. (2000).
The Catatonia Rating Scale IDevelopment, reliability, and use. Comprehensive Psychiatry, 41, 147158.
Brune, M. (2000). Rethinking Karl Ludwig Kahlbaums contribution to
biological psychiatry. Australian & New Zealand Journal of Psychiatry,
34, 873 874.
Brune, M. (2002). Toward an integration of interpersonal and biological
processes: Evolutionary psychiatry as an empirically testable framework
for psychiatric research. PsychiatryInterpersonal and Biological Processes, 65, 48 57.
Bush, G., Fink, M., Petrides, G., Dowling, F., & Francis, A. (1996a).
Catatonia. I. Rating scale and standardized examination. Acta Psychiatrica Scandinavica, 93, 129 136.
Bush, G., Fink, M., Petrides, G., Dowling, F., & Francis, A. (1996b).
Catatonia. II. Treatment with lorazepam and electroconvulsive therapy.
Acta Psychiatrica Scandinavica, 93, 137143.
Bush, G., Petrides, G., & Francis, A. (1997). Catatonia and other motor
syndromes in a chronically hospitalized psychiatric population. Schizophrenia Research, 27, 8392.
Buss, D. M. (1995). Evolutionary psychology: A new paradigm for psychological science. Psychological Inquiry, 6, 130.
Cannon, W. B. (1928). The mechanism of emotional disturbance of bodily
functions. New England Journal of Medicine, 198, 877 884.
Cannon, W. B. (1957). Voodoo death. Psychosomatic Medicine, 19,
182190.
Carli, G. (1977). Animal hypnosis in the rabbit. Psychological Record, 1,
123143.
Caroff, S. N. (1980). The neuroleptic malignant syndrome. Journal of
Clinical Psychiatry, 41, 79 83.
Carroll, B. T. (1992). Catatonia on the consultation-liaison service. Psychosomatics, 33, 310 315.
Carroll, B. T. (1999). GABAa versus GABAb hypothesis of catatonia.
Movement Disorders, 14, 702703.
Carroll, B. T., Kennedy, J. C., & Goforth, H. W. (2000). Catatonic signs in
medical and psychiatric conditions. CNS Spectrums, 5(7), 58 65.
Castillo, E., Rubin, R. T., & Holsboer-Trachsler, E. (1989). Clinical
differentiation between lethal catatonia and neuroleptic malignant syndrome. American Journal of Psychiatry, 146, 324 328.
Chandler, J. D. (1991). Psychogenic catatonia with elevated creatine kinase
and autonomic hyperactivity. Canadian Journal of PsychiatryRevue
Canadienne de Psychiatrie, 36, 530 532.
Clark, T., & Rickards, H. (1999). Catatonia. 1: History and clinical features. Hospital Medicine (London), 60, 740 742.
Cosmides, L., & Tooby, J. (1999). Toward an evolutionary taxonomy of
treatable conditions. Journal of Abnormal Psychology, 108, 453 464.
Cottencin, O., Thomas, P., Vaiva, G., Rascle, C., & Goudemand, M.
(1999). A case of agitated catatonia. Pharmacopsychiatry, 32, 38 40.
Delisle, J. D. (1991). Catatonia unexpectedly reversed by midazolam.
American Journal of Psychiatry, 148, 809.
de Ryck, M., & Teitelbaum, P. (1984). Morphine catalepsy as an adaptive
reflex state in rats. Behavioral Neuroscience, 98, 243261.
Dias, R., Robbins, T. W., & Roberts, A. C. (1996, March 7). Dissociation
in prefrontal cortex of affective and attentional shifts. Nature, 380,
69 72.
Dixon, A. K. (1998). Ethological strategies for defence in animals and
humans: Their role in some psychiatric disorders. British Journal of
Medical Psychology, 71, 417 445.
Eddy, T. J., & Gallup, G. G. (1990). Thermal correlates of tonic immobility
and social isolation in chickens. Physiology & Behavior, 47, 641 646.
Ekman, P., & Friesen, W. V. (1978). Facial Action Coding System. Palo
Alto, CA: Consulting Psychologist Press.
Escobar, R., Rios, A., Montoya, I. D., Lopera, F., Ramos, D., Carvajal, C.,
et al. (2000). Clinical and cerebral blood flow changes in catatonic
patients treated with ECT. Journal of Psychosomatic Research, 49,
423 429.
Ewell, A. H., & Cullen, J. M. (1981). Tonic immobility as a predatordefense in the rabbit (Oryctolagus cuniculus). Behavioral and Neural
Biology, 31, 483 489.
Fanselow, M. S. (1991). The midbrain periaquaductal gray as a coordinator
of action in response to fear and anxiety. In R. Bandler (Ed.), The
midbrain periaquaductal gray matter: Functional, anatomical and immunohistochemical organization (pp. 151173). New York: Plenum.
Fanselow, M. S., & Lester, L. S. (1988). A functional behavioristic approach to aversively motivated behavior: Predatory imminence as a
determinant of the topography of defensive behavior. In M. D. Beecher
(Ed.), Evolution and learning (pp. 185212). Hillsdale, NJ: Erlbaum.
Fein, S., & McGrath, M. G. (1990). Problems in diagnosing bipolar
disorder in catatonic patients. Journal of Clinical Psychiatry, 51, 203
205.
Fendt, M., & Fanselow, M. S. (1999). The neuroanatomical and neurochemical basis of conditioned fear. Neuroscience & Biobehavioral Reviews, 23, 743760.
Fink, M. (1996). Neuroleptic malignant syndrome and catatonia: One
entity or two? Biological Psychiatry, 39, 1 4.
Fink, M. (1997). Catatonia. In J. L. Cummings (Ed.), Contemporary
behavioral neurology (Vol. 16, pp. 289 309). Woburn, MA:
Butterworth-Heinemann.
Fink, M. (2001). Catatonia: Syndrome or schizophrenia subtype? Recognition and treatment. Journal of Neural Transmission, 108, 637 644.
CATATONIA AS A FEAR RESPONSE
Fink, M., & Taylor, M. A. (1991). Catatonia: A separate category in
DSMIV? Integrative Psychiatry, 7, 210.
Fink, M., & Taylor, M. A. (2001). The many varieties of catatonia.
European Archives of Psychiatry & Clinical Neuroscience, 251(7),
I8 I13.
Fink, M., & Taylor, M. A. (2003). Catatonia: A clinicians guide to
diagnosis and treatment. Cambridge, England: Cambridge University
Press.
Fleischhacker, W. W., Unterweger, B., Kane, J. M., & Hinterhuber, H.
(1990). The neuroleptic malignant syndrome and its differentiation from
lethal catatonia. Acta Psychiatrica Scandinavica, 81, 35.
Fricchione, G. L. (1985). Neuroleptic catatonia and its relationship to
psychogenic catatonia. Biological Psychiatry, 20, 304 313.
Fricchione, G., Cassem, N. H., Hooberman, D., & Hobson, D. (1983).
Intravenous lorazepam in neuroleptic-induced catatonia. Journal of
Clinical Psychopharmacology, 3, 338 342.
Fricchione, G., Mann, S. C., & Caroff, S. N. (2000). Catatonia, lethal
catatonia, and neuroleptic malignant syndrome. Psychiatric Annals, 30,
347355.
Galliano, G., Noble, L. M., Travis, L. A., & Puechl, C. (1993). Victim
reactions during rape/sexual assault: A preliminary study of the immobility response and its correlates. Journal of Interpersonal Violence, 8,
109 114.
Gallup, G. G. (1974). Animal hypnosis: Factual status of a fictional
concept. Psychological Bulletin, 81, 836 853.
Gallup, G. G. (1977). Tonic immobility: The role of fear and predation.
Psychological Record, 27, 41 61.
Gallup, G. G., Boren, J. L., Suarez, S. D., Wallnau, L. B., & Gagliardi, G. J.
(1980). Evidence for the integrity of central processing during tonic
immobility. Physiology & Behavior, 25, 189 194.
Gallup, G. G., Ledbetter, D. H., & Maser, J. D. (1976). Strain differences
among chickens in tonic immobility: Evidence for an emotionality
component. Journal of Comparative & Physiological Psychology, 90,
10751081.
Gallup, G. G., Jr., & Maser, J. D. (1977). Tonic immobility: Evolutionary
underpinnings of human catalepsy and catatonia. In M. E. P. Seligman
(Ed.), Psychopathology: Experimental models (pp. 334 357). New
York: W. H. Freeman.
Gallup, G. G., Jr., & Rager, D. R. (1996). Tonic immobility as a model of
extreme stress of behavioral inhibition: Issues of methodology and
measurement. In M. Kavaliers (Ed.), Motor activity and movement
disorders (pp. 57 80). Totowa, NJ: Humana Press.
Gelenberg, A. J. (1976). The catatonic syndrome. Lancet, 1, 1339 1341.
Gilbert, P. (Ed.). (1998). Evolutionary approaches to psychopathology
[Special issue]. British Journal of Medical Psychology, 71(4).
Gilbert, P. (2001). Evolutionary approaches to psychopathology: The role
of natural defences. Australian & New Zealand Journal of Psychiatry,
35, 1727.
Gilbert, P., & Allan, S. (1998). The role of defeat and entrapment (arrested
flight) in depression: An exploration of an evolutionary view. Psychological Medicine, 28, 585598.
Gjessing, L. R. (1974). A review of periodic catatonia. Biological Psychiatry, 8, 23 45.
Gjessing, L. R., Harding, G. F. A., Jenner, F. A., & Johannessen, N. B.
(1967). The EEG in three cases of periodic catatonia. British Journal of
Psychiatry, 113, 12711282.
Gjessing, R. (1938). Disturbances of somatic functions in catatonia with a
periodic course, and their compensation. Journal of Mental Science, 84,
608 621.
Goldar, J. C. (1988). Historical and clinical data on catatonia. Acta Psiquiatrica y Psicologica de America Latina, 34, 197209.
Goldar, J. C., & Starkstein, S. E. (1995). Karl Ludwig Kahlbaums concept
of catatonia. History of Psychiatry, 6(22), 201207.
999
Graeff, F. G. (1993). Role of 5-HT in defensive behavior and anxiety.
Reviews in the Neurosciences, 4, 181211.
Gray, J. A., & McNaughton, N. (2000). The neuropsychology of anxiety
(2nd ed.). Oxford, England: Oxford University Press.
Greenfeld, D., Conrad, C., Kincare, P., & Bowers, M. B., Jr. (1987).
Treatment of catatonia with low-dose lorazepam. American Journal of
Psychiatry, 144, 1224 1225.
Gurrera, R. J. (1999). Sympathoadrenal hyperactivity and the etiology of
neuroleptic malignant syndrome. American Journal of Psychiatry, 156,
169 180.
Hamilton, M. (1959). The assessment of anxiety states by rating. British
Journal of Medical Psychology, 32, 50 55.
Harris, D., & Menza, M. A. (1989). Benzodiazepines and catatonia: A case
report. Canadian Journal of Psychiatry, 34, 725727.
Heim, C., & Nemeroff, C. B. (2001). The role of childhood trauma in the
neurobiology of mood and anxiety disorders: Preclinical and clinical
studies. Biological Psychiatry, 49, 10231039.
Heim, C., Newport, D. J., Heit, S., Graham, Y. P., Wilcox, M., Bonsall, R.,
et al. (2000). Pituitary-adrenal and autonomic responses to stress in
women after sexual and physical abuse in childhood [Comment]. Journal of the American Medical Association, 284, 592597.
Hennig, C. W. (1978). Tonic immobility in the squirrel monkey (Saimiri
sciureus). Primates, 19, 333342.
Henry, C., Van den Bulke, D., Bellivier, F., Etain, B., Rouillon, F., &
Leboyer, M. (2003). Anxiety disorders in 318 bipolar patients: Prevalence and impact on illness severity and response to mood stabilizer.
Journal of Clinical Psychiatry, 64, 331335.
Hoch, A. (1921). Benign stupors: A study of a new manic-depressive
reaction type. New York: Macmillan.
Hofer, M. A. (1970). Cardiac and respiratory function during sudden
prolonged immobility in wild rodents. Psychosomatic Medicine, 32,
633 647.
Holcombe, V., Sterman, M. B., Goodman, S. J., & Fairchild, M. B. (1979).
The immobilization response in rhesus monkey: A behavioral and electroencephalographic study. Experimental Neurology, 63, 420 435.
Horowitz, M. J. (1978). Stress response syndromes. New York: Jason
Aronson.
Israel, M., & Beaudry, P. (1988). Carbamazepine in psychiatry: A review.
Canadian Journal of PsychiatryRevue Canadienne de Psychiatrie, 33,
577584.
Johnson, D. (1984). Just in case: A passengers guide to safety and
survival. New York: Plenum.
Johnson, J. (1984). Stupor: A review of 25 cases. Acta Psychiatrica
Scandinavica, 70, 370 377.
Johnson, J. (1993). Catatonia: The tension insanity. British Journal of
Psychiatry, 162, 733738.
Jones, I., & Blackshaw, J. K. (2000). An evolutionary approach to psychiatry. Australian & New Zealand Journal of Psychiatry, 34, 8 13.
Joseph, R. (1999). Frontal lobe psychopathology: Mania, depression, confabulation, catatonia, perseveration, obsessive compulsions, and schizophrenia. Psychiatry, 62, 138 172.
Kahlbaum, K. L. (1973). Catatonia (T. Pridan, Trans.). Baltimore: Johns
Hopkins University Press. (Original work published 1874)
Kahn, R. S., van Pragg, H. M., Wetzler, S., Asnis, G. M., & Barr, G.
(1988). Serotonin and anxiety revisited. Biological Psychiatry, 23, 189
208.
Kalin, N. H. (1993). The neurobiology of fear. Scientific American, 268(5),
94 101.
Kardiner, A., & Speigel, H. (1947). War stress and neurotic illness. New
York: Hoeber.
Kendler, K. S., Kessler, R. C., Neale, M. C., Heath, A. C., & Eaves, L. J.
(1993). The prediction of major depression in women: Toward an
integrated model. American Journal of Psychiatry, 150, 1139 1148.
1000
MOSKOWITZ
Kirby, G. H. (1913). The catatonic syndrome and its relation to manicdepressive insanity. Journal of Nervous & Mental Disease, 40, 694 704.
Klein, D. F. (1993). Panic may be a misfiring suffocation alarm. In S. A.
Montgomery (Ed.), Psychopharmacology of panic (Vol. 12, pp. 6773).
New York: Oxford University Press.
Klemm, W. R. (1971). Neurophysiologic studies of the immobility reflex
(animal hypnosis). Neurosciences Research, 4, 165212.
Klemm, W. R. (1989). Drug effects on active immobility responses: what
they tell us about neurotransmitter systems and motor functions.
Progress in Neurobiology, 32, 403 422.
Klemm, W. R. (2001). Behavioral arrest: In search of the neural control
system. Progress in Neurobiology, 65, 453 471.
Kraepelin, E. (1899). Psychiatrie: Ein Lehrbuch fur Studirende und Aerzte
(6th ed.) [Psychiatry: A textbook for students and physicians]. Leipzig,
Germany: Verlag von Johann Ambrosius Barth.
Krishnan, K. R. (2003). Comorbidity and depression treatment. Biological
Psychiatry, 53, 701706.
Kritzinger, P. R., & Jordaan, G. P. (2001). Catatonia: An open prospective
series with carbamazepine. International Journal of Neuropsychopharmacology, 4, 251257.
Krueger, S., & Braeunig, P. (2000). Catatonia in affective disorder: New
findings and a review of the literature. CNS Spectrums, 5(7), 48 53.
Krystal, H. (1993). Integration and self healing: Affect, trauma, alexithymia. Hillsdale, NJ: Analytic Press.
LeDoux, J. (1998). Fear and the brain: Where have we been, and where are
we going? Biological Psychiatry, 44, 1229 1238.
Lee, J. W., Schwartz, D. L., & Hallmayer, J. (2000). Catatonia in a
psychiatric intensive care facility: Incidence and response to benzodiazepines. Annals of Clinical Psychiatry, 12, 89 96.
Leite-Panissi, C. R. A., Coimbra, N. C., & Menescal-de-Oliveira, L.
(2003). The cholinergic stimulation of the central amygdala modifying
the tonic immobility response and antinociception in guinea pigs depends on the ventrolateral periaqueductal gray. Brain Research Bulletin,
60, 167178.
Leite-Panissi, C. R., Rodrigues, C. L., Brentegani, M. R., & Menescal-deOliveira, L. (2001). Endogenous opiate analgesia induced by tonic
immobility in guinea pigs. Brazilian Journal of Medical & Biological
Research, 34, 245250.
Lew, T. Y., & Tollefson, G. (1983). Chlorpromazine-induced neuroleptic
malignant syndrome and its response to diazepam. Biological Psychiatry, 18, 14411446.
Lingjaerde, O. (1963). Contributions to the study of schizophrenia and the
acute malignant deliria. Journal of Oslo City Hospital, 14, 43 83.
Ljubisavlijevic, V., & Schneider, P. (2002). Lethal catatonia. Australian &
New Zealand Journal of Psychiatry, 36, 563564.
Mahendra, B. (1981). Where have all the catatonics gone? Psychological
Medicine, 11, 669 671.
Malizia, A. L. (2000). Positron emitting ligands in the study of clinical
psychopharmacology of anxiety and anxiety disorders. Unpublished
masters thesis, University of Briston, Briston, England.
Malizia, A. L., Cunningham, V. J., Bell, C. J., Liddle, P. F., Jones, T., &
Nutt, D. J. (1998). Decreased brain GABA(A)-benzodiazepine receptor
binding in panic disorder: Preliminary results from a quantitative PET
study. Archives of General Psychiatry, 55, 715720.
Mann, S. C., Caroff, S. N., Bleier, H. R., Welz, W. K. R., Kling, M. A., &
Hayashida, M. (1986). Lethal catatonia. American Journal of Psychiatry,
143, 1374 1381.
Mann, S. C., Caroff, S. N., Keck, P. E., & Lazarus, A. (2003). Neuroleptic
malignant syndrome and related conditions (2nd ed.). Arlington, VA:
American Psychiatric Publishing.
Marks, I. M. (1987). Fears, phobias, and rituals: Panic, anxiety, and their
disorders. New York: Oxford University Press.
Marks, I. M., & Nesse, R. M. (1994). Fear and fitness: An evolutionary
analysis of anxiety disorders. Ethology and Sociobiology, 15, 247261.
McCall, W. V., Shelp, F. E., & McDonald, W. M. (1992). Controlled
investigation of the amobarbital interview for catatonic mutism [Comment]. American Journal of Psychiatry, 149, 202206.
McElroy, S. L., Altshuler, L. L., Suppes, T., Keck, P. E., Frye, M. A.,
Denicoff, K. D., et al. (2001). Axis I psychiatric comorbidity and its
relationship to historical illness variables in 288 patients with bipolar
disorder. American Journal of Psychiatry, 158, 420 426.
Menza, M. A., & Harris, D. (1989). Benzodiazepines and catatonia: An
overview. Biological Psychiatry, 26, 842 846.
Mills, A. D., & Faure, J.-M. (1991). Divergent selection for duration of
tonic immobility and social reinstatement behavior in Japanese quail
(Coturnix coturnix japonica) chicks. Journal of Comparative Psychology, 105, 2538.
Miu, A. C., & Olteanu, A. I. (2002). Catatonia in Alzheimers disease: The
role of the amygdalo-hippocampal circuits. Behavioral and Brain Sciences, 25, 588 589.
Monassi, C. R., Leite-Panissi, C. R., & Menescal-de-Oliveira, L. (1999).
Ventrolateral periaqueductal gray matter and the control of tonic immobility. Brain Research Bulletin, 50, 201208.
Mora, G. (1973). Introduction to Kahlbaums catatonia. Baltimore: Johns
Hopkins University Press.
Morrison, J. R. (1973). Catatonia: Retarded and excited types. Archives of
General Psychiatry, 28, 39 41.
Nadel, L., & Jacobs, W. J. (1996). The role of the Hippocampus in PTSD,
panic, and phobia. In N. Kato (Ed.), The hippocampus: Functions and
clinical relevance (pp. 455 463). Amsterdam: Elsevier Science.
Nash, R. F., Gallup, G. G., & Czech, D. A. (1976). Psychophysiological
correlates of tonic immobility in the domestic chicken (Gallus gallus).
Physiology & Behavior, 17, 413 418.
Nauta, W. J. H. (1971). The problem of the frontal lobe: A reinterpretation.
Journal of Psychiatric Research, 8, 167187.
Nauta, W. J. H. (1979). Expanding borders of the limbic system concept.
In R. Marino (Ed.), Functional neurosurgery (pp. 723). New York:
Raven Press.
Nesse, R. M. (2001). The smoke detector principle. Natural selection and
the regulation of defensive responses. In A. R. Damasio, A. Harrington,
J. Kagan, B. McEwen, H. Moss, & R. Shaikh (Eds.), Annals of the New
York Academy of Sciences: Vol. 935. Unity of knowledge: The convergence of natural and human science (pp. 75 85). New York: New York
Academy of Sciences.
Nesse, R. M., & Williams, G. C. (1994). Why we get sick: The new science
of Darwinian medicine. New York: Vintage.
Nijenhuis, E. R. S., Vanderlinden, J., & Spinhoven, P. (1998). Animal
defensive reactions as a model for trauma-induced dissociative reactions.
Journal of Traumatic Stress, 11, 243260.
Northoff, G. (2002). What catatonia can tell us about top-down modulation: A neuropsychiatric hypothesis. Behavioral and Brain Sciences,
25, 555 604.
Northoff, G., Braus, D. F., Sartorius, A., Khoram-Sefat, D., Russ, M.,
Eckert, J., et al. (1999). Reduced activation and altered laterality in two
neuroleptic naive catatonic patients during a motor task in functional
MRI. Psychological Medicine, 29, 9971002.
Northoff, G., Eckert, J., & Fritze, J. (1997). Glutamatergic dysfunction in
catatonia? Successful treatment of three acute akinetic catatonic patients
with the NMDA antagonist amantadine. Journal of Neurology, Neurosurgery & Psychiatry, 62, 404 406.
Northoff, G., Koch, A., Wenke, J., Eckert, J., Boeker, H., Pflug, B., &
Bogerts, B. (1999). Catatonia as a psychomotor syndrome: A rating scale
and extrapyramidal symptoms. Movement Disorders, 14, 404 416.
Northoff, G., Krill, W., Wenke, J., Gille, B., Russ, M., Eckert, J., et al.
(1998). Major differences in subjective experience of akinetic states in
catatonic and parkinsonian patients. Cognitive Neuropsychiatry, 3, 161
178.
Northoff, G., Richter, A., Gessner, M., Baumgart, F., Leschinger, A.,
CATATONIA AS A FEAR RESPONSE
Danos, P., et al. (in press). Alteration in orbitofrontal and prefrontal
cortical spatiotemporal activation pattern in catatonia during negative
emotional stimulation: A combined fMRI/MEG study. Schizophrenia
Bulletin.
Northoff, G., Richter, A., Gessner, M., Tempelmann, C., Bargel, B.,
Bogerts, B., & Heinze, H. J. (2001). GABA-eric modulation of prefrontal cortical spatiotemporal activation pattern: A fMRI-MEG study with
lorazepam challenge in catatonia. Schizophrenia Research, 49, 182.
Northoff, G., Steinke, R., Czcervenka, C., Krause, R., Ulrich, S., Danos, P.,
et al. (1999). Decreased density of GABA-A receptors in the left
sensorimotor cortex in akinetic catatonia: Investigation of in vivo benzodiazepine receptor binding. Journal of Neurology, Neurosurgery &
Psychiatry, 67, 445 450.
Northoff, G., Steinke, R., Krug, M., Cervenka, C., Pfennig, A., Otto, H., &
Bogerts, B. (1998). Left fronto-parietal dysfunction of GABA-A receptors and movement-related potentials in akinetic catatonia, a combined
SPECT- and MRP study. Schizophrenia Research, 29, 178.
Northoff, G., Steinke, R., Nagel, D., Czerwenka, C., Grosser, O., Danos,
P., et al. (2000). Right lower prefronto-parietal cortical dysfunction in
akinetic catatonia: A combined study of neuropsychology and regional
cerebral blood flow. Psychological Medicine, 30, 583596.
Northoff, G., Wenke, J., Demisch, L., Eckert, J., Gille, B., & Pflug, B.
(1995). Catatonia: short-term response to lorazepam and dopaminergic
metabolism. Psychopharmacology, 122, 182186.
Nutt, D. J., & Malizia, A. L. (2001). New insights into the role of the
GABA-A benzodiazepine receptor in psychiatric disorder. British Journal of Psychiatry, 179, 390 396.
Ohman, A. (1992). Fear and anxiety as emotional phenomena: Clinical,
phenomenological, evolutionary perspectives, and informationprocessing mechanisms. In M. Lewis & J. Haviland (Eds.), Handbook of
the emotions (pp. 511536). New York: Guilford Press.
Olsen, C. K., Hogg, S., & Lapiz, M. D. S. (2002). Tonic immobility in
guinea pigs: A behavioural response for detecting an anxiolytic-like
effect? Behavioural Pharmacology, 13, 261269.
Orland, R. M., & Daghestani, A. N. (1987). A case of catatonia induced by
bacterial meningoencephalitis. Journal of Clinical Psychiatry, 48, 489
490.
Oulis, P., Lykouras, L., Tomaras, V., Panayotopoulou, V., Gournellis, R.,
& Stefanis, C. (1997). DSM-IV catatonic features among psychiatric
inpatients: A preliminary study. European Psychiatry, 12, 412 414.
Peralta, V., & Cuesta, M. J. (2001). Motor features in psychotic disorders.
IIDevelopment of diagnostic criteria for catatonia. Schizophrenia Research, 47, 117126.
Peralta, V., Cuesta, M. J., Serrano, J. F., & Martinez-Larrea, J. A. (2001).
Classification issues in catatonia. European Archives of Psychiatry &
Clinical Neuroscience, 251(7), I14 I16.
Peralta, V., Cuesta, M. J., Serrano, J. F., & Mata, I. (1997). The Kahlbaum
syndrome: A study of its clinical validity, nosological status, and relationship with schizophrenia and mood disorder. Comprehensive Psychiatry, 38, 61 67.
Perkins, R. J. (1982). Catatonia: The ultimate response to fear? Australian
& New Zealand Journal of Psychiatry, 16, 282287.
Petrides, G., Divadeenam, K. M., Bush, G., & Francis, A. (1997). Synergism of lorazepam and electroconvulsive therapy in the treatment of
catatonia. Biological Psychiatry, 42, 375381.
Pfuhlmann, B., & Stoeber, G. (2001). The different conceptions of catatonia: Historical overview and critical discussion. European Archives of
Psychiatry & Clinical Neuroscience, 251(7), I4 I7.
Philbrick, K. L., & Rummans, T. A. (1994). Malignant catatonia. Journal
of Neuropsychiatry and Clinical Neurosciences, 6, 113.
Platek, S. M., & Gallup, G. G. (2002). A self frozen in time and space:
Catatonia as a kinesthetic analog to mirrored self-misidentification.
Behavioral and Brain Sciences, 25, 589 590.
Popkin, M. K., & Tucker, G. J. (1992). Secondary and drug-induced
1001
mood, anxiety, psychotic, catatonic, and personality disorders: A review
of the literature. Journal of Neuropsychiatry and Clinical Neurosciences, 4, 369 385.
Porges, S. W. (1995). Orienting in a defensive world: Mammalian modifications of our evolutionary heritage: A polyvagal theory. Psychophysiology, 32, 301318.
Porges, S. W. (1997). Emotion: An evolutionary by-product of the neural
regulation of the autonomic nervous system. In I. I. Lederhendler (Ed.),
Annals of The New York Academy of Sciences: Vol. 807. The integrative
neurobiology of affiliation (pp. 6277). New York: New York Academy
of Sciences.
Porges, S. W. (2001). The polyvagal theory: Phylogenetic substrates of a
social nervous system. International Journal of Psychophysiology, 42,
123146.
Porges, S. W., Doussard-Roosevelt, J. A., & Maita, A. K. (1994). Vagal
tone and the physiological regulation of emotion. Monographs of the
Society for Research in Child Development, 59, 250 283.
Post, R. M., Putnam, F., Contel, N. R., & Goldman, B. (1984). Electroconvulsive seizures inhibit amygdala kindling: implications for mechanisms of action in affective illness. Epilepsia, 25, 234 239.
Rager, D. R., Gallup, G. G., & Beckstead, J. W. (1986). Chlordiazepoxide
and tonic immobility: A paradoxical enhancement. Pharmacology, Biochemistry & Behavior, 25, 12371243.
Raitiere, M. N. (1986). Subcortical dysrhythmia and catatonia. Biological
Psychiatry, 21, 13511352.
Ramos, C., Leite-Panissi, R., Monassi, R., & Menescal-de-Oliveira, L.
(1999). Role of the amygdaloid nuclei in the modulation of tonic
immobility in guinea pigs. Physiology & Behavior, 67, 717724.
Rankel, H. W., & Rankel, L. E. (1988). Carbamazepine in the treatment of
catatonia. American Journal of Psychiatry, 145, 361362.
Rasmussen, K. G. (2003). Clinical applications of recent research on
electroconvulsive therapy. Bulletin of the Menninger Clinic, 67, 18 31.
Ratner, S. C. (1958). Hypnotic reactions of rabbits. Psychological Reports,
4, 209 210.
Ratner, S. C. (1967). Comparative aspects of hypnosis. In J. E. Gordon
(Ed.), Handbook of clinical and experimental hypnosis (pp. 550 587).
New York: Macmillan.
Ries, R. K. (1985). DSMIII implications of the diagnoses of catatonia and
bipolar disorder. American Journal of Psychiatry, 142, 14711474.
Robinson, M. D. (1998). Running from William James bear: A review of
preattentive mechanisms and their contributions to emotional experience. Cognition & Emotion, 12, 667 696.
Rohland, B. M., Carroll, B. T., & Jacoby, R. G. (1993). ECT in the
treatment of the catatonic syndrome. Journal of Affective Disorders, 29,
255261.
Rosebush, P. (2003). McMaster University faculty webpage. Retrieved
November 13, 2003, from: http://www.fhs.mcmaster.ca/psychiatryneuroscience/faculty/rosebush/index.html
Rosebush, P. I., Hildebrand, A. M., Furlong, B. G., & Mazurek, M. F.
(1990). Catatonic syndrome in a general psychiatric inpatient population: Frequency, clinical presentation, and response to lorazepam. Journal of Clinical Psychiatry, 51, 357362.
Rosebush, P. I., & Mazurek, M. F. (1999). Catatonia: Re-awakening to a
forgotten disorder. Movement Disorders, 14, 395397.
Rosebush, P., & Stewart, T. (1989). A prospective analysis of 24 episodes
of neuroleptic malignant syndrome. American Journal of Psychiatry,
146, 717725.
Sahar, T., Shalev, A. Y., & Porges, S. W. (2001). Vagal modulation of
responses to mental challenge in posttraumatic stress disorder. Biological Psychiatry, 49, 637 643.
Salam, S. A., Pillai, A. K., & Beresford, T. P. (1987). Lorazepam for
psychogenic catatonia. American Journal of Psychiatry, 144, 1082
1083.
Salva, P., & Costa, J. (1995). Clinical pharmacokinetics and pharmacody-
1002
MOSKOWITZ
namics of zolpidem. Therapeutic implications. Clinical Pharmacokinetics, 29, 142153.
Sanderson, W. C., Beck, A. T., & Beck, J. (1990). Syndrome comorbidity
in patients with major depression or dysthymia: Prevalence and temporal
relationships. American Journal of Psychiatry, 147, 10251028.
Sanderson, W. C., DiNardo, P. A., Rapee, R. M., & Barlow, D. H. (1990).
Syndrome comorbidity in patients diagnosed with a DSMIIIR anxiety
disorder. Journal of Abnormal Psychology, 99, 308 312.
Sargeant, A. B., & Eberhardt, L. E. (1975). Death feigning by ducks in
response to predation by red foxes (Vulpes fulva). American Midland
Naturalist, 94, 108 119.
Savodnik, I. (2002). The disease status of catatonia. Behavioral and Brain
Sciences, 25, 590 591.
Schmider, J., Standhart, H., Deuschle, M., Drancoli, J., & Heuser, I.
(1999). A double-blind comparison of lorazepam and oxazepam in
psychomotor retardation and mutism. Biological Psychiatry, 46, 437
441.
Schore, A. N. (1994). Affect regulation and the origin of the self: The
neurobiology of emotional development. Hillsdale, NJ: Erlbaum.
Schore, A. N. (2001). The effects of early relational trauma on right brain
development, affect regulation, and infant mental health. Infant Mental
Health Journal, 22, 201269.
Schore, A. N. (2002). Dysregulation of the right brain: A fundamental
mechanism of traumatic attachment and the psychopathogenesis of
posttraumatic stress disorder. Australian & New Zealand Journal of
Psychiatry, 36, 9 30.
Seligman, M. E. P. (1971). Phobias and preparedness. Behavior Therapy,
2, 307320.
Shalev, A., Hermesh, H., & Munitz, H. (1989). Mortality from neuroleptic
malignant syndrome. Journal of Clinical Psychiatry, 50, 18 25.
Starkstein, S. E., Petracca, G., Teson, A., Chemerinski, E., Merello, M.,
Migliorelli, R., & Leiguarda, R. (1996). Catatonia in depression: Prevalence, clinical correlates, and validation of a scale. Journal of Neurology, Neurosurgery & Psychiatry, 60, 326 332.
Stoeber, G., & Ungvari, G. S. (Eds.). (2001). [Special issue]. European
Archives of Psychiatry and Clinical Neurosciences, 251(Suppl. 1).
Suarez, S. D., & Gallup, G. G. (1979). Tonic immobility as a response to
rape in humans: A theoretical note. The Psychological Record, 29,
315320.
Svorad, D. (1957). Animal hypnosis (Totstellreflex) as experimental
model for psychiatry: Electroencephalographic and evolutionary aspect.
Archives of Neurology & Psychiatry, 77, 533539.
Takahashi, S., & Gjessing, L. R. (1972). Studies of periodic catatonia: IV.
Longitudinal study of catecholamine metabolism, with and without
drugs. Journal of Psychiatric Research, 9, 293314.
Tamam, L., & Ozpoyraz, N. (2002). Comorbidity of anxiety disorder
among patients with bipolar I disorder in remission. Psychopathology,
35, 203209.
Taylor, M. A. (1990). Catatonia: A review of a behavioral neurologic
syndrome. Neuropsychiatry Neuropsychology & Behavioral Neurology,
3, 48 72.
Taylor, M. A., & Fink, M. (2003). Catatonia in psychiatric classification:
A home of its own. American Journal of Psychiatry, 160, 12331241.
Thomas, P., Rascle, C., Mastain, B., Maron, M., & Vaiva, G. (1997). Test
for catatonia with zolpidem. Lancet, 349, 702.
Thompson, R. K. R., Foltin, R. W., Boylan, R. J., Sweet, A., Graves, C. A.,
& Lowitz, C. E. (1981). Tonic immobility in Japanese quail can reduce
the probability of sustained attack by cats. Animal Learning & Behavior,
9, 145149.
Tooby, J., & Cosmides, L. (1990). The past explains the present: Emotional
adaptations and the structure of ancestral environments. Ethology and
Sociobiology, 11, 375 424.
UK ECT Review Group. (2003). Efficacy and safety of electroconvulsive
therapy in depressive disorders: A systematic review and meta-analysis.
Lancet, 361, 799 808.
Ungvari, G. S., Chiu, H. F. K., Chow, L. Y., Lau, B. S. T., & Tang, W. K.
(1999). Lorazepam for chronic catatonia: A randomized, double-blind,
placebo-controlled cross-over study. Psychopharmacology, 142, 393
398.
Ungvari, G. S., Kau, L. S., Wai-Kwong, T., & Shing, N. F. (2001). The
pharmacological treatment of catatonia: An overview. European Archives of Psychiatry & Clinical Neuroscience, 251(Suppl. 1), I31I34.
Ungvari, G. S., Leung, H. C. M., & Lee, T. S. (1994). Benzodiazepines and
the psychopathology of catatonia. Pharmacopsychiatry, 27, 242245.
Ungvari, G. S., Leung, C. M., Wong, M. K., & Lau, J. (1994). Benzodiazepines in the treatment of catatonic syndrome. Acta Psychiatrica
Scandinavica, 89, 285288.
Wakefield, J. C. (1992). The concept of mental disorder: On the boundary
between biological facts and social values. American Psychologist, 47,
373388.
Wakefield, J. C. (1999). Evolutionary versus prototype analyses of the
concept of disorder. Journal of Abnormal Psychology, 108, 374 399.
Wetzel, H., Heuser, I., & Benkert, O. (1987). Stupor and affective state:
Alleviation of psychomotor disturbances by lorazepam and recurrence of
symptoms after Ro 15-1788. Journal of Nervous & Mental Disease, 175,
240 242.
Wetzel, H., Heuser, I., & Benkert, O. (1988). Benzodiazepines for catatonic symptoms, stupor, and mutism. Pharmacopsychiatry, 21, 394
395.
Whishaw, I. Q., Schallert, T., & Kolb, B. (1979). The thermal control of
immobility in developing infant rats: Is the neocortex involved? Physiology & Behavior, 23, 757762.
White, D. A. C. (1992). Catatonia and the neuroleptic malignant syndromeA single entity? British Journal of Psychiatry, 161, 558 560.
White, D. A. C., & Robins, A. H. (2000). An analysis of 17 catatonic
patients diagnosed with neuroleptic malignant syndrome. CNS Spectrums, 5(7), 58 65.
Young, L. T., Cooke, R. G., Robb, J. C., Levitt, A. J., & Joffe, R. T. (1993).
Anxious and non-anxious bipolar disorder. Journal of Affective Disorders, 29, 49 52.
Zaw, Z. F., & Bates, G. D. (1997). Replication of zolpidem test for
catatonia in an adolescent. Lancet, 349, 1914.
Zimmerman, M., Chelminski, I., & McDermut, W. (2002). Major depressive disorder and Axis I diagnostic comorbidity. Journal of Clinical
Psychiatry, 63, 187193.
Received December 15, 2002
Revision received September 6, 2003
Accepted October 28, 2003
Vous aimerez peut-être aussi
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Child Murder by Parents and Evolutionary PsychologyDocument15 pagesChild Murder by Parents and Evolutionary Psychologyeduardobar2000Pas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Relationship Between Dissociation and Voices: A Systematic Literature Review and Meta-AnalysisDocument52 pagesThe Relationship Between Dissociation and Voices: A Systematic Literature Review and Meta-Analysiseduardobar2000100% (1)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Borderline - An Adjective in Search of A NoumDocument8 pagesBorderline - An Adjective in Search of A Noumeduardobar2000Pas encore d'évaluation
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Hunger Genes: Pathways To ObesityDocument14 pagesThe Hunger Genes: Pathways To Obesityeduardobar2000Pas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Thrifty Psychiatric PhenotypeDocument3 pagesThe Thrifty Psychiatric Phenotypeeduardobar2000Pas encore d'évaluation
- Neural Control of Energy Balance: Translating Circuits To TherapiesDocument13 pagesNeural Control of Energy Balance: Translating Circuits To Therapieseduardobar2000Pas encore d'évaluation
- Nutrition: Applied Nutritional InvestigationDocument6 pagesNutrition: Applied Nutritional Investigationeduardobar2000Pas encore d'évaluation
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Relation of Obesity To Consummatory and Anticipatory Food RewardDocument25 pagesRelation of Obesity To Consummatory and Anticipatory Food Rewardeduardobar2000Pas encore d'évaluation
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Clinical Effectiveness and Costeffectiveness of Long-Term Weight Management Schemes For Adults: A Systematic ReviewDocument6 pagesThe Clinical Effectiveness and Costeffectiveness of Long-Term Weight Management Schemes For Adults: A Systematic Revieweduardobar2000Pas encore d'évaluation
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Ellness F T I O: Rom He Nside UtDocument5 pagesEllness F T I O: Rom He Nside UthbgossPas encore d'évaluation
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- 5AB 783651 CompleteBook R39 Jan12Document146 pages5AB 783651 CompleteBook R39 Jan12Gdb HassenePas encore d'évaluation
- Form Lplpo Pustu Dan PoskesdesDocument3 pagesForm Lplpo Pustu Dan PoskesdesristiPas encore d'évaluation
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Fractures NoteDocument31 pagesFractures NoteNoor AlblushiPas encore d'évaluation
- AH1N1 PPT PresentationDocument28 pagesAH1N1 PPT PresentationIna Isabela CostiboloPas encore d'évaluation
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Stroke PamphletDocument12 pagesStroke Pamphletapi-232971337Pas encore d'évaluation
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Ifosfamide Nephrotoxicity - UpToDateDocument7 pagesIfosfamide Nephrotoxicity - UpToDateZurya UdayanaPas encore d'évaluation
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- Summarised Clinchers Created For The Exam - Credits - Audi Maglalang-ReedDocument9 pagesSummarised Clinchers Created For The Exam - Credits - Audi Maglalang-ReedflashjetPas encore d'évaluation
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- SIPDocument2 pagesSIPRowena Abdula BaronaPas encore d'évaluation
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Gap AnalysisDocument9 pagesGap Analysisapi-706947027Pas encore d'évaluation
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Development of A Taste-Masked Orodispersible FilmDocument12 pagesDevelopment of A Taste-Masked Orodispersible FilmKhoa DuyPas encore d'évaluation
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Q1 Health Status QuestionnaireDocument2 pagesQ1 Health Status QuestionnaireKathleen ChuaPas encore d'évaluation
- Laporan Iud 2019Document91 pagesLaporan Iud 2019Yuli AntiPas encore d'évaluation
- Consent ModelDocument4 pagesConsent ModelSundaresan ChockalingamPas encore d'évaluation
- Validity and Reliability Study of The Turkish Version of Ego Identity Process QuestionairreDocument6 pagesValidity and Reliability Study of The Turkish Version of Ego Identity Process QuestionairreSergio F. GonzalezPas encore d'évaluation
- Manual Aromaterapia Español PDFDocument60 pagesManual Aromaterapia Español PDFPablo Andrés Mora SolísPas encore d'évaluation
- Written Assignment Unit 2 - HS 2212Document5 pagesWritten Assignment Unit 2 - HS 2212bnvjPas encore d'évaluation
- Nupa BrochureDocument1 pageNupa BrochureLaboule KimozackPas encore d'évaluation
- Women Devlopment-Government Policies and ProgrammesDocument19 pagesWomen Devlopment-Government Policies and ProgrammesVishalMishraPas encore d'évaluation
- 2022 Projects City of BethlehemDocument17 pages2022 Projects City of BethlehemLVNewsdotcomPas encore d'évaluation
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Discursive StudiesDocument11 pagesDiscursive StudiesSohag LTCPas encore d'évaluation
- Final Brochure 23rd AprilDocument24 pagesFinal Brochure 23rd AprilPreethi sureshPas encore d'évaluation
- Prevention and Control of Infectious Disease Act 1988Document16 pagesPrevention and Control of Infectious Disease Act 1988smuf_2Pas encore d'évaluation
- Readycult Coliforms 100: Ordering Number: 1.01298.0001Document4 pagesReadycult Coliforms 100: Ordering Number: 1.01298.0001Maria Alejandra VillalbaPas encore d'évaluation
- Hematinics: Dr. Monalisa Mondal Demonstrator Department of PharmacologyDocument28 pagesHematinics: Dr. Monalisa Mondal Demonstrator Department of PharmacologyShirsh JauriharPas encore d'évaluation
- Brain Tumors - KY Cancer RegistryDocument45 pagesBrain Tumors - KY Cancer RegistryMohammad Galih PratamaPas encore d'évaluation
- Nitroimidazole Wps OfficeDocument10 pagesNitroimidazole Wps OfficeCamelle DiniayPas encore d'évaluation
- Allocating Hospital Resources To Improve Patient ExperienceDocument6 pagesAllocating Hospital Resources To Improve Patient ExperienceMichael0% (1)
- 80020120LITPDFDocument37 pages80020120LITPDFPraistonPas encore d'évaluation
- 10 1007@s00068-mfjrbtDocument14 pages10 1007@s00068-mfjrbtJGunar VasquezPas encore d'évaluation
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)