Académique Documents
Professionnel Documents
Culture Documents
7 Gastrointestinalsystemfull 120226085536 Phpapp01
Transféré par
didikekoCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
7 Gastrointestinalsystemfull 120226085536 Phpapp01
Transféré par
didikekoDroits d'auteur :
Formats disponibles
1
Gastrointestinal System
Introduction to the gastrointestinal system
Basic structure of the gastrointestinal system
Individual components of the gastrointestinal system
o
o
o
o
o
o
o
o
o
Oral cavity
Salivary glands
Oesophagus
Stomach
Small intestine
Large intestine
Liver
Gall bladder
Pancreas
Introduction to the gastrointestinal system
The gastrointestinal tract (GIT) consists of a hollow muscular tube starting
from the oral cavity, where food enters the mouth, continuing through the
pharynx, oesophagus, stomach and intestines to the rectum and anus, where
food is expelled. There are various accessory organs that assist the tract
by secreting enzymes to help break down food into its component nutrients.
Thus the salivary glands, liver, pancreas and gall bladder have important
functions in the digestive system. Food is propelled along the length of the
GIT by peristaltic movements of the muscular walls.
The primary purpose of the gastrointestinal tract is to break food down into
nutrients, which can be absorbed into the body to provide energy. First food
must be ingested into the mouth to be mechanically processed and
moistened. Secondly, digestion occurs mainly in the stomach and small
intestine where proteins, fats and carbohydrates are chemically broken down
into their basic building blocks. Smaller molecules are then absorbed across
the epithelium of the small intestine and subsequently enter the circulation.
The large intestine plays a key role in reabsorbing excess water. Finally,
undigested material and secreted waste products are excreted from the body
via defecation (passing of faeces).
In the case of gastrointestinal disease or disorders, these functions of the
gastrointestinal tract are not achieved successfully. Patients may develop
symptoms of nausea, vomiting, diarrhoea, malabsorption, constipation or
obstruction. Gastrointestinal problems are very common and most people
will have experienced some of the above symptoms several times
throughout their lives.
Basic structure
The gastrointestinal tract is a muscular tube lined by a special layer of cells,
called epithelium. The contents of the tube are considered external to the
body and are in continuity with the outside world at the mouth and the anus.
Although each section of the tract has specialised functions, the entire tract
has a similar basic structure with regional variations.
The wall is divided into four layers as follows:
Mucosa : The innermost layer of the digestive tract has specialised epithelial
cells supported by an underlying connective tissue layer called the lamina
propria. The lamina propria contains blood vessels, nerves, lymphoid tissue
and glands that support the mucosa. Depending on its function, the
epithelium may be simple (a single layer) or stratified (multiple layers).
Areas such as the mouth and oesophagus are covered by a stratified
squamous (flat) epithelium so they can survive the wear and tear of passing
food. Simple columnar (tall) or glandular epithelium lines the stomach and
intestines to aid secretion and absorption. The inner lining is constantly shed
and replaced, making it one of the most rapidly dividing areas of the body!
Beneath the lamina propria is the muscularis mucosa. This comprises layers
of smooth muscle which can contract to change the shape of the lumen.
Submucosa: The submucosa surrounds the muscularis mucosa and consists
of fat, fibrous connective tissue and larger vessels and nerves. At its outer
margin there is a specialized nerve plexus called the submucosal plexus or
Meissner plexus. This supplies the mucosa and submucosa.
Muscularis externa: This smooth muscle layer has inner circular and outer
longitudinal layers of muscle fibres separated by the myenteric plexus or
Auerbach plexus. Neural innervations control the contraction of these
muscles and hence the mechanical breakdown and peristalsis of the food
within the lumen.
Serosa/mesentery: The outer layer of the GIT is formed by fat and another
layer of epithelial cells called mesothelium.
Individual components of the gastrointestinal system
Oral cavity: The oral cavity or mouth is responsible for the intake of food. It
is lined by a stratified squamous oral mucosa with keratin covering those
areas subject to significant abrasion, such as the tongue, hard palate and
roof of the mouth. Mastication refers to the mechanical breakdown of food by
chewing and chopping actions of the teeth. The tongue, a strong muscular
organ, manipulates the food bolus to come in contact with the teeth. It is
also the sensing organ of the mouth for touch, temperature and taste using
its specialised sensors known as papillae.
Insalivation refers to the mixing of the oral cavity contents with salivary
gland secretions. The mucin (a glycoprotein) in saliva acts as a lubricant. The
oral cavity also plays a limited role in the digestion of carbohydrates. The
enzyme serum amylase, a component of saliva, starts the process of
digestion of complex carbohydrates. The final function of the oral cavity is
absorption of small molecules such as glucose and water, across the mucosa.
From the mouth, food passes through the pharynx and oesophagus via the
action of swallowing.
Salivary glands: Three pairs of salivary glands communicate with the oral
cavity. Each is a complex gland with numerous acini lined by secretory
epithelium. The acini secrete their contents into specialised ducts. Each
gland is divided into smaller segments called lobes. Salivation occurs in
response to the taste, smell or even appearance of food. This occurs due to
nerve signals that tell the salivary glands to secrete saliva to prepare and
moisten the mouth. Each pair of salivary glands secretes saliva with slightly
different compositions.
Parotids: The parotid glands are large, irregular shaped glands located
under the skin on the side of the face. They secrete 25% of saliva. They are
situated below the zygomatic arch (cheekbone) and cover part of the
mandible (lower jaw bone). An enlarged parotid gland can be easier felt
when one clenches their teeth. The parotids produce a watery secretion
which is also rich in proteins. Immunoglobins are secreted help to fight
microorganisms and a-amylase proteins start to break down complex
carbohydrates.
Submandibular: The submandibular glands secrete 70% of the saliva in the
mouth. They are found in the floor of the mouth, in a groove along the inner
surface of the mandible. These glands produce a more viscid (thick)
secretion, rich in mucin and with a smaller amount of protein. Mucin is a
glycoprotein that acts as a lubricant.
Sublingual: The sublinguals are the smallest salivary glands, covered by a
thin layer of tissue at the floor of the mouth. They produce approximately 5%
of the saliva and their secretions are very sticky due to the large
concentration of mucin. The main functions are to provide buffers and
lubrication.
Oesophagus: The oesophagus is a muscular tube of approximately 25cm in
length and 2cm in diameter. It extends from the pharynx to the stomach
after passing through an opening in the diaphragm. The wall of the
oesophagus is made up of inner circular and outer longitudinal layers of
muscle that are supplied by the oesophageal nerve plexus. This nerve plexus
surrounds the lower portion of the oesophagus. The oesophagus functions
primarily as a transport medium between compartments.
Stomach: The stomach is a J shaped expanded bag, located just left of the
midline between the oesophagus and small intestine. It is divided into four
main regions and has two borders called the greater and lesser curvatures.
The first section is the cardia which surrounds the cardial orifice where the
oesophagus enters the stomach. The fundus is the superior, dilated portion
of the stomach that has contact with the left dome of the diaphragm. The
body is the largest section between the fundus and the curved portion of the
J.
This is where most gastric glands
are located and where most mixing of the food occurs. Finally the pylorus is
the curved base of the stomach. Gastric contents are expelled into the
proximal duodenum via the pyloric sphincter. The inner surface of the
stomach is contracted into numerous longitudinal folds called rugae. These
allow the stomach to stretch and expand when food enters. The stomach can
hold up to 1.5 litres of material. The functions of the stomach include:
1. The short-term storage of ingested food.
2. Mechanical breakdown of food by churning and mixing motions.
3. Chemical digestion of proteins by acids and enzymes.
4. Stomach acid kills bugs and germs.
5. Some absorption of substances such as alcohol.
Most of these functions are achieved by the secretion of stomach juices by
gastric glands in the body and fundus. Some cells are responsible for
secreting acid and others secrete enzymes to break down proteins.
Small intestine: The small intestine is composed of the duodenum,
jejunum, and ileum. It averages approximately 6m in length, extending from
the pyloric sphincter of the stomach to the ileo-caecal valve separating the
ileum from the caecum. The small intestine is compressed into numerous
folds and occupies a large proportion of the abdominal cavity.
The duodenum is the proximal C-shaped section that curves around the head
of the pancreas. The duodenum serves a mixing function as it combines
digestive secretions from the pancreas and liver with the contents expelled
from the stomach. The start of the jejunum is marked by a sharp bend, the
duodenojejunal flexure. It is in the jejunum where the majority of digestion
and absorption occurs. The final portion, the ileum, is the longest segment
and empties into the caecum at the ileocaecal junction.
The small intestine performs the majority of digestion and absorption of
nutrients. Partly digested food from the stomach is further broken down by
enzymes from the pancreas and bile salts from the liver and gallbladder.
These secretions enter the duodenum at the Ampulla of Vater. After further
digestion, food constituents such as proteins, fats, and carbohydrates are
broken down to small building blocks and absorbed into the body's blood
stream.
The lining of the small intestine is made up of numerous permanent folds
called plicae circulares. Each plica has numerous villi (folds of mucosa) and
each villus is covered by epithelium with projecting microvilli (brush border).
This increases the surface area for absorption by a factor of several hundred.
The mucosa of the small intestine contains several specialised cells. Some
are responsible for absorption, whilst others secrete digestive enzymes and
mucous to protect the intestinal lining from digestive actions.
Large intestine: The large intestine is horse-shoe shaped and extends
around the small intestine like a frame. It consists of the appendix, caecum,
ascending, transverse, descending and sigmoid colon, and the rectum. It has
a length of approximately 1.5m and a width of 7.5cm.
The caecum is the expanded pouch that receives material from the ileum
and starts to compress food products into faecal material. Food then travels
along the colon. The wall of the colon is made up of several pouches
(haustra) that are held under tension by three thick bands of muscle (taenia
coli).
The rectum is the final 15cm of the large intestine. It expands to hold faecal
matter before it passes through the anorectal canal to the anus. Thick bands
of muscle, known as sphincters, control the passage of faeces.
10
The mucosa of the large intestine lacks villi seen in the small intestine. The
mucosal surface is flat with several deep intestinal glands. Numerous goblet
cells line the glands that secrete mucous to lubricate faecal matter as it
solidifies. The functions of the large intestine can be summarised as:
1. The accumulation of unabsorbed material to form faeces.
2. Some digestion by bacteria. The bacteria are responsible for the
formation of intestinal gas.
3. Reabsorption of water, salts, sugar and vitamins.
Liver: The liver is a large, reddish-brown organ situated in the right upper
quadrant of the abdomen. It is surrounded by a strong capsule and divided
into four lobes namely the right, left, caudate and quadrate lobes. The liver
has several important functions. It acts as a mechanical filter by filtering
blood that travels from the intestinal system. It detoxifies several
metabolites including the breakdown of bilirubin and oestrogen. In addition,
the liver has synthetic functions, producing albumin and blood clotting
factors. However, its main roles in digestion are in the production of bile and
metabolism of nutrients. All nutrients absorbed by the intestines pass
through the liver and are processed before traveling to the rest of the body.
The bile produced by cells of the liver, enters the intestines at the
duodenum. Here, bile salts break down lipids into smaller particles so there is
a greater surface area for digestive enzymes to act.
Gall bladder: The gallbladder is a hollow, pear shaped organ that sits in a
depression on the posterior surface of the liver's right lobe. It consists of a
fundus, body and neck. It empties via the cystic duct into the biliary duct
system. The main functions of the gall bladder are storage and concentration
of bile. Bile is a thick fluid that contains enzymes to help dissolve fat in the
intestines. Bile is produced by the liver but stored in the gallbladder until it is
needed. Bile is released from the gall bladder by contraction of its muscular
11
walls in response to hormone signals from the duodenum in the presence of
food.
Pancreas: Finally, the pancreas is a lobular, pinkish-grey organ that lies
behind the stomach. Its head communicates with the duodenum and its tail
extends to the spleen. The organ is approximately 15cm in length with a
long, slender body connecting the head and tail segments. The pancreas has
both exocrine and endocrine functions. Endocrine refers to production of
hormones which occurs in the Islets of Langerhans. The Islets produce
insulin, glucagon and other substances and these are the areas damaged in
diabetes mellitus. The exocrine (secretrory) portion makes up 80-85% of the
pancreas and is the area relevant to the gastrointestinal tract.
It is made up of numerous acini (small glands) that secrete contents into
ducts which eventually lead to the duodenum. The pancreas secretes fluid
rich in carbohydrates and inactive enzymes. Secretion is triggered by the
hormones released by the duodenum in the presence of food. Pancreatic
enzymes include carbohydrases, lipases, nucleases and proteolytic enzymes
that can break down different components of food. These are secreted in an
inactive form to prevent digestion of the pancreas itself. The enzymes
become active once they reach the duodenum.
Vous aimerez peut-être aussi
- Human PhysiologyDocument444 pagesHuman PhysiologyAnas AhmedhPas encore d'évaluation
- Digestive System Anatomy and PhysiologyDocument18 pagesDigestive System Anatomy and PhysiologyKBDPas encore d'évaluation
- Digestive SystemDocument73 pagesDigestive Systemsnp88Pas encore d'évaluation
- The Digestive SystemDocument44 pagesThe Digestive SystemJoy NatividadPas encore d'évaluation
- Anatomy and Physiology of Gastrointestinal TractDocument20 pagesAnatomy and Physiology of Gastrointestinal TractKrupa Jyothirmai100% (1)
- Essay ModelDocument4 pagesEssay ModelEmma MalekPas encore d'évaluation
- Intestinal Diseases, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsD'EverandIntestinal Diseases, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsPas encore d'évaluation
- Clinical Evaluation and Management of Spasticity PDFDocument397 pagesClinical Evaluation and Management of Spasticity PDFRicardo Pedro100% (1)
- DIGESTIVE Lecture Notes PDFDocument20 pagesDIGESTIVE Lecture Notes PDFAaliya Minar100% (4)
- Concise Guide To Forgetting How Much You SuckDocument7 pagesConcise Guide To Forgetting How Much You SuckihatemakingusernamesPas encore d'évaluation
- Anatomy and PhysiologyDocument7 pagesAnatomy and PhysiologyMarkAnthonyFallorinaPas encore d'évaluation
- Digestive SystemDocument25 pagesDigestive SystemHerry HermawanPas encore d'évaluation
- Science Project - Digestive SystemDocument28 pagesScience Project - Digestive Systemapi-35222133565% (17)
- GERD (Gastroesophageal Reflux Disease)Document112 pagesGERD (Gastroesophageal Reflux Disease)Mharj Alfelor Cecilio100% (7)
- Anatomy and Physiology:gastrointestinal Tract Powerpoint PresentationDocument28 pagesAnatomy and Physiology:gastrointestinal Tract Powerpoint PresentationKatherine 'Chingboo' Leonico Laud100% (15)
- NCMB 316 M1 Cu1Document23 pagesNCMB 316 M1 Cu1Maica Lectana100% (1)
- Digestive System DraftDocument39 pagesDigestive System DraftDiosa BakingPas encore d'évaluation
- Your Super Gut Feeling Restored – How to Restore Your Life Energy and Overall Health from The Inside OutD'EverandYour Super Gut Feeling Restored – How to Restore Your Life Energy and Overall Health from The Inside OutPas encore d'évaluation
- Basic First Aid TrainingDocument32 pagesBasic First Aid Trainingtukaram patilPas encore d'évaluation
- 2016 PAD ACC+AHA SlidesDocument74 pages2016 PAD ACC+AHA SlidesPonpimol Odee BongkeawPas encore d'évaluation
- Digestive System Anatomy and Physiology - NurseslabsDocument33 pagesDigestive System Anatomy and Physiology - NurseslabsMari FePas encore d'évaluation
- EsophagogastroduodenosDocument34 pagesEsophagogastroduodenosAngela Beatriz Dela Vega100% (1)
- Anatomy and Physiology: Gastrointestinal TractDocument15 pagesAnatomy and Physiology: Gastrointestinal TractninrosePas encore d'évaluation
- Anatomy:: Basic StructureDocument7 pagesAnatomy:: Basic StructureCharish Dwayne Bautista PondalesPas encore d'évaluation
- Introduction To The Gastrointestinal SystemDocument10 pagesIntroduction To The Gastrointestinal Systemjaninesimbol24Pas encore d'évaluation
- Introduction To The Gastrointestinal SystemDocument10 pagesIntroduction To The Gastrointestinal Systemjaninesimbol24Pas encore d'évaluation
- Anatomy AND Physiology: (Gastrointestinal System)Document6 pagesAnatomy AND Physiology: (Gastrointestinal System)Antonette LeiPas encore d'évaluation
- Digestive System Anatomy PhysiologyDocument20 pagesDigestive System Anatomy PhysiologyKids JangPas encore d'évaluation
- Functions of The Digestive SystemDocument8 pagesFunctions of The Digestive SystemPOTENCIANA MAROMAPas encore d'évaluation
- Karthik Bharadwaj'S: PresentationDocument32 pagesKarthik Bharadwaj'S: PresentationMahir AfranPas encore d'évaluation
- Digestive System 258754Document17 pagesDigestive System 258754Musharaf RehmanPas encore d'évaluation
- A & PDocument2 pagesA & PSahil KulkarniPas encore d'évaluation
- CORRECHE HA12Unit9NotesDocument8 pagesCORRECHE HA12Unit9NotesleiannbellecorrechePas encore d'évaluation
- BIO Lect Powerpoint InfoDocument18 pagesBIO Lect Powerpoint InfoEarl ReyesPas encore d'évaluation
- TomdDocument15 pagesTomdduinnemerriedithcastroPas encore d'évaluation
- Human Digestive System - Grade 11 & 12Document23 pagesHuman Digestive System - Grade 11 & 12Ishita SinghPas encore d'évaluation
- Chapter22notes DIGESTIONDocument42 pagesChapter22notes DIGESTIONpancit cantonPas encore d'évaluation
- The Digestive System 1Document28 pagesThe Digestive System 1AnnPas encore d'évaluation
- Review Digestive SystemDocument7 pagesReview Digestive Systemcaryl james faith abrenicaPas encore d'évaluation
- GI - Anatomy To DiagnosticsDocument39 pagesGI - Anatomy To DiagnosticsIvan FernandezPas encore d'évaluation
- AnaPhy - Digestive SystemDocument5 pagesAnaPhy - Digestive SystemJan Mark SotoPas encore d'évaluation
- Anatomy Digestive SystemDocument6 pagesAnatomy Digestive SystemcristinejoyfernandoPas encore d'évaluation
- Physiology, Gastrointestinal Article - StatPearls PDFDocument5 pagesPhysiology, Gastrointestinal Article - StatPearls PDFThanh TrúcPas encore d'évaluation
- Digestive System: Human AnatomyDocument42 pagesDigestive System: Human Anatomycristobal melegritoPas encore d'évaluation
- Strategic Intervention Material: Dig Esti Ve Syst emDocument16 pagesStrategic Intervention Material: Dig Esti Ve Syst emKarla Javier PadinPas encore d'évaluation
- Definition of TermsDocument3 pagesDefinition of TermsJoanne Sianson BucayanPas encore d'évaluation
- Unit 8 The Digestive System: Learning OutcomesDocument12 pagesUnit 8 The Digestive System: Learning OutcomesDeolita BadiangPas encore d'évaluation
- Digestion and AbsorptionDocument82 pagesDigestion and AbsorptionCoc FanPas encore d'évaluation
- Human Anatomy The Gastrointestinal TractDocument53 pagesHuman Anatomy The Gastrointestinal TractGadzikaPas encore d'évaluation
- Unit Ten: Digestive SystemDocument9 pagesUnit Ten: Digestive SystemKath RubioPas encore d'évaluation
- Caballero DigestiveDocument5 pagesCaballero DigestiveClairyssa Myn D CaballeroPas encore d'évaluation
- BIO 1133 Exercise 9 (Digestive Sytem of The Frog)Document6 pagesBIO 1133 Exercise 9 (Digestive Sytem of The Frog)Tonet LapePas encore d'évaluation
- Clase 10-16-2015Document9 pagesClase 10-16-2015jv9937Pas encore d'évaluation
- Digestive System.: Nur112: Anatomy and Physiology ISU Echague - College of NursingDocument9 pagesDigestive System.: Nur112: Anatomy and Physiology ISU Echague - College of NursingWai KikiPas encore d'évaluation
- Digestive SystemDocument7 pagesDigestive Systemmaria del carmen rodriguez garridoPas encore d'évaluation
- Digestive SystemDocument47 pagesDigestive SystemKhant Si ThuPas encore d'évaluation
- Digestive System AnatomyDocument11 pagesDigestive System AnatomyYeni Jesika SilitongaPas encore d'évaluation
- Study Guide 1 Assessment of Digestive and Gastrointestinal Function and Treatment ModalitiesDocument10 pagesStudy Guide 1 Assessment of Digestive and Gastrointestinal Function and Treatment ModalitiesKc Cabanilla LizardoPas encore d'évaluation
- Pemicu 1 Blok GIT: Theffany 405120198 Fakultas Kedokteran Universitas TarumanagaraDocument99 pagesPemicu 1 Blok GIT: Theffany 405120198 Fakultas Kedokteran Universitas TarumanagaraTheffany KasiranPas encore d'évaluation
- GastronotesDocument50 pagesGastronotesLibi FarrellPas encore d'évaluation
- Digestion and AbsorptionDocument7 pagesDigestion and AbsorptionlalitPas encore d'évaluation
- Digestive System - Lecture GuideDocument11 pagesDigestive System - Lecture GuideJEFFERSON ANDAYAPas encore d'évaluation
- Flow and Parts of The Digestive SystemDocument52 pagesFlow and Parts of The Digestive SystemKAnn RuedasPas encore d'évaluation
- Anatomy and Physiology DigestiveDocument7 pagesAnatomy and Physiology DigestiveFretzgine Lou ManuelPas encore d'évaluation
- Dara NewDocument48 pagesDara NewdidikekoPas encore d'évaluation
- Cholangitis Pathway 2014Document1 pageCholangitis Pathway 2014didikekoPas encore d'évaluation
- Colonization With Methicillin-Resistant Staphylococcus: Aureus After Liver TransplantationDocument7 pagesColonization With Methicillin-Resistant Staphylococcus: Aureus After Liver TransplantationdidikekoPas encore d'évaluation
- Pre Op MRSA Screening 2010Document5 pagesPre Op MRSA Screening 2010didikekoPas encore d'évaluation
- Co 631Document7 pagesCo 631didikekoPas encore d'évaluation
- Corelation Between TBC and HIVDocument8 pagesCorelation Between TBC and HIVdidikekoPas encore d'évaluation
- Rural Indonesia Women 'S Traditional Beliefs About Antenatal CareDocument8 pagesRural Indonesia Women 'S Traditional Beliefs About Antenatal CaredidikekoPas encore d'évaluation
- Article - Rapid Endovascular Treatmenrt of Ischemic StrokeDocument12 pagesArticle - Rapid Endovascular Treatmenrt of Ischemic StrokeIgnatius BramPas encore d'évaluation
- Acromioclavicular Joint InstabilityDocument1 pageAcromioclavicular Joint InstabilitydidikekoPas encore d'évaluation
- Nutrition Noteworthy, 4 (1) Garcia, Marcela EsperanzaDocument7 pagesNutrition Noteworthy, 4 (1) Garcia, Marcela EsperanzadidikekoPas encore d'évaluation
- Pengaruh Pendidikan Kesehatan Tentang 3 M Terhadap SikapDocument4 pagesPengaruh Pendidikan Kesehatan Tentang 3 M Terhadap SikapdidikekoPas encore d'évaluation
- Neuromuscular Blocking AgentsDocument89 pagesNeuromuscular Blocking Agentslorenzo08Pas encore d'évaluation
- DA Sistemik TerapiDocument11 pagesDA Sistemik TerapiariyatiPas encore d'évaluation
- Monograph On Lung Cancer July14Document48 pagesMonograph On Lung Cancer July14PatPas encore d'évaluation
- Datasheet Reagent SansureDocument3 pagesDatasheet Reagent Sansuredanang setiawanPas encore d'évaluation
- The Effects of Virus Variants On COVID-19 Vaccines: Inglés Nivel II Examen FinalDocument4 pagesThe Effects of Virus Variants On COVID-19 Vaccines: Inglés Nivel II Examen FinalDIEGOPas encore d'évaluation
- Glove Utilization in The Prevention of Cross Transmission - A Systematic Review 2015Document12 pagesGlove Utilization in The Prevention of Cross Transmission - A Systematic Review 2015CTPas encore d'évaluation
- Figo Misoprostol IufdDocument0 pageFigo Misoprostol IufdAntoni KurniawanPas encore d'évaluation
- Opalescence Boost Whitening PDFDocument2 pagesOpalescence Boost Whitening PDFVikas AggarwalPas encore d'évaluation
- Nguyen 2019Document6 pagesNguyen 2019ClintonPas encore d'évaluation
- Claim IntimationDocument2 pagesClaim IntimationSyed's Way PoolPas encore d'évaluation
- IAA Protein Conjugadotes 2008Document6 pagesIAA Protein Conjugadotes 2008shady182Pas encore d'évaluation
- ElectrocardiogramDocument17 pagesElectrocardiogramvinnu kalyanPas encore d'évaluation
- UntitledDocument75 pagesUntitledMelissa DrakePas encore d'évaluation
- Presentation On Hysterosalpingography: BY Mahmud M Alkali I.D: 12/01/09/069 Radiography, Unimaid. 2014/2015 SESSIONDocument23 pagesPresentation On Hysterosalpingography: BY Mahmud M Alkali I.D: 12/01/09/069 Radiography, Unimaid. 2014/2015 SESSIONMubarak M AlkaliPas encore d'évaluation
- Primary Health Care Notes Health What Is Illness and Causes of Illness?Document22 pagesPrimary Health Care Notes Health What Is Illness and Causes of Illness?Nano KaPas encore d'évaluation
- Orofacial CleftsDocument19 pagesOrofacial CleftsTj AngelaPas encore d'évaluation
- Pioped PDFDocument7 pagesPioped PDFaiPas encore d'évaluation
- Big Data Final ReportDocument34 pagesBig Data Final Reportclinfox100% (2)
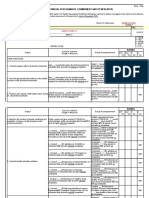
- Individual Performance Commitment and Review (Ipcr) : Name of Employee: Approved By: Date Date FiledDocument12 pagesIndividual Performance Commitment and Review (Ipcr) : Name of Employee: Approved By: Date Date FiledTiffanny Diane Agbayani RuedasPas encore d'évaluation
- COVID 19 Guideline To Resume Paediatric Dental Services in MalaysiaDocument29 pagesCOVID 19 Guideline To Resume Paediatric Dental Services in MalaysiaEnrita DianPas encore d'évaluation
- Hazard Identification and Risk AssesmentDocument4 pagesHazard Identification and Risk AssesmentsuyatnofkmundipPas encore d'évaluation
- ABUUU (AutoRecovered)Document14 pagesABUUU (AutoRecovered)Tariku TadesaPas encore d'évaluation
- Principles of Inheritance and Variations MCQs IDocument13 pagesPrinciples of Inheritance and Variations MCQs IMahendhiran MariappanPas encore d'évaluation